
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Cardiovasc. Med., 09 December 2020
Sec. Heart Failure and Transplantation
Volume 7 - 2020 | https://doi.org/10.3389/fcvm.2020.612818
This article is part of the Research TopicWhat do we know about COVID-19 implications for cardiovascular disease?View all 109 articles
 Gregorio Tersalvi1,2*
Gregorio Tersalvi1,2* Dario Winterton3
Dario Winterton3 Giacomo Maria Cioffi1,4
Giacomo Maria Cioffi1,4 Simone Ghidini5
Simone Ghidini5 Marco Roberto1
Marco Roberto1 Luigi Biasco6,7
Luigi Biasco6,7 Giovanni Pedrazzini1,7
Giovanni Pedrazzini1,7 Jeroen Dauw8,9
Jeroen Dauw8,9 Pietro Ameri10,11
Pietro Ameri10,11 Marco Vicenzi5,12
Marco Vicenzi5,12During the Coronavirus Disease 2019 worldwide pandemic, patients with heart failure are a high-risk group with potential higher mortality if infected. Although lockdown represents a solution to prevent viral spreading, it endangers regular follow-up visits and precludes direct medical assessment in order to detect heart failure progression and optimize treatment. Furthermore, lifestyle changes during quarantine may trigger heart failure decompensations. During the pandemic, a paradoxical reduction of heart failure hospitalization rates was observed, supposedly caused by patient reluctance to visit emergency departments and hospitals. This may result in an increased patient mortality and/or in more complicated heart failure admissions in the future. In this scenario, different telemedicine strategies can be implemented to ensure continuity of care to patients with heart failure. Patients at home can be monitored through dedicated apps, telephone calls, or devices. Virtual visits and forward triage screen the patients with signs or symptoms of decompensated heart failure. In-hospital care may benefit from remote communication platforms. After discharge, patients may undergo remote follow-up or telerehabilitation to prevent early readmissions. This review provides a comprehensive appraisal of the many possible applications of telemedicine for patients with heart failure during Coronavirus disease 2019 and elucidates practical limitations and challenges regarding specific telemedicine modalities.
The Coronavirus Disease 2019 (COVID-19) pandemic has caused considerable morbidity and mortality worldwide. Epidemiological data from China indicate that patients with concomitant cardiovascular disease are more likely to develop life-threatening complications from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection (1–7). The risk of complications may be even higher in patients with heart failure (HF) because they are older and have more comorbidities, but also due to the specific characteristics of this syndrome (8). Lockdown of social activities has allowed limiting the spreading of SARS-CoV-2, but it has also decreased medical contacts. For HF patients, this might have led to late recognition and treatment of episodes of decompensation and missed opportunities for optimization of medical and nonmedical therapy. In addition, lifestyle changes adopted during lockdown, such as dietary changes, increased alcohol consumption and decreased physical activity, may trigger HF decompensations (9, 10).
Telemedicine represents a useful tool to prevent negative direct and indirect consequences of SARS-CoV-2, and the present situation might be the right moment to implement a structured telemedicine program in clinical practice. Its main benefits include guiding the treatment of patients in primary care to minimize the risk of disease transmission during referral, continuing to provide optimal treatment to the patients with cardiovascular disease who are isolated at home or are discharged from the hospital to prevent clinical deterioration, monitoring early signs of new onset or worsening HF, and reducing unnecessary visits to the hospital to decrease the incidence of cluster infections (11).
In this review, we provide an overview of the many possible applications of telemedicine, its limitations and challenges, in patients with HF during COVID-19.
Already in the first months of the COVID-19 pandemic, the impact of cardiovascular comorbidities on disease course became clear in observational studies, indicating that patients with previous cardiovascular disease had higher COVID-19 disease severity and mortality (2, 6, 7). In addition, myocardial injury in COVID-19 has been broadly described (6, 7, 12, 13), which might further impair myocardial function and worsen prognosis in patients with known HF.
Patients with chronic HF represent a vulnerable group during a pandemic of infectious respiratory disease. Previous studies have shown that they are at increased risk for adverse consequences of seasonal influenza (14) and other causes of pneumonia (15). Furthermore, acute infections may trigger HF exacerbations (16).
