- 1Department of Endocrinology, Aerospace Center Hospital, Beijing, China
- 2Department of Rheumatology, Aerospace Center Hospital, Beijing, China
- 3Department of Cardiovascular Medicine, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
Background: The relationship between serum calcium and left ventricular function in patients with acute coronary syndrome (ACS) has not been explored. Our aim was to investigate the correlation of admission serum calcium with left ventricular dysfunction in ACS patients.
Methods: In this cross-sectional study, 658 ACS patients who were admitted in the Department of Cardiovascular Disease from June 1st, 2019 to December 31st, 2019 were enrolled in the present study. Serum calcium and B-type natriuretic peptide (BNP) were measured at admission. Left ventricular ejection fraction (LVEF) was assessed using echocardiography. The correlation between admission serum calcium and left ventricular dysfunction was analyzed.
Results: When stratified by serum calcium quartiles calculated from all patients, patients with lower serum calcium quartile showed a markedly higher BNP and lower LVEF (P < 0.05). Patients with LVEF ≤ 50% showed a significantly lower serum calcium and higher BNP compared to those with LVEF> 50% (P < 0.05). Admission serum calcium was positively correlated with LVEF (P < 0.01) but negatively correlated with BNP (P < 0.01). Multivariate logistic regression analysis showed that lower serum calcium (adjusted OR: 0.720, 95% CI: 0.519–0.997, P = 0.048) was independently associated with BNP ≥ 300 pg/ml in ACS patients. Using LVEF as a dependent variable, no significant correlation between low serum calcium and left ventricular systolic dysfunction was found in ACS patients.
Conclusions: In patients with ACS, admission serum calcium was positively correlated with LVEF and negatively with BNP. Lower admission serum calcium was an independent risk factor for elevated BNP.
Introduction
Cardiovascular disease is the major cause of death globally (1, 2). Acute coronary syndrome (ACS) represents a severe type of atherosclerotic cardiovascular disease. Studies reported that about 30–50% of ACS patients had left ventricular systolic dysfunction (3–5) which was an important determinant of poor outcome (3, 6, 7).
Serum calcium is a common monitored clinical biomarker. Calcium plays a critical role in excitation, contraction and relaxation of the myocardium (8, 9). Both clinical electrophysiology studies and preclinical experiments demonstrated that abnormal intracellular calcium concentration was a key biomarker of heart failure with preserved ejection fraction (10–12). Previous studies indicated that high level of serum calcium concentration was independently associated with heart failure (10–12). However, Wang et al. (13) found that low serum calcium was associated with left ventricular systolic dysfunction in patients with coronary artery disease (CAD).
The relationship between serum calcium and left ventricular function in ACS patients has not been investigated. Therefore, our aim was to explore the correlation between admission serum calcium and left ventricular dysfunction in ACS patients.
Methods
Study participants
Patients with ACS who were admitted to the Department of Cardiovascular Disease, Beijing Tiantan Hospital, Capital Medical University from June 1st, 2019 to December 31st, 2019 were screened. The ACS included unstable angina pectoris, acute ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (non-STEMI) (14). The inclusion criteria were as follows: (1) age > 18 years; (2) ACS was confirmed by coronary angiography; (3) complete information of echocardiographic examination; (4) signed informed consent form. Patients with any of the following conditions were excluded: preexisting cardiomyopathy, endocarditis, severe valvular heart disease, cerebrovascular disease, liver dysfunction, chronic renal insufficiency, acute infection, known malignancies, thyroid diseases, parathyroid disorders, mal-absorption, bone disease, systemic immune disease, hemorrhagic diathesis or coagulation disorders. In total, 658 ACS patients were eligible for the study. The study was performed according to the Declaration of Helsinki and approved by the ethical committee of Beijing Tiantan hospital. Written informed consents were obtained from all patients or their legal representatives.
Demographic and clinical data
Clinical data including height, weight, body mass index, blood pressure, heart rate, and Global Registry of Acute Coronary Events (GRACE) risk score were collected at admission. Medical history, history of smoking and drinking were also collected upon admission. GRACE score was calculated based on the following eight indexes: age, heart rate, systolic blood pressure, blood creatinine concentration, Killip classification, prehospital cardiac arrest, ST-segment deviation on electrocardiography, and cardiac enzyme elevation.
Biochemical measurements
Fasting blood samples were obtained from the peripheral veins on the first morning after admission. Levels of serum calcium, phosphate, albumin, serum lipid, serum glucose and creatinine were measured by the Hitachi LABOSPECT 008 automatic biochemical analyzer (Hitachi Corporation, Japan). Glycosylated hemoglobin A1c (HbA1c), C-reactive protein (CRP), and B-type natriuretic peptide (BNP) were determined using routine methods. Abnormal elevated BNP was defined as ≥300 pg/ml (15–17). The troponin I (TnI), and creatine kinase isoenzymes MB (CK-MB) levels were also measured using the Architect system (Abbott Diagnostics).
