- 1Leviev Heart Center, Sackler School of Medicine, Tel Aviv University, Tel Aviv, Israel
- 2Laboratory for Industrial and Applied Mathematics, Department of Mathematics and Statistics, Centre for Disease Modelling, York University, Toronto, ON, Canada
- 3St George's Hospital Medical School, University of London, London, United Kingdom
- 4Heart Research Follow-Up Program, University of Rochester Medical Center, Rochester, NY, United States
- 5Department of Cardiology, Cardiovascular Research Institute Maastricht, Maastricht University Medical Center, Maastricht, Netherlands
Background: Long-term morbidity and mortality data among ischemic heart disease (IHD) patients of different ethnicities are conflicting. We sought to determine the independent association of ethnicity and all-cause mortality over two decades of follow-up of Israeli patients.
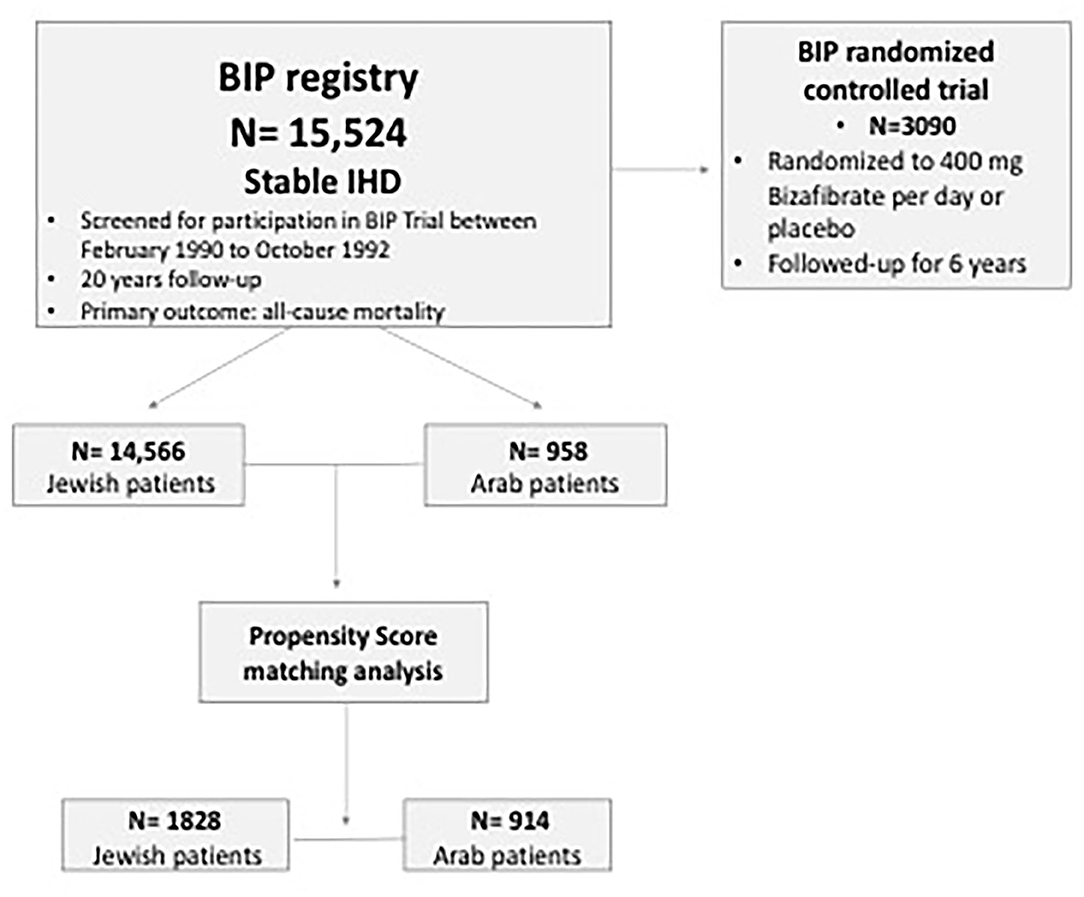
Methods: Our study comprised 15,524 patients including 958 (6%) Arab patients who had been previously enrolled in the Bezafibrate Infarction Prevention (BIP) registry between February 1, 1990, and October 31, 1992, and subsequently followed-up for long-term mortality. We compared clinical characteristics and outcomes of Israeli Arabs and Jews. Propensity score matching (PSM) (1:2 ratios) was used for validation.
