
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med. , 01 July 2021
Sec. General Cardiovascular Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.679105
This article is part of the Research Topic Highlights in General Cardiovascular Medicine: 2021 View all 12 articles
An increasing number of cardiovascular adverse effects, emergency room visits, and deaths have been linked to energy drinks. In this review, we summarized available published literature assessing electrophysiological and ischemic adverse effects associated with energy drink consumption. Overall, 32 case reports and 19 clinical trials are included in this review. Ventricular arrhythmia, supraventricular arrhythmia, and myocardial ischemia were amongst the most commonly reported in case reports with 3 having a fatal outcome. Although serious ischemic changes, arrhythmias, or death were not observed in clinical trials, significant electrophysiological changes, such as PR/PQ interval shortening/prolongation, QT/QTc shortening/prolongation, and ST-T changes, were noted. QT/QTc interval prolongation appears to be the most significant finding in clinical trials, and there appears to be a dose-response relationship between energy drink consumption and QTc prolongation. The exact mechanisms and the particular combination of ingredients behind energy drink-induced cardiac abnormalities require further evaluation. Until more information is available, energy drink use should be considered as part of the differential diagnosis in appropriate patients presenting with electrocardiographic changes. Further, certain patient populations should exercise caution and limit their energy drink consumption.
Energy drinks (ED) are an increasingly utilized niche in the beverage market and are gaining popularity in recent years, especially amongst teenagers and young adults. According to the National Health and Nutrition Examination Surveys, ED consumption has grown substantially amongst adolescents and adults in the United States (1). A United States Substance Abuse Services and Mental Health Administration (SAMHSA) report revealed patients aged 18 to 39 were most commonly involved in ED-related emergency department visits (2). Energy drinks are generally available in a variety of sizes ranging from a 60 ml “shot” form, to a larger 710 ml container. They typically contain caffeine in conjunction with presumed energy-enhancing ingredients such as taurine, B vitamins, and herbal extracts. Caffeine content in ED typically vary from 70 to 200 mg per 473 ml serving (3). Beneficial claims of ED include improvements in alertness, physical endurance, metabolism and concentration. Energy drink-associated emergency department visits have sharply increased in recent years. According to a report by SAMHSA, the number of emergency department visits due to EDs increased from 10,068 to 20,783 between 2007 and 2011 (2). In a recent study conducted in Air Force personnel, nearly 1% of energy drink users reported needing to see a physician or going to the emergency department because of adverse effects from energy drinks (4). The Center for Science in the Public Interest reports 34 deaths linked to energy drink consumption (5). An analysis of poison control data of 5,156 reports suggests cardiac and neurological adverse effects are amongst the most common (6). It is important to note, however, that the number of adverse events due to ED is likely underestimated in these reports since such reporting is completely voluntary. Accordingly, we reviewed available literature of published case reports and clinical research studies evaluating electrophysiological abnormalities related to ED consumption. This review serves to better inform clinicians of the notable connection between ED and electrocardiogram (ECG) changes. The information may provide additional insight in the differential diagnosis of patients presenting with ECG changes in the emergency department.
A qualitative review was conducted by searching for relevant articles in PubMed, EMBASE, Cochrane database from 2001 to July 1, 2019 along with hand searching references from appropriate articles. Case reports and clinical trials assessing the effects of energy drink on electrophysiological and ischemic abnormalities were included. Studies assessing energy capsule, bar, soda or sports drink were excluded. Due to the sparsity of randomized, placebo-controlled trials and the heterogeneity among these studies, a meta-analysis was not performed.
A total of 32 individual cases (28 case report publications) have been described in the literature regarding ED and cardiac rhythm abnormalities (Table 1) (7–35). Three cases were described in two publications by Mattioli et al. and each case was only counted once as the authors assumed that the two publications were referring to the same patients. The majority of patients were male (84%) with a median age of 25 years (range 13–53). Seventeen cases were from the United States. The most common presentations were chest pain, palpitation, nausea/vomiting, and cardiac arrest. Twenty-two cases involved consumption of ED only, while 10 reported coingestion of an ED with another substance (5 with alcohol, 3 with amphetamine salts, 1 with additional caffeine, and 1 with a caffeinated soda). A total of 3 cases resulted in death, with one of the cases reporting coingestion with 3, 4-methylenedioxymethamphetamine (MDMA). Arrhythmia was reported in 20 cases (9 supraventricular [includes one case of Wolff-Parkinson-White Syndrome], 10 ventricular and 1 being supraventricular and ventricular). Fourteen cases reported ST-segment changes, 1 of which was fatal, 5 were found to have coronary artery occlusion, 2 were diagnosed with spontaneous coronary artery dissection, 1 had a normal repeat exercise treadmill test without ED, 4 revealed normal coronary arteries post coronary angiography, 1 was diagnosed with Brugada syndrome, and 1 was diagnosed with coronary artery vasospasm. QT/QTc prolongation was evident in 4 cases. One case was associated with ventricular tachycardia, 2 were discharge with a diagnosis of Long QT type 1 (LQTS1), and QTc prolongation resolved without intervention in 1 case involving a healthy volunteer. One patient was identified as having reverse Takotsubo cardiomyopathy.