Coronary angiography
Coronary angiography was carried out via the radial or femoral artery approach according to the standard Judkins technique in ACS patients. CAD was defined as having a single or multiple coronary artery stenosis with at least 50% diameter reduction according to the American College of Cardiology/American Heart Association lesion classification (18). Based on the results of coronary angiography, CAD severity was estimated by the number of coronary artery lesions and classified as three groups: single-vessel disease, double-vessel disease, triple-vessel disease. And left main lesion was equivalent to triple-vessel disease (19).
Left ventricular systolic function assessment
Echocardiography was performed with a Vivid 7 Dimension equipped with a multifrequency transducer (GE Healthcare, Vingmed, Norway) within 24 h after admission. Left ventricular systolic function was evaluated by left ventricular ejection fraction (LVEF). LVEF was measured using the Simpson's method based on two-dimensional echocardiography in all patients. Low LVEF was defined as LVEF ≤ 50% (20, 21).
Statistical analysis
Normality of the distribution of the studied variables was assessed by normal probability plots and one-sample Kolmogorov–Smirnov test. Continuous variables were presented as mean ± standard deviation (SD) or median (interquartile range), as appropriate. Differences in normally distributed variables were determined by independent-samples t-test or one-way ANOVA, while the non-parametric Mann-Whitney U-test or Kruskal-Wallis test was used for the variables not normally distributed. Categorical variables were given as ratio or percentage. The Chi-square test was applied for categorical variables. Pearson correlation was performed to determine the association between serum calcium and left ventricular function. Multivariate logistic regression analyses were used to examine the relationship between left ventricular dysfunction based on BNP ≥ 300 pg/ml or LVEF ≤ 50% and related factors, after adjustment for potential confounders, including age, gender, biochemical parameters and GRACE score. The odds ratio (OR) and 95% confidence interval (95% CI) were reported separately. A two-tailed P-value < 0.05 was considered as statistically significant difference.
The data were analyzed with SPSS version 26 (SPSS for Windows, IBM Corp., USA).
Results
Comparisons of clinical characteristics of ACS patients according to serum calcium quartiles
In total, 658 ACS patients were included, with a mean age of 62.0 ± 10.1 years, (range: 23–85 years). Four hundred and seventy-seven participants (72.5%) were males. The average serum calcium level was 2.27 ± 0.10 mmol/l. The average LVEF was 60.7 ± 6.8% and the proportion of LVEF ≤ 50 was 9.3%.
All patients were divided into four groups according to serum calcium quartiles: Quartile 1 (serum calcium level ≤ 2.19 mmol/L), Quartile 2 (2.20–2.25 mmol/L), Quartile 3 (2.26–2.32 mmol/L), and Quartile 4 (≥2.33 mmol/L). The biochemical indexes and clinical data of ACS patients in the different groups were shown in Table 1. When stratified by serum calcium quartiles, the mean age, proportion of acute myocardial infarction, troponin I at admission, BNP and GRACE score were significantly higher in Quartile 1 group as compared with Quartile 3 group and Quartile 4 group (P < 0.01). At the same time, the patients in Quartile 2 group were older than those in Quartile 4 group and also had higher troponin I at admission, BNP and GRACE score than those in Quartile 3 group and Quartile 4 group (P < 0.05). However, patients in Quartile 1 group showed an obviously lower LVEF than those in Quartile 3 group and Quartile 4 group (P < 0.01). A lower triglycerides and total cholesterol were found in Quartile 1 group than those in Quartile 4 group (P < 0.01). And body mass index was also lower in Quartile 1 group than that in Quartile 2 group and Quartile 3 group (P < 0.01). With increasing serum calcium, serum albumin and serum phosphorus showed a significant increase (P < 0.05). No differences in gender, previous history, blood pressure, creatinine or number of coronary artery lesions were observed among four groups.
