- 1Affiliated Hospital of Integrated Traditional Chinese and Western Medicine, Nanjing University of Chinese Medicine, Nanjing, China
- 2Nanjing Lishui District Hospital of Traditional Chinese Medicine, Nanjing, China
- 3School of Basic Medicine and Clinical Pharmacy, China Pharmaceutical University, Nanjing, China
Aim: The purpose of this systematic review was to evaluate the efficiency of telemedicine on the secondary level of prevention of patients with arteriosclerotic cardiovascular disease (ASCVD), provide evidence for the application of telemedicine in secondary prevention and promote the development of telemedicine in secondary prevention.
Methods: A computer-based search was conducted in MEDLINE, Embase, Pubmed, EBSCO, CINAHL, the Cochrane Library, and Web of Science. Randomized controlled trials regarding the effect of telemedicine on secondary prevention of ASCVD were included from inception to May, 2022. Meta-analysis was used to compare the results of the included studies by RevMan5.4 software. The Cochrane Collaboration bias risk tool was used to perform risk of bias assessment in this study. Outcomes included risk factors, physical activity and exercise, muscle function, exercise compliance, medication adherence, healthy diet, depression and anxiety, self-efficacy, knowledge score, economy, and safety endpoints. Subgroup analysis was carried out for different main intervention measures included in the literature.
Results: A total of 32 randomized clinical studies (n = 10 997 participants) were included in the meta-analysis. Compared with usual secondary prevention (USP) group, participants in telemedicine of secondary prevention (TOSP) group showed significant improvement in some risk factors including BMI (MD –0.87, p = 0.002), SBP (MD –4.09, p = 0.007) and DBP (MD –2.91, p = 0.0002) when they use the telephone as the intervention. In physical activity and exercise, Patients in TOSP showed an improvement in VO2 Peak (mL⋅kg–1⋅min–1) (OR 1.58, p = 0.02), 6MWT (MD 21.41, p = 0.001), GSLTPA score (MD 2.89, p = 0.005). Effects on medication adherence, exercise compliance, muscle function, healthy diet, economy and self-efficacy were synthesized narratively. Patients in TOSP did not show a reduction in knowledge score, depression, anxiety and safety endpoints.
Conclusion: There is a net benefit of secondary prevention supported by telemedicine (especially when using the telephone as an intervention) in patients with ASCVD in the terms of some risk factors, physical activity and exercise. There are still controversies in the improvement of medication adherence, exercise compliance, muscle function, healthy diet, knowledge score, self-efficacy and economy via telemedicine, which is worth exploring. Larger samples size and longer-term follow-ups are needed in future studies.
Systematic review registration: [https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=330478], identifier [CRD42022330478].
Introduction
Although the morbidity and mortality of atherosclerotic cardiovascular disease (ASCVD) are declining in many developed countries, it remains a leading cause of incidence and mortality (1). ASCVD caused by plaque buildup in arterial walls is a series of circulatory system diseases referring to the following conditions: coronary heart disease (CHD), cerebrovascular disease, and peripheral arterial disease (PAD) (2, 3). Nowadays several studies have indicated that the application of secondary cardiovascular prevention plays an important role in the intervention of ASCVD and its complications (4–7). The main interventions of secondary prevention include lifestyle modifications; lipid-lowering therapy; control of risk factors and antiplatelet therapy (8, 9). Efficient secondary prevention can reduce the recurrence of ASCVD and decrease mortality. The United Nations emphasizes secondary prevention of cardiovascular disease (CVD) as an important public priority. Besides, the United Nations has declared to adopt a global “25 × 25” goal to reduce by 25% premature (< 70 years) mortality from cancer, CVD, chronic respiratory disease, and diabetes by 2025. The designated action plan includes taking measures to reduce modifiable cardiovascular risk factors, improving the availability of drug therapy and counseling to prevent CVD, and increasing access to affordable fundamental technologies and essential drugs to manage non-communicable diseases (10).
The main risk factors have been identified for ASCVD in the past several decades, including hypertension, smoking, dyslipidemia, obesity, diabetes and so on (2, 11, 12). Nowadays risk factors could be treated effectively and safely, and most medicines are now easy to access and inexpensive. However, a high percentage of people experience an unhealthy lifestyle, and even in the high (residual) CVD risk population, few people are treated properly in the field of risk factors intervention (1).
Although it is important to carry out secondary prevention, it has been shown that the use of secondary prevention of ASCVD is insufficient for patients (6, 13, 14). Especially in the COVID-19 setting, there are likely to be potential implications for the patients with ASCVD to access secondary prevention measures. The pandemic leads to sick people being absent from in-person events in hospitals and rehabilitation centers (9). At the same time, medical resources become unavailable for patients needing secondary cardiovascular prevention due to COVID-19 (15). Enhanced systems of telemedicine and other remote support could provide medical services for patients with CVD and moderate the influence of the COVID-19 pandemic (16). The development of telemedicine has been kicked into high gear. Furthermore, the break of the COVID-19 pandemic has accelerated its use to reduce risk factors and support in the field of physical, psychological, and social wellbeing (17). Telemedicine, and eHealth, provide medical services via information and telecommunication technologies, which is a promising approach (18, 19). These interventions in telemedicine vary from individual to population levels, including text messages, phone calls, webpage, wearable devices, and mobile devices. Nevertheless, it is still unclear whether telemedicine can improve the efficient effect of secondary prevention in patients with ASCVD. To further address this issue, this study systematically reviewed the studies on the impact of telemedicine on the secondary prevention of patients with ASCVD.
Materials and methods
Protocol and registration
The study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement (20). The protocol of this systematic review and meta-analysis was prospectively registered at the International Prospective Register of Systematic Reviews (PROSPERO) (Prospero registration number: CRD42022330478).
Inclusion and exclusion criteria
Participants
The included participants were adults with ASCVD aged 18 or older, who met the diagnostic criteria for (1) CHD, (2) myocardial infarction (MI), (3) acute coronary syndrome (ACS), (4) cerebral arterial thrombosis, (5) PAD or patients who have received arterial revascularization, including coronary intervention and coronary artery bypass surgery. Patients who are diagnosed with other diseases such as heart failure will not be included.
Intervention
Telemedicine of secondary prevention (TOSP) group: participants received remote intervention by investigators through mobile devices, including text messages, phone calls, mobile applications, mobile websites, e-mails, or other remote monitoring.
Usual secondary prevention (USP) group: participants received usual care or secondary prevention treatment without telemedicine intervention. There is no difference between the interventions of the trial group and the control group except for the remote intervention. The studies will be excluded If the intervention is unclear in studies.
Type of study
Only the randomized controlled trial was eligible as it is the most appropriate design for examining the efficient effect of telemedicine on the secondary prevention of ASCVD. We have conducted a pilot search and the result shows that a considerable number of randomized controlled trials were published. The studies were published in English.