Results: Arab patients were significantly younger (56 ± 7 years vs. 60 ± 7 years; p < 0.001; respectively), and had more cardiovascular disease (CVD) risk factors. Kaplan-Meier survival analysis showed that all-cause mortality was significantly higher among Arab patients (67 vs. 61%; log-rank p < 0.001). Multivariate adjusted analysis showed that mortality risk was 49% greater (HR 1.49; 95% CI: 1.37–1.62; p < 0.001) among Arabs.
Conclusions: Arab ethnicity is independently associated with an increased 20-year all-cause mortality among patients with established IHD.
Introduction
Despite the latest medical achievements, ischemic heart disease (IHD) continues to be a leading cause of death in some of middle and high-income countries (1). In Israel, IHD is the second leading cause of death (2). Several studies reported ethnic disparities in presentation and outcome of cardiovascular diseases over the world which have been attributed to variability in prevalence of cardiovascular risk factors, differences in screening for primary prevention as well as poor health literacy, health care seeking behaviors and compliance to treatment among specific ethnicities (3, 4).
Jews constitute the majority of Israeli citizens (74.7%) while Arabs are a sizable minority of the whole population (20.8%) (5). Interestingly, genetic studies suggest common genetic features of Arabs and Jews demonstrated by remarkable similarity in Y-chromosome haplotype composition and average frequency (6). Yet, there are major differences seen in some disorders that are typical for each group members (7, 8). National studies have shown conflicting results in the role of ethnicity in cardiovascular diseases (CVD) outcomes. Some showed an increased mortality among Arabs following acute myocardial infarction (9) and greater frequency of non-ischemic cardiomyopathy as well as of sudden cardiac death, while others showed no difference (10, 11). We hypothesized that Israeli Arabs and Jews with established IHD may have diverse characteristics due to differences in their environmental and socioeconomic background. Accordingly, we aimed to evaluate these differences and to assess their impact on long-term all-cause mortality.
Methods
Study Population
The present study population comprised patients who were screened for participation in the prospective multicenter randomized Bezafibrate Infarction Prevention (BIP) trial from February 1990 to October 1992 and enrolled in the BIP Registry. The design and rationale of the BIP Registry and study were published previously (12–14). Briefly, the BIP Registry included 15,524 patients aged 40–74 years with stable IHD. Of these patients, 20% were enrolled in the randomized prospective interventional 6-year BIP study that compared Bezafibrate to placebo (Figure 1). Major exclusion criteria for the BIP study were permanent pacemaker implantation, chronic hepatic or chronic kidney disease (CKD) (GFR < 60 mL/min/1.73 m2 or Creatinine >2 mg/dl), peripheral vascular disease, malignant diseases, and type 1 diabetes mellitus.
The study was approved by our institute's internal review board and was performed according to the principles expressed in the Declaration of Helsinki and the ethics policy of the institute and patients signed an informed consent upon their enrollment.
Definitions and Endpoints
Ethnic Groups
Ethnic groups were categorized according to the Statistical Abstract of Israel 2020 (15): Jews and Arabs. Arabs included Muslims (including Circassians), Arab Christians (including Armenians), Arab Druze and others (non-Arab Christians, members of other religions, and not classified by religion).
Primary End Point
The primary end point of this study was all-cause mortality.
