- 1The Fourth School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, China
- 2Department of Cardiology, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 3Department of Translation Medicine Center, Affiliated Hangzhou First People’s Hospital, Zhejiang University School of Medicine, Hangzhou, China
Background: Coronary microvascular dysfunction (CMD) may play an important role in various cardiovascular diseases, including HFpEF and both obstructive and non-obstructive coronary artery disease (CAD). To date, there has been no bibliometric analysis to summarize this field. Here, we aim to conduct a bibliometric analysis of CMD to determine the current status and frontiers in this field.
Materials and methods: Publications about CMD were taken from the Web of Science Core Collection database (WOSCC). WOSCC’s literature analysis wire, the VOSviewer 1.6.16, and CiteSpace 5.1.3 were used to conduct the analysis.
Results: A total of 785 publications containing 206 reviews and 579 articles are included in the sample. The leading authors are Iacopo Olivotto, Paolo G. Camici, and Carl J. Pepine. The most productive institutions are the University of Florence, Cedars Sinai Medical Center, and Harvard University. The most productive countries are the USA, Italy, and England. There are a total of 237 journals that contribute to this field, and the leading journals in our study were the International Journal of Cardiology, the European Heart Journal and the JACC. From 2012 to 2021, the top three most-cited articles focused on the association between HFpEF and CMD. The important keywords are heart failure, hypertrophic cardiomyopathy, chest pain, women, coronary flow reserve (CFR), endothelial dysfunction and prognostic value. “Positron emission tomography” shows the strongest burst strength, followed by “blow flow” and “artery.” The keywords that started to burst from 2015 are particularly emphasized, including “heart failure,” “coronary flow reserve,” and “management.”
Conclusion: Studies about CMD are relatively limited, and the largest contribution comes from the USA, Italy and England. More studies are needed, and publications from other countries should be enhanced. The main research hotspots in the CMD field include CMD in patients with HFpEF, sex differences, the new methods of diagnosis for CMD, and the effective treatment of CMD. Attention should be given to CMD in patients with HFpEF, and untangling the association between CMD and HFpEF could be helpful in the development of physiology-stratified treatment for patients with CMD and HFpEF.
Introduction
Coronary microvascular dysfunction (CMD) is an underdiagnosed and underrecognized condition that is related to an increased incidence of adverse cardiac events (1–4). CMD could present as chest pain with imaging abnormalities and/or electrocardiographic changes evident in stress testing but without obstructive coronary artery disease on angiography. The risk factors for CMD are similar to those for coronary artery disease (CAD), including chronic inflammation, hyperlipidemia, hyperglycemia, hypertension, and aging (1, 5–7). CMD could be diagnosed by the use of non-invasive coronary assessment via PET, CMR, or echocardiography and invasive coronary assessment via doppler or thermodilution. The treatment of CMD encompasses antianginal medications including ranolazine, ivabradine, and nicorandil, anti-atherosclerotic drugs including statins, ACEIs, and calcium-channel blockers, and some non-pharmacological treatments including a well-balanced diet, lifestyle modifications, cognitive behavioral therapy (CBT) and enhanced external counterpulsation (5).
Coronary microvascular dysfunction can be divided into four types including dysfunction in the presence of obstructive CAD, dysfunction due to myocardial diseases, dysfunction in the absence of myocardial and CAD diseases, and iatrogenic dysfunction. CMD is prevalent across various cardiovascular diseases (CVDs) including non-ischemic cardiomyopathies, angina with and without obstructive CAD, takotsubo syndrome, myocardial infarction, and heart failure (HF). Among them, CMD in heart failure with HFpEF has drawn increasing attention. In Shah’s study, the high prevalence of CMD in HFpEF (75%) was demonstrated (8). Taqueti et al. found that impaired CFR in symptomatic patients without overt CAD was independently associated with adverse events such as HFpEF hospitalization (9). In specific populations, CMD may have a pathophysiological and prognostic role. Previous studies have shown that CMD may play an important role in different cardiovascular diseases including HFpEF, obstructive and non-obstructive CAD. To date, there has been no bibliometric analysis to summarize this field. We aim to conduct a bibliometric analysis of CMD to determine the current status and frontiers in this field.
Materials and methods
Search strategy
The WoSCC has been widely used for bibliometric analysis widely (10, 11). In our study, publications about CMD were taken from the WoSCC. The search term used was TS = “coronary microvascular dysfunction” OR “Coronary Microvascular Endothelia Inflammation” OR “Coronary Microvascular Rarefaction” OR “coronary microvascular endothelial dysfunction.” The search results were narrowed by publication data including a date range of: 1 January 2000 to 31 December 2021, a publication language of English and the article types of reviews and articles.
Data collection and analysis
The VOSviewer 1.6.16 (Rotterdam, Netherlands), CiteSpace 5.1.3 (Philadelphia, PA, USA), and WoSCC literature analysis wire were used to conduct the our study’s analysis (12, 13). The h-index was used to evaluate the citations of the selected publications. In our study, VOSviewer1.6.16 software was used to determine co-authorship keywords, authors, countries/regions, and institutions. Publication year, document type, categories, the distribution of authors, country/region, institutions, and h-index were analyzed by the WoSCC literature analysis wire. CiteSpace 5.1.3 was used to the burst detection analysis of keywords. Total link strength (TLS) was used to evaluate the cooperation relationship.
Results
Publication output
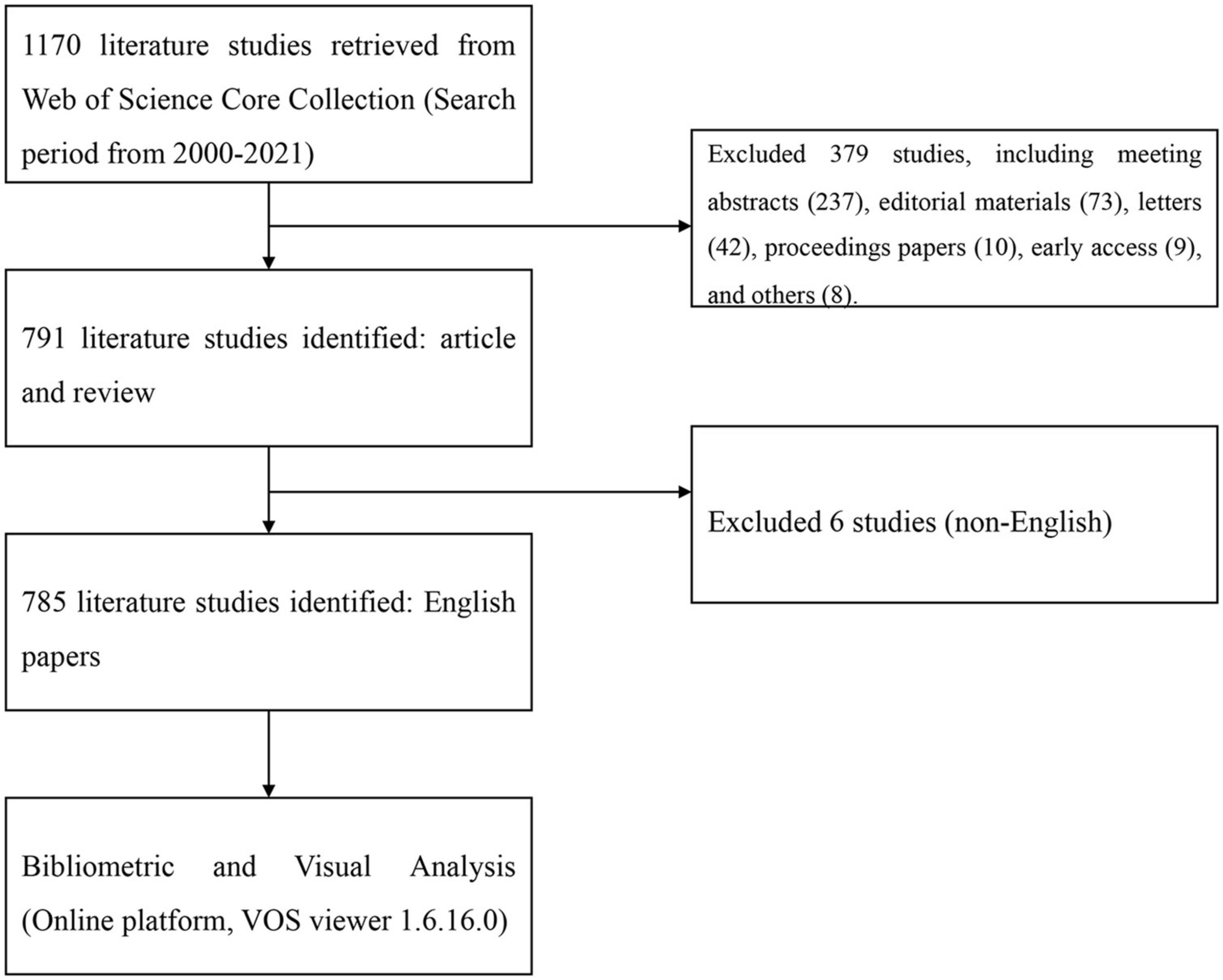
A total of 785 publications containing 206 reviews and 579 articles were included (Figure 1). The publications generally showed an upward trend from 2006. The major subject categories were cardiac cardiovascular systems (505 publications), peripheral vascular disease (103 publications), radiology nuclear medicine medical imaging (99 publications), medicine general internal (43 publications), and pharmacology pharmacy (38 publications), which is shown in Figure 2.