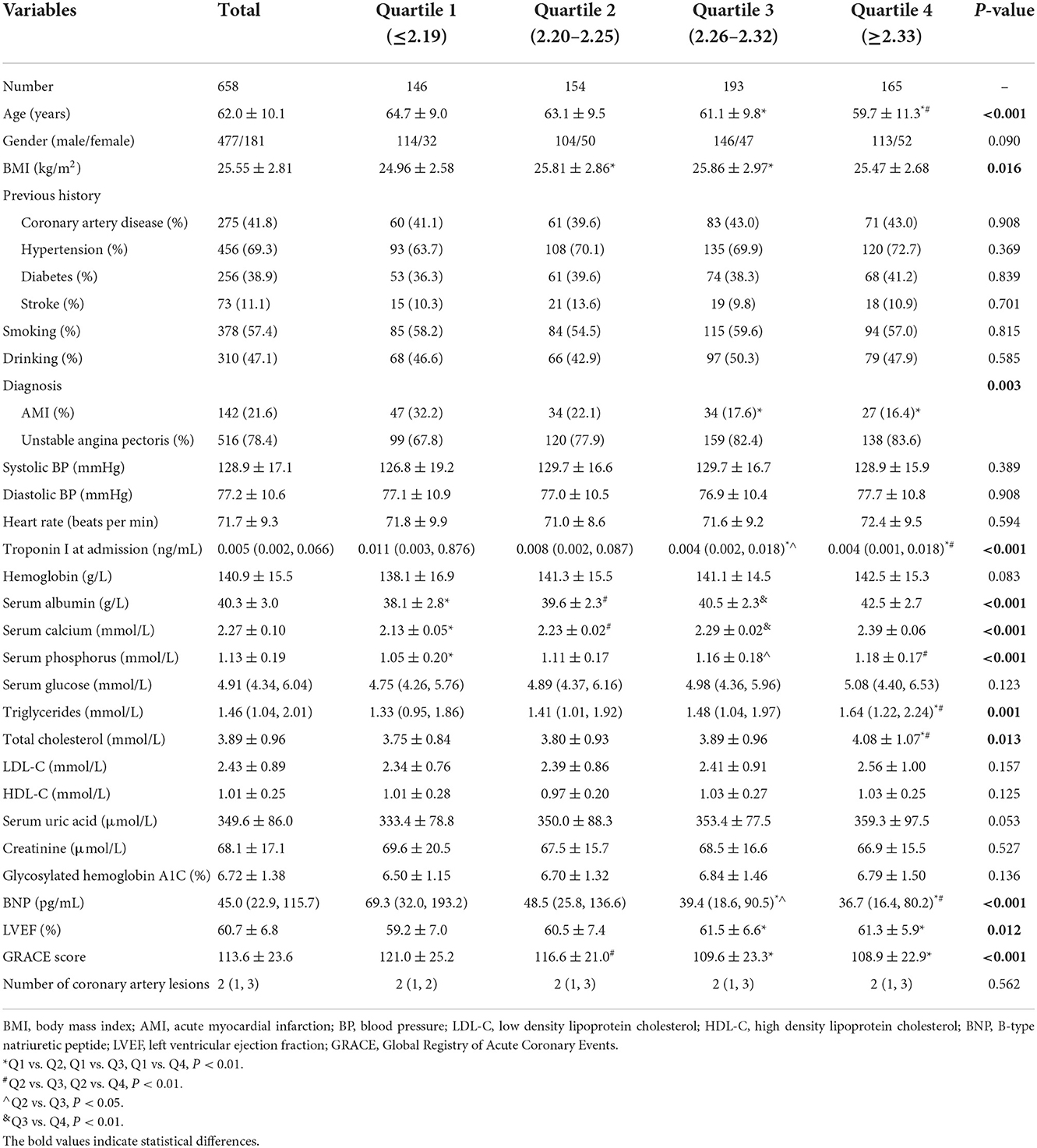
Table 1. Comparisons of clinical characteristics of ACS patients according to serum calcium quartiles.
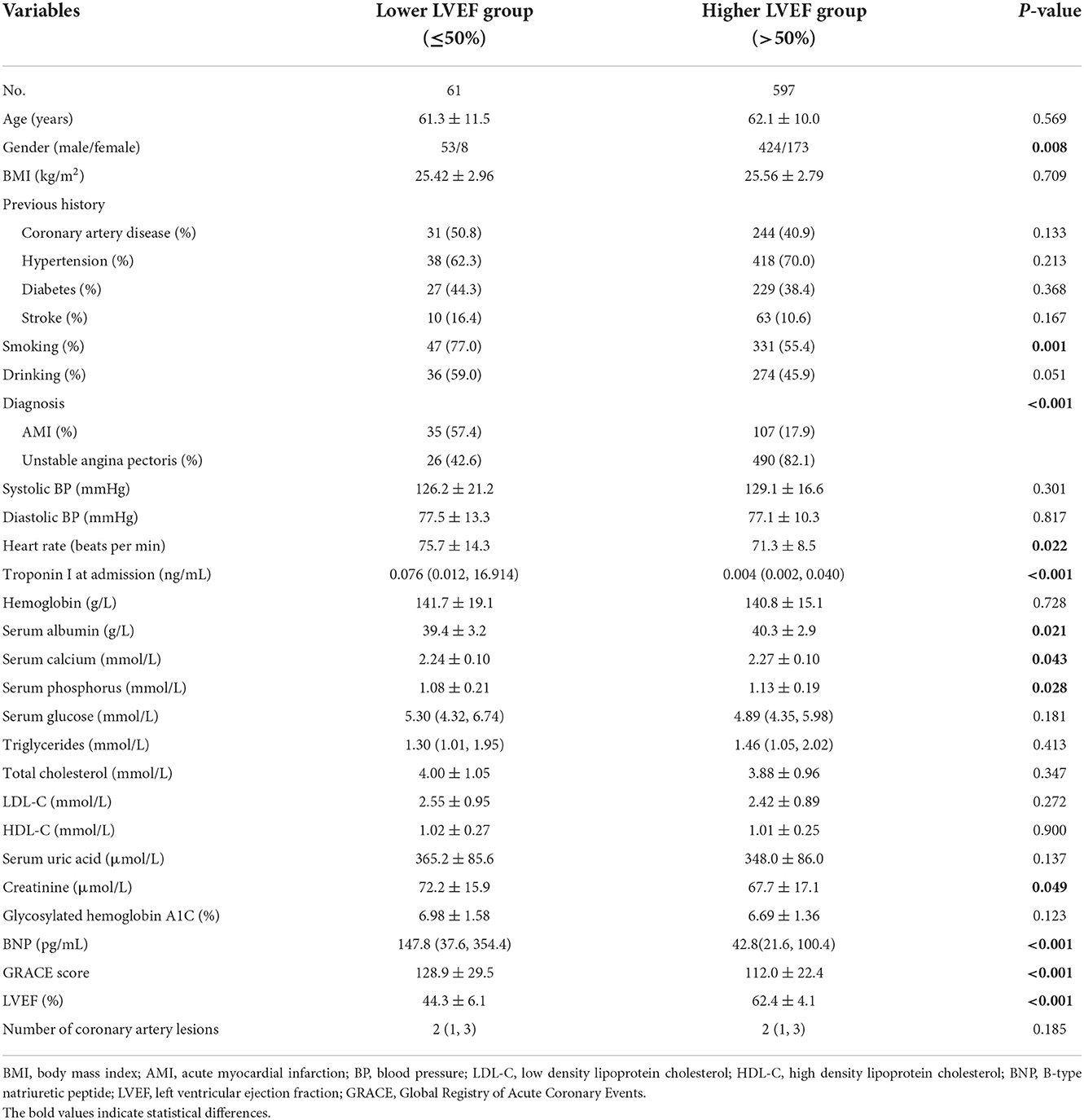
Comparisons of clinical characteristics of ACS patients according to LVEF
The ACS patients were categorized into two groups according to LVEF, with one group of ACS patients with lower LVEF (LVEF ≤ 50%, n = 61) and one group with higher LVEF (LVEF > 50%, n = 597). Seen from Table 2, the male, smoking, proportion of acute myocardial infarction, heart rate, troponin I at admission, creatinine, BNP, and GRACE score were obviously higher in lower LVEF group than in higher LVEF group (P < 0.05). As compared to those with higher LVEF, the patients with lower LVEF