Statistical Analysis
Variables were expressed as means ± standard deviation (SD) or median and inter-quartile range (IQR). Categorical data were summarized as numbers and percentages. The demographic, clinical characteristics and laboratory values of patients at baseline according to the pre-specified groups were compared with the use of the t-test for continuous variables normally distributed and the Mann-Whitney test for a parametric comparison, the chi-square test was performed to compare categorical variables.
Kaplan–Meier survival analysis was used to estimate survival of subjects among the groups. The subsequent long-term survival probability, was compared using the Log rank test. Univariate and multivariate Cox proportional hazard (PH) regression modeling was used to assess the association between ethnicity and long-term mortality. This was adjusted for different covariates.
In addition, Propensity score matching (1:2 ratio) analysis was constructed from patient's characteristics to control for substantial difference between study groups. Using logistic regression model, we computed conditional probability for each subject to be in the Arab group using multiple covariate and explanatory variables (Supplementary Table 1).
We also performed a sensitivity analysis excluding subjects randomized to the BIP study (n = 3,090).
Statistical significance was accepted as two-sided p < 0.05. Statistical analysis was performed with IBM SPSS version 20·0 (Chicago, IL, USA) R programming.
Results
Clinical Characteristics
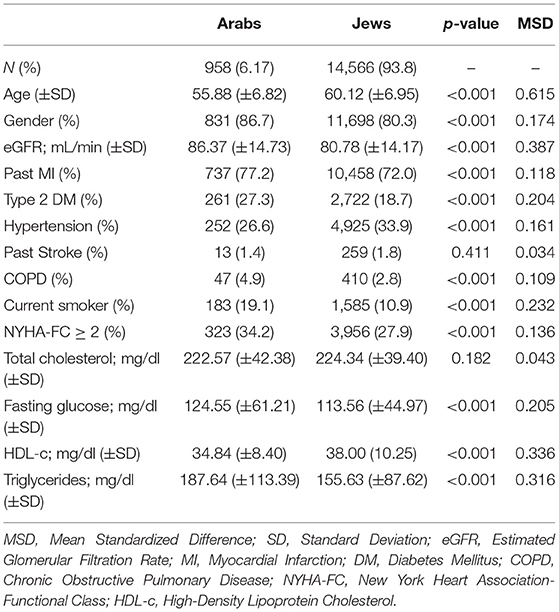
Our current study population comprised 15,524 patients aged 59 ± 6 years, of whom 80.7% were males. The vast majority of patients were Jews [14,566 subjects (93.8%)] while only 6.17% (958 subjects) were Arabs. The baseline characteristics of patients by ethnic origin are summarized in Table 1.
Notably, Arabs patients were significantly younger than Jews (56 ± 7 years vs. 60 ± 7 years), had higher prevalence of CVD risk factors, higher rates of previous myocardial infarction as well as lower functional status according to New York Heart Association (NYHA). In fact, Arabs were active smokers almost twice the amount compared to Jews (19.1 vs. 10.9%; p < 0.001). Arab patients were also found to have higher prevalence of diabetes (27.3 vs. 18.7%; p < 0.001), prior myocardial infarction (77.2 vs. 72%; p = 0.001), chronic obstructive pulmonary disease (4.9 vs. 2.8%; p < 0.001), and suffered more from congestive heart failure (NYHA ≥ 2: 34.2 vs. 27.9%; p < 0.001).
Primary Outcome
Kaplan-Meier survival analysis showed significantly higher all-cause mortality among Arabs throughout a 20-years follow up, reaching mortality rates of 67% (n = 631) compared to 62% (n = 8,893) (Arabs vs. Jews, log-rank p < 0.001) (Figure 2A).

Figure 2. (A) Kaplan-Meier of 20-year survival estimates for the entire cohort according to ethnicity. (B) Kaplan-Meier of 20-year survival estimates for the propensity score matched cohort according to ethnicity.
Accordingly, multivariate analysis showed that Arab ethnicity remained a significant cause for total mortality, with a hazard ratio of 1.49 (95% CI: 1.37–1.62; p < 0.001). Other significant factors are shown in Supplementary Table 1.
