- 1British Heart Foundation Centre of Research Excellence, School of Cardiovascular Medicine and Sciences, King’s College London, London, United Kingdom
- 2King’s College Hospital NHS Foundation Trust, London, United Kingdom
Aim: Acute myocarditis (AM) is a heterogeneous condition with variable estimates of survival. Contemporary criteria for the diagnosis of clinically suspected AM enable non-invasive assessment, resulting in greater sensitivity and more representative cohorts. We aimed to describe the demographic characteristics and long-term outcomes of patients with AM diagnosed using non-invasive criteria.
Methods and results: A total of 199 patients with cardiac magnetic resonance (CMR)-confirmed AM were included. The majority (n = 130, 65%) were male, and the average age was 39 ± 16 years. Half of the patients were White (n = 99, 52%), with the remainder from Black and Minority Ethnic (BAME) groups. The most common clinical presentation was chest pain (n = 156, 78%), with smaller numbers presenting with breathlessness (n = 25, 13%) and arrhythmias (n = 18, 9%). Patients admitted with breathlessness were sicker and more often required inotropes, steroids, and renal replacement therapy (p < 0.001, p < 0.001, and p = 0.01, respectively). Over a median follow-up of 53 (IQR 34–76) months, 11 patients (6%) experienced an adverse outcome, defined as a composite of all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy. Patients in the arrhythmia group had a worse prognosis, with a nearly sevenfold risk of adverse events [hazard ratio (HR) 6.97; 95% confidence interval (CI) 1.87–26.00, p = 0.004]. Sex and ethnicity were not significantly associated with the outcome.
Conclusion: AM is highly heterogeneous with an overall favourable prognosis. Three-quarters of patients with AM present with chest pain, which is associated with a benign prognosis. AM presenting with life-threatening arrhythmias is associated with a higher risk of adverse events.
Introduction
Acute myocarditis (AM) is an inflammatory disease of the myocardium occurring most commonly after viral infection, autoimmune disease, or exposure to toxins (1–3). It is characterised by a heterogeneous clinical presentation, ranging from subclinical or minimally symptomatic forms to a life-threatening fulminant presentation with cardiogenic shock or cardiac arrest (4–6).
Early studies of AM mostly included patients with endomyocardial biopsy (EMB)-confirmed AM and suggested a relatively high mortality rate (∼25% at 5 years) (7–11). However, EMB is invasive and therefore reserved for more severe cases, and these studies are likely to have selected more high-risk patients. Recent studies, using cardiovascular magnetic resonance (CMR) in place of EMB to confirm the diagnosis of AM (12, 13), have suggested a more benign clinical course and that clinical presentation can predict prognosis (14–20).
Many of these studies were either small or included small numbers of cases from contributing hospitals, with a consequent risk of selection bias. Furthermore, very few studies report patient ethnicity, and a vast majority of patients in studies where it is reported are White, reflecting local demographics (8, 15, 18). Finally, the impact of sex in a robust, CMR-proven cohort has not been investigated. The objective of this study was to describe the demographic characteristics and outcomes of a large, unselected and ethnically diverse population of patients with AM admitted to a large tertiary Centre in the UK.
Materials and methods
Study design
This was a retrospective cohort study. We included all consecutive patients aged ≥18 years admitted to two hospitals within one hospital Trust (King’s College Hospital, London, UK and Princess Royal University Hospital, Orpington, UK), which has a dedicated myocarditis service, between 12th February 2009 and 4th October 2021 with a diagnosis of AM.
The study was conducted under London South-East Research Ethics Committee approval (reference 18/LO/2048) granted to the King’s Electronic Records Research Interface (KERRI) (21). We used an open-source retrieval system for unstructured clinical data (CogStack) to identify patients. The CogStack engine, developed at King’s College London (22), was used with Elasticsearch to process structured and unstructured textual clinical data from various hospital databases. Additional data cleansing was performed using Python in JupyterLab and returned as CSV spreadsheets.
Further unique patients were identified from our local Hospital Episode Statistics (HES) data if they had a discharge diagnosis of AM in the first diagnostic position according to appropriate ICD codes (B33.2 viral carditis, I01.2 acute rheumatic myocarditis, I09.0 rheumatic myocarditis, I40 AM, I41 myocarditis in diseases classified elsewhere, I51.4 myocarditis, unspecified). We also searched the hospital and Intensive Care Unit (ICU) discharge summaries for inpatients discharged alive containing the keywords “myocarditis” or “myopericarditis.” Finally, we searched for patients that died during the study period where the keywords “myocarditis” or “myopericarditis” were given as a cause of death on the death notification. Patients and public were not involved in the design of this study.
Diagnostic criteria for AM were defined according to 2013 ESC-position statement on myocarditis and 2018 Lake Louise Criteria for AM (4, 11, 23, 24), which were independently applied to retrieved data by a minimum of two authors. Patients were included if they presented to the hospital with a consistent clinical presentation and one or more diagnostic criteria based on ECG, cardiac enzymes or cardiac imaging structure and function, in the absence of significant coronary artery disease (CAD) on invasive or non-invasive coronary imaging or low likelihood of CAD (patients <40 years with low clinical suspicion). In addition, all patients had CMR confirmation of AM according to consensus recommendations (24). CMR was considered acceptable if it included cine imaging, late-gadolinium enhancement imaging, and parametric mapping of myocardial T1 and T2. Patients with suspected/confirmed COVID-19 or vaccine-related AM were excluded. Patients with cardiac sarcoidosis were also excluded. All patients underwent a history and physical examination. Laboratory parameters, echocardiography and CMR findings were recorded.
Clinical presentation, demographic characteristics, and outcomes
We categorised patients into three groups based on their main clinical presentation: (1) chest pain; (2) breathlessness; and (3) arrhythmia. Chest pain presentations were defined as acute chest pain (either ischaemic or pericarditic-sounding) in the absence of CAD and significant left ventricular systolic dysfunction (LVSD). Breathlessness presentations were defined as new onset or progressive HF syndrome. Life-threatening arrhythmias were defined as advanced atrioventricular block, sustained ventricular arrhythmias, or aborted sudden cardiac death. We also categorised patents according to their self-reported ethnicity, and sex. Main clinical presentation was defined by interrogation of the medical record by two authors (DB and AC). Disagreements were resolved by a third author (PS). For each patient, data on baseline co-morbidities and cardiovascular risk factors were obtained using a mix of CogStack retrieval, which was manually validated, and manual searches of the electronic patient record. The primary outcome was a composite of all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy following hospital discharge. Appropriate ICD therapy was defined as an appropriate shock for life-threatening arrhythmias.
Statistical analysis
The results were reported in line with the “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) guidelines (Supplementary Table 1) (25). Continuous variables were expressed as mean and standard deviation, or median and interquartile range (IQR), where appropriate. Categorical variables were expressed as counts and percentage. Comparisons between groups were made by the analysis of variance (ANOVA) test on continuous variables or the Student’s t-test, or by the non-parametric Mann–Whitney test when appropriate. The Chi-square test or the Fisher’s exact tests were calculated for discrete variables.
Survival curves for the primary outcome were estimated and compared between groups by means of the log-rank test. Univariable Cox regression models were performed to obtain hazard ratios for adverse events in the study population. Given the low number of events in the population, multivariable analysis was not performed to avoid overfitting. p < 0.05 was considered significant. All analyses were performed with IBM SPSS Statistics Version 28.0 (IBM Corp., Armonk, NY, USA) and R (R Foundation for Statistical Computing, Vienna, Austria).
Results
Derivation of the cohort
Screening hospital and ICU discharge summaries for keywords “myocarditis” or “myopericarditis” revealed 683 unique patients. Three additional patients were identified by screening death notifications for the same keywords. A further 152 unique patients were identified by searching for admissions with ICD-10 codes corresponding to myocarditis. Discharge summaries and patient records were screened for eligibility and 207 cases were excluded due to not being a discharge diagnosis or death notification of AM. A further eight patients were excluded as they were younger than 18 years old at time of admission. Next, data on diagnostic criteria were extracted. 196 patients had insufficient evidence of AM, CAD was not sufficiently excluded in 18, and an alternative diagnosis was evident in 161. A further 49 patients had clinically suspected AM that was not proven by CMR or EMB. Finally, 199 patients with CMR-proven AM were included in our cohort. Only one patient underwent EMB.