Outcomes
Included studies should at least include one of the following outcomes: (1) primary outcomes: cardiovascular risk factor control; (2) secondary outcomes: physical activity and exercise, muscle function, exercise compliance, medication adherence, and healthy diet; (3) tertiary outcomes: depression and anxiety, self-efficacy, knowledge score, economy, safety endpoints, We extensively included all telemedicine studies on secondary prevention in patients with ASCVD in order to comprehensively analyze the effects of secondary prevention for patients with ASCVD.
Search strategy
We searched seven databases: PubMed, Web of Science, CINAHL, EBSCO, MEDLINE, Embase, and Cochrane Library (May 2022) updating from the construction of the bank to May 2022. The search strategy is presented in Supplementary Table 1.
Studies selection and quality evaluation
Two investigators (FD and QW) independently conducted the screening of studies according to the inclusion and exclusion criteria. Inconsistent or uncertain opinions of the included studies were judged by a third person (LYD).
We used the “risk of bias” according to the Cochrane Handbook for the quality evaluation of the included literature. Risks of bias were independently assessed for each study by two of the researchers (FD and QW) using the Cochrane Risk of Bias Assessment Tool, and the third review author (LYD) checked them for assessing the risk of bias including selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias. The risk of bias for each outcome was assessed as low (green), unclear (yellow), or high (red).
Statistical analysis
All calculations for the meta-analysis were conducted by Review Manager 5.4. For studies that measured outcomes at multiple time points, we decided to include outcomes with the longest follow-up after intervention in the meta-analysis due to wide variation in time points across studies. The mean difference (MD) with 95% CI was calculated for continuous data. Standardized mean difference (SMD) was used when varying outcome measurement instruments were used. The Risk Ratio (RR) and 95% confidence intervals (CI) were calculated for dichotomous data. Heterogeneity between studies was explored by Cochran’s Q statistic and I2 index. We adopted a random-effects model to perform the meta-analysis if p ≤ 0.1 or I2 > 50%; otherwise, a fixed-effects model was used. A random-effects model was used If there was no heterogeneity (I2 ≤ 50%, p > 0.1), the weights varied considerably between included studies and the number of studies was no higher than 3. Subgroup analysis was performed for our primary outcomes for our meta-analysis containing more than 10 studies according to the type of main intervention measures. The results are presented as forest plots with a 95% CI, with p < 0.05 deemed to be indicative of a statistically significant difference. In studies where median and interquartile ranges were reported, mean and standard deviations were estimated through methods recommended by Wan et al. (21). Studies that could not be analyzed for meta-analysis were using narrative synthesis instead. Sensitivity analysis was carried out by excluding each study one by one. We explored publication bias using funnel plots when the outcomes contain more than 10 studies.
Results
Search results
We identified 18,103 records from the initial search in the seven electronic databases and removed 4,676 duplicates. 13,278 records that were irrelevant and not met the inclusion criteria were excluded after the title and abstracts of 13,427 records were screened. We further conducted a full-text review of the remaining 149 studies and confirm whether they conform to eligibility criteria. At last, we included 32 items of studies for our systematic review and 25 items of studies for our meta-analysis (Figure 1).
Characteristics of included studies
The 32 studies included 10,997 participants for analysis. We presented their main characteristics in Table 1. These studies were conducted in North America (n = 5) (22–26), Europe (n = 10) (14, 27–35), Asia (n = 9) (19, 36–43), Africa (n = 1) (44), Australia and New Zealand (n = 6) (45–50), South America (n = 1) (13). We included participants who were diagnosed with MI (24, 29, 32, 34, 35, 37, 44, 47), ACS (14, 22, 31, 33, 49), CHD (13, 19, 23, 27, 28, 30, 40, 41, 45, 46, 48, 50), Ischemic stroke (13, 30) and PAD (13, 19, 30) or received coronary revascularization (13, 19, 23, 25, 26, 28, 29, 33, 36, 38, 39, 42, 43, 45, 48, 49) in our review. The participants’ mean age varies from 55.8 to 70.36 and 20.04% of them are female. Due to the existence of mixed intervention measures, we assume the main intervention measures as the measures of contact and interaction between researchers and patients. We classified the main intervention measures as telephone (14, 26, 28, 33, 35, 37, 39, 47, 48), e-mail and telephone (27), text message (22, 24, 31, 36, 49, 50), mobile application (13, 19, 32, 38, 42–46), website (23, 25, 29, 30, 34, 41) and website and mobile application (40).
Included studies quality evaluation
26 studies of the 32 included RCTs were found to be clearly detailed in random sequence generation. Unclear risk of selection bias existed in 7 studies for not describing the way allocation concealment was undertaken. It is impossible to blind participants and personnel in all studies because of the characteristics of the intervention. Therefore, performance bias cannot be avoided to have a high risk. In our included studies, there are 24 studies in which blinding research staff and participants have not been carried out. In 16 studies, the outcome assessors were blinded to avoid detection bias. Twenty-nine studies showed that the low risk of attrition bias was due to either the study’s appropriate solution for missing data or no significant differences in dropouts between the two groups. 18 studies had a protocol and reported predicted outcome indicators according to the protocol and were considered to have a low risk of reporting bias. There is no other bias. A summary of the results of the risk of bias was presented in Supplementary Figure 1. The risk of bias assessment included studies was presented in Figure 2.
Outcomes
Primary outcomes
Risk factors
The primary outcomes included modifiable risk factors body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), low-density lipoprotein cholesterol (LDL-C), fasting glucose, glycosylated hemoglobin (HbA1c), and smoking cessation rates.
Among the changeable risk factors, BMI, DBP and SBP showed no significant difference (BMI: MD –0.16, 95% CI –0.33 to –0.01; p = 0.07; I2 = 38%; Figure 3A. DBP: MD –0.72, 95% CI –1.42 to –0.01; p = 0.05; I2 = 31%; Figure 3B. SBP: MD –2.06, 95% CI –4.24 to –0.11; p = 0.06; I2 = 82%; Figure 3C). However, only the TOSP had significant differences in the field of using the telephone as a remote telemedicine intervention compared with that in USP according to subgroup analysis (BMI: MD –0.87, 95% CI –1.42 to –0.31; p = 0.002; I2 = 0%; Figure 3A. DBP: MD –2.91, 95% CI –4.45 to –1.37; p = 0.0002; I2 = 0%; Figure 3B. SBP: MD –4.09, 95% CI –7.04 to –1.15; p = 0.007; I2 = 60%; Figure 3C). However, it is observed that high heterogeneity existed in SBP. Leave one out sensitivity analysis showed that when we removed three studies respectively, by Dorje et al. (43), Yudi et al. (46), and Hu et al. (39), the overall effect still did not change between the two groups (MD –1.47, 95 CI –3.06–0.12; p = 0.07; I2 = 48).
Figure 3. Forest plots of the effects of telemedicine on risk factors— (A) BMI; (B) DBP; (C) SBP; (D) LDL-C; TOSP, telemedicine of secondary prevention; USP, usual secondary prevention.
