
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 18 February 2021
Sec. General Cardiovascular Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.630816
This article is part of the Research TopicHighlights in General Cardiovascular Medicine: 2021View all 12 articles
Background: Knowledge of the impact of the 2019 novel coronavirus disease (COVID-19) pandemic on the performance of a cardiovascular department in a medical referral hub center from a non-epidemic area of China is limited.
Method: The data on the total number of non-emergency medical cares (including the number of out-patient clinic attendances, the number of patients who were hospitalized in non-intensive care wards, and patients who underwent elective cardiac intervention procedures) and emergency medical cares [including the number of emergency department (ED attendances) and chest pain center (CPC attendances), as well as the number of patients who were hospitalized in coronary care unit (CCU) and the number of patients who underwent emergency cardiac intervention procedures] before and during the pandemic (time before the pandemic: 20th January 2019 to 31st March 2019 and time during the pandemic: 20th January 2020 to 31st March 2020) in the Department of Cardiology and Macrovascular Disease, Beijing Tiantan Hospital, Capital Medical University were collected and compared.
Results: Both the non-emergency medical and emergency medical cares were affected by the pandemic. The total number of out-patient clinic attendance decreased by 44.8% and the total number of patients who were hospitalized in non-intensive care wards decreased by 56.4%. Pearson correlation analysis showed that the number of out-patient clinic attendance per day was not associated with the number of new confirmed COVID-19 cases and the cumulative number of confirmed COVID-19 patients in Beijing (r = −0.080, p = 0.506 and r = −0.071, p = 0.552, respectively). The total number of patients who underwent non-emergency cardiac intervention procedures decreased during the pandemic, although there were no statistically significant differences except for patent foramen ovale (PFO) occlusion (1.7 ± 2.9 vs. 8.3 ± 2.3, p = 0.035). As for the emergency medical cares, the ED attendances decreased by 22.4%, the total number of CPC attendances increased by 10.3%, and the number of patients who were hospitalized in CCU increased by 8.9%: these differences were not statistically significant. During the pandemic, the proportion of hospitalized patients with ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI) significantly increased (19.0 vs. 8.7%, p < 0.001; 28.8 vs. 18.0%, p < 0.001, respectively); also, the number of primary percutaneous coronary intervention (PCI) increased by 10.3%. There was no significant difference between patients before and during the pandemic regarding the age, gender, baseline and discharge medication therapy, as well as length of stay and in-hospital mortality.
Conclusions: Our preliminary results demonstrate that both the non-emergency and emergency medical cares were affected by the COVID-19 pandemic even in a referral medical center with low cross-infection risk. The number of the out-patient clinic attendances not associated with the number of confirmed COVID-19 cases could be due to different factors, such as the local government contamination measures. The proportion of hospitalized patients with acute myocardial infarction increased in our center during the pandemic since other hospitals stopped performing primary angioplasty. A hub-and-spoke model could be effective in limiting the collateral damage for patients affected by cardiovascular diseases when the medical system is stressed by disasters, such as COVID-19 pandemic.
The 2019 novel coronavirus disease (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), has become a global pandemic since March 2020 (1), compromising the normal performance of health-care facilities in different aspects (2–5). Patients with acute or chronic cardiovascular diseases (CVD) encountered difficulties during this historical pandemic (6–9). Actually, a significant reduction of patient admissions due to different types of CVDs was observed (10–13).
Compared with other regions like Hubei province with high risk of cross-infection, the overall risk of cross-infection in Beijing was relatively low (the total number people who lives in Beijing is more than 20 million and the total confirmed number of COVID-19 infection was 580 by 31st March 2020). The reason for the lack of involvement by the pandemic in Beijing is largely attributed to the strict counter-contamination measures that local government applied during the pandemic. Those measures included wearing masks; closing public places such as restaurants, theaters, and clubs; encouraging telecommuting; etc. Most of the hospitals in Beijing stopped performing primary percutaneous coronary intervention (PCI) considering the possible risk of cross-infection. Our hospital, however, continued to perform primary PCI because we were relatively far from the center of Beijing.
Beijing Tiantan Hospital, Capital Medical University is a local medical referral center in the southwest of Beijing, with 1,650 beds; there are more than 400 out-patient clinic attendances in the Department of Cardiology and Macrovascular Disease per day, with 99 beds (including coronary care unit, CCU). We applied a detailed cardiovascular disease management system, which has been reported elsewhere for non-emergency and emergency medical cares (14, 15). In particular, patients without signs of infection and without medical contact history could receive medical service as usual after checking their body temperature. For patients with infection symptoms or with medical contact history, an isolated clinic room was prepared for them. Emergency cardiac intervention procedures like primary PCI were performed after the patients performed blood routine tests, chest computed tomography, and nucleic acid tests. For hemodynamically unstable critical patients, isolated patient wards were prepared for them before they finished the screening tests and fibrinolysis therapy was recommended for ST segment elevation myocardial infarction (STEMI) patients. None of the critical patients were hospitalized in our center during the pandemic. Hospitalized patients were also required to finish these tests before hospitalization.
