
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med., 21 January 2022
Sec. Cardiac Rhythmology
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.795750
This article is part of the Research TopicWhat do we know about COVID-19 implications for cardiovascular disease?View all 109 articles
Background: Arrhythmia is a very common complication of coronavirus disease 2019 (COVID-19); however, the prevalence of ventricular arrhythmia and associated outcomes are not well-explored. Here, we conducted a systematic review and meta-analysis to determine the prevalence and associated death of ventricular arrhythmia and sudden cardiac death (SCD) in patients with COVID-19.
Methods: Databases of PubMed, Cochrane Library, Embase, and MdeRxiv were searched. Studies that could calculate the prevalence of ventricular arrhythmia/SCD during hospital admission or associated death in patients with COVID-19 were included. The study was registered with the PROSPERO (CRD42021271328).
Results: A total of 21 studies with 13,790 patients were included. The pooled prevalence of ventricular arrhythmia was 5% (95% CI: 4–6%), with a relatively high-SCD prevalence (1.8% in hospitalized COVID-19 and 10% in deceased cases of COVID-19). Subgroup analysis showed that ventricular arrhythmia was more common in patients with elevated cardiac troponin T [ES (effect size): 10%, 95% CI: −0.2 to 22%] and in European (ES: 20%, 95% CI: 11–29%) populations. Besides, ventricular arrhythmia was independently associated with an increased risk of death in patients with COVID-19 [odds ratio (OR) = 2.83; 95% CI: 1.78–4.51].
Conclusion: Ventricular arrhythmia and SCD resulted as a common occurrence with a high prevalence in patients with COVID-19 admitted to the hospital. Furthermore, ventricular arrhythmia significantly contributed to an increased risk of death in hospitalized patients with COVID-19. Clinicians might be vigilant of ventricular arrhythmias for patients with COVID-19, especially for severe cases.
Systematic Review Registration: www.york.ac.uk/inst/crd, identifier: CRD42021271328.
Coronavirus disease 2019 (COVID-19) is a serious life-threatening disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, which first occurred in November 2019 (1), and then rapidly spread throughout the rest of the world. As of July 31, 2021, more than 198 million individuals were diagnosed with cases of COVID-19, exceeding 420 thousand deaths. Although COVID-19 is characterized by substantial respiratory pathology, several extrapulmonary manifestations, such as thrombotic complications, myocardial dysfunction, and arrhythmia, acute kidney injury are also commonly found in patients afflicted with the virus (2–4).
Cardiac arrhythmias, such as new-onset atrial fibrillation, heart block, and ventricular arrhythmias, are prevalent in the patients with COVID-19. An early report study on 138 patients from Wuhan, China, showed that 17% of the hospitalized patients suffered from total arrhythmia (5). Our recent meta-analysis also showed that the atrial fibrillation reached 10% and was associated with increased death in COVID-19 (6). Ventricular arrhythmia is still the major leading cause of death from the cardiovascular diseases (7). According to a multicenter cohort from the US, 6% of 4,250 patients with COVID-19 had prolonged QTc interval (corrected QT; >500 ms) at admission (8). This result suggested that COVID-19 might significantly contribute to an increased risk of ventricular tachycardia as QTc prolongation is believed to predispose to the ventricular arrhythmias associated with sudden death in certain cardiac diseases. Although several studies have reported the increased risk of ventricular tachycardia among patients with COVID-19, the exact prevalence of ventricular tachycardia in patients with COVID-19 remains unknown. Moreover, a case series also reported ventricular tachycardia and ventricular fibrillation as the primary cause of death in hospitalized patients with COVID-19 without a prior history of the structural heart disease (9). However, it remains unclear whether COVID-19 associated the ventricular arrhythmias are independently linked to increased death in the patients with COVID-19.
Furthermore, sudden cardiac death (SCD) is the most devastating manifestation of ventricular arrhythmias that has emerged as one of the disturbing concerns associated with the infection of COVID-19. Thus, we conducted a systematic review and meta-analysis to determine the prevalence and associated death of ventricular arrhythmia and SCD in patients with COVID-19.
This study has been registered with PROSPERO (International prospective register of systematic reviews. www.york.ac.uk/inst/crd)-registration number-CRD42021271328. Furthermore, we conducted the meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (2020) (Supplementary Table 1).
The search was accomplished by two authors independently. PubMed, Embase, the Cochrane Library, and MedRxiv (https://www.medrxiv.org/) databases were searched mainly for the related studies up to July 21, 2021, without language restrictions. The search terms according to PICOS were as follows:
Population:
For COVID-19: “COVID-19” or “COVID-19 Virus Disease” or “COVID-19 Virus Infection” or “2019-nCoV Infection” or “Coronavirus Disease-19” or “2019 Novel Coronavirus Disease” or “2019 Novel Coronavirus Infection” or “2019-nCoV Disease” or “Coronavirus Disease 2019” or “SARS Coronavirus 2 Infection” or “SARS-CoV-2 Infection” or “COVID-19 Pandemic.”