The social and environmental effects of lockdown must also be mentioned. A significant decline in hospitalization rates for acute HF during the COVID-19 pandemic, compared to before the pandemic and each of the preceding 3 years, was described, which might be the consequence of fear for infection leading to reluctance to seek medical attention when needed (17). Notably, hospitalized patients had more severe symptoms on admission, possibly suggesting that patients have waited longer before presenting to the hospital or less severe cases did not come to the hospital at all. Further, lifestyle changes during lockdown, such as dietary changes, increased alcohol consumption and decreased physical activity, may trigger HF decompensations (9, 10).
Although lockdown represents a solution to prevent viral spreading, it may complicate regular follow-up visits, therefore encumbering optimization of medical therapy and limiting detection of development of complications or disease progression that may require a change in management.
For these reasons, the great challenge of patients with HF during COVID-19 is keeping them safe from infection risk, but equally continuing with strict monitoring in order to prevent hospitalizations. As a result, health systems have largely transitioned to noncontact care delivery methods for ambulatory care (9). In this setting, various strategies of telemedicine and remote monitoring were developed rapidly and implemented more widely in HF patients (Table 1, Figure 1).
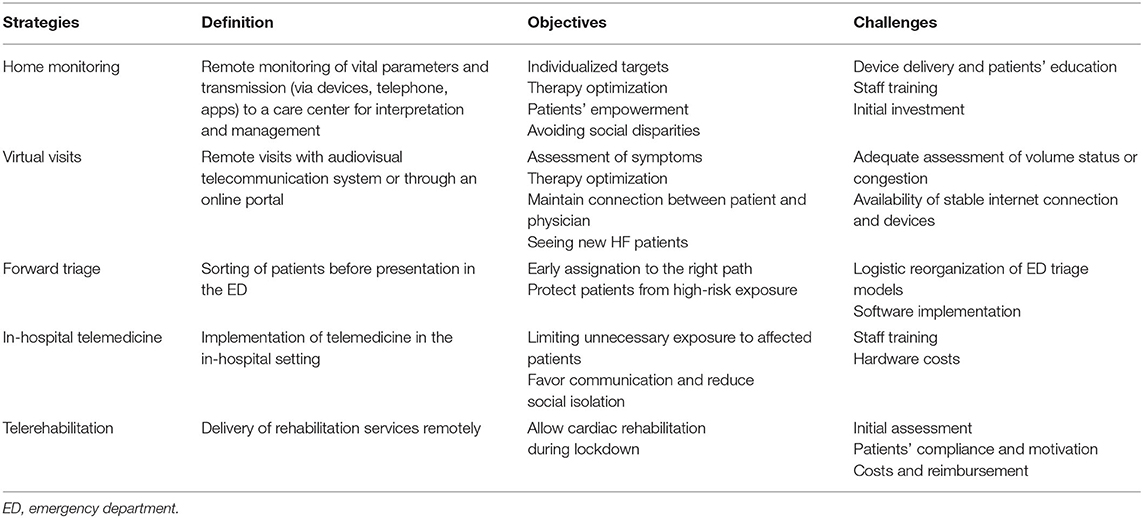
Table 1. Strengths and weaknesses of different telemedicine strategies for patients with heart failure during COVID-19.
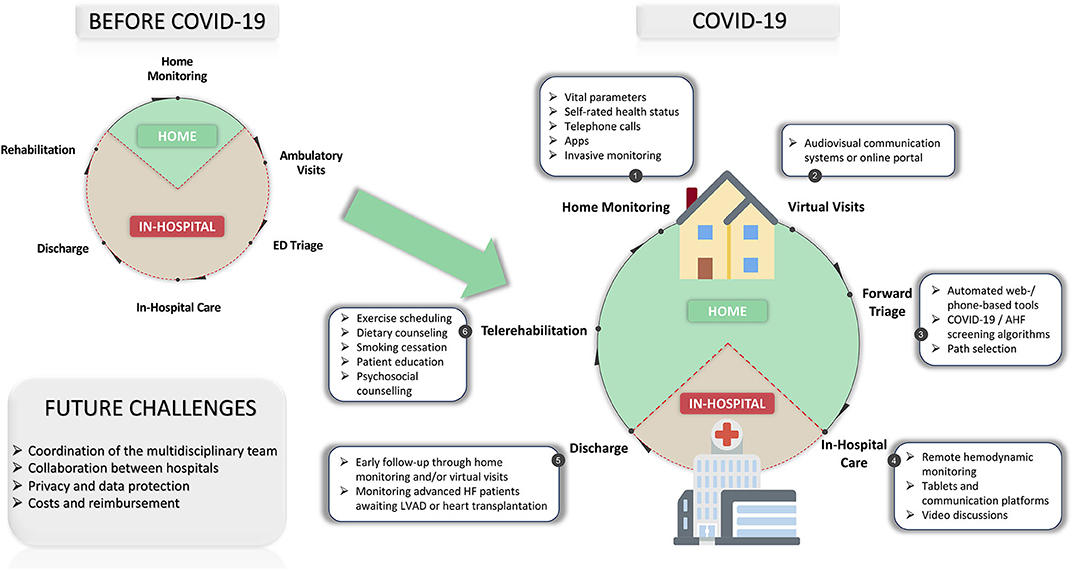
Figure 1. Telemedicine in patients with heart failure before and during COVID-19. AHF, acute heart failure; COVID-19, coronavirus disease 2019; ED, emergency department; LVAD, left ventricular assist device. Modified from https://github.com/emojione/emojione/tree/2.2.7 and https://github.com/twitter/twemoji/. Licensed under a CC BY-SA License (https://creativecommons.org/licenses/by-sa/4.0).