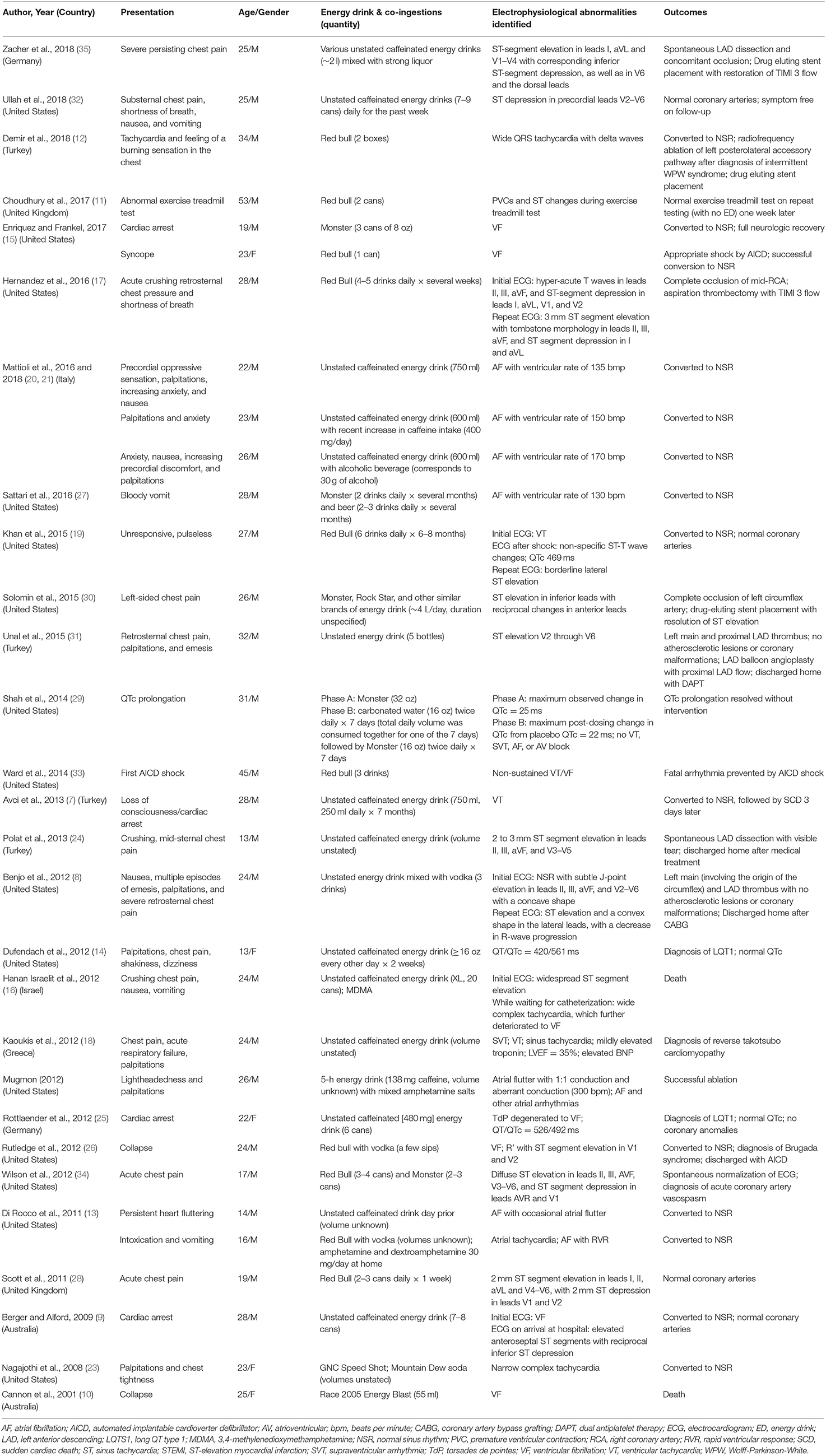
Table 1. Case reports of energy drinks and related electrophysiological and ischemic abnormalities (7–35).
Table 2 contains a list of all 19 original research articles (36–54). The smallest sample size studied was 1 (this study was designed as a clinical trial but stopped early due to administrative reasons and the emergence of new data), and the largest study included 80 participants. Subjects were generally young healthy volunteers with the exception of the study by Gray et al. which evaluated subjects with long QT syndrome (LQTS). Caffeinated EDs were used in all studies. The volume of EDs or matching control drinks ranged from 60 to 1,000 ml. The shortest total duration of assessment was 30 min, while the longest lasted 24 h. Ten out of the 19 studies were performed in the United States. Thirteen were controlled trials, whereas 6 were non-controlled. Three studies employed a parallel study design, 8 employed crossover, and 1 study used both parallel and crossover design. All trials assessed the effect of ED on QTc interval. In 8 of the 19 studies, ED was associated with statistically significant QTc prolongation compared to at least one comparator group. In contrast, 1 study showed ED-associated QTc shortening. QT interval correction were most commonly calculated using the Bazett's formula (9 out of 19 studies). Of the remaining studies, 3 used both Bazett's and Fridericia formula, and 7 did not specify the formula used for QTc correction. Eighteen of the trials evaluated the effect of ED on heart rate (HR). Of these studies, 5 demonstrated a statistically significant increase in HR with ED in at least one comparison, and 1 found a statistically significant HR decline. ED was associated with more frequent ST-T changes in 1 study, and none of the studies noted any clinically significant arrhythmias.