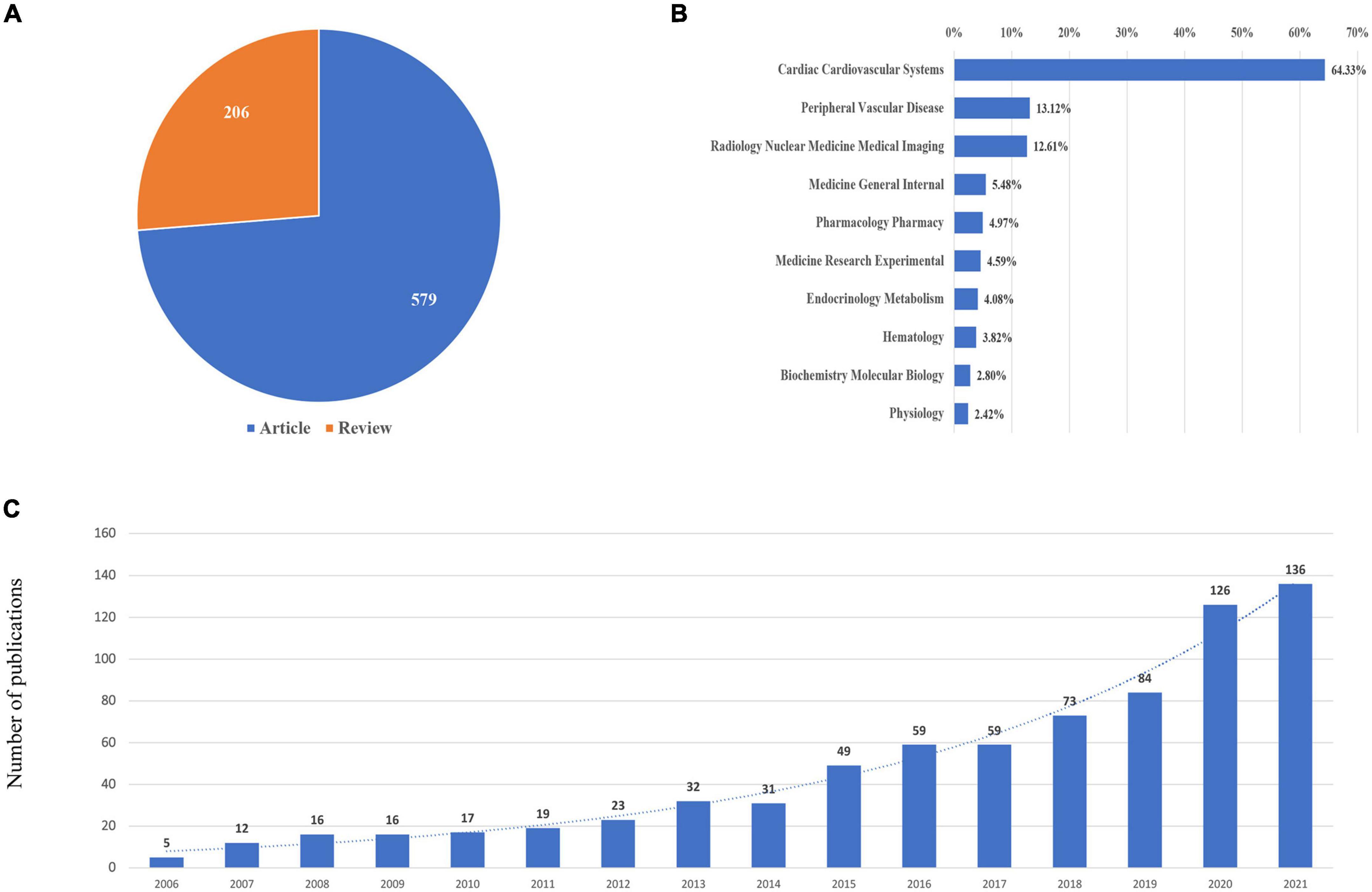
Figure 2. Yearly quantity and literature type of publications on CMD from 2000 to 2021. (A) Literature types distribution. (B) Subject categories distribution. (C) Annual publications quantitative distribution.
Distribution of authors
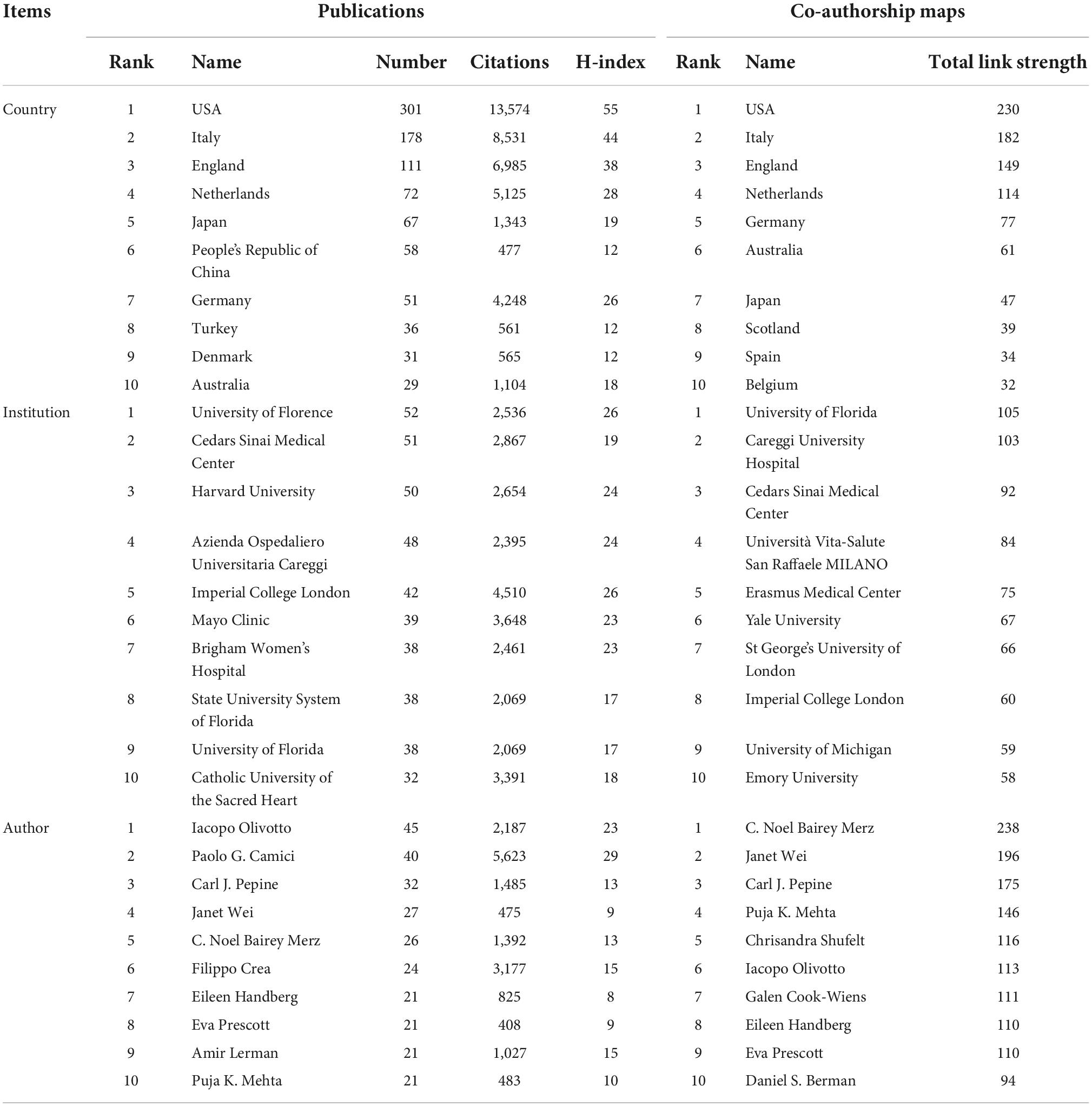
From this field, a total of 4,207 authors were included. Among them, Iacopo Olivotto was the leading author from Italy with 45 publications, followed by Paolo G Camici with 40 publications, Carl J Pepine with 32 publications, Janet Wei with 27 publications, and C Noel Bairey Merz with 26 publications. Paolo G Camici, Filippo Crea, and Iacopo Olivotto were the most highly cited authors. The uppermost h-index value was for Paolo G Camici (h-index: 29), followed by Iacopo Olivotto (h-index: 23), Filippo Crea (h-index: 15) and Amir Lerman (h-index: 15). The coauthorship map of authors is shown in Figure 3A. The top three coauthorship triads of authors were C Noel Bairey Merz (TLS = 238), Janet Wei (TLS = 196) and Carl J. Pepine (TLS = 175).