Baseline characteristics
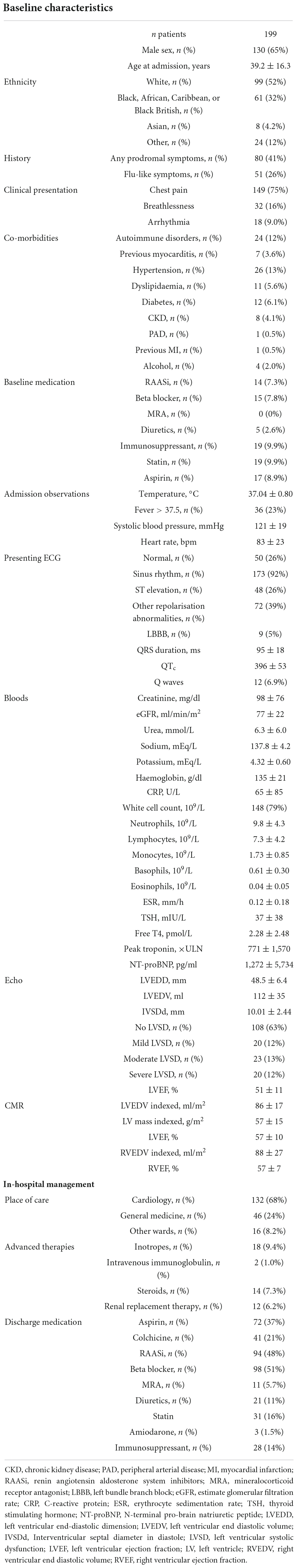
A total of 199 patients with CMR-proven AM were included in the study (Table 1). The majority (n = 130, 65%) were male and the average age was 39 ± 16 years. The study population was ethnically diverse. While most patients were White (n = 99, 52%), Black, African, Caribbean, or Black British (n = 61, 32%), Asian (n = 8, 4%), and “other” (n = 24, 12%) ethnicities were also represented. The most common clinical presentation was with chest pain (n = 149, 75%), with smaller numbers presenting with breathlessness (n = 32, 16%) and arrhythmias (n = 18, 9%). Fewer than half of patients (n = 80, 41%) experienced prodromal symptoms, which included flu-like symptoms in 26% (n = 51). Only a small number of patients had a pre-existing autoimmune disorder (n = 24, 12%) and the most common cardiac co-morbidity was hypertension (n = 26, 13%). Among those with arrhythmic presentation, 14 patients had sustained ventricular tachycardia or ventricular fibrillation.
At admission, all patients underwent ECG, blood testing and CMR as a minimum. Most patients had an abnormal ECG at presentation (n = 149, 74%), predominantly consisting of repolarisation abnormalities (n = 72, 39%) with a smaller proportion demonstrating ST elevation (n = 48, 26%). Overall, renal function was mildly impaired (eGFR 77 ± 22 ml/min/m2) with elevated inflammatory markers (CRP 65 ± 85 U/L). Peak troponin was elevated at 771 times the upper limit of normal (×ULN). Of patients that had an echo at baseline (n = 173, 87%), two thirds presented with normal left ventricular ejection fraction (LVEF).
Overall, most patients (n = 132, 68%) were managed in a cardiology ward. Only a small minority were treated with advanced therapies, including inotropes (n = 18, 9%), and renal replacement therapy (RRT) (n = 12, 6%). Immunosuppression was started in 16 patients (8%). Specifically, 2 patients (1%) received intravenous immunoglobulin (IVIG) and 14 patients received steroids (7%). At discharge, approximately half of patients were on renin-angiotensin-aldosterone system (RAAS) inhibitors. Cardiac devices were present in 21 patients (8%).
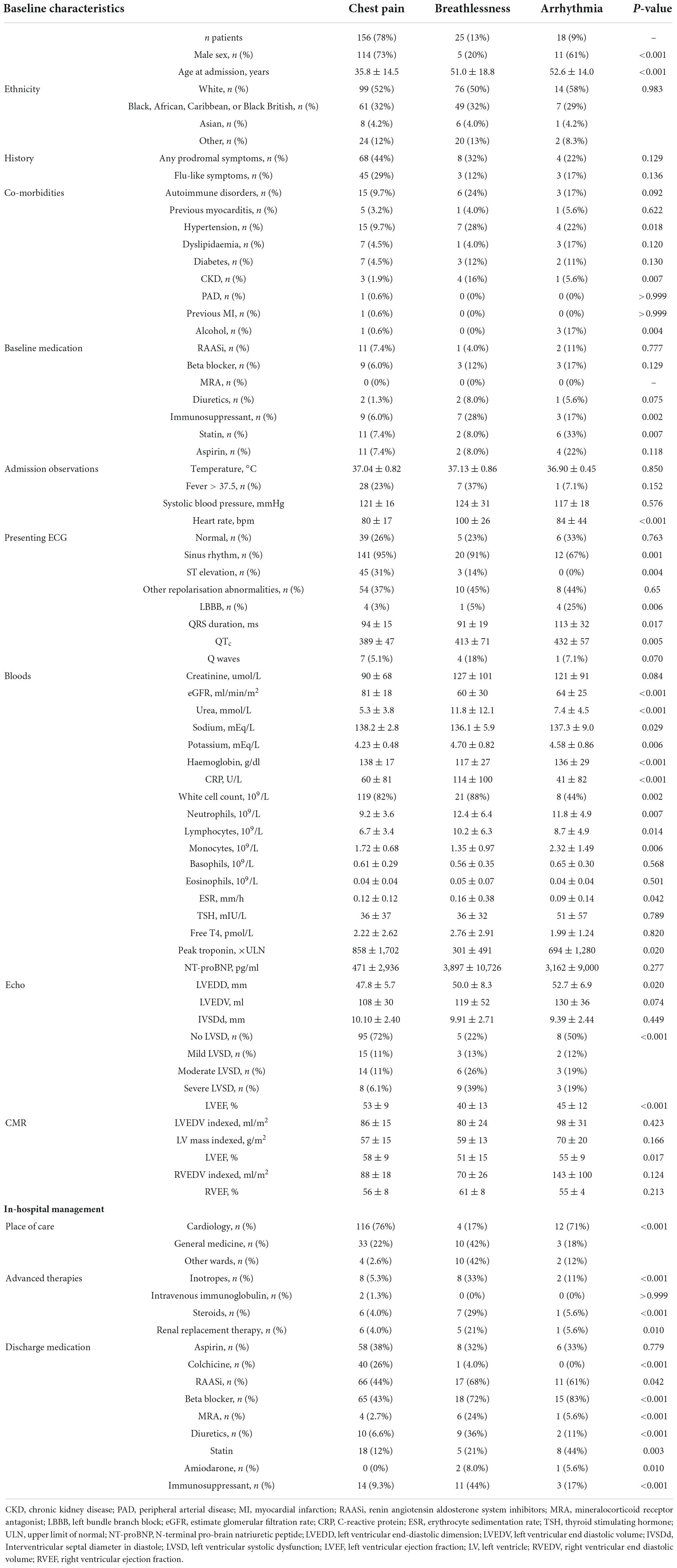
Clinical presentation
Baseline characteristics according to clinical presentation are summarised in Table 2. Patients presenting with chest pain were younger and more frequently male compared to other presentations, while ethnicity was equally distributed. Co-morbidities and baseline medications were broadly similar between patients with different presentations, although fewer patients with a chest pain presentation had hypertension (p = 0.018) and more patients in the breathlessness group were on immunosuppression (p = 0.002). Admission observations were similar between groups, though patients with a breathlessness presentation had a significantly higher heart rate than chest pain or arrhythmia presentations (p < 0.001).