had a significantly decreased serum albumin, serum calcium and phosphorus (P < 0.05). The age, blood pressure, serum lipid, or number of coronary artery lesions didn't differ between both groups.
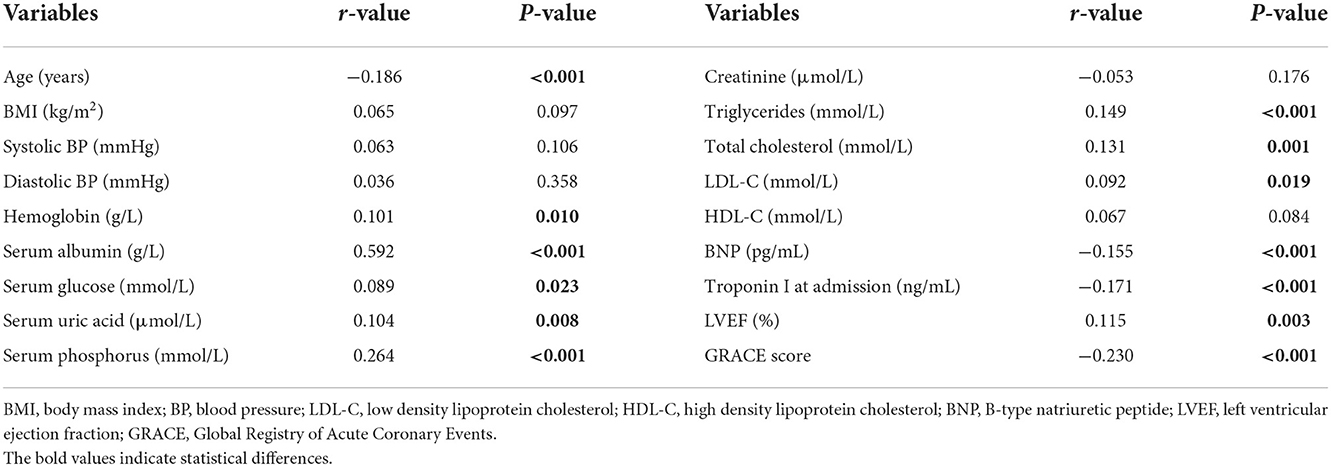
Correlations of serum calcium with left ventricular function in ACS patients
In Table 3, Pearson correlation analysis found that admission serum calcium level showed a significantly positive correlation with hemoglobin, serum albumin, serum glucose, serum uric acid, serum phosphorus, triglycerides, total cholesterol, low density lipoprotein cholesterol, and LVEF (P < 0.05). And serum calcium was significantly and negatively associated with age, BNP, troponin I at admission, and GRACE score (P < 0.001).