Exposure:
For the ventricular arrhythmia: “ventricular arrhythmia” or “premature ventricular beats” or “ventricular ectopic beats” or “ventricular premature complex” or “premature ventricular contractions” or “ventricular tachycardia” or “ventricular tachyarrhythmia” or “ventricular flutter” or “ventricular fibrillation.”
For sudden cardiac death: “cardiac sudden death” or “sudden cardiac arrest” or “sudden cardiac death.”
Outcomes:
For death: “death” or “mortality.”
A detailed search strategy was described in Supplementary Table 2.
All the results were organized by EndNote X9 software (Thomson Reuters, New York, NY, USA). After deleting the duplicate literature, the titles and abstracts were checked, and the relevant literature was preliminarily screened. Subsequently, full-texts of the relevant studies were searched to make sure they met the inclusion criteria. The inclusion criteria included the following: (1) studies that included adult patients diagnosed with COVID-19 based on the polymerase chain reaction tests; (2) studies that could calculate the prevalence of ventricular arrhythmia/SCD during hospital admission or reported the estimated effect between ventricular arrhythmia and death in patients with COVID-19.
If the same population was used in multiple studies, we selected the article with the most informative or the largest sample size. Studies that reported the effect of chloroquine/hydroxychloroquine and azithromycin in patients with COVID-19 were excluded because of the potential drug-induced ventricular arrhythmias risk. Certain publication types without sufficient data (reviews, meta-analysis, cases, editorials, and comments) were also excluded.
The following information was independently abstracted by two researchers: the first author, publication year, country, time, study design, patient characteristics (sample size, age, and sex), number of ventricular arrhythmias, death, odds ratios (ORs), and the corresponding 95% CI and adjustments.
For studies that reported the prevalence, the Joanna Briggs Institute (JBI) critical appraisal checklist was used to assess the study quality, where 0 score represented a failure to meet the requirements; 1 represented the lack of detailed description, 2 score represented detailed and comprehensive description. For studies that reported the association between ventricular arrhythmia and death in patients with COVID-19, the Newcastle-Ottawa Scale (NOS) was applied. Studies with scores of NOS ≥ 7 and JBI ≥ 14 were considered as high-quality researches (10).
RevMan software, version 5.3 (The Cochrane Collaboration 2014, Nordic Cochrane Center Copenhagen, Denmark) and Stata software (Version 14.0, Stata Corp LP, College Station, Texas, US) were both applied in our analysis. To explore the prevalence of ventricular arrhythmia and SCD in hospitalized patients with COVID-19, the exact binomial (Clopper–Pearson) method was used to calculate 95% CIs. Freeman–Tukey double arcsine transformation was used for standard estimates. To elucidate the outcome of ventricular arrhythmia and SCD in hospitalized patients with COVID-19, we pooled the ORs for each studies using the inverse variance method. We also estimated the adjusted ORs by calculating the natural logarithm of the OR (log [OR]) and its standard error (SElog [OR]), which is shown with 95% CIs. We evaluated the degree of heterogeneity using the I2 test (25, 50, and 75% represent low, moderate, and high heterogeneity). We used the random effect model in our study to improve the reliability.
Subgroup analyses were performed to study possible factors influencing our results, including ventricular arrhythmia, region, cardiac injury, and population. To ensure the reliability of study outcomes, we carried out sensitivity analyses by omitting each study in turn. P < 0.05 was considered statistically significant.
The flow chart for the study selection process is shown in Figure 1. A total of 1,342 publications were identified following initial search (PubMed = 430; the Cochrane Library = 119; Embase = 405; MedRxiv = 388). After deleting 584 duplications and 680 irrelevant studies, the full-text assessment was performed on 78 studies. Subsequently, 57 articles were excluded due to the following reasons: (1) studies without insufficient data (n = 19); (2) certain publication types with no data (review = 11; case report = 3); (3) studies without appropriate population or exposure (n = 11); (4) studies that did not report target outcome (n = 13). Finally, 21 studies were included in the meta-analysis (11–31). All the excluded studies with reasons (n = 57) are shown in Supplementary Table 3.
The basic characteristics of all the included articles are shown in Table 1. Twenty-one studies (11–31), which included 13,790 hospitalized patients with COVID-19 with a mean age ranging from 50 to 70.3 years, and with sample sizes ranging from 54 to 4,526, were published from 2020 to 2021 [eight of them published in 2021 (11, 15, 16, 19, 24–26, 31), others in 2020 (12–14, 17, 18, 20–23, 27–30)]. Nine reports were from Asia [eight from China (13, 16, 18, 21, 22, 28, 29, 31), one from Iran (19)], seven from USA (11, 12, 14, 15, 17, 25, 30), and five from Europe [three from Italy (20, 24, 27), one from Netherland (23), one from Germany (26)]. Besides, 15 of them were retrospective studies (11, 13, 15–19, 21–23, 27–31), 5 were prospective studies (12, 14, 20, 25, 26), and 1 was cross-section study (24).