Propensity Score Matching
Following further adjustments using propensity score matching (Supplementary Table 2), the survival rates of Arabs remained lower compared to Jews (Figure 2B). In order to avoid statistical bias, we further performed a sensitivity analysis excluding patients enrolled into the BIP randomized trial (Figure 1). Similar results were likewise obtained.
Subgroup Analysis
We further explored the independent association between Arab ethnicity and long-term mortality in pre-defined subgroups of patients (Figure 3). This analysis showed that HR for mortality was 1.34 (95% CI: 1.23–1.47) in subjects aged equal to or <65 years vs. HR of 1.71 (95% CI: 1.40–2.10) in individuals aged >65 years (p-value for interaction 0.033). HR for mortality was 1.29 (95% CI: 1.17–1.41) in people with BMI equal to or >30 kg/m2 vs. HR of 0.93 (95% CI: 0.79–1.10) in those with BMI < 30 kg/m2 (p-value for interaction 0.01). Finally, HR for mortality was 1.26 (95% CI: 1.15–1.38) in those with a past history of MI vs. HR of 0.99 (95% CI: 0.82–1.19) in those without a history of MI (p-value for interaction 0.02). Gender (p-value for interaction 0.676), smoking status (p-value for interaction 0.847), DM (p-value for interaction 0.188), hypertension (p-value for interaction 0.685) and creatinine (p-value for interaction 0.144) did not achieve statistical significance.
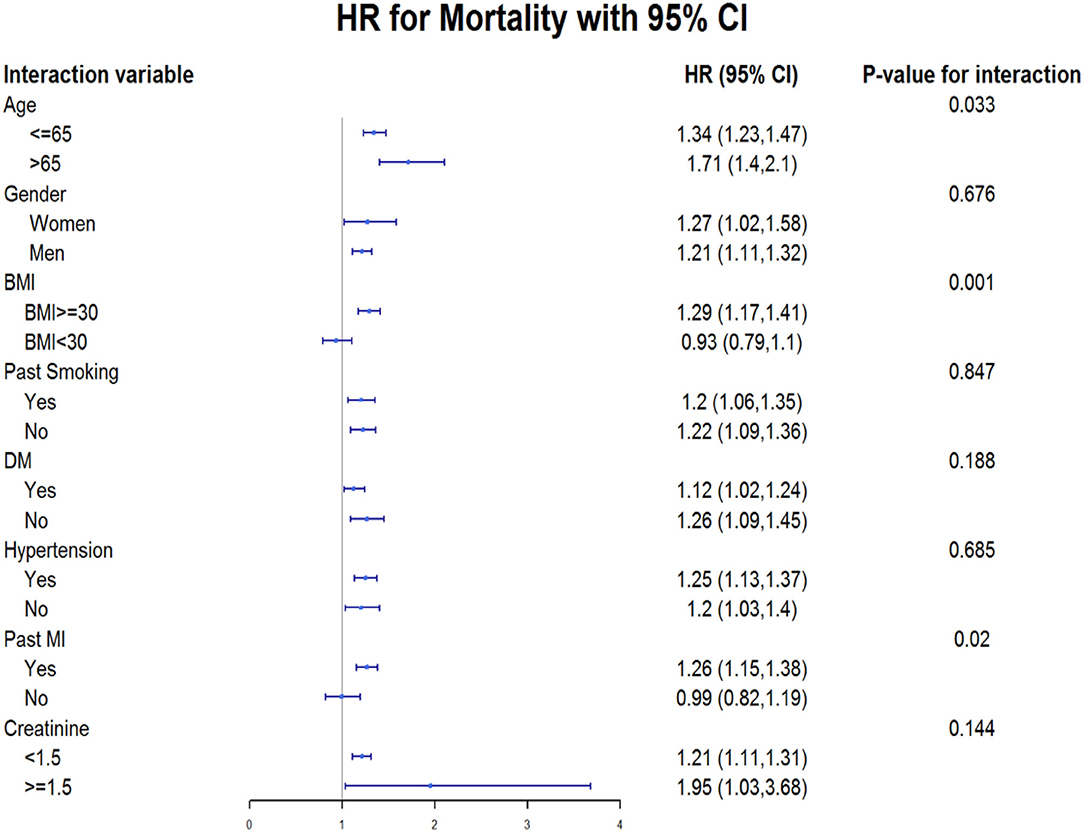
Figure 3. Subgroup analysis predicting the association between 20-year all-cause mortality and Arab ethnicity. HR, Hazard Ratio; CI, Confidence Interval; BMI, Body Mass Index; DM, Diabetes Mellitus; MI, Myocardial Infarction.
