
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 25 November 2021
Sec. Atherosclerosis and Vascular Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.745539
This article is part of the Research Topic Lipids and Inflammation in Health and Disease View all 26 articles
 Jiayi Dong1†
Jiayi Dong1† Song Yang2†
Song Yang2† Qian Zhuang2
Qian Zhuang2 Junxiang Sun2
Junxiang Sun2 Pengfei Wei2
Pengfei Wei2 Xianghai Zhao2
Xianghai Zhao2 Yanchun Chen2
Yanchun Chen2 Xiaotian Chen1
Xiaotian Chen1 Mengxia Li1
Mengxia Li1 Lai Wei1
Lai Wei1 Changying Chen1
Changying Chen1 Yao Fan3
Yao Fan3 Chong Shen1,3*
Chong Shen1,3*Background: Dyslipidemia is one of the modifiable risk factors for cardiovascular diseases (CVD). Identifying subjects with lipid abnormality facilitates preventative interventions.
Objectives: To evaluate the effects of lipid indices on the risks of ischemic stroke (IS), coronary heart disease (CHD), CVD, all-cause death, and CVD death.
Methods: The cohort study of 4,128 subjects started in May 2009 and followed up to July 2020. Restricted cubic spline (RCS) regression analysis was used to explore the dose-response relationship between lipid indices with outcomes. Cox proportional hazard regression analysis was used to estimate the association with a hazard ratio (HR) and 95% CI.
Results: RCS analysis showed that there were significant linear associations of TG with IS, non-high-density lipoprotein cholesterol (HDL-C), apolipoprotein B (ApoB), and total cholesterol (TC)/HDL-C ratio with all-cause death, non-HDL-C and RC with CVD death, and significant non-linear associations of ApoB with IS and CVD, TC, LDL-C, ApoAI, and TC/HDL-C ratio with CHD, and TC with all-cause death (all P <0.1). Cox regression analysis revealed that subjects with TC <155 mg/dl (vs. 155–184 mg/dl), > 185 mg/dl (vs. 155–184 mg/dl), and ApoB <0.7 g/l (vs. ≥0.7 g/l) had higher risks of CHD (P < 0.05), the adjusted HRs (95% CIs) were 1.933 (1.248–2.993), 1.561 (1.077–2.261), and 1.502 (1.01–2.234), respectively. Subjects with ApoAI > 2.1 g/l (vs. 1.6–2.1 g/l) and TG <80 mg/dl (vs. 80–177 mg/dl) had higher risks of CVD and all-cause death (P < 0.05), the adjusted HRs (95% CIs) were 1.476 (1.031–2.115) and 1.234 (1.002–1.519), respectively.
Conclusions: Lower or higher levels of TC, higher level of ApoAI, and lower level of ApoB were associated with increased risks of CVD, and lower level of TG was associated with increased all-cause death. Maintaining optimal lipid levels would help to prevent CVD and reduce mortality.
Cardiovascular disease remains a major cause of premature mortality and rising health care costs across the world (1). In China, the prevalence rate of cardiovascular disease (CVD) increased significantly by 14.7% from 1990 to 2016 (2), which was likely to increase substantially in pace with population growth and aging. Among the major drivers of CVD, atherogenic dyslipidemia is one of the major and modifiable risk factors for CVD (3, 4). In recent years, the blood lipid level of the Chinese population has shown a significant upward trend (5), with a 30% and above prevalence rate of dyslipidemia in adults, whereas the rates of awareness, treatment, and control of dyslipidemia remain low (6). Therefore, it is necessary to evaluate the effect of lipid profiles on CVD and mortality, identify the high-risk population, and tailor risk reduction strategies.