Patients with a chest pain presentation were more likely to have ST elevation than other presentations (31% compared to 14% with breathlessness and none with arrhythmia, p = 0.004), while patients in the arrhythmia group were more likely to have LBBB (p = 0.006). Patients with breathlessness had worse renal function, lower Hb and higher inflammatory markers than other presentations (p < 0.001 for all). Peak troponin was highest in the chest pain group and lowest in those presenting with breathlessness (p = 0.02). Mean LVEF was higher in the chest pain group compared to breathlessness and arrhythmia patients (53 ± 9 vs. 40 ± 13 vs. 45 ± 12%, respectively, p < 0.001). A total of 78% of patients presenting with breathlessness had LVSD, and more often had moderate or severe LVSD compared to those with chest pain or arrhythmias at presentation (65 vs. 17 vs. 38%, respectively, p < 0.001).
In-hospital management was significantly different between groups. Less than one fifth of patients admitted with breathlessness were managed on a cardiology ward compared to three quarters for other presentations (17% for breathlessness vs. 76% for chest pain vs. 71% for arrhythmia, p < 0.001). With the exception of IVIG, advanced therapies were more commonly used in breathlessness presentations (inotropes p < 0.001, steroids p < 0.001, RRT p = 0.01). Furthermore, patients with a breathlessness presentation were more likely to be treated with RAAS inhibitors (p = 0.042) as well as mineralocorticoid receptor antagonists (MRA, p < 0.001), diuretics (p < 0.001) and/or immunosuppression (p < 0.001). Arrhythmia patients were more likely to be treated with beta blockers (p < 0.001) or statins (p = 0.003), while patients presenting with chest pain were more likely to be treated with colchicine (p < 0.001).
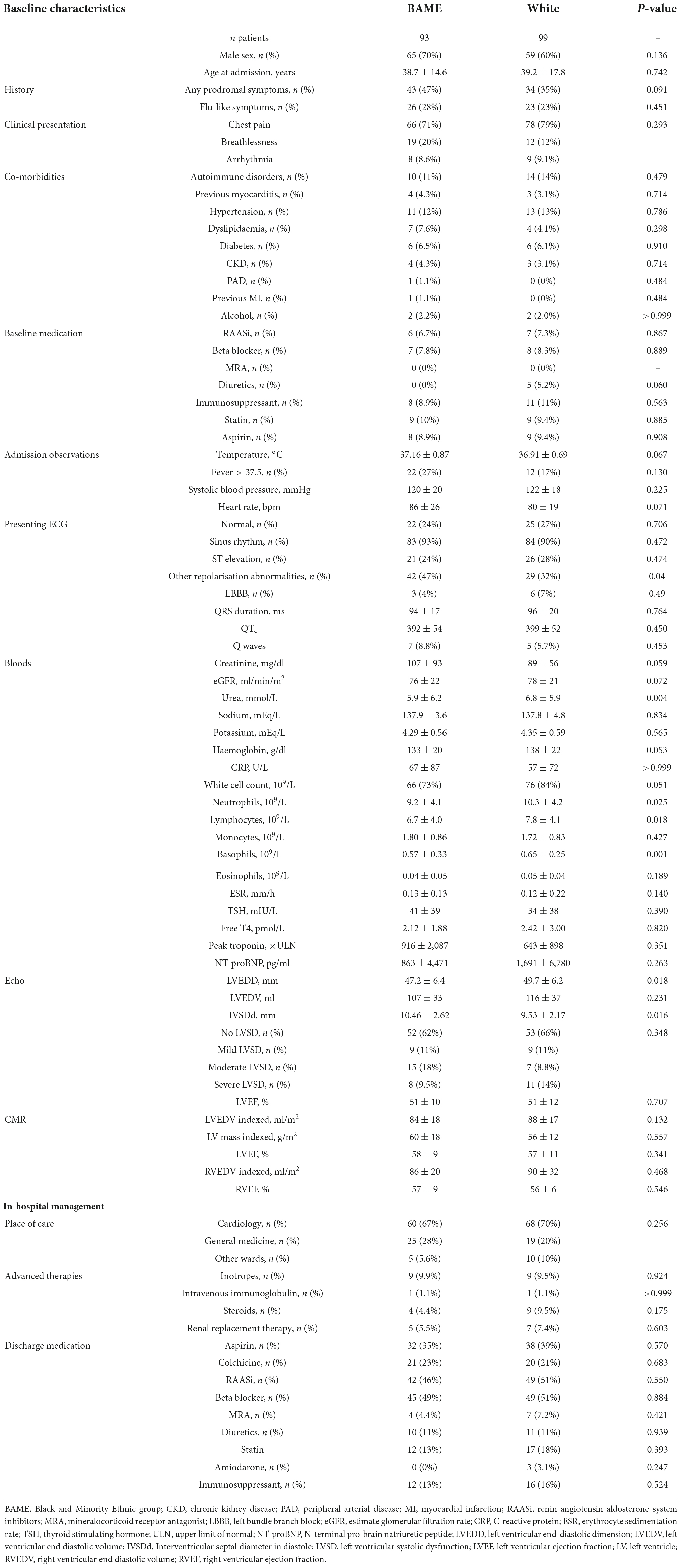
Ethnicity differences in acute myocarditis
Ethnic differences among patients presenting with AM are presented in Table 3. No differences in age, sex, clinical presentation, comorbidities, or baseline treatment were evident. Compared to White patients, Black and Minority Ethnic (BAME) patients had more repolarisation abnormalities on ECG (47 vs. 32%, p = 0.04) and a more pronounced leucocytosis (neutrophils 10.3 ± 4.2 vs. 9.2 ± 4.1 × 109/L, p = 0.025; lymphocytes 7.8 ± 4.1 vs. 6.7 ± 4.0 × 109/L, p = 0.018). BAME and White patients had similar rates of moderate or severe left ventricular (LV) systolic dysfunction, measured with echo (23 vs. 27%, p = 0.47), and no differences on CMR. Inpatient and discharge medications were also indistinct between groups.
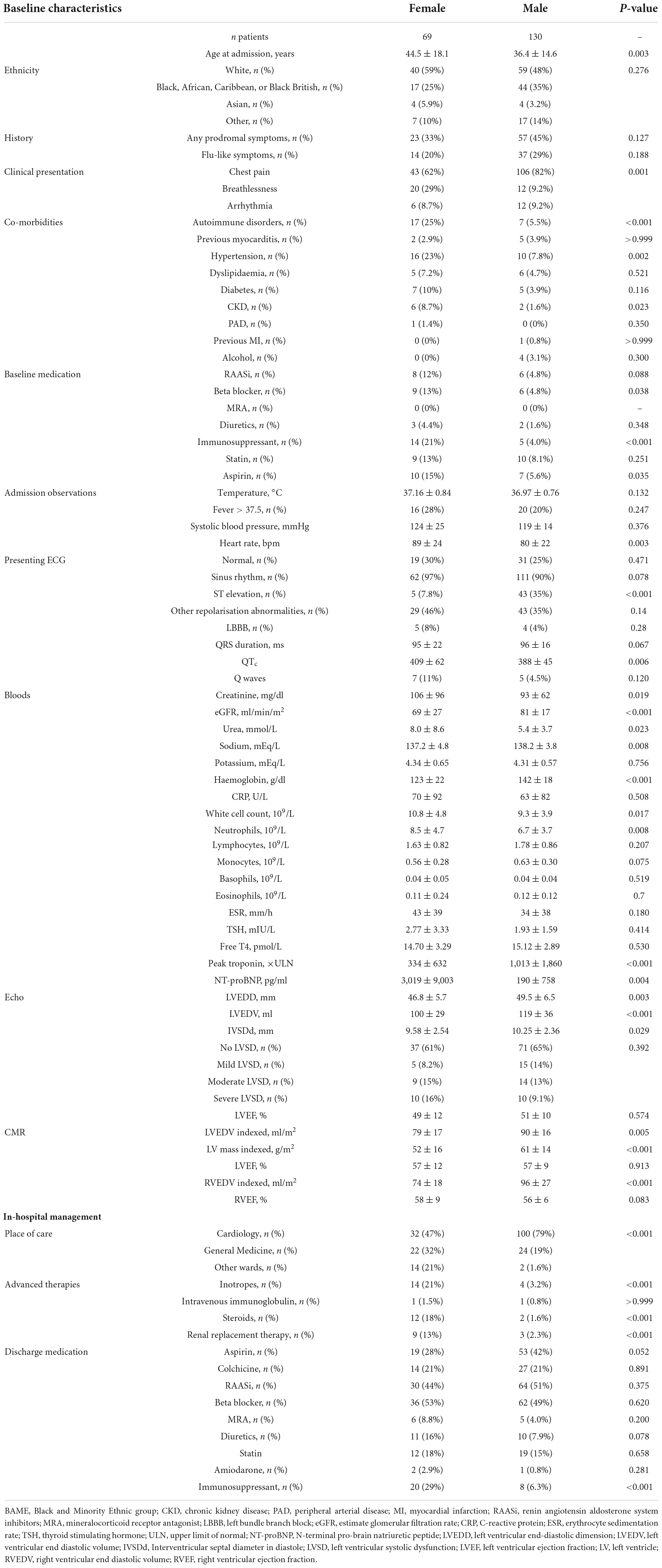
Sex differences in acute myocarditis
Baseline characteristics according to sex are summarised in Table 4. Compared to men, women were older (44.5 ± 18.1 vs. 36.4 ± 14.6, p = 0.003), while ethnicity was equally distributed. Women were also more likely to have a prior autoimmune disorder (p < 0.001), hypertension (p = 0.002) and renal insufficiency (eGFR < 60 mL/min/m2, p = 0.023). More women were on aspirin and/or immunosuppression at the time of presentation (p = 0.035 and <0.001, respectively).
