- 1Department of Cardiovascular Medicine, The Second Xiangya Hospital, Central South University, Changsha, China
- 2Department of Emergency Medicine, Second Xiangya Hospital, Central South University, Changsha, China
- 3Emergency Medicine and Difficult Diseases Institute, Central South University, Changsha, China
Objective: Patients with well-developed coronary collateral circulation (CC) usually have low mortality, improved cardiac function, and reduced infarct size. Currently, there is conflicting evidence on the association between traditional cardiovascular risk factors (diabetes, hypertension, and smoking habit) and CC.
Design: We performed a meta-analysis of case-control studies to better understand such associations.
Data Sources: We searched the MEDINE, EMBASE, and Science Citation Index databases to identify relevant studies.
Eligibility Criteria for Selecting Studies: Case control studies reporting data on risk factors (smoking habit, hypertension, and diabetes mellites) in comparing cases between poor CC and well-developed CC groups. Well-developed CC was the primary outcome of this meta-analysis
Data Extraction and Synthesis: Relevant data were extracted by two independent investigators. We derived pooled odds ratios (ORs) with random effects models. We performed quality assessments, publication bias, and sensitivity analysis to ensure the reliability of our results.
Results: In total, 18 studies that had 4,746 enrolled patients were analyzed. Our results showed that hypertension and smoking habit did not (OR = 0.94, 95% CI: 0.75–1.17, p = 0.564 and OR = 1.00, 95% CI: 0.84–1.18, p = 0.970, respectively), and diabetes did (OR = 0.50, 95% CI: 0.38–0.67, p = 0.00001) affect the development of CC.
Conclusion: Unlike hypertension and smoking habit, diabetes was associated with poor CC formation.
Trial Registration Number: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=87821, identifier: CRD42018087821.
Strengths and Limitations of This Study
-This is the largest meta-analysis to study the relationship between traditional risk factors and coronary collateral circulation.
-In order to give a solid conclusion, sensitivity and subgroup analyses were performed.
-Along with real operators/equipment, the definition/identification of the presence or absence of coronary collaterals can vary between different studies.
Background
Traditional cardiovascular risk factors, including diabetes mellitus, smoking habit, and hypertension are associated with increased cardiovascular morbidity and mortality. These risk factors are predictors of poor clinical outcomes in patients with myocardial infarction, stroke, and peripheral artery diseases (1–3). Collateral circulation (CC) is beneficial in reducing cardiac ischemia and infarction in cases of chronic stenosis or acute occlusion. Well-developed coronary CC is associated with improved cardiac function and decreased instances of cardiac mortality (4, 5). Coronary collaterals are arterio-arterial anastomoses that develop neonatally and are present at birth (6). These anastomoses can remodel into arteries up to 20-fold larger in diameter than the original arterioles when a coronary artery is occluded. However, many acquired factors affect its arterial remodeling, which ultimately manifests as differences in the quality of collateral circulation in patients. Despite these beneficial effects, a large proportion of patients lack well-developed CC. Furthermore, an effective treatment to promote coronary CC has thus far been limited to humans (7). A number of studies have demonstrated that traditional cardiovascular risk factors can impair the remodeling of CC. Moore et al. found that traditional cardiovascular risk factors were associated with the premature rarefaction of the coronary CC, leading to greater cardiac ischemia (8). However, in comparison to the findings of Moore et al., some researchers have reported nearly opposite results (9, 10). The number of collateral circulation is also related to the degree of coronary artery obstruction. Given the conflicting evidence of the association between traditional cardiovascular risk factors (e.g., smoking habit, hypertension, and diabetes mellitus) and coronary collaterals, we performed a meta-analysis of case-control studies to better understand such relationships in patients with coronary artery chronic total occlusion. This is the largest meta-analysis to study the relationship between traditional risk factors and CC.
Method
This meta-analysis is presented in accordance with the Preferred Reporting Items for System Reviews and Meta-Analyses (PRISMA) Statement and has been registered with the International Prospective Register of Systematic Reviews (CRD42018087821) (11). The protocol of this meta-analysis has been described previously (12).
Search Strategies
We searched the MEDLINE, EMBASE, and Web of Science databases to identify relevant studies published from inception of those databases to January 1, 2021. We used the “coronary collaterals” as the key words, “collateral circulation” as the MeSH terms to identify relevant studies.
Studies
Studies were included in our analyses if (1) they reported the extent of coronary CC, describing it as well-developed or poorly developed; (2) they reported data on risk factors (smoking habit, hypertension, and diabetes mellites) in comparing cases between poor CC and well-developed CC groups; (3) they were case-control studies; and (4) they contained sufficient information (for instance, the sample size of each group, the number of smokers in different groups, etc.). Studies were excluded if (1) they reported only the p-values of the data of interest without any numerical values in each group; (2) they were not published in English peer-reviewed journals; and/or (3) they presented data that were previously published.
Exposure Factors and Grades of CC
Traditional coronary risk factors (smoking habit, diabetes mellitus, and hypertension) were defined as exposure factors. We used the Rentrop scoring system to grade CC (13). A Rentrop score of 2 or 3 was defined as well-developed CC, while a Rentrop score of 0 or 1 was classified as poor CC.
Data Selection
Data selection was conducted independently (JY Pei and XP Wang).
Disagreements were resolved through discussion with all authors or by consulting a third author (ZH Xing). We selected the following data from the included articles: study characteristics (e.g., first author, publication date), the characteristics of included participants (e.g., age, sex, smoking habit, diabetes, and hypertension), the definition of coronary CC, and the risk factors of coronary CC. We used the Review manager and Stata to organize included articles and data.
If quantitative analysis was not appropriate, we performed a narrative, qualitative summary. Results are presented both in the text and in tables.