The results of this meta-analysis indicated that at 10 weeks to 36 months of follow-up there was no significant difference in LDL - C between TOSP and USP [12 studies (14, 19, 27, 30, 32, 33, 36, 39, 41, 43, 46, 50), MD –0.02, 95% CI –0.22–0.18; p = 0.83; I2 = 94%; Figure 3D], the result of the subgroup analysis also showed that there was no significant difference. However, it is also observed that high heterogeneity existed in studies. Leave one out sensitivity analysis showed that when we removed five studies respectively, by Avila et al. (27), Hu et al. (39), Bae et al. (36), Greving et al. (30) and Wong et al. (41), the overall effect changed into a small but significant difference in favor of TOSP (MD –0.11; 95% CI –0.17 to –0.05; p = 0.0002; I2 = 47%).
No statistically significant difference was found in fasting glucose (MD –0.04, 95% CI –0.15 to –0.23; p = 0.68; I2 = 0%; Supplementary Figure 2A), HbA1c (%) (MD –0.03, 95% CI –0.08 to –0.13; p = 0.62; I2 = 0%; Supplementary Figure 2B). A statistically significant difference was seen in smoking cessation rates (RR 0.74, 95% CI 0.59–0.94; p = 0.01; I2 = 0%; Supplementary Figure 2C), however, USP had a better improvement in smoking cessation rates compared with TOSP.
Secondary outcomes
Physical activity and exercise
Fifteen studies (19, 24–28, 32, 33, 35, 36, 38, 41, 43, 46, 50) investigated outcomes on exercise capability at 6 weeks to 6 months of follow-up. Between TOSP and USP, a statistically significant difference was seen in 6 min walk test (6MWT) (MD 21.41, 95% CI 8.40–34.43; p = 0.001; I2 = 0%; Figure 4A), Godin-Sheppard Leisure-Time Physical Activity Questionnaire (GSLTPA score) (MD 2.89, 95% CI 0.88–4.90; p = 0.005; I2 = 0%; Figure 4B), peak oxygen consumption (VO2 Peak, mL⋅kg–1⋅min–1) (MD 1.58, 95% CI 0.20–2.96; p = 0.02; I2 = 0%; Figure 4C).
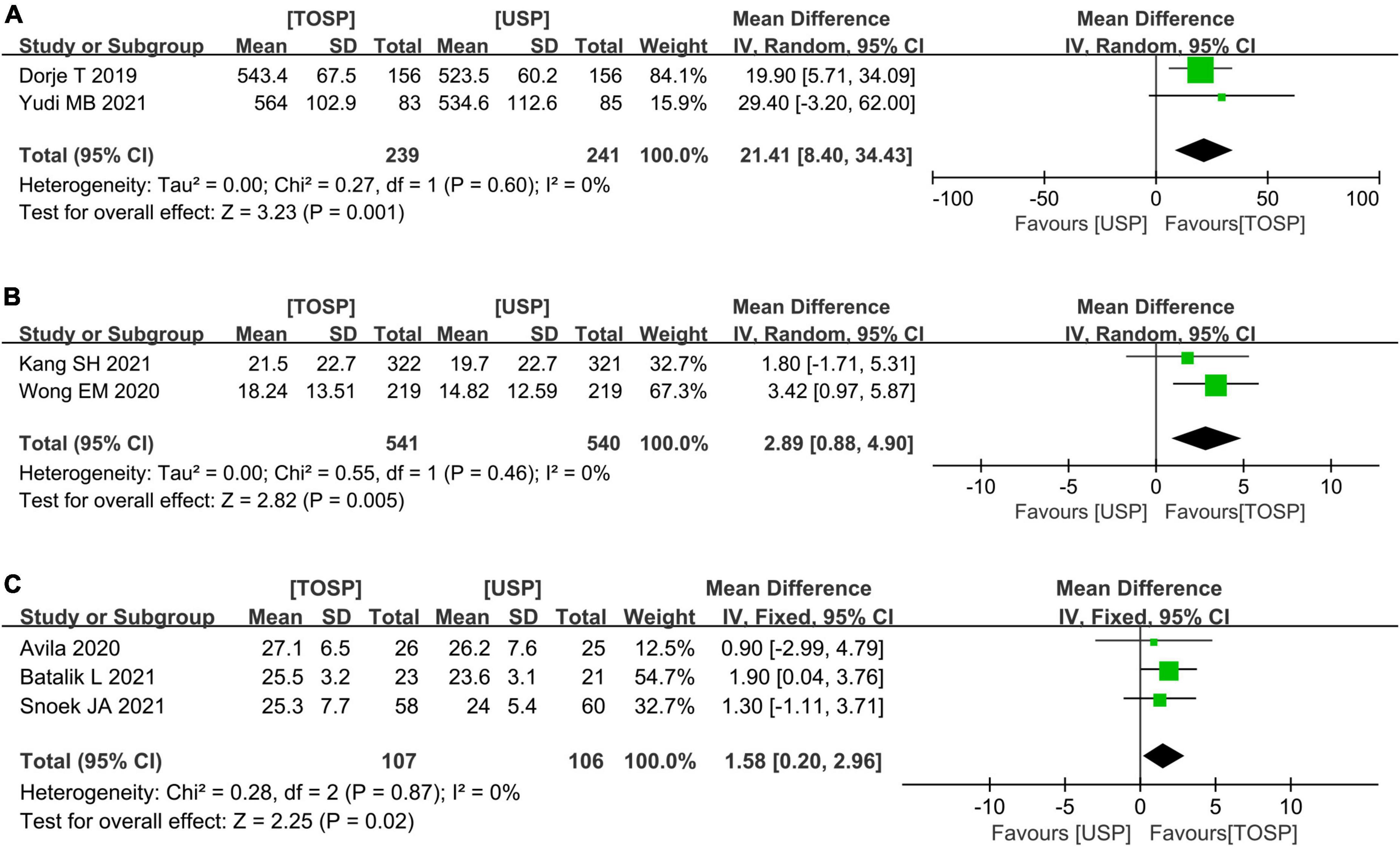
Figure 4. Forest plots of the effects of telemedicine on physical activity and exercise— (A) 6MWT; (B) GSLTPA score; (C) VO2 Peak (mL⋅kg–1⋅min–1); TOSP, telemedicine of secondary prevention; USP, usual secondary prevention.
No statistically significant difference was detected among workload peak (Watt) (MD 15.11, 95% CI –2.05 to 32.28; p = 0.08; I2 = 0%; Supplementary Figure 3A), rating of perceived exertion [RPE (Borg)] (MD –0.18, 95% CI –0.63–0.27; p = 0.43; I2 = 0%; Supplementary Figure 3B), Peak heart rate (Peak HR) (MD 0.00, 95% CI –0.03–0.03, p = 0.87; I2 = 0%; Supplementary Figure 3C), VO2 Peak (ml/min) (MD 99.67, 95% CI –8.48–207.83; p = 0.07; I2 = 0%; Supplementary Figure 3D)and peak respiratory exchange ratio (Peak RER) (MD 0.00, 95% CI –0.03–0.03, p = 0.87; I2 = 0%; Supplementary Figure 3E).