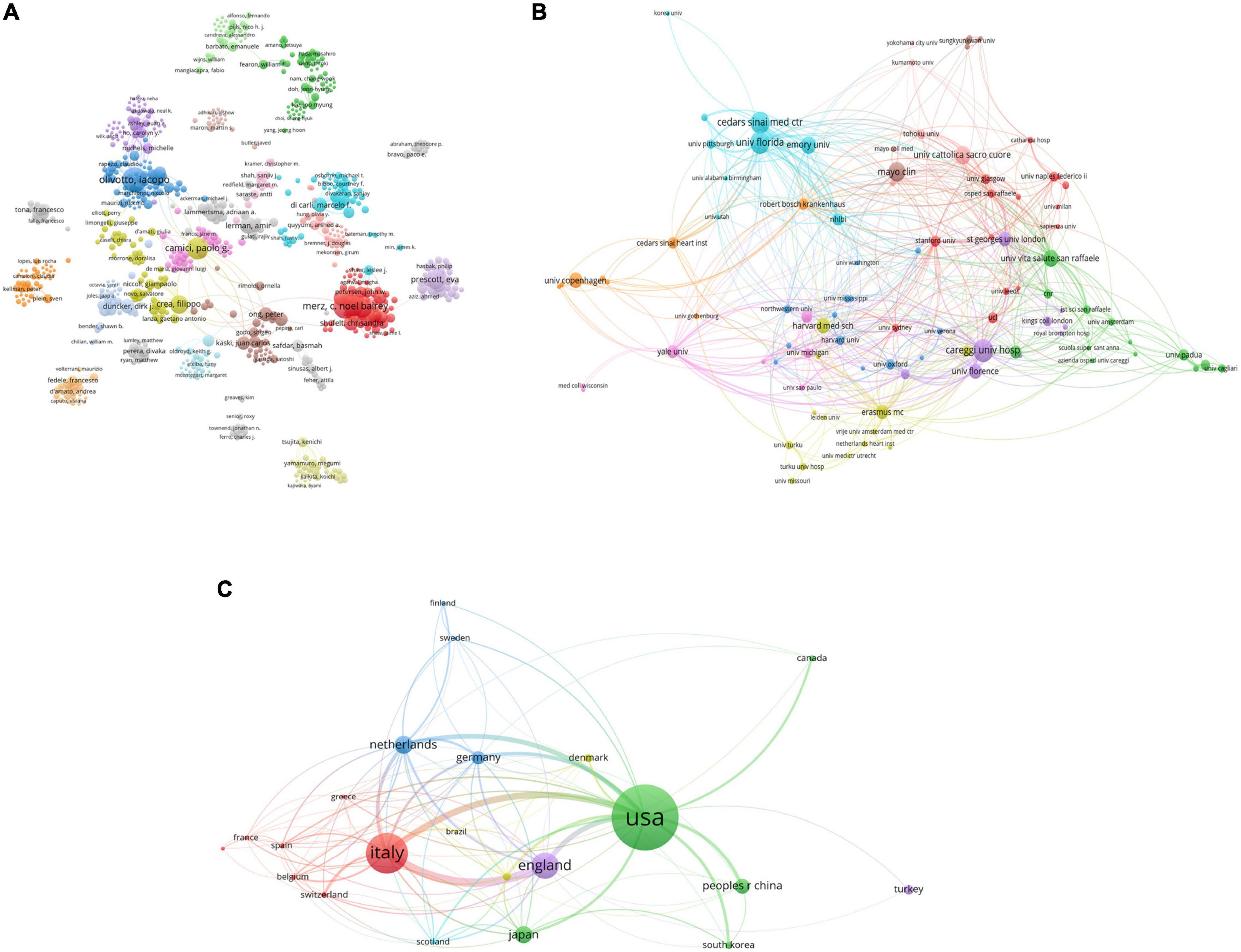
Figure 3. Visualization knowledge maps of the co-authorship. (A) The co-authorship map of authors which indicates the authors that cooperate in the field of CMD; (B) the co-authorship map of organizations. The institution with the strongest total link strength is the University of Florida. (C) The co-authorship map of countries. The number of collaborators with the USA is 300 and the total link strength is 230. Different colors indicate different clusters and the size of nodes indicates the number of publications. The thickness of the lines represents the link strength of the countries.
Distribution by countries/regions and institutions
All publications were taken from 48 countries/regions and 1,064 organizations. The most productive institutions were the University of Florence (52 publications with 2,536 citations), the Cedars Sinai Medical Center (51 publications with 2,867 citations), Harvard University (50 publications with 2,654 citations), the Azienda Ospedaliero Universitaria Careggi (48 publications with 2,395 citations), and Imperial College London (42 publications with 4,510 citations). The coauthorship map of institutions is shown in Figure 3B. The top three institutions involved in coauthorship were the University of Florida, Careggi University Hospital and Cedars Sinai Medical Center. For countries/regions, the USA had the most publications (301 documents), followed by Italy (178 documents), England (111 documents), Netherlands (72 documents), and Japan (67 documents). The top three countries/regions involved in coauthorship were the USA, Italy, and England. The coauthorship map of countries/regions and the top 10 high-yield countries/regions, institutions and authors are summarized in Figure 3C and Table 1.
Distribution by journal
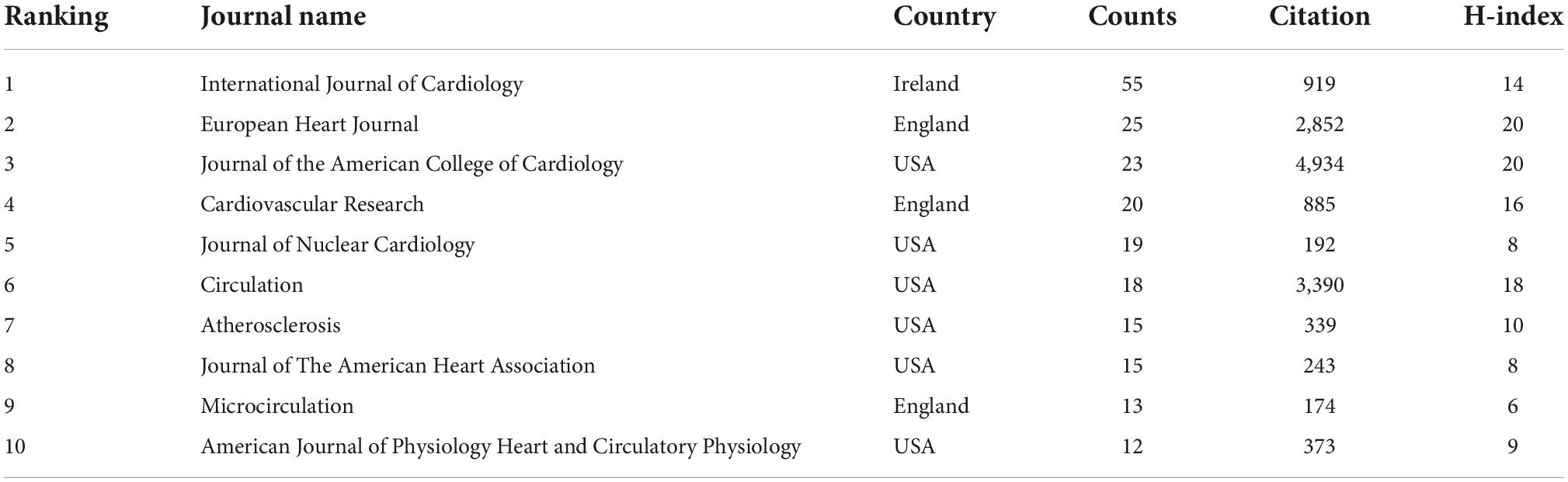
A total of 237 journals contribute to this field. Among them, the International Journal of Cardiology was the leading journal with 55 documents, followed by EHJ with 25 documents and JACC with 23 documents. The coauthorship map of journals and the top 10 high-yield journals are summarized in Figure 4A and Table 2.