Discussion
To the best of our knowledge, this study entailed the largest Israeli national sample of IHD patients evaluating ethnic disparities and assessing their impact on clinical outcomes throughout a span of time longer than 20 years.
The findings of our study can be summarized as follow:
1. The study identified Arab ethnicity as an independent risk for all-cause mortality among patients with IHD.
2. Survival rates remained lower among Arabs throughout the follow-up period.
3. Arabs with IHD are younger compared to Jews and have higher rates of previous myocardial infarction.
4. Arabs were found to have more CVD risk factors including diabetes, high triglycerides levels, high BMI, low HDL levels, and higher smoking rates.
Despite the genetic affinities between Jews and Arabs, disparities in mortality have been reported. A previous study found that Israeli Arabs had 1.4-times greater all-cause mortality during a relatively short term follow up of 1 year. Death rate was 1.8-times higher due to heart diseases, doubled higher due to diabetes mellitus and 1.7-times greater due to cerebrovascular diseases (16). In contrast to these reports, other studies (10, 11) failed to detect any mortality differences.
For example, Gotsman et al. explored the differences in heart failure patients. Their study included 6,773 patients and found no differences in mortality. They, however, reported that Arab males had higher rates of cardiac-related hospitalizations and death (10). Our study reported on significant higher mortality rates in a much larger patient population. In contrast to previous studies which had a limited follow up of 12–18 months, our study continued for more than two decades. We show here for the first time that the differences in overall mortality persisted throughout the entire follow up period.
Potential Contributing Factors
Diabetes, Obesity, and Metabolic Syndrome
In keeping with previous studies (10), we also report higher rates of classic CVD risk factors including diabetes and obesity in the Arab population. In fact, Arabs are diagnosed with diabetes 10 years earlier compared to Jew (17, 18). This could be attributed to genetic factors, lower socio-economic status, in addition to consumption of unhealthy diet and lower level of physical activity (18). Furthermore, Arabs have higher BMI values especially among women (17, 19) as well as higher prevalence (70%) of metabolic syndrome among obese population (20). Similar findings were also shown in a study of the pediatric population, where obesity and overweight were higher among Arab children across all age groups compared to Jewish children (21). As metabolic syndrome and diabetes are major contributors to all-cause mortality and cardiovascular mortality in the long term (22), the above mentioned could explain the differences in mortality trends demonstrated in our study.
Cigarette Smoking
In 2014, the Israeli Ministry of Health reported higher prevalence of smoking among Arab men in Israel (46%), and similar rates persisted over the past decade. In contrast, smoking among Jewish men has declined by 48% over the last 30 years (to ~20% in 2014) (23). Those observations are highlighted by our study, where Arabs were found to be more active smokers than Jews. Despite education, data suggests that Arabs are less likely to quit smoking. It could be that other advanced measures should be taken in the Arab population, addressing cultural complexity (24).
Coronary Artery Disease
Several previous reports showed that Arabs presented at a younger age with acute myocardial infarction or heart failure (9–11, 25). This is consistent with our data, showing that history of myocardial infarction was more prevalent among Arabs during study enrollment. Thus, suggesting that early onset of coronary artery disease (25) may eventually lead to premature death. Other studies involving the Arab population in other countries reported similar results (25, 26). These data might imply genetic factors as contributing to accelerated atherosclerosis rather than environmental factors (27).