Several strategies can be applied to perform home monitoring of HF patients. Two small studies performed in Boston and New York City showed initial encouraging results of implantable hemodynamic monitoring in COVID-19 (18, 19). However, device and hemodynamic monitoring can only be performed in those patients, which had implanted a device or hemodynamic sensor before the lockdown, which are a minority of the HF population.
A new home monitoring system should be easy to install, be intuitive to users, and provide robust communication (20). Hence, structured telephone support (STS), defined as monitoring, self-care management, or both, delivered using telephone calls (21), may represent the most simple and affordable system for HF centers starting with telemedicine during COVID-19.
A recent study on 103 patients in an Italian tertiary referral center investigated whether a telemedicine service expressly set up during the COVID-19 outbreak changed HF outcomes compared with the same period of 2019 without telemedicine (22). Around 60% of patients accessed telemedicine services at least once, and half of contacts led to a clinical decision (e.g., adjustment of diuretic doses, change of blood pressure drugs, rate controls, and anticoagulant management). In this study, the telemedicine service reduced the composite of HF hospitalization and death compared to patients in the 2019 cohort, which is nevertheless to be interpreted cautiously in light of the previously mentioned reduction of HF hospitalizations during lockdown. In fact, new-established STS interventions are expected to give significant advantages only in the long term, since they could be influenced by a learning-to-care curve due to staff training (23). However, the main goal of telemonitoring during COVID-19 is not to provide superior care than standard, but to offer patients with HF a “health maintenance strategy” which provides an individualized target for each HF patient and adjusts treatment to maintain the monitored parameters as close as possible to ideal (20).
Besides HF patients in general, HF patients who suffer SARS-CoV-2 infection and are treated at home could even more benefit from STS as they are at high risk for complications (8). Remote monitoring can also encourage patients to maintain home isolation and assist in correct timing of stopping the isolation precautions (24).
Virtual visits (VV) include remote visits, in which an audiovisual telecommunication system is used, and e-visits, which are communications between patients and providers through an online portal (9).
A recent statement from the Heart Failure Society of America provides information regarding platforms, workflows, and care models for VV in HF patients (25). Some institutions have already balanced the deferred or canceled face-to-face HF visits with rapid adoption of VV while employing several novel virtual health technologies with overall positive results (26). Specifically, the potential benefits of VV for HF patients are providing access to care and medical advice which would be otherwise difficult to obtain and reducing in-person exposure to SARS-CoV-2. Involvement of caregivers who may be present at home, but not in the outpatient clinic because of restrictions to hospital access, is an additional advantage of VV during the pandemic (25).
Hypothetically, this might represent also a smart working possibility for healthcare personnel, a class of workers for which this possibility is not usually considered or available.
VV may be best utilized for medication titration and optimization in stable patients with chronic HF. While substantial patient information can be gained from such visits, certain challenges remain, such as the adequate assessment of volume status or congestion (27). Thus, in-person visits should be reserved for recently hospitalized patients, patients approaching or with advanced HF, who are new post implantation of a left ventricular assist device (LVAD) or heart transplant, and those with new-onset HF (9).
Respiratory symptoms, as well as functional decline and fatigue, may be early signs of both COVID-19 and of decompensated HF. Hence, stratification of patients before arriving in the emergency department (ED), the so-called forward triage, represents another potential strategy for health care surge control.
