
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 04 November 2021
Sec. Cardiovascular Surgery
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.728568
This article is part of the Research Topic Current Trends and Strategies for the Management of Type A Aortic Dissection View all 11 articles
 Hongliang Yuan1,2†
Hongliang Yuan1,2† Zhenxing Sun1,2†
Zhenxing Sun1,2† Yongxing Zhang1,2†
Yongxing Zhang1,2† Wenqian Wu1,2
Wenqian Wu1,2 Manwei Liu1,2
Manwei Liu1,2 Yali Yang1,2
Yali Yang1,2 Jing Wang1,2
Jing Wang1,2 Qing Lv1,2
Qing Lv1,2 Li Zhang1,2*
Li Zhang1,2* Yuman Li1,2*
Yuman Li1,2* Mingxing Xie1,2*
Mingxing Xie1,2*Objective: Acute type A aortic dissection (ATAAD) is a fatal condition that requires emergency surgery. The aim of the present study was to determine pre- and intra-operative risk factors for in-hospital mortality in patients with ATAAD.
Methods: Consecutive 313 patients with ATAAD who underwent emergency surgery at our hospital from February 2012 to February 2017 were enrolled in our study. Univariate and multivariate logistic regression analysis were performed to identify the pre-operative and intra-operative risk factors for in-hospital mortality.
Results: Of the 313 patients, 32 patients (10.2%) died. Compared with survivors, non-survivors had higher heart rate, serum potassium level and EuroSCORE II, and higher incidence of moderate to severe pericardial effusion, supra-aortic vessels involvement, myocardial ischemia and lower-extremity ischemia. As for surgery-related factors, the duration of surgery and cardiopulmonary bypass time were longer in non-survivors than survivors. In addition, non-survivors were more likely to undergo coronary-artery bypass graft compared with survivors. On multivariate analysis, elevated plasma potassium level (OR: 43.0, 95% CI: 3.8–51.5, p < 0.001), high incidence of supra-aortic vessels involvement (OR: 4.4, 95% CI: 1.5–7.0, p = 0.008) and lower-extremity ischemia (OR: 4.9, 95% CI: 1.6–6.9; p = 0.009), and longer duration of surgery (OR 6.0, 95% CI: 1.8–18.7, p = 0.000) and cardiopulmonary bypass time (OR: 3.7, 95% CI: 1.3–9.3, p = 0.001) were independently predictive of higher mortality in patients with ATAAD.
Conclusions: Supra-aortic vessels involvement, lower-extremity ischemia and elevated plasma potassium level are independent predictors of mortality in patients with ATAAD. A significant decrease in duration of surgery and cardiopulmonary bypass time is helpful to improve survival of patients.
Acute type A aortic dissection (ATAAD) is a life-threatening cardiovascular condition that requires emergent surgery. In recent years, the incidence of ATAAD has been increasing significantly due to high prevalence and poor control of hypertension (1). The development of advanced imaging technology had resulted in improving the diagnosis of ATAAD. Despite the improvement in medical management and surgical technique, the hospital mortality in patients with ATAAD remains high. Previous studies reported that the mortality was 16.9–18.4% after surgical repair of ATAAD (1–3). Therefore, it is necessary to recognize pre- and intra-operative risk factors for hospital mortality in patients with ATAAD.
Therefore, the aim of our study was to identify pre- and intra-operative risk factors for in-hospital mortality in patients with ATAAD.
Consecutive 321 patients with ATAAD who were admitted to the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology from February 2012 to February 2017 were enrolled. Patients treated with endovascular repair (n = 6) or conservative treatment (n = 2) were excluded. Finally, 313 patients who underwent emergency surgery were included in our study. All patients were diagnosed by computed tomography angiography, magnetic resonance imaging or echocardiography. The study was approved by the institutional ethics board of Union Hospital Tongji Medical College, Huazhong University of Science and Technology.