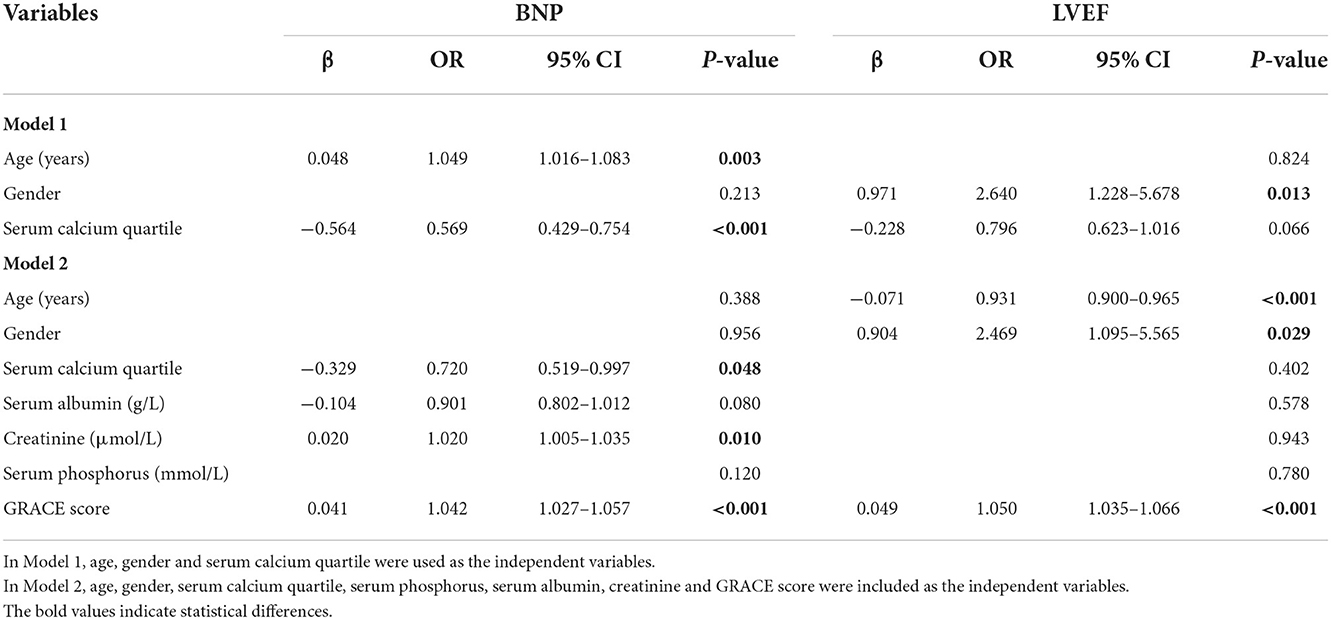
Multivariate logistic regression in ACS patients
In multivariate logistic regression analysis, BNP was defined as 1 when BNP ≥ 300 pg/ml, and BNP was defined as 0 when BNP < 300 pg/ml. LVEF was considered as 1 when LVEF ≤ 50%, and LVEF was considered as 0 when LVEF > 50%. Male was defined as 1 while female was as 0. Multivariate backward stepwise logistic regression analysis was used to explore the independent factors associated with BNP ≥ 300 pg/ml or LVEF ≤ 50%.
In model 1, age, gender and serum calcium quartile were used as the independent variables. The data in Table 4 exhibited that age (OR: 1.049, 95% CI: 1.016–1.083, P = 0.003) and lower serum calcium quartile (OR: 0.569, 95% CI: 0.429–0.754, P < 0.001) were independently associated with BNP ≥ 300 pg/ml after adjustment for potential confounding factors in ACS patients. In contrast, male (OR: 2.640, 95% CI: 1.228–5.678, P = 0.013) and lower serum calcium quartile (OR: 0.796, 95% CI: 0.623–1.016, P = 0.066) correlated with LVEF ≤ 50%.