Newcastle-Ottawa Scale
We assessed the methodological quality of the included studies by the Newcastle-Ottawa Scale. A maximum of two stars could be given for comparability measurements. A star system of the scale (range, 0–9) was used in the current study.
Statistical Analysis
The relationship between cardiovascular risk factors (hypertension, diabetes, and smoking habit) and CC in patients with chronic coronary occlusion was expressed in terms of the odds ratio (OR) and its 95% confidence interval (CI). An OR >1 indicated that the studied factors were positively correlated with the formation of CC, while an OR <1 indicated that the studied factors were negatively correlated with the formation of CC. P-values < 0.05 were considered statistically significant. Heterogeneity was assessed by the Cochran Q-test, and statistical heterogeneity was summarized by the I2, which quantifies the percent of variation in study results that is because of heterogeneity rather than to chance. When I2 was <25%, the heterogeneity was small, and a fixed-effect model will be used. When I2 ≥ 25%, the included studies were considered to have moderate heterogeneity, the I2 ≥ 50%, there is a significant heterogeneity (14). When the moderate or significant heterogeneity was found, the random-effects model will be used. Accordingly, a sensitivity analysis was also conducted to verify whether the effect was stable. Random-effects and fixed-effect models were used to calculate the respective effect, and whether the observed result was affected by the statistical method; each study was excluded, and the effect of the remaining studies was recalculated to determine whether the observed results were affected by any individual study. The Begg and Egger methods were used to verify whether there was publication bias.
Results
Included Studies
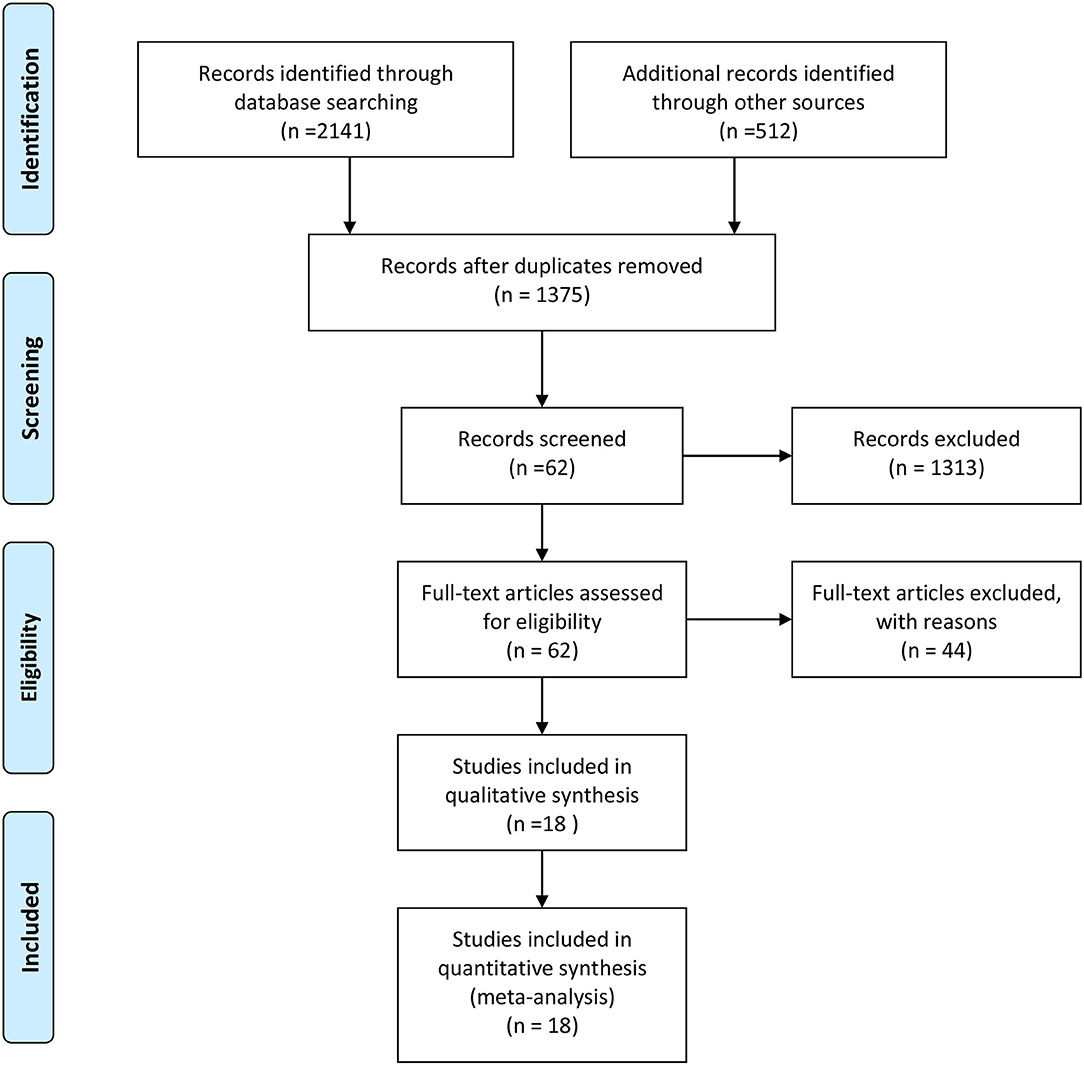
An outline of the screening process is shown in Figure 1. A total of 2,653 documents were identified manually by searching the MEDLINE, Embase, and Web of Science databases, as well as other sources. After the removal of duplicates, 1,375 articles were retained. Subsequently, after screening the titles and abstracts of the literature, 1,313 studies were excluded. Thus, a total of 62 relevant articles were identified. Finally, after reading the full text, 44 articles were excluded [3 non-English articles, 33 non-coronary chronic total occlusions (CTO), 3 similar articles by the same author, and 5 unrelated research], and 18 articles were included for further analyses.
