- 1Critical Care Unit, Whipps Cross University Hospital, Barts Health NHS Trust, London, United Kingdom
- 2Critical Care Department, Faculty of Medicine, Alexandria University, Alexandria, Egypt
- 3Department of Pathology, Mohammed Bin Rashid University of Medicine and Health Sciences, Dubai, United Arab Emirates
- 4National Pulmonary Hypertension Unit-Cardiology Department, Royal Free Hospital, London, United Kingdom
- 5Institute of Cardiovascular Science, UCL, London, United Kingdom
Importance: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-associated cardiac injury has been postulated secondary to several mechanisms. While tissue diagnosis is limited during the acute illness, postmortem studies can help boost our understanding and guide management.
Objective: To report the cardiac tissue autopsy findings in coronavirus disease 2019 (COVID-19) decedents.
Evidence Review: Articles published in PubMed and Embase reporting postmortem cardiac pathology of COVID-19 decedents till September 2020. We included adult studies excluding preprints. The Joanna Briggs Institute Critical Appraisal Checklist for Case Reports was used to assess quality. We extracted gross and histology data as well as the incidence of myocarditis, cardiac ischemia, thrombosis, and dilatation. We also looked at the reported cause of death (PROSPERO registration CRD42020190898).
Findings: Forty-one relevant studies identified including 316 cases. The deceased were mostly male (62%) and elderly (median age, 75; range, 22–97 years). The most common comorbidities were hypertension (48%) and coronary artery disease (33%). Cardiac pathologies contributed to the death of 15 cases. Besides chronic cardiac pathologies, postmortem examination demonstrated cardiac dilatation (20%), acute ischemia (8%), intracardiac thrombi (2.5%), pericardial effusion (2.5%), and myocarditis (1.5%). SARS-CoV-2 was detected within the myocardium of 47% of studied hearts.
Conclusions and Relevance: SARS-CoV-2 can invade the heart, but a minority of cases were found to have myocarditis. Cardiac dilatation, ischemia, mural, and microthrombi were the most frequent findings. The systematic review was limited by the small number of cases and the quality of the studies, and there is a need to standardize the cardiac postmortem protocols.
Key Points
• Question: What are the pathological cardiac findings in postmortem autopsies of COVID-19 patients?
• Findings: The systematic review included 41 studies and 316 cases. Apart from chronic pathological findings, postmortem examination demonstrated cardiac dilatation (20%), acute ischemia (8%), intracardiac thrombi (2.5%), pericardial effusion (2.5%), and myocarditis (1.5%). SARS-CoV-2 was detected within the myocardium of 47% of studied hearts.
• Meaning: The main pathological findings in patients dying during the acute COVID-19 illness were cardiac dilatation, ischemia, and (micro)thrombosis. Myocarditis was a rare finding in this cohort of patients.
Introduction
While coronavirus disease 2019 (COVID-19) primarily affects the lungs, it is increasingly recognized as a multiorgan disease. The underlying mechanism may be direct viral invasion or secondary to the systematic effect of the infection (e.g., hypoperfusion, hypoxia, massive inflammatory response/cytokine storm).
Cardiac comorbidity and standard coronary risk factors (e.g., obesity, diabetes, and hypertension) are associated with adverse outcomes among patients with COVID-19 (1). COVID-19 is also associated with release of the highly specific marker of myocardial cell death—Troponin. Where this is tested in all hospitalized patients, the prevalence of elevated Troponin has been reported in up to 71% and is a predictor of outcome (40% mortality vs. 8% in those without myocardial injury) (2). A recent meta-analysis of published retrospective observational studies identified a positive troponin in 27% of 1,550 patients, with a similar impact on increased mortality and increased probability of needing intensive care (3).
Acute setting cardiac imaging (mainly echocardiography), while a valuable tool to assess the cardiac function and structure, suffers many limitations (4). Endomyocardial biopsies (EMBs) are rarely performed due to logistics and infection control reasons.
Postmortem examination (PM) is a valuable resource to understand the pathophysiology, cause of death, and the extent of organ involvement. Lessons from previous infectious diseases [e.g., human immunodeficiency virus (HIV)] have demonstrated the benefit of PMs (5).
To date, single case reports to modest-sized autopsy series have failed to clarify the nature of cardiac involvement. Histological findings vary from interstitial edema with or without myocarditis (6), lymphocytic endothelialitis (7), microvascular microthrombi and venous thrombosis (8), to extensive interstitial fibrosis with no endothelialitis (9), and no evidence of myocarditis (10). Optimal management depends on knowledge of the mechanism of myocardial injury, as the treatment and required follow-up will differ among the various pathologies outlined above.
To gain a better understanding of the prevalent cardiac findings in patients dying of COVID-19—we undertook a systematic review of all reported autopsies that included cardiac findings.
Methodology
A protocol of a systematic review was registered on PROSPERO database (CRD42020190898) on the 23rd June 2020. The aim was to investigate autopsy findings for patients who died from a confirmed COVID-19 infection (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=190898).