A possible mechanistic explanation for the above findings may be attributed to higher levels of GlycA in Palestinians compared to Israelis living in Jerusalem (21). This is a novel biomarker of systemic inflammation (28) that has been shown to predict cardiovascular diseases and is associated with increased risk for all-cause and cardiovascular mortality (21). Further studies are needed for wider validation of this theory.
Adherence to Medical Treatment and Advice
Our study and other studies (10) report that both glucose and lipid profiles were consistently higher in Arabs as compared to Jews. This finding might be related to different response to medication, but could also be attributed to lower compliance rates among Arabs. Ethnic disparity in adherence to medication was previously described. Minorities (Asians, Hispanics, Native Americans, and African Americans) were less adherent to heart failure medications even after adjusting for income and drug coverage (29), a factor that might serve as possible explanation for dissimilarities in outcomes. In addition, Arabs participate less in cardiac prevention and rehabilitation programs following acute coronary syndrome, a fact that could further contribute to our findings (30).
Socioeconomic Status and Access to Medical Therapy
The Arab has a lower income per capita compared to the Jewish population (31) and is generally defined as a “lower socioeconomic status community” in Israel. Interestingly, socioeconomic deprivation has been linked to high incidence of heart failure as well as poor outcomes regardless of cardiovascular risk factors (32). This correlation could be attributed to decreased access to healthcare services, transportation cost, inequalities in treatment and lower affordability of medications (32, 33). This interesting finding was also observed among hypertrophic cardiomyopathy patients (34).
Limitations
This is a retrospective analysis of a prospective study. Possible unmeasured confounders such as socioeconomic status, may have biased the results; therefore, our results should be interpreted as hypothesis generating. In order to minimize this bias, we performed PSM as well as sensitivity analysis. Despite the many advantages of using long-term data from randomized controlled trials, patients from these trials may do better than real world patients. Thus, our results may not be applicable to elderly (age >80 years) or those with advance renal dysfunction (GFR < 60 mL/min/1.73 m2 or Creatinine >2mg/dl) which have been excluded from the beginning. Furthermore, our study doesn't include cardiovascular outcomes and instead, it included only all-cause mortality as the only available long-term outcome in the BIP-study. This fact limits our ability to imply a cardiovascular etiology to patient's outcomes.
Conclusions
Arab Ethnicity is independently associated with increased 20-year all-cause mortality in patients with stable CAD. This association was consistent even after performing a propensity score matching. Different factors, that included early development of diabetes and obesity, cigarette smoking and premature CAD were highly correlated with the poor outcome. Intensive screening and prevention programs are needed to address those factors early in adulthood.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by IRB Sheba Center, Tel Aviv University, Tel Aviv, Israel. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AA-M and RB conceived the study and drafted the study. NS, EN, and NB analyzed data. EN, AnY, DH, ArY, NS, AF, IG, and RK critically revised the paper. All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.661390/full#supplementary-material
References
1. World Health Organization. The Top 10 Causes of Death, Fact Sheet. World Health Organization (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
2. Goldberger N, Aburbeh M, Haklai Z. Leading Causes of Death in Israel 2000-2014. Jerusalem: Ministry of Health Israel (2017).
3. Dégano IR, Salomaa V, Veronesi G, Ferriéres J, Kirchberger I, Laks T, et al. Twenty-five-year trends in myocardial infarction attack and mortality rates, and case-fatality, in six European populations. Heart. (2015) 101:1413–21. doi: 10.1136/heartjnl-2014-307310
4. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am College Cardiol. (2014) 64:337–45. doi: 10.1016/j.jacc.2014.04.054
5. On the Eve of Israel's 69th Independence Day −8.7 Million Residents in the State of Israel, Jerusalem: Central Bureau of Statistics Israel (2017).