Muscle function
Avila et al. (27) found that no statistically significant difference was seen in muscle function including sit-to-stand test (p = 0.22), isometric quadriceps extension (p = 0.33), isokinetic total work (p = 0.77), and handgrip strength in the two groups (p = 0.49). Nevertheless, Foccardi et al. (38) found that there was a statistically significant difference in the 30 s sit-to-stand test (p = 0.03) between TOSP and USP.
Exercise compliance
A study reported on exercise compliance. Pandey et al. (24) reported that the mean days of exercise per month and mean hours of exercise per month at the 12th-month follow-up of TOSP had an additional from 4.2 to 17.2 days (P < 0.001) and 4.0 h (P < 0.001) respectively, compared with USP.
Medication adherence
Dorje et al. (43) reported that at the 2nd (p = 0.0048), 6th (p = 0.019), and 12-month (p = 0.011) follow-up, the participants of TOSP tend to be adherent to all four core cardioprotective medications. In addition, Pandey et al. (24) reported on medication adherence (the percentage of days covered), the Figure for participants who were reminded by text messages had a mean 14.2 percentage point improvement compared with USP (p < 0.001).
Healthy diet
Ögmundsdóttir Michelsen et al. (32) found that the Healthy diet index (p = 0.03) differed significantly between patients with MI who were intervened by mobile applications and the patients who received usual care. Hu et al. (39) reported that the patients who received monitoring and follow-up by telephone achieved significantly better dietary control (p = 0.0001). Besides, Vale et al. (48) found that patients in the field of intake of fat (p = 0.04) and fiber (p = 0.02) intervened by telephone differ significantly from the patients in USP. While Maddison et al. (49) and Pfaeffli Dale et al. (50) found that there is no statistically significant difference in fruit and vegetable intake of patients who intervened by sending text messages (p > 0.05).
Tertiary outcomes
Depression and anxiety
Four studies (33, 46, 47, 50) were performed by Hospital Anxiety and Depression Scale (HADS). The data of HADS Anxiety (HADS-A) and HADS Depression (HADS-D) from 6 months to 13 months follow-up showed that no difference was noted between USP and TOSP. (HADS-A: MD –0.03, 95% CI –1.37–1.31; p = 0.97; I2 = 80%. HADS-D: MD –0.21, 95% CI –0.73–0.30; p = 0.42; I2 = 0%; Supplementary Figures 4A,B). However, there was high heterogeneity across studies. Leave one out sensitivity analysis showed that when we removed the study by Pfaeffli Dale et al. (50) the overall effect changed into a small but statistically significant difference in favor of TOSP (MD –0.73; 95% CI –1.42–0.04; P = 0.04, I2 = 0%). In addition, no statistically significant difference was detected in the Depression Anxiety Stress Scales (40) (DASS) (p = 0.90) and the Generalized Anxiety Disorder 7-item scale (43) (p = 0.17).
Self-efficacy
Self-efficacy was reported in 4 studies (22, 40, 41, 50). Due to the different selection of indicators and expressions, it cannot be included in the meta-analysis. Therefore, A narrative synthesis is carried out. Two studies (22, 40) reported Cardiac Self-Efficacy Scale (CSE Scale). Su and Yu (40) found that the improvement of self-efficacy in TOSP was significantly higher than that in USP at 12 weeks (P < 0.001), but there was no significant difference in self-efficacy at 6 weeks (p = 0.402). Ross et al. (22) showed that there was no significant difference except in the self-efficacy domain (Total plus), where the improvement in self-efficacy of the telemedicine group was worse than that of USP (Control symptoms: p = 0.10; Maintain function: p = 0.05; Total: p = 0.05; Total plus: p = 0.03). Wong et al. (41) found that in the terms of Self-efficacy for Exercise (SEE), TOSP showed no improvement at either 6 months or 12 months (6 months: P = 0.17;12 months: p = 0.90). Pfaeffli Dale et al. (50) reported that no statistically significant difference was noted in the overall self-efficacy for TOSP at 6 months of follow-up (p = 0.73).
Knowledge score
Three trials reported data on the knowledge score of ACS or CHD. The SMD was used because of the differences in measurement scales. Meta-analysis of the included trials did not show a significant difference in knowledge score between TOSP and USP (SMD 0.38; 95% CI –0.25–1.00; P = 0.23, I2 = 94%). It is observed that high heterogeneity existed in the Knowledge score. Leave one out sensitivity analysis showed that when we removed one study by Dorje et al. (43), the overall effect still did not change between the two groups (SMD = 0.05; 95% CI –0.10–0.20; P = 0.53, I2 = 0%).
Economy
Two studies (30, 45) have reported the cost of secondary prevention. Brouwers et al. (45) found that after the 1-year follow-up, overall heart health care costs of TOSP compared with USP were reduced by 40 €, but no significant difference was noted statistically (p = 0.36). The study (30) showed that after the 1-year follow-up, patients in the TOSP group and USP group underwent the same health benefits, namely the QALY gain of 0.86–0.85, and the less cost of TOSP than USP of 219 € (95% CI: –2301€ to 1825 €).
Safety endpoints
4 studies (13, 22, 26, 37) reported that TOSP and USP in the 2–12 month had no statistical significant differences in all-cause hospitalization (RR 0.89, 95% CI 0.70–1.13; p = 0.34; I2 = 0%, Supplementary Figure 5A). Three studies (13, 22, 37) of cardiac-related hospitalization showed that there is no significant difference between TOSP and USP in the 2–12 months (RR 0.86, 95% CI 0.55–1.36; p = 0.53; I2 = 0%, Supplementary Figure 5B). Meta-analysis of 3 studies (30, 33, 34) about major adverse cardiovascular events (MACE) showed that TOSP and USP in years 1 to 13 months of follow-up study showed no statistical difference (RR 0.73, 95% CI 0.50–1.08; p = 0.12; I2 = 0%, Supplementary Figure 5C). Similarly, Bermon et al. (13) and Treskes et al. (34) comparing the effect of TOSP and USP, did not find statistical differences between all-cause mortality and cardiac-related mortality.
Assessment of publication bias
We explored publication bias using funnel plots for the primary outcomes: (1) BMI; (2) SBP; (3) DBP); (4) low-density lipoprotein cholesterol (LDL-C). Funnel plots were shown in Supplementary Figure 6. Symmetry was observed in the BMI and DBP. However, there is dissymmetry observed in the funnel plots of SBP and LDL-C. Publication bias may exist in the meta-analysis.
Discussion
32 RCTs were included in our meta-analysis. We compared the outcomes of the patients with ASCVD who received secondary prevention in TOSP and those in USP. In this systematic review, we found that telemedical interventions have successfully been implemented for the improvement of some risk factors, physical activity, and exercise. No statistically significant difference was noted in blood lipids, blood glucose, depression and anxiety, and safety endpoints. It remained controversial in muscle function, medication adherence, exercise compliance, knowledge score, healthy diet, self-efficacy, and economy.