In model 2, serum phosphorus, serum albumin, creatinine and GRACE score were also included in addition to those used in model 1. Multivariate backward stepwise logistic regression showed that lower serum calcium quartile (OR: 0.720, 95% CI: 0.519–0.997, P = 0.048), lower serum albumin (OR: 0.901, 95% CI: 0.802–1.012, P = 0.080), increased creatinine (OR: 1.020, 95% CI: 1.005–1.035, P = 0.010) and GRACE score (OR: 1.042, 95% CI: 1.027–1.057, P < 0.001) were independently correlated with BNP ≥ 300 pg/ml after adjusting for other potential confounders in ACS patients. When LVEF was used as the dependent variable, male (OR: 2.469, 95% CI: 1.095–5.565, P = 0.029), age (OR: 0.931, 95% CI: 0.900–0.965, P < 0.001) and increased GRACE score (OR: 1.050, 95% CI: 1.035–1.056, P < 0.001) were independently associated with LVEF ≤ 50%.
Discussion
The present study analyzed the correlation between the level of admission serum calcium and left ventricular dysfunction in ACS patients. Admission serum calcium was positively correlated with LVEF and negatively correlated with BNP. Low level of serum calcium was independently associated with BNP ≥ 300 pg/ml after adjusting for other potential confounders. No significant association between low level of serum calcium and left ventricular systolic dysfunction was detected.
Previous studies investigated the correlation between serum calcium and left ventricular function and found that patients with low concentration of serum calcium were more likely to have LVEF < 50% (22). And patient with established heart failure presented low level of serum calcium concentration (13, 23). Wang et al. (13) suggested that low serum calcium was independently associated with left ventricular systolic dysfunction in CAD patients with and without acute myocardial infarction. Batra and Agarwal (24) observed severe hypocalcemia and increased BNP in a patient with hypocalcemic cardiomyopathy and severe heart failure. Our results were consistent with these previous findings.
Other studies, on the contrary, showed different results. Li et al. (11) indicated that an increase in serum calcium concentration was correlated with an increased risk of heart failure with preserved ejection fraction in patients with type 2 diabetes mellitus. Additionally, Lutsey et al. (10) also demonstrated that baseline high serum calcium was independently correlated with greater risk of incident heart failure in this population-based cohort.
Many reasons may contribute to these different observations. It is well-known that serum calcium is affected by many factors, such as diseases, drugs and measurement techniques. In aforementioned studies, patients with diabetes mellitus or communities population from the Atherosclerosis Risk in Communities (ARIC) cohort were recruited. But severely ill patients or patients with history of LVEF < 50% were excluded. In contrast, ACS patients who were severely ill or in emergency condition were enrolled in our study. Additionally, albumin-adjusted serum calcium concentration was used in the previous study while admission serum calcium was measured in this study. By multivariate logistic regression analysis, low serum calcium was independently correlated with elevated BNP after adjustment for potential confounding factors such as age, serum albumin, and so on in ACS patients.
BNP and LVEF are objective indexes for assessment of left ventricular function (17, 25). To the best of our knowledge, this is the first study to evaluate the association between the level of admission serum calcium and left ventricular function in ACS patients. We demonstrated that low serum calcium quartile was independently associated with elevated BNP and serum calcium level was positively correlated with LVEF. However, no significant association of serum calcium with left ventricular systolic dysfunction was observed. The potential reason includes the small number of patients with LVEF ≤ 50%. Meanwhile, we noticed that serum calcium level was no longer correlated with the LVEF ≤ 50% when adjusted by GRACE score. Killip classification is used to stratify patients according to the severity of their post-myocardial infarction heart failure and included in the calculation of GRACE score, which may cause the futile correlation. By contrast, GRACE score was not included in the regression model in Wang et al.'s study (13).
The possible mechanism of the correlation between serum calcium and left ventricular dysfunction is unclear. Serum calcium ions play a vital role in many metabolic and regulatory processes associated with cardiovascular disease, such as platelet adhesion and aggregation, blood coagulation, enzymatic activity, myocardial excitation, contraction and relaxation (8, 9). In view of the roles of serum calcium in myocardial excitation-contraction coupling and cardiac electrophysiologic effect, abnormalities of serum calcium may cause disarrangement of calcium homeostasis in the cytoplasm of cardiomyocytes and lead to myocardial dysfunction (22). On the other side, hypocalcemia reduces renal sodium excretion (26), thus contributes to fluid overload and decreased myocardial contractility, as demonstrated by decreased left ventricular work index (9, 27). In addition, decreased serum calcium was correlated with various common cardiovascular risk profiles, such as hypertension, dyslipidemia, and so on (8).
This study had some limitations. First, it was a single-center, observational study, whether similar results are obtained in other patient categories remains to be investigated. Second, the current study included a relatively small number of patients with LVEF ≤ 50%. Third, recent studies (28, 29) found that high curvatures and branching of coronary arteries were associated with the risk of development of atherosclerosis and plaque formation, however, coronary curvatures and branching were not considered in our study. ACS patients with non-obstructive coronary artery were not included. Fourth, serum calcium measurement was performed on a single occasion after admission. Serum calcium levels might vary over time, therefore a longitudinal study is required. Finally, the pathophysiologic mechanism of the association between hypocalcaemia and left ventricular dysfunction was not investigated in the present study. However, with the explorative results generated from this study, a further study will be conducted.