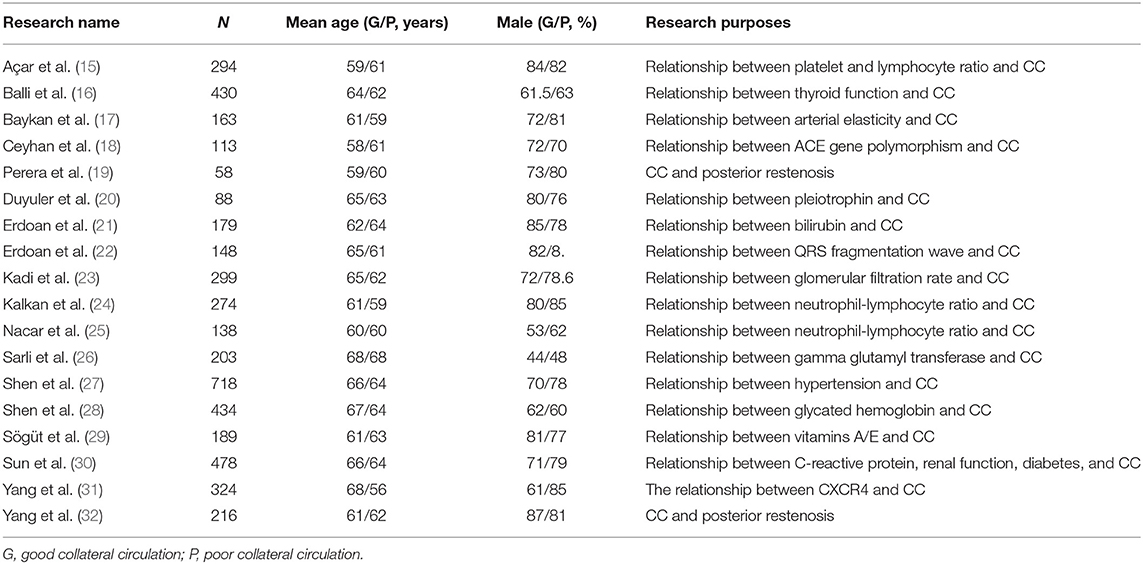
A total of 4,746 CTO patients were enrolled in the selected studies, including 2,928 (61.7%) patients with hypertension, 1907 (40.2%) patients with diabetes, and 2,146 (45.2%) patients with a history of smoking. Most of these studies were cross-sectional studies that study the relationship between blood biochemical indicators and coronary collateral circulation. These biochemical indicators have been shown to be related to the severity of cardiovascular disease in previous studies. In most studies, male patients accounted for the majority. This might be because the formation of coronary collateral circulation was related to the severity of coronary atherosclerosis, and male patients usually have more severe symptoms than female patients (Table 1). The baseline patient's characteristics was shown in Table 2.
Newcastle-Ottawa Scale
The Newcastle-Ottawa Scale was used to evaluate the quality of the included studies. Each of the included studies had a score above seven points, and thus, all these studies were included in our analyses.
Outcomes
Hypertension and CC
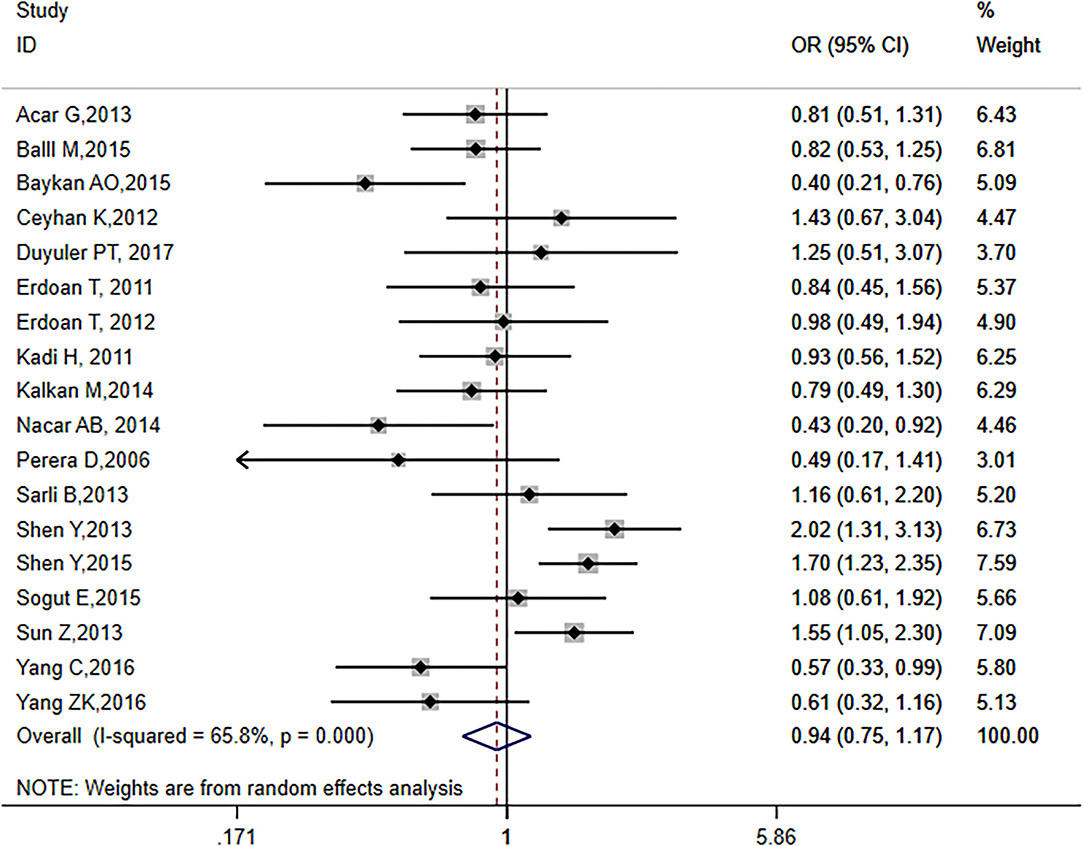
The analysis included 18 articles, representing a total of 4,746 patients, including 2,928 hypertensive patients. The I2 score was 65.8% (p = 0.0001), indicating that the included literature was heterogeneous, thus requiring a random-effects model (OR = 0.94, 95% CI: 0.75–1.17, p = 0.564; Figure 2). The effect value was close to 1, suggesting that hypertension had no effect on the formation of CC in CTO patients.