We found some evidence of differences in the primary outcomes of TOSP compared to USP under different interventions (mobile application, telephone, text message, website, website, and mobile application). When the telephone was used as an main intervention, significantly favorable changes in BMI, SPB, DBP. However, a Meta-analysis for blood lipids and smoking cessation did not confirm better results for TOSP than for USP. Huang et al. (51) reported that there was no difference in changeable risk factors (blood lipids, blood pressure, smoking, and weight) between patients with telemedical intervention and those with center-based cardiac rehabilitation in the short-term (12 weeks to 12 months) and long-term (up to 6 years) follow-up. However, it is reported by Turan Kavradim et al. (52) that telemedical intervention was associated with an increase in Waist circumference, total cholesterol (TC), and triglycerides when compared with the usual care group. In a meta-analysis (53), it is observed that significant improvements existed in the TC, SBP, and smoking in patients who received the telemedical intervention. The reasons might be as follows: (1) The inclusion of patients in our study included all ASCVD diseases, which is wider than the range of CHD included in previous systematic reviews. (2) Compared with previous systematic reviews, this study was analyzed with interventions as subgroups. In addition, Turan Kavradim et al. (52) reported that using the telephone as an intervention is the most popular telemedical intervention. Klimis et al. (54) also found that text messages were more effective compared with mobile applications in the systematic review. Huang et al. (51) reported that telephone-based interventions have the greatest evidence value for secondary prevention. Our systematic review also showed that telephone-based intervention was more effective in reducing risk factors. The reasons might be (1) the majority of ASCVD patients are elderly, but the elderly use smartphones, apps, and websites rarely; (2) successful contact by telephone is better than that by text messages. Telemedicine is an acceptable and appropriate method to improve the coverage and utilization of secondary prevention. However, pragmatic implementation studies are needed to realize the impact of telemedicine on the accessibility of secondary prevention.
We found that a statistically significant MD of 1.58 mL⋅kg–1⋅min–1 in the VO2 Peak (mL⋅kg–1⋅min–1) was noted between TOSP and USP. In the early study, a 1 mL⋅kg–1 ⋅min–1 increase of VO2 Peak (mL⋅kg–1⋅min–1) can lead to a 10% decrease in Cardiovascular mortality (55), and it can be regarded as an important indicator of morbidity and mortality in patients with CVD (56). Nevertheless, Sumeet Gandhi et al. (57) reported that there is no statistically significant difference in the terms of VO2 Peak (mL⋅kg–1⋅min–1) between the e-health group and the control group. We offer some possible explanations for the inconsistency as follows: the inconsistency of duration, intensity, frequency, and engagement of intervention, which may affect the action and effectiveness of interventions. Therefore, it is important to explore an effective and accessible intervention method. Besides, it’s necessary to have more evidence to assess the outcomes. We also found that in terms of subjective measures (GSLTPA score), TOSP had improvement in physical activity compared with USP while no statistically significant difference was noted for other objective measures [RPE (BORG),Peak HR, VO2 Peak (mL/min),Peak RER]. The reason probably is few studies analyze the indicators. Therefore, firmer conclusions need more research.
In the terms of muscle function, we made a narrative synthesis for the two included studies. Due to the selection of different indicators, it is difficult to measure the effect of these outcomes and confirm the outcomes by meta-analysis. A 24-year follow-up study including 1 142 599 participants shows that low muscle strength is associated with all-cause and cardiovascular mortality in CVD (58). Similarly, in a population-based prospective cohort study, people with higher grip strength had a lower risk of all-cause mortality and CVD morbidity and mortality (59). However, at present, it is unclear whether telemedical interventions make a difference in muscle strength in patients with ASCVD. It is a prospective topic in future studies.
A narrative synthesis was done in the area of a healthy diet. It is difficult to make definitive conclusions in this section because of the limited number of included studies and the different indicators in each study. The guidelines recommend a healthy diet as a cornerstone of CVD prevention and suggest a Mediterranean diet or a similar diet for ASCVD patients. The Mediterranean diet includes high intakes of fruits, vegetables, legumes, whole grain products, fish and olive oil, moderate alcohol consumption, and small amounts of (red) meat, dairy products, and saturated fatty acids (1). A meta-analysis showed that better adherence to the Mediterranean diet was significantly associated with a 10% reduction in cardiovascular morbidity or mortality and an 8% reduction in all-cause mortality (60). A multicenter study that included 7,447 subjects showed that a nut-rich Mediterranean diet reduced the risk of ASCVD by 28% and a diet rich in olive oil by 31% (61). Therefore, a healthy diet is necessary for the secondary prevention of ASCVD (62). At present, it is inconclusive whether telemedicine can have a beneficial effect on the healthy diet of ASCVD patients. This could be a focus of future research in telemedicine.
In the system review, there was no statistically significant difference in knowledge score. There is a gap between knowledge of CVD conditions and their risk factors in patients with CVD, which are important barriers between the effective prevention and treatment of CVD (63). Kim et al. reported that specialized interventions should focus on groups with less knowledge of CVD (64). Because of educational needs, it is a good choice to use telemedicine to learn knowledge of ASCVD.
A study reported that self-efficacy, a robust predictor of behavioral persistence, should be scheduled to improve exercise adherence (65). Besides, general and exercise-specific self-efficacy are relevant to the quality of life (66). Therefore, the improvement of self-efficacy supported by telemedicine is worth exploring. In the adherence part of secondary prevention through telemedicine, we classified adherence as medication adherence, and exercise compliance. In our systematic review, both the subjective and objective indicators showed that telemedicine can improve medication adherence and exercise adherence to some extent. In the economic part, we found that the patients in the telemedicine group paid less tuition for secondary prevention compared with the usual care group, but not significantly. In this systematic review, the adherence part and the economics part are both descriptive analyses, and the conclusions drawn may be one-sided.
Limitations: (1) There was a difference in the follow-up time of RCTs included in our studies. Here, we choose the outcomes with the longest follow-up time of RCTs. Therefore, inconsistency of research time existed in our study. (2) Due to a limited number of studies, it is impossible to determine which intervention is more effective for some indicators. (3) Because of the intervention methods included in RCTs, it is difficult to blind participants in studies. Therefore, the third item of assessing the risk of bias (blinding of participants and personnel) cannot be avoided. (4) Few studies included patients with ischemic stroke and PAD who received secondary prevention through telemedicine. It is found that secondary prevention supported by telemedicine may be probably effective in cerebrovascular disease and PAD (67, 68). However, existing studies often lack adequate patients, standardized endpoints, and confirmation of independent researchers. Therefore, a larger scale with standardized powerful trials of endpoints is worth exploring.