In summary, admission serum calcium was positively correlated with LVEF and negatively with BNP in ACS patients. Low admission serum calcium was an independent biomarker for elevated BNP.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethical Committee of Beijing Tiantan Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
HW contributed to assembly of data, performed data analysis and interpretation, and wrote the manuscript. RW carried out the studies, collected and analyzed data, and participated in manuscript writing. JT conceived and designed this study, provided administrative support, collected and analyzed data, and wrote the manuscript. All authors have read and approved the final manuscript.
Funding
This work was supported by the Basic and Clinical Research Collaboration Programme (15JL55), Capital Medical University.
Acknowledgments
The authors thank all the staff in Department of Cardiovascular Medicine, Beijing Tiantan Hospital, Capital Medical University for their generous supports in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. (2019) 16:203–12. doi: 10.1038/s41569-018-0119-4
2. Mahmood SS, Levy D, Vasan RS, Wang TJ. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet. (2014) 383:999–1008. doi: 10.1016/S0140-6736(13)61752-3
3. Yahud E, Tzuman O, Fink N, Goldenberg I, Goldkorn R, Peled Y, et al. Trends in long-term prognosis according to left ventricular ejection fraction after acute coronary syndrome. J Cardiol. (2020) 76:303–8. doi: 10.1016/j.jjcc.2020.03.012
4. Kwok CS, Bachmann MO, Mamas MA, Stirling S, Shepstone L, Myint PK, Zaman MJ. Effect of age on the prognostic value of left ventricular function in patients with acute coronary syndrome: a prospective registry study. Eur Heart J Acute Cardiovasc Care. (2017) 6:191–8. doi: 10.1177/2048872615623038
5. HananiaG, CambouJP, Guéret P, Vaur L, Blanchard D, Lablanche JM, et al. USIC 2000 Investigators. Management and in-hospital outcome of patients with acute myocardial infarction admitted to intensive care units at the turn of the century: results from the French nationwide USIC 2000 registry. Heart. (2004) 90:1404–10. doi: 10.1136/hrt.2003.025460
6. Lopez-Jimenez F, Goraya TY, Hellermann JP, Jacobsen SJ, Reeder GS, Weston SA, et al. Measurement of ejection fraction after myocardial infarction in the population. Chest. (2004) 125:397–403. doi: 10.1378/chest.125.2.397
7. Khaled S, Matahen R. Cardiovascular risk factors profile in patients with acute coronary syndrome with particular reference to left ventricular ejection fraction. Indian Heart J. (2018) 70:45–9. doi: 10.1016/j.ihj.2017.05.019
8. Zhang C, Cao B, Huang X, Gu J, Xia M, Yang X, et al. Association between serum calcium and first incident acute myocardial infarction: a cross-sectional study. Iran J Public Health. (2020) 49:1278–88. doi: 10.18502/ijph.v49i7.3581
9. Yan S, Liu XJ, Peng Y, Xia TL, Liu W, Tsauo JY, et al. Admission serum calcium levels improve the grace risk score prediction of hospital mortality in patients with acute coronary syndrome. Clin Cardiol. (2016) 39:516–23. doi: 10.1002/clc.22557
10. Lutsey PL, Alonso A, Michos ED, Loehr LR, Astor BC, Coresh J, Folsom AR. Serum magnesium, phosphorus, and calcium are associated with risk of incident heart failure: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Clin Nutr. (2014) 100:756–64. doi: 10.3945/ajcn.114.085167
11. Li J, Wu N, Dai W, Jiang L, Li Y, Li S, Wen Z. Association of serum calcium and heart failure with preserved ejection fraction in patients with type 2 diabetes. Cardiovasc Diabetol. (2016) 15:140. doi: 10.1186/s12933-016-0458-6
12. Cubbon RM, Thomas CH, Drozd M, Gierula J, Jamil HA, Byrom R, et al. Calcium, phosphate and calcium phosphate product are markers of outcome in patients with chronic heart failure. J Nephrol. (2015) 28:209–15. doi: 10.1007/s40620-014-0075-y
13. Wang Y, Ma H, Hao X, Yang J, Chen Q, Lu L, et al. Low serum calcium is associated with left ventricular systolic dysfunction in a Chinese population with coronary artery disease. Sci Rep. (2016) 6:22283. doi: 10.1038/srep22283
14. Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyauchi K, et al. Japanese Circulation Society Joint Working Group. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J. (2019) 83:1085–96. doi: 10.1253/circj.CJ-19-0133