Patients' demographic characteristics, medical histories, comorbidities, echocardiographic data, laboratory results, vessel involvement, organ ischemia, primary tear location, surgical type, duration of surgery, and outcomes were retrieved from electronic medical records. Medical histories included hypertension, diabetes, dyslipidemia, coronary artery disease and previous heart surgery. Echocardiographic data were composed of diameter of ascending aorta, moderate to severe pericardial effusion, aortic regurgitation and left ventricular ejection fraction. The diameter of ascending aorta was measured from the parasternal long-axis view. Left ventricular ejection fraction was assessed by M-mode echocardiography. Involvement of vessel branches included ascending aorta, aortic arch and supra-aortic vessels involvements. Surgical type encompassed ascending aorta replacement, aortic valve replacement, aortic arch replacement, elephant truck procedure, Coronary Artery Bypass Graft (CABG), and aortic sinus repair. Outcomes was defined as in-hospital mortality after operation. EuroSCORE II were calculated based on the prior method (http://www.euroscore.org/calc.html).
Operative techniques were composed of cardiopulmonary bypass (CPB), moderate hypothermia, circulatory arrest, and unilateral antegrade cerebral perfusion (u-ACP). The central venous pressure, bilateral radial artery pressure, electrocardiography, nasopharyngeal and rectal temperature and intermittent arterial blood gas analysis were monitored. Near-infrared spectroscopy (NIRS) was used to monitor cerebral saturation. When u-ACP was used, cerebral perfusion was performed through the right axillary artery. If the vessel was dissected, the true lumen of the branch vessel was cannulated. The flow rate for u-ACP was 10–15 mL/kg/min with perfusion pressure of 50–70 mmHg. After CPB was established, cooling was initiated. After clamping of the ascending aorta, cardiac arrest was accomplished with cold cardioplegic solution. Subsequently, the aortic root procedure depending on the severity and extent of the disease, including aortic root formation or Bentall procedure with or without CABG were performed.
Categorical variables are presented as frequencies and percentages. Normally distributed continuous variables are presented as the means and standard deviations. Non-normally distributed continuous variables are presented as medians with quartiles. Continuous variables were compared using the t-test or Mann-Whitney U test. Categorical data were compared using the Fisher's exact or Chi-square tests. Receiver-operating characteristic (ROC) curves were used to obtain diagnostic cutoff values, as well as specificity and sensitivity. Estimations of the risk factors of mortality were performed using univariate and multivariate logistic regression models. To avoid the interaction between the pre-operative and intra-operative variable when the pre-operative and intra-operative variables were enrolled together in multivariate logistic regression analysis, we analyzed the pre- or intra-operative data independently. The possible pre-operative risk factors, including demographics, comorbidities, echocardiographic measurements, vessel involvement and laboratory results, were included in the pre-operative univariate logistic regression analysis. The potentially intra-operative predictors of higher mortality, including surgical type and duration of surgery, were entered into in the intra-operative univariate logistic regression analysis. Variables with p values <0.05 in univariate logistic regression analysis were entered into multivariate logistic regression models. The results of the logistic regressions are presented as odds ratio (OR) with confidence intervals (CI). The statistical analyses were performed with SPSS version 21.0 (SPSS Inc., Chicago, IL, USA). A 2-sided p value <0.05 was considered to indicate statistical significance.
A total of 313 patients were included in our study. Pre-operative characteristics of patients with ATAAD are summarized in Table 1. The mean age of patients with ATAAD was 48 years, and 264 (84%) were men. Only unilateral antegrade cerebral perfusion was performed in every patient with supra-aortic vessels involvement. NIRS was used in the intra-operative assessment of brain perfusion. Of these patients, 32 patients (10.2%) died. Non-survivors had higher heart rate and plasma potassium level than survivors. Compared with survivors, non-survivors displayed higher prevalence of moderate to severe pericardial effusion, involvement of supra-aortic vessels, myocardial ischemia and lower limb ischemia. There were no significant differences in age, sex, systemic arterial pressure, comorbidities (hypertension, diabetes, dyslipidemia and coronary artery disease), antihypertensive drug use between non-survivors and survivors. With regard to echocardiographic data, the diameter of ascending aorta, left ventricular ejection fraction and the prevalence of aortic regurgitation were similar in survivors and non-survivors. In addition, leukocyte, neutrophil and platelets counts, and creatinine level did not differ between survivors and non-survivors.