Conclusion
The meta-analysis shows that there is a net benefit of secondary prevention supported by telemedicine (especially when using the telephone as an intervention) in patients with ASCVD in the terms of some risk factors, physical activity and exercise. There are still controversies to improve medication adherence, exercise compliance, muscle function, knowledge score, and self-efficacy via telemedicine, which is worth exploring. Larger samples size and longer-term follow-ups are needed in future studies.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
HJT, LXW, and BLZ designed the research project. LYD, QW, and FD performed the studies selection and quality evaluation of included studies. LYD, QW, FD, and YFL analyzed the data and wrote the manuscript. HJT revised the manuscript. All authors contributed to the preparation of the manuscript and agreed to be accountable for all aspects of the work ensuring integrity and accuracy.
Funding
This research was supported by the National Natural Science Foundation of China (no. 81873274), the Pharmaceutical Care Special Scientific Research Project of Jiangsu Pharmaceutical Society (no. H202018), the Jiangsu Western Learning Middle and Senior Talents Training Project (Jiangsu Traditional Chinese Medicine Science and Education [2020] no. 7), the Science and Technology Project of Nanjing Lishui District Hospital of Traditional Chinese Medicine (no. LSZYJN202004), the Jiangsu Academy of Traditional Chinese Medicine Science and Technology Project (KYCX20_1482), and the TCM Science and Technology Development Program of Jiangsu Province (no. QN202005).
Acknowledgments
We thank HJT, LXW, and KHS for help with valuable suggestions regarding improving the quality of the manuscript. We also gratefully acknowledge the support provided by QW, FD, YL, JPS, YFL, and Ziwen Chen.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.1020744/full#supplementary-material
References
1. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2021) 42:3227–337.
2. Poredos P, Jezovnik M. Do the effects of secondary prevention of cardiovascular events in PAD patients differ from other atherosclerotic disease? IJMS. (2015) 16:14477–89. doi: 10.3390/ijms160714477
3. Virani SS, Smith SC, Stone NJ, Grundy SM. Secondary prevention for atherosclerotic cardiovascular disease: comparing recent US and European guidelines on dyslipidemia. Circulation. (2020) 141:1121–3. doi: 10.1161/CIRCULATIONAHA.119.044282
4. Tsivgoulis G, Safouris A, Kim DE, Alexandrov AV. Recent advances in primary and secondary prevention of atherosclerotic stroke. J Stroke. (2018) 20:145–66. doi: 10.5853/jos.2018.00773
5. Scott LJ. Rivaroxaban: a review for secondary CV prevention in CAD and PAD. Drugs. (2020) 80:1465–75. doi: 10.1007/s40265-020-01397-7
6. Høgh AL. The use of secondary medical prevention after pri- mary vascular reconstruction: studies on usage and effectiveness. Dan Med J. (2012) 59:B4514.
7. Santiago de Araújo Pio C, Chaves GS, Davies P, Taylor RS, Grace SL. Interventions to promote patient utilisation of cardiac rehabilitation. Cochrane Database Syst Rev. (2019) 2:CD007131. doi: 10.1002/14651858.CD007131.pub4
8. Schorr EN, Gepner AD, Dolansky MA, Forman DE, Park LG, Petersen KS, et al. Harnessing mobile health technology for secondary cardiovascular disease prevention in older adults: a scientific statement from the American heart association. Circ Cardiovasc Qual Outcomes. (2021) 14:e000103. doi: 10.1161/HCQ.0000000000000103
9. Nicholls SJ, Nelson M, Astley C, Briffa T, Brown A, Clark R, et al. Optimising secondary prevention and cardiac rehabilitation for atherosclerotic cardiovascular disease during the COVID-19 pandemic: a position statement from the cardiac society of Australia and New Zealand (CSANZ). Heart Lung Circ. (2020) 29:e99–104. doi: 10.1016/j.hlc.2020.04.007
10. Schwalm JD, McKee M, Huffman MD, Yusuf S. Resource effective strategies to prevent and treat cardiovascular disease. Circulation. (2016) 133:742–55. doi: 10.1161/CIRCULATIONAHA.115.008721
11. American Diabetes Association. 8. Cardiovascular disease and risk management. Diabetes Care. (2016) 39:S60–71. doi: 10.2337/dc16-S011
12. Yang X, Li J, Hu D, Chen J, Li Y, Huang J, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in chinese population: the China-PAR project (Prediction for ASCVD risk in China). Circulation. (2016) 134:1430–40. doi: 10.1161/CIRCULATIONAHA.116.022367
13. Bermon A, Uribe AF, Pérez-Rivero PF, Prieto-Merino D, Saaibi JF, Silva FA, et al. Efficacy and safety of text messages targeting adherence to cardiovascular medications in secondary prevention: TXT2HEART Colombia randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e25548. doi: 10.2196/25548
14. Henriksson R, Huber D, Mooe T. Nurse-led, telephone-based follow-up after acute coronary syndrome yields improved risk factors after 36 months: the randomized controlled NAILED-ACS trial. Sci Rep. (2021) 11:17693. doi: 10.1038/s41598-021-97239-x
15. Volpe M, Battistoni A The Board of the Italian Society of Cardiovascular Prevention, Bellotti P, Bellone S, Bertolotti M. Recommendations for cardiovascular prevention during the Sars-Cov-2 pandemic: an executive document by the board of the Italian society of cardiovascular prevention. High Blood Press Cardiovasc Prev. (2020) 27:373–7. doi: 10.1007/s40292-020-00401-1
16. Arnold RH, Tideman PA, Devlin GP, Carroll GE, Elder A, Lowe H, et al. Rural and remote cardiology during the COVID-19 pandemic: cardiac society of Australia and New Zealand (CSANZ) consensus statement. Heart Lung Circ. (2020) 29:e88–93. doi: 10.1016/j.hlc.2020.05.001
17. Subedi N, Rawstorn JC, Gao L, Koorts H, Maddison R. Implementation of telerehabilitation interventions for the self-management of cardiovascular disease: systematic review. JMIR Mhealth Uhealth. (2020) 8:e17957. doi: 10.2196/17957
18. Pappot N, Taarnhøj GA, Pappot H. Telemedicine and e-health solutions for COVID-19: patients’ perspective. Telemed E Health. (2020) 26:847–9. doi: 10.1089/tmj.2020.0099
19. Kang SH, Baek H, Cho J, Kim S, Hwang H, Lee W, et al. Management of cardiovascular disease using an mHealth tool: a randomized clinical trial. NPJ Digit Med. (2021) 4:165. doi: 10.1038/s41746-021-00535-z
20. Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
21. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
22. Ross ES, Sakakibara BM, Mackay MH, Whitehurst DGT, Singer J, Toma M, et al. The use of SMS text messaging to improve the hospital-to-community transition in patients with acute coronary syndrome (Txt2Prevent): results from a pilot randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e24530. doi: 10.2196/24530
23. Lear SA, Singer J, Banner-Lukaris D, Horvat D, Park JE, Bates J, et al. Improving access to cardiac rehabilitation using the internet: a randomized trial. Stud Health Technol Inform. (2015) 209:58–66.