Previous studies have evaluated the impact of the COVID-19 pandemic on the management of patients with CVD and acute myocardial infarction (AMI) (16–19). However, the impact of the COVID-19 pandemic on the standard performance of cardiovascular departments in hub-and-spoke organization systems, moreover in non-epidemic centers, has not been systemically evaluated so far. In this study, we investigated the impact of the COVID-19 pandemic on the normal performance of a cardiovascular department in a large non-epidemic hub center from Beijing, China.
In this single-center, retrospective, observational study, data on out-patient clinic attendances, emergency department (ED) attendances, chest pain center (CPC) attendances, patients who were hospitalized in our department, and patients who underwent non-emergency and emergency cardiac intervention procedures in the Department of Cardiology and Macrovascular Disease, Beijing Tiantan Hospital, Capital Medical University, which was a referral hub center for primary PCI, before and during the pandemic were collected and analyzed. The period before the pandemic was defined from 20th January 2019 to 31st March 2019 and the period during the pandemic was defined from 20th January 2020 to 31st March 2020. For the out-patient clinic, ER, and CPC attendances, patients <years of age were not included in this study. Demographic variables and clinical information, including comorbidities, length of stay (LOS), and in-hospital mortality for hospitalized patients, were retrieved from electronic medical records. The cumulative number of confirmed COVID-19 cases in Beijing was retrieved from the official website of the National Health Commission of the People's Republic of China (http://www.nhc.gov.cn). The Beijing Tiantan Hospital, Capital Medical University Review Board approved the study and waived patient consent due to the retrospective nature of the study.
The primary outcomes evaluated were non-emergency medical cares including the attendances to the out-patient clinic, the number of patients who were hospitalized in the non-intensive care wards, and the number of patients who underwent elective cardiac intervention procedures. Secondary outcomes were emergency medical cares including the attendances to the ED and CPC, the total number of patients who were hospitalized in coronary care unit (CCU), and the number of patients who underwent primary PCI.
Continuous variables were expressed as means ± standard deviation or median (25 and 75% quartiles) according to the normality of distribution. We performed a Student t-test or Mann–Whitney U-test as appropriate. Categorical variables were expressed as numbers (percentages) and compared using Pearson's chi-squared tests. Pearson correlation analysis was used to evaluate the associations of the out-patient clinic and ED and CPC attendances with the cumulative number of confirmed COVID-19 cases in Beijing. SPSS 22 (Chicago) was used for all statistical analyses, and a p < 0.05 was considered statistically significant.
The number of out-patient clinic attendances per month during the pandemic is decreased compared with the number of out-patient clinic attendances per month before the pandemic (4330.7 ± 1884.4 vs. 7847.0 ± 3686.3, p = 0.215) although this is not significantly different. Pearson correlation analysis showed that the number of out-patient clinic attendances per day was not associated with the number of new confirmed COVID-19 patients in Beijing and the cumulative number of confirmed COVID-19 patients in Beijing (r = −0.080, p = 0.506 and r = −0.071, p = 0.552, respectively) (Figure 1). There was no significant difference in the number of patients who underwent elective cardiac intervention procedures per month during the pandemic when comparing the number of patients before the pandemic in coronary angiography (74.0 ± 32.9 vs. 118.3 ± 62.1, p = 0.336), PCI (51.3 ± 28.4 vs. 74.0 ± 40.0, p = 0.468), permanent pacemaker implantation (2.3 ± 2.1 vs. 5.0 ± 4.4, p = 0.393), and radiofrequency ablation (0.3 ± 0.6 vs. 2.7 ± 1.5, p = 0.069) except for patent foramen ovale (PFO) occlusion (1.7±2.9 vs. 8.3±2.3, p = 0.035).
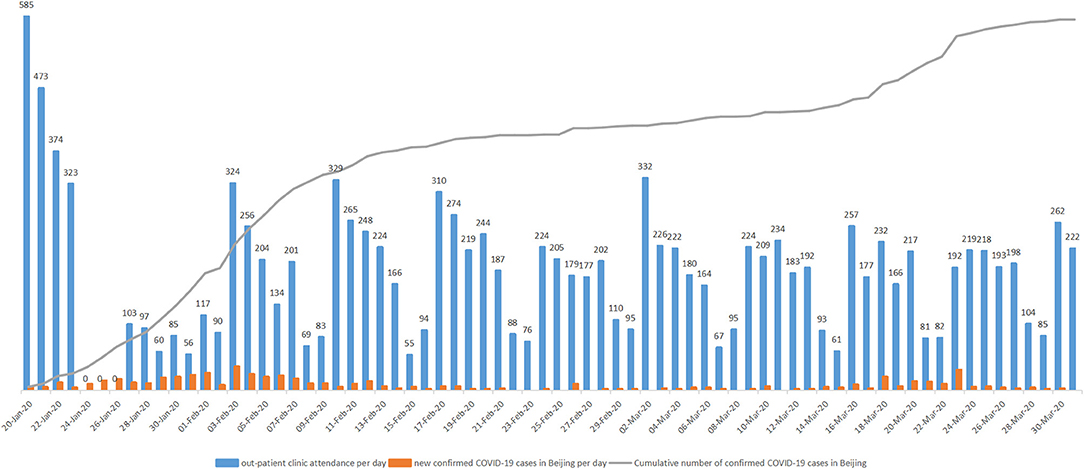
Figure 1. The association of the total number of out-patient attendance per day with the new confirmed COVID-19 patients and cumulative number of confirmed COVID-19 patients in Beijing.