Epidemiological studies have investigated the associations between lipid profiles and CVD, including stroke and coronary heart disease (CHD). Two large-scale, prospective cohort studies indicated that the elevated levels of conventional lipids indices including total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG), and the reduced level of high-density lipoprotein cholesterol (HDL-C) contributed to the increased risk of CVD incidence (7, 8). However, there was an inconsistency of the relationships between TC, HDL-C, LDL-C, and the risk of CVD incidence of all-cause death with a “U” or “J” pattern (9, 10). Due to the limitation in using a single lipid index to evaluate the relationship between dyslipidemia and CVD events and all-cause mortality, some studies proposed that apolipoprotein B (ApoB), apolipoprotein AI (ApoAI), lipoprotein (a) [Lp(a)] or lipid ratios had an additional clinical value, and recommended to attach importance to the measurement of ApoB in clinical practice (11–14). Interestingly, some studies indicated that the apolipoproteins and calculated lipid ratio as derived lipid indices have comparable CVD predictive value with conventional lipid indices (15, 16).
Most of the previous studies dealt with lipid indices as continuous variables for linear correlation or divided lipid indices into categorical variables according to the existing guidelines and percentage scales. Limited data were available on the non-linear relationship between lipids, especially the effect of low blood lipid and CVD events and mortality. Recently, restricted cubic spline (RCS) analyses have been widely used to explore the dose-response relationship in public health research. Therefore, this prospective cohort study aimed to quantitatively evaluate the effects of lipid profiles on CVD and death with a 10-year follow-up.
A cluster sampling survey was conducted in Guanlin and Xushe towns at Yixing City, Jiangsu province, from May 2009 to August 2009 (17). A total of 4,128 community-dwelling adults aged 24–96 years old were included at baseline. The first field follow-up survey proceeded from May to October in 2014. From the local disease and death register system of the centers for disease control and prevention (CDCs), CVD and death events were further followed up till July 27, 2020. The flow chart of study subjects is shown in Figure 1. All the subjects were followed for the outcome of all-cause death (n = 4,128), while the subjects with the corresponding disease at baseline were excluded for IS patients (n = 30), coronary heart disease (CHD) patients (n = 50), and CVD patients (n = 78).
All subjects were well-informed and signed informed consent before inclusion in the cohort study. The study was approved by the ethics committee of Nanjing Medical University (#200803307), Nanjing, China.
All subjects were interviewed using a questionnaire, underwent physical examinations and laboratory tests by trained investigators as previously described (18).
Smokers were defined as individuals who smoked ≥ 20 cigarettes/week lasting for at least 3 months a year. Drinkers were defined as those whose current or past alcohol consumption ≥ two times per week lasting for at least 6 months per year. Body mass index (BMI) was calculated as weight (kg)/height squared (m2). Individuals with an average systolic pressure (SBP) ≥ 140 mmHg or diastolic pressure (DBP) ≥ 90 mmHg, or a self-reported hypertension history or currently receiving antihypertensive medication were defined as hypertension cases. Individuals with fasting plasma glucose (FPG) ≥ 7 mmol/l, or a self-reported diabetes history, or currently receiving hypoglycemic medication were defined as diabetes cases.
Blood samples were collected after overnight fasting (>8 h), plasma TC, TG, HDL-C, LDL-C, ApoAI, ApoB, Lp(a), and glucose (GLU) levels were measured with an automatic biochemistry analyzer Olympus AU2700. Non-high-density lipoprotein cholesterol (non-HDL-C), remnant-cholesterol (RC), TC/HDL-C, TG/HDL-C, LDL-C/HDL-C, and ApoB/ApoAI were further calculated. The non-HDL-C value was calculated as TC minus HDL-C. RC was calculated as TC minus LDL-C minus HDL-C. The judgment of abnormal lipid levels determined dyslipidemia according to commonly detected clinical lipid indices of TC, TG, HDL-C, and LDL-C (TC ≥ 240 mg/dl, or TG ≥ 200 mg/dl, or LDL-C ≥ 160 mg/dl, or HDL-C <40 mg/dl) or the self-reported history of the disease, or taking lipid-lowering drugs (19).
Lipid indices were categorized according to the dose-response relationships with CVD events and mortality tested by RCS regression analyses. If the relationship of lipid parameter and outcome was linear or no overall association, considering selecting the median or guidelines reference value as a cut-off point, if the median was close to the guidelines reference value, choose the latter as the final cut-off point, otherwise select the former. If the relationship of lipid parameter and outcome was U-shaped, select the lipid level with the corresponding HR of 1 in the RCS regression analyses or guidelines reference value as cut-off points. If there was a range with a corresponding HR value of 1, and the range was close to the guideline reference, the latter was chosen as the final cut-off point, otherwise the former was selected.