Before COVID-19, many EDs modified their triage model by allowing a remote provider to perform intake (28). In an emergency situation, web-conferencing software with a direct line from a triage room to a clinician can be rapidly implemented (29). An automated web- or phone-based tool could guide HF patients with concerning symptoms to determine the need for self-isolation, symptom monitoring, urgent VV, or presenting to the ED (30). Through a structured telemedicine program, detailed medical and exposure histories might be easily obtained. Screening algorithms can be integrated and local epidemiological information can be used to standardize screening and practice patterns across providers (29). The ultimate goal is to guide patients to the right diagnostic–therapeutic pathway while protecting them from unnecessary risk and exposure.
Patients with suspected COVID-19 are isolated immediately upon arrival to emergency departments. In several centers in the USA, telemedicine carts (i.e., systems that integrate displays, cameras, microphones, speakers, and network access) were already successfully deployed into COVID-19 isolation rooms. This initiative increased provider/patient communication and attention to staff safety, improved palliative care and patient support services, lowered consumption of personal protective equipment, increased patient comfort, and reduced the psychological toll of isolation (31).
Certain principles of virtual medicine might be considered when approaching an HF patient seeking acute cardiac care during COVID-19. In this setting, telemedicine measures must aim at limiting unnecessary exposure to affected patients, utilizing remote hemodynamic monitoring and ICU flowcharts to evaluate patient progress and adjust medications (32). These data can be implemented with clinical assessments performed by a single bedside operator to generate operable conditions for safe, remote decision-making, using tools such as electronic stethoscopes and mobile ultrasound probes (32). Initial results of basic thoracic ultrasound programs in ICU are encouraging with rapid adoption of point-of-care ultrasound and commensurate reduction in formal imaging studies (26).
Importantly, COVID-19 has presented healthcare professionals with new and unusual barriers to effective communication between physician, patient, and family. As hospital visits are now frequently prohibited to patients' relatives, novel telecommunication and video options might be considered for patients to speak with loved ones, review treatment choices, and even discuss objectives of care (32). For this purpose, several hospitals introduced use of tablets and video calls with the ultimate goal to favor communication and reduce social isolation of hospitalized patients (33).
Cardiovascular rehabilitation (CR) represents a cornerstone in the treatment of patients with HF. The term telerehabilitation has been used in much of the literature to date and is defined as the delivery of rehabilitation services via information and communication technologies (34). Before COVID-19, it has been shown to be a viable and effective alternative for individuals who are unable to access in-person healthcare services for the management of many conditions. During COVID-19, the reallocation of medical resources as well as the lockdown caused the cessation of all nonurgent medical services, including CR. Therefore, centers had to switch to alternative ways to deliver the core components of CR remotely.
A technology-driven CR model has been proposed, with the assistance of any form of technology (e.g., smartphones, mobile apps, internet, e-mail, webcams, and use of wearable sensors) (35). A recent survey about the implementation of cardiac telerehabilitation services during the COVID-19 pandemic in Belgium (36) showed that half of the answering centers switched to telerehabilitation during the pandemic, mainly for patients that were already undergoing CR. The most frequently used medium to deliver the CR components were online videos (71%) followed by website information (64%) and emails (64%). As the authors of this survey suggested, the remote delivery of CR can also play an important role after the reopening of the rehabilitation centers because of a reduced capacity due to social distancing measures (36). For this purpose, a recent call for action paper of the European Association of Preventive Cardiology provides a practical guide for the setup of a comprehensive cardiac telerehabilitation intervention during the COVID-19 pandemic, which could also be relevant to any cardiovascular disease patient not able to visit CR centers regularly after the COVID-19 pandemic ceases (37).
The evaluation of patients with advanced HF awaiting LVAD placement or heart transplantation may be interrupted during the pandemic, as traditional social work, nutrition, pharmacy referrals, and diagnostic procedures are delayed. Telemedicine offers a platform for these multidisciplinary assessments to occur serially or simultaneously without delay (10). Furthermore, heart transplant recipients on stable immunosuppression at low risk for allograft rejection and hemodynamically optimized LVAD patients may be managed remotely without exposing them to further unnecessary risks (9). A telemonitoring algorithm for patients with LVAD has been recently proposed (38), and it is potentially adaptable to every LVAD center, regardless of the number of LVAD patients or previous experiences.