All studies (11–31) scored between 16 and 20 on the Joanna Briggs Institute Critical Appraisal Checklist, which meant these articles took rigorous methodology. In addition, five studies (16, 19, 21, 25, 27) involved the association between ventricular arrhythmia and death in patients with COVID-19, with NOS scores > 7, thus were regarded as moderate high-quality studies (Supplementary Table 4).
A total of 20 (11–30) studies with 13,509 patients reported the prevalence of ventricular arrhythmia in patients with COVID-19. As shown in Figure 2, the pooled prevalence of the ventricular arrhythmia was 5% (95% CI: 4–6%).
Subgroup analysis showed that premature ventricular complex was the most common type in patients with COVID-19 (ES: 13%; 95% CI: 7–19%), followed by ventricular tachycardia (ES: 10%; 95% CI: 6–13%) and ventricular fibrillation (ES: 1%; 95% CI: 1–2%) (Figure 3A). According to area subgroup analysis, Europe had the highest prevalence (ES: 20%; 95% CI: 11–29%), followed by the United States (ES: 7%; 95% CI: 1–13%), while the lowest prevalence was found in Asia (ES: 6%; 95% CI: 3–8%) (Figure 3B). Furthermore, the prevalence of the ventricular arrhythmia in hospitalized patients with elevated cardiac troponin T was 1.25-fold higher than that without elevated cardiac troponin T (ES: 10 vs. 8%) (Figure 3C). The prevalence of ventricular arrhythmia in living and deceased hospitalized patients with COVID-19 was 6 and 12%, respectively (Figure 3D).
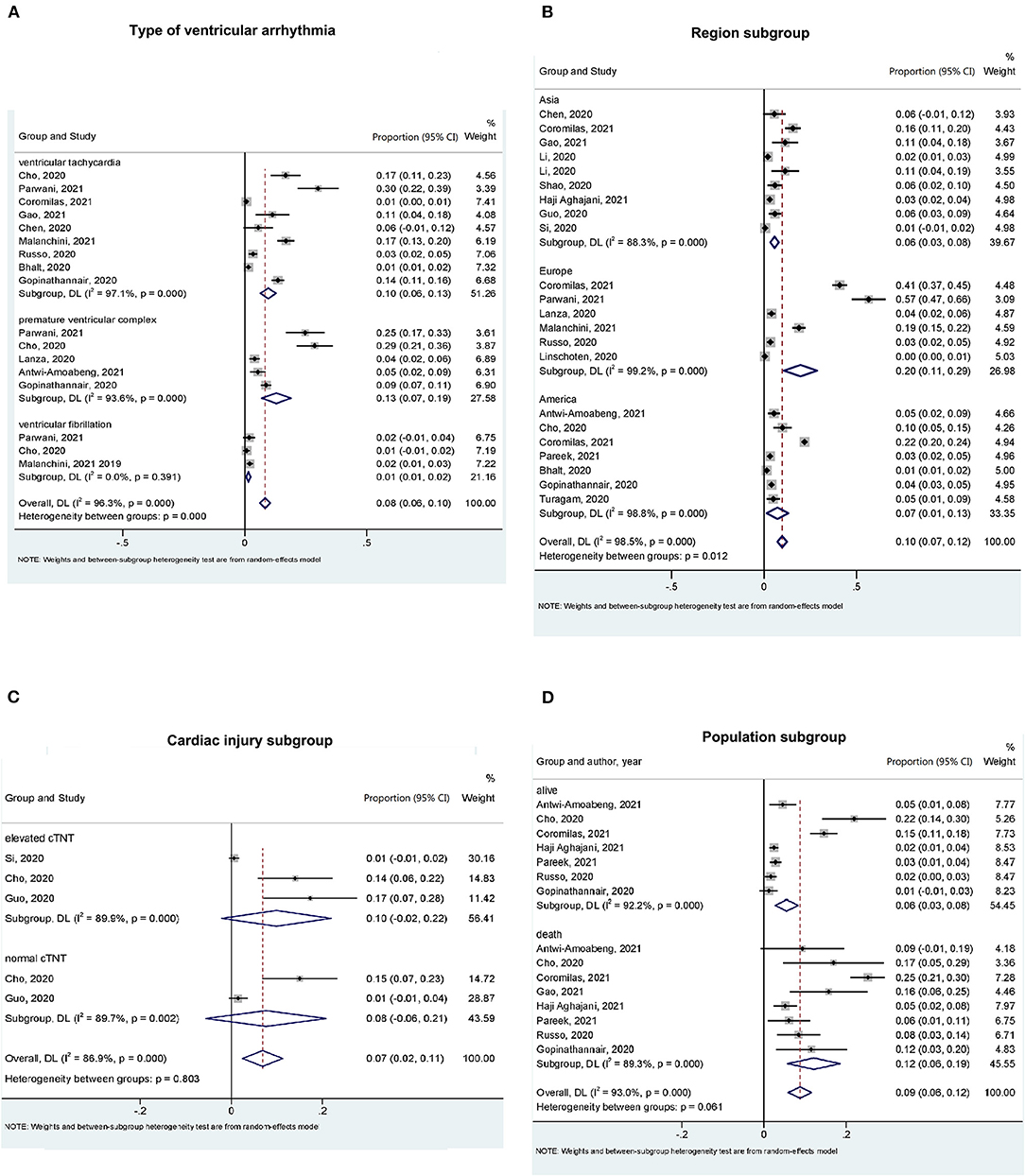
Figure 3. Subgroup analysis for the prevalence of ventricular arrhythmia in patients with COVID-19. (A) Ventricular arrhythmia type subgroup. According to ventricular arrhythmia type, ventricular tachycardia, premature ventricular complex, and ventricular fibrillation group were divided. (B) Region subgroup. According to region, Asia, Europe, and the United States group were divided. (C) Cardiac injury (cardiac troponin T level) subgroup. All the researches were divided into elevated cTNT and normal cTNT group according to cTNT level. (D) Population (alive and dead) subgroup. Alive and death population were divided.