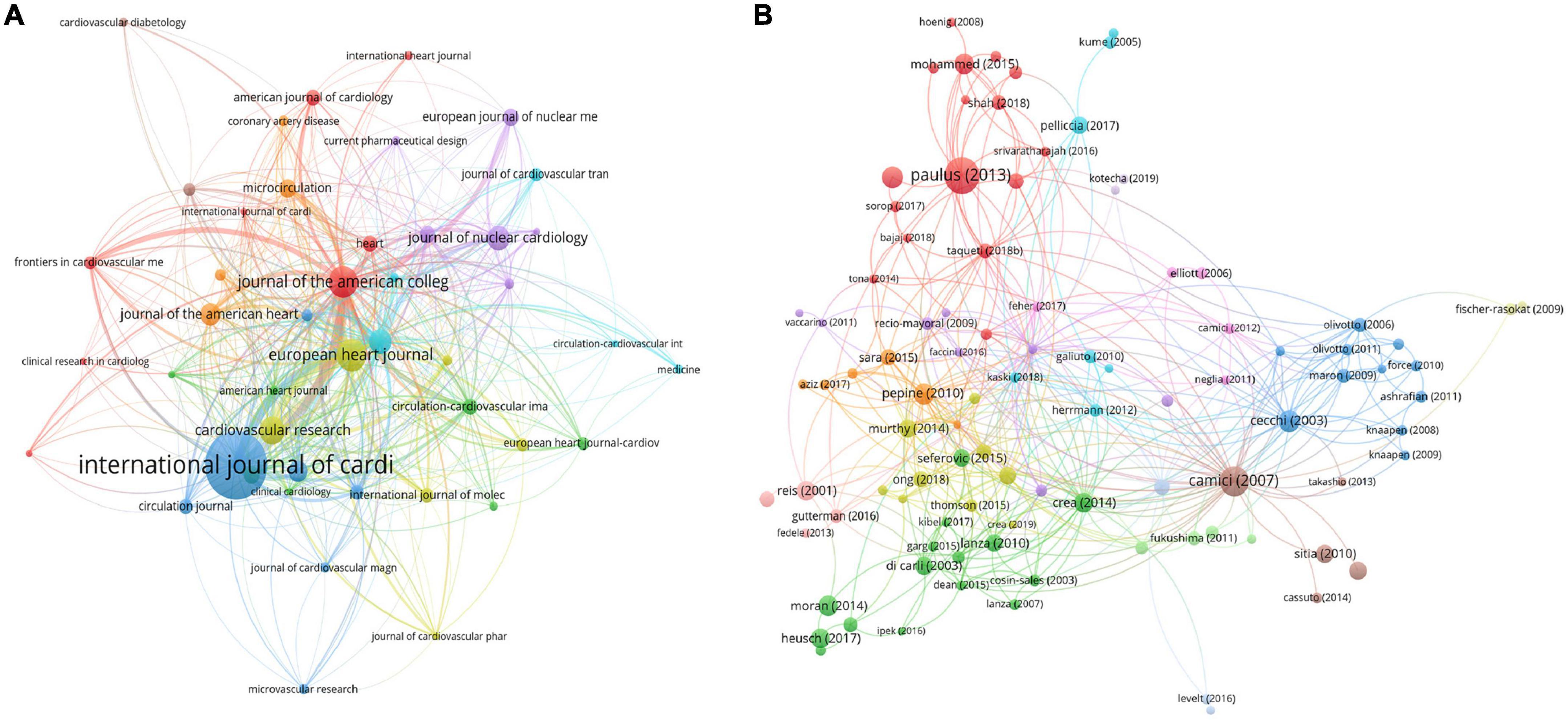
Figure 4. Visualization knowledge maps of citation. (A) Citation map of Journal; (B) citation map of documents. Different color indicates different clusters. The size of the nodes represents the counts of citations. The distance between the two nodes indicates their correlation.
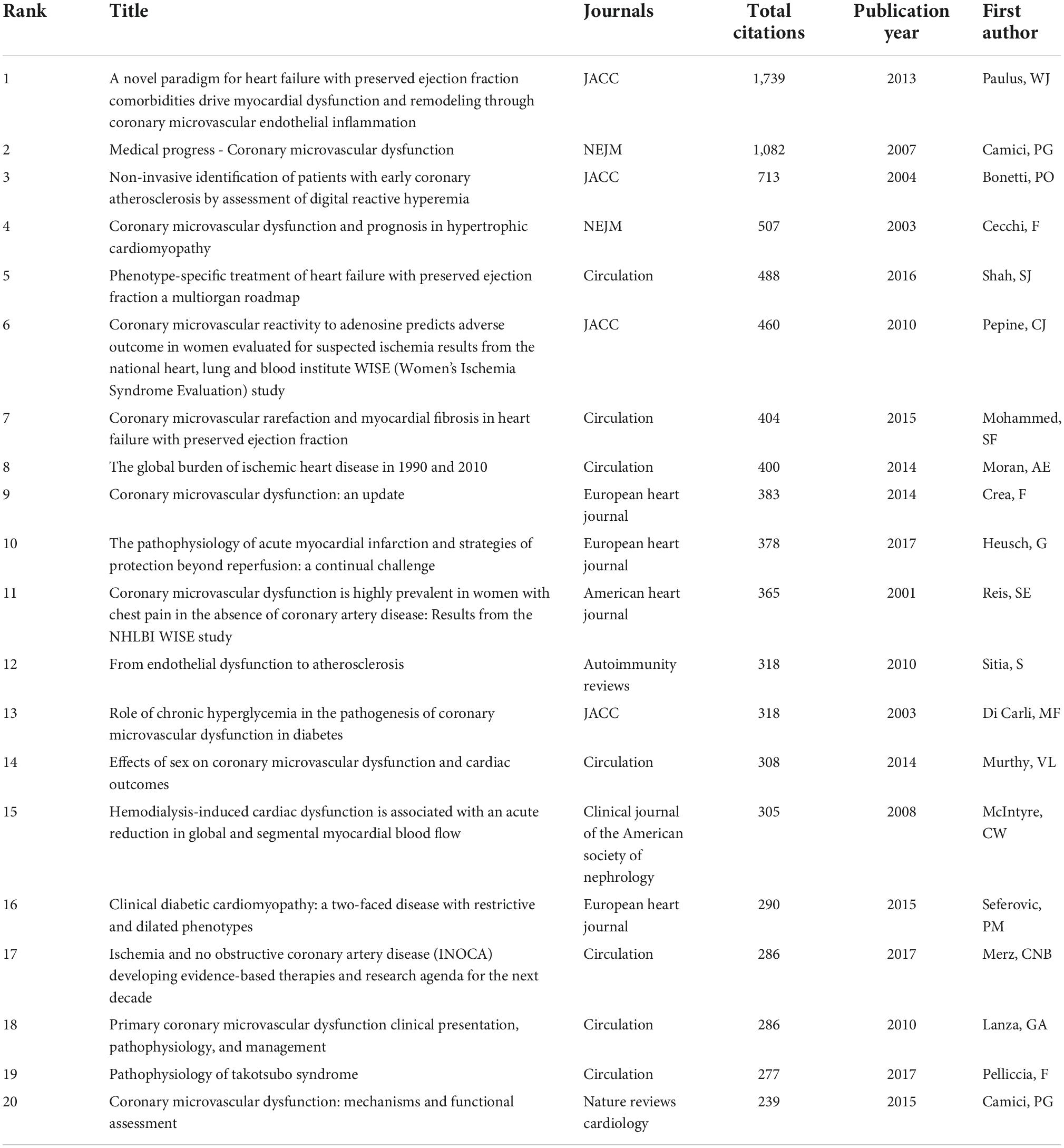
Analysis of high-cited references
The characteristics of publications were summarized in Table 3 (1, 14–32). The most-cited reference was published in the JACC and authored by Paulus W. J. and Tschope C. The second most-cited reference was published in NEJM and authored by Paolo G. Camici and Filippo Crea in 2007. The third most-cited reference was published in the JACC and authored by Piero O. Bonetti et al in 2004. To explore the hotspots in this field over recent years, we summarize the top three most highly cited articles in the last decade (2012–2021) The most highly cited article was published in the JACC by Paulus W. J. in 2013 (26). In this article, Paulus first proposed the association between CMD and HFpEF, which differs from that between HFpEF and HFrEF. Attention should be given to this new HFpEF paradigm of CMD with potential important diagnostic and therapeutic implications. The second most highly cited article was published by Shah S. J. in 2016 (31). Shah believed that CMD played an important role in HFPEF and proposed personalized therapeutic strategies. The third most cited article was published by Mohammed SF in 2015, who found that patients with HFpEF had coronary microvascular rarefaction compared with controls following autopsy. The citation map of documents is shown in Figure 4B.
Analysis of keywords co-occurrence clusters
Figure 5 shows the co-occurrence map of keywords, and four research directions are also shown. The green cluster includes heart failure, hypertrophic cardiomyopathy, and disease. The red cluster includes artery disease, chest pain, women, and cardiac syndrome. The blue cluster includes coronary flow reserve (CFR), endothelial dysfunction, and inflammation. The yellow cluster includes blow flow, PET, and prognostic value.