Women were more likely to present with breathlessness compared to men (p = 0.001), and were also more tachycardic at admission (89 ± 24 vs. 80 ± 22 bpm, p = 0.003). Men were more likely to have a chest pain presentation along with ST elevation (p < 0.001 for both).
Women with AM had worse renal function (p < 0.001 for eGFR), lower Hb (p < 0.001) and higher NT-proBNP (p = 0.004) than men. However, men had significantly higher peak troponin (p < 0.001). Inflammatory markers were similar between the groups. Mean LVEF was similar between the groups using both echo and CMR, but both modalities indicated more LV dilatation in men (p < 0.001 for echo).
In-hospital management was significantly different between groups with higher use of steroids, inotropes and RRT in women (p < 0.001 for all). Immunosuppression was also more commonly prescribed for women at discharge (p < 0.001), but other treatments were similar.
Outcomes
Over a median follow-up of 53 (IQR 34–76) months, 11 patients (6%) experienced the primary outcome. Of those, 10 died (5 in the chest pain group, 2 in the breathlessness group and 3 in the arrhythmia group) and 1 patient experienced a successful appropriate ICD shock for monomorphic VT. No patients had resuscitated cardiac arrest.
Overall, 3-year, event-free survival was 96%. Patients in the chest pain group had a more favourable prognosis compared to those presenting with breathlessness or arrhythmia (Figure 1, 3-year event-free survival 98% in the chest pain group, 96% in the breathlessness group, and 89% in the arrhythmia group, p = 0.003). Outcomes were similar between ethnicities (Figure 2, 3-year event-free survival 97% in White patients vs. 96% in BAME patients, p = 0.6) and sexes (Figure 3, 3-year event-free survival 96% in females vs. 97% in males, p = 0.82).
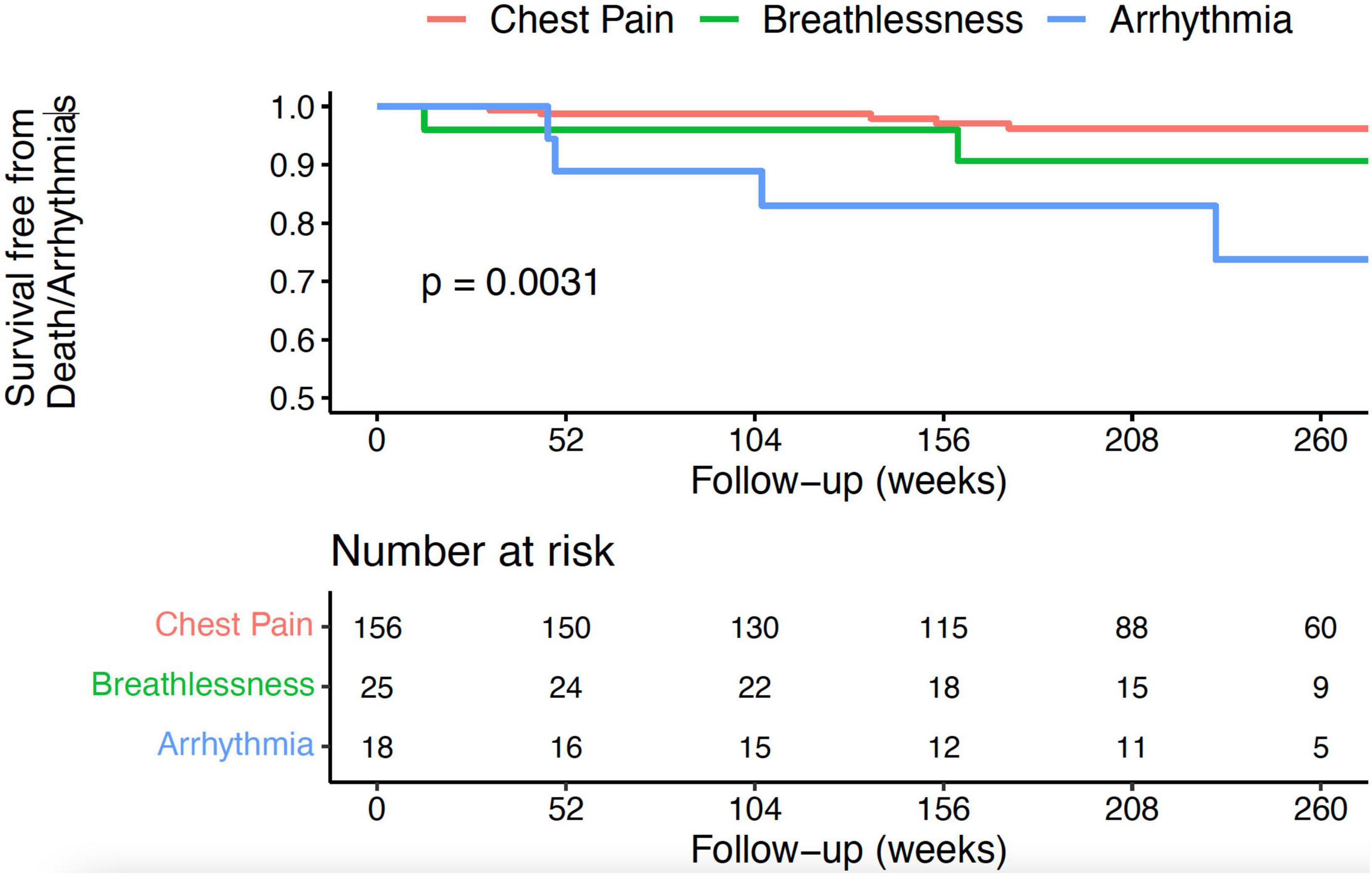
Figure 1. Kaplan–Meier curve for all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy following hospital discharge in patients with AM, according to clinical presentation.