Two articles reported the prevalence of SCD in hospitalized patients with COVID-19 (28, 31). Article of Shao reported that the prevalence of SCD was 1.8% in the population with COVID-19 (28). Also, according to Yang et al. there was a higher SCD prevalence (10%) in the deceased population with COVID-19 (31).
Five multivariable-adjusted publications with 2,568 patients were included in the analysis (16, 19, 21, 25, 27). The results showed a positive association between ventricular arrhythmia and risk of death in hospitalized patients with COVID-19 (OR = 2.83; 95% CI: 1.78–4.51%; I2 = 50%) (Figure 4), revealing a moderate heterogeneity. These results were stable when excluding Pareek et al. (25) with no evidence of heterogeneity (OR = 2.35; 95% CI: 1.74–2.39%; I2 = 0%). After deleting each study in turn, sensitivity analyses indicated that our results were stable, with a range from 2.35 (95% CI: 1.74–3.19%) to 3.41 (95% CI: 1.94–6.00%) (Supplementary Figure 1).
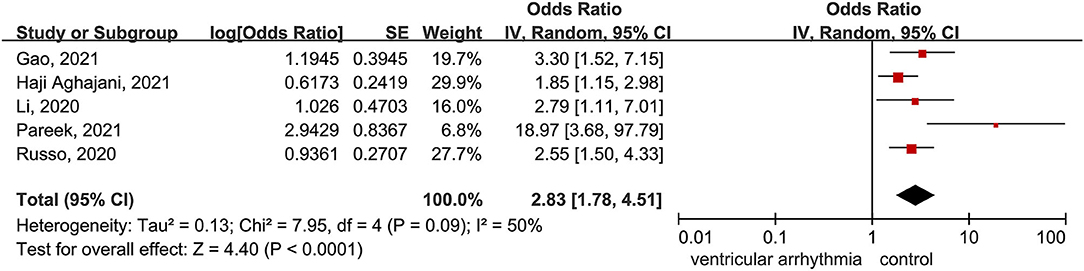
Figure 4. Forest plot for the association between the ventricular arrhythmia and death in patients with COVID-19.
The potential publication bias for death was not performed due to the limited number of studies (N < 10).
In this study, we pooled data from 21 studies with 13,790 hospitalized patients with COVID-19, finding that: (i) the prevalence of ventricular arrhythmia in hospitalized patients with COVID-19 was 5%. Specifically, the premature ventricular complex, ventricular tachycardia, and ventricular fibrillation occurred in 13, 10, 1% in the hospitalized patients, respectively. (ii) Ventricular arrhythmia was independently related to an increased risk of death in hospitalized patients with COVID-19. Overall, the ventricular arrhythmia and SCD were not uncommon and were associated with adverse outcomes in the hospitalized patients. To the best of our knowledge, this is the first meta-analysis that reported the prevalence of ventricular arrhythmia, SCD, and associated prognosis in the hospitalized patients with COVID-19.
Cardiac arrhythmia was identified as one of the major complications of SARS-COV during the outbreak in China in 2003 (32). Tachycardia was the most common type of arrhythmia among the patients infected with SARS-COV and was independent of fever (33, 34). Similarly, in hospitalized patients with COVID, arrhythmic events are not uncommon among the COVID-19 related cardiovascular complications. As we previously reported, atrial fibrillation is the most prevalent arrhythmia in hospitalized patients (6). Regarding ventricular arrhythmia, evidence from earliest cohorts from Wuhan, China, showed that ventricular arrhythmia occurred in 7% of patients (13/187) and that the rate of ventricular arrhythmia was almost doubled in patients with elevated troponin T levels on ICU admission (18), which is consistent with our results (Figure 3). However, the exact pathophysiology underlying ventricular arrhythmia in COVID-19 may be multifactorial and remains elusive.