Diabetes and CC
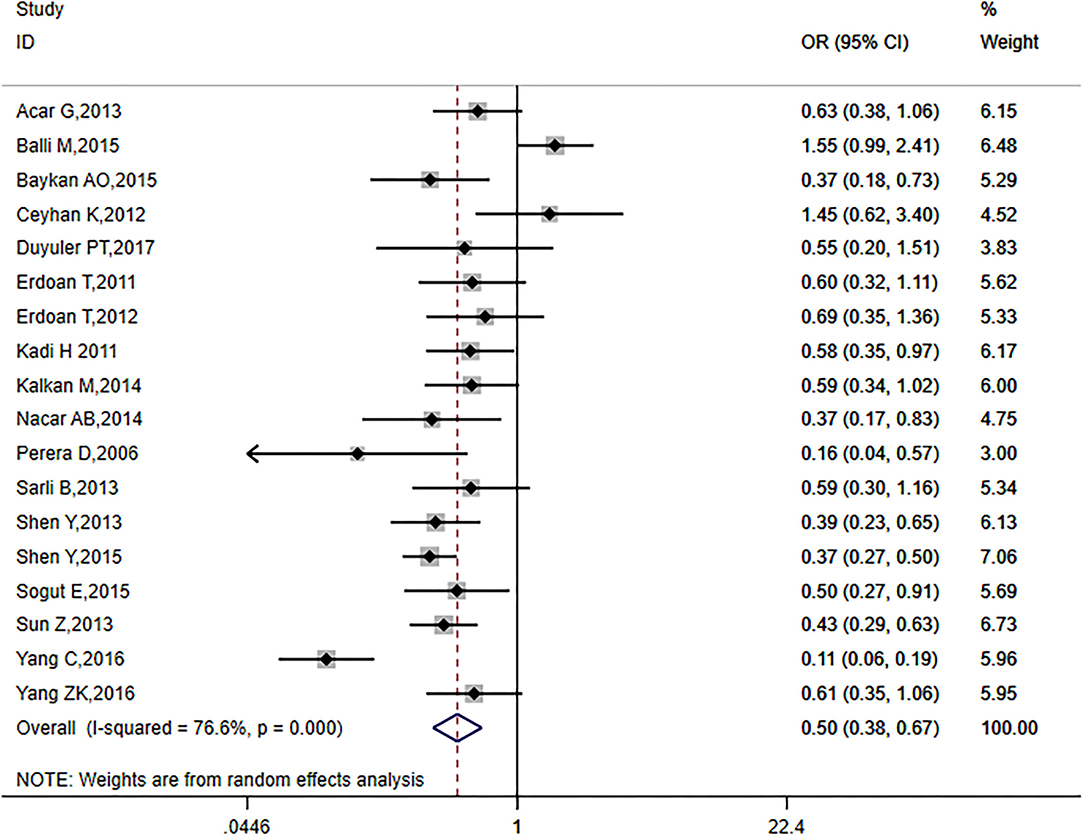
The analysis included 18 articles with a total of 4,746 patients, including 1907 (40.2%) diabetic patients. I2 = 76.6% (p = 0.0001) indicated that the included literature was heterogeneous; thus, requiring a random-effects model (OR = 0.50, 95% CI: 0.38–0.67, p = 0.00001; Figure 3). These results suggest that CC formation was inhibited in patients with diabetes mellitus.
Smoking Habit and CC
The analysis included 18 articles with a total of 4,746 patients, including 2,146 (45.2%) patients with a history of smoking. I2 = 40.4% (p = 0.06) indicated that the included literature showed significant heterogeneity. Therefore, a random-effects model was used (OR = 1.00, 95% CI: 0.84–1.18, p = 0.970; Figure 4). These results suggest that smoking habit did not affect the formation of CC in CTO patients.
Sensitivity Analysis and Publishing Bias
The use of a fixed-effect model showed that the statistical methods did not influence the observed results (Hypertension and CC: OR = 1.03, 95% CI: 0.91–1.16, Supplementary Figure 1), (Diabetes and CC: OR = 0.49, 95% CI: 0.43–0.56, p = 0.0001, Supplementary Figure 2), (Smoking habit and CC: OR = 1.01, 95% CI: 0.89–1.14, Supplementary Figure 3). Subsequently, each study was excluded, and the effect of the remaining studies was recalculated to determine whether the observed results were affected by any individual study. No study was found to alter the effect size.
The Begg and Egger methods were used to test publication bias. No publication bias was observed for hypertension (p = 0.225, Begg method; p = 0.142, Egger method), diabetes (p = 0.695, Begg method; p = 0.663, Egger method), and smoking habit (p = 0.596, Begg method; p = 0.996, Egger method).