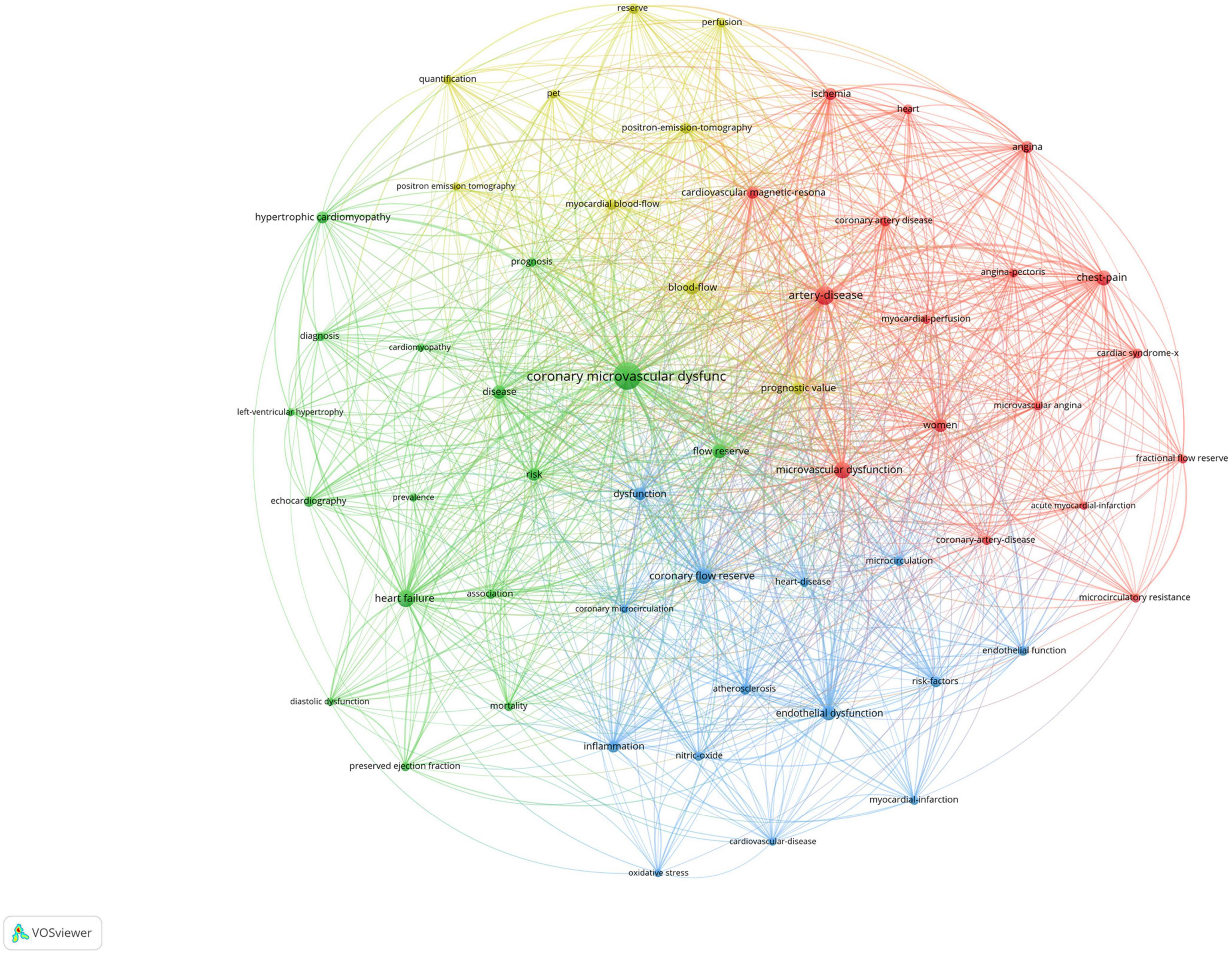
Figure 5. Visualization of keyword co-occurrence analysis. The size of nodes indicates the frequency of occurrences of the keywords. The lines between the nodes represent their co-occurrence in the same publication. The shorter the distance between two nodes, the larger the number of co-occurrence of the two keywords.
Burst detection of keywords
CiteSpace 5.1.3 is used to perform burst detection of keywords. The burst detection analysis of keywords can predict frontier research directions, reflect emerging academic trends, and display the hotspots in a field. Twenty prominent words were obtained by the burst detection analysis. “Positron emission tomography” shows the strongest burst strength, followed by “blow flow” and “artery.” The keywords that started to burst from 2015 are particularly emphasized, including “heart failure” (burst strength 4.98), “coronary flow reserve” (burst strength 4.79), and “management” (burst strength 4.47), which is shown in Figure 6.
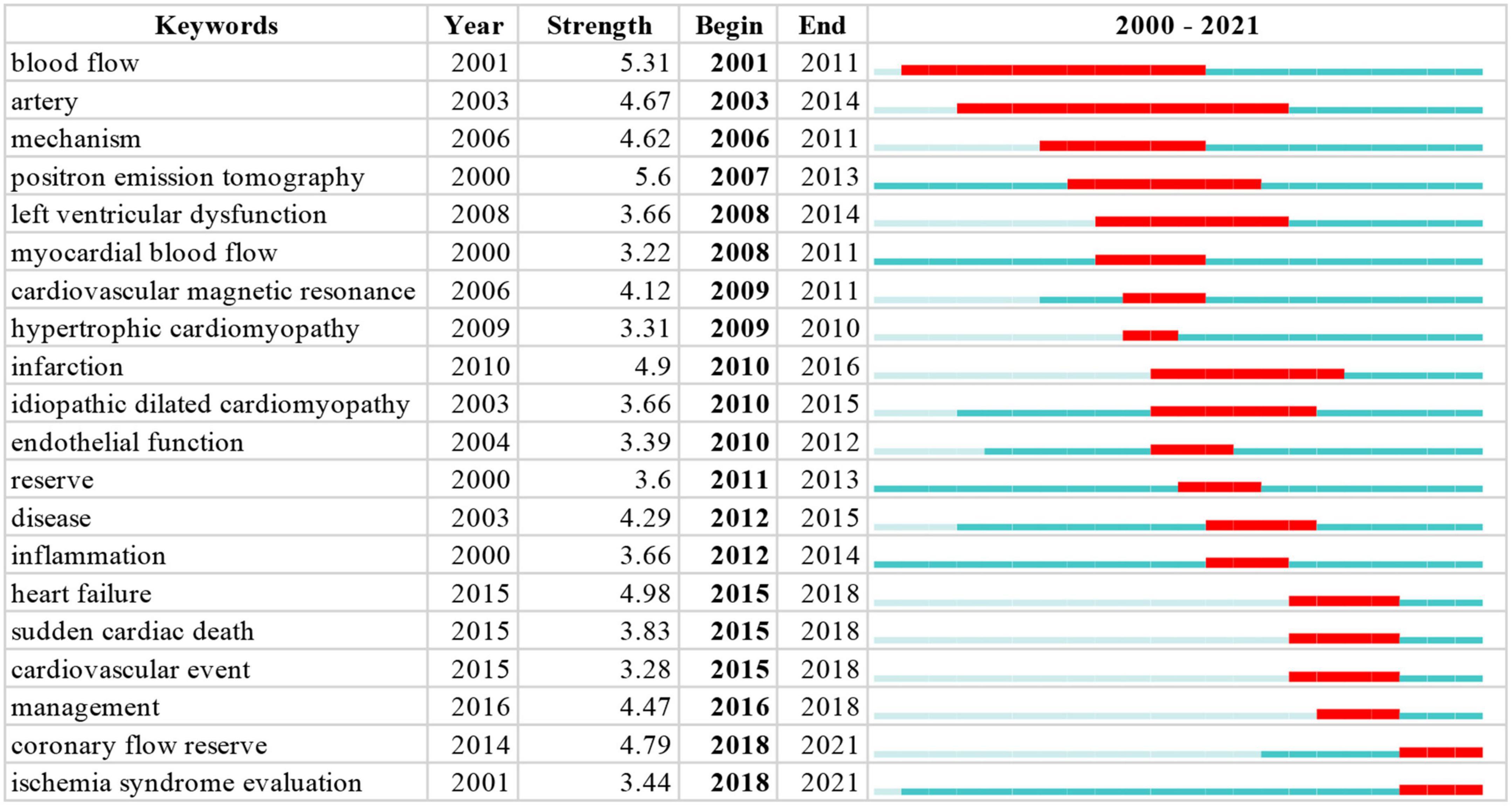
Figure 6. Top 20 Keywords with the strongest citation bursts. The blue indicates the timeline. The red segment indicates the start year, end year, and duration of the burst.
Discussion
General information
To the best of our knowledge, this is the first bibliometric study in the field of CMD. A total of 785 publications are included. The leading authors are Iacopo Olivotto, Paolo G Camici and Carl J Pepine. The uppermost h-index value is for Paolo G. Camici, followed by Iacopo Olivotto, Filippo Crea, and Amir Lerman. The top three authors involved in coauthorship are C. Noel Bairey Merz, Janet Wei and Carl J. Pepine. All publications are taken from 48 countries/regions and 1,064 organizations. The most productive institutions are the University of Florence, the Cedars Sinai Medical Center, and Harvard University. The most productive countries are the USA, Italy, and England. The top three institutions involved in coauthorship are the University of Florida, Careggi University Hospital and Cedars Sinai Medical Center, and the top three countries/regions involved in coauthorship are the USA, Italy, and England. A total of 237 journals contribute to this field, and the leading journals are the International Journal of Cardiology, EHJ and JACC. From 2012 to 2021, the top three most-cited articles focused on the association between HFpEF and CMD. The important keywords used in this study are heart failure, hypertrophic cardiomyopathy, chest pain, women, CFR, endothelial dysfunction and prognostic value. “Positron emission tomography” shows the strongest burst strength, followed by “blow flow” and “artery.” The keywords that started to burst from 2015 are particularly emphasized, including “heart failure,” “coronary flow reserve,” and “management.”