Outcome events of stroke, CHD, CVD, death, and CVD death were recorded from the disease and death register system, further inspected by certified neurologists and cardiologists of People's Hospital of Yixing City. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) was used to identify for stroke (I60–I64), ischemic stroke (I63), hemorrhagic stroke (I60, I61, I62, and I64), and CHD (I20, I21, I22, I25.5, I25.6, and I46.1). In this study, CVD only included stroke and CHD.
Quantitative variables were presented as median (interquartile range) for the data with non-normal distribution, and the difference between the two groups was compared with the Mann-Whitney U-test. Qualitative variables were presented as frequencies and proportions, the difference among groups was compared with Chi-square (χ2) test. The dose-response relationships of lipid levels with CVD events and death were characterized by multiple adjusted RCS regression with four knots at the 5th, 35th, 65th, and 95th percentiles. Incidence density was calculated with censor data and Cox proportional hazard regression analysis was performed to estimate the hazard ratios (HRs) and 95% CIs and also multiple factor analysis with adjustment for age, gender, smoking, drinking, BMI, hypertension, diabetes, and lipid-lowering treatments.
For the linear and non-linear relationship analysis of RCS, a P-value <0.1 was defined as statistical significance for the non-linearity and linearity tests. A two-tailed P-value <0.05 was defined as statistical significance for the association analyses. All statistical analyses were performed with SAS version 9.4 (SAS Institute, Inc, Cary, NC).
Baseline characteristics of 4,128 subjects were summarized in Table 1. During a median duration of 10.75-years follow-up, a total of 272, 189, 434, 519, 157 subjects developed IS, CHD, CVD, all-cause death, and CVD death, respectively. The proportion of subjects with dyslipidemia was 36.07% at baseline. Compared with subjects without dyslipidemia, those with dyslipidemia were more likely to have a higher level of BMI, and higher proportions of hypertension and diabetes (P < 0.05). Age, gender, and the proportion of smokers and drinker were comparable between the two groups (Table 1).
The results of RCS regression analyses are shown in Supplementary Figures 1–13. ApoB had a non-linear association, and TG had a linear association with IS, respectively (P < 0.1). TC, LDL-C, ApoAI, and TC/HDL-C ratio had a non-linear association with CHD (P < 0.1). Also, ApoB had a non-linear association with CVD (P < 0.1). TC had a non-linear association, and non-HDL-C, ApoB, and TC/HDL-C ratio had a linear association with all-cause death, respectively (P < 0.1). Moreover, non-HDL-C and RC had a linear association with CVD death (P < 0.1).
According to the results of RCS regression analyses, each lipid index was differentially divided into categories by estimating the risk of IS, CHD, CVD, all-cause death, and CVD death. The cut-off points or reference ranges of lipid parameters for different outcome events were presented in Table 2.
The results of Cox proportional hazard regression analysis were summarized in Figure 2. TG ≥ 115 mg/dl (vs. <115 mg/dl) was significantly associated with increased risk of IS (unadjusted HR [95% CI]: 1.329 [1.044–1.691]), while the association was weakened after adjustment for confounding factors (adjusted HR [95% CI]: 1.216 [0.944–1.565]). Compared with the reference interval of 155–185 mg/dl, TC <155 mg/dl and > 185 mg/dl were both significantly associated with the increased risk of CHD (adjusted HRs [95% CIs]: 1.933 [1.248–2.993], 1.561 [1.077–2.261]) and CVD (adjusted HRs [95% CIs]: 1.375 [1.032–1.831], 1.272 [1.01–1.602]). Additionally, ApoAI > 2.1 g/l (vs. 1.6–2.1 g/l) was associated with the increased risk of CVD (adjusted HR [95% CI]: 1.476 [1.031–2.115]) and ApoB <0.7 g/l (vs. 0.7–0.9 g/l) was associated with increased risk of CHD (adjusted HR [95% CI]: 1.502 [1.01–2.234]). Moreover, TG <80 mg/dl (vs. 80–177 mg/dl) was associated with the increased risk of all-cause death (adjusted HR [95% CI]: 1.234 [1.002–1.519]). Furthermore, ApoB ≥0.9 g/l (vs. <0.9 g/l) was associated with decreased risk of CVD death (unadjusted HR [95% CI]:0.702 [0.511–0.964]) while the association was weakened after adjustment for confounding factors (adjusted HRs [95% CIs]:0.749 [0.54–1.038]).