First, as we previously described, cardiac injury or myocarditis commonly occurs due to the inhibited activity of angiotensin-converting enzyme 2 (ACE2) by SARS-COV2, which was found in 19% of hospitalized patients with COVID-19, and has been estimated to double among those with pre-existing cardiovascular and non-cardiovascular diseases (e.g., diabetes, hypertension, and cancers). These comorbidities might make their cardiomyocytes more vulnerable to be attacked by SARS-COV2 and thus causing a higher incidence of cardiac injury (35, 36). This cardiac injury might contribute to the abnormalities in cardiac electrophysiology, eventually inducing ventricular arrhythmia. This supposition is consistent with our subgroup analysis, which showed that the incident rate of ventricular arrhythmia increased with cardiac injury. Secondly, it is well-known that COVID-19 is characterized by the dysregulated immune response and cytokine release syndrome. Numerous studies have shown an elevation of serum inflammatory markers, such as C-reactive protein, ferritin, erythrocyte sedimentation rate (37). It has also been identified as a predictor of severity and death in patients with COVID-19. On the other hand, various pro-inflammatory factors, such as C-reactive protein and tumor necrosis factor α, have also been shown to promote ventricular arrhythmia significantly (38). Third, thrombotic complications are the main extrapulmonary manifestations of COVID-19 (37). For example, autopsies performed at a single academic medical center revealed deep venous thrombosis in 7 out of 12 patients (58%) who were not suspected of venous thromboembolism before death. Pulmonary embolism was the direct cause of death in four of these patients (39).
Limited studies reported the incidence of SCD in patients with COVID-19, our review showed it to be 1.8% in the all-hospitalized population with COVID-19 and 10% in the decreased patients. This incident rate is strikingly higher than that reported in the US in patients without COVID-19 (40). One study reported that the incidence of SCD was 14.9–110.8 per 100,000 in population with a non-COVID-19 in different regions (41). Nonetheless, the above results were consistent with several reports. For example, a cohort from Pennsylvania reported a 1.3% incidence of cardiac arrest amongst 700 urban patients admitted for COVID-19 (12). Furthermore, a multicenter cohort study in the US showed that 2.2% of non-ICU (intensive care unit) patients developed in-hospital sudden arrest (42). In the context of COVID-19, Acharya et al. showed the incidence of in-hospital sudden arrest for ICU patients was 15.4% in hospital patients (42). Yet, only ~7% of the patients with COVID-19 survived to discharge after experiencing in-hospital sudden arrest according to their report (42). Currently, the reason for this high SCD or cardiac arrest rate is not fully evident, and both the cardiac (e.g., undetected ventricular fibrillation) or non-cardiac (e.g., missed pulmonary embolisms) factors might be responsible for this condition.
Our results also showed that ventricular arrhythmia was more likely to occur in American and European patients compared to Asian patients. This should be interpreted considering the limited sample size and differences in baseline characteristics. Notably, the hospitalized American and European patients were mostly older compared with Chinese patients (Table 1). Additionally, the prevalence of common comorbidities, such as obesity and diabetes, was also higher in American and European populations than in Asia. All the aforementioned risk factors might be contributing to a higher incidence rate of cardiac injury or severity of COVID-19 cases in American and European populations. Therefore, the regional difference should be validated by further studies.
Previous studies have proved that COVID-19 can significantly affect the cardiovascular system of the patient, leading to serious cardiovascular diseases (3, 4, 43). Also, the previous studies had revealed a positive relationship between arrhythmia and COVID-19 (4, 24, 43, 44). Two meta-analyses studied the relationship between COVID-19 and ventricular arrhythmia. However, one of them focused on the patients after chloroquine or hydroxychloroquine treatment (45), while another explored the effect of COVID-19 on QTd, Tp-e/QTc ratio, and Tp-e interval (46). In addition, two meta-analyses described the relationship between COVID-19 and all types of arrhythmias (47, 48). Nevertheless, most of the included studies reported atrial fibrillation. Our meta-analysis extended the previous study and quantified'prevalence of ventricular arrhythmias and is associated with the clinical outcomes in hospitalized patients with COVID-19.
Considering the prevalence of the ventricular arrhythmias in patients with COVID-19, clinicians should be vigilant of ventricular arrhythmias in patients with COVID-19. Screening of high-risk groups for ventricular arrhythmias should be performed at admission. ECG monitoring at admission is suggested for those hospitalized patients who might be at higher risk for the cardiac arrhythmias, such as those with the cardiac injury, palpitations, dizziness, unexplained syncope, and prolonged QTc. In addition, although it is still being debated whether hydroxychloroquine and azithromycin are linked to increased risk of ventricular arrhythmia (49), hydroxychloroquine, and azithromycin can significantly prolong QT interval, which might lead to the ventricular arrhythmia (50, 51). The non-pharmacological treatment (e.g., nutrition support) might also benefit (51). Therefore, these aforementioned treatments might be more carefully evaluated before application or avoided for patients with COVID-19 who were susceptible to ventricular arrhythmias.
Our study has several limitations. First, a high degree of heterogeneity was observed in our results, which might be due to study design of the patients and baseline characteristics. For example, ventricular arrhythmia was monitored by a telemetry monitor in the study of Cho (14), while other studies used regular ECG or electrocardiography monitoring. Second, all the studies included hospitalized patients, which may overestimate the prevalence of the ventricular arrhythmia and its clinical impact on patients with COVID-19 compared with the community patients. Third, due to data restrictions, we could not explore the sex or age differences in the association between the ventricular arrhythmia and death. Third, as shown in Table 1, a number of patients receiving drugs tend to prolong the QT interval, which might overestimate the prevalence of the ventricular arrhythmia or SCD. Finally, considering the limited sample size, the incident rate related to the regional differences still needs to be validated by further studies.