Discussion
This is the largest meta-analysis to study the relationship between traditional risk factors and CC, which included 18 case-control studies that had 4,746 CTO patients. No association was found between hypertension or smoking habit and CC in patients with CTO. However, CC was found to be inhibited in diabetic patients.
In the 1970s, the measurement of functional collaterals of coronary arteries in vivo was performed for the first time, showing the “direct relationship between the appearance and functional performance of coronary collaterals in bypass surgery (33).” Rentrop et al. proposed a method of intracoronary angiography to divide the coronary collateral circulation into four levels, which we used in this research (13). But this method still has certain limitations. This method was a qualitative judgment method, and it was not suitable for epicardial collaterals. In recent years, a quantitative assessment method of coronary collateral function based on the measurement of coronary occlusion pressure has emerge, which called the collateral flow index (CFI) (34, 35). This method can be used as a reference method for evaluating functional collaterals in patients with chronic stable coronary heart disease (36, 37). It has been confirmed that CFI >0.20–0.25 was related to the absence of signs of ischemia on the intra-coronary electrocardiogram during 1 min of coronary balloon occlusion (38, 39).
One characteristic of hypertension is an increase in the stiffness of blood vessels. This stiffness may increase the sheer force of the bloodstream to the collaterals. The increase in shear force is likely to increase the activity of endothelial nitric oxide synthase (eNOS), leading to an increase in nitric oxide (NO) synthesis (40). However, hypertension is associated with vascular dysfunction (i.e., decreased vascular compliance). In patients with hypertension, angiotensin II can inhibit angiogenesis, but can also enhance NAD (P) H oxidase activity, leading to increased vascular wall reactive oxygen species and superoxide. This then leads to the uncoupling of eNOS, which inhibits the synthesis of NO, resulting in vascular endothelial dysfunction. At the cellular level, the relationship between hypertension and CC may be more complicated, both promoting and inhibiting the formation of CC. Thus, the relationship between hypertension and CC can be complicated—promoting and inhibiting the formation of CC (41). There are a few observational clinical studies on the association between hypertension and CC, but these studies have produced varied conclusions (40, 42).
Diabetes is a relatively important risk factor for coronary heart disease, and it can lead to poor short-term and long-term cardiovascular outcomes (43). Abaci et al. studied 205 diabetic patients with severe coronary artery stenosis and found that coronary artery CC was poorly formed in these patients than in non-diabetic patients with severe coronary artery stenosis (44). Subsequent studies have also found that patients with diabetes exhibited poor CC formation (45). However, in sharp contrast to the above studies, several studies have drawn completely opposite conclusions (46). Similar to the findings of studies that examined patients with hypertension, there was a considerable heterogeneity among patients enrolled in these studies. Diabetes may lead to severe coronary lesions, which may aggravate tissue ischemia and promote CC formation. In the current study, only patients who were diagnosed with CTO were included, thus avoiding differences in the results of the relevant studies due to differences in the degree of vascular stenosis. CC in patients with diabetes and CTO can be related to various clinical, biochemical, and angiographic factors. It involves multiple mechanisms, such as an increase in the serum levels of glycated albumin, cystatin C, and adipokine C1q tumor necrosis factor related protein 1 (47).
Revascularization of patients with chronic complete coronary occlusion can significantly improve the patient's left ventricular function and reduce the risk of cardiovascular events (48) and current evidence favors coronary artery bypass grafting as the preferred revascularization modality for type 2 diabetic patients with multivessel coronary disease, which is likely to reflect the more complete revascularization and global protection provided by arterial conduits against rapid atherosclerosis progression in PCI and untreated segment (49, 50). Jane et al. found that after revascularization of CTO patients, patients with better collateral circulation have a lower risk of cardiovascular events (51). Recent studies have found that PCI can reduce the risk of cardiovascular events and improve the survival rate of non-diabetic CTO patients, but it has no obvious effect on CTO patients with diabetes (52). However, some clinical studies have found that vascular recanalization can indeed improve the survival rate of CTO patients with diabetes (53). Therefore, whether revascularization should be performed on CTO patients should not only rely on clinical symptoms, but also comprehensively consider the patient's vascular conditions, of which the quality of collateral circulation is a very important factor.
Moreover, tobacco consumption may both promote and inhibit the formation of CC. Heeschen et al. found that nicotine promoted the adhesion of monocytes to endothelial cells and thus, may promote the development of CC (54). However, a long history of smoking can lead to endothelial dysfunction and impaired monocyte migration. Such impaired endothelial function and the dysfunction of inflammatory cells caused by cigarette consumption can inhibit the positive remodeling of CC to some extent.
Limitation
The current study has a few limitations. First, this is a meta-analysis of observational studies, and thus, it was not possible to consider all confounding factors between groups with and without good CC formation, which may affect the evaluation of our results. There are many factors that can affect the formation of coronary collateral circulation, such as age, weight, ethnicity, body mass index or cholesterol level. The data obtained from the original study can only show the average age or average weight of all patients. As far as we know, we cannot adjust in statistical methods based on these data, so we did not adjust age and weight in the statistical process. As for race, because most of the included studies are single-center case-control studies, the original article did not provide exact race data, these may have some influence on the results. Additionally, along with real operators/equipment, the definition/identification of the presence or absence of coronary collaterals can vary between different studies, and therefore, such differences can affect the quality assessment of CC. And we used the Rentrop scores to evaluate the quality of CC, not the CFI, because Rentrop scores was used in most studies. We were unable to obtain relevant data from these original studies, so we did not perform the inter and intra-observer variability analyses. The OR value of hypertension and smoking habit was 0.92 and 1.01, respectively. The effect values and 95% CI of these two variables were very close to 1. However, the effect values and 95% CI for diabetes was close to 0.5. Even if there were confounding factors that may have affected the outcome measures, they are unlikely to overturn the observed results of this study since our meta-analysis incorporated a large population base, and subgroup/sensitivity analyses were used to verify the reliability of our conclusions. Since the included studies were all case-control studies, data of patient's hypertension stage cannot be collected from the original article, so we cannot perform the analysis of the impact of hypertension stage and collateralization. As well for diabetes, data of patient's hypertension stage cannot be collected from the original article, we cannot perform the analysis of the HbA1c and collateralization status in diabetics either. Second, despite a detailed search of different databases, some studies could have been missed during the initial search. Finally, the bulk of the studies included in our meta-analysis was performed in China and Turkey, which may limit the generalizability of our results in other (European, American, and African) populations.