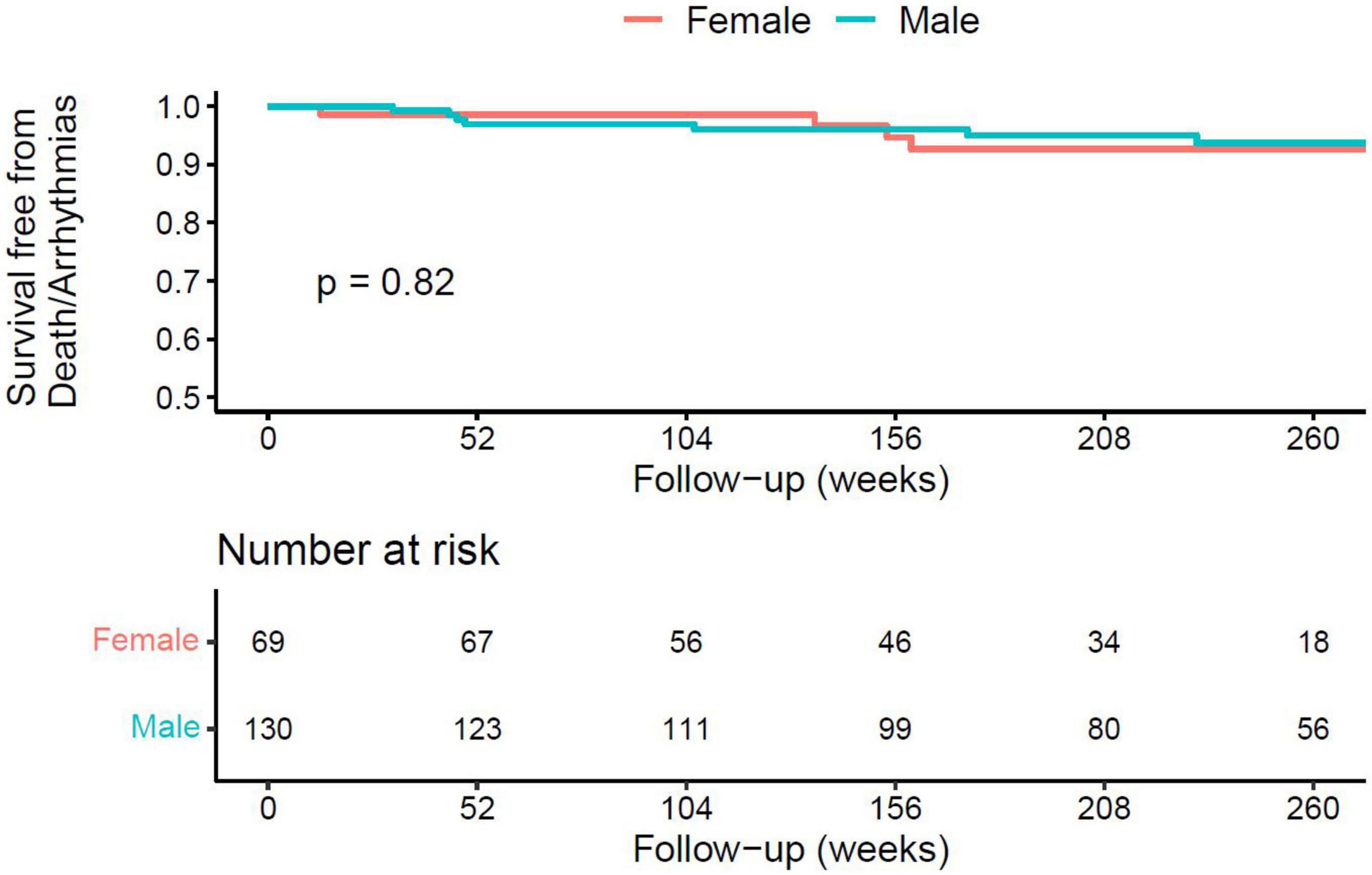
Figure 2. Kaplan–Meier curve for all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy following hospital discharge in patients with AM, according to ethnicity.
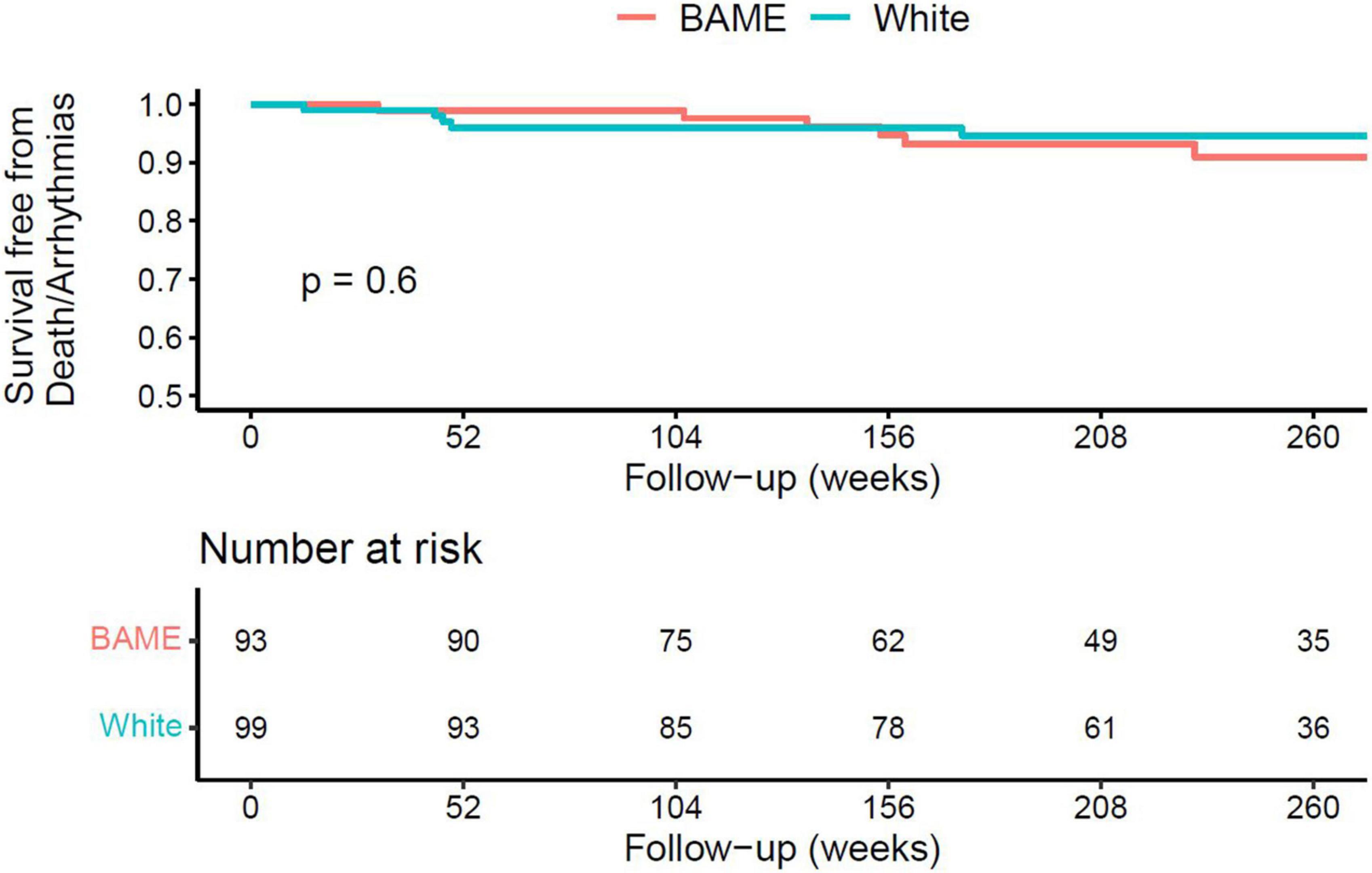
Figure 3. Kaplan–Meier curve for all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy following hospital discharge in patients with AM, according to sex.
In univariable analyses, the variables most strongly associated with the primary outcome were increasing age (p = 0.003), arrhythmia clinical presentations (p = 0.004), comorbidities including hypertension, dyslipidaemia and diabetes (all p < 0.001), sodium (p = 0.003), and LV septal wall thickness (p = 0.045) (Table 5). Compared to chest pain presentations, arrhythmia presentations were associated with a nearly sevenfold risk of the primary outcome [hazard ratio (HR) 6.97; 95% confidence interval (CI) 1.87–26.00, p = 0.004], whereas breathlessness presentations were not significantly associated with outcome. Sex and ethnicity were not associated with the outcome.
