Corrigendum: Impact of Renal Function on Long-Term Clinical Outcomes in Patients With Coronary Chronic Total Occlusions: Results From an Observational Single-Center Cohort Study During the Last 12 Years
- 1Department of Cardiology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
- 2Department of Radiology, Fuyang Hospital of Anhui Medical University, Fuyang, China
- 3Department of Cardiology, Capital Medical University Affiliated Beijing Friendship Hospital, Beijing, China
Background: The number of coronary chronic total occlusion (CTO) patients with renal insufficiency is huge, and limited data are available on the impact of renal insufficiency on long-term clinical outcomes in CTO patients. We aimed to investigate clinical outcomes of CTO percutaneous coronary intervention (PCI) vs. medical therapy (MT) in CTO patients according to baseline renal function.
Methods: In the study population of 2,497, 1,220 patients underwent CTO PCI and 1,277 patients received MT. Patients were divided into four groups based on renal function: group 1 [estimated glomerular filtration rate (eGFR) ≥ 90 ml/min/1.73 m2], group 2 (60 ≤ eGFR <90 ml/min/1.73 m2), group 3 (30 ≤ eGFR <60 ml/min/1.73 m2), and group 4 (eGFR <30 ml/min/1.73 m2). Major adverse cardiac event (MACE) was the primary end point.
Results: Median follow-up was 2.6 years. With the decline in renal function, MACE (p < 0.001) and cardiac death (p < 0.001) were increased. In group 1 and group 2, MACE occurred less frequently in patients with CTO PCI, as compared to patients in the MT group (15.6% vs. 22.8%, p < 0.001; 15.6% vs. 26.5%, p < 0.001; respectively). However, there was no significant difference in terms of MACE between CTO PCI and MT in group 3 (21.1% vs. 28.7%, p = 0.211) and group 4 (28.6% vs. 50.0%, p = 0.289). MACE was significantly reduced for patients who received successful CTO PCI compared to patients with MT (16.7% vs. 22.8%, p = 0.006; 16.3% vs. 26.5%, p = 0.003, respectively) in group 1 and group 2. eGFR < 30 ml/min/1.73 m2, age, male gender, diabetes mellitus, heart failure, multivessel disease, and MT were identified as independent predictors for MACE in patients with CTOs.
Conclusions: Renal impairment is associated with MACE in patients with CTOs. For treatment of CTO, compared with MT alone, CTO PCI may reduce the risk of MACE in patients without chronic kidney disease (CKD). However, reduced MACE from CTO PCI among patients with CKD was not observed. Similar beneficial effects were observed in patients without CKD who underwent successful CTO procedures.
Introduction
Renal insufficiency is associated with an increased risk of mortality and cardiovascular events in patients with coronary artery disease (