Since the first wave of the pandemic, clinical trials unrelated to COVID-19 have been paused in most institutions. Telemedicine might avoid the loss of data during lockdown, which can jeopardize the entire research validity. In clinical trials, measurements and data collection are traditionally performed during patient visits. As stated by a recent document of the Heart Failure Association (39), endpoints like symptom status, quality of life questionnaires, or even vital signs could be assessed using home-based testing, with alternative methods such as telephone contacts, app-based self-assessments, or video links.
Although telemedicine provides numerous advantages in many fields, it currently still carries practical limitations and pitfalls, which must be taken into consideration.
First, the hardware required for telemonitoring (i.e., smartphones, tablets, as well as blood pressure machines, scales, etc.) and exercise equipment for telerehabilitation (i.e., treadmill, stationary bike, etc.) may represent a significant financial burden, so either patients must be able to afford this or their health insurance/national health service must provide or reimburse the equipment. Moreover, patients who are unable to utilize the required devices or participate in a telemedicine session unaided either because of old age, poor hearing, cognitive dysfunction, language barriers, or limited education which may require the assistance of a family member or caregiver, who may not be available (40, 41). Finally, the use of telemedicine may be technically limited by poor phone and internet connectivity in rural areas (42, 43).
Telephone support is the most readily applicable and can be performed competently by trained nurses. However, home monitoring creates a large amount of data which must be screened and interpreted by trained staff (44), a process that could be time-consuming. In addition, it requires a dedicated physician to act on critical laboratory abnormalities, all of which can be challenging for physicians managing their practices and possibly receiving limited reimbursement.
The care of a patient with HF requires a multidisciplinary collaboration among physicians, pharmacologists, nurses, physical therapists, nutritionists, and medical social workers. Hence, technology should be conjugated also to ensure communication between the team (e.g., virtual multidisciplinary meetings using video calling in times of social restrictions) (37). In addition, patients with HF often have several comorbidities and may be looked after by more than one hospital, thus requiring intensive collaboration between different specialists and clinics. Authors analyzing the impact of the first COVID-19 wave on patients with chronic diseases described a poor interconnection between telemedicine services operating at higher levels (i.e., secondary or tertiary care facilities) and those deployed in primary care clinics or community pharmacies, preventing to obtain the maximum benefit from these digital solutions (45). Future developments should encourage the collaboration between different professional figures, departments, hospitals, and care institutions.
Due to the fact that telemedicine involves the transmission of patients' confidential information, whether those data are processed and transferred via telephone calls, videoconference, mobile apps, or other platforms, their monitoring requires safe encrypted storage systems which only allow for authorized access to data and protect patient privacy. The interfaces used must be compliant with local regulations both regarding data protection (i.e., GDPR) and encryption (i.e., HIPAA requirements) (46, 47). Physicians implementing telemedicine in clinical practice during COVID-19 suggest using device management software for telehealth devices to create security settings and enforce encryption for devices given to patients (48).
The inclusion of new patients in a telerehabilitation program will be challenging during lockdown, especially with respect to the initial assessment (i.e., baseline stress test) and initial interview, a hurdle that may be overcome by a structured technology-based program with predefined remote assessment methods and audio-visual communication systems (35). However, not all patients could be comfortable with this mode of action, and the problem of financing and delivering technologies to the single patients still persists. An effective approach to reorganize CR could be to start a rehabilitation path in person and subsequently integrate this with a patient-tailored remote telerehabilitation program in order to optimize performance and extend patients' education.
Finally, telemedicine services are not yet included in the essential levels of care in many countries (9, 29, 45). During COVID-19, some efforts were already made by agencies like the US Food and Drug Administration, which is facilitating the use of remote monitoring devices, and Centers for Medicare and Medicaid Services, which is paying for telehealth services at the same rate they would have been paid, if provided in person (27). However, these costs were covered only due to the emergency situation. In order to continue after the pandemic, the shift to telemedicine should be done in parallel with developments in policymaking (27).
Evidence coming from observational studies on telemedicine during COVID-19 is of great importance. Centers having a dedicated HF unit should collect information regarding their own telemedicine approach, with the aim of defining strengths and weaknesses of each program and its impact on HF patients' care. This enormous amount of data provided during the pandemic should then be evaluated to be wisely implemented in daily clinical practice also after the crisis.
By evaluating results of telemedicine programs during COVID-19, one should keep in mind that in the particular setting of a pandemic, a system that is cost-efficient, user-friendly, and person-centered does not need to show that it improves outcome, but only that it is not inferior to traditional ways of delivering care and thus allows a safe maintenance of the status quo (20).