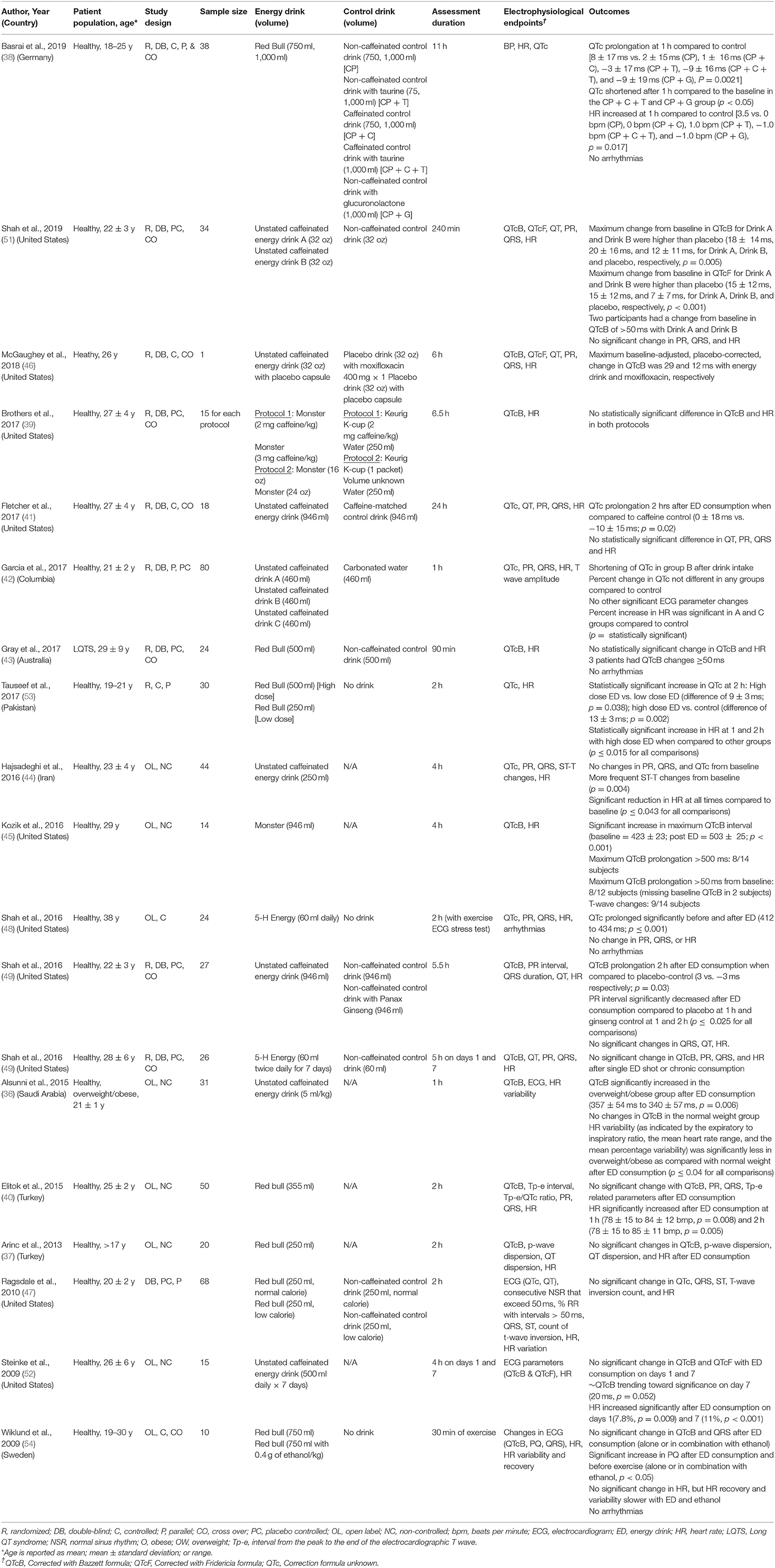
Table 2. Clinical trials of energy drinks and related electrophysiological and ischemic abnormalities (36–54).
In our comprehensive review of case reports with a documented electrophysiological abnormality, ventricular arrhythmia, supraventricular arrhythmia, and myocardial ischemia were amongst the most commonly reported. Although serious arrhythmias or death were not observed in clinical trials, a multitude of significant ECG changes (PR/PQ interval shortening/prolongation, QT/QTc shortening/prolongation, ST-T changes) with ED were noted. QTc prolongation was the most common and significant finding in clinical trials. In controlled trials showing a significant prolongation of the QT interval, the average change in QT/QTc was small (6–10 ms) (38, 41, 50, 51), but this magnitude of change can still be meaningful. The FDA requires thorough QT/QTc evaluation for all new drug entities with a QT/QTc prolongation of at least 5 ms (55), and results of such evaluation may carry drug labeling significance. As an example, azithromycin bears a warning in its package insert for prolonging the QTc by 5–9 ms with the administration of 500–1,500 mg of oral azithromycin (56). QT/QTc changes >50 ms or an absolute value >500 ms are generally considered clinically significant in practice (55), and this degree of QT/QTc prolongation was observed in a few cases and several clinical trials participants (14, 25, 43, 45, 51).
Our review identified 3 cases resulting in death, all of which had a documented ventricular arrhythmia prior to the fatal event. Sudden cardiac death in patients under the age of 35 is usually attributed to an underlying cardiac condition but is also frequently idiopathic (57); however, the temporal relationship between energy drink consumption, ventricular arrhythmia, and fatality is concerning. As noted in prior studies, QT/QTc prolongation can induce early after depolarizations, provoke Torsades de Pointes, or lead to ventricular fibrillation, which can potentially cause sudden cardiac death. As such, QT/QTc prolongation appears to provide a plausible explanation for energy drink-induced ventricular arrhythmias. The relation between QTc and all-cause mortality, cardiac mortality, and sudden cardiac death has also been well-established in population studies (58). However, it is important to note that QTc prolongation does not always lead to Torsades de Pointes or ventricular arrhythmias, therefore additional markers for arrhythmia risk prediction should also be incorporated in future studies.