Most of the included publications come from the USA, Italy, and England (590/785, 75.2%). Of the top 10 productive authors, six were from the USA, and the remaining four were from Italy. Of the top 10 institutions, 6 were from the USA, 3 were from Italy, and 1 was from England. Among cooperative relationships of authors, institutions and countries/regions, the USA, Italy and England were also prominent. The prominent countries in this field were again the USA, Italy, and England. Studies from and cooperation among other countries should be enhanced.
Hotspots and frontiers
In accordance with the most cited references and the important keywords, the research frontiers and hotspots were found to be as follows: (1) The first relates to sex difference among CMD patients. Among the most-cited references, three explored sex differences in CMD patients (25, 28, 29). The keyword of women was in the red cluster. In the Women’s Ischemia Syndrome Evaluation (WISE) study (29, 33, 34). The keyword “women” occurred in the red cluster. The results of the Women’s Ischemia Syndrome Evaluation (WISE) study demonstrated that CMD was present in approximately 50% of women with NOCAD and chest pain. Murthy et al showed that CMD was highly prevalent in both men and women who were at-risk, and was associated with adverse outcomes irrespective of sex (25). Kobayashi et al. found that the microvascular function was similar in men and women (35). Recently, Chandramouli et al found that the drivers of CMD may differ by sex, but the prevalence of CMD in HFpEF was similar in women and men. They demonstrated that fibrosis and derangement in ventricular remodeling potentially predominate in women while the inflammatory paradigm of CMD seems to play a more important role in men (36). Based on recent evidence, the prevalence of CMD were similar in both women and men, but the mechanisms might be different, which should be considered in future therapeutic interventions. (2) The next hotspot involves the new methods of diagnosis for CMD. Among the most-cited references, four explored the diagnosis of CMD (1, 14, 15, 17). The keywords of coronary flow reserve, blow flow, PET, and prognostic value occur in the blue and yellow clusters. The diagnosis of CMD is usually made by the measurement of CFR or IMR with invasive coronary assessment via Doppler or thermodilution or CFR with non-invasive coronary assessment via PET, CMR, or echocardiography (37). the approaches of diagnosis for CMD are limited, and new methods are needed. A recent systematic review and meta-analysis showed that CFR was related to the rate of major adverse cardiovascular events (MACE) and all-cause mortality, and suggested that, CFR should be measured more routinely in clinical practice (38). In addition, coronary flow velocity reserve (CFVR) as assessed by echocardiography to evaluate the CMD is feasible and could predict the adverse outcomes in women with no obstructive CAD and angina (39). More diagnostic approaches are being developed. (3) The next hotspot involves the effective treatment of CMD, which was explored by five of the most cited references (15, 17, 20, 22, 31). The treatment of CMD includes the use of antianginal drugs, anti-atherosclerotic medication, and new therapeutic strategies such as phosphodiesterase-5 inhibitors and ivabradine (40–43). It is necessary to explore more effective treatments for CMD in further studies. In this regard, it is essential to distinguish between endothelium-independent and endothelium-dependent CMD since they may require different treatments. (4) The final hotspot involves CMD in HFpEF. Among the most-cited references, three explored the association between CMD and HFpEF (23, 26, 31), and all top three most-cited articles over recent 10 years were about it (23, 26, 31). The keyword of heart failure occurs in the green cluster. In 2013, the association between CMD and HFpEF was first proposed. In 2016, Kato et al conducted the first study and showed that the prevalence of CMD diagnosed with non-invasive coronary assessment was 76%, while Dryer et al demonstrated that the prevalence CMD diagnosed with invasive measurement in patients with HFpEF was 73.4% (44, 45). The largest multi-national study (PROMIS-HFpEF) showed that the prevalence of CMD was 75% (8). In 2022, a study conducted by Arnold et al demonstrated that the prevalence of CMD was 70% in patients with HFpEF, and it was the first study to explore the association between the CMR-measured indexes of microvascular function and clinical outcomes (46). several studies have explored the prevalence and correlation of CMD in patients with HFpEF. The prevalence of CMD was high in patients with HFpEF (over 70%) (8, 46–49). At present, all large-scale clinical trials had neutral results regarding the efficacy of pharmaceutical treatments for HFpEF with the exception of SGLT2 inhibitors (50–75), and even the effect of empagliflozin was attenuated in patients with an ejection fraction >65% (76). The heterogeneity of HFpEF may be the reason behind the failure of previous clinical trials to determine effective treatment for patients with HFpEF. Some patients could benefit from certain interventions, while others might not benefit or even be harmed by the same treatment. When these patients are mixed and treated together, it is difficult to identify an effective treatment. Untangling the association between CMD and HFpEF may be helpful to the development of physiology-stratified treatment for patients with CMD and HFpEF (CMD–HFpEF), to improving their life quality and to their prognosis. At present, none of the RCTs on HFpEF have been conducted in consideration of the presence of CMD. Interventions for HFpEF based on CMD may be effective. Targeted interventions may be effective for different types of patients with HFpEF according to microvascular function. For example, patients with impaired endothelium independent CMD may benefit more from soluble guanylate cyclase stimulators and phosphodiesterase inhibitors (PDEs). Patients with impaired endothelium-dependent CMD, on the other hand, may benefit more from inorganic nitrates that target the NO-PKG pathway of endothelial cells (77–79).
There are some limitations in our study. First, all publications were taken from the WoSCC as it is the best citation-based database, potentially resulting in bias and incompleteness. Second, only publications in English were included. Additionally, the literature information in 2022 was not counted due to the time of extraction.
Conclusion
The studies about CMD are relatively limited, and the most prominent contribution is from the USA, Italy, and England. More studies are needed, and publications of other countries should be enhanced. The main research hotspots in the CMD field are CMD in patients with HFpEF, sex differences in CMD patients, the new methods of diagnosis for CMD, and the effective treatment of CMD. Further attention should be given to CMD in patients with HFpEF, and untangling the association between CMD and HFpEF may be helpful to the development of physiology-stratified treatment for patients with CMD and HFpEF.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
XL, GW, and BG were responsible for data collection, investigation, figures and tables construction, and writing the original draft. JH and SW contributed to the discussion and final review and editing. All authors reviewed and edited the final manuscript.