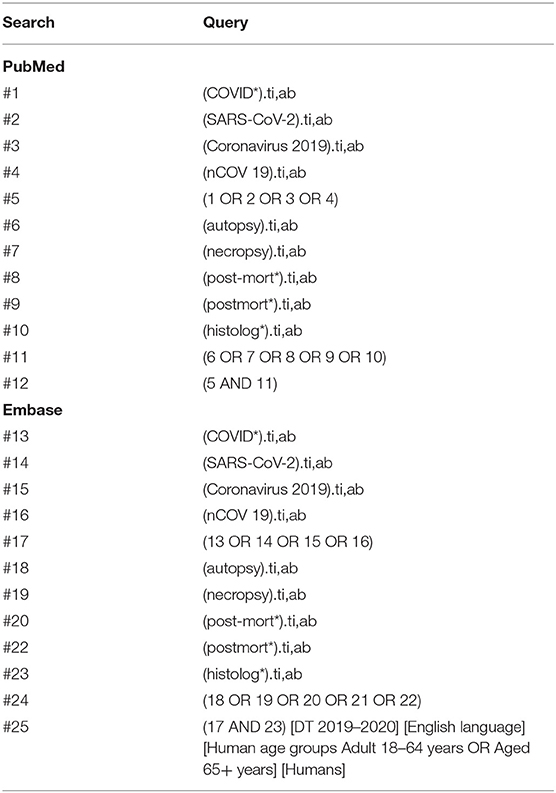
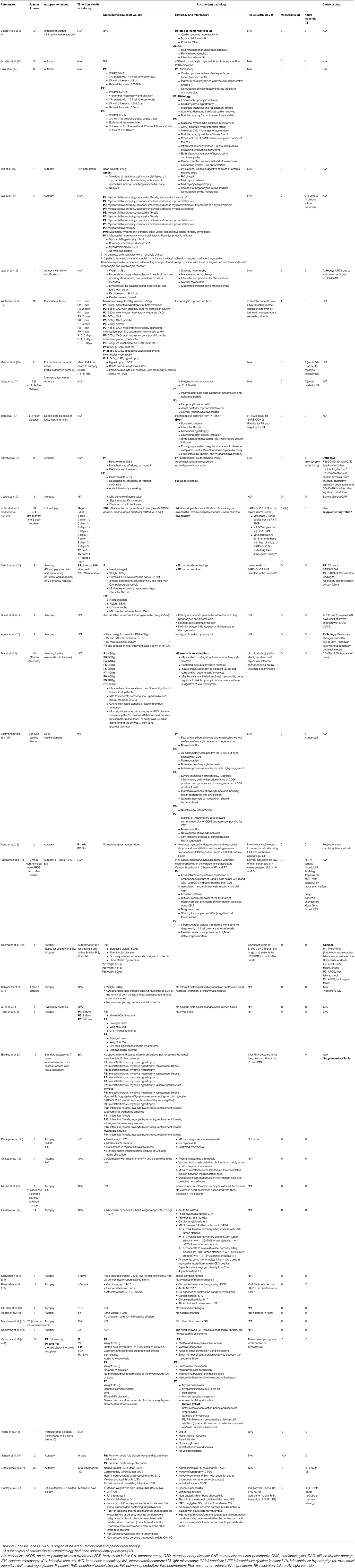
An initial systematic search was conducted through the NHS Healthcare Databases Advanced Search tool (HDAS) on 7th of June 2020 for published articles in PubMed and Embase databases. The search strategy is shown in Table 1. An electronic search alert was set to identify any new study on the EMBASE database through Healthcare Databases Advanced Search (HDAS) (option not available for PubMed) till the 21st of September 2020. The search was done by AR and included the period from 1st January 2019 to the search date. AR screened the references for additional articles. We identified 88 articles that reported PM tissue pathology. AR reviewed the full-text to retrieve articles which reported PM cardiac pathology. We reviewed only published articles in journals (excluding pre-prints) in the English language and included humans since 2019 (Figure 1: PRISMA diagram). Articles or cases with duplicate reporting have been excluded to the best of our knowledge. AR assessed the quality of the case series studies using the Joanna Briggs Institute Critical Appraisal Checklist for Case Reports (12) (Supplementary Table 2). SZ and AR extracted the data from the included studies. Any conflict was resolved by discussion and mutual agreement.
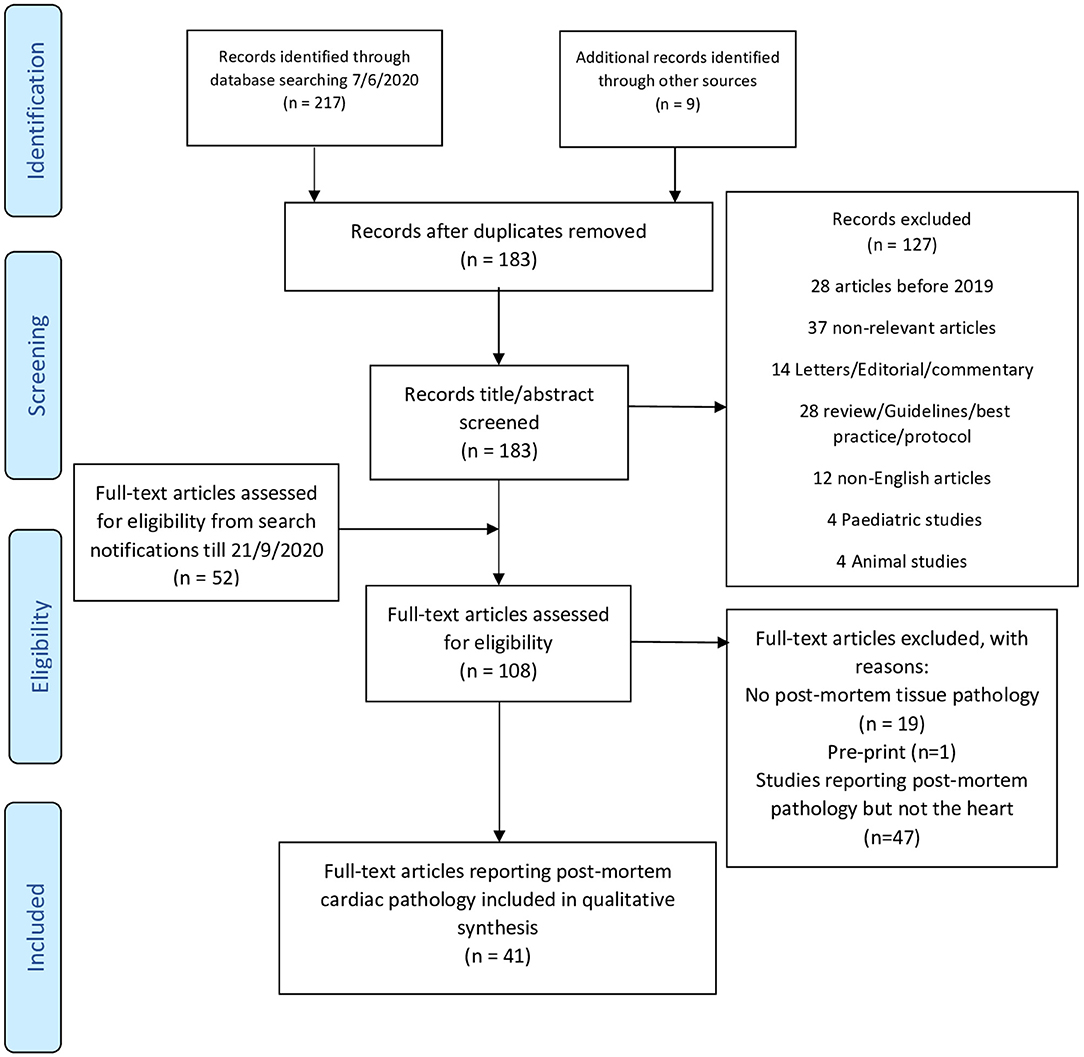
Figure 1. PRISMA 2009 flow diagram. Adapted from (11).