Supraventricular arrhythmia and myocardial ischemia were also frequently documented in case reports, but these abnormalities cannot necessarily be explained by the prolongation of the QT/QTc interval. A multitude of risk factors exist for supraventricular arrhythmias such as atrial fibrillation and atrial flutter, including high dose caffeine, alcohol, amphetamine salts, excessive sympathetic stimulation, and stress amongst others. That being the case, coingestion of ED with another substance may explain the supraventricular arrhythmias seen in published cases. Interestingly, of the 10 cases of supraventricular arrhythmia, 6 involved coingestion of a second substance (2 with alcohol, 2 with amphetamine salts, 1 with caffeine, and 1 with a caffeinated soda). In contrast, coingestants were only involved in 2 of the 11 cases of ventricular arrhythmia and 4 of the 14 cases with ST-segment changes.
Consumption of ED has also been linked to myocardial ischemia in multiple case reports (8, 9, 11, 16, 17, 19, 24, 26, 28, 30–32, 34, 35). Changes in platelet aggregation post-ED consumption has been suggested by some studies (59), warranting further exploration of this phenomenon as a pathway leading to coronary thrombosis.
Even though inconsistencies in outcome have been observed in clinical trials due to heterogeneity in study design and small sample size, one interesting trend was observed. There appears to be a dose-related relationship between ED consumption and QTc prolongation. In studies showing significant QTc prolongation with ED, the median volume of ED consumed was >800 ml, compared to <500 ml in studies showing a lack of association. The majority of reported cases also involved consumption of large amounts of ED. Limiting the volume of energy drinks acutely therefore should be encouraged.
Certain patient population may be at particular risk for developing ED-related adverse effects. The majority of the studies included young health volunteers; however, one study had a cohort of overweight or obese students (36) and another looked at patients with underlying LQTS (43). While QTc was not changed in the normal weight group, the overweight/obese group demonstrated significantly increased QTc at 60 min post-ED consumption (p = 0.006) (36). A meta-analysis conducted by Omran et al. seems to confirm the association between overweight/obesity and QTc prolongation (60), therefore this population may require further risk assessment. Although a significant change in QTc was not observed in the study conducted in patients with LQTS, 3 out of 24 patients in the study developed QTc increase of at least 50 ms after the ED consumption (43). Energy drink consumption also unmasked LQTS in 2 of the published cases (14, 25). Together, these data suggest that the consumption of ED should be limited in patients with underlying LQTS.
Whether it is an individual component in energy drinks, multiple ingredients, or their combination that may induce ECG abnormalities requires further investigation. Though most energy drinks contain caffeine, caffeine is generally recognized as safe at doses under 400 mg and seems unlikely to be the sole ingredient contributing to rhythm abnormalities in EDs. In a small study of 10 healthy volunteers, no ECG changes were evident 3 h post 400 mg of caffeine ingestion (61). Based on population studies, moderate caffeine consumption is also thought to be an unlikely cause of arrhythmias (62). As such, in the study by Fletcher et al. where ED was compared to a matching caffeine-only control, the QTc was 10 ms higher in the ED group when compared to the caffeine group (41). However, there was not a non-caffeinated-control group which would have allowed for a more ideal comparison. A recent study by Basrai et al. also evaluated the impact of a commercial ED against ingredients commonly included in ED. Comparator groups in the study included placebo, placebo with caffeine, placebo with taurine, placebo with glucuronolactone and placebo with caffeine and taurine (38). Despite the complex structure of the design, QTc prolongation was observed in the ED group while all other groups either had no change or QTc shortening. Lastly, in a study comparing ED, panax ginseng and a placebo control, panax ginseng did not appear to have an effect on ECG parameters while ED prolonged the QTc interval (50). It appears likely that the unique combination of ingredients in ED, as opposed to caffeine alone, may be responsible for inducing ED-associated ECG changes in clinical studies. Based on available information, taurine or panax ginseng alone does not appear to drive any ECG effects associated with EDs.
One important consideration in studies investigating the effect of ED and QTc is the formula used for QT interval correction. While Bazett's formula is most commonly used clinically, it has been known to overcorrect at higher heart rates and undercorrect at lower heart rates. Several other correction formulas exist, and some data suggest that the Fridericia and Framingham correction formulas have the best rate correction and significantly improved prediction of 30-day and 1-year mortality compared to the Bazett's correction formula (63). Most trials included in this review used the Bazett's correction formula, but future studies should consider reporting multiple correction formulas.
The impact of acute vs. chronic consumption also warrants further evaluation. In a number of case reports, subjects had been consuming energy beverages for an extended period of time before presenting with a cardiac abnormality (7, 14, 17, 19, 27, 28, 30, 32). Only 2 clinical trials evaluated the effects of chronic (1 week) ED consumption (49, 52). However, interpretation of these studies is difficult due to discordant results and study design limitations. With emerging data, multiple organizations started to raise a note of caution with ED consumption. In 2011, the American Academy of Pediatrics, an organization of 60,000 pediatricians recommended against kids and teens from drinking EDs (64). In 2013, the American Medical Association called for a ban in advertising EDs to children under 18 (65). Lithuania was the first country to enact a ban against the sale of EDs to minors (66). Aiming to safeguard the development of EDs in Europe, all European Union member states must now abide to specific provisions for the labeling of EDs under the Code of Practice for the Marketing and Labeling of Energy Drinks. Countries have either adopted specific rules on EDs (Germany, Switzerland) or provided principles for the composition of EDs through corresponding food guidelines (Austria) (67). Subsequently, the American Beverage Association also developed voluntary guidelines to label EDs for their age appropriateness in 2014 (68).