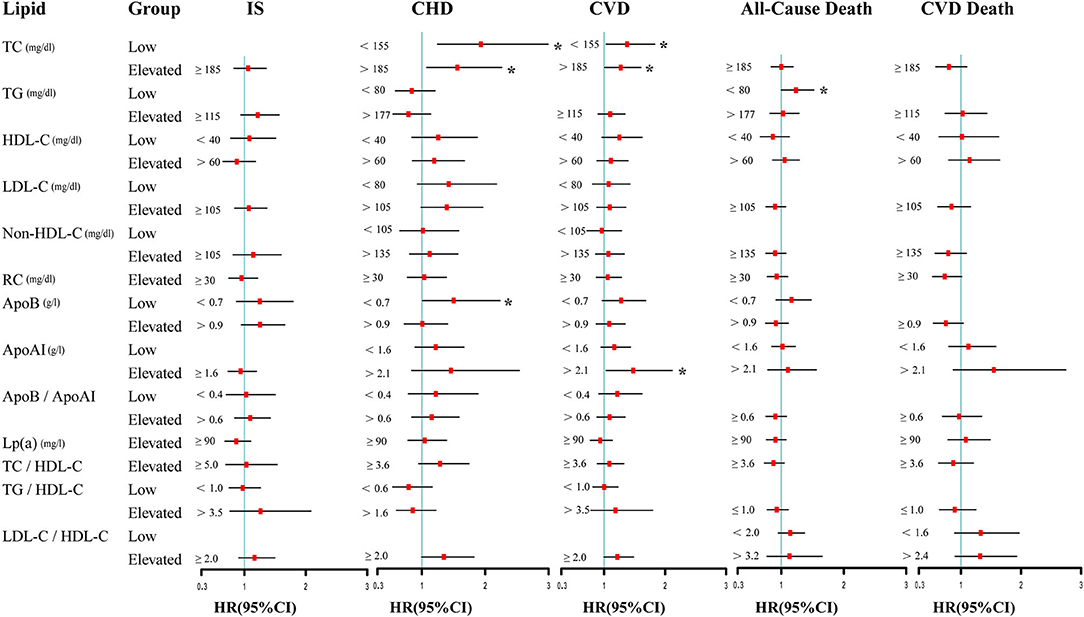
Figure 2. Multivariable adjusted association of lipid indices and IS, CHD, CVD, all-cause death, and CVD death. Cox regression was used to estimate adjusted hazard ratios (HRs) [95% confidence intervals (CIs)] for a low or elevated group of lipid indexes. Adjusted for age, gender, BMI, smoking, drinking, hypertension, diabetes, and lipid-lowering treatment. Lipid indices were divided into two groups (normal group and elevated group, or normal group and low group) or three groups (normal, low, and elevated groups) for different outcomes. Each square has an area inversely proportional to the variance of the log risk. The horizontal lines represent the 95% CI. ApoAI, Apolipoprotein AI; ApoB, Apolipoprotein B; CHD, coronary heart disease; CVD, cardiovascular diseases; HDL-C, high-density lipoprotein cholesterol; IS, ischemic stroke; LDL-C, low-density lipoprotein cholesterol; Lp(a), Lipoprotein(a); Non-HDL-C, non-high-density lipoprotein cholesterol; RC, remnant cholesterol; TC, total cholesterol; TG, triglycerides. *P < 0.05.