Intra-operative characteristics of patients with ATAAD are presented in Table 2. Compared with survivors, non-survivors had longer operation time and cardiopulmonary bypass time (CPBT). Non-survivors were more likely to undergo CABG than survivors. There was no statistically significant difference in aorta occlusion time, circulatory arrest time, lowest rectal temperature and cerebral perfusion time between non-survivors and survivors. Additionally, non-survivors had a similar treatment with ascending aorta replacement, aortic valve replacement, half or whole arch replacement, elephant trunk technique and aortic sinus repair as survivors.
ROC curves were used to determine the optimal cut-off values for operation time, extracorporeal circulation time, admission heart rate and blood potassium level to identify mortality in ATAAD patients (Table 3; Figure 1). ROC analysis revealed that duration of operation > 9.5 h [area under the curve (AUC): 0.73], CPBT > 227 min (AUC: 0.72), heart rate > 82 beats/min (AUC: 0.65) and plasma potassium > 4.4 mmol/L (AUC: 0.92) were associated with in-hospital mortality in patients with ATAAD.
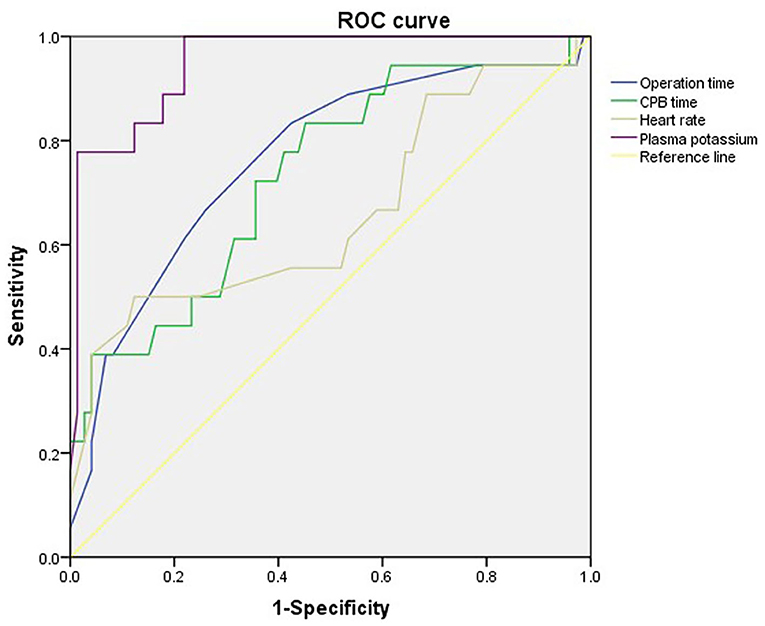
Figure 1. Receiver-operating characteristic curves of operation time, extracorporeal circulation time, admission heart rate and blood potassium level to identify mortality in ATAAD patients.
Univariate logistic regression analysis including pre-operative variables revealed that plasma potassium > 4.4 mmol/L, supra-aortic branch involvement, lower limb ischemia, and myocardial ischemia were predictors of higher mortality in patients with ATAAD. Multivariable logistic regression analysis demonstrated that plasma potassium > 4.4 mmol/L (OR: 43.0, 95% CI: 3.8–51.5, p < 0.001), supra-aortic branch involvement (OR: 4.4; 95% CI: 1.5–7.0, p = 0.008), and lower limb ischemia (OR: 4.9, 95% CI: 1.6–6.9, p = 0.009) were independently predictive of in-hospital mortality (Table 4).
Univariate logistic regression analysis including intra-operative variables showed that elephant truck procedure, CABG, operation time > 9.7 h, CPBT > 227 min could predict higher mortality in patients with ATAAD. Multivariable logistic regression analysis revealed that operation time >9.7 h (OR: 6.0, 95% CI: 1.8–18.7, p < 0.001), CPBT > 227 min (OR: 3.7, 95% CI: 1.3–9.3, p = 0.002), and elephant truck procedure (OR: 4.1, 95% CI: 1.4–6.9, p = 0.008) were independent predictors of in-hospital mortality (Table 5).
In this study of 313 consecutive patients with ATAAD who underwent emergency surgery from February 2012 and February 2017, the overall hospital mortality was 10.2%. Although the hospital mortality was lower than that of previous studies (1–3), it is still unacceptable. It is necessary to summarize the risk factors for in-hospital mortality in patients with ATAAD. Our results indicated that pre- and intra-operative risk factors for in-hospital mortality in patients with ATAAD were elevated level of plasma potassium, higher incidence of supra-aortic vessels involvement and lower-extremity ischemia, and longer duration of operation and cardiopulmonary bypass time.