Funding
This research was supported by the fellowship of the China Postdoctoral Science Foundation (Grant No. 2021M692802), the Key Research, Development Program of Zhejiang Province (Grant No. 2020C03018), the Hangzhou Medical and Health Science and Technology Project (Grant No. Z20210019), and the Hangzhou Science and Technology Development Plan (Grant No. 20201203B178).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Camici PG, d’Amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat Rev Cardiol. (2015) 12:48–62. doi: 10.1038/nrcardio.2014.160
2. Del Buono MG, Montone RA, Camilli M, Carbone S, Narula J, Lavie CJ, et al. Coronary microvascular dysfunction across the spectrum of cardiovascular diseases: JACC state-of-the-art review. J Am Coll Cardiol. (2021) 78:1352–71. doi: 10.1016/j.jacc.2021.07.042
3. Ford TJ, Rocchiccioli P, Good R, McEntegart M, Eteiba H, Watkins S, et al. Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur Heart J. (2018) 39:4086–97. doi: 10.1093/eurheartj/ehy529
4. Jansen TPJ, Konst RE, Elias-Smale SE, van den Oord SC, Ong P, de Vos AMJ, et al. Assessing microvascular dysfunction in angina with unobstructed coronary arteries: JACC review topic of the week. J Am Coll Cardiol. (2021) 78:1471–9. doi: 10.1016/j.jacc.2021.08.028
5. Dean J, Cruz SD, Mehta PK, Merz CN. Coronary microvascular dysfunction: sex-specific risk, diagnosis, and therapy. Nat Rev Cardiol. (2015) 12:406–14. doi: 10.1038/nrcardio.2015.72
6. Sorop O, Olver TD, van de Wouw J, Heinonen I, van Duin RW, Duncker DJ, et al. The microcirculation: a key player in obesity-associated cardiovascular disease. Cardiovasc Res. (2017) 113:1035–45. doi: 10.1093/cvr/cvx093
7. Wei J, Cheng S, Bairey Merz CN. Coronary microvascular dysfunction causing cardiac ischemia in women. JAMA. (2019) 322:2334–5. doi: 10.1001/jama.2019.15736
8. Shah SJ, Lam CSP, Svedlund S, Saraste A, Hage C, Tan RS, et al. Prevalence and correlates of coronary microvascular dysfunction in heart failure with preserved ejection fraction: PROMIS-HFpEF. Eur Heart J. (2018) 39:3439–50. doi: 10.1093/eurheartj/ehy531
9. Taqueti VR, Solomon SD, Shah AM, Desai AS, Groarke JD, Osborne MT, et al. Coronary microvascular dysfunction and future risk of heart failure with preserved ejection fraction. Eur Heart J. (2018) 39:840–9. doi: 10.1093/eurheartj/ehx721
10. Sun HL, Bai W, Li XH, Huang H, Cui XL, Cheung T, et al. Schizophrenia and inflammation research: a bibliometric analysis. Front Immunol. (2022) 13:907851. doi: 10.3389/fimmu.2022.907851
11. Mu F, Tang M, Guan Y, Lin R, Zhao M, Zhao J, et al. Knowledge mapping of the links between the gut microbiota and heart failure: a scientometric investigation (2006-2021). Front Cardiovasc Med. (2022) 9:882660. doi: 10.3389/fcvm.2022.882660
12. van Eck NJ, Waltman L. Visualizing bibliometric networks. In: Ding Y, Rousseau R, Wolfram D editors. Measuring Scholarly Impact. Cham: Springer (2014). p. 285–320. doi: 10.1007/978-3-319-10377-8_13
13. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. (2010) 84:523–38. doi: 10.1007/s11192-009-0146-3
14. Bonetti PO, Pumper GM, Higano ST, Holmes DR, Kuvin JT, Lerman A. Noninvasive identification of patients with early coronary atherosclerosis by assessment of digital reactive hyperemia. J Am Coll Cardiol. (2004) 44:2137–41. doi: 10.1016/j.jacc.2004.08.062
15. Camici PG, Crea F. Medical progress - Coronary microvascular dysfunction. N Engl J Med. (2007) 356:830–40. doi: 10.1056/NEJMra061889
16. Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. (2003) 349:1027–35. doi: 10.1056/NEJMoa025050
17. Crea F, Camici PG, Merz CNB. Coronary microvascular dysfunction: an update. Eur Heart J. (2014) 35:1101–11. doi: 10.1093/eurheartj/eht513
18. Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol. (2003) 41:1387–93. doi: 10.1016/S0735-1097(03)00166-9
19. Heusch G, Gersh BJ. The pathophysiology of acute myocardial infarction and strategies of protection beyond reperfusion: a continual challenge. Eur Heart J. (2017) 38:774–84. doi: 10.1093/eurheartj/ehw224
20. Lanza GA, Crea F. Primary coronary microvascular dysfunction clinical presentation, pathophysiology, and management. Circulation. (2010) 121:2317–25. doi: 10.1161/CIRCULATIONAHA.109.900191
21. McIntyre CW, Burton JO, Selby NM, Leccisotti L, Korsheed S, Baker CS, et al. Hemodialysis-induced cardiac dysfunction is associated with an acute reduction in global and segmental myocardial blood flow. Clin J Am Soc Nephrol. (2008) 3:19–26. doi: 10.2215/CJN.03170707
22. Merz CNB, Pepine CJ, Walsh MN, Fleg JL. Ischemia and no obstructive coronary artery disease (INOCA) developing evidence-based therapies and research agenda for the next decade. Circulation. (2017) 135:1075–92. doi: 10.1161/CIRCULATIONAHA.116.024534
23. Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation. (2015) 131:550–9. doi: 10.1161/CIRCULATIONAHA.114.009625
24. Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Flaxman A, et al. The global burden of ischemic heart disease in 1990 and 2010. Circulation. (2014) 129:1493–501. doi: 10.1161/CIRCULATIONAHA.113.004046
25. Murthy VL, Naya M, Taqueti VR, Foster CR, Gaber M, Hainer J, et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation. (2014) 129:2518–27. doi: 10.1161/CIRCULATIONAHA.113.008507
26. Paulus WJ, Tschope CA. Novel paradigm for heart failure with preserved ejection fraction comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. (2013) 62:263–71.
27. Pelliccia F, Kaski JC, Crea F, Camici PG. Pathophysiology of takotsubo syndrome. Circulation. (2017) 135:2426–41. doi: 10.1161/CIRCULATIONAHA.116.027121
28. Pepine CJ, Anderson D, Sharaf BL, Reis SE, Smith KM, Handberg EM, et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the national heart, lung and blood institute WISE (Women’s Ischemia Syndrome Evaluation) Study. J Am Coll Cardiol. (2010) 55:2825–32.
29. Reis SE, Holubkov R, Smith AJC, Kelsey SF, Sharaf BL, Reichek N, et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J. (2001) 141:735–41. doi: 10.1067/mhj.2001.114198
30. Seferovic PM, Paulus WJ. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Eur Heart J. (2015) 36:1718–U20. doi: 10.1093/eurheartj/ehv134
31. Shah SJ, Kitzman DW, Borlaug BA, van Heerebeek L, Zile MR, Kass DA, et al. Phenotype-specific treatment of heart failure with preserved ejection fraction a multiorgan roadmap. Circulation. (2016) 134:73–90. doi: 10.1161/CIRCULATIONAHA.116.021884
32. Sitia S, Tomasoni L, Atzeni F, Ambrosio G, Cordiano C, Catapano A, et al. From endothelial dysfunction to atherosclerosis. Autoimmun Rev. (2010) 9:830–4. doi: 10.1016/j.autrev.2010.07.016
33. Bairey Merz CN, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. (2006) 47(3 Suppl):S21–9.
34. Shaw LJ, Bairey Merz CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. (2006) 47(3 Suppl):S4–20.
35. Kobayashi Y, Fearon WF, Honda Y, Tanaka S, Pargaonkar V, Fitzgerald PJ, et al. Effect of sex differences on invasive measures of coronary microvascular dysfunction in patients with angina in the absence of obstructive coronary artery disease. JACC Cardiovasc Interv. (2015) 8:1433–41. doi: 10.1016/j.jcin.2015.03.045
36. Chandramouli C, Ting TW, Tromp J, Agarwal A, Svedlund S, Saraste A, et al. Sex differences in proteomic correlates of coronary microvascular dysfunction among patients with heart failure and preserved ejection fraction. Eur J Heart Fail. (2022) 24:681–4. doi: 10.1002/ejhf.2435
37. Taqueti VR, Di Carli MF. Coronary microvascular disease pathogenic mechanisms and therapeutic options: JACC state-of-the-art review. J Am Coll Cardiol. (2018) 72:2625–41. doi: 10.1016/j.jacc.2018.09.042
38. Kelshiker MA, Seligman H, Howard JP, Rahman H, Foley M, Nowbar AN, et al. Coronary flow reserve and cardiovascular outcomes: a systematic review and meta-analysis. Eur Heart J. (2022) 43:1582–93. doi: 10.1093/eurheartj/ehab775
39. Schroder J, Michelsen MM, Mygind ND, Suhrs HE, Bove KB, Bechsgaard DF, et al. Coronary flow velocity reserve predicts adverse prognosis in women with angina and no obstructive coronary artery disease: results from the iPOWER study. Eur Heart J. (2021) 42:228–39. doi: 10.1093/eurheartj/ehaa944
40. Bairey Merz CN, Handberg EM, Shufelt CL, Mehta PK, Minissian MB, Wei J, et al. A randomized, placebo-controlled trial of late Na current inhibition (ranolazine) in coronary microvascular dysfunction (CMD): impact on angina and myocardial perfusion reserve. Eur Heart J. (2016) 37:1504–13. doi: 10.1093/eurheartj/ehv647
41. Corcoran D, Radjenovic A, Mordi IR, Nazir SA, Wilson SJ, Hinder M, et al. Vascular effects of serelaxin in patients with stable coronary artery disease: a randomized placebo-controlled trial. Cardiovasc Res. (2021) 117:320–9. doi: 10.1093/cvr/cvz345
42. Denardo SJ, Wen X, Handberg EM, Bairey Merz CN, Sopko GS, Cooper-Dehoff RM, et al. Effect of phosphodiesterase type 5 inhibition on microvascular coronary dysfunction in women: a Women’s Ischemia Syndrome Evaluation (WISE) ancillary study. Clin Cardiol. (2011) 34:483–7. doi: 10.1002/clc.20935
43. Timmis AD, Chaitman BR, Crager M. Effects of ranolazine on exercise tolerance and HbA1c in patients with chronic angina and diabetes. Eur Heart J. (2006) 27:42–8. doi: 10.1093/eurheartj/ehi495
44. Dryer K, Gajjar M, Narang N, Lee M, Paul J, Shah AP, et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am J Physiol Heart Circ Physiol. (2018) 314:H1033–42. doi: 10.1152/ajpheart.00680.2017
45. Kato S, Saito N, Kirigaya H, Gyotoku D, Iinuma N, Kusakawa Y, et al. Impairment of coronary flow reserve evaluated by phase contrast cine-magnetic resonance imaging in patients with heart failure with preserved ejection fraction. J Am Heart Assoc. (2016) 5:e002649. doi: 10.1161/JAHA.115.002649
46. Arnold JR, Kanagala P, Budgeon CA, Erosch-Herold M, Gulsin GS, Singh A, et al. Prevalence and prognostic significance of microvascular dysfunction in heart failure with preserved ejection fraction. JACC Cardiovasc Imaging. (2022) 15:1001–11. doi: 10.1016/j.jcmg.2021.11.022
47. Ahmad A, Corban MT, Toya T, Verbrugge FH, Sara JD, Lerman LO, et al. Coronary microvascular dysfunction is associated with exertional haemodynamic abnormalities in patients with heart failure with preserved ejection fraction. Eur J Heart Fail. (2021) 23:765–72. doi: 10.1002/ejhf.2010
48. Rush CJ, Berry C, Oldroyd KG, Rocchiccioli JP, Lindsay MM, Touyz RM, et al. Prevalence of coronary artery disease and coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. JAMA Cardiol. (2021) 6:1130–43. doi: 10.1001/jamacardio.2021.1825
49. Yang JH, Obokata M, Reddy YNV, Redfield MM, Lerman A, Borlaug BA. Endothelium-dependent and independent coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Eur J Heart Fail. (2020) 22:432–41. doi: 10.1002/ejhf.1671
50. Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. (2006) 114:397–403. doi: 10.1161/CIRCULATIONAHA.106.628347
51. Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. (2008) 359:2456–67. doi: 10.1056/NEJMoa0805450
52. Edelmann F, Wachter R, Schmidt AG, Kraigher-Krainer E, Colantonio C, Kamke W, et al. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction the aldo-DHF randomized controlled trial. JAMA. (2013) 309:781–91. doi: 10.1001/jama.2013.905
53. Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. (2021) 385:1451–61.