To our knowledge, this is the most comprehensive review as other reviews are only driven by case reports or have not captured the totality of available literature (69, 70). However, several limitations should be noted when interpreting our findings in this review. It is important to note that the majority of the studies were small, mainly studied in young healthy volunteers, assessed only the acute cardiovascular effects of ED consumptions and with some, lacked a control arm. This review also does not extend to soda type beverages which may also contribute to the total daily caffeine consumed by individuals (e.g., soft drinks typically contain between 20 and 70 mg of caffeine per 12 fluid ounces) (71).
The preponderance of data suggests a significant correlation between ED and electrophysiological changes. While case reports have noted both ventricular and supraventricular arrhythmias, these were not evident in clinical trials. Large volume ED consumption appears to mildly prolong the QTc interval which may in part explain the mechanism behind some of the ventricular arrhythmias and associated deaths. Coingestion of other substances was seen in the majority cases of supraventricular arrhythmias. ST-segment changes and myocardial ischemia were also frequently noted in case reports. The exact mechanisms and the particular combination of ingredients behind these cardiac abnormalities require further evaluation. Until more information is available, energy drink use should be considered as part of the differential diagnosis in appropriate patients presenting with electrocardiographic changes. Appropriate labeling or warnings for consumers are also worthy of consideration by policy makers.
Energy drinks are an increasingly utilized niche in the beverage market and are gaining popularity in recent years, especially among teenagers and young adults. An increasing number of cardiovascular adverse effects, emergency room visits, and deaths have been linked to the consumption of energy drinks. To our knowledge, this is the most comprehensive review assessing electrophysiological and ischemic adverse effects associated with energy drink consumption. Overall, 32 case reports and 19 clinical trials are included in this review, suggesting the need for thorough patient evaluation presenting with electrocardiographic changes. The exact mechanisms and the particular combination of ingredients behind energy drink-induced cardiac abnormalities require further evaluation. Until further information is available, certain patient populations should exercise caution and limit their energy drink consumption.
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
The views expressed in this material are solely those of the authors and do not reflect the official policy or position of the US Government, the Department of Defense, the US Air Force, the Marshall B. Ketchum University, or the University of the Pacific.
SS has served as an expert witness in legal cases related to caffeinated energy drinks.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Vercammen KA, Koma JW, Bleich SN: Trends in energy drink consumption among U.S. adolescents and adults, 2003-2016. Am J Prev Med. (2019) 56:827–33. doi: 10.1016/j.amepre.2018.12.007
2. Substance Abuse and Mental Health Services Administration and Center for Behavioral Health Statistics and Quality. The DAWN Report: Update on Emergency Department Visits Involving Energy Drinks: A Continuing Public Concern. Available online at https://www.samhsa.gov/data/sites/default/files/DAWN126/DAWN126/sr126-energy-drinks-use.htm (accessed August 13, 2019).
3. Higgins JP, Tuttle TD, Higgins CL. Energy beverages: content and safety. Mayo Clin Proc. (2010) 85:1033–41. doi: 10.4065/mcp.2010.0381
4. Milazzo NA, Cao DX, Diwaker G, Thornton JA, Shah SA. A survey of energy drink consumption and associated adverse effects in air force personnel. Mil Med. (2020) 186, usaa362. doi: 10.1093/milmed/usaa362
5. Center for Science in the Public Interest. Documents Link More Deaths to Energy Drinks. Available online at: https://cspinet.org/news/documents-link-more-deaths-energy-drinks-20140625 (accessed August 13, 2019).
6. American Heart Association. Poison Control Data Show Energy Drinks and Young Kids Don't Mix. Available online at: https://newsarchive.heart.org/poison-control-data-show-energy-drinks-young-kids-dont-mix/ (accessed August 13, 2019).