The present study showed that supra-aortic vessels involvement was a risk factor for hospital death. The extension of ATAAD with involvement of the supra-aortic branches largely determined the pre-operative state of the patients and influenced the post-operative outcome. Mortality may increase rapidly if the supra-aortic vessels are involved in the dissection process. Patients with ATAAD with supra-aortic vessel involvement have a higher risk of post-operative stroke. Understandably, anastomosis of branch vessels is required during surgery in these patients, which prolonged the time of extracorporeal circulation and operation, and further may lead to diminished blood supply to the brain. Thus, cerebral malperfusion further increase in-hospital mortality (1, 4). In the current study, we found that 186 patients had supra-aortic vessels involvement. Twenty six of these patients (14.0%) died during hospitalization. Thereby, an appropriate protection procedure is important to prevent irreversible brain injury. The various cerebral protection (antegrade/ retrograde; monolateral/bilateral) can be used during aortic arch surgery. The unilateral antegrade cerebral perfusion was performed during aortic arch surgery in this study. The relative benefits of unilateral antegrade cerebral perfusion compared with bilateral antegrade cerebral perfusion as cerebral perfusion strategies remained undetermined. Tong et al. revealed that bilateral antegrade cerebral perfusion did not significantly reduce 30-days mortality and permanent neurologic dysfunction compared to unilateral antegrade cerebral perfusion (5). However, Misfeld et al. showed that early mortality and medium-term survival was not affected by the type of cerebral protection used (6). In addition, Zierer et al. demonstrated that unilateral antegrade cerebral perfusion had the equal brain protection compared to bilateral antegrade cerebral perfusion (7). More and more data show that unilateral cerebral perfusion in moderate hypothermia is safe when performed during NIRS monitoring and that avoiding deep hypothermia preserves cerebral autoregulation blood flow, resulting in an optimal unilateral perfusion. Only unilateral antegrade cerebral perfusion was performed in every patient with supra-aortic vessels involvement during February 2012 to February 2017 in this study. So, we did not determine the different impact of the type of cerebral protection on clinical outcomes in cases of an aortic arch surgery and involvement of supra-aortic vessels in our hospital. It deserves further investigation whether unilateral antegrade cerebral perfusion is superior to bilateral antegrade cerebral perfusion in patients with ATAAD with supra-aortic vessels involvement.
In this study, non-survivors had the higher incidence of lower limb ischemia than survivors. Moreover, multivariate logistic regression analysis showed that lower limb ischemia was a risk factor for mortality in patients with ATAAD, which was similar as previous studies (8, 9). Poor perfusion of the lower extremities can lead to serious post-operative complications (10). In our study, lower-extremity ischemia was diagnosed in 27 patients with no palpable pulses in the femoral artery before surgery. Eleven of these patients (40.7%) died during hospitalization. Uchida et al. showed that improvements of the blood supply of lower-extremity by draining the brachial arterial blood to the ischemic lower limb arteries, may significantly improve symptoms (11). Whether this strategy should be mandatory is highly controversial. Preece et al. demonstrated that inferior-limb ischemic artery reperfusion before aortic repair increased intra-operative mortality in ATAAD patients (12).