6. Hammer MF, Redd AJ, Wood ET, Bonner MR, Jarjanazi H, Karafet T, et al. Jewish and Middle Eastern non-Jewish populations share a common pool of Y-chromosome biallelic haplotypes. Proc Natl Acad Sci USA. (2000) 97:6769–74. doi: 10.1073/pnas.100115997
7. Gross SJ, Pletcher BA, Monaghan KG. Carrier screening in individuals of Ashkenazi Jewish descent. Genet Med. (2008) 10:54–6. doi: 10.1097/GIM.0b013e31815f247c
8. Zayed H. Krabbe disease in the Arab world. J Pediatr Genet. (2015) 04:001–8. doi: 10.1055/s-0035-1554981
9. The Sprint Study Group. Ethnic differences in mortality of male and female patients surviving acute myocardial infarction: long-term follow-up of 5,700 patients. The secondary prevention reinfarction israeli nifedipine trial (SPRINT) study Group. Eur J Epidemiol. (1997) 13:745–54.
10. Gotsman I, Avishai-Eliner S, Jabara R, Zemora Z, Shauer A, Lotan C, et al. Ethnic disparity in the clinical characteristics of patients with heart failure: ethnic disparity in heart failure. Eur J Heart Fail. (2015) 17:801–8. doi: 10.1002/ejhf.285
11. Plakht Y, Gilutz H, Shiyovich A. Ethnical disparities in temporal trends of acute myocardial infarction (AMI) throughout a decade in Israel. Soroka acute myocardial infarction (SAMI-II) project. Int J Cardiol. (2016) 214:469–76. doi: 10.1016/j.ijcard.2016.04.009
12. Bezafibrate Infarction Prevention (BIP) study. Secondary prevention by raising HDL cholesterol and reducing triglycerides in patients with coronary artery disease. Circulation. (2000) 102:21–7. doi: 10.1161/01.CIR.102.1.21
13. Lipids and lipoproteins in symptomatic coronary heart disease. Distribution, intercorrelations, and significance for risk classification in 6,700 men and 1,500 women. The Bezafibrate Infarction Prevention (BIP) Study Group, Israel. Circulation. (1992) 86:839–48. doi: 10.1161/01.CIR.86.3.839
14. Goldbourt U, Brunner D, Behar S, Reicher-Reiss H. Baseline characteristics of patients participating in the Bezafibrate infarction prevention (BIP) study. Eur Heart J. (1998) 19 (Suppl. H):H42–7.
15. Central Bureau of Statistics Israel. Statistical Abstract of Israel 2020. Jerusalem: Central Bureau of Statistics Israel (2020).
16. Ministry of Health in Israel. Leading Causes of Death in Israel 2000 – 2015. Jerusalem: Ministry of Health in Israel (2018).
17. Kalter-Leibovici O, Chetrit A, Lubin F, Atamna A, Alpert G, Ziv A, et al. Adult-onset diabetes among Arabs and Jews in Israel: a population-based study: adult-onset diabetes among Arabs and Jews in Israel. Diabetic Med. (2012) 29:748–54. doi: 10.1111/j.1464-5491.2011.03516.x
18. Jaffe A, Giveon S, Wulffhart L, Oberman B, Baidousi M, Ziv A, et al. Adult Arabs have higher risk for diabetes mellitus than Jews in Israel. PLoS ONE. (2017) 12:e0176661. doi: 10.1371/journal.pone.0176661
19. Keinan-Boker L, Noyman N, Chinich A, Green MS, Nitzan-Kaluski D. Overweight and obesity prevalence in Israel: findings of the first national health and nutrition survey (MABAT). Isr Med Assoc J. (2005) 7:219–23.
20. Abdul-Ghani MA, Sabbah M, Muati B, Dakwar N, Kashkosh H, Minuchin O, et al. High frequency of pre-diabetes, undiagnosed diabetes and metabolic syndrome among overweight Arabs in Israel. Isr Med Assoc J. (2005) 7:143–7.