Conclusion
This meta-analysis found that hypertension and smoking habit were not associated with CC formation. However, diabetes was associated with poor CC formation.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
ZX designed the study and provided methodological expertise. JP and XW data selection was conducted independently and relevant studies were searched by 2 independent investigators. JP and ZX drafted the manuscript. All authors have read, provided critical feedback on, and approved the final manuscript.
Funding
This work was supported in part by National Science Foundation of China Project No. 82000298 and Natural Science Foundation of Hunan Province 2021JJ40883 to ZX.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.743234/full#supplementary-material
References
1. Chin CT, Chen AY, Wang TY, Alexander KP, Mathews R, Rumsfeld JS, et al. Risk adjustment for in-hospital mortality of contemporary patients with acute myocardial infarction: the acute coronary treatment and intervention outcomes network (ACTION) registry-get with the guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. (2011) 161:113–22e2. doi: 10.1016/j.ahj.2010.10.004
2. Koennecke HC, Belz W, Berfelde D, Endres M, Fitzek S, Hamilton F, et al. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology. (2011) 77:965–72. doi: 10.1212/WNL.0b013e31822dc795
3. Virkkunen J, Heikkinen M, Lepäntalo M, Metsänoja R, Salenius JP. Diabetes as an independent risk factor for early postoperative complications in critical limb ischemia J Vasc Surg. (2004) 40:761–7. doi: 10.1016/j.jvs.2004.07.040
4. Helfant RH, Vokonas PS, Gorlin R. Functional importance of the human coronary collateral circulation. N Engl J Med. (1971) 284:1277–81. doi: 10.1056/NEJM197106102842301
5. Cui K, Lyu S, Song X, Yuan F, Xu F, Zhang M, et al. Effect of coronary collaterals on prognosis in patients undergoing primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: a meta-analysis. Angiology. (2018) 69:803–11. doi: 10.1177/0003319718768399
6. Zimarino M, D'andreamatteo M, Waksman R, Epstein SE, De Caterina R. The dynamics of the coronary collateral circulation. Nat Rev Cardiol. (2014) 11:191–7 doi: 10.1038/nrcardio.2013.207
7. Lin S, Chen Y, Li Y, Li J, Lu X. Physical ischaemia induced by isometric exercise facilitated collateral development in the remote ischaemic myocardium of humans. Clin Sci (Lond). (2014) 127:581–8. doi: 10.1042/CS20130618
8. Moore SM, Zhang H, Maeda N, Doerschuk CM, Faber JE. Cardiovascular risk factors cause premature rarefaction of the collateral circulation and greater ischemic tissue injury. Angiogenesis. (2015) 18:265–81. doi: 10.1007/s10456-015-9465-6
9. Bhatt H, Kochar S, Htun WW, Julliard K, Fernaine G. Coronary collateral circulation and cardiovascular risk factors: is there a paradox? Angiology. (2015) 66:588–94. doi: 10.1177/0003319714545342
10. Heeschen C, Weis M, Cooke JP. Nicotine promotes arteriogenesis. J Am Coll Cardiol. (2003) 41:489–96. doi: 10.1016/S0735-1097(02)02818-8
11. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. (2015) 350:g7647. doi: 10.1136/bmj.g7647
12. Xing Z, Pei J, Tang L, Hu X. Traditional cardiovascular risk factors and coronary collateral circulation: protocol for a systematic review and meta-analysis of case-control studies. Medicine (Baltimore). (2018) 97:e0417. doi: 10.1097/MD.0000000000010417
13. Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol. (1985) 5:587–92. doi: 10.1016/S0735-1097(85)80380-6
14. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
15. Açar G, Kalkan ME, Avci A, Alizade E, Tabakci MM, Toprak C, et al. The relation of platelet-lymphocyte ratio and coronary collateral circulation in patients with stable angina pectoris and chronic total occlusion. Clin Appl Thromb Hemost. (2015) 21:462–8. doi: 10.1177/1076029613508599
16. Balli M, Çetin M, Tasolar H, Uysal OK, Yilmaz M, Durukan M, et al. The relationship between serum thyroid hormone levels, subclinical hypothyroidism, and coronary collateral circulation in patients with stable coronary artery disease. Turk Kardiyol Dern Ars. (2016) 44:130–6. doi: 10.5543/tkda.2015.00905
17. Baykan AO, Gür M, Acele A, Seker T, Quisi A, Yildirim A, et al. Coronary collateral development and arterial stiffness in patients with chronic coronary total occlusions. Scand Cardiovasc J. (2015) 49:228–34. (2015). doi: 10.3109/14017431.2015.1062130
18. Ceyhan K, Kadi H, Celik A, Burucu T, Koc F, Sogut E, et al. Angiotensin-converting enzyme DD polymorphism is associated with poor coronary collateral circulation in patients with coronary artery disease. J Investig Med. (2012) 60:49–55. doi: 10.2310/JIM.0b013e31823908e2