In addition to supra-aortic vessels involvement and lower limb ischemia, elevated level of plasma potassium was found to be another independent risk factor of higher in-hospital mortality in patients with ATAAD. Indeed, our study demonstrated that non-survivors had higher blood potassium level than survivors. Moreover, the current observation demonstrated that the optimal cut-off value of plasma potassium level for predicting higher mortality in patients with ATAAD was over 4.4 mmol/L. Patients who had higher level of plasma potassium above the cutoffs had increased risk of mortality. Potassium serum levels within the high normal range (>4.4 to < 5.0 mmol/L), which were frequently ignored by clinicians in the emergency department, were associated with higher in-hospital mortality. This finding is consistent with the results of Chen et al., who found that the blood potassium level other than 3.5 to 4.5 mmol/L at admission was related to higher in-hospital and long-term mortality in ATAAD patients (13). Previous studies found a U-shaped relationship between serum potassium levels at admission and in-hospital mortality, which potassium levels outside the interval of <3.5 to 4.5 mmol/L were associated with higher risk in all-cause mortality (13, 14). The risk of cardiovascular mortality increases with the elevated potassium levels, due to the fact that the heart is more susceptible to potassium fluctuation than other tissues. An increase in serum potassium level is associated with reduced ventricular excitability and has been shown to cause increased diastolic threshold of excitability in experimental animals and humans (15, 16), which would be associated with an increased prevalence of cardiac arrhythmias. A large body of evidences have demonstrated that even a mild change within the normal range is associated with higher mortality in patients with various cardiovascular diseases, such as hypertension (17), acute coronary syndrome (14, 18), and heart failure (19, 20), which reveal that the optimal blood potassium level may be different from the definite clinical normal range in diverse cardiovascular diseases. ATAAD patients with more severe circumstances (such as use of antihypertensive drugs, hemorrhage and hemolysis) may experience a serum potassium disturbance, which is similar to that in other cardiovascular diseases. However, current guidelines do not underscore potassium management in patients with aortic diseases (21, 22). Our results demonstrated that higher potassium levels at admission had an adverse effect on the in-hospital mortality of patients with ATAAD, and accordingly, more active management may be necessary.
The duration of extracorporeal circulation was significantly longer in non-survivors than survivors. Furthermore, a multivariable analysis showed that the duration of surgery and the duration of extracorporeal circulation were risk factors for in-hospital mortality. Our findings are consistent with previous studies (23). A long operation time reflects the severity of ATAAD; moreover, it had an adverse effect on organ perfusion. Therefore, these may be the reason why longer duration of operation is associated with unfavorable outcomes in patients with ATAAD.
Previous researches indicated that myocardial ischemia was a risk factor for in-hospital mortality in patients with ATAAD. In our study, univariate regression analysis demonstrated that myocardial ischemia was a predictor of mortality in patients with ATAAD. However, in multivariate logistic regression analysis, myocardial ischemia was no longer significantly predictive of in-hospital mortality. In our series, 37 patients had myocardial infarction before surgery, and 9 of them (24.3%) died during hospitalization. This may be the reason that most patients with myocardial ischemia were simultaneously treated with coronary artery bypass graft during the aortic replacement, which markedly improved myocardial ischemia and the prognosis.
In our study, 188 patients with ATAAD presented with medium to large amounts of pericardial effusion. Non-survivors had a higher incidence of medium to large amounts of pericardial effusion than survivors. However, univariate and multiple regression analysis revealed that moderate to severe pericardial effusion could not predict higher in-hospital death in patients with ATAAD. This finding was not in line with the study of Santi Trimarchi et al., which demonstrated that pericardial tamponade was an independent predictor of post-operative mortality in patients with ATAAD (8).
Our study revealed that elephant truck procedure was a risk factor of mortality in patients with ATAAD. This result was not in keeping with the observation of Goda et al., which indicated that various surgical methods did not affect the early post-operative mortality in ATAAD patients (9). However, Tan et al. found that simultaneous aortic valve replacement or Bentall surgery in ATAAD patients was a protective factor for post-operative mortality (23). Future studies are needed to confirm the effect of various surgical treatment on outcomes in patients with ATAAD.
Our study had some limitations. First, this was a retrospectively single-center study, extrapolation of our findings could be affected by local bias. In addition, sample size of this study is relatively limited. Future multicenter studies with larger sample sizes are needed to verify our findings. Another limitation of our study is that we did not determine the different impact of the type of cerebral protection on clinical outcomes in cases of an aortic arch surgery and involvement of supra-aortic vessels, because that only unilateral antegrade cerebral perfusion was performed in every patient with supra-aortic vessels involvement in our study. The effect of cerebral protection type on outcomes in patients with supra-aortic vessels involvement is an interesting topic. Future study that investigates the different impact of cerebral protection type on clinical outcomes could be the next step. Finally, the numbers of non-survivors were small, the exiguous number of the mortality group and the great numeric difference between the two groups could represent a statistical limitation for a solid conclusion based on this study.