15. Yamauchi Y, Fujita SI, Shibata K, Morita H, Ito T, Sohmiya K, et al. Is serum uric acid independently associated with left ventricular mass index, ejection fraction, and B-type natriuretic peptide among female and male cardiac patients? Int Heart J. (2017) 58:562–9. doi: 10.1536/ihj.16-359
16. Berman J, Lee L, Monga R, Ye K, Sprayregen S, Haramati LB. Clearing the congestion: chest radiography and BNP to rule-out congestive heart failure. J Thorac Imaging. (2021) 1–5. doi: 10.1097/RTI.0000000000000625
17. Logeart D, Saudubray C, Beyne P, Thabut G, Ennezat PV, Chavelas C, et al. Comparative value of Doppler echocardiography and B-type natriuretic peptide assay in the etiologic diagnosis of acute dyspnea. J Am Coll Cardiol. (2002) 40:1794–800. doi: 10.1016/S0735-1097(02)02482-8
18. Douglas PS, Patel MR, Bailey SR Dai D, Kaltenbach L, Brindis RG, et al. Hospital variability in the rate of finding obstructive coronary artery disease at elective, diagnostic coronary angiography. J Am Coll Cardiol. (2011) 58:801–9. doi: 10.1016/j.jacc.2011.05.019
19. Perumalsamy S, Wan Ahmad WA, Zaman Huri H. Single Nucleotide Polymorphism rs17173608 in the Chemerin Encoding Gene: is it a predictor of insulin resistance and severity of coronary artery disease in non-obese type 2 diabetes? Healthcare. (2021) 9:623. doi: 10.3390/healthcare9060623
20. Albert J, Lezius S, Störk S, Morbach C, Güder G, Frantz S, et al. Trajectories of left ventricular ejection fraction after acute decompensation for systolic heart failure: concomitant echocardiographic and systemic changes, predictors, and impact on clinical outcomes. J Am Heart Assoc. (2021) 10:e017822. doi: 10.1161/JAHA.120.017822
21. Spitzer E, Pavo N, Abdelghani M, Beitzke D, Ren B, García-Ruiz V, et al. Assessment of left ventricular ejection fraction with late-systolic and mid-diastolic cardiac phases using multi-slice computed tomography. Radiography. (2018) 24:e85–90. doi: 10.1016/j.radi.2018.04.007
22. Su W, Zhu JG, Zhao XQ, Chen H, Li WP Li HW. Altered serum calcium homeostasis independently predicts mortality in patients with acute coronary syndrome: a retrospective observational cohort study. BMJ Open. (2021) 11:e049957. doi: 10.1136/bmjopen-2021-049957
23. Jensen AC, Polcwiartek C, Søgaard P, Mortensen RN, Davidsen L, Aldahl M, et al. The association between serum calcium levels and short-term mortality in patients with chronic heart failure. Am J Med. (2019) 132:200–8. doi: 10.1016/j.amjmed.2018.10.006
24. Batra CM, Agarwal R. Hypocalcemic cardiomyopathy and pseudohypoparathyroidism due to severe vitamin D deficiency. J Assoc Phys India. (2016) 64:74–6.
25. Wong KK, Wang D, Ko JK, Mazumdar J, Le TT, Ghista D. Computational medical imaging and hemodynamics framework for functional analysis and assessment of cardiovascular structures. Biomed Eng Online. (2017) 16:35. doi: 10.1186/s12938-017-0326-y
26. Levine SN, Rheams CN. Hypocalcemic heart failure. Am J Med. (1985) 78:1033–5. doi: 10.1016/0002-9343(85)90228-1
27. Hurley K, Baggs D. Hypocalcemic cardiac failure in the emergency department. J Emerg Med. (2005) 28:155–9. doi: 10.1016/j.jemermed.2004.06.014
28. Wong KKL, Wu J, Liu G, Huang W, Ghista DN. Coronary arteries hemodynamics: effect of arterial geometry on hemodynamic parameters causing atherosclerosis. Med Biol Eng Comput. (2020) 58:1831–43. doi: 10.1007/s11517-020-02185-x
Keywords: acute coronary syndrome, serum calcium, left ventricular dysfunction, left ventricular ejection fraction, B-type natriuretic peptide
Citation: Wang H, Wang R and Tian J (2022) Association of admission serum calcium level with left ventricular dysfunction in patients with acute coronary syndrome. Front. Cardiovasc. Med. 9:1018048. doi: 10.3389/fcvm.2022.1018048
Received: 12 August 2022; Accepted: 15 November 2022;
Published: 29 November 2022.
Edited by:
Ruizheng Shi, Central South University, ChinaReviewed by:
Ronak Soni, Jack Stephens Heart Institute, United StatesDefu Qiu, China University of Mining and Technology, China
Copyright © 2022 Wang, Wang and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junping Tian, dGlhbmpwNTA2QDE2My5jb20=
 Hong Wang
Hong Wang Rongrong Wang
Rongrong Wang Junping Tian
Junping Tian