This study systematically analyzed the effects of lipid profiles on CVD events and death. The major findings indicated that lower and higher TC levels were associated with an increased risk of CVD. Lower ApoB levels and higher ApoAI levels were also associated with increased risk of CVD incidence. Furthermore, a lower level of TG was associated with an increased risk of all-cause death.
As an important lipid parameter, TC was used to explore the relationships between cholesterol and CVD events since Framingham Heart Study. The Asia Pacific Cohort Studies Collaboration (APCSC) integrated 30 cohort studies found a positive association between TC and CVD events; each 1 mmol/l increased for TC level was associated with a 41% greater risk of CHD incidence and 23% greater risk of IS incidence (20). However, further subgroup analysis by region indicated that such a relationship was observed among Australia and New Zealand populations but presented a “J” shaped relationship among Asian populations, including Chinese. Additionally, a recent cohort study of 364,486 UK populations free of CVD found a “U” shaped relationship between TC and the risk of CVD incidence (12). The above findings were inconsistent with traditional views but similar to our result, which revealed that lower and higher TC levels were associated with increased risk of CVD incidence. The discrepancy might be explained by the variation of cholesterol levels across countries. The cholesterol level of the Chinese rural population was lower than those in developed countries, in which the proportion of the population with low cholesterol levels was relatively small (21). As a result, it's difficult to find the hazard effect of low TC levels on CVD incidence in those studies carried out in developed countries. Potential mechanisms accounting for the effect of low TC level on CVD may be due to the dysfunction of the cell membrane and the absence in the synthesis of important hormones, including estrogen (22). Estrogens can promote vasodilation, inhibit the renin-angiotensin system (23), reduce blood pressure, and regulate specific inflammatory markers and cytokines (24). Moreover, a multi-ethnic Study of Atherosclerosis of post-menopausal women observed that higher estradiol levels were associated with a lower CHD risk (25).
High-density lipoprotein cholesterol was regarded as “good cholesterol” for its reverse cholesterol transport function, and ApoAI was the important component of HDL for functioning normal biosynthesis (26, 27). Previous studies indicated that the level of ApoAI was inversely associated with CVD events. In the Apolipoprotein Mortality RISk (AMORIS) Study, per 1 SD increase of ApoAI accompanied a 19% reduction of risk of major cardiovascular events (MACE) (28). Similarly, a study from UK Biobank observed that ApoAI per 1 SD (0.27 g/l) increased was inversely associated with risk of CVD, but did not explore potential non-linear relationship (15). In contrast, a significant association of elevated ApoAI with the increased risk of CVD was observed in our study, whereas not for stroke or CHD, the underlying mechanism accounting for the impact of elevated HDL-C and or ApoAI on CVD deserves further exploration.
The key role of LDL-C played in the development and progression of CVD events has been well-illustrated. ApoB was highly related to LDL-C (r > 0.9), and one molecule of ApoB was mostly presented in each atherogenic lipoprotein (12, 13, 29). Therefore, ApoB could accurately reflect the total atherogenic lipoprotein in blood and is considered a superior CVD predictor. A cohort from the Stockholm area (Sweden) indicated that elevated ApoB level was a risk predictor of early CVD. Additionally, another large-scale cohort study showed that ApoB was positively correlated with CVD risk; 1 SD increased ApoB, resulting in a 23% increase in CVD risk (12). Unexpectedly, we observed that low ApoB level (< 0.7 g/l) also increased the risk of CHD, and this finding was firstly reported in this study.
In previous studies, TG presented a positive relationship with all-cause death, and elevated TG level was associated with increased all-cause death risk (30, 31). Inconsistent with the above results reduced TG level was associated with a higher risk of all-cause death in our analysis. Recently, some studies proposed the concept of the “TG paradox,” they found that the level of TG showed a negative relationship with the risk of all-cause death in the CVD patients (32, 33). The adverse effects of low TG level could be that TG level was highly associated with BMI (34), low level of TG reflected the poor nutritional status of subjects, and BMI was negatively associated with the risk of all-cause death (35), which named “obesity paradox” (36).