Supra-aortic vessels involvement, lower-extremity ischemia and elevated plasma potassium level are pre-operative risk factors for in-hospital mortality in patients with ATAAD. Among intra-operative factors, longer operation time and cardiopulmonary bypass time are associated with increased in-hospital mortality. For further improvement of outcomes, quicker diagnosis, more appropriate pre-operative management and minimizing any delay in surgery are mandatory.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Ethical Committee of Tongji Medical College of Huazhong University of Science and Technology. Written informed consent was not required for this study, in accordance with the local legislation and institutional requirements.
MX and LZ contributed to the conception of the study. HY, ZS, and YL analyzed and interpreted the clinical data and imaging findings, and they were major contributors in writing the manuscript. YZ, WW, and ML helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
This work was supported by National Natural Science Foundation of China (Grant Nos. 81727805, 81701716, 81922033), the Key Research and Development Program of Hubei (Grant No. 2020DCD015), the Fundamental Research Funds for the Central Universities (Grant No. 5003530082), and the Shenzhen Science and Technology under (Grant No. SGDX20190917094601717).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Conzelmann LO, Hoffmann I, Blettner M, Kallenbach K, Karck M, Dapunt O, et al. Analysis of risk factors for neurological dysfunction in patients with acute aortic dissection type A: data from the German registry for acute aortic dissection type a (geraada). Eur J Cardiothorac Surg. (2012) 42:557–65. doi: 10.1093/ejcts/ezs025
2. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17- year trends from the international registry of acute aortic dissection. J Am Coll Cardiol. (2015) 66:350–8. doi: 10.1016/j.jacc.2015.05.029
3. Lee TC, Kon Z, Cheema FH, Grau-Sepulveda MV, Englum B, Kim S, et al. Contemporary management and outcomes of acute type A aortic dissection: an analysis of the STS adult cardiac surgery database. J Card Surg. (2018) 33:7–18. doi: 10.1111/jocs.13511
4. Furukawa T, Uchida N, Takahashi S, Yamane Y, Mochizuki S, Yamada K, et al. Management of cerebral malperfusion in surgical repair of acute type A aortic dissection. Eur J Cardiothorac Surg. (2017) 52:327–32. doi: 10.1093/ejcts/ezx056
5. Tong G, Zhang B, Zhou X, Tao Y, Yan T, Wang X, et al. Bilateral versus unilateral antegrade cerebral perfusion in total arch replacement for type A aortic dissection. J Thorac Cardiovasc Surg. (2017) 154:767–75. doi: 10.1016/j.jtcvs.2017.02.053
6. Misfeld M, Leontyev S, Borger MA, Gindensperger O, Lehmann S, Legare JF, et al. What is the best strategy for brain protection in patients undergoing aortic arch surgery? A single center experience of 636 patients. Ann Thorac Surg. (2012) 93:1502–8. doi: 10.1016/j.athoracsur.2012.01.106
7. Zierer A, Ahmad AES, Papadopoulos N, Moritz A, Diegeler A, Urbanski PP. Selective antegrade cerebral perfusion and mild (28°C-30°C) systemic hypothermic circulatory arrest for aortic arch replacement: results from 1002 patients. J Thorac Cardiovasc Surg. (2012) 144:1042–49. doi: 10.1016/j.jtcvs.2012.07.063
8. Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Mehta RH, et al. Contemporary results of surgery in acute type A aortic dissection: the international registry of acute aortic dissection experience. J Thorac Cardiovasc Surg. (2005) 129:112–22. doi: 10.1016/j.jtcvs.2004.09.005
9. Goda M, Imoto K, Suzuki S, Uchida K, Yanagi H, Yasuda S, et al. Risk analysis for hospital mortality in patients with acute type A aortic dissection. Ann Thoracic Surg. (2010) 90:1246–50. doi: 10.1016/j.athoracsur.2010.05.069