7. Avci S, Sarikaya R, Buyukcam F. Death of a young man after overuse of energy drink. Am J Emerg Med. (2013) 31:1624.e3–4. doi: 10.1016/j.ajem.2013.06.031
8. Benjo AM, Pineda AM, Nascimento FO, Zamora C, Lamas GA, Escolar E. Left main coronary artery acute thrombosis related to energy drink intake. Circulation. (2012) 125:1447–8. doi: 10.1161/CIRCULATIONAHA.111.086017
9. Berger AJ, Alford K. Cardiac arrest in a young man following excess consumption of caffeinated “energy drinks”. Med J Aust. (2009) 190:41–3. doi: 10.5694/j.1326-5377.2009.tb02263.x
10. Cannon ME, Cooke CT, McCarthy JS. Caffeine-induced cardiac arrhythmia: an unrecognised danger of healthfood products. Med J Aust. (2001) 174:520–1. doi: 10.5694/j.1326-5377.2001.tb143404.x
11. Choudhury TR, Abdool MA, Galasko G. Energy drinks give you wings but also an abnormal exercise test. BMJ Case Rep. (2017) 2017:bcr2017220017. doi: 10.1136/bcr-2017-220017
12. Demir V, Celik Y, Hidayet S, Ede H, Turan Y. Coexistence of unstable angina pectoris and wolff-parkinson-white syndrome developed after consumption of energy drink. J Ankara Univer Fac Med. (2018) 71:184–7. doi: 10.4274/atfm.00710
13. Di Rocco JR, During A, Morelli PJ, Heyden M, Biancaniello TA. Atrial fibrillation in healthy adolescents after highly caffeinated beverage consumption: two case reports. J Med Case Rep. (2011) 5:18. doi: 10.1186/1752-1947-5-18
14. Dufendach KA, Horner JM, Cannon BC, Ackerman MJ. Congenital type 1 long QT syndrome unmasked by a highly caffeinated energy drink. Heart Rhythm. (2012) 9:285–8. doi: 10.1016/j.hrthm.2011.10.011
15. Enriquez A, Frankel DS. Arrhythmogenic effects of energy drinks. J Cardiovasc Electrophysiol. (2017) 28:711–7. doi: 10.1111/jce.13210
16. Hanan Israelit S, Strizevsky A, Raviv B. ST elevation myocardial infarction in a young patientafter ingestion of caffeinated energy drink and ecstasy. World J Emerg Med. (2012) 3:305–7. doi: 10.5847/wjem.j.issn.1920-8642.2012.04.012
17. Hernandez RJ, Thangam M, Anderson HV, Higgins JP. Coronary artery thrombosis associated with energy drink consumption. Imaging J Clin Medical Sci. (2016) 3:17–9. doi: 10.17352/2455-8702.000030
18. Kaoukis A, Panagopoulou V, Mojibian HR, Jacoby D. Reverse takotsubo cardiomyopathy associated with the consumption of an energy drink. Circulation. (2012) 125:1584–5. doi: 10.1161/CIRCULATIONAHA.111.057505
19. Khan R, Osman M, Zafar S, Sen S. Energy drink induced ventricular fibrillation and cardiac arrest: a successful outcome. J Med Cases. (2015) 6:409–12. doi: 10.14740/jmc2259w
20. Mattioli AV, Pennella S, Farinetti A, Manenti A. Energy drinks and atrial fibrillation in young adults. Clin Nutr. (2018) 37:1073–4. doi: 10.1016/j.clnu.2017.05.002
21. Mattioli AV, Pennella S, Manenti A, Farinetti A. Energy drink overconsumption can trigger atrial fibrillation. J Cardiovasc Med. (2016) 17:902–4. doi: 10.2459/JCM.0000000000000416
22. Mugmon M. Atrial flutter with aberrant conduction in a patient taking amphetamine salts and caffeine. J Community Hosp Intern Med Perspect. (2012) 1:10. doi: 10.3402/jchimp.v1i4.10663
23. Nagajothi N, Khraisat A, Velazquez-Cecena JL, Arora R, Raghunathan K, Patel R, et al. Energy drink-related supraventricular tachycardia. Am J Med. (2008) 121:e3–4. doi: 10.1016/j.amjmed.2007.12.003
24. Polat N, Ardic I, Akkoyun M, Vuruskan E. Spontaneous coronary artery dissection in a healthy adolescent following consumption of caffeinated “energy drinks”. Turk Kardiyol Dern Ars. (2013) 41:738–42. doi: 10.5543/tkda.2013.37542
25. Rottlaender D, Motloch LJ, Reda S, Larbig R, Hoppe UC. Cardiac arrest due to long QT syndrome associated with excessive consumption of energy drinks. Int J Cardiol. (2012) 158:e51–2. doi: 10.1016/j.ijcard.2011.10.017
26. Rutledge M, Witthed A, Khouzam RN. It took a RedBull to unmask brugada syndrome. Int J Cardiol. (2012) 161:e14–5. doi: 10.1016/j.ijcard.2012.03.095
27. Sattari M, Sattari A, Kazory A. Energy drink consumption and cardiac complications: a case for caution. J Addict Med. (2016) 10:280–2. doi: 10.1097/ADM.0000000000000234
28. Scott MJ, El-Hassan M, Khan AA. Myocardial infarction in a young adult following the consumption of a caffeinated energy drink. BMJ Case Rep. (2011) 2011:bcr0220113854. doi: 10.1136/bcr.02.2011.3854
29. Shah SA, Lacey CS, Bergendahl T, Kolasa M, Riddock IC. QTc interval prolongation with high dose energy drink consumption in a healthy volunteer. Int J Cardiol. (2014) 172:e336–7. doi: 10.1016/j.ijcard.2013.12.218
30. Solomin D, Borron SW, Watts SH. STEMI associated with overuse of energy drinks. Case Rep Emerg Med. (2015) 2015:537689. doi: 10.1155/2015/537689
31. Unal S, Sensoy B, Yilmaz S, Unal GG, Suleymanoglu M, Sen F, et al. Left main coronary artery thrombosis and acute anterior myocardial infarction related to energy drink. Int J Cardiol. (2015) 179:66–7. doi: 10.1016/j.ijcard.2014.10.073
32. Ullah MW, Lakhani S, Siddiq W, Handa A, Kahlon Y, Siddiqui T. Energy drinks and myocardial infarction. Cureus. (2018) 10:e2658. doi: 10.7759/cureus.2658