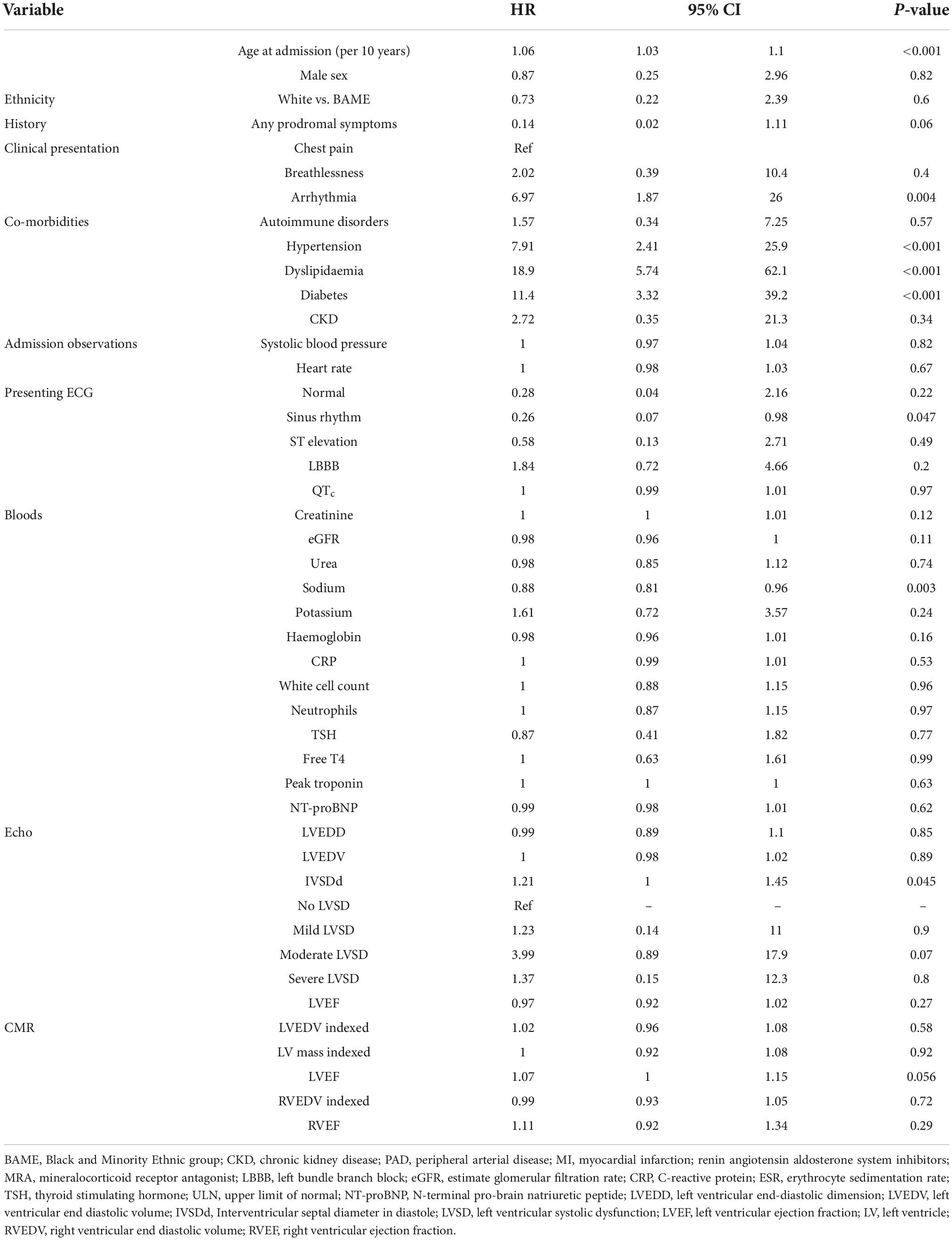
Table 5. Cox proportional univariable analyses evaluating the association of baseline characteristics with all-cause mortality, resuscitated cardiac arrest, and appropriate implantable cardioverter defibrillator (ICD) therapy following hospital discharge.
Discussion
We report one of the largest, single-centre observational analyses of patients hospitalised with AM. We used the ESC position statement on myocarditis and 2018 Lake Louise Criteria to identify nearly 200 patients with CMR-confirmed AM. Importantly, this is the first study of AM in an ethnically diverse population and the first to examine, in detail, sex differences in CMR-proven AM. There are three main findings from our analysis. First, the overall prognosis of CMR-proven AM is benign, with a 3-year event-free survival of 96%. Furthermore, adverse outcomes were virtually exclusively confined to patients with arrhythmia presentations (11% at 3 years of follow-up). Second, there are no major differences in baseline characteristics between patients with different ethnicities. Third, while outcomes are similar for men and women with myocarditis, women have a distinct phenotype, including prior autoimmune disease, more comorbidities, and more breathlessness presentations.
The presentation of AM is highly heterogeneous. Consequently, its epidemiology is incompletely understood (5, 6, 23, 26). Historically, the diagnosis of AM relied on histology obtained from EMB. However, EMB is invasive and not universally available, significantly limiting the widespread applicability of this technique and likely underestimating the real prevalence of the disease (23). Furthermore, most data on the natural history of AM comes from highly selected, EMB-confirmed cases. With increasing availability of CMR, the diagnosis of AM has become more accessible (5, 24, 26, 27). As a result, there is increasing research interest in the use of CMR, rather than EMB, to confirm AM cases. The increased diagnostic yield achieved with CMR has allowed a more detailed and accurate characterisation of patients across the spectrum of AM presentations.
In our cohort, the most common presentation was with chest pain, accounting for three-quarters of cases, with smaller numbers presenting with breathlessness or malignant arrhythmias. These findings are very similar to those of Ammirati et al., who described the clinical course of 443 patients with AM in Italy (15). In their cohort, 73% of patients presented with uncomplicated AM, defined as AM with preserved LVEF and no significant arrhythmia, of whom 97% presented with chest pain. Furthermore, the 5-year incidence of heart transplantation or death in their study was low (5.2%) (15). They found that adverse events were virtually completely confined to patients with a breathlessness or arrhythmia presentations, and that outcomes in patients presenting with chest pain without significant LVSD were good (5-year incidence of death or heart transplantation of 18 vs. 0.3%, respectively). Our study supports these findings in a different healthcare system, time period, and diverse patient population.
Interestingly, we observed a worse prognosis in the arrhythmia compared to breathlessness group. This is contrary to a previous study that described worse clinical outcomes in patients with heart failure presentations than observed in our cohort (11). However, this study used heart transplantation in EMB-proven AM as an endpoint, which is likely to select for sicker patients and may partially account for the different findings. Furthermore, our breathlessness cohort was not limited to patients with LVSD. Our analysis provides a more heterogeneous and contemporary population, and therefore reflects the current prognosis across the spectrum of AM. Arrhythmia patients were older (53 ± 14 years) and, interestingly, less pro-inflammatory than breathless patients. Arrhythmia patients also had larger LV dimensions at presentation, which might suggest AM is a “second hit” in these patients (28, 29).
A higher incidence of AM among men is consistent across studies (4). Previous epidemiological studies have found women with AM to be older, less frequently present with ST elevation, and have no differences in LVEF or all-cause mortality (30, 31). This is consistent with our findings. Mirna et al. also observed lower presenting CRP in women. Animal models of autoimmune myocarditis have suggested attenuation of the immune response in female rats (32). In particular, female rats display preserved LVEF, higher anti-inflammatory Arg1+ macrophages, and a lack of increase in pro-inflammatory modulators (such as TLR4, IL6, IL1β, and iNOS). However, we did not observe differences in CRP, instead finding more neutrophils despite significantly lower troponin. We also observed more autoimmune disorders and immunosuppression in women, suggesting complex interactions between AM, sex and immunity. Finally, this is the first study to specifically examine the role of ethnicity in AM. Ethnic variation has been implicated in several cardiovascular conditions, including heart failure, and response to treatment (33–35). We did not observe any major difference between White and BAME patients, and ethnicity was not associated with outcome in univariable analyses.