Ventricular arrhythmia and SCD resulted as a common occurrence with a high prevalence in the hospitalized patients with COVID-19. Furthermore, the ventricular arrhythmia significantly contributed to an increased risk of death in hospitalized patients with COVID-19. Clinicians might be vigilant of ventricular arrhythmias for patients with COVID-19, especially for the severe cases.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
XL and PY were responsible for the entire project and revised the draft. ZT, KM, and ML performed the data extraction, statistical analysis, drafted the first version of the manuscript, and interpreting the data. All authors participated in the interpretation of the results and prepared the final version of the manuscript.
This work was supported in part by the National Natural Science Foundation of China (XL: 82100347, PY: 81760050 and 81760048), China Postdoctoral Science Foundation (XL: 2021M703724), and the Jiangxi Provincial Natural Science Foundation for Youth Scientific Research (PY: 20192ACBL21037).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We acknowledge all people who fought against COVID-19.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.795750/full#supplementary-material
1. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. (2021) 19:141–54. doi: 10.1038/s41579-020-00459-7
2. Babapoor-Farrokhran S, Rasekhi RT, Gill D, Babapoor S, Amanullah A. Arrhythmia in COVID-19. SN comprehensive. Clin Med. (2020) 2:1430–5. doi: 10.1007/s42399-020-00454-2
3. Stasi C, Fallani S, Voller F, Silvestri C. Treatment for COVID-19: An overview. Eur J Pharmacol. (2020) 889:173644. doi: 10.1016/j.ejphar.2020.173644
4. Chang WT, Toh HS, Liao CT Yu WL. Cardiac involvement of COVID-19: a comprehensive review. Am J Med Sci. (2021) 361:14–22. doi: 10.1016/j.amjms.2020.10.002
5. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061–9. doi: 10.1001/jama.2020.1585
6. Li Z, Shao W, Zhang J, Ma J, Huang S, Yu P, et al. Prevalence of atrial fibrillation and associated mortality among hospitalized patients with COVID-19: a systematic review and meta-analysis. Front Cardiovasc Med. (2021) 8:720129. doi: 10.3389/fcvm.2021.720129
7. Weiss JN, Nademanee K, Stevenson WG, Singh B. Ventricular arrhythmias in ischemic heart disease. Ann Intern Med. (1991) 114:784–97. doi: 10.7326/0003-4819-114-9-784
8. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. (2020) 323:2052–9. doi: 10.1001/jama.2020.6775
9. Abrams MP, Coromilas EJ, Wan EY, Rubin GA, Garan H, Dizon JM. Malignant ventricular arrhythmias in patients with severe acute respiratory distress syndrome due to COVID-19 without significant structural heart disease. HeartRhythm Case Rep. (2020) 6:858–62. doi: 10.1016/j.hrcr.2020.08.017
10. Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
11. Antwi-Amoabeng D, Beutler BD, Singh S, Taha M, Ghuman J, Hanfy A, et al. Association between electrocardiographic features and mortality in COVID-19 patients. Ann Noninvasive Electrocardiol. (2021) 26:e12833. doi: 10.1111/anec.12833
12. Bhatla A, Mayer MM, Adusumalli S, Hyman MC, Oh E, Tierney A, et al. COVID-19 and cardiac arrhythmias. Heart Rhythm. (2020) 17:1439–44. doi: 10.1016/j.hrthm.2020.06.016
13. Chen Q, Xu L, Dai Y, Ling Y, Mao J, Qian J, et al. Cardiovascular manifestations in severe and critical patients with COVID-19. Clin Cardiol. (2020) 43:796–802. doi: 10.1002/clc.23384
14. Cho JH, Namazi A, Shelton R, Ramireddy A, Ehdaie A, Shehata M, et al. Cardiac arrhythmias in hospitalized patients with COVID-19: a prospective observational study in the western United States. PLoS ONE. (2020) 15:e0244533. doi: 10.1371/journal.pone.0244533
15. Coromilas EJ, Kochav S, Goldenthal I, Biviano A, Garan H, Goldbarg S, et al. Worldwide survey of COVID-19-associated arrhythmias. Circ Arrhythm Electrophysiol. (2021) 14:e009458. doi: 10.1161/CIRCEP.120.009458
16. Gao P, Wu W, Tian R, Yan X, Qian H, Guo F, et al. Association between tachyarrhythmia and mortality in a cohort of critically ill patients with coronavirus disease 2019 (COVID-19). Ann Transl Med. (2021) 9:2282. doi: 10.21037/atm-21-2282