19. Perera D, Postema P, Rashid R, Patel S, Blows L, Marber M, et al. Does a well-developed collateral circulation predispose to restenosis after percutaneous coronary intervention? An intravascular ultrasound study. Heart. (2006) 92:763–67. doi: 10.1136/hrt.2005.067322
20. Türker Duyuler P, Duyuler S, Gök M, Kundi H, Topçuoglu C, Güray Ü. Pleiotrophin levels are associated with improved coronary collateral circulation. Coron Artery Dis. (2018) 29:68–73. doi: 10.1097/MCA.0000000000000556
21. Erdogan T, Çiçek Y, Kocaman SA, Çanga A, Çetin M, Durakoglugil E et al. Increased serum bilirubin level is related to good collateral development in patients with chronic total coronary occlusion. Intern Med. (2012) 51:249–55. doi: 10.2169/internalmedicine.51.6417
22. Erdogan T, Kocaman SA, Çetin M, Çanga A, Durakoglugil ME, Çiçek Y, et al. Relationship of fragmented QRS complexes with inadequate coronary collaterals in patients with chronic total occlusion. J Cardiovasc Med. 13:499–504. (2012). doi: 10.2459/JCM.0b013e328353683c
23. Kadi H, Ceyhan K, Sogut E, Koc F, Celik A, Onalan O et al. Mildly decreased glomerular filtration rate is associated with poor coronary collateral circulation in patients with coronary artery disease. Clin Cardiol. (2011) 34, 617–21. doi: 10.1002/clc.20951
24. Kalkan ME, Sahin M, Kalkan AK, Güler A, Taş MH, Bulut M, et al. The relationship between the neutrophil-lymphocyte ratio and the coronary collateral circulation in patients with chronic total occlusion. Perfusion. (2014) 29:360–6. doi: 10.1177/0267659114521102
25. Nacar AB, Erayman A, Kurt M, Buyukkaya E, Karakaş MF, Akcay AB, et al. The relationship between coronary collateral circulation and neutrophil/lymphocyte ratio in patients with coronary chronic total occlusion. Med Princ Pract. (2015) 24:65–9. doi: 10.1159/000365734
26. Sarli B, Baktir AO, Saglam H, Arinc H, Kurtul S, Akpek M, et al. The relation of serum γ-glutamyl transferase levels and coronary collateral circulation in patients with chronic coronary total occlusion. Coron Artery Dis. (2013) 24:298–302. doi: 10.1097/MCA.0b013e32835f301d
27. Shen Y, Ding FH, Wu F, Lu L, Zhang RY, Zhang Q, et al. Association of blood pressure and coronary collateralization in type 2 diabetic and nondiabetic patients with stable angina and chronic total occlusion. J Hypertens. (2015) 33:621–6. doi: 10.1097/HJH.0000000000000455
28. Shen Y, Ding FH, Wu F, Lu L, Zhang RY, Zhang Q, et al. Association of increased serum glycated albumin levels with low coronary collateralization in type 2 diabetic patients with stable angina and chronic total occlusion. Cardiovasc Diabetol. (2013) 12:165. doi: 10.1186/1475-2840-12-165
29. Sögüt E, Kadi H, Karayakali M, Mertoglu C. The association of plasma vitamin A and E levels with coronary collateral circulation. Atherosclerosis. (2015) 239:547–51. doi: 10.1016/j.atherosclerosis.2015.02.029
30. Sun Z, Shen Y, Lu L, Zhang RY, Pu LJ, Zhang Q, et al. Clinical and angiographic features associated with coronary collateralization in stable angina patients with chronic total occlusion. J Zhejiang Univ Sci B. (2013) 14:705–12. doi: 10.1631/jzus.BQICC704
31. Yang C, Zhu W, Han X, Ma A, Bai L, Xu F. Association of CXCR4 expression with coronary collateralization in patients with chronic total coronary occlusion: a nested case-control study. Int J Cardiol. (2017) 228:501–6. doi: 10.1016/j.ijcard.2016.11.068
32. Yang ZK, Shen Y, Hu J, Zhang Q, Ding FH, Zhang RY, et al. Impact of coronary collateral circulation on angiographic in-stent restenosis in patients with stable coronary artery disease and chronic total occlusion. Int J Cardiol. (2017) 227:485–9. doi: 10.1016/j.ijcard.2016.10.117
33. Goldstein RE, Stinson EB, Scherer JL, Seningen RP, Grehl TM, Epstein SE. Intraoperative coronary collateral function in patients with coronary occlusive disease nitroglycerin responsiveness and angiographic correlations. Circulation. (1974) 49:298–308. doi: 10.1161/01.CIR.49.2.298
34. Seiler C, Fleisch M, Garachemani A, Meier B. Coronary collateral quantitation in patients with coronary artery disease using intravascular flow velocity or pressure measurements. J Am Coll Cardiol. (1998) 32:1272–9. doi: 10.1016/S0735-1097(98)00384-2
35. Pijls NH, van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation. (1993) 87:1354–67. doi: 10.1161/01.CIR.87.4.1354
36. Matsuo H, Watanabe S, Kadosaki T, Yamaki T, Tanaka S, Miyata S, et al. Validation of collateral fractional flow reserve by myocardial perfusion imaging. Circulation. (2002) 105:1060–5. doi: 10.1161/hc0902.104719
37. Vogel R, Zbinden R, Indermühle A, Windecker S, Meier B, Seiler C. Collateral-flow measurements in humans by myocardial contrast echocardiography: validation of coronary pressure-derived collateral-flow assessment. Eur Heart J. (2006) 27:157–65. doi: 10.1093/eurheartj/ehi585