10. Bossone E, Rampoldi V, Nienaber CA, Yrimarchi S, Ballotta A, Cooper JV, et al. Usefulness of pulse deficit to predict in-hospital complications and mortality in patients with acute type A aortic dissection. Am J Cardiol. (2002) 89:851–85. doi: 10.1016/S0002-9149(02)02198-7
11. Uchida K, Karube N, Kasama K, Minami T, Yasuda S, Goda M, et al. Early reperfusion strategy improves the outcomes of surgery for type A acute aortic dissection with malperfusion. J Thorac Cardiovasc Surg. (2018) 156:483–9. doi: 10.1016/j.jtcvs.2018.02.007
12. Preece R, Srivastava V, Akowuah E, Kendall S. Should limb revascularization take priority over dissection repair in type A aortic dissection presenting as isolated acute limb ischaemia. Interact Cardiovasc Thorac Surg. (2017) 25:643–6. doi: 10.1093/icvts/ivx169
13. Chen Z, Huang B, Lu H, Zhao Z, Hui R, Zhang S, et al. The effect of admission serum potassium levels on in-hospital and long-term mortality in type A acute aortic dissection. Clin Biochem. (2017) 50:843–50. doi: 10.1016/j.clinbiochem.2017.05.008
14. Goyal A, Spertus JA, Gosch K, Venkitachalam L, Jones PG, Berghe GVD, et al. Serum potassium levels and mortality in acute myocardial infarction. JAMA. (2012) 307:157–64. doi: 10.1001/jama.2011.1967
15. Surawicz B, Chlebus H, Reeves JT, Gettes LS. Increase of ventricular excitability threshold by hyperpotassemia: possible cause of internal pacemaker failure. JAMA. (1965) 191:1049–54. doi: 10.1001/jama.1965.03080130009002
16. Gettes LS, Shabetai R, Downs TA, Surawicz B. Effect of changes in potassium and calcium concentrations on diastolic threshold and strength-interval relationships of the human heart. Ann N Y Acad Sci. (1969) 167:693–705. doi: 10.1111/j.1749-6632.1969.tb34130.x
17. Krogager ML, Torp-Pedersen C, Mortensen RN, Køber L, et al. Short-term mortality risk of serum potassium levels in hypertension: a retrospective analysis of nationwide registry data. Eur Heart J. (2017) 38:104–12. doi: 10.1093/eurheartj/ehw129
18. Peng Y, Huang F, Liu W, Zhang C, Zhao Z, Huang B, et al. Relation between admission serum potassium levels and long-term mortality in acute coronary syndrome. Intern Emerg Med. (2015) 10:927–35. doi: 10.1007/s11739-015-1253-1
19. Pitt B, Bakris G, Ruilope LM, DiCarlo L, Mukherjee R, Investigators E. Serum potassium and clinical outcomes in the eplerenone post-acute myocardial infarction heart failure efficacy and survival study (EPHESUS). Circulation. (2008) 118:1643–50. doi: 10.1161/CIRCULATIONAHA.108.778811
20. Rossignol P, Girerd N, Bakris G, Vardeny O, Claggett B, McMurray JJV, et al. Impact of eplerenone on cardiovascular outcomes in heart failure patients with hypokalaemia. Eur J Heart Fail. (2017) 19:792–9. doi: 10.1002/ejhf.688
21. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Caset DE Jr, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/ SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. J. Am. Coll. Cardiol. (2010) 55:e27–129. doi: 10.1161/CIR.0b013e3181d4739e
22. Erbel R, Aboyans V, Boileau C, Bossone E, Eggebrecht HE, Evangelista A, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. (2014) 35:2873–926. doi: 10.1093/eurheartj/ehu281
Keywords: acute type A aortic dissection, surgery, mortality, risk factors, retrospective
Citation: Yuan H, Sun Z, Zhang Y, Wu W, Liu M, Yang Y, Wang J, Lv Q, Zhang L, Li Y and Xie M (2021) Clinical Analysis of Risk Factors for Mortality in Type A Acute Aortic Dissection: A Single Study From China. Front. Cardiovasc. Med. 8:728568. doi: 10.3389/fcvm.2021.728568
Received: 21 June 2021; Accepted: 13 October 2021;
Published: 04 November 2021.
Edited by:
Antonio Miceli, Istituto Clinico Sant'Ambrogio, ItalyReviewed by:
Bleri Celmeta, Istituto Clinico Sant'Ambrogio, ItalyCopyright © 2021 Yuan, Sun, Zhang, Wu, Liu, Yang, Wang, Lv, Zhang, Li and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingxing Xie, eGllbXhAaHVzdC5lZHUuY24=; Yuman Li, bGl5bUBodXN0LmVkdS5jbg==; Li Zhang, emxpNDI5QGh1c3QuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.