Patient, Intervention, Comparison, and Outcome (PICO) Statement
Patient
Adult patients (≥18 years old) who died and had a laboratory confirmation of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Intervention
None.
Comparison
None or other patients who died from another cause.
Outcome
Pathological description of PM cardiac involvement.
Results
Search Strategy
The search resulted in 226 titles. After duplicate removal of and title screening, we screened the full text of 108 articles (52 from weekly alerts) that yielded 88 articles reporting PM tissue pathology. Among those, 41 studies reported PM heart examination and included 336 cases (Figure 1). Studies were mostly case reports (n = 13) or case series (n = 24), while three studies compared cases to controls (6–10, 13–48) (Table 2, Figure 2). Authors reported cases from 14 countries, mostly developed westernized ones (Supplementary Table 1). Two studies reported on the same population, with one mainly focusing on PM cardiac examination (22, 23). The quality of the included studies was mostly moderate (Supplementary Table 2).
We analyzed the PM cardiac histopathology for 316 cases [after excluding cases unconfirmed as COVID-19 (n = 6) or with no PM cardiac tissue examination (n = 14)].
General Characteristics of the Studies
Study characteristics and pathological findings are detailed in Supplementary Tables 1, 2, respectively. Cases were predominantly male (172/275, 62%). The deceased were mostly elderly [median: 75 years; interquartile range (IQR), 63–84 years; range, 22–97 years, n = 228] and overweight [body mass index (BMI): median, 27; IQR, 22.9–34.7 kg/m2; range = 15.4–61.2 kg/m2, n = 148).
Comorbidities
Cardiovascular comorbidities were prevalent, most commonly hypertension (n = 152, 48.1%), coronary artery disease (CAD) (n = 105, 33.2%), cardiomyopathy and heart failure (n = 68, 21.5%), and atrial fibrillation (AF) (n = 35, 11.1%). Other comorbidities included chronic respiratory diseases (n = 91, 28.7%), diabetes mellitus (n = 81, 25.6%), chronic kidney disease (CKD) (n = 53, 16.7%), dementia (n = 40, 12.7%), and cancer (n = 39, 12.3%).
Timing
The median duration of prehospital symptoms (n = 82) and hospital stay (n = 158) were 5 (IQR, 2–7) and 6 days (IQR, 3–10), respectively. In total, the median duration from the onset of symptoms to death was 12 days (range, 0–52 days, n = 98). The median time interval between death to PM autopsy was 1.2 days (n = 31).
Pathological Findings
Cardiac abnormalities either on gross pathology or histology were identified in almost all cases. Most autopsies demonstrated chronic cardiac pathologies [hypertrophy (n = 85), fibrosis (n = 72), and amyloidosis (n = 11)], which may have contributed to the increased heart weight where this was reported (median, 455 g; IQR, 399–576 g; range, 250–1,070 g, exceeded normal range in 39/44 (normal reference: male, 270–360 g; female, 200–280 g)] (47).
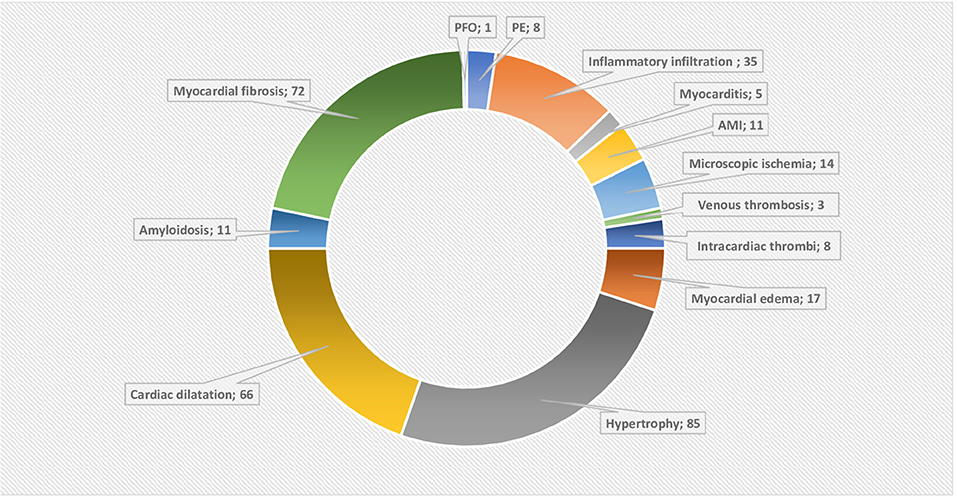
Figure 2. Doughnut chart showing the reported post-mortem acute and chronic pathologies. AMI, Acute myocardial infarction; PE, pericardial effusion; PFO, patent foramen ovale. The data labels show the number of reported acute or chronic pathologies, note that they can overlap in the single patient. Chronic pathologies include hypertrophy and amyloidosis, while myocardial fibrosis, pericardial effusion and dilatation can be acute or chronic. The rest are considered as acute pathologies.
While myocardial fibrosis was identified in only 72 cases, in a series where this was specifically reported, the prevalence was high (9, 10). Myocyte and ventricular wall hypertrophy were reported in 85 cases, again highly prevalent where specifically reported (18). Significant cardiac dilatation/cardiomegaly was described in 66 cases (10, 14, 15, 21, 24, 27, 30).
Overall changes consistent with cardiac ischemia and thrombosis were the most frequently reported acute findings. Acute myocardial ischemia was evident in 25 cases either in the form of acute myocardial infarction (MI) (n = 11) or microscopic evidence of acute or early ischemia (n = 14). Moreover, fibrin microvascular thrombi were identifiable in 27 cases (6, 8, 35, 36, 42, 47, 48). Thrombi in cardiac veins were described in three cases (8, 10). Lastly, there was eight cases with mural thrombi including the heart valves (n = 3) and the right atrium (RA) (n = 1) (10, 35, 47, 48).
Viral Invasion of Myocardium
Twelve studies explored the presence of SARS-CoV-2 within the myocardium using different techniques (Table 2) (8, 9, 17, 19, 23, 24, 29, 30, 39, 41, 44, 48). In those studies, SARS-CoV-2 was detected in 50 of 105 hearts (47%). However, clear myocarditis meeting the Dallas criteria was described in only five cases (6, 9, 17, 22). In an additional 35 cases, minimal lymphocytic (n = 33) or mononuclear infiltration (n = 2) not meeting the criteria for myocarditis was identified (13, 15, 27, 28). In three cases, authors attributed those changes as consistent with ischemic damage response (28). Overall, lymphocytic infiltration was scarce but can be detected in any of the pericardium, myocardium, epicardium, or endothelium. Lastly, pericardial affection was described in the form of pericardial effusion (n = 8) and pericarditis (n = 5, one had chronic pericarditis).
Cause of Death
The cause of death was reported for 190 cases and, for the majority of these, was respiratory in origin (Supplementary Tables 1, 2). However, cardiac contribution to death was mentioned for 15 cases while pulmonary embolism (PE) was mentioned in eight cases.
Discussion
Our review confirms that among patients dying from COVID-19, cardiac abnormalities are prevalent, but that specific changes of acute myocarditis are uncommon (1.5% of cases). Myocardial ischemia, thrombosis, and cardiac dilatation were the most dominant acute findings (Figure 2). Prevalence of the non-specific myocardial edema (ME) was 100% in the six studies reporting it (6, 15, 19, 35, 44, 45). The highly prevalent chronic cardiac pathologies not only reflect the impact of cardiac comorbidities but also complicated the histopathological interpretation.
Role of Ischemia, Endotheliitis, and Hypercoagulability
The most alarming finding is the intracardiac, coronary arterial, and venous thrombosis, which may be in part explained by the COVID-19-associated coagulopathy (CAC). Myocardial ischemia can be further aggravated by the frequent pre-existing CAD and myocardial supply–demand mismatch.
By means of its receptor, SARS-CoV-2 can directly invade the endothelium leading to endothelial cell (EC) inflammation (i.e., endothelialitis), dysfunction, and death (49). Endothelial dysfunction can also result from an inappropriate immune and cytokine response. Endothelialitis, and hence EC dysfunction, subsequently induces a procoagulant state (CAC), loss of barrier function, inflammatory tissue infiltration, edema, and injury (49, 50). Cardiovascular comorbidities are usually associated with chronic EC dysfunction, which can explain the worse outcome when further acute insult is superadded.
However, endothelialitis was not a consistent finding in our reviewed studies but, when detected, was associated with microthrombi and had multiorgan distribution. Varga et al. showed multiorgan endotheliitis in all three studied cases (7). Ackermann et al. showed widespread endotheliitis and capillary thrombosis in COVID-19-affected lungs in a much more common prevalence than in non-COVID acute respiratory distress syndrome (ARDS) lungs (51). In contrast, Bradley et al. concluded not only no evidence of endothelialitis but also little evidence of cardiac microthrombi (9). Rapkiewics et al. noted no endothelial abnormalities but a platelet-rich microthrombi in all seven hearts examined, despite anticoagulation (8). It appears that alternate mechanisms of ischemia overlap, and while anticoagulation may be highly relevant in limiting pulmonary thrombosis, this may be less likely to significantly ameliorate any cardiac contribution to poor outcomes. Nicolai et al. highlighted thrombi to be rich in platelets, fibrin, and neutrophil extracellular traps (NETs), while Jensen et al. described platelet-rich cerebral microangiopathy (36, 46). The role of NET and platelets may be significant and could support other potential therapies (e.g., antiplatelet therapy).
Chamber Dilatation and Myocardial Edema
Heart weight exceeded the normal range in 90% of cases reflecting a combination of chronic pathologies (e.g., hypertrophy), myocardial edema (marker of injury), and chambers dilatation. The observed cardiac dilatation (especially of the right heart) may be long standing or acute and hence relate to preload or afterload (pulmonary hypertension) changes occurring during the acute illness and its treatment.
ME reflects myocardial tissue response to most types of injury and hence its nonspecificity. Ischemia, septic cardiomyopathy, viral, or inflammatory infiltration can all contribute to it. Schmittinger et al. showed ME in 90% of PM septic hearts in a patchy distribution (median of 25% of tissue sections) (52). Of note, ME can reflect an early tissue change after insult (as early as 3 min in the setting of ischemia due to the disruption of the Na+/K+ pump) (53). Detecting ME has therapeutic implications, as it causes less energetic efficiency, arrhythmias, and reduced cardiac wall compliance. All of these are expected to impair systolic and diastolic function and can ultimately lead to fibrosis (53, 54). While cardiac MRI (CMR) can detect it in vivo, histological diagnosis remains technically challenging (53). This challenge, combined with the lack of standardized protocol guidelines for PM cardiac pathology reporting, may mean that ME was overlooked in many of the published reports.
Myocardial Fibrosis
Myocardial fibrosis was reported in nearly a quarter of cases. It is the end result of cardiac injury arising from different acute or chronic mechanisms. Cytokines were also implicated in cardiac fibroblast activation (55, 56).
The interpretation in COVID-19 is difficult and depends on many factors. It can reflect a chronic or a de novo subacute process. Aging and many reported comorbidities are strongly associated with fibrosis (56). Of note, amyloidosis (a pathology associated with fibrosis) was described in 11 cases and was significantly more prevalent when compared to a historical age-matched cohort (18, 37, 48).
Myocardial fibrosis can be divided into two types: interstitial fibrosis and replacement fibrosis, with considerable overlap between the two (55). While interstitial fibrosis is considered reactive and potentially reversible, replacement fibrosis is not (55). Interstitial fibrosis was previously detected in 100% of PM septic hearts but in a patchy nature (52). Such focal nature means that an extensive PM cardiac pathological examination is necessary. In fact, CMR may be superior as a diagnostic modality despite the difficultly to perform in unstable patients (55, 57).
Myocardial fibrosis represents the structural equivalent of heart failure. While ME is expected in the “reversible” septic cardiomyopathy, increased fibrous deposition (i.e., replacement fibrosis) would not be a likely finding in such reversible pathology (52, 57, 58).
Viral Invasion, Inflammatory Infiltrate, and Myocarditis
Studies investigating the presence of SARS-CoV-2 within the myocardium were positive in about half the cases. In 1986, The Dallas criteria were proposed for the histopathological categorization and diagnosis of myocarditis based on endomyocardial biopsies. The “Dallas criteria” defines acute myocarditis as “an inflammatory infiltrate associated with myocyte necrosis or damage not characteristic of myocardial ischemia.” Borderline myocarditis requires a less intense inflammatory infiltrate with no light microscopic signs of myocyte destruction (59). In COVID-19 PM studies, inflammatory infiltrate (mainly lymphocytic) was observed in a minor proportion (about 10%) and was limited in extent for the majority of cases. As such, when interstitial edema and inflammatory infiltrate were observed, they did not meet the diagnostic criteria of myocarditis, except in five cases. In fact, some authors attributed such inflammatory infiltrate to an ischemic process (28). This suggests that contrary to early conjectures, acute and fulminant myocarditis are rare during the acute illness.
Clinical and Imaging Correlation
Correlating the histopathological data to the clinical, imaging, and investigational data can provide more insights into the likely mechanisms of cardiac involvement in COVID-19. Clinical presentation varies from ST elevation MI due to thrombotic occlusion of epicardial coronaries, to ischemia and/or infarction without obstructive coronary disease, through to tachy and brady arrhythmias, depressed left and right ventricular function, and occasional pericardial involvement (60). A review of published literature suggests that elevated Troponin and heart failure dominate the clinical presentations (61).
Echocardiography is readily performed in the acute setting but provides limited insights into the cause when compared to CMR. In a large multinational survey, Dweck et al. reported the echocardiographic findings in 1,216 studies performed over 17 days (62). Fifty-five percent of scans were abnormal. Impaired LV function or dilation (39%) followed by RV abnormalities (33%) dominated. These findings are non-specific, but clear wall motion abnormalities suggesting infarction were rare (3%). The RV abnormalities most likely relate to increased afterload given the high prevalence of pulmonary thromboembolism and extensive lung damage associated with COVID-19 infection (63). The LV abnormalities are non-specific but provide further evidence of the high prevalence of cardiac damage.
CMR-based studies have focused on patients post recovery (too late for confirmation of myocarditis) but have shown a high prevalence of abnormalities. The largest to date is a German study of relatively young patients (mean age, 49 years), largely managed at home (67 of 100), studied a median of 71 days post infection. Seventy-eight percent were reported to show abnormalities, including reduction in LV function, elevated T1 and T2 (the latter suggesting ME) and late gadolinium enhancement (LGE) (non-ischemic pattern in 20, ischemic in 12). Three patients with very elevated T2 were referred for endomyocardial biopsy and typical features of myocarditis reported. The T1 and T2 abnormalities suggest ongoing myocardial edema, and the LGE enhancement suggests fibrosis—both of which are common in the autopsy data (64).
The second CMR-based study included only patients in whom Troponin had been elevated during hospital admission. Fifty-one patients were studied 27 days post hospital discharge. In 22 patients, pulmonary embolism and/or coronary ischemia were identified before scanning as the most likely cause of troponin leakage. Among 29 patients (mean age, 64 years) with no clinically identified cause for myocardial injury, an ischemic pattern injury (LGE) was identified in 5, dual pathology (ischemic and non-ischemic) in 4, and non-ischemic in 11. Intriguingly, T1 and T2 were not abnormal in this study. This study thus also supports the histological finding of significant myocardial fibrosis but suggests that edema clears fairly quickly in those that recover (2). Again, Rajpal et al. performed CMR on 26 athletes with a history of mild COVID-19 infection. Four of them (15%) had criteria of myocarditis despite mild or no symptoms, and 30% showed signs of previous cardiac injury (65).
What Can We Conclude From Integrating All Available Data?
Merging the clinical, investigational, and autopsy data, we are presented with a picture that demonstrates a high prevalence of cardiac abnormalities, in part due to exacerbation of underlying cardiac pathology and partly coagulation disorders affecting the pulmonary and coronary vessels. Direct cardiac involvement mainly takes the form of non-coronary myocyte death, myocyte dysfunction, and interstitial fibrosis without substantial inflammatory infiltration or clear ischemia.
The role of direct viral cellular damage remains to be fully explored, and if this is the driving force, it is intriguing that the inflammatory response appears muted. However, it is possible that while the virus is rarely causing a fulminant or acute myocarditis, it can cause a persistent chronic myocardial inflammation with significant long-term implications. It is also important to note the reporting of a delayed immune response in the form of Kawasaki's disease in pediatric patients supporting the issue of long-term sequelae of the SARS-CoV-2 infection (66). Whether immunosuppressive treatment (e.g., dexamethasone and Tocilizumab) during the acute illness is of benefit or causes more harm to the heart should await randomized controlled studies including long-term follow-up.
Thus, on balance, the data strongly suggest significant viral replication in the myocardium without true acute myocarditis in most instances, with frequent non-MI pattern fibrosis—consistent with microvascular ischemia/thrombi and, in some cases, endothelial inflammation. Given the frequent presence of fibrosis associated with cell death, it is likely that complete recovery is unlikely—a clear distinction from septic cardiomyopathy. In addition, the exacerbation of underlying disease would appear to frequently unmask coronary disease, further increasing the benefit of careful cardiological follow-up.
As the vast majority of studied patients in this review died during the acute illness and cardiac abnormality was prevalent in the population studied, we can conclude that myocarditis was not a dominant cause of cardiac dysfunction identified premortem in COVID-19 patients, while the role of endothelialitis needs further clarification.
Limitations
Our work delineates the importance of PM to guide the understanding of COVID-19. However, the small number of published PM cases in a disease, which has caused more than 1 million fatalities, highlights a hugely missed opportunity. Cardiac pathological changes are more likely to be focal in nature and hence easily missed if the heart is not examined in its entirety. Furthermore, the high prevalence of myocardial fibrosis, myocyte damage, or viral RNA in some studies but not others suggest a need to standardize histological reporting to establish common ground between pathologists and clinicians. There is also a genuine need for an international case register to gather the largest possible data in the shortest interval.
While our work is limited by the quality and small number of cases per study, we think it can contribute to a better understanding of COVID-19-associated cardiac injury. Other limits include the probable selection and reporting bias. PM is performed for patients who died during the acute illness and for certain subgroups of patients due to clinical or legal reasons. The longest duration of illness in our cohort is 52 days, which means that the long-term evolution or complications of the disease cannot be covered by this review.
Conclusions
To conclude, our review confirmed the high prevalence of cardiac pathological findings in COVID-19 patients. Cardiac dilatation, ischemia, and thrombosis were the most prevalent findings. SARS-CoV-2 was present in nearly half of the examined hearts, but true myocarditis was evident in just 1.5% of the deceased patients.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
AR: conceptualization and design, registration of the protocol, conduct of the search, quality assessment, data extraction, data interpretation, and manuscript drafting. SZ: conceptualization, design, and writing of the protocol, extraction and interpretation of the data, and manuscript drafting. HF: data analysis and interpretation and writing and revising the manuscript. JC: data analysis and interpretation and writing and reviewing the manuscript. All authors: contributed to the article and approved the submitted version.
Conflict of Interest
JC received grants and personal fees from Actelion, GSK, Bayer, Endotronix, Pfizer, and United Therapeutics. AR has minor shares in Gilead Sciences.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Professor Sebastian Lucas (Professor of cellular pathology, St Thomas' hospital, UK) and Professor Alawi Al Sheikh-Ali (Professor of cardiovascular medicine and Provost and Dean of the College of Medicine, Mohammed bin Rashid University for Medicine and Health Sciences, UAE) for their valuable advice and guidance during the development of this review.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2020.626975/full#supplementary-material
References
1. Cummings MJ, Baldwin MR, Abrams D, Jacobson SD, Meyer BJ, Balough EM, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. (2020) 395:1763–70. doi: 10.1016/S0140-6736(20)31189-2
2. Knight DS, Kotecha T, Razvi Y, Chacko L, Brown JT, Jeetley PS, et al. COVID-19: myocardial injury in survivors. Circulation. (2020) 142:1120–2. doi: 10.1161/CIRCULATIONAHA.120.049252
3. Santoso A, Pranata R, Wibowo A, Al-Farabi MJ, Huang I, Antariksa B. Cardiac injury is associated with mortality and critically ill pneumonia in COVID-19: a meta-analysis. Am J Emerg Med. (2020). doi: 10.1016/j.ajem.2020.04.052. [Epub ahead of print].
4. Roshdy A. Echodynamics: interpretation, limitations, and clinical integration! J Intensive Care Med. (2018) 33:439–46. doi: 10.1177/0885066617734151
5. Schwartz DA, Herman CJ. The importance of the autopsy in emerging and reemerging infectious diseases. Clin Infect Dis. (1996) 23:248–54. doi: 10.1093/clinids/23.2.248
6. Duarte-Neto AN, Monteiro RAA, da Silva LFF, Malheiros DMAC, de Oliveira EP, Theodoro-Filho J, et al. Pulmonary and systemic involvement of COVID-19 assessed by ultrasound-guided minimally invasive autopsy. Histopathology. (2020) 77:186–97. doi: 10.1111/his.14160
7. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. (2020) 395:1417–8. doi: 10.1016/S0140-6736(20)30937-5
8. Rapkiewicz AV, Mai X, Carsons SE, Pittaluga S, Kleiner DE, Berger JS, et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. EClinicalMedicine. (2020) 24:100434. doi: 10.1016/j.eclinm.2020.100434
9. Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, Xu H, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. (2020) 396:320–32. doi: 10.1016/S0140-6736(20)31305-2
10. Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. (2020) 173:350–61. doi: 10.7326/M20-2566
11. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed1000097
12. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI (2020) 248–61. Available online at: https://synthesismanual.jbi.global. doi: 10.46658/JBIMES-20-08
13. Schaller T, Hirschbühl K, Burkhardt K, Braun G, Trepel M, Märkl B, et al. Postmortem examination of patients with COVID-19. JAMA. (2020) 323:2518–20. doi: 10.1001/jama.2020.8907
14. Buja LM, Wolf DA, Zhao B, Akkanti B, McDonald M, Lelenwa L, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc Pathol. (2020) 48:107233. doi: 10.1016/j.carpath.2020.107233
15. Yan L, Mir M, Sanchez P, Beg M, Peters J, Enriquez O, et al. COVID-19 in a Hispanic Woman. Arch Pathol Lab Med. (2020) 144:1041–7. doi: 10.5858/arpa.2020-0217-SA
16. Lacy JM, Brooks EG, Akers J, Armstrong D, Decker L, Gonzalez A, et al. COVID-19: postmortem diagnostic and biosafety considerations. Am J Forensic Med Pathol. (2020) 41:143–51. doi: 10.1097/PAF.0000000000000567
17. Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. (2020) 173:268–77. doi: 10.7326/L20-1206
18. Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. (2020) 77:198–209. doi: 10.1111/his.14134
19. Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. (2020) 33:1007–14. doi: 10.1038/s41379-020-0536-x
20. Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 autopsies, Oklahoma, USA. Am J Clin Pathol. (2020) 153:725–33. doi: 10.1093/ajcp/aqaa062
21. Navarro Conde P, Alemany Monraval P, Medina Medina C, Jiménez Sánchez A, Andrés Teruel JC, Ferrando Marco J, et al. Autopsy findings from the first known death from Severe Acute Respiratory Syndrome SARS-CoV-2 in Spain. Revista Española de Patol. (2020) 53:188–92 doi: 10.1016/j.patol.2020.04.002
22. Edler C, Schröder AS, Aepfelbacher M, Fitzek A, Heinemann A, Heinrich F, et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int J Legal Med. (2020) 134:1275–84. doi: 10.1007/s00414-020-02317-w
23. Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol. (2020) 5:1281–5. doi: 10.1001/jamacardio.2020.3551
24. Sekulic M, Harper H, Nezami BG, Shen DL, Sekulic SP, Koeth AT, et al. Molecular detection of SARS-CoV-2 infection in FFPE samples and histopathologic findings in fatal SARS-CoV-2 cases. Am J Clin Pathol. (2020) 154:190–200. doi: 10.1093/ajcp/aqaa091
25. Suess C, Hausmann R. Gross and histopathological pulmonary findings in a COVID-19 associated death during self-isolation. Int J Legal Med. (2020) 134:1285–90. doi: 10.1007/s00414-020-02319-8
26. Aguiar D, Lobrinus JA, Schibler M, Fracasso T, Lardi C. Inside the lungs of COVID-19 disease. Int J Legal Med. (2020) 134:1271–4. doi: 10.1007/s00414-020-02318-9
27. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. (2020) 8:681–6. doi: 10.1016/S2213-2600(20)30243-5
28. Beigmohammadi MT, Jahanbin B, Safaei M, Amoozadeh L, Khoshavi M, Mehrtash V, et al. Pathological findings of postmortem biopsies from lung, heart, and liver of 7 deceased COVID-19 patients. Int J Surg Pathol. (2020) 1–11. doi: 10.1177/1066896920935195. [Epub ahead of print].
29. Wang C, Xie J, Zhao L, Fei X, Zhang H, Tan Y, et al. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine. (2020) 57:102833. doi: 10.1016/j.ebiom.2020.102833
30. Bösmüller H, Traxler S, Bitzer M, Häberle H, Raiser W, Nann D, et al. The evolution of pulmonary pathology in fatal COVID-19 disease: an autopsy study with clinical correlation. Virchows Arch. (2020) 477:349–57. doi: 10.1007/s00428-020-02881-x
31. Schweitzer W, Ruder T, Baumeister R, Bolliger S, Thali M, Meixner E, et al. Implications for forensic death investigations from first Swiss post-mortem CT in a case of non-hospital treatment with COVID-19. Forensic Imaging. (2020) 21:200378. doi: 10.1016/j.fri.2020.200378
32. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. (2020) 8:420–2. doi: 10.1016/S2213-2600(20)30076-X
33. Youd E, Moore L. COVID-19 autopsy in people who died in community settings: the first series. J Clin Pathol. (2020) 73:840–4. doi: 10.1136/jclinpath-2020-206710
34. Ducloyer M, Gaborit B, Toquet C, Castain L, Bal A, Arrigoni PP, et al. Complete post-mortem data in a fatal case of COVID-19: clinical, radiological and pathological correlations. Int J Legal Med. (2020) 134:2209–14. doi: 10.1007/s00414-020-02390-1
35. Cîrstea AE, Buzulică RL, Pirici D, Ceauşu MC, Iman RV, Gheorghe OM, et al. Histopathological findings in the advanced natural evolution of the SARS-CoV-2 infection. Rom J Morphol Embryol. (2020) 61:209–18. doi: 10.47162/RJME.61.1.23
36. Nicolai L, Leunig A, Brambs S, Kaiser R, Weinberger T, Weigand M, et al. Immunothrombotic dysregulation in COVID-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation. (2020) 142:1176–89. doi: 10.1161/CIRCULATIONAHA.120.048488
37. Grosse C, Grosse A, Salzer HJF, Dünser MW, Motz R, Langer R. Analysis of cardiopulmonary findings in COVID-19 fatalities: high incidence of pulmonary artery thrombi and acute suppurative bronchopneumonia. Cardiovasc Pathol. (2020) 49:107263. doi: 10.1016/j.carpath.2020.107263
38. Schwensen HF, Borreschmidt LK, Storgaard M, Redsted S, Christensen S, Madsen LB. Fatal pulmonary fibrosis: a post-COVID-19 autopsy case. J Clin Pathol. (2020). doi: 10.1136/jclinpath-2020-206879. [Epub ahead of print].
39. Remmelink M, De Mendonça R, D'Haene N, De Clercq S, Verocq C, Lebrun L, et al. Unspecific post-mortem findings despite multiorgan viral spread in COVID-19 patients. Crit Care. (2020) 24:495. doi: 10.1186/s13054-020-03218-5
40. Okudela K, Hayashi H, Yoshimura Y, Sasaki H, Horiuchi H, Miyata N, et al. A Japanese case of COVID-19: an autopsy report. Pathol Int. (2020) 70:820–4. doi: 10.1111/pin.13002
41. Adachi T, Chong JM, Nakajima N, Sano M, Yamazaki J, Miyamoto I, et al. Clinicopathologic and immunohistochemical findings from autopsy of patient with COVID-19, Japan. Emerg Infect Dis. (2020) 26:2157–61. doi: 10.3201/eid2609.201353
42. Nadkarni GN, Lala A, Bagiella E, Chang HL, Moreno PR, Pujadas E, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients With COVID-19. J Am Coll Cardiol. (2020) 76:1815–26. doi: 10.1016/j.jacc.2020.08.041
43. Al-Dalahmah O, Thakur KT, Nordvig AS, Prust ML, Roth W, Lignelli A, et al. Neuronophagia and microglial nodules in a SARS-CoV-2 patient with cerebellar hemorrhage. Acta Neuropathol Commun. (2020) 8:147. doi: 10.1186/s40478-020-01024-2
44. Oprinca GC, Muja LA. Postmortem examination of three SARS-CoV-2-positive autopsies including histopathologic and immunohistochemical analysis. Int J Legal Med. (2020) 135:329–39. doi: 10.1007/s00414-020-02406-w
45. Wang XX, Shao C, Huang XJ, Sun L, Meng LJ, Liu H, et al. Histopathological features of multiorgan percutaneous tissue core biopsy in patients with COVID-19. J Clin Pathol. (2020). doi: 10.1136/jclinpath-2020-206623. [Epub ahead of print].
46. Jensen MP, Le Quesne J, Officer-Jones L, Teodòsio A, Thaventhiran J, Ficken C, et al. Neuropathological findings in two patients with fatal COVID-19. Neuropathol Appl Neurobiol. (2020). doi: 10.1111/nan.12662. [Epub ahead of print].
47. Elsoukkary SS, Mostyka M, Dillard A, Berman DR, Ma LX, Chadburn A, et al. Autopsy findings in 32 patients with COVID-19: a single-institution experience. Pathobiology. (2020) 1–13. doi: 10.1159/000511325. [Epub ahead of print].
48. Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe. (2020) 1:e245–53. doi: 10.1016/S2666-5247(20)30115-4
49. Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. (2020) 7:389–91. doi: 10.1038/s41577-020-0343-0
50. Iba T, Connors JM, Levy JH. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm Res. (2020) 69:11819. doi: 10.1007/s00011-020-01401-6
51. Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid19. N Engl J Med. (2020) 383:120–8. doi: 10.1056/NEJMoa2015432
52. Schmittinger CA, Dünser MW, Torgersen C, Luckner G, Lorenz I, Schmid S, et al. Histologic pathologies of the myocardium in septic shock: a prospective observational study. Shock. (2013) 39:329–35. doi: 10.1097/SHK.0b013e318289376b
53. Friedrich MG. Myocardial edema–a new clinical entity? Nat Rev Cardiol. (2010) 7:292–6. doi: 10.1038/nrcardio.2010.28
54. Vasques-Nóvoa F, Laundos TL, Madureira A, Bettencourt N, Nunes JPL, Carneiro F, et al. Myocardial Edema: an Overlooked Mechanism of Septic Cardiomyopathy? Shock. (2020) 53:616–9. doi: 10.1097/SHK.0000000000001395
55. Bing R, Dweck MR. Myocardial fibrosis: why image, how to image and clinical implications. Heart. (2019) 105:1832–40. doi: 10.1136/heartjnl-2019-315560
56. Hinderer S, Schenke-Layland K. Cardiac fibrosis - a short review of causes and therapeutic strategies. Adv Drug Deliv Rev. (2019) 146:77–82. doi: 10.1016/j.addr.2019.05.011
57. Siddiqui Y, Crouser ED, Raman SV. Nonischemic myocardial changes detected by cardiac magnetic resonance in critical care patients with sepsis. Am J Respir Crit Care Med. (2013) 188:1037–9. doi: 10.1164/rccm.201304-0744LE
58. Aneman A, Vieillard-Baron A. Cardiac dysfunction in sepsis. Intensive Care Med. (2016) 42:2073–6. doi: 10.1007/s00134-016-4503-4
59. Aretz HT. Myocarditis: the Dallas criteria. Hum Pathol. (1987) 18:619–24. doi: 10.1016/S0046-8177(87)80363-5
60. Hendren NS, Drazner MH, Bozkurt B, Cooper LT Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. (2020) 141:1903–14. doi: 10.1161/CIRCULATIONAHA.120.047349
61. Singh R, Kashyap R, Hutton A, Sharma M, Surani S. a review of cardiac complications in coronavirus disease 2019. Cureus. (2020) 12:e8034. doi: 10.7759/cureus.8034
62. Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. (2020) 21:949–58. doi: 10.1093/ehjci/jeaa178
63. Sakr Y, Giovini M, Leone M, Pizzilli G, Kortgen A, Bauer M, et al. Pulmonary embolism in patients with coronavirus disease-2019 (COVID-19) pneumonia: a narrative review. Ann. Intensive Care. (2020) 10:124. doi: 10.1186/s13613-020-00741-0
64. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. (2020) 5:1265–73. doi: 10.1001/jamacardio.2020.3557
65. Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, Simonetti OP, et al. Cardiovascular magnetic resonance findings in competitive athletes recovering from COVID-19 infection. JAMA Cardiol. (2020) e204916. doi: 10.1001/jamacardio.2020.4916. [Epub ahead of print].
Keywords: COVID-19, SARS-CoV-2, post-mortem, cardiac injury, autopsy
Citation: Roshdy A, Zaher S, Fayed H and Coghlan JG (2021) COVID-19 and the Heart: A Systematic Review of Cardiac Autopsies. Front. Cardiovasc. Med. 7:626975. doi: 10.3389/fcvm.2020.626975
Received: 07 November 2020; Accepted: 17 December 2020;
Published: 28 January 2021.
Edited by:
Shuyang Zhang, Peking Union Medical College Hospital, ChinaReviewed by:
Hui Gong, Fudan University, ChinaNazareno Paolocci, Johns Hopkins University, United States
Copyright © 2021 Roshdy, Zaher, Fayed and Coghlan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shroque Zaher, c2hyb3F1ZS56YWhlckBtYnJ1LmFjLmFl
 Ashraf Roshdy
Ashraf Roshdy Shroque Zaher
Shroque Zaher Hossam Fayed4,5
Hossam Fayed4,5 John Gerry Coghlan
John Gerry Coghlan