33. Ward AE, Lipshultz SE, Fisher SD. Energy drink-induced near-fatal ventricular arrhythmia prevented by an intracardiac defibrillator decades after operative “repair” of tetralogy of fallot. Am J Cardiol. (2014) 114:1124–5. doi: 10.1016/j.amjcard.2014.07.028
34. Wilson RE, Kado HS, Samson R, Miller AB. A case of caffeine-induced coronary artery vasospasm of a 17-year-old male. Cardiovasc Toxicol. (2012) 12:175–9. doi: 10.1007/s12012-011-9152-9
35. Zacher J, May E, Horlitz M, Pingel S. Binge drinking alcohol with caffeinated “energy drinks”, prolonged emesis and spontaneous coronary artery dissection: a case report, review of the literature and postulation of a pathomechanism. Clin Res Cardiol. (2018) 107:975–79. doi: 10.1007/s00392-018-1262-y
36. Alsunni A, Majeed F, Yar T, AlRahim A, Alhawaj AF, Alzaki M. Effects of energy drink consumption on corrected QT interval and heart rate variability in young obese Saudi male University students. Ann Saudi Med. (2015) 35:282–7. doi: 10.5144/0256-4947.2015.282
37. Arinc H, Sarli B, Baktir AO, Yolcu M, Ozyildirim S, Kayardi M, et al. Effects of single dose energy drink on QT and p-wave dispersion. Acta Med Anatol. (2013) 1:26–9. doi: 10.15824/actamedica.40460
38. Basrai M, Schweinlin A, Menzel J, Mielke H, Wikert C, Dusemund B, et al. Energy drinks induce acute cardiovascular and metabolic changes pointing to potential risks for young adults: a randomized controlled trial. J Nutr. (2019) 149:441–50. doi: 10.1093/jn/nxy303
39. Brothers RM, Christmas KM, Patik JC, Bhella PS. Heart rate, blood pressure and repolarization effects of an energy drink as compared to coffee. Clin Physiol Funct Imaging. (2017) 37:675–81. doi: 10.1111/cpf.12357
40. Elitok A, Oz F, Panc C, Sarikaya R, Sezikli S, et al. Acute effects of red bull energy drink on ventricular repolarization in healthy young volunteers: a prospective study. Anatol J Cardiol. (2015) 15:919–22. doi: 10.5152/akd.2015.5791
41. Fletcher EA, Lacey CS, Aaron M, Kolasa M, Occiano A, Shah SA. Randomized controlled trial of high-volume energy drink versus caffeine consumption on ECG and hemodynamic parameters. J Am Heart Assoc. (2017) 6:e004448. doi: 10.1161/JAHA.116.004448
42. Garcia A, Romero C, Arroyave C, Giraldo F, Sanchez L, Sanchez J. Acute effects of energy drinks in medical students. Eur J Nutr. (2017) 56:2081–91. doi: 10.1007/s00394-016-1246-5
43. Gray B, Ingles J, Medi C, Driscoll T, Semsarian C. Cardiovascular effects of energy drinks in familial long QT syndrome: a randomized cross-over study. Int J Cardiol. (2017) 231:150–4. doi: 10.1016/j.ijcard.2016.12.019
44. Hajsadeghi S, Mohammadpour F, Manteghi MJ, Kordshakeri K, Tokazebani M, Rahmani E, et al. Effects of energy drinks on blood pressure, heart rate, and electrocardiographic parameters: an experimental study on healthy young adults. Anatol J Cardiol. (2016) 16:94–9. doi: 10.5152/akd.2015.5930
45. Kozik TM, Shah S, Bhattacharyya M, Franklin TT, Connolly TF, Chien W, et al. Cardiovascular responses to energy drinks in a healthy population: the C-energy study. Am J Emerg Med. (2016) 34:1205–9. doi: 10.1016/j.ajem.2016.02.068
46. McGaughey TJ, Kelly SE, Williams B, et al. QTc prolongation with energy drinks comparable to moxifloxacin. Progr Pediatr Cardiol. (2018) 49:63–5. doi: 10.1016/j.ppedcard.2018.04.005
47. Ragsdale FR, Gronli TD, Batool N, Haight N, Mehaffey A, McMahon EC, et al. Effect of red bull energy drink on cardiovascular and renal function. Amino Acids. (2010) 38:1193–200. doi: 10.1007/s00726-009-0330-z
48. Shah R, Gholkar G, Steigerwalt S, Machado C. Evaluation of hemodynamic and electrocardiographic effects of an energy drink in healthy adults. J Innovat Card Rhythm Manage. (2016) 7:2330–5. doi: 10.19102/icrm.2016.070403
49. Shah SA, Dargush AE, Potts V, Lee M, Millard-Hasting BM, Williams B, et al. Effects of single and multiple energy shots on blood pressure and electrocardiographic parameters. Am J Cardiol. (2016) 117:465–8. doi: 10.1016/j.amjcard.2015.11.017
50. Shah SA, Occiano A, Nguyen TA, Chan A, Sky JC, Bhattacharyya M, et al. Electrocardiographic and blood pressure effects of energy drinks and panax ginseng in healthy volunteers: a randomized clinical trial. Int J Cardiol. (2016) 218:318–23. doi: 10.1016/j.ijcard.2016.05.007
51. Shah SA, Szeto AH, Farewell R, Shek A, Fan D, Quach KN, et al. Impact of high volume energy drink consumption on electrocardiographic and blood pressure parameters: a randomized trial. J Am Heart Assoc. (2019) 8:e011318. doi: 10.1161/JAHA.118.011318
52. Steinke L, Lanfear DE, Dhanapal V, Kalus JS. Effect of “energy drink” consumption on hemodynamic and electrocardiographic parameters in healthy young adults. Ann Pharmacother. (2009) 43:596–602. doi: 10.1345/aph.1L614
53. Tauseef A, Akmal A, Hasan S, Waheed A, Zafar A, Cheema A, et al. Effect of energy drink on reaction time, haemodynamic and electrocardiographic parameters. Pak J Physiol. (2017) 13:7–10.