24. Pandey A, Krumme AA, Patel T, Choudhry NK. The impact of text messaging on medication adherence and exercise among postmyocardial infarction patients: randomized controlled pilot trial. JMIR Mhealth Uhealth. (2017) 5:e110. doi: 10.2196/mhealth.7144
25. Reid RD, Morrin LI, Beaton LJ, Papadakis S, Kocourek J, McDonnell L, et al. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur J Prev Cardiol. (2012) 19:1357–64. doi: 10.1177/1741826711422988
26. Smith KM, McKelvie RS, Thorpe KE, Arthur HM. Six-year follow-up of a randomised controlled trial examining hospital versus home-based exercise training after coronary artery bypass graft surgery. Heart. (2011) 97:1169–74. doi: 10.1136/hrt.2010.202036
27. Avila A, Claes J, Buys R, Azzawi M, Vanhees L, Cornelissen V. Home-based exercise with telemonitoring guidance in patients with coronary artery disease: does it improve long-term physical fitness? Eur J Prev Cardiol. (2020) 27:367–77. doi: 10.1177/2047487319892201
28. Batalik L, Dosbaba F, Hartman M, Konecny V, Batalikova K, Spinar J. Long-term exercise effects after cardiac telerehabilitation in patients with coronary artery disease: 1-year follow-up results of the randomized study. Eur J Phys Rehabil Med. (2021) 57:807–14. doi: 10.23736/S1973-9087.21.06653-3
29. Bruggmann C, Adjedj J, Sardy S, Muller O, Voirol P, Sadeghipour F. Effects of the interactive web-based video “mon coeur, mon basic” on drug adherence of patients with myocardial infarction: randomized controlled trial. J Med Internet Res. (2021) 23:e21938. doi: 10.2196/21938
30. Greving JP, Kaasjager HAH, Vernooij JWP, Hovens MMC, Wierdsma J, Grandjean HMH, et al. Cost-effectiveness of a nurse-led internet-based vascular risk factor management programme: economic evaluation alongside a randomised controlled clinical trial. BMJ Open. (2015) 5:e007128. doi: 10.1136/bmjopen-2014-007128
31. Blasco A, Carmona M, Fernández-Lozano I, Salvador CH, Pascual M, Sagredo PG, et al. Evaluation of a telemedicine service for the secondary prevention of coronary artery disease. J Cardiopulm Rehabil Prev. (2012) 32:25–31. doi: 10.1097/HCR.0b013e3182343aa7
32. Ögmundsdóttir Michelsen H, Sjölin I, Bäck M, Gonzalez Garcia M, Olsson A, Sandberg C, et al. Effect of a lifestyle-focused web-based application on risk factor management in patients who have had a myocardial infarction: randomized controlled trial. J Med Internet Res. (2022) 24:e25224. doi: 10.2196/25224
33. Snoek JA, Meindersma EP, Prins LF, van’t Hof AW, de Boer MJ, Hopman MT, et al. The sustained effects of extending cardiac rehabilitation with a six-month telemonitoring and telecoaching programme on fitness, quality of life, cardiovascular risk factors and care utilisation in CAD patients: the TeleCaRe study. J Telemed Telecare. (2021) 27:473–83. doi: 10.1177/1357633X19885793
34. Treskes RW, van Winden LAM, van Keulen N, van der Velde ET, Beeres SLMA, Atsma DE, et al. Effect of smartphone-enabled health monitoring devices vs regular follow-up on blood pressure control among patients after myocardial infarction: a randomized clinical trial. JAMA Netw Open. (2020) 3:e202165. doi: 10.1001/jamanetworkopen.2020.2165
35. Hanssen TA, Nordrehaug JE, Eide GE, Hanestad BR. Improving outcomes after myocardial infarction: a randomized controlled trial evaluating effects of a telephone follow-up intervention. Eur J Cardiovasc Prev Rehabil. (2007) 14:429–37. doi: 10.1097/HJR.0b013e32801da123
36. Bae JW, Woo SI, Lee J, Park SD, Kwon SW, Choi SH, et al. mHealth interventions for lifestyle and risk factor modification in coronary heart disease: randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e29928. doi: 10.2196/29928
37. Chan MY, Koh KWL, Poh SC, Marchesseau S, Singh D, Han Y, et al. Remote postdischarge treatment of patients with acute myocardial infarction by allied health care practitioners vs standard care: the IMMACULATE randomized clinical trial. JAMA Cardiol. (2021) 6:830. doi: 10.1001/jamacardio.2020.6721
38. Foccardi G, Vecchiato M, Neunhaeuserer D, Mezzaro M, Quinto G, Battista F, et al. Effectiveness of text messaging as an incentive to maintain physical activity after cardiac rehabilitation: a randomized controlled pilot study. Int J Environ Res Public Health. (2021) 18:6645. doi: 10.3390/ijerph18126645
39. Hu X, Zhu X, Gao L. Intensive nursing care by an electronic followup system to promote secondary prevention after percutaneous coronary intervention: a randomized trial. J Cardiopulm Rehabil Prev. (2014) 34:396–405. doi: 10.1097/HCR.0000000000000056
40. Su JJ, Yu DS. Effects of a nurse-led eHealth cardiac rehabilitation programme on health outcomes of patients with coronary heart disease: a randomised controlled trial. Int J Nurs Stud. (2021) 122:104040. doi: 10.1016/j.ijnurstu.2021.104040
41. Wong EM, Leung DYP, Chair S, Sit JWH. Effects of a web-based educational support intervention on total exercise and cardiovascular risk markers in adults with coronary heart disease. Worldviews Evid Based Nurs. (2020) 17:283–92. doi: 10.1111/wvn.12456
42. Yu C, Liu C, Du J, Liu H, Zhang H, Zhao Y, et al. Smartphone-based application to improve medication adherence in patients after surgical coronary revascularization. Am Heart J. (2020) 228:17–26. doi: 10.1016/j.ahj.2020.06.019
43. Dorje T, Zhao G, Tso K, Wang J, Chen Y, Tsokey L, et al. Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): a parallel-group, single-blind, randomised controlled trial. Lancet Digit Health. (2019) 1:e363–74. doi: 10.1016/S2589-7500(19)30151-7
44. Kamel H, Hafez MS, Bastawy I. Telemedicine improves the short-term medical care of acute st-segment elevation myocardial infarction after primary percutaneous coronary intervention. Front Cardiovasc Med. (2021) 8:693731. doi: 10.3389/fcvm.2021.693731
45. Brouwers RWM, van der Poort EKJ, Kemps HMC, van den Akker-van Marle ME, Kraal JJ. Cost-effectiveness of cardiac telerehabilitation with relapse prevention for the treatment of patients with coronary artery disease in the Netherlands. JAMA Netw Open. (2021) 4:e2136652. doi: 10.1001/jamanetworkopen.2021.36652
46. Yudi MB, Clark DJ, Tsang D, Jelinek M, Kalten K, Joshi SB, et al. SMARTphone-based, early cardiac REHABilitation in patients with acute coronary syndromes: a randomized controlled trial. Coron Artery Dis. (2021) 32:432–40. doi: 10.1097/MCA.0000000000000938
47. O’Neil A, Hawkes AL, Atherton JJ, Patrao TA, Sanderson K, Wolfe R, et al. Telephone-delivered health coaching improves anxiety outcomes after myocardial infarction: the ‘ProActive Heart’ trial. Eur J Prev Cardiol. (2014) 21:30–8.