17. Gopinathannair R, Merchant FM, Lakkireddy DR, Etheridge SP, Feigofsky S, Han JK, et al. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J Interv Card Electrophysiol. (2020) 59:329–36. doi: 10.1007/s10840-020-00789-9
18. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. (2020) 5:811–8. doi: 10.1001/jamacardio.2020.1017
19. Haji Aghajani M, Toloui A, Aghamohammadi M, Pourhoseingholi A, Taherpour N, Sistanizad M, et al. Electrocardiographic findings and in-hospital mortality of covid-19 patients; a retrospective cohort study. Arch Acad Emerg Med. (2021) 9:e45. doi: 10.22037/aaem.v9i1.1250
20. Lanza GA, De Vita A, Ravenna SE, D'Aiello A, Covino M, Franceschi F, et al. Electrocardiographic findings at presentation and clinical outcome in patients with SARS-CoV-2 infection. Europace. (2021) 23:123–9. doi: 10.1093/europace/euaa245
21. Li J, Guo T, Dong D, Zhang X, Chen X, Feng Y, et al. Defining heart disease risk for death in COVID-19 infection. QJM. (2020) 113:876–82. doi: 10.1093/qjmed/hcaa246
22. Li L, Zhang S, He B, Chen X, Wang S, Zhao Q. Risk factors and electrocardiogram characteristics for mortality in critical inpatients with COVID-19. Clin Cardiol. (2020) 43:1624–30. doi: 10.1002/clc.23492
23. Linschoten M, Peters S, van Smeden M, Jewbali LS, Schaap J, Siebelink HM, et al. Cardiac complications in patients hospitalised with COVID-19. Euro Heart J. (2020) 9:817–23. doi: 10.1177/2048872620974605
24. Malanchini G, Ferrari P, Leidi C, Ferrari G, Racheli M, Senni M, et al. Ventricular arrhythmias among patients with implantable cardioverter-defibrillator during the COVID-19 pandemic. J Arrhythmia. (2021) 37:407–13. doi: 10.1002/joa3.12518
25. Pareek M, Singh A, Vadlamani L, Eder M, Pacor J, Park J, et al. Relation of cardiovascular risk factors to mortality and cardiovascular events in hospitalized patients with coronavirus disease 2019 (from the Yale COVID-19 cardiovascular registry). Am J Cardiol. (2021) 146:99–106. doi: 10.1016/j.amjcard.2021.01.029
26. Parwani AS, Haug M, Keller T, Guthof T, Blaschke F, Tscholl V, et al. Cardiac arrhythmias in patients with COVID-19: Lessons from 2300 telemetric monitoring days on the intensive care unit. J Electrocardiol. (2021) 66:102–7. doi: 10.1016/j.jelectrocard.2021.04.001
27. Russo V, Di Maio M, Mottola FF, Pagnano G, Attena E, Verde N, et al. Clinical characteristics and prognosis of hospitalized COVID-19 patients with incident sustained tachyarrhythmias: a multicenter observational study. Eur J Clin Invest. (2020) 50:e13387. doi: 10.1111/eci.13387
28. Shao F, Xu S, Ma X, Xu Z, Lyu J, Ng M, et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. (2020) 151:18–23. doi: 10.1016/j.resuscitation.2020.04.005
29. Si D, Du B, Ni L, Yang B, Sun H, Jiang N, et al. Death, discharge and arrhythmias among patients with COVID-19 and cardiac injury. Cmaj. (2020) 192:E791–8. doi: 10.1503/cmaj.200879
30. Turagam MK, Musikantow D, Goldman ME, Bassily-Marcus A, Chu E, Shivamurthy P, et al. Malignant arrhythmias in patients with COVID-19: incidence, mechanisms, and outcomes. Circ Arrhythm Electrophysiol. (2020) 13:e008920. doi: 10.1161/CIRCEP.120.008920
31. Yang N, Tian K, Jin M, Zhang X, Zhang F, Shi X, et al. Sudden death of COVID-19 patients in Wuhan, China: a retrospective cohort study. J Glob Health. (2021) 11:05006. doi: 10.7189/jogh.11.05006
32. Lin L, Xu Y, He D, Han Y, Tang G-H, Yang Z-M, et al. A retrospective study on clinical features of and treatment methods for 77 severe cases of SARS. Am J Chin Med. (2003) 31:821–39. doi: 10.1142/S0192415X03001521
33. Yu CM, Wong RS, Wu EB, Kong SL, Wong J, Yip GW, et al. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J. (2006) 82:140–4. doi: 10.1136/pgmj.2005.037515
34. Lau ST, Yu WC, Mok NS, Tsui PT, Tong WL, Cheng SW. Tachycardia amongst subjects recovering from severe acute respiratory syndrome (SARS). Int J Cardiol. (2005) 100:167–9. doi: 10.1016/j.ijcard.2004.06.022
35. Quagliariello V, Bonelli A, Caronna A, Conforti G, Iovine M, Carbone A, et al. SARS-CoV-2 infection and cardioncology: from cardiometabolic risk factors to outcomes in cancer patients. Cancers. (2020) 12:3316. doi: 10.3390/cancers12113316
36. de Lucena TMC, da Silva Santos AF, de Lima BR, de Albuquerque Borborema ME, de Azevêdo Silva J. Mechanism of inflammatory response in associated comorbidities in COVID-19. Diab Metab Syndrome. (2020) 14:597–600. doi: 10.1016/j.dsx.2020.05.025
37. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. (2020) 26:1017–32. doi: 10.1038/s41591-020-0968-3
38. Chung MK, Martin DO, Sprecher D, Wazni O, Kanderian A, Carnes CA, et al. C-reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. (2001) 104:2886–91. doi: 10.1161/hc4901.101760
39. Wichmann D, Sperhake JP, Lutgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. (2020) 173:268–77. doi: 10.7326/L20-1206
40. Perman SM, Stanton E, Soar J, Berg RA, Donnino MW, Mikkelsen ME, et al. Location of in-hospital cardiac arrest in the United States-variability in event rate and outcomes. J Am Heart Assoc. (2016) 5:e003638. doi: 10.1161/JAHA.116.003638
41. Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, et al. Epidemiology of sudden cardiac death: global and regional perspectives. Heart Lung Circ. (2019) 28:6–14. doi: 10.1016/j.hlc.2018.08.026
42. Acharya P, Ranka S, Sethi P, Bharati R, Hu J, Noheria A, et al. Incidence predictors, and outcomes of in-hospital cardiac arrest in COVID-19 patients admitted to intensive and non-intensive care units: insights from the AHA COVID-19 CVD registry. J Am Heart Assoc. (2021) 10:e021204. doi: 10.1161/JAHA.120.021204
43. Salian VS, Wright JA, Vedell PT, Nair S, Li C, Kandimalla M, et al. COVID-19 transmission, current treatment, and future therapeutic strategies. Mol Pharm. (2021) 18:754–71. doi: 10.1021/acs.molpharmaceut.0c00608
44. Rav-Acha M, Orlev A, Itzhaki I, Zimmerman SF, Fteiha B, Bohm D, et al. Cardiac arrhythmias amongst hospitalised Coronavirus 2019 (COVID-19) patients: prevalence, characterisation, and clinical algorithm to classify arrhythmic risk. Int J Clin Pract. (2021) 75:13788. doi: 10.1111/ijcp.13788
45. Tleyjeh IM, Kashour Z, AlDosary O, Riaz M, Tlayjeh H, Garbati MA, et al. Cardiac toxicity of chloroquine or hydroxychloroquine in patients with COVID-19: a systematic review and meta-regression analysis. Mayo Clin Proc. (2021) 5:137–50. doi: 10.1016/j.mayocpiqo.2020.10.005
46. Tondas AE, Mulawarman R, Trifitriana M, Nurmaini S, Irfannuddin I. Arrhythmia risk profile and ventricular repolarization indices in COVID-19 patients: a systematic review and meta-analysis. J Infect Dev Ctries. (2021) 15:224–9. doi: 10.3855/jidc.13922
47. Liao SC, Shao SC, Cheng CW, Chen YC, Hung MJ. Incidence rate and clinical impacts of arrhythmia following COVID-19: a systematic review and meta-analysis of 17,435 patients. Crit Care. (2020) 24:690. doi: 10.1186/s13054-020-03368-6
48. Pellicori P, Doolub G, Wong CM, Lee KS, Mangion K, Ahmad M, et al. COVID-19 and its cardiovascular effects: a systematic review of prevalence studies. Cochrane Database Syst Rev. (2021) 3:Cd013879. doi: 10.1002/14651858.CD013879
49. Abrams MP, Wan EY, Waase MP, Morrow JP, Dizon JM, Yarmohammadi H, et al. Clinical and cardiac characteristics of COVID-19 mortalities in a diverse New York City Cohort. J Cardiovasc Electrophysiol. (2020) 31:3086–96. doi: 10.1111/jce.14772
50. Carron J, Sharif Z, Hussein H, Kennedy M, McAdam B, Sheahan R. Clinical guidance for navigating the QTc-prolonging and arrhythmogenic potential of pharmacotherapy during the COVID-19 pandemic. Ir J Med Sci. (2021) 190:403–9. doi: 10.1007/s11845-020-02291-7
Keywords: arrhythmia, ventricular arrhythmia, coronavirus disease 2019, prevalence, death, prognosis
Citation: Tan Z, Huang S, Mei K, Liu M, Ma J, Jiang Y, Zhu W, Yu P and Liu X (2022) The Prevalence and Associated Death of Ventricular Arrhythmia and Sudden Cardiac Death in Hospitalized Patients With COVID-19: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 8:795750. doi: 10.3389/fcvm.2021.795750
Received: 15 October 2021; Accepted: 07 December 2021;
Published: 21 January 2022.
Edited by:
Hendrik Tevaearai Stahel, Bern University Hospital, SwitzerlandReviewed by:
Nicola Maurea, G. Pascale National Cancer Institute Foundation (IRCCS), ItalyCopyright © 2022 Tan, Huang, Mei, Liu, Ma, Jiang, Zhu, Yu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peng Yu, eXVwZW5nX2p4bmRlZnlAMTYzLmNvbQ==; Xiao Liu, bGl1eDU4N0BtYWlsLnN5c3UuZWR1LmNu
†These authors share first authorship
‡These authors share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.