The current study has several strengths. First, prospective cohort design spanning over 10 years to investigate the effects of lipid profiles including routine lipids, apolipoproteins, and lipid ratios on the risk of CVD and death, making the conclusion more reliable. Second, the blood lipids levels were comparable to the national level from the 2013–2014 China Chronic Disease and Risk Factor Surveillance (CCDRFS) consisting of 163,641 adults, making the conclusion more representative (37).
There were limitations in this study. Firstly, the sample size is relatively small, which may limit the power of detection. Secondly, we did not collect information on physical activity, which may affect the relationship between lipid and CVD morbidity and mortality. Thirdly, as lipid levels vary among different ethnicities, it could be cautious about generalizing the conclusion to other populations. Thus, a prospective cohort study with a larger sample size and more comprehensive baseline information is warranted to elucidate precise associations between lipid profiles and CVD and death.
Our findings suggested that the non-linear relationship between TC and CVD events, both lower and higher levels of TC, contributed to the increased risk of CVD. Higher ApoAI levels and lower ApoB levels were associated with the increased risk of CVD, while the lower level of TG was associated with the increased risk of all-cause death. Although the underlying mechanism had not been fully elucidated, maintaining optimal lipid levels would help to prevent CVD and reduce mortality.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Nanjing Medical University. The patients/participants provided their written informed consent to participate in this study.
JD, SY, and CS: conceived and designed the study. JD, QZ, JS, PW, XZ, YC, XC, ML, LW, CC, YF, and CS: data collection, analysis, and interpretation. JD: drafted the manuscript. XC, YF, and CS: revised the manuscript critically for intellectual content. All authors contributed to the article and approved the submitted version.
This work was supported by grants from the National Natural Science Foundation of China (Grant Nos. 81872686 and 81573232), Jiangsu Provincial Fourth 333 Project, the Priority Academic Program Development of Jiangsu Higher Education Institutions (Public Health and Preventive Medicine), and the Flagship Major Development of Jiangsu Higher Education Institutions. The Funders had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.745539/full#supplementary-material
1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
2. Liu S, Li Y, Zeng X, Wang H, Yin P, Wang L, et al. Burden of cardiovascular diseases in China, 1990-2016: findings from the 2016 Global Burden of Disease Study. JAMA Cardiol. (2019) 4:342–52. doi: 10.1001/jamacardio.2019.0295
3. Stamler J, Daviglus ML, Garside DB, Dyer AR, Greenland P, Neaton JD. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA. (2000) 284:311–8. doi: 10.1001/jama.284.3.311
4. Cui R, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, et al. Serum total cholesterol levels and risk of mortality from stroke and coronary heart disease in Japanese: the JACC study. Atherosclerosis. (2007) 194:415–20. doi: 10.1016/j.atherosclerosis.2006.08.022
5. Song PK, Man QQ, Li H, Pang SJ, Jia SS, Li YQ, et al. Trends in lipids level and dyslipidemia among Chinese adults, 2002-2015. Biomed Environ Sci. (2019) 32:559–70. doi: 10.3967/bes2019.074
6. Pan L, Yang Z, Wu Y, Yin RX, Liao Y, Wang J, et al. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis. (2016) 248:2–9. doi: 10.1016/j.atherosclerosis.2016.02.006
7. Sun L, Clarke R, Bennett D, Guo Y, Walters RG, Hill M, et al. Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat Med. (2019) 25:569–74. doi: 10.1038/s41591-019-0366-x
8. Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, et al. Association of lipids with ischemic and hemorrhagic stroke. Stroke. (2019) 50:3376–84. doi: 10.1161/STROKEAHA.119.026402
9. Curb JD, Abbott RD, Rodriguez BL, Masaki K, Popper J, Chen R, et al. Prospective association between low and high total and low-density lipoprotein cholesterol and coronary heart disease in elderly men. J Am Geriatr Soc. (2004) 52:1975–80. doi: 10.1111/j.1532-5415.2004.52551.x
10. Zhong GC, Huang SQ, Peng Y, Wan L, Wu YQ, Hu TY, et al. HDL-C is associated with mortality from all causes, cardiovascular disease and cancer in a J-shaped dose-response fashion: a pooled analysis of 37 prospective cohort studies. Euro J Prev Cardiol. (2020) 27:1187–203. doi: 10.1177/2047487320914756
11. Ingelsson E, Schaefer EJ, Contois JH, McNamara JR, Sullivan L, Keyes MJ, et al. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. (2007) 298:776–85. doi: 10.1001/jama.298.7.776
12. Welsh C, Celis-Morales CA, Brown R, Mackay DF, Lewsey J, Mark PB, et al. Comparison of conventional lipoprotein tests and apolipoproteins in the prediction of cardiovascular disease. Circulation. (2019) 140:542–52. doi: 10.1161/CIRCULATIONAHA.119.041149
13. Sierra-Johnson J, Fisher RM, Romero-Corral A, Somers VK, Lopez-Jimenez F, Ohrvik J, et al. Concentration of apolipoprotein B is comparable with the apolipoprotein B/apolipoprotein A-I ratio and better than routine clinical lipid measurements in predicting coronary heart disease mortality: findings from a multi-ethnic US population. Euro Heart J. (2009) 30:710–7. doi: 10.1093/eurheartj/ehn347
14. Walldius G, Jungner I. The apoB/apoA-I ratio: a strong, new risk factor for cardiovascular disease and a target for lipid-lowering therapy–a review of the evidence. J Intern Med. (2006) 259:493–519. doi: 10.1111/j.1365-2796.2006.01643.x
15. Yokokawa H, Yasumura S, Tanno K, Ohsawa M, Onoda T, Itai K, et al. Serum low-density lipoprotein to high-density lipoprotein ratio as a predictor of future acute myocardial infarction among men in a 2.7-year cohort study of a Japanese northern rural population. J Atheroscler Thromb. (2011) 18:89–98. doi: 10.5551/jat.5215
16. Taskinen MR, Barter PJ, Ehnholm C, Sullivan DR, Mann K, Simes J, et al. Ability of traditional lipid ratios and apolipoprotein ratios to predict cardiovascular risk in people with type 2 diabetes. Diabetologia. (2010) 53:1846–55. doi: 10.1007/s00125-010-1806-9
17. Wang W, Shen C, Zhao H, Tang W, Yang S, Li J, et al. A prospective study of the hypertriglyceridemic waist phenotype and risk of incident ischemic stroke in a Chinese rural population. Acta Neurol Scand. (2018) 138:156–62. doi: 10.1111/ane.12925
18. Chen J, Zhao X, Wang H, Chen Y, Wang W, Zhou W, et al. Common variants in TGFBR2 and miR-518 genes are associated with hypertension in the Chinese population. Am J Hypertens. (2014) 27:1268–76. doi: 10.1093/ajh/hpu047
19. Joint committee issued Chinese guideline for the management of dyslipidemia in adults. 2016 Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. (2016). 44:833–53. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005
20. Asia Pacific Cohort Studies Collaboration. Cholesterol, diabetes and major cardiovascular diseases in the Asia-Pacific region. Diabetologia. (2007) 50:2289–97. doi: 10.1007/s00125-007-0801-2
21. NCD Risk Factor Collaboration (NCD-RisC). Repositioning of the global epicentre of non-optimal cholesterol. Nature. (2020) 582:73–7. doi: 10.1038/s41586-020-2338-1
22. Luo J, Yang H, Song BL. Mechanisms and regulation of cholesterol homeostasis. Nat Rev Mol Cell Biol. (2020) 21:225–45. doi: 10.1038/s41580-019-0190-7