38. de Marchi SF, Streuli S, Haefeli P, Gloekler S, Traupe T, Warncke C, et al. Determinants of prognostically relevant intracoronary electrocardiogram ST-segment shift during coronary balloon occlusion. Am J Cardiol. (2012) 110:1234–9. doi: 10.1016/j.amjcard.2012.06.023
39. Traupe T, Gloekler S, de Marchi SF, Werner GS, Seiler C. Assessment of the human coronary collateral circulation. Circulation. (2010) 122:1210–20. doi: 10.1161/CIRCULATIONAHA.109.930651
40. Benndorf R, Böger RH, Ergün S, Steenpass A, Wieland T. Angiotensin II type 2 receptor inhibits vascular endothelial growth factor-induced migration and in vitro tube formation of human endothelial cells. Circ Res. (2003) 93:438–47. doi: 10.1161/01.RES.0000088358.99466.04
41. Meier P, Schirmer SH, Lansky AJ, Timmis A, Pitt B, Seiler C. The collateral circulation of the heart. BMC Med. (2013) 11:143. doi: 10.1186/1741-7015-11-143
42. Kyriakides ZS, Kremastinos DT, Michelakakis NA, Matsakas EP, Demovelis T, Toutouzas PK. Coronary collateral circulation in coronary artery disease and systemic hypertension. Am J Cardiol. (1991) 67:687–90. doi: 10.1016/0002-9149(91)90522-M
43. Haffner SM. Coronary heart disease in patients with diabetes. N Engl J Med. (2000) 342:1040–2. doi: 10.1056/NEJM200004063421408
44. Abaci A, Oguzhan A, Kahraman S, Eryol NK, Unal S, Arinç H, et al. Effect of diabetes mellitus on formation of coronary collateral vessels. Circulation. (1999) 99:2239–42. doi: 10.1161/01.CIR.99.17.2239
45. Mouquet F, Cuilleret F, Susen S, Sautiere K, Marboeuf P, Ennezat PV. Metabolic syndrome and collateral vessel formation in patients with documented occluded coronary arteries: association with hyperglycaemia, insulin-resistance, adiponectin and plasminogen activator inhibitor-1. Eur Heart J. (2009) 30:840–9. doi: 10.1093/eurheartj/ehn569
46. Niccoli G, Giubilato S, Di Vito L, Leo A, Cosentino N, Pitocco D, et al. Severity of coronary atherosclerosis in patients with a first acute coronary event: a diabetes paradox. Eur Heart J. (2013) 34:729–41. doi: 10.1093/eurheartj/ehs393
47. Shen Y, Ding FH, Dai Y, Wang XQ, Zhang RY, Lu L, et al. Reduced coronary collateralization in type 2 diabetic patients with chronic total occlusion. Cardiovasc Diabetol. (2018) 17:26. doi: 10.1186/s12933-018-0671-6
48. Khan MF, Wendel CS, Thai HM, Movahed MR. Effects of percutaneous revascularization of chronic total occlusions on clinical outcomes: a meta-analysis comparing successful versus failed percutaneous intervention for chronic total occlusion. Catheter Cardiovasc Interv. (2013) 82:95–107. doi: 10.1002/ccd.24863
49. Kennedy MW, Fabris E, Suryapranata H, Kedhi E. Is ischemia the only factor predicting cardiovascular outcomes in all diabetes mellitus patients. Cardiovasc Diabetol. (2017) 16:51. doi: 10.1186/s12933-017-0533-7
50. Bundhun PK, Wu ZJ, Chen MH. Coronary artery bypass surgery compared with percutaneous coronary interventions in patients with insulin-treated type 2 diabetes mellitus: a systematic review and meta-analysis of 6 randomized controlled trials. Cardiovasc Diabetol. (2016) 15:2. doi: 10.1186/s12933-015-0323-z
51. Jang WJ, Yang JH, Choi SH, Song YB, Hahn JY, Choi JH, et al. Long-term survival benefit of revascularization compared with medical therapy in patients with coronary chronic total occlusion and well-developed collateral circulation. JACC Cardiovasc Interv. (2015) 8:271–9. doi: 10.1016/j.jcin.2014.10.010
52. Choi KH, Yang JH, Song YB, Hahn JY, Choi JH, Gwon HC, et al. Long-term clinical outcomes of patients with coronary chronic total occlusion treated with percutaneous coronary intervention versus medical therapy according to presence of diabetes mellitus. EuroIntervention. (2017) 13:970–7. doi: 10.4244/EIJ-D-16-00737
53. Sanguineti F, Garot P, O'Connor S, Watanabe Y, Spaziano M, Lefèvre T, et al. Chronic total coronary occlusion treated by percutaneous coronary intervention: long-term outcome in patients with and without diabetes. EuroIntervention. (2017) 12:e1889–97. doi: 10.4244/EIJ-D-15-00278
Keywords: coronary collateral circulation, smoking habit, hypertension, diabetes, meta-analysis
Citation: Pei J, Wang X and Xing Z (2021) Traditional Cardiovascular Risk Factors and Coronary Collateral Circulation: A Meta-Analysis. Front. Cardiovasc. Med. 8:743234. doi: 10.3389/fcvm.2021.743234
Received: 17 July 2021; Accepted: 30 September 2021;
Published: 03 November 2021.
Edited by:
Alexandra R. Lucas, Arizona State University, United StatesReviewed by:
Erhan Tenekecioglu, University of Health Sciences, TurkeyVivek Nanda, University of Alabama at Birmingham, United States
Copyright © 2021 Pei, Wang and Xing. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhenhua Xing, eGluZzIwMTJ4QGNzdS5lZHUuY24=
 Junyu Pei1
Junyu Pei1 Zhenhua Xing
Zhenhua Xing