54. Armstrong PW, Lam CSP, Anstrom KJ, Ezekowitz J, Hernandez AF, O’Connor CM, et al. Effect of vericiguat vs placebo on quality of life in patients with heart failure and preserved ejection fraction: the VITALITY-HFpEF randomized clinical trial. JAMA. (2020) 324:1512–21. doi: 10.1001/jama.2020.15922
55. Borlaug BA, Anstrom KJ, Lewis GD, Lewis GD, Shah SJ, Levine JA, et al. Effect of inorganic nitrite vs placebo on exercise capacity among patients with heart failure with preserved ejection fraction: the INDIE-HFpEF randomized clinical trial. JAMA. (2018) 320:1764–73. doi: 10.1001/jama.2018.14852
56. Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J, et al. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. (2006) 27:2338–45. doi: 10.1093/eurheartj/ehl250
57. Conraads VM, Metra M, Kamp O, De Keulenaer GW, Pieske B, Zamorano J, et al. Effects of the long-term administration of nebivolol on the clinical symptoms, exercise capacity, and left ventricular function of patients with diastolic dysfunction: results of the ELANDD study. Eur J Heart Fail. (2012) 14:219–25. doi: 10.1093/eurjhf/hfr161
58. Filippatos G, Maggioni AP, Lam CSP, Pieske-Kraigher E, Butler J, Spertus J, et al. Patient-reported outcomes in the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED ejection fraction (SOCRATES-PRESERVED) study. Eur J Heart Fail. (2017) 19:782–91. doi: 10.1002/ejhf.800
59. Komajda M, Isnard R, Cohen-Solal A, Pieske B, Ponikowski P, Voors AA, et al. Effect of ivabradine in patients with heart failure with preserved ejection fraction: the EDIFY randomized placebo-controlled trial. Eur J Heart Fail. (2017) 19:1495–503. doi: 10.1002/ejhf.876
60. Lewis GA, Dodd S, Clayton D, Bedson E, Eccleson H, Schelbert EB, et al. Pirfenidone in heart failure with preserved ejection fraction: a randomized phase 2 trial. Nat Med. (2021) 27:1477–82. doi: 10.1038/s41591-021-01452-0
61. Nassif ME, Windsor SL, Borlaug BA, Kitzman DW, Shah SJ, Tang F, et al. The SGLT2 inhibitor dapagliflozin in heart failure with preserved ejection fraction: a multicenter randomized trial. Nat Med. (2021) 27:1954–60. doi: 10.1038/s41591-021-01536-x
62. Pieske B, Maggioni AP, Lam CSP, Pieske-Kraigher E, Filippatos G, Butler J, et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur Heart J. (2017) 38:1119–27. doi: 10.1093/eurheartj/ehw593
63. Pieske B, Wachter R, Shah SJ, Baldridge A, Szeczoedy P, Ibram G, et al. Effect of sacubitril/valsartan vs standard medical therapies on plasma NT-proBNP concentration and submaximal exercise capacity in patients with heart failure and preserved ejection fraction: the PARALLAX randomized clinical trial. JAMA. (2021) 326:1919–29.
64. Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. (2014) 370:1383–92. doi: 10.1056/NEJMoa1313731
65. Redfield MM, Anstrom KJ, Levine JA, Koepp GA, Borlaug BA, Chen HH, et al. Isosorbide mononitrate in heart failure with preserved ejection fraction. N Engl J Med. (2015) 373:2314–24. doi: 10.1056/NEJMoa1510774
66. Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. (2013) 309:1268–77. doi: 10.1001/jama.2013.2024
67. Shah SJ, Voors AA, McMurray JJV, Kitzman DW, Viethen T, Bomfim Wirtz A, et al. Effect of neladenoson bialanate on exercise capacity among patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. (2019) 321:2101–12. doi: 10.1001/jama.2019.6717
68. Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. (2019) 381:1609–20.
69. Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. (2012) 380:1387–95. doi: 10.1016/S0140-6736(12)61227-6
70. Udelson JE, Lewis GD, Shah SJ, Zile MR, Redfield MM, Burnett J Jr., et al. Effect of praliciguat on peak rate of oxygen consumption in patients with heart failure with preserved ejection fraction: the CAPACITY HFpEF randomized clinical trial. JAMA. (2020) 324:1522–31. doi: 10.1001/jama.2020.16641
71. van Veldhuisen DJ, McMurray JJ. Pharmacological treatment of heart failure with preserved ejection fraction: a glimpse of light at the end of the tunnel? Eur J Heart Fail. (2013) 15:5–8. doi: 10.1093/eurjhf/hfs194
72. Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. (2003) 362:777–81. doi: 10.1016/S0140-6736(03)14285-7
73. Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, et al. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J. (2006) 27:178–86. doi: 10.1093/eurheartj/ehi687
74. Rector TS, Carson PE, Anand IS, McMurray JJ, Zile MR, McKelvie RS, et al. Assessment of long-term effects of irbesartan on heart failure with preserved ejection fraction as measured by the minnesota living with heart failure questionnaire in the irbesartan in heart failure with preserved systolic function (I-PRESERVE) trial. Circ Heart Fail. (2012) 5:217–25. doi: 10.1161/CIRCHEARTFAILURE.111.964221
75. Zile MR, Bourge RC, Redfield MM, Zhou D, Baicu CF, Little WC. Randomized, double-blind, placebo-controlled study of sitaxsentan to improve impaired exercise tolerance in patients with heart failure and a preserved ejection fraction. JACC Heart Fail. (2014) 2:123–30. doi: 10.1016/j.jchf.2013.12.002
76. Butler J, Packer M, Filippatos G, Ferreira JP, Zeller C, Schnee J, et al. Effect of empagliflozin in patients with heart failure across the spectrum of left ventricular ejection fraction. Eur Heart J. (2022) 43:416–26. doi: 10.1093/eurheartj/ehab798
77. Berry C, Sykes R. Microvascular dysfunction in heart failure with preserved ejection fraction: a modifiable therapeutic target? JACC Cardiovasc Imaging. (2022) 15:1012–4. doi: 10.1016/j.jcmg.2022.04.008
78. Weerts J, Mourmans SGJ, Barandiaran Aizpurua A, Aizpurua A, Schroen BLM, Knackstedt C, et al. The role of systemic microvascular dysfunction in heart failure with preserved ejection fraction. Biomolecules. (2022) 12:278. doi: 10.3390/biom12020278
Keywords: coronary microvascular dysfunction (CMD), bibliometric analysis, visual maps, HFpEF, treatment
Citation: Lin X, Wu G, Gao B, Wang S and Huang J (2022) Bibliometric and visual analysis of coronary microvascular dysfunction. Front. Cardiovasc. Med. 9:1021346. doi: 10.3389/fcvm.2022.1021346
Received: 17 August 2022; Accepted: 31 October 2022;
Published: 15 November 2022.
Edited by:
Tingting Hong, The University of Utah, United StatesReviewed by:
Blanche Schroen, Maastricht University, NetherlandsYan Liu, Dalian Medical University, China
Copyright © 2022 Lin, Wu, Gao, Wang and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuai Wang, ZHJ3YW5nc2h1YWlAemp1LmVkdS5jbg==; Jinyu Huang, emRzeWhqeTA5MDJAemp1LmVkdS5jbg==
 Xiaoxiao Lin1
Xiaoxiao Lin1 Shuai Wang
Shuai Wang Jinyu Huang
Jinyu Huang