54. Wiklund U, Karlsson M, Ostrom M, Messner T. Influence of energy drinks and alcohol on post-exercise heart rate recovery and heart rate variability. Clin Physiol Funct Imaging. (2009) 29:74–80. doi: 10.1111/j.1475-097X.2008.00837.x
55. U.S. Food & Drug Administration. E14 Clinical Evaluation of of QT/QTc Interval Prolongation and Proarrhythmic Potential for Non-Antiarrhythmic Drugs. Available online at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/e14-clinical-evaluation-qtqtc-interval-prolongation-and-proarrhythmic-potential-non-antiarrhythmic-0 (accessed August 13, 2019).
56. Pfizer Laboratories Div Fizer Inc. Zithromax Prescribing Information. Available online at: http://labeling.pfizer.com/ShowLabeling.aspx?id=511 (accessed August 13, 2019).
57. Eckart RE, Shry EA, Burke AP, McNear JA, Appel DA, Castillo-Rojas LM, et al. Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. J Am Coll Cardiol. (2011) 58:1254–61. doi: 10.1016/j.jacc.2011.01.049
58. Nielsen JB, Graff C, Rasmussen PV, Pietersen A, Lind B, Olesen MS, et al. Risk prediction of cardiovascular death based on the QTc interval: evaluating age and gender differences in a large primary care population. Eur Heart J. (2014) 35:1335–44. doi: 10.1093/eurheartj/ehu081
59. Olas B, Brys M. Effects of coffee, energy drinks and their components on hemostasis: the hypothetical mechanisms of their action. Food Chem Toxicol. (2019) 127:31–41. doi: 10.1016/j.fct.2019.02.039
60. Omran J, Firwana B, Koerber S, Bostick B, Alpert MA. Effect of obesity and weight loss on ventricular repolarization: a systematic review and meta-analysis. Obes Rev. (2016) 17:520–30. doi: 10.1111/obr.12390
61. Ammar R, Song JC, Kluger J, White CM. Evaluation of electrocardiographic and hemodynamic effects of caffeine with acute dosing in healthy volunteers. Pharmacotherapy. (2001) 21:437–42. doi: 10.1592/phco.21.5.437.34502
62. Pelchovitz DJ, Goldberger JJ. Caffeine and cardiac arrhythmias: a review of the evidence. Am J Med. (2011) 124:284–9. doi: 10.1016/j.amjmed.2010.10.017
63. Vandenberk B, Vandael E, Robyns T, Vandenberghe J, Garweg C, Foulon V, et al. Which QT correction formulae to use for QT monitoring? J Am Heart Assoc. (2016) 5:e003264. doi: 10.1161/JAHA.116.003264
64. Committee on Nutrition and the Council on Sports Medicine and Fitness. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. (2011) 127:1182–9. doi: 10.1542/peds.2011-0965
65. Mitka M. Hearing raises questions on energy drink marketing. JAMA. (2013) 310:1015. doi: 10.1001/jama.2013.277676
66. Thrastardottir A. A Country in Europe Bans Energy Drinks for Minors. Available online at: https://www.businessinsider.com/lithuania-bans-energy-drinks-for-minors-2014-11 (accessed August 8, 2019).
67. Energy Drinks Europe. Regulation. Available online at: http://www.energydrinkseurope.org/regulation/ (accessed August 8, 2019).
68. American Beverage Association. ABA Guidance for the Responsible Labeling and Marketing of Energy Drinks. Available online at https://www.ameribev.org/files/resources/2014-energy-drinks-guidance-approved-by-bod-43020c.pdf (accessed August 8, 2019).
69. Lévy S, Santini L, Capucci A, Oto A, Santomauro M, Riganti C, et al. European cardiac arrhythmia society statement on the cardiovascular events associated with the use or abuse of energy drinks. J Interv Card Electrophysiol. (2019) 56:99–115. doi: 10.1007/s10840-019-00610-2
70. Piccioni A, Covino M, Zanza C, Longhitano Y, Tullo G, Bonadia N, et al. Energy drinks: a narrative review of their physiological and pathological effects Intern Med J. (2020) 51:636–46. doi: 10.1111/imj.14881
71. Center for Science in the Public Interest. Caffeine Chart. Available online at https://cspinet.org/eating-healthy/ingredients-of-concern/caffeine-chart (accessed April 11, 2021).
Keywords: energy drinks, electrophysiology, arrhythmia, ischemia, adverse effects
Citation: Cao DX, Maiton K, Nasir JM, Estes NAM and Shah SA (2021) Energy Drink-Associated Electrophysiological and Ischemic Abnormalities: A Narrative Review. Front. Cardiovasc. Med. 8:679105. doi: 10.3389/fcvm.2021.679105
Received: 11 March 2021; Accepted: 12 May 2021;
Published: 01 July 2021.
Edited by:
Maurizio Acampa, Siena University Hospital, ItalyReviewed by:
Marina Cerrone, New York University, United StatesCopyright © 2021 Cao, Maiton, Nasir, Estes and Shah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sachin A. Shah, c3NoYWhAcGFjaWZpYy5lZHU=; orcid.org/0000-0001-5850-1113
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.