There is no significant difference between the number of ED attendances per month during the pandemic compared with the number of ED attendances per month before the pandemic (8288.7 ± 3294.9 vs. 11636.0 ± 350.3, p = 0.923) as well as the number of CPC visits per month (569.7 ± 334.3 vs. 543.3 ± 294.6, p = 0.295). The number of patients who underwent primary PCI per month is increased during the pandemic compared with the number of patients before the pandemic (20.3 ± 5.5 vs. 18.0 ± 6.1, p = 0.648). However, these differences are not statistically significant.
Comparisons of the total number and clinical outcomes of patients who were hospitalized before and during the pandemic are shown in Table 1. Compared with the number of hospitalized patients before the pandemic, the total number of patients who were hospitalized in the non-intensive care wards per month is decreased (113.7 ± 82.1 vs. 173.3 ± 43.0, p = 0.327), whereas the total number of patients who were hospitalized in CCU per month during the pandemic is increased (53.0 ± 4.6 vs. 48.7 ± 4.5, p = 0.308), but there is no significant difference. Also, there are no significant differences with respect to gender distribution, age, medication therapy on admission and discharge, reasons for admission, LOS, and in-hospital mortality between hospitalized patients before and during the pandemic. The reasons for mortality before the pandemic were as follows: cardiac shock (n = 4), cardiac rupture (n = 3), respiratory failure (n = 1), and coronary perforation (n = 1), and the reasons for mortality during the pandemic were as follows: cardiac shock (n = 4), cardiac rupture (n = 2), and respiratory failure (n = 1). Compared with the hospitalized patients before the pandemic, the proportion of hospitalized patients with ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI) is significantly increased during the pandemic (19.0 vs. 8.7%, p < 0.001; 28.8 vs. 18.0%, p < 0.001, respectively). The proportions of hospitalized patients with unstable angina pectoris (38.6 vs. 48.8%, p = 0.005), PFO (3.2 vs. 6.9%, p = 0.026), and others (0.6 vs. 4.0%, p = 0.003) are significantly decreased during the pandemic, while the proportions of hospitalized patients with stable angina pectoris (1.9 vs. 3.2%, p = 0.375), heart failure (4.7 vs. 8.1%, p = 0.066), and arrhythmia (3.2 vs. 2.4%, p = 0.511) are not significantly different.
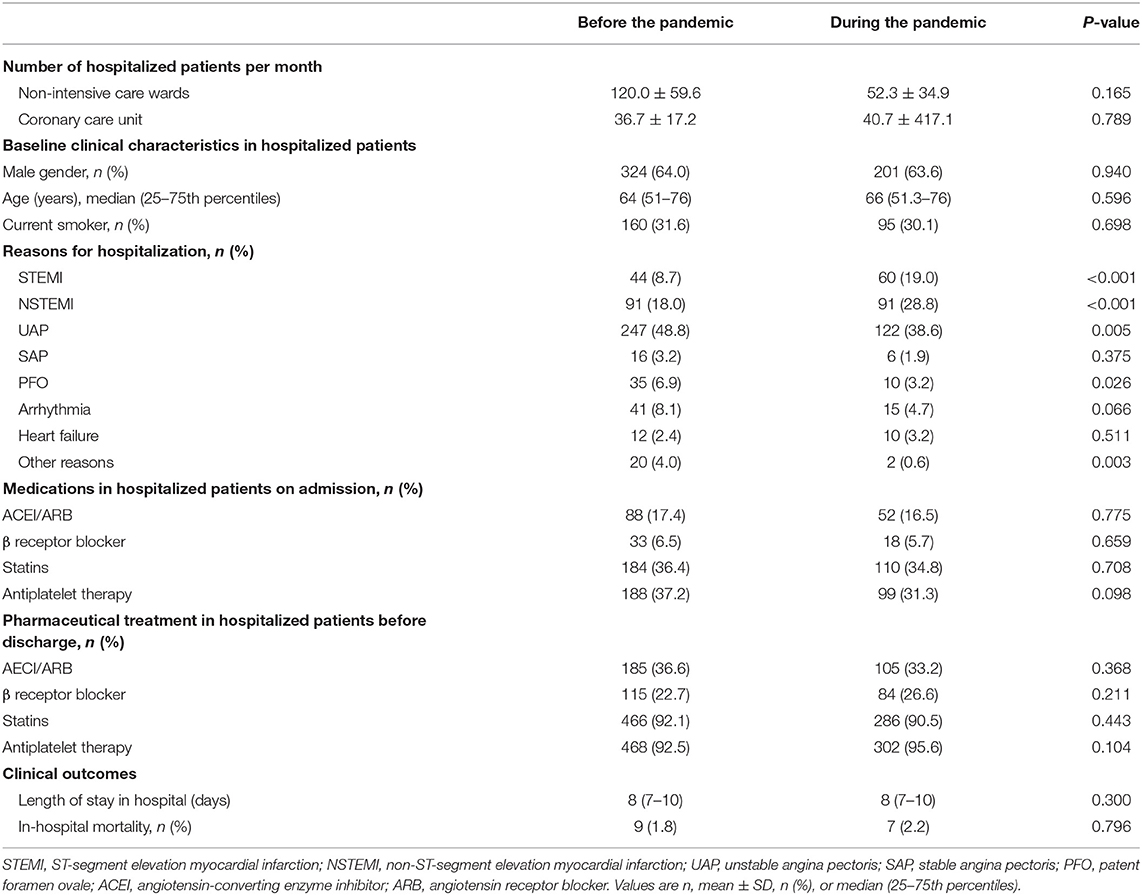
Table 1. Comparison of the total number, clinical characteristics, and clinical outcomes in hospitalized patients before and during the COVID-19 pandemic.
The result are shown in Table 2. As compared with the number before the pandemic, the number of non-emergency medical care decreased (out-patient clinic attendances are decreased by 44.8%, the total number of patients who were hospitalized in the non-intensive care wards is decreased by 22.4%, and patients who underwent elective cardiac intervention procedures are all decreased); however, the number of patients who needed emergency medical care is increased (CPC attendances is increased by 10.3%, the number of patients who were hospitalized in CCU is increased by 8.9%, and the number of patients who underwent primary PCI is increased by 13.0%) except for the attendances to the ED, which is decreased by 22.4%.
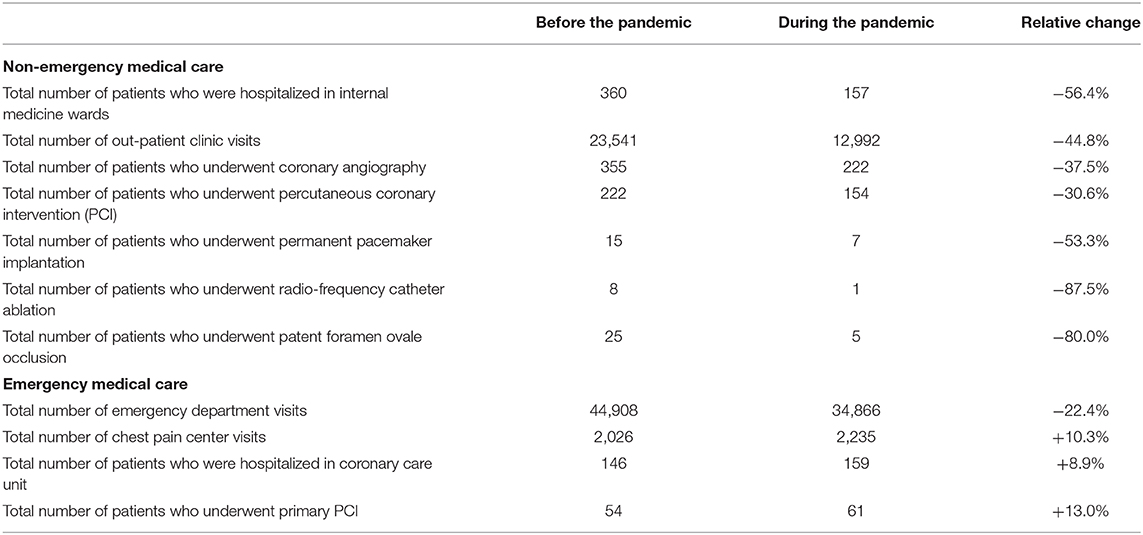
Table 2. Relative change of total number of non-emergency and emergency medical care before and during the pandemic.
The key findings of this retrospective study indicated that the COVID-19 pandemic caused impact on the normal performance of a cardiovascular department both in non-emergency medical cares and emergency medical cares.
The first finding of this study is that the number of patients who needed non-emergency medical cares including out-patient clinic, non-intensive care ward hospitalization, and non-emergency cardiac intervention procedures decreased during the pandemic. As a regional medical hub-and-spoke organization with relatively large volume of patients, non-emergency cares were decreased during the COVID-19 pandemic. This result is quite similar to other studies. As a matter of fact, the reduction in out-patient clinic attendances was also observed during the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) epidemics (20–23). In this study, we also explored the association between the number of out-patient clinic attendances and the number of infection patients by Pearson analysis; however, no significant correlation was found between them. This result reveals that the reduction of non-emergency medical cares in low-risk regions like Beijing might not be associated with the number of confirmed COVID-19 cases but with other factors like local government quarantine protocol. The reduction of patients who underwent non-emergency cardiac intervention procedures during the COVID-19 pandemic has also been observed in multiple studies. Elliott et al. demonstrated a 56% reduction in elective coronary angiography (CA) and PCI (24). Furthermore, the number of patients who underwent electrophysiology procedures and those with structural heart disease who underwent invasive procedures decreased (25–27). These results are similar to our study. However, the number of PFO occlusion in our center significantly decreased while there was no statistically significant differences in other procedures when comparing with the procedure number before the pandemic. There are many reasons for this. First of all, most of the patients who underwent PFO occlusion in our center came from other provinces. The contamination protocol is stricter for them than local patients. Secondly, the number of other procedures including pacemaker implantation and RFCA were limited, which may affect the statistics and might explain this situation. The underlying reasons for the reduction of non-emergency medical cares are complicated during the pandemic: fear of cross-infection, greater use of telemedicine, lack of medical resources for non-communicable disease, possible lower incidence rate of cardiovascular disease due to the lower physical stress and different diet activity, and increased number of financially vulnerable patients who could not pay for medications or clinical follow-up during the socioeconomic depression could all be associated with this phenomenon (28–33).
The second finding of this study is that the number of emergency medical cares was also affected during the pandemic even in a medical referral hub. For emergency medical cares, the number of CPC attendances, the number of patients who were hospitalized in CCU, and those who underwent primary PCI increased in our center during the pandemic, except for the number of ED attendances, which was decreased. First of all, the reduction of the number of ED attendances is consistent with previous studies. The Attend Study compared the daily ED attendances before and during the pandemic and observed a reduction by 30% daily ED visits (34). Franchini et al. described the impact of the COVID-19 outbreak on an urban major-hospital ED attendance in Italy and observed a reduction in ED attendance by 37% (35). Hartnett et al. (36) observed a 42% of reduction in ED visits in the USA. Boserup et al. (37) also reported a significant reduction of ED visits during the pandemic especially in high-risk regions. The reason for the reduction of ED visits is believed to be associated with fear of cross-infection, unawareness of more critical illnesses than COVID-19, as well as lower physical stress and lower rate of accidents (38–40). In our study, the CPC attendances were increased in our center during the pandemic, which was not consistent with a recent report that demonstrated that the number of STEMI cases reported to China Chest Pain Centers was reduced during the COVID-19 pandemic (41). It is worthy to note that as a multi-center analysis, that study enrolled different hospitals from several different places in China that had different cross-infection risk and cardiovascular management protocols. Also, we observed that in our center, the number of primary PCI was increased; this result was not consistent with the results from other studies worldwide (41–49). There are several explanations for this difference. First, the cross-infection risk in Beijing was relatively lower than other regions. Second, Beijing Tiantan Hospital continued to perform primary PCI as a hub-and-spoke organization when many hospitals stopped performing primary PCI and transferred patients to our center during the pandemic in Beijing.
The third finding of this study is that the number of patients who were hospitalized for STEMI and NSTEMI increased significantly, and patients who were hospitalized for unstable angina pectoris, PFO, and others decreased significantly. The number of patients who were hospitalized for other conditions, like stable angina pectoris, heart failure, and arrhythmia, decreased, but there were no statistically significant differences. This result is not similar with previous studies. Folino et al. (42) observed a significant reduction in NSTEMI but not for STEMI patients admitted to the coronary care unit during the COVID-19 pandemic. De Filippo et al. (43) also observed a reduced admission for acute coronary syndrome (ACS) during the pandemic. Braiteh et al. (44) reported a 40.7% decrease in ACS (STEMI and NSTEMI) presentation in upstate New York. The reasons for this difference between our study and theirs are as follows: first, our study was single hub-and-spoke experience where AMI patients were transferred from other hospitals. Second, as we mentioned above, the overall cross-infection risk in Beijing was lower than those studies.
The fourth finding of our study is that both the LOS and in-hospital mortality remained unchanged for hospitalized patients during the COVID-19 pandemic when comparing before the pandemic. This result is similar to previous studies. Daoulah et al. (45) enrolled STEMI patients from 16 centers during the COVID-19 pandemic and found that there were no differences with respect to in-hospital events and the LOS for these patients. Fileti et al. (50) evaluated the impact of the COVDI-19 pandemic on in-hospital outcome for ACS patients who underwent coronary invasive procedures, showing that both the percutaneous coronary intervention procedural success rate and in-hospital mortality were not different.
There are some limitations in this study. First of all, this is a single-center retrospective study. Second, the severity of the COVID-19 situation in Beijing is not like other provinces, so the result of our study is not suitable for all facilities. Third, the treatment strategy for AMI patients (primary PCI or fibrinolysis therapy for STEMI patients) might be different in other hospitals. Fourth, the major limitation of this retrospective study is represented by the fact that no adjustment was made, using appropriate statistical methodology, for potential confounders, affecting the validity of the results.
Our study shows that a hub-and-spoke model could be effective in limiting the collateral damage for patients affected by cardiovascular diseases when the medical system is stressed by disasters, such as pandemics or wars.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
JN, TZ, KS, QF, YM, QL, and ZJ were responsible for the conception and design of the article, the implementation and feasibility analysis of the research, and the analysis and interpretation of the results. JN, TZ, and YT were responsible for data collection. JN, TZ, YT, KS, QL, YM, and QF were responsible for statistical processing and writing of the paper. ZJ were responsible for the quality control, review, supervision, and management of the article. All authors read and approved the final manuscript.
This work was supported by the Chinese Cardiovascular Association-V.G. fund (2017-CCA-VG-042) and the Beijing Key Clinical Department Project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
2. Medjeral-Thomas NR, Thomson T, Ashby D, Muthusamy A, Nevin M, Duncan N, et al. Cohort study of outpatient hemodialysis management strategies for COVID-19 in North-West London. Kidney Int Rep. (2020) 11:2055–65. doi: 10.1016/j.ekir.2020.08.022
3. Parsonage WA, Cullen L, Brieger D, Hillis GS, Nasis A, Dwyer N, et al. CSANZ position statement on the evaluation of patients presenting with suspected acute coronary syndromes during the COVID-19 pandemic. Heart Lung Circ. (2020) 7:e105–10. doi: 10.1016/j.hlc.2020.05.003
4. Arnold RH, Tideman PA, Devlin GP, Carroll GE, Elder A, Lowe H, et al. Rural and remote cardiology during the COVID-19 pandemic: cardiac society of Australia and New Zealand (CSANZ) Cconsensus statement. Heart Lung Circ. (2020) 7:e88–93. doi: 10.1016/j.hlc.2020.05.001
5. DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations forheart failure care during the COVID-19 pandemic. JACC Heart Fail. (2020) 8:681–91. doi: 10.1016/j.jchf.2020.05.006
6. Alsaied T, Aboulhosn JA, Cotts TB, Daniels CJ, Etheridge SP, Feltes TF, et al. Coronavirus disease 2019 (COVID-19) pandemic implications in pediatric and adult congenital heart disease. J Am Heart Assoc. (2020) 9:e017224. doi: 10.1161/JAHA.120.017224
7. El-Saiedi SA, Haeffele C, Hanna BM, Lui GK. The hidden victims of the COVID-19 pandemic: congenital heart disease patients. JACC Case Rep. (2020) 2:1411–3. doi: 10.1016/j.jaccas.2020.05.081
8. Reza N, DeFilippis EM, Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Heart Fail. (2020) 13:e007219. doi: 10.1161/CIRCHEARTFAILURE.120.007219
9. Tay EL, Hayashida K, Chen M, Yin WH, Park DW, Seth A, et al. Transcatheter aortic valve implantation during the COVID-19 pandemic: clinical expert opinion and consensus statement for Asia. J Card Surg. (2020) 35:2142–6. doi: 10.1111/jocs.14722
10. Frankfurter C, Buchan TA, Kobulnik J, Lee DS, Luk A, McDonald M, et al. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto, Canada. Can J Cardiol. (2020) 36:1680–4. doi: 10.1016/j.cjca.2020.07.006
11. Tan W, Parikh RV, Chester R, Harrell J, Franco V, Aksoy O, et al. Single center trends in acute coronary syndrome volume and outcomes during the COVID-19 pandemic. Cardiol Res. (2020) 11:256–9. doi: 10.14740/cr1096
12. Ryan JJ, Melendres-Groves L, Zamanian RT, Oudiz RJ, Chakinala M, Rosenzweig EB, et al. Care of patients with pulmonary arterial hypertension during the coronavirus (COVID-19) pandemic. Pulm Circ. (2020) 10:2045894020920153. doi: 10.1177/2045894020920153
13. Nadar SK, Tayebjee MH, Stowasser M, Byrd JB. Managing hypertension during the COVID-19 pandemic. J Hum Hypertens. (2020) 34:415–7. doi: 10.1038/s41371-020-0356-y
14. Nan J, Meng S, Hu H, Jia R, Chen W, Li Q, et al. Comparison of clinical outcomes in patients with ST elevation myocardial infarction with percutaneous coronary intervention and the use of a telemedicine app before and after the COVID-19 pandemic at a Center in Beijing, China, from august 2019 to march 2020. Med Sci Monit. (2020) 17:e927061. doi: 10.12659/MSM.927061
15. Cao X, Spratt JC, Jin Z. Coronavirus disease 2019 (COVID-19) and acute cardiovascular disease management: a Chinese perspective on striking the balance. Resuscitation. (2020) 152:36–8. doi: 10.1016/j.resuscitation.2020.05.010
16. Huang B, Xu C, Liu H, Deng W, Yang Z, Wan J, et al. In-hospital management and outcomes of acute myocardial infarction before and during the coronavirus disease 2019 pandemic. J Cardiovasc Pharmacol. (2020) 76:540–8. doi: 10.1097/FJC.0000000000000909
17. Little CD, Kotecha T, Candilio L, Jabbour RJ, Collins GB, Ahmed A, et al. COVID-19 pandemic and STEMI: pathway activation and outcomes from the pan-London heart attack group. Open Heart. (2020) 7:e001432. doi: 10.1136/openhrt-2020-001432
18. Scholz KH, Lengenfelder B, Thilo C, Jeron A, Stefanow S, Janssens U, et al. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin Res Cardiol. (2020) 109:1511–21. doi: 10.1007/s00392-020-01703-z
19. Boeddinghaus J, Nestelberger T, Kaiser C, Twerenbold R, Fahrni G, Bingisser R, et al. Effect of COVID-19 on acute treatment of ST-segment elevation and Non-ST-segment elevation acute coronary syndrome in northwestern Switzerland. Int J Cardiol Heart Vasc. (2020) 32:100686. doi: 10.1016/j.ijcha.2020.100686
20. Chen WK, Cheng YC, Chung YT, Lin CC. The impact of the SARS outbreak on an urban emergency department in Taiwan. Med Care. (2005) 43:168–72. doi: 10.1097/00005650-200502000-00010
21. Huang HH, Yen DH, Kao WF, Wang LM, Huang CI, Lee CH. Declining emergency department visits and costs during the severe acute respiratory syndrome (SARS) outbreak. J Formos Med Assoc. (2006) 105:31–7. doi: 10.1016/S0929-6646(09)60106-6
22. Tsai MC, Arnold JL, Chuang CC, Chi CH, Liu CC, Yang YJ. Impact of an outbreak of severe acute respiratory syndrome on a hospital in Taiwan, ROC. Emerg Med J. (2004) 21:311–6. doi: 10.1136/emj.2003.011122
23. Lee SY, Khang YH, Lim HK. Impact of the 2015 middle east respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. (2019) 60:796–803. doi: 10.3349/ymj.2019.60.8.796
24. Elliott JM, Crozier IG. Decreases in cardiac catheter laboratory workload during the COVID-19 level 4 lockdown in New Zealand. Intern Med J. (2020) 50:1000–3. doi: 10.1111/imj.14922
25. Boriani G, Palmisano P, Guerra F, Bertini M, Zanotto G, Lavalle C, et al. AIAC ricerca network investigators. Impact of COVID-19 pandemic on the clinical activities related to arrhythmias and electrophysiology in Italy: results of a survey promoted by AIAC (Italian Association of Arrhythmology and Cardiac Pacing). Intern Emerg Med. (2020) 15:1445–56. doi: 10.1007/s11739-020-02487-w
26. Rubin GA, Biviano A, Dizon J, Yarmohammadi H, Ehlert F, Saluja D, et al. Performance of electrophysiology procedures at an academic medical center amidst the 2020 coronavirus (COVID-19) pandemic. J Cardiovasc Electrophysiol. (2020) 31:1249–54. doi: 10.1111/jce.14493
27. Banerjee S, Tarantini G, Abu-Fadel M, Banerjee A, Little BB, Sorajja P, et al. Coronavirus disease 2019 catheterization laboratory survey. J Am Heart Assoc. (2020) 9:e017175. doi: 10.1161/JAHA.120.017175
28. Ganatra S, Dani SS, Shah S, Asnani A, Neilan TG, Lenihan D, et al. Management of cardiovascular disease during coronavirus disease (COVID-19) pandemic. Trends Cardiovasc Med. (2020) 30:315–25. doi: 10.1016/j.tcm.2020.05.004
29. Sharma S. COVID-19: a concern for cardiovascular disease patients. Cardiovasc Toxicol. (2020) 20:443–7. doi: 10.1007/s12012-020-09596-0
30. Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis. (2020) 30:1409–17. doi: 10.1016/j.numecd.2020.05.020
31. Kulkarni P, Mahadevappa M, Alluri S. COVID-19 pandemic and the impact on the cardiovascular disease patient care. Curr Cardiol Rev. (2020) 16:173–7. doi: 10.2174/1573403X16666200621154842
32. Szymanski FM, Smuniewski C, Platek AE. Will the COVID-19 pandemic change national security and healthcare in the spectrum of cardiovascular disease? Curr Probl Cardiol. (2020) 45:100645. doi: 10.1016/j.cpcardiol.2020.100645
33. Mattioli AV, Nasi M, Cocchi C, Farinetti A. COVID-19 outbreak: impact of the quarantine-induced stress on cardiovascular disease risk burden. Future Cardiol. (2020) 16:539–42. doi: 10.2217/fca-2020-0055
34. Leow SH, Dean W, MacDonald-Nethercott M, MacDonald-Nethercott E, Boyle AA. The attend study: a retrospective observational study of emergency department attendances during the early stages of the COVID-19 pandemic. Cureus. (2020) 12:e9328. doi: 10.7759/cureus.9328
35. Franchini S, Spessot M, Landoni G, Piani C, Cappelletti C, Mariani F, et al. Stranger months: how SARS-CoV-2, fear of contagion, and lockdown measures impacted attendance and clinical activity during february and march 2020 at an Urban Emergency Department in Milan. Disaster Med Public Health Prep. (2020) 27:1–10. doi: 10.1017/dmp.2020.265
36. Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. National syndromic surveillance program community of practice. Impact of the COVID-19 pandemic on emergency department visits-United States, january 1, 2019-may 30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:699–704. doi: 10.15585/mmwr.mm6923e1
37. Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. (2020) 38:1732–6. doi: 10.1016/j.ajem.2020.06.007
38. Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:795–800. doi: 10.15585/mmwr.mm6925e2
39. Wongtanasarasin W, Srisawang T, Yothiya W, Phinyo P. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: a hospital-based study. Emerg Med Australas. (2020) 13666:1–8. doi: 10.1111/1742-6723.13666
40. Barbieri G, Spinelli S, Filippi M, Foltran F, Giraldi M, Carola Martino M, et al. COVID-19 pandemic management at the emergency department: the changing scenario at the university hospital of Pisa. Emerg Care J. (2020) 9146:108–13. doi: 10.4081/ecj.2020.9146
41. Xiang D, Xiang X, Zhang W, Yi S, Zhang J, Gu X, et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J Am Coll Cardiol. (2020) 76:1318–24. doi: 10.1016/j.jacc.2020.06.039
42. Folino AF, Zorzi A, Cernetti C, Marchese D, Pasquetto G, Roncon L, et al. Impact of COVID-19 epidemic on coronary care unit accesses for acute coronary syndrome in Veneto region, Italy. Am Heart J. (2020) 226:26–8. doi: 10.1016/j.ahj.2020.04.021
43. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. (2020) 383:88–9. doi: 10.1056/NEJMc2009166
44. Braiteh N, Rehman WU, Alom M, Skovira V, Breiteh N, Rehman I, et al. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. (2020) 226:147–51. doi: 10.1016/j.ahj.2020.05.009
45. Daoulah A, Hersi AS, Al-Faifi SM, Alasmari A, Aljohar A, Balghith M, et al. STEMI and COVID-19 pandemic in Saudi Arabia. Curr Probl Cardiol. (2020) 100656:1–20. doi: 10.1016/j.cpcardiol.2020.100656
46. Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, et al. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. (2020) 6:210–6. doi: 10.1093/ehjqcco/qcaa046
47. Zitelny E, Newman N, Zhao D. STEMI during the COVID-19 pandemic-an evaluation of incidence. Cardiovasc Pathol. (2020) 48:107232. doi: 10.1016/j.carpath.2020.107232
48. De Rosa S, Spaccarotella C, Basso C, Calabrò MP, Curcio A, Filardi PP, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. (2020) 41:2083–8. doi: 10.1093/eurheartj/ehaa409
49. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. (2020) 75:2871–2. doi: 10.1016/j.jacc.2020.04.011
Keywords: 2019 novel coronavirus disease, ST-segment elevation myocardial infarction, percutaneous coronary intervention, coronary angiography, Door-2-Door
Citation: Nan J, Zhang T, Tian Y, Song K, Li Q, Fu Q, Ma Y and Jin Z (2021) Impact of the 2019 Novel Coronavirus Disease Pandemic on the Performance of a Cardiovascular Department in a Non-epidemic Center in Beijing, China. Front. Cardiovasc. Med. 8:630816. doi: 10.3389/fcvm.2021.630816
Received: 18 November 2020; Accepted: 20 January 2021;
Published: 18 February 2021.
Edited by:
Maurizio Acampa, Siena University Hospital, ItalyReviewed by:
Simone Meini, Azienda USL Toscana Nord Ovest, ItalyCopyright © 2021 Nan, Zhang, Tian, Song, Li, Fu, Ma and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zening Jin, amluX3plbmluZ0BjY211LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.