Although this pandemic has accelerated implementation of technology in the clinical setting, telemedicine should not be considered a cure-all for clinical scenarios. At its core, it remains a synergistic extension of the care team (49) and cannot entirely reproduce the bond-forming element of the traditional doctor–patient relationship based on direct face-to-face interactions (50).
COVID-19 represents a serious threat for the HF population due to both higher risk of severe disease and death and reduced availability of outpatient care. Telemedicine in all its different forms and possibilities can be adopted to ensure continued healthcare delivery to patients with HF. Thus, we are witnessing its rapid, large-scale implementation during the pandemic. However, there are still several limitations and issues that should be solved in order to continue providing high-quality telemedicine services in patients with HF also after COVID-19.
GT and DW drafted the manuscript. GMC, SG, MR, LB, GP, JD, PA, and MV critically reviewed the manuscript. All authors have participated in the work and have reviewed and agreed with the content of the article. None of the article contents are under consideration for publication in any other journal or have been published in any journal.
JD is a researcher for the Limburg Clinical Research Center (LCRC) UHasselt-ZOL-Jessa, supported by the foundation Limburg Sterk Merk (LSM), province of Limburg, Flemish government, Hasselt University, Ziekenhuis Oost-Limburg, and Jessa Hospital.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. (2020) 323:1061. doi: 10.1001/jama.2020.1585
2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
3. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
4. Guan W, Ni Z, Hu Y, Liang W-h, Qu C-q, He J-x, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
5. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
6. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. (2020) 5:802–10. doi: 10.1001/jamacardio.2020.0950
7. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. (2020) 5:811–18. doi: 10.1001/jamacardio.2020.1017
8. Zhang Y, Stewart Coats AJ, Zheng Z, Adamo M, Ambrosio G, Anker SD, et al. Management of heart failure patients with COVID-19. A Joint Position Paper of the Chinese Heart Failure Association & National Heart Failure Committee and the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. (2020) 22:941–56. doi: 10.1002/ejhf.1915
9. DeFilippis EM, Reza N, Donald E, Givertz MM, Lindenfeld J, Jessup M. Considerations for heart failure care during the coronavirus disease 2019 (COVID-19) pandemic. JACC Heart Fail. (2020) 8:681–91. doi: 10.1016/j.jchf.2020.05.006
10. Reza N, DeFilippis EM, Jessup M. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Heart Fail. (2020) 13:e007219. doi: 10.1161/CIRCHEARTFAILURE.120.007219
11. Han Y, Zeng H, Jiang H, Yang Y, Yuan Z, Cheng X, et al. CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic. Circulation. (2020) 141:e810–e816. doi: 10.1161/CIRCULATIONAHA.120.047011
12. Tersalvi G, Vicenzi M, Calabretta D, Biasco L, Pedrazzini G, Winterton D. Elevated troponin in patients with coronavirus disease 2019: possible mechanisms. J Card Fail. (2020) 26:470–5. doi: 10.1016/j.cardfail.2020.04.009
13. Tersalvi G, Veronese G, Winterton D. Emerging evidence of myocardial injury in COVID-19: a path through the smoke. Theranostics. (2020) 10:9888–9. doi: 10.7150/thno.50788
14. Alon D, Stein GY, Korenfeld R, Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS One. (2013) 8:e72476. doi: 10.1371/journal.pone.0072476
15. Sandoval C, Walter SD, Krueger P, Smieja M, Smith A, Yusuf S, et al. Risk of hospitalization during influenza season among a cohort of patients with congestive heart failure. Epidemiol Infect. (2007) 135:574–82. doi: 10.1017/S095026880600714X
16. Kytömaa S, Hegde S, Claggett B, Udell JA, Rosamond W, Temte J, et al. Association of influenza-like illness activity with hospitalizations for heart failure: the atherosclerosis risk in communities study. JAMA Cardiol. (2019) 4:363. doi: 10.1001/jamacardio.2019.0549
17. Bromage DI, Cannatà A, Rind IA, Gregorio C, Piper S, Shah AM, et al. The impact of COVID-19 on heart failure hospitalization and management: report from a Heart Failure Unit in London during the peak of the pandemic. Eur J Heart Fail. (2020) 22:978–84. doi: 10.1002/ejhf.1925