The use of advanced or immunosuppressive therapy in hospital was low, and mostly confined to patients presenting with breathlessness. In the total population there was limited use of inotropes (9%), IVIG (1%), steroids (7%), and/or RRT (6%). Use of these therapies was slightly lower than described elsewhere, likely reflecting differences in local practices but also reflecting the benign nature of most AM cases diagnosed using CMR. In our study, a lower proportion of patients with breathlessness were managed on cardiology wards. This was not associated with worse outcomes in our study, despite being well known that patients with acute HF have worse outcomes when managed on general medical wards (36–38).
The adverse event rate in our study is significantly lower than that seen in many previous studies. Most of these studies were performed prior to the widespread availability of CMR and used EMB to confirm AM. It is therefore likely that this predominantly reflects differences in study design and patient selection, leading to lower estimates of mortality. Most studies with ≥90% of cases confirmed by CMR indicate 100% survival with follow-up up to 5 years (14–16, 19, 20, 39, 40), with the most conservative estimate being 95.7% survival at 4.7 years of follow-up (17). This is significantly higher than EMB-selected cohorts, that have reported mortality as high as 56% at 4.3 years (41). The variables with the strongest association with adverse events were clinical presentation, and markers of organ damage or compromised haemodynamics. Most of these variables are available at initial presentation and may help identify which patients might need more advanced support or observation.
Limitations
As a retrospective study of prospectively collected data we recognise several important limitations. We attempted to capture all patients admitted with AM by performing keyword searches of electronic health records and death certificates. However, some patients with AM may have been missed, potentially leading to selection bias. We included patients admitted to two hospitals with AM. The patient populations served by these hospitals may not reflect the general population in the UK or other countries. Furthermore, clinical practice may differ from other national and international centres, which may limit the generalisability of our results. Although all cardiac follow-up that occurred in our institution was captured, it was possible that some endpoints were missed. Patients that moved abroad and subsequently died would have been missed, as would patients that had ICDs implanted at another centre. Finally, unstable patients who could not undergo CMR may have been missed. EMB was not routinely performed and post-mortem analysis was not available, so we were unable to assess aetiology. Despite these limitations, our findings are very similar to those of a comparable multicentre study in terms of clinical presentation and outcomes (15). Finally, although ours is a relatively large study by the standards of AM, our cohort was small with a low number of events. We could therefore not perform multivariable analysis and our study power was limited in identifying variables with a less strong association with adverse events. The use of surrogate endpoints in future AM studies (such as change in EF) may provide sufficient power to identify factors that are independently associated with outcome, especially in male and female subgroups. In addition, studies that examine inflammation in patients with AM would be welcomed.
Conclusion
Acute myocarditis has highly heterogeneous clinical presentations. In our analysis, two thirds of patients with myocarditis present with chest pain and we identified several differences between male and female patients. Overall, AM is associated with a benign prognosis, especially for chest pain presentations. Those presenting with life-threatening arrhythmias are at higher risk of adverse events.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
AC, TM, PS, and DB: design of the study. AC, PB, RR, MA-A, AD, EF, AJ, AS, JH, BC, SB, AK, MS, SR, AB, IR, SP, DS, PS, and DB: data collection. AC, PS, and DB: data analysis and writing the manuscript. MG, AMS, TM, PS, and DB: supervision. All authors critically revised the manuscript.
Funding
AC was supported by the British Heart Foundation (FS/CRTF/21/24175). AMS was supported by the British Heart Foundation (CH/1999001/11735). DB was supported by the King’s BHF Centre of Research Excellence (RE/18/2/34213). The funders played no role in study design, collection, analysis, interpretation of data, writing of the report, or in the decision to submit the manuscript for publication. They accept no responsibility for the contents.
Acknowledgments
We wish to acknowledge the CogStack team at King’s College Hospital NHS Foundation NHS Trust for their support with data retrieval.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.1037837/full#supplementary-material
References
1. Pollack A, Kontorovich AR, Fuster V, Dec GW. Viral myocarditis–diagnosis, treatment options, and current controversies. Nat Rev Cardiol. (2015) 12:670–80. doi: 10.1038/nrcardio.2015.108
2. Khawaja A, Bromage DI. The innate immune response in myocarditis. Int J Biochem Cell Biol. (2021) 134:105973. doi: 10.1016/j.biocel.2021.105973
3. Silverblatt JA, Ziff OJ, Dancy L, Daniel A, Carter B, Scott P, et al. Therapies to limit myocardial injury in animal models of myocarditis: a systematic review and meta-analysis. Basic Res Cardiol. (2019) 114:48. doi: 10.1007/s00395-019-0754-x
4. Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy: an expert consensus document. Circ Heart Failure. (2020) 13:e007405. doi: 10.1161/CIRCHEARTFAILURE.120.007405
5. Sinagra G, Anzini M, Pereira NL, Bussani R, Finocchiaro G, Bartunek J, et al. Myocarditis in clinical practice. Mayo Clin Proc. (2016) 91:1256–66. doi: 10.1016/j.mayocp.2016.05.013
6. Tschope C, Ammirati E, Bozkurt B, Caforio ALP, Cooper LT, Felix SB, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. (2021) 18:169–93. doi: 10.1038/s41569-020-00435-x
7. Magnani JW, Danik HJ, Dec GW Jr., DiSalvo TG. Survival in biopsy-proven myocarditis: a long-term retrospective analysis of the histopathologic, clinical, and hemodynamic predictors. Am Heart J. (2006) 151:463–70. doi: 10.1016/j.ahj.2005.03.037
8. McCarthy RE III, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Hare JM, et al. Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. New England J Med. (2000) 342:690–5. doi: 10.1056/NEJM200003093421003
9. Mason JW, O’Connell JB, Herskowitz A, Rose NR, McManus BM, Billingham ME, et al. A clinical trial of immunosuppressive therapy for myocarditis. The myocarditis treatment trial investigators. New England J Med. (1995) 333:269–75. doi: 10.1056/NEJM199508033330501
10. Merlo M, Anzini M, Bussani R, Artico J, Barbati G, Stolfo D, et al. Characterization and long-term prognosis of postmyocarditic dilated cardiomyopathy compared with idiopathic dilated cardiomyopathy. Am J Cardiol. (2016) 118:895–900. doi: 10.1016/j.amjcard.2016.05.063
11. Anzini M, Merlo M, Sabbadini G, Barbati G, Finocchiaro G, Pinamonti B, et al. Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation. (2013) 128:2384–94. doi: 10.1161/CIRCULATIONAHA.113.003092
12. Baccouche H, Mahrholdt H, Meinhardt G, Merher R, Voehringer M, Hill S, et al. Diagnostic synergy of non-invasive cardiovascular magnetic resonance and invasive endomyocardial biopsy in troponin-positive patients without coronary artery disease. Eur Heart J. (2009) 30:2869–79. doi: 10.1093/eurheartj/ehp328
13. Abdel-Aty H, Boye P, Zagrosek A, Wassmuth R, Kumar A, Messroghli D, et al. Diagnostic performance of cardiovascular magnetic resonance in patients with suspected acute myocarditis: comparison of different approaches. J Am Coll Cardiol. (2005) 45:1815–22. doi: 10.1016/j.jacc.2004.11.069
14. Aquaro GD, Perfetti M, Camastra G, Monti L, Dellegrottaglie S, Moro C, et al. Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY study. J Am College Cardiol. (2017) 70:1977–87. doi: 10.1016/j.jacc.2017.08.044
15. Ammirati E, Cipriani M, Moro C, Raineri C, Pini D, Sormani P, et al. Clinical presentation and outcome in a contemporary cohort of patients with acute myocarditis: multicenter lombardy registry. Circulation. (2018) 138:1088–99. doi: 10.1161/CIRCULATIONAHA.118.035319
16. Sanguineti F, Garot P, Mana M, O’H-Ici D, Hovasse T, Unterseeh T, et al. Cardiovascular magnetic resonance predictors of clinical outcome in patients with suspected acute myocarditis. J Cardiovasc Magn Reson. (2015) 17:78. doi: 10.1186/s12968-015-0185-2
17. Grani C, Eichhorn C, Biere L, Murthy VL, Agarwal V, Kaneko K, et al. Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol. (2017) 70:1964–76. doi: 10.1016/j.jacc.2017.08.050
18. Ammirati E, Cipriani M, Lilliu M, Sormani P, Varrenti M, Raineri C, et al. Survival and left ventricular function changes in fulminant versus nonfulminant acute myocarditis. Circulation. (2017) 136:529–45. doi: 10.1161/CIRCULATIONAHA.117.026386
19. White JA, Hansen R, Abdelhaleem A, Mikami Y, Peng M, Rivest S, et al. Natural history of myocardial injury and chamber remodeling in acute myocarditis. Circ Cardiovasc Imaging. (2019) 12:e008614. doi: 10.1161/CIRCIMAGING.118.008614
20. Younis A, Matetzky S, Mulla W, Masalha E, Afel Y, Chernomordik F, et al. Epidemiology characteristics and outcome of patients with clinically diagnosed acute myocarditis. Am J Med. (2020) 133:492–9. doi: 10.1016/j.amjmed.2019.10.015
21. Bean DM, Teo J, Wu H, Oliveira R, Patel R, Bendayan R, et al. Semantic computational analysis of anticoagulation use in atrial fibrillation from real world data. PLoS One. (2019) 14:e0225625. doi: 10.1371/journal.pone.0225625
22. Jackson R, Kartoglu I, Stringer C, Gorrell G, Roberts A, Song X, et al. CogStack - experiences of deploying integrated information retrieval and extraction services in a large national health service foundation trust hospital. BMC Med Inform Decis Mak. (2018) 18:47. doi: 10.1186/s12911-018-0623-9
23. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European society of cardiology working group on myocardial and pericardial diseases. Eur Heart J. (2013) 34: 2636–48; 2648a–2648d. doi: 10.1093/eurheartj/eht210
24. Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. (2018) 72:3158–76. doi: 10.1016/j.jacc.2018.09.072
25. Noah N. The STROBE initiative: STrengthening the reporting of OBservational studies in epidemiology (STROBE). Epidemiol Infect. (2008) 136:865. doi: 10.1017/S0950268808000733
26. Heymans S, Eriksson U, Lehtonen J, Cooper LT Jr. The quest for new approaches in myocarditis and inflammatory cardiomyopathy. J Am College Cardiol. (2016) 68:2348–64. doi: 10.1016/j.jacc.2016.09.937
27. Fung G, Luo H, Qiu Y, Yang D, McManus B. Myocarditis. Circ Res. (2016) 118:496–514. doi: 10.1161/CIRCRESAHA.115.306573
28. Artico J, Merlo M, Delcaro G, Cannata A, Gentile P, De Angelis G, et al. Lymphocytic myocarditis: a genetically predisposed disease? J Am Coll Cardiol. (2020) 75:3098–100. doi: 10.1016/j.jacc.2020.04.048
29. Cannata A, Artico J, Gentile P, Merlo M, Sinagra G. Myocarditis evolving in cardiomyopathy: when genetics and offending causes work together. Eur Heart J Suppl. (2019) 21:B90–5. doi: 10.1093/eurheartj/suz033
30. Mirna M, Schmutzler L, Topf A, Hoppe UC, Lichtenauer M. Biological sex and its impact on clinical characteristics in patients presenting with myocarditis. Med Princ Pract. (2022) 31:74–82. doi: 10.1159/000520870
31. Kyto V, Sipila J, Rautava P. The effects of gender and age on occurrence of clinically suspected myocarditis in adulthood. Heart. (2013) 99:1681–4. doi: 10.1136/heartjnl-2013-304449
32. Barcena ML, Jeuthe S, Niehues MH, Pozdniakova S, Haritonow N, Kuhl AA, et al. Sex-specific differences of the inflammatory state in experimental autoimmune myocarditis. Front Immunol. (2021) 12:686384. doi: 10.3389/fimmu.2021.686384
33. Gupta DK, Claggett B, Wells Q, Cheng S, Li M, Maruthur N, et al. Racial differences in circulating natriuretic peptide levels: the atherosclerosis risk in communities study. J Am Heart Assoc. (2015) 2015:4. doi: 10.1161/JAHA.115.001831
34. Helmer A, Slater N, Smithgall SA. Review of ACE inhibitors and ARBs in black patients with hypertension. Ann Pharmacother. (2018) 52:1143–51. doi: 10.1177/1060028018779082
35. Holm N, Bromage DI, Cannata A, DeCourcey J, Bhatti P, Huang M, et al. Association between ethnicity and degree of improvement in cardiac function following initiation of sacubitril/valsartan. J Cardiovasc Med. (2022) 23:37–41. doi: 10.2459/JCM.0000000000001268
36. Bromage DI, Cannata A, Rind IA, Gregorio C, Piper S, Shah AM, et al. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail. (2020) 22:978–84. doi: 10.1002/ejhf.1925
37. Cannata A, Bromage DI, Rind IA, Gregorio C, Bannister C, Albarjas M, et al. Temporal trends in decompensated heart failure and outcomes during COVID-19: a multisite report from heart failure referral centres in London. Eur J Heart Fail. (2020) 22:2219–24. doi: 10.1002/ejhf.1986
38. Carriere C, Stolfo D, Baglio V, Gerloni R, Merlo M, Barbati G, et al. Outcome of the multidimensional prognostic index in ultra-octogenarian patients hospitalized for cardiovascular diseases. J Cardiovasc Med. (2018) 19:536–45. doi: 10.2459/JCM.0000000000000699
39. Berg J, Lovrinovic M, Baltensperger N, Kissel CK, Kottwitz J, Manka R, et al. Non-steroidal anti-inflammatory drug use in acute myopericarditis: 12-month clinical follow-up. Open Heart. (2019) 6:e000990. doi: 10.1136/openhrt-2018-000990
40. Imazio M, Angelico G, Andriani M, Lobetti-Bodoni L, Davini O, Giustetto C, et al. Prevalence and prognostic impact of septal late gadolinium enhancement in acute myocarditis with or without preserved left ventricular function. Am J Cardiol. (2018) 122:1955–8. doi: 10.1016/j.amjcard.2018.08.038
Keywords: myocarditis, presentation, sex, ethnicity, outcomes, cardiac magnetic resonance (CMR)
Citation: Cannata A, Bhatti P, Roy R, Al-Agil M, Daniel A, Ferone E, Jordan A, Cassimon B, Bradwell S, Khawaja A, Sadler M, Shamsi A, Huntington J, Birkinshaw A, Rind I, Rosmini S, Piper S, Sado D, Giacca M, Shah AM, McDonagh T, Scott PA and Bromage DI (2022) Prognostic relevance of demographic factors in cardiac magnetic resonance-proven acute myocarditis: A cohort study. Front. Cardiovasc. Med. 9:1037837. doi: 10.3389/fcvm.2022.1037837
Received: 06 September 2022; Accepted: 28 September 2022;
Published: 13 October 2022.
Edited by:
Piero Gentile, Niguarda Ca’ Granda Hospital, ItalyReviewed by:
Emanuele Bobbio, Sahlgrenska University Hospital, SwedenPaolo Manca, Papa Giovanni XXIII Hospital, Italy
Copyright © 2022 Cannata, Bhatti, Roy, Al-Agil, Daniel, Ferone, Jordan, Cassimon, Bradwell, Khawaja, Sadler, Shamsi, Huntington, Birkinshaw, Rind, Rosmini, Piper, Sado, Giacca, Shah, McDonagh, Scott and Bromage. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daniel I. Bromage, ZGFuaWVsLmJyb21hZ2VAa2NsLmFjLnVr
†These authors have contributed equally to this work
 Antonio Cannata
Antonio Cannata Prashan Bhatti
Prashan Bhatti Roman Roy
Roman Roy Mohammad Al-Agil
Mohammad Al-Agil Allen Daniel2
Allen Daniel2 Barbara Cassimon
Barbara Cassimon Susie Bradwell
Susie Bradwell Matthew Sadler
Matthew Sadler Josef Huntington
Josef Huntington Alexander Birkinshaw
Alexander Birkinshaw Irfan Rind
Irfan Rind Susan Piper
Susan Piper Mauro Giacca
Mauro Giacca Ajay M. Shah
Ajay M. Shah