48. Vale MJ, EpidBiostat D, Jelinek MV, Best JD, Dart AM, Grigg LE, et al. Coaching patients on achieving cardiovascular health (COACH). Arch Intern Med. (2003) 163:9. doi: 10.1001/archinte.163.22.2775
49. Maddison R, Jiang Y, Stewart R, Scott T, Kerr A, Whittaker R, et al. An intervention to improve medication adherence in people with heart disease (Text4HeartII): randomized controlled trial. JMIR Mhealth Uhealth. (2021) 9:e24952. doi: 10.2196/24952
50. Pfaeffli Dale L, Whittaker R, Jiang Y, Stewart R, Rolleston A, Maddison R. Text message and internet support for coronary heart disease self-management: results from the Text4Heart randomized controlled trial. J Med Internet Res. (2015) 17:e237. doi: 10.2196/jmir.4944
51. Huang K, Liu W, He D, Huang B, Xiao D, Peng Y, et al. Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. (2015) 22:959–71. doi: 10.1177/2047487314561168
52. Turan Kavradim S, Özer Z, Boz İ. Effectiveness of telehealth interventions as a part of secondary prevention in coronary artery disease: a systematic review and meta-analysis. Scand J Caring Sci. (2020) 34:585–603. doi: 10.1111/scs.12785
53. Neubeck L, Redfern J, Fernandez R, Briffa T, Bauman A, Freedman SB. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. Eur J Cardiovasc Prev Rehabil. (2009) 16:281–9. doi: 10.1097/HJR.0b013e32832a4e7a
54. Klimis H, Thakkar J, Chow CK. Breaking barriers: mobile health interventions for cardiovascular disease. Can J Cardiol. (2018) 34:905–13. doi: 10.1016/j.cjca.2018.02.012
55. Keteyian SJ, Brawner CA, Savage PD, Ehrman JK, Schairer J, Divine G, et al. Peak aerobic capacity predicts prognosis in patients with coronary heart disease. Am Heart J. (2008) 156:292–300. doi: 10.1016/j.ahj.2008.03.017
56. Woo J, Yau F, Leung J, Chan R. Peak oxygen uptake, six-minute walk distance, six-meter walk speed, and pulse pressure as predictors of seven year all-cause and cardiovascular mortality in community-living older adults. Exp Gerontol. (2019) 124:110645. doi: 10.1016/j.exger.2019.110645
57. Gandhi S, Chen S, Hong L, Sun K, Gong E, Li C, et al. Effect of mobile health interventions on the secondary prevention of cardiovascular disease: systematic review and meta-analysis. Can J Cardiol. (2017) 33:219–31. doi: 10.1016/j.cjca.2016.08.017
58. Ortega FB, Silventoinen K, Tynelius P, Rasmussen F. Muscular strength in male adolescents and premature death: cohort study of one million participants. BMJ. (2012) 345:e7279–7279. doi: 10.1136/bmj.e7279
59. Celis-Morales CA, Petermann F, Hui L, Lyall DM, Iliodromiti S, McLaren J, et al. Associations between diabetes and both cardiovascular disease and all-cause mortality are modified by grip strength: evidence from UK biobank, a prospective population-based cohort study. Diabetes Care. (2017) 40:1710–8. doi: 10.2337/dc17-0921
60. Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. (2010) 92:1189–96. doi: 10.3945/ajcn.2010.29673
61. Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. (2018) 378:e34. doi: 10.1056/NEJMoa1800389
62. Eilat-Adar S, Sinai T, Yosefy C, Henkin Y. Nutritional recommendations for cardiovascular disease prevention. Nutrients. (2013) 5:3646–83. doi: 10.3390/nu5093646
63. Boateng D, Wekesah F, Browne JL, Agyemang C, Agyei-Baffour P, Aikins AD. Knowledge and awareness of and perception towards cardiovascular disease risk in sub-Saharan Africa: a systematic review. PLoS One. (2017) 12:e0189264. doi: 10.1371/journal.pone.0189264
64. Kim H, Lee S, Chung JH. Knowledge and poor understanding factors of stroke and heart attack symptoms. Int J Environ Res Public Health. (2019) 16:3665. doi: 10.3390/ijerph16193665
65. Banik A, Schwarzer R, Knoll N, Czekierda K, Luszczynska A. Self-efficacy and quality of life among people with cardiovascular diseases: a meta-analysis. Rehabil Psychol. (2018) 63:295–312. doi: 10.1037/rep0000199
66. Rodgers WM, Murray TC, Selzler AM, Norman P. Development and impact of exercise self-efficacy types during and after cardiac rehabilitation. Rehabil Psychol. (2013) 58:178–84. doi: 10.1037/a0032018
67. Kraft P, Hillmann S, Rücker V, Heuschmann PU. Telemedical strategies for the improvement of secondary prevention in patients with cerebrovascular events—A systematic review and meta-analysis. Int J Stroke. (2017) 12:597–605. doi: 10.1177/1747493017706188
Keywords: telemedicine, secondary prevention, atherosclerotic cardiovascular disease (ASCVD), effect, systematic review, meta-analysis
Citation: Deng L, Wu Q, Ding F, Liu Y, Shen J, Lin Y, Shi K, Zeng B, Wu L and Tong H (2022) The effect of telemedicine on secondary prevention of atherosclerotic cardiovascular disease: A systematic review and meta-analysis. Front. Cardiovasc. Med. 9:1020744. doi: 10.3389/fcvm.2022.1020744
Received: 02 September 2022; Accepted: 18 October 2022;
Published: 03 November 2022.
Edited by:
Francesco Spannella, Università Politecnica delle Marche, ItalyReviewed by:
Bartosz Krzowski, Medical University of Warsaw, PolandBasuni Radi, National Cardiovascular Center Harapan Kita, Indonesia
Copyright © 2022 Deng, Wu, Ding, Liu, Shen, Lin, Shi, Zeng, Wu and Tong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huangjin Tong, dG9uZ2hqQGpzYXRjbS5jb20=; Lixing Wu, d3VsaXhpbmdAanNhdGNtLmNvbQ==; Bailin Zeng, YmFpbGluemVuZ0AxMjYuY29t
†These authors share first authorship
 Liangying Deng
Liangying Deng Qing Wu3†
Qing Wu3† Yanfeng Liu
Yanfeng Liu Huangjin Tong
Huangjin Tong