21. Ram E, Marcus O, Joubran S, Abdo B, Asal NR. Prevalence of obesity among Arab school children in Nazareth, Israel: comparison with national (Jewish) and international data: obesity among Arab children in Nazareth. Pediatric Obesity. (2013) 8:428–38. doi: 10.1111/j.2047-6310.2012.00128.x
22. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. (2005) 28:1769–78. doi: 10.2337/diacare.28.7.1769
23. Minister of Health Report on Smoking in Israel in 2015 Jerusalem: Ministry of Health Israel (2016).
24. Daoud N, Hayek S, Sheikh Muhammad A, Abu-Saad K, Osman A, Thrasher JF, et al. Stages of change of the readiness to quit smoking among a random sample of minority Arab -male smokers in Israel. BMC Public Health. (2015) 15:672. doi: 10.1186/s12889-015-1950-8
25. Kark JD, Fink R, Adler B, Goldberger N, Goldman S. The incidence of coronary heart disease among Palestinians and Israelis in Jerusalem. Int J Epidemiol. (2006) 35:448–57. doi: 10.1093/ije/dyl012
26. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. (2004) 364:937–52. doi: 10.1016/S0140-6736(04)17018-9
27. Joseph PG, Pare G, Asma S, Engert JC, Yusuf S, Anand SS. Impact of a genetic risk score on myocardial infarction risk across different ethnic populations. Can J Cardiol. (2016) 32:1440–6. doi: 10.1016/j.cjca.2016.05.014
28. Gruppen EG, Riphagen IJ, Connelly MA, Otvos JD, Bakker SJL, Dullaart RPF. GlycA, a pro-inflammatory glycoprotein biomarker, and incident cardiovascular disease: relationship with C-reactive protein and renal function. PLoS ONE. (2015) 10:e0139057. doi: 10.1371/journal.pone.0139057
29. Zhang Y, Baik SH. Race/ethnicity, disability, and medication adherence among medicare beneficiaries with heart failure. J Gen Intern Med. (2014) 29:602–7. doi: 10.1007/s11606-013-2692-x
30. Reges O, Vilchinsky N, Leibowitz M, Khaskia A, Mosseri M, Kark JD. Change in health behaviours following acute coronary syndrome: Arab–Jewish differences. Eur J Prev Cardiolog. (2015) 22:458–67. doi: 10.1177/2047487314520924
31. Bleikh H. Poverty and Inequality in Israel: Trends and Decompositions-State of the Nation Report: Society, Economy and Policy, Jerusalem: Taub Center (2016).
32. Hawkins NM, Jhund PS, McMurray JJV, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. (2012) 14:138–46. doi: 10.1093/eurjhf/hfr168
33. Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. (2014) 371:818–27. doi: 10.1056/NEJMoa1311890
Keywords: ischemic heart disease, ethnicity, all-cause mortality, disparity, heart disease
Citation: Abu-Much A, Nof E, Bragazzi NL, Younis A, Hochstein D, Younis A, Shlomo N, Fardman A, Goldenberg I, Klempfner R and Beinart R (2021) Ethnic Disparity in Mortality Among Ischemic Heart Disease Patients. A-20 Years Outcome Study From Israel. Front. Cardiovasc. Med. 8:661390. doi: 10.3389/fcvm.2021.661390
Received: 30 January 2021; Accepted: 07 June 2021;
Published: 30 June 2021.
Edited by:
Hack-Lyoung Kim, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, South KoreaReviewed by:
Sang-Ho Jo, Hallym University Sacred Heart Hospital, South KoreaMinkwan Kim, Yonsei University, South Korea
Copyright © 2021 Abu-Much, Nof, Bragazzi, Younis, Hochstein, Younis, Shlomo, Fardman, Goldenberg, Klempfner and Beinart. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arsalan Abu-Much, YXJzYWxhbmFidW11Y2gxQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Arsalan Abu-Much
Arsalan Abu-Much Eyal Nof1†
Eyal Nof1† Nicola Luigi Bragazzi
Nicola Luigi Bragazzi David Hochstein
David Hochstein