23. Miller VM, Duckles SP. Vascular actions of estrogens: functional implications. Pharmacol Rev. (2008) 60:210–41. doi: 10.1124/pr.107.08002
24. Baker L, Meldrum KK, Wang M, Sankula R, Vanam R, Raiesdana A, et al. The role of estrogen in cardiovascular disease. J Surg Res. (2003) 115:325–44. doi: 10.1016/S0022-4804(03)00215-4
25. Zhao D, Guallar E, Ouyang P, Subramanya V, Vaidya D, Ndumele CE, et al. Endogenous sex hormones and incident cardiovascular disease in post-menopausal women. J Am Coll Cardiol. (2018) 71:2555–66. doi: 10.1016/j.jacc.2018.01.083
26. Kosmas CE, Silverio D, Sourlas A, Garcia F, Montan PD, Guzman E. Primary genetic disorders affecting high density lipoprotein (HDL). Drugs Context. (2018) 7:212546. doi: 10.7573/dic.212546
27. Umemoto T, Han CY, Mitra P, Averill MM, Tang C, Goodspeed L, et al. Apolipoprotein AI and high-density lipoprotein have anti-inflammatory effects on adipocytes via cholesterol transporters: ATP-binding cassette A-1, ATP-binding cassette G-1, and scavenger receptor B-1. Circul Res. (2013) 112:1345–54. doi: 10.1161/CIRCRESAHA.111.300581
28. Holme I, Aastveit AH, Hammar N, Jungner I, Walldius G. Inflammatory markers, lipoprotein components and risk of major cardiovascular events in 65,005 men and women in the Apolipoprotein MOrtality RISk study (AMORIS). Atherosclerosis. (2010) 213:299–305. doi: 10.1016/j.atherosclerosis.2010.08.049
29. Elovson J, Chatterton JE, Bell GT, Schumaker VN, Reuben MA, Puppione DL, et al. Plasma very low density lipoproteins contain a single molecule of apolipoprotein B. J Lipid Res. (1988) 29:1461–73. doi: 10.1016/S0022-2275(20)38425-X
30. Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. (2007) 298:299–308. doi: 10.1001/jama.298.3.299
31. Liu J, Zeng FF, Liu ZM, Zhang CX, Ling WH, Chen YM. Effects of blood triglycerides on cardiovascular and all-cause mortality: a systematic review and meta-analysis of 61 prospective studies. Lipids Health Dis. (2013) 12:159. doi: 10.1186/1476-511X-12-159
32. Xia TL, Li YM, Huang FY, Chai H, Huang BT, Li Q, et al. The triglyceride paradox in the mortality of coronary artery disease. Lipids Health Dis. (2019) 18:21. doi: 10.1186/s12944-019-0972-0
33. Jain M, Jain A, Yerragondu N, Brown RD, Rabinstein A, Jahromi BS, et al. The triglyceride paradox in stroke survivors: a prospective study. Neurosci J. (2013) 2013:870608. doi: 10.1155/2013/870608
34. Ford ES, Li C, Zhao G, Pearson WS, Mokdad AH. Hypertriglyceridemia and its pharmacologic treatment among US adults. Arch Internal Med. (2009) 169:572–8. doi: 10.1001/archinternmed.2008.599
35. Hastie CE, Padmanabhan S, Slack R, Pell AC, Oldroyd KG, Flapan AD, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Euro Heart J. (2010) 31:222–6. doi: 10.1093/eurheartj/ehp317
36. Eryürek FG, Sürmen E, Oner P, Altug T, Oz H. Gamma-glutamyl transpeptidase and acetylcholinesterase activities in brain capillaries of cholesterol-fed rabbits. Res Commun Chem Pathol Pharmacol. (1990) 69:245–8.
Keywords: lipids, apolipoprotein, derived lipid indices, cardiovascular diseases, death, cohort study
Citation: Dong J, Yang S, Zhuang Q, Sun J, Wei P, Zhao X, Chen Y, Chen X, Li M, Wei L, Chen C, Fan Y and Shen C (2021) The Associations of Lipid Profiles With Cardiovascular Diseases and Death in a 10-Year Prospective Cohort Study. Front. Cardiovasc. Med. 8:745539. doi: 10.3389/fcvm.2021.745539
Received: 22 July 2021; Accepted: 25 October 2021;
Published: 25 November 2021.
Edited by:
Vasily Sukhorukov, Research Institute of Human Morphology, RussiaReviewed by:
Mengling Tang, Zhejiang University, ChinaCopyright © 2021 Dong, Yang, Zhuang, Sun, Wei, Zhao, Chen, Chen, Li, Wei, Chen, Fan and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chong Shen, c2NAbmptdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.