18. Almufleh A, Ahluwalia M, Givertz MM, Weintraub J, Young M, Cooper I, et al. Short-term outcomes in ambulatory heart failure during the COVID-19 pandemic: insights from pulmonary artery pressure monitoring. J Card Fail. (2020) 26:633–4. doi: 10.1016/j.cardfail.2020.05.021
19. Oliveros E, Mahmood K, Mitter S, Pinney SP, Lala A. Letter to the Editor: pulmonary artery pressure monitoring during the COVID-19 pandemic in New York city. J Card Fail. (2020) 26:900–1. doi: 10.1016/j.cardfail.2020.08.003
20. Cleland JGF, Clark RA, Pellicori P, Inglis SC. Caring for people with heart failure and many other medical problems through and beyond the COVID-19 pandemic: the advantages of universal access to home telemonitoring. Eur J Heart Fail. (2020) 22:995–8. doi: 10.1002/ejhf.1864
21. Bui AL, Fonarow GC. Home monitoring for heart failure management. J Am Coll Cardiol. (2012) 59:97–104. doi: 10.1016/j.jacc.2011.09.044
22. Salzano A, D'Assante R, Stagnaro FM, Valente V, Crisci G, Giardino F, et al. Heart failure management during COVID-19 outbreak in Italy. Telemedicine experience from a heart failure university tertiary referral centre. Eur J Heart Fail. (2020) 22:1048–50. doi: 10.1002/ejhf.1911
23. Tersalvi G, Vicenzi M, Kirsch K, Gunold H, Thiele H, Lombardi F, et al. Structured telephone support programs in chronic heart failure may be affected by a learning curve. J Cardiovasc Med. (2020) 21:231–7. doi: 10.2459/JCM.0000000000000934
24. Razonable RR, Pennington KM, Meehan AM, Wilson JW, Froemming AT, Bennett CE, et al. A collaborative multidisciplinary approach to the management of coronavirus disease 2019 in the hospital setting. Mayo Clin Proc. (2020) 95:1467–81. doi: 10.1016/j.mayocp.2020.05.010
25. Gorodeski EZ, Goyal P, Cox ZL, Thibodeau JT, Reay RE, Rasmusson K, et al. Virtual visits for care of patients with heart failure in the era of COVID-19: a statement from the heart failure society of America. J Card Fail. (2020) 26:448–56. doi: 10.1016/j.cardfail.2020.04.008
26. Almufleh A, Givertz MM. Virtual health during a pandemic: redesigning care to protect our most vulnerable patients. Circ Heart Fail. (2020) 13:e007317. doi: 10.1161/CIRCHEARTFAILURE.120.007317
27. Abraham WT, Fiuzat M, Psotka MA, O'Connor CM. Heart failure collaboratory statement on heart failure remote monitoring in the landscape of COVID-19 and social distancing. JACC Heart Fail. (2020) 8:423–5. doi: 10.1016/j.jchf.2020.03.005
28. Joshi AU, Randolph FT, Chang AM, Slovis BH, Rising KL, Sabonjian M, et al. Impact of emergency department tele-intake on left without being seen and throughput metrics. Acad Emerg Med. (2020) 27:139–47. doi: 10.1111/acem.13890
29. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. (2020) 382:1679–81. doi: 10.1056/NEJMp2003539
30. Alwashmi MF. The use of digital health in the detection and management of COVID-19. Int J Environ Res Public Health. (2020) 17:2906. doi: 10.3390/ijerph17082906
31. Bains J, Greenwald PW, Mulcare MR, Leyden D, Kim J, Shemesh AJ, et al. Utilizing telemedicine in a novel approach to COVID-19 management and patient experience in the emergency department. Telemed J E Health. (2020). doi: 10.1089/tmj.2020.0162. [Epub ahead of print].
32. Katz JN, Sinha SS, Alviar CL, Dudzinski DM, Gage A, Brusca SB, et al. Disruptive modifications to cardiac critical care delivery during the Covid-19 pandemic: an international perspective. J Am Coll Cardiol. (2020) 76:72–84. doi: 10.1016/j.jacc.2020.04.029
33. Goulabchand R, Boclé H, Vignet R, Sotto A, Loubet P. Digital tablets to improve quality of life of COVID-19 older inpatients during lockdown. Eur Geriatr Med. (2020) 11:705–6. doi: 10.1007/s41999-020-00344-9
34. Brennan D, Tindall L, Theodoros D, Brown J, Campbell M, Christiana D, et al. A blueprint for telerehabilitation guidelines. Int J Telerehab. (2010) 2:31–4. doi: 10.5195/IJT.2010.6063
35. Babu AS, Arena R, Ozemek C, Lavie CJ. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol. (2020) 36:792–4. doi: 10.1016/j.cjca.2020.04.023
36. Scherrenberg M, Frederix I, De Sutter J, Dendale P. Use of cardiac telerehabilitation during COVID-19 pandemic in Belgium. Acta Cardiol. (2020) :1-4. doi: 10.1080/00015385.2020.1786625
37. Scherrenberg M, Wilhelm M, Hansen D, Völler H, Cornelissen V, Frederix I, et al. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. (2020). doi: 10.1177/2047487320939671. [Epub ahead of print].
