- 1Department of Vascular Medicine, Amsterdam UMC Location University of Amsterdam, Amsterdam, Netherlands
- 2Amsterdam Cardiovascular Sciences, Pulmonary Hypertension and Thrombosis, Amsterdam, Netherlands
- 3INSERM, Clinical Investigator Center 1408 – Centre Hospitalier Universitaire de Saint-Etienne, Saint-Etienne, France
- 4F CRIN, INNOVTE Network, Saint-Etienne, France
Background: Potential hazards of vena cava filters include migration, tilt, perforation, fracture, and in-filter thrombosis. Due to physiological changes during pregnancy, the incidence of these complications might be different in pregnant women.
Aim: To evaluate the use and safety of inferior vena cava filters in both women who had an inferior vena cava filter inserted during pregnancy, and in women who became pregnant with an inferior vena cava filter in situ.
Methods: We performed two searches in the literature using the keywords “vena cava filter”, “pregnancy” and “obstetrics”.
Results: The literature search on women who had a filter inserted during pregnancy yielded 11 articles compiling data on 199 women. At least one filter complication was reported in 33/177 (19%) women and included in-filter thrombosis (n = 14), tilt (n = 6), migration (n = 5), perforation (n = 2), fracture (n = 3), misplacement (n = 1), air embolism (n = 1) and allergic reaction (n = 1). Two (1%) filter complications led to maternal deaths, of which at least one was directly associated with a filter insertion. Filter retrieval failed in 9/149 (6%) women. The search on women who became pregnant with a filter in situ resulted in data on 21 pregnancies in 14 women, of which one (6%) was complicated by uterine trauma, intraperitoneal hemorrhage and fetal death caused by perforation of the inferior vena cava filter.
Conclusion: The risks of filter complications in pregnancy are comparable to the nonpregnant population, but could lead to fetal or maternal death. Therefore, only in limited situations such as extensive thrombosis with a contraindication for anticoagulants, inferior vena filters should be considered in pregnant women.
Introduction
Vena cava filters are intravascular devices that trap thrombi migrating from deep veins toward the pulmonary arteries, and therefore prevent new pulmonary embolisms. Currently, major guidelines agree on the recommended use of vena cava filters in patients with acute venous thromboembolism (VTE, comprising deep vein thrombosis [DVT] and pulmonary embolism) while therapeutic anticoagulant treatment is contraindicated if there is active bleeding or a high risk of bleeding—such as recent or planned surgery or delivery, and in patients with recurrent VTE despite adequate anticoagulant treatment (1–5). Complications occurring directly after insertion of the vena cava filter include access site thrombosis, infection, bleeding and perforation of the vena cava wall (2, 4, 6). Long-term complications of vena cava filters can occur in the days or months after insertion and include filter migration, filter tilt, perforation of the vena cava wall, fracture and embolization of filter struts, or in-filter thrombosis with or without concomitant deep-vein thrombosis (2, 6). These complications have been reported in 7–22% of the nonpregnant population (7, 8). Failure of filter retrieval was reported in 11–12% of nonpregnant patients (8, 9).
When a VTE occurs during pregnancy, the indicated anticoagulant treatment should temporarily be interrupted around time of delivery. This poses hemostatic challenges when VTE is diagnosed shortly prior to the expected date of delivery, since the risk of progression or recurrence of VTE is highest during the first month after diagnosis, while at the same time anticoagulant treatment can worsen peripartum bleeding.
Due to physiological changes that occur during pregnancy, pregnant women may be at increased risk of inferior vena cava filter complications. As a result of the dilated and curved inferior vena cava during pregnancy, the filter might be more likely to tilt and/or migrate, which could make the filter less effective and harder to retrieve. Moreover, the effect of compression of the gravid uterus on the inferior vena cava, contractions and increased intra-abdominal pressure while pushing, has not yet been established. Therefore, evidence-based guidance on the use of vena cava filters in pregnant women is paramount. In this review we aim to provide an overview of the available literature on the use and safety of inferior vena cava filters in pregnant women. We will separately report results for women who got an inferior vena cava filter inserted during pregnancy and for women who became pregnant with an inferior vena cava filter in situ.
Inferior vena cava filters for acute venous thromboembolism inserted during pregnancy
In the first part of this review, we aim to evaluate the use, obstetric outcomes, and filter complications of patients who had an inferior vena cava filter inserted during pregnancy.
Literature search—methods
A systematic search of literature published between January 2015 and May 2022 was conducted on Medline and Embase. The search strategy was based on the following keywords: “vena cava filter”, “pregnancy” and “obstetrics”. We searched for original studies, case series and case reports. No restrictions with regard to study design or geographic location were applied. Articles were included if they reported data on inferior vena cava filters inserted during pregnancy. Information about filter indication, route and timing of filter insertion, filter complications, indwelling time, and maternal and fetal outcomes was collected. All reference lists of included manuscripts were manually searched to identify related articles that were not yet identified.
Results
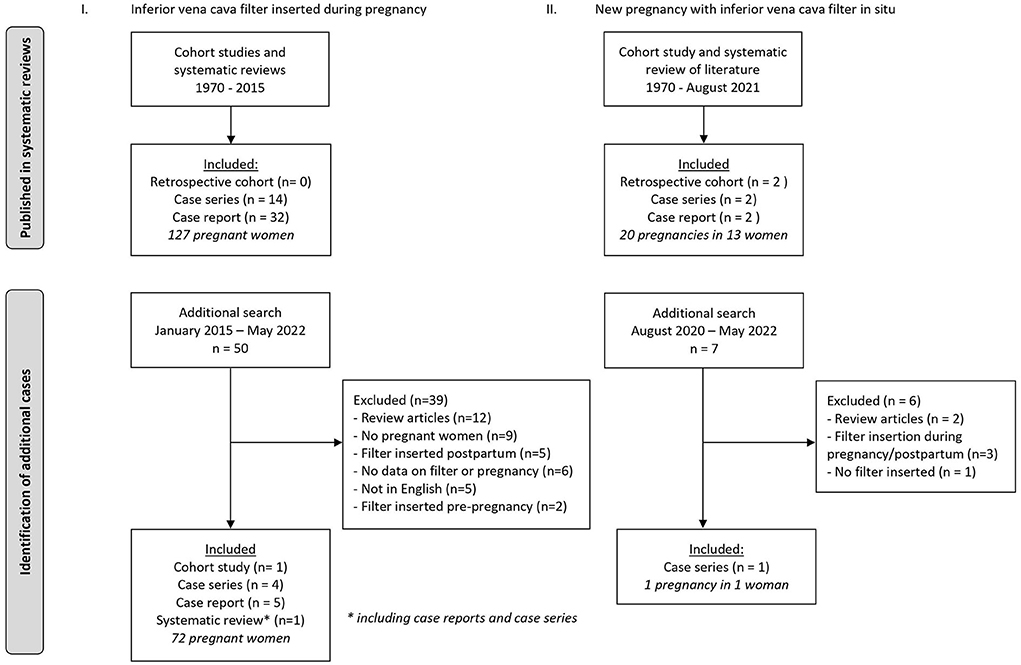
Literature search yielded 50 articles based on titles and abstracts, and eleven articles were included after full text screening: one cohort study (10), four case series (8, 11–13), five case reports (14–18) and a systematic review with case series and case reports (19). The reasons for excluding the other 39 manuscripts were: review articles without case reports (n = 12), not concerning pregnant women (9), postpartum filter insertion (n = 5), article not in the English language (n = 5), no details provided concerning either the pregnancy or the filter (n = 6), and filter insertion prior to pregnancy (n = 2) (Figure 1). One of the included articles was a case report accompanied by an overview of the English language literature from January 1970 to 2014 on vena cava filters during pregnancy (14). In this overview (14), a total of 64 cases were reported and all these cases—except for three—were also included in another systematic review on inferior vena cava filters in pregnancy, published in 2016 (19). In a case series published in 2015 (11), 11 of the 20 cases were duplicates of previously published cases (20) included in the systematic review of Harris et al (19). From this article (11) we only retained the nine cases which were never previously published. Hence our systematic search yielded a total of 199 women who had an inferior vena cava filter inserted during pregnancy.
Filter insertion
Of the 199 pregnant women, 45 women (23%) had a permanent filter (36 Greenfield, 4 Cardial, 2 Bird's Nest, 1 TrapEase, 2 undetermined) and 154 women (77%) had a retrievable filter (26 Neuhaus Protect, 20 Günther Tulip, 19 OptEase, 12 Antheor, 10 ALN, 5 Tempofilter, 4 Celect, 2 Recovery, 1 Zontik, 1 Prolyser, 1 Cardial and 53 undetermined) inserted. The filter locations were reported for 138 women: inferior vena cava filters were inserted in a suprarenal position in 96 women (70%) and in an infrarenal position in 42 women (30%).
The indication for filter insertion in all women was venous thromboembolism during pregnancy: 90 women (45%) had a proximal DVT, 17 women (9%) had pulmonary embolism with or without concomitant DVT, and in 51 women (26%) the exact thrombosis location remained unspecified (Table 1) (8, 10–18, 21–50). Additionally, 27 women (19%) had progression of VTE despite adequate anticoagulant treatment (13–15, 24, 25, 29, 32, 35, 36, 48, 50–59), and 9 women (5%) had a proximal DVT and a contraindication for anticoagulant treatment due to significant risk of bleeding (8, 13, 18, 24, 25, 48, 51). Deep-vein thrombosis and heparin induced thrombocytopenia occurred in 5 women (3%) (24, 25, 35, 51, 60). In more than half of the women (107/199, 54%), an inferior vena cava filter was inserted in the third trimester of pregnancy (Table 1).
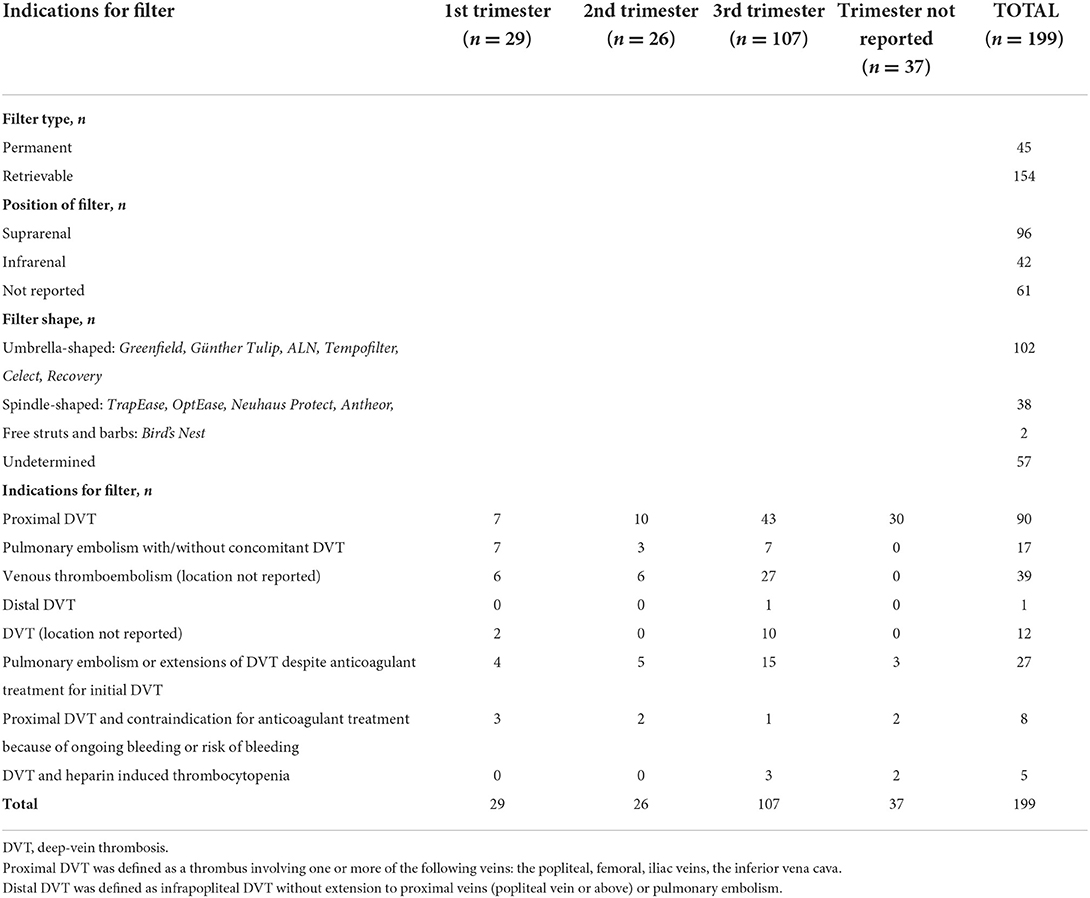
Table 1. Characteristics, indications and timing of insertion of inferior vena cava filters during pregnancy.
Obstetric outcomes
Obstetric outcomes were reported in 162 cases: 73 women (46%) had a vaginal delivery and 85 women (52%) had a caesarean section. Four women (2%) had a medically indicated termination of pregnancy. No fetal deaths were recorded. Two neonates (1%) suffered from mild respiratory distress (51), but data concerning the fetal outcomes were often lacking.
Filter complications
Individual data on follow-up of inferior vena cava filters after insertion in pregnant women were reported for 177 women: at least one complication of the inferior vena cava filter was reported in 33 women (19%). Filter complications are summarized in Table 2. Immediate complications (within 24 h of filter insertion) occurred in three women (2%) and long-term complications (days to months after filter insertion) occurred in 30 women (17%). Two maternal deaths (1%) were reported: one woman had a fatal air embolism during the insertion of a Kimray-Greenfield filter (53), the other woman with an in-filter thrombosis died as a consequence of catastrophic antiphospholipid syndrome (13). The most frequently reported complication was in-filter thrombosis. Some authors reported in-filter thrombosis as a consequence of extended proximal DVT (13, 54, 58, 61), while others described captured thrombi as a successful filter function or as a consequence of discontinuation of anticoagulant therapy (12, 17, 20, 41). Of the 14 in-filter thromboses (8%), concomitant symptomatic pulmonary embolism was reported in one woman (54). These in-filter thromboses or captured thrombi were observed in almost all types of retrievable filters (Celect, Neuhaus Protect, Antheor, OptEase) and in one case with a permanent filter (Greenfield). Filter complications occurred in 21% (20 of 96 women) of suprarenal positioned and in 24% (10 of 42 women) of infrarenal positioned inferior vena cava filters. Overall the complications occurred with all types of filters. Therefore, it is not possible to clearly establish a link between a type of filter and a type of complication. Of note, the level of DVT that justified the need for filter placement in these women was femoral in four women (12, 58), iliofemoral in four women (12, 17, 20, 61), and not specified in six women (13, 18, 41, 54). Among the women with in-filter thrombosis, time since filter insertion was 5 days or less for three women (21%) (12, 61) and 7 days or more for 11 women (79%).
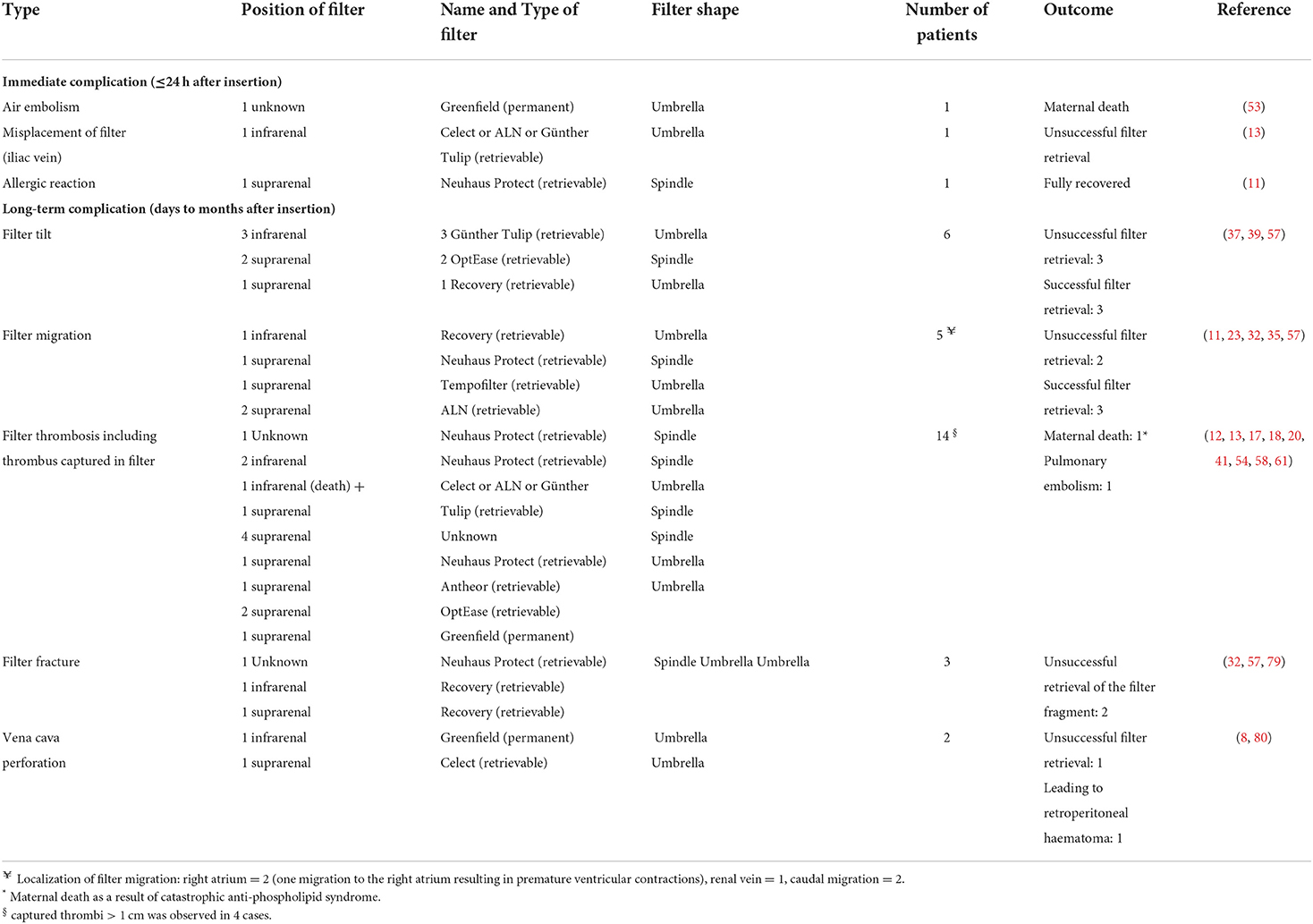
Table 2. Immediate and long-term complications of inferior vena cava filters inserted during pregnancy.
Other complications of the filter were observed in 19 women and included in a descending order of frequency: tilts (six women, 3%), migrations (five women, 3%), fractures (three women, 2%), vena cava perforation (two women, 1%), misplacement (one woman, < 1%) and allergy (one woman, < 1%). The most important consequence of these complications was the failure of filter retrieval in nine of the women concerned.
Filter retrieval
In the large majority of women with retrievable filters, the vena cava filter could be retrieved (140/154, 91 %). Data on time to filter retrieval was available for 98 women, in 81 women (83%) the inferior vena cava filter was left in situ for a maximum of 30 days and in the remaining 17 women (17%) filters were retrieved after 1 month. For eight of these women (47%), time since filter insertion was more than 90 days with a maximum of 287 days (15). In nine of the 154 women with a retrievable filter (6%) failed attempts of retrieval were reported (8, 13, 35, 36, 39, 57, 59). Two of these retrieval failures (22%) occurred after a very long time after insertion (167 and 659 days), the other six attempts (66%) were performed after an in situ time varying between 6 and 73 days, and for one woman (11%) data were missing. In five women (5/154, 3%), no attempt of filter retrieval was made and the filter was left in situ. The reasons were persistent extensive DVT despite of anticoagulants (62), in-filter thrombosis (41), filter misplacement into external iliac vein (13) or maternal dead (13). Hence, in total 9% of the filters were not retrieved.
New pregnancy in women with a permanent vena cava filter
In the second part of this review, we aim to evaluate the use, obstetric outcomes, and filter complications of patients who became pregnant with an inferior vena cava filter already in situ prior to conception.
Literature search—methods
Similar to the first part of the review, a literature search was conducted. However, a review on this exact same subject has been recently performed and published by one of the authors of this review (63). In that publication a comprehensive search of the English language literature was conducted in MEDLINE, Embase, and abstracts of conferences between 1970 and August 2020 (63). For the current review, we have repeated the same search for the period from August 2020 to May 2022 (Figure 1). No restrictions with regard to study design nor geographic location were applied. Articles were included if they reported data on pregnancies after insertion of an inferior vena cava filter that was left in situ. Information about filter indication, route and timing of filter insertion, filter complications, indwelling time, and maternal and fetal outcomes was collected. All reference lists of included manuscripts were manually searched to identify related articles that were not yet identified.
Results
The extended literature search yielded seven new articles based on titles and abstracts, and only one article was included after full text screening. The reasons for exclusion of the six other manuscripts were: review articles (n = 2), filter insertion during pregnancy or postpartum (n = 3), and no inferior vena cava filter inserted (n = 1) (Figure 1). The included study was a case series of Taiwanese patients with inferior vena cava thrombosis (64). This case series included one 46-year old woman who was pregnant and had an unretrieved inferior vena cava filter in situ. However, other than the inferior vena cava thrombosis, no details or outcomes of interest were reported. The recently published review (63) revealed one cohort study (13), two case series (36, 48) and two case reports (65, 66). Additionally, the review also reported data from its own cohort. In total, data on 21 pregnancies in 14 women were available.
Filter insertion
Among 14 women, six women (43%) had a permanent vena cava filter (3 Bird's Nest, 1 Greenfield, 2 TrapEase) inserted, six women (43%) had a retrievable inferior vena cava filter (2 Günther Tulip, 2 OptEase, 2 undetermined retrievable filter) inserted, and for two women (14%) the filter type was unknown. Of the women with a retrievable filter, retrieval attempts failed in five women (83%) and in one woman (17%) no attempts were made. The filter position was infrarenal in six women (43%) and was not reported for the other eight (57%) women. Indication for an inferior vena cava filter was pre-pulmonary endarterectomy because of chronic thrombo-embolic pulmonary hypertension in two women (14%) (63), pulmonary embolism or recurrent VTE and contraindication for anticoagulant therapy due to surgery or bleeding in three women (21%) (36, 63, 65), DVT or pulmonary embolism during pregnancy in four women (29%) (13, 36, 63), recurrent VTE despite anticoagulant therapy in two women (14%), and VTE outside of pregnancy in two women (14%) (48, 66). The indication was unknown in one woman (64). Time between filter insertion and pregnancy ranged from < 1–8 years.
Obstetric outcomes
Obstetric outcomes were reported for 17 pregnancies: 15 pregnancies (87%) ended in life-births, one pregnancy (7%) ended in miscarriage before the 10th weeks of gestation (63), and one pregnancy (7%) ended in an emergency cesarean section at 24 weeks of gestation (65). The later was the result of a filter complication described below. The fetus died shortly after birth.
Filter complications
Filter complications were reported for 16 pregnancies and summarized in Table 3. In 14 pregnancies (88%) no complications occurred, but follow-up and imaging of the filter was poorly performed. One pregnancy (6%) was complicated by uterine trauma and major intraperitoneal hemorrhage caused by perforation of the vena cava wall and uterus by the inferior vena cava filter's barbs and struts (65). In this case, the infrarenally positioned TrapEase filter was already known to have perforated the inferior vena cava wall prior to pregnancy, but the woman had been asymptomatic up until the uterine laceration occurred (65). Other filter complications were reported by one other study (64), information was limited to the occurrence of inferior vena cava filter thrombosis. It was not reported whether this was caused by an in-filter thrombosis.
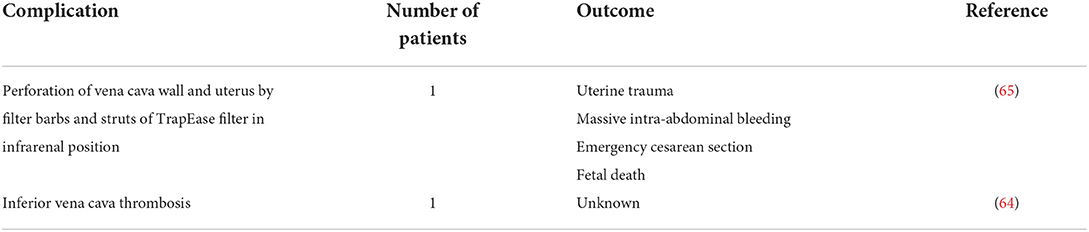
Table 3. Complications of inferior vena cava filters in women with new pregnancy with inferior vena cava filter in situ.
Discussion
Our literatures searches compiled data on 199 women who had an inferior vena cava filter inserted during pregnancy, and data on 21 pregnancies that occurred in 14 women who had an inferior vena cava filter in situ prior to conception. In women who had a filter inserted during pregnancy, 77% had a retrievable filter and in more than half of these women the filter was inserted in the third trimester of pregnancy. At least one complication was reported in 19% of women, most women had in-filter thrombosis. Two women died after filter insertion, however for one of them it was unclear whether this was a direct complication of the filter insertion. Retrieval failure was reported in 6%. These numbers are comparable to the nonpregnant population. In women who became pregnant with a filter in situ, complications were poorly evaluated but one filter complication resulting in major hemorrhage and fetal death was reported.
Although VTE risk increases up to 7–10-fold during pregnancy compared to age-matched controls, the overall incidence remains low (around 1–2 per 1,000 pregnancies) (67). Consequently, it is not surprising that the number of pregnant women who had an inferior vena cava filter inserted for an acute VTE reported in the English literature was low: only 199 cases have been reported since 1970 and no randomized-controlled trials on the safety and efficacy of inferior vena cava filters in pregnancy have been conducted. Moreover, the very low number of women who became pregnant with an inferior vena cava filter in situ was also expected. In the recent American Society of Hematology (ASH) guideline on venous thromboembolism management in pregnant women, the question whether to insert a vena cava filter for the treatment of acute VTE in the third trimester of pregnancy has not been addressed (68). The older American College of Chest Physicians (ACCP) guideline discusses the use of vena cava filters which was restricted to women with very high risk of recurrence, such as women with proven DVT and recurrent pulmonary embolism despite anticoagulant treatment (69).
From the data provided in this review, we can conclude that most women who had an inferior vena cava filter inserted during pregnancy did not meet these indications and should not have had a filter inserted. At most, only 4 % of the women had an absolute contraindication for anticoagulant therapy and failure of anticoagulant treatment was the indication for filter insertion in 14% of pregnant women. The occurrence of VTE was the most frequently reported reason for filter insertion, while patients were not at very high risk of recurrence. This might be based on the fear of a pulmonary embolism occurrence or recurrence related to the temporary withdrawal of anticoagulant treatment peripartum. Higher VTE incidence during the third trimester of pregnancy and in the early postpartum period is well reported (70, 71), but the risk of thrombosis extension or new pulmonary embolism some hours after anticoagulation withdrawal is poorly evaluated in the literature. There is one retrospective study reporting 344 nonpregnant patients with VTE who had a vena cava filter inserted and received no anticoagulants. In 42% of patients there was a contraindication for anticoagulants because of a significant risk of bleeding. These patients were matched using propensity scores with 344 other patients treated with only anticoagulants without having a vena cava filter inserted. After 30 days of treatment, the risk-adjusted pulmonary embolism related mortality rate was lower for filter insertion compared to no filter insertion (1.7 vs. 4.9%; p = 0.03), but the risk-adjusted recurrent VTE rates were higher for filter insertion compared to no filter insertion (6.1 vs. 0.6%; p < 0.001) (72). The authors concluded that despite an increased risk of VTE events, including in-filter thrombosis, filter insertion did not allow for a large pulmonary embolism to occur (73).
The most frequently reported filter complication was in-filter thrombosis. This is a well-known complication of vena cava filters and usually occurs at long-term use (>30 days) (7, 74). Early in-filter thrombosis has also been described as a captured large thrombus that can appear only a very few days after its insertion (11, 12, 17). These findings argue for optimal peripartum management and require a multidisciplinary approach: the window without anticoagulant therapy should kept as short as possible and both induction of labor and bridging with unfractionated heparin should be considered. Furthermore, anticoagulant therapy should be resumed as soon as possible after delivery and filter retrieval should be planned. The incidence of other filter complications is lower and similar to incidence rates of the nonpregnant population. Some authors suspected that during the second stage of labor and delivery intra-abdominal pressure could cause tilt, fracture and migration of the filter (20, 75). Due to the low number of patients in our review, we were unable to statistically compare such complications for patients with vaginal delivery compared to patient who had a caesarean section. Finally, the rate of filter complications in our review might be overestimated because of selection and publication biases.
The failure rate of filter retrieval is low (6 %) and comparable to the one in nonpregnant population (76, 77). However, in 3% no filter retrieval was attempted. When the filter remains in situ, women will be exposed to complications described by Decousus in a nonpregnant cohort with a follow-up period of 8 years (78), these include DVT recurrence and in-filter thrombosis.
In conclusion, only in pregnant women with clear indication such as acute proximal DVT shortly prior to delivery and contraindication for anticoagulant therapy, or progression of DVT despite adequate anticoagulant therapy, should inferior vena filters be considered. When inserted, retrieval should be planned as soon as possible and temporary filters are to be preferred over permanent filters. This would help to avoid long-term complications in young women who might be planning future pregnancies.
Author contributions
IB and AB performed the literature searches, interpreted extracted data, and wrote the first draft of the manuscript. BT critically reviewed and revised the manuscript. The final version of the manuscript was approved by all authors.
Acknowledgments
We thank Daniel Petrov for his critical suggestions and feedback.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, et al. Antithrombotic Therapy for VTE Disease CHEST Guideline and Expert Panel Report. Chest. (2016) 149:315–52. doi: 10.1016/j.chest.2015.11.026
2. Duffett L, Carrier M. Inferior vena cava filters. J Thromb Haemostasis. (2017) 15:3–12. doi: 10.1111/jth.13564
3. Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A, et al. American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv. (2020) 4:4693–738. doi: 10.1182/bloodadvances.2020001830
4. Kaufman JA, Kinney TB, Streiff MB. Guidelines for the use of retrievable and convertible vena cava filters: report from the Society of Interventional Radiology multidisciplinary consensus conference (vol 17, pg 449, 2006). J Vasc Interven Radiol. (2017) 28:1338. doi: 10.1097/01.RVI.0000203418-39769.0D
5. DeYoung E, Minocha J. Inferior Vena Cava Filters: Guidelines, Best Practice, and Expanding Indications. Semin Intervent Radiol. (2016) 33:65–70. doi: 10.1055/s-0036-1581088
6. Caplin DM, Nikolic B, Kalva SP, Ganguli S, Saad WE, Zuckerman DA. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J Vasc Interv Radiol. (2011) 22:1499–506. doi: 10.1016/j.jvir.2011.07.012
7. Angel LF, Tapson V, Galgon RE, Restrepo MI, Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interven Radiol. (2011) 22:1522–30. doi: 10.1016/j.jvir.2011.08.024
8. Crosby DA, Ryan K, McEniff N, Dicker P, Regan C, Lynch C, et al. Retrievable Inferior vena cava filters in pregnancy: Risk versus benefit? Eur J Obstetr Gynecol Reprod Biol. (2018) 222:25–30. doi: 10.1016/j.ejogrb.2017.12.035
9. Cohoon KP, McBride J, Friese JL, McPhail IR. Retrievable inferior vena cava filters can be placed and removed with a high degree of success: initial experience. Catheter Cardio Inte. (2015) 86:719–25. doi: 10.1002/ccd.25716
10. Elgendy IY, Fogerty A, Blanco-Molina A, Rosa V, Schellong S, Skride A, et al. Clinical Characteristics and Outcomes of Women Presenting with Venous Thromboembolism during Pregnancy and Postpartum Period: Findings from the RIETE Registry. Thromb Haemost. (2020) 120:1454–62. doi: 10.1055/s-0040-1714211
11. Konishi H, Miyoshi T, Neki R, Fukuda T, Ishibashi-Ueda H, Ogo T, et al. Intrapartum temporary inferior vena cava filters are rarely indicated in pregnant women with deep venous thromboses. J Vasc Surg Venous Lymphat Disord. (2015) 3:370–5. doi: 10.1016/j.jvsv.2015.04.004
12. Hara N, Miyamoto T, Yamaguchi J, Iwai T, Hijikata S, Watanabe K, et al. Treatment Outcomes of Anticoagulant Therapy and Temporary Inferior Vena Cava Filter Implantation for Pregnancy Complicated by Venous Thrombosis. Ann Vasc Dis. (2018) 11:106–11. doi: 10.3400/avd.oa.17-00100
13. Rottenstreich A, Kalish Y, Elchalal U, Klimov A, Bloom AI. Retrievable inferior vena cava filter utilization in obstetric patients. J Matern-Fetal Neo M. (2019) 32:3045–53. doi: 10.1080/14767058.2018.1456521
14. Gonzalez-Mesa E, Azumendi P, Marsac A, Armenteros A, Molina N, Narbona I, et al. Use of a temporary inferior vena cava filter during pregnancy in patients with thromboembolic events. J Obstet Gynaecol. (2015) 35:771–6. doi: 10.3109/01443615.2015.1007928
15. Du Plessis LE, Mol BW, Svigos JM. The use of retrievable inferior vena cava filters in pregnancy: Another successful case report, but are we actually making a difference? Obstet Med. (2016) 9:102–5. doi: 10.1177/1753495X16648026
16. Abdul-Rahim O, Weinstein J, Brady P. Comments on: inferior vena cava filters in pregnancy: a systematic review. J Vasc Interv Radiol. (2016) 27:1774–6. doi: 10.1016/j.jvir.2016.05.021
17. Takahashi N, Isoda K, Hiki M, Fujimoto S, Daida H. Thrombolytic therapy and aspiration of clots were effective in the removal of a transient inferior vena cava (IVC) filter that captured a large thrombus. Intern Med. (2017) 56:1369–73. doi: 10.2169/internalmedicine.56.8175
18. Tajima H, Kasai H, Sugiura T, Tatsumi K. Pulmonary arteriovenous fistula complicated by venous thromboembolism and paradoxical cerebral infarction during early pregnancy. BMJ Case Rep. (2018) 2018:bcr-2017. doi: 10.1136/bcr-2017-222519
19. Harris SA, Velineni R, Davies AH. Inferior vena cava filters in pregnancy: a systematic review. J Vasc Interven Radiol. (2016) 27:354-60.e8. doi: 10.1016/j.jvir.2015.11.024
20. Kawamata K, Chiba Y, Tanaka R, Higashi M, Nishigami K. Experience of temporary inferior vena cava filters inserted in the perinatal period to prevent pulmonary embolism in pregnant women with deep vein thrombosis. J Vasc Surg. (2005) 41:652–6. doi: 10.1016/j.jvs.2005.01.023
21. Narayan H, Cullimore J, Krarup K, Thurston H, Macvicar J, Bolia A. Experience with the Cardial inferior vena cava filter as prophylaxis against pulmonary embolism in pregnant women with extensive deep venous thrombosis. Br J Obstet Gynaecol. (1992) 99:637–40. doi: 10.1111/j.1471-0528.1992.tb13845.x
22. Owen RJ, Krarup KC. Case report: the successful use and removal of the Gunther Tulip inferior vena caval filter in pregnancy. Clin Radiol. (1997) 52:241–3. doi: 10.1016/S0009-9260(97)80283-8
23. Kelly IMG, Boyd CS. Buckling of the tethering catheter causes migration of a temporary caval filter to the right atrium. Clin Radiol. (1999) 54:398–401. doi: 10.1053/crad.1999.0206
24. Aburahma AF, Boland JP. Management of deep vein thrombosis of the lower extremity in pregnancy: a challenging dilemma. Am Surg. (1999) 65:164–7.
25. AbuRahma AF, Mullins DA. Endovascular caval interruption in pregnant patients with deep vein thrombosis of the lower extremity. J Vasc Surg. (2001) 33:375–8. doi: 10.1067/mva.2001.111488
26. Ferraro F, D'Ignazio N, Matarazzo A, Rusciano G, Iannuzzi M, Belluomo Anello C. Thromboembolism in pregnancy: a new temporary caval filter. Minerva Anestesiol. (2001) 67:381–5.
27. Brenner C, Molloy M, McEniff N. Use of inferior vena cava filters in thromboembolic disease two case reports with a literature review. Ir Med J. (2001) 94:267–8.
28. Ishikawa T, Okabe T, Ogawa K, Fuse J, Oshiba Y, Ono A, et al. Usefulness of a second temporary vena cava filter for preventing acute pulmonary thromboembolism. Circ J. (2003) 67:718–20. doi: 10.1253/circj.67.718
29. Burov VP, Kapranov SA. Temporary placement of the cava filter to the suprarenal segment of the inferior vena cava. Angiol Sosud Khir. (2005) 11:45–7.
30. Clark SL, Blatter DD, Jackson GM. Placement of a temporary vena cava filter during labor. Am J Obstet Gynecol. (2005) 193:1746–7. doi: 10.1016/j.ajog.2005.05.014
31. Ioakeimidou C, Aziz AI. To filter or not to filter the inferior vena cava in pregnancy? Case Rep J Obstet Gynaecol. (2005) 25:310. doi: 10.1080/01443610500106553
32. Cheung MC, Asch MR, Gandhi S, Kingdom JC. Temporary inferior vena caval filter use in pregnancy. J Thromb Haemost. (2005) 3:1096–7. doi: 10.1111/j.1538-7836.2005.01299.x
33. Jamjute P, Reed N, Hinwood D. Use of inferior vena cava filters in thromboembolic disease during labor: case report with a literature review. J Matern Fetal Neonatal Med. (2006) 19:741–4. doi: 10.1080/14767050600631443
34. Opara E, Gile J, Zaidi J. Inferior vena cava filter thrombo-prophylaxis in high-risk twin pregnancy. Int J Gynaecol Obstet. (2007) 98:62–3. doi: 10.1016/j.ijgo.2006.11.027
35. Sendon S, Deruelle P, Dalmas AF, Lions C, Legrand A. Use of temporary inferior vena cava filter placement in pregnant women near term. Eur J Obstet Gyn R B. (2008) 140:143–4. doi: 10.1016/j.ejogrb.2007.10.013
36. Gupta S, Ettles DF, Robinson GJ, Lindow SW. Inferior vena cava filter use in pregnancy: preliminary experience. Bjog-Int J Obstet Gy. (2008) 115:785–8. doi: 10.1111/j.1471-0528.2008.01704.x
37. Kocher M, Krcova V, Cerna M, Prochazka M. Retrievable Gunther Tulip Vena Cava Filter in the prevention of pulmonary embolism in patients with acute deep venous thrombosis in perinatal period. Eur J Radiol. (2009) 70:165–9. doi: 10.1016/j.ejrad.2007.12.011
38. Milford W, Chadha Y, Lust K. Use of a retrievable inferior vena cava filter in term pregnancy: case report and review of literature. Aust N Z J Obstet Gynaecol. (2009) 49:331–3. doi: 10.1111/j.1479-828X.2009.01004.x
39. McConville RM, Kennedy PT, Collins AJ, Ellis P. Failed retrieval of an inferior vena cava filter during pregnancy because of filter tilt: report of two cases. Cardiovasc Inter Rad. (2009) 32:174–7. doi: 10.1007/s00270-008-9393-6
40. Lonjaret L, Lairez O, Galinier M, Minville V. Thrombolysis by recombinant tissue plasminogen activator during pregnancy: a case of massive pulmonary embolism. Am J Emerg Med. (2011) 29:694 e1–2. doi: 10.1016/j.ajem.2010.05.022
41. Liu Y, Sun Y, Zhang S, Jin X. Placement of a retrievable inferior vena cava filter for deep venous thrombosis in term pregnancy. J Vasc Surg. (2012) 55:1042–7. doi: 10.1016/j.jvs.2011.10.107
42. Nakajima Y, Masaoka N, Tsuzuki Y, Morooka M, Sakai M. May-Thurner syndrome resulting in acute iliofemoral deep vein thrombosis during the second trimester of pregnancy. J Obstet Gynaecol Res. (2012) 38:1106–10. doi: 10.1111/j.1447-0756.2011.01840.x
43. Valadares S, Serrano F, Torres R, Borges A. Inferior vena cava filter placement during pregnancy: an adjuvant option when medical therapy fails. Case Rep Obstet Gynecol. (2013) 2013:821635. doi: 10.1155/2013/821635
44. Yamagami T, Yoshimatsu R, Okubo T, Tanaka O, Miura H, Yamada K, et al. Symptomatic deep venous thrombosis of the lower extremity in a pregnant woman successfully treated with endovascular procedures. J Obstet Gynaecol Res. (2013) 39:1059–64. doi: 10.1111/j.1447-0756.2012.02071.x
45. DeStephano CC, Werner EF, Holly BP, Lessne ML. Diagnosis and management of iliac vein thrombosis in pregnancy resulting from May-Thurner Syndrome. J Perinatol. (2014) 34:566–8. doi: 10.1038/jp.2014.38
46. Zeybek B, Terek MC, Guven C, Cinar C. Placement of a vena cava filter in term pregnancy: case report and review of the literature. Clin Exp Obstet Gynecol. (2011) 38:96–8.
47. Barnes AB, Kanarek DJ, Greenfield AJ, Brewster DC. Vena caval filter placement during pregnancy. Am J Obstet Gynecol. (1981) 140:707–8. doi: 10.1016/0002-9378(81)90209-X
48. Thomas LA, Summers RR, Cardwell MS. Use of greenfield filters in pregnant women at risk for pulmonary embolism. Southern Med J. (1997) 90:215–7. doi: 10.1097/00007611-199702000-00010
49. Neri E, Civeli L, Benvenuti A, Toscano T, Miraldi F, Capannini G, et al. Protected iliofemoral venous thrombectomy in a pregnant woman with pulmonary embolism and ischemic venous thrombosis. Tex Heart Inst J. (2002) 29:130–2.
50. Hynek K, Spalova I, Spatenka J, Mates M. Possibilities of using vena cava filters in pregnant women with venous thromboembolism. Case reports Sb Lek. (2002) 103:451–4.
51. Hux CH, Wapner RJ, Chayen B, Rattan P, Jarrell B, Greenfield L. Use of the Greenfield filter for thromboembolic disease in pregnancy. Am J Obstet Gynecol. (1986) 155:734–7. doi: 10.1016/S0002-9378(86)80009-6
52. Banfield PJ, Pittam M, Marwood R. Recurrent pulmonary embolism in pregnancy managed with the Greenfield vena caval filter. Int J Gynaecol Obstet. (1990) 33:275–8. doi: 10.1016/0020-7292(90)90015-D
53. Eagle CJ, Davies JM. Lethal air embolism during placement of a Kimray-Greenfield filter. J Cardiothorac Anesth. (1990) 4:616–20. doi: 10.1016/0888-6296(90)90412-9
54. Arbogast JD, Blessed WB, Lacoste H, Gross WS, Gonda RL, Welch RA. Use of two Greenfield caval filters to prevent recurrent pulmonary embolism in a heparin-allergic gravida. Obstet Gynecol. (1994) 84:652–4.
55. Neill AM, Appleton DS, Richards P. Retrievable inferior vena caval filter for thromboembolic disease in pregnancy. Br J Obstet Gynaecol. (1997) 104:1416–8. doi: 10.1111/j.1471-0528.1997.tb11015.x
56. Geary M, Lamont R. Retrievable inferior vena cava filter for thrombolic disease in pregnancy. Br J Obstet Gynaecol. (1998) 105:1039. doi: 10.1111/j.1471-0528.1998.tb10274.x
57. Ganguli S, Tham JC, Komlos F, Rabkin DJ. Fracture and migration of a suprarenal inferior vena cava filter in a pregnant patient. J Vasc Interven Radiol. (2006) 17:1707–11. doi: 10.1097/01.RVI.0000236717.27681.09
58. Hidaka N, Hachisuga M, Tsukimori K, Onohara T, Maehara Y, Wake N. Intrapartum placement of an inferior vena cava filter for a woman with hereditary antithrombin III deficiency: its role in the prevention of fatal pulmonary embolism. J Obstet Gynaecol Res. (2008) 34:95–9. doi: 10.1111/j.1447-0756.2007.00708.x
59. Sparrow PJ. Response to “Failed retrieval of an inferior vena cava filter during pregnancy because of filter tilt: report of two cases”. Cardiovasc Intervent Radiol. (2009) 32:388–9. doi: 10.1007/s00270-008-9452-z
60. Quayle SS, Germain MM, Wolf EJ, Miller RC. Case Report of Placement of a Bird's Nest Filter During Pregnancy. J Matern Fetal Med. (1994) 3:187–9. doi: 10.3109/14767059409017272
61. Horie K, Suzuki H, Ohkuchi A, Matsubara S, Ikemoto T, Suzuki M. Thrombus just beneath a retrievable inferior vena cava filter in a pregnant woman with deep vein thrombosis: its removal requiring catheter thrombus fragmentation with fibrinolysis. J Obstet Gynaecol Res. (2014) 40:590–4. doi: 10.1111/jog.12169
62. Adams E, Maguire N, Richmond D, Rowlands P. Retrievable inferior vena cava filter for thrombolic disease in pregnancy. Br J Obstet Gynaecol. (1998) 105:1039. doi: 10.1111/j.1471-0528.1998.tb10273.x
63. Bistervels IM, Geerlings AE, Bonta PI, Ganzevoort W, Zijlstra IAJ, Middeldorp S. Pregnancy in women with an inferior vena cava filter: a tertiary center experience and overview of the literature. Blood Adv. (2021) 5:4044–53. doi: 10.1182/bloodadvances.2020003930
64. Lin HY, Lin CY, Shen MC. Review article inferior vena cava thrombosis: a case series of patients observed in Taiwan and literature review. Thromb J. (2021) 19:43. doi: 10.1186/s12959-021-00296-5
65. Maijub JG, Ross CB, Houser MV, Morris ME. Fetal demise due to uterine trauma with massive intraperitoneal hemorrhage associated with chronic perforation of the inferior vena cava by an infrarenal filter: a case report with call for definitive consensus regarding filter positioning in nonpregnant women of childbearing age. J Vasc Surg. (2012) 56:1823. doi: 10.1016/j.jvs.2012.10.039
66. Lee BS, Selvaratnam V, Sathar J, Yap YY, Fann RJ. She Won't Stop Clotting Despite on Anticoagulants: A Challenging Case (2019).
67. Bourjeily G, Paidas M, Khalil H, Rosene-Montella K, Rodger M. Pulmonary embolism in pregnancy. Lancet. (2010) 375:500–12. doi: 10.1016/S0140-6736(09)60996-X
68. Bates SM, Rajasekhar A, Middeldorp S, McLintock C, Rodger MA, James AH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. (2018) 2:3317–59. doi: 10.1182/bloodadvances.2018024802
69. Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO, et al. thrombophilia, antithrombotic therapy, and pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. (2012) 141:e691S−736S. doi: 10.1378/chest.11-2300
70. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ. 3rd. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. (2005) 143:697–706. doi: 10.7326/0003-4819-143-10-200511150-00006
71. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. (2006) 194:1311–5. doi: 10.1016/j.ajog.2005.11.008
72. Muriel A, Jimenez D, Aujesky D, Bertoletti L, Decousus H, Laporte S, et al. Survival effects of inferior vena cava filter in patients with acute symptomatic venous thromboembolism and a significant bleeding risk. J Am Coll Cardiol. (2014) 63:1675–83. doi: 10.1016/j.jacc.2014.01.058
73. Casazza F, Becattini C, Bongarzoni A, Cuccia C, Roncon L, Favretto G, et al. Clinical features and short term outcomes of patients with acute pulmonary embolism. The Italian Pulmonary Embolism Registry (IPER) Thromb Res. (2012) 130:847–52. doi: 10.1016/j.thromres.2012.08.292
74. Tardy B, Mismetti P, Page Y, Decousus H, Da Costa A, Zeni F, et al. Symptomatic inferior vena cava filter thrombosis: clinical study of 30 consecutive cases. Eur Respir J. (1996) 9:2012–6. doi: 10.1183/09031936.96.09102012
75. Kalaitzopoulos DR, Panagopoulos A, Samant S, Ghalib N, Kadillari J, Daniilidis A, et al. Management of venous thromboembolism in pregnancy. Thromb Res. (2022) 211:106–13. doi: 10.1016/j.thromres.2022.02.002
76. Mismetti P, Laporte S, Pellerin O, Peck-Palmer OM, Barnato AE, Weissfeld LA, et al. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA. (2015) 313:1627–35. doi: 10.1001/jama.2015.3780
77. Lagana D, Carrafiello G, Lumia D, Vizzari FA, Xhepa G, Mangini M, et al. Removable vena cava filter: single-centre experience with a single device. Radiol Med. (2013) 118:816–25. doi: 10.1007/s11547-012-0893-7
78. Decousus H, Barral FG, Buchmuller-Cordier A, et al. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism—The PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. (2005) 112:416–22. doi: 10.1161/CIRCULATIONAHA.104.512834
79. Miyahara T, Miyata T, Shigematsu K, Deguchi J, Kimura H, Ishii S, et al. Clinical outcome and complications of temporary inferior vena cava filter placement. J Vasc Surg. (2006) 44:620–4. doi: 10.1016/j.jvs.2006.05.019
Keywords: venous thromboembolism, pregnancy, safety, anticoagulants, vena cava filter
Citation: Bistervels IM, Buchmüller A and Tardy B (2022) Inferior vena cava filters in pregnancy: Safe or sorry? Front. Cardiovasc. Med. 9:1026002. doi: 10.3389/fcvm.2022.1026002
Received: 23 August 2022; Accepted: 19 October 2022;
Published: 07 November 2022.
Edited by:
Nicola Mumoli, ASST Ovest Milanese, ItalyCopyright © 2022 Bistervels, Buchmüller and Tardy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernard Tardy, YmVybmFyZHRhcmR5QHlhaG9vLmZy
†ORCID: Ingrid M. Bistervels orcid.org/0000-0002-1155-4143
Andrea Buchmüller orcid.org/0000-0002-4254-5362
Bernard Tardy orcid.org/0000-0002-4655-0652
 Ingrid M. Bistervels
Ingrid M. Bistervels Andrea Buchmüller
Andrea Buchmüller Bernard Tardy
Bernard Tardy