38. Mariani S, Hanke JS, Dogan G, Schmitto JD. Out of hospital management of LVAD patients during COVID-19 outbreak. Artif Organs. (2020) 44:873–6. doi: 10.1111/aor.13744
39. Anker SD, Butler J, Khan MS, Abraham WT, Bauersachs J, Bocchi E, et al. Conducting clinical trials in heart failure during (and after) the COVID-19 pandemic: an Expert Consensus Position Paper from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. (2020) 41:2109–17. doi: 10.1093/eurheartj/ehaa461
40. Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One. (2019) 14:e0221848. doi: 10.1371/journal.pone.0221848
41. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare. (2018) 24:4–12. doi: 10.1177/1357633X16674087
42. Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, et al. Telehealth in response to the Covid-19 Pandemic: implications for rural health disparities. J Am Med Inform Assoc. (2020) 27:1816–8. doi: 10.1093/jamia/ocaa156
43. Zachrison KS, Boggs KM, Hayden EM, Espinola JA, Camargo CA. Understanding barriers to telemedicine implementation in rural emergency departments. Ann Emerg Med. (2020) 75:392–9. doi: 10.1016/j.annemergmed.2019.06.026
44. Angermann CE, Störk S, Gelbrich G, Faller H, Jahns R, Frantz S, et al. Mode of action and effects of standardized collaborative disease management on mortality and morbidity in patients with systolic heart failure: the interdisciplinary network for heart failure (INH) study. Circ Heart Fail. (2012) 5:25–35. doi: 10.1161/CIRCHEARTFAILURE.111.962969
45. Omboni S. Telemedicine during the COVID-19 in Italy: a missed opportunity? Telemed J E Health. (2020) 26:973–5. doi: 10.1089/tmj.2020.0106
46. HealthITSecurity. Healthcare Data Encryption not 'Required,' but Very Necessary. HealthITSecurity (2017). Available online at: https://healthitsecurity.com/news/healthcare-data-encryption-not-required-but-very-necessary (accessed September 17, 2020).
47. HIPAA Encryption Requirements. HIPAA Journal. Available online at: https://www.hipaajournal.com/hipaa-encryption-requirements/ (accessed September 17, 2020).
48. Heslin SM, Nappi M, Kelly G, Crawford J, Morley EJ, Lingam V, et al. Rapid creation of an emergency department telehealth program during the COVID-19 pandemic. J Telemed Telecare. (2020). doi: 10.1177/1357633X20952632. [Epub ahead of print].
49. Czartoski T. Commentary: Telehealth Holds Promise, but Human Touch Still Needed. Articles, Abstracts, and Reports. 1278 (2019). Available online at: https://digitalcommons.psjhealth.org/publications/1278
Keywords: COVID-19, coronavirus, telemedicine, heart failure, remote monitoring, virtual visits, forward triage, telerehabilitation
Citation: Tersalvi G, Winterton D, Cioffi GM, Ghidini S, Roberto M, Biasco L, Pedrazzini G, Dauw J, Ameri P and Vicenzi M (2020) Telemedicine in Heart Failure During COVID-19: A Step Into the Future. Front. Cardiovasc. Med. 7:612818. doi: 10.3389/fcvm.2020.612818
Received: 30 September 2020; Accepted: 10 November 2020;
Published: 09 December 2020.
Edited by:
Hendrik Tevaearai Stahel, Bern University Hospital, SwitzerlandReviewed by:
Elizabeth S. Kaufman, The MetroHealth System, United StatesCopyright © 2020 Tersalvi, Winterton, Cioffi, Ghidini, Roberto, Biasco, Pedrazzini, Dauw, Ameri and Vicenzi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gregorio Tersalvi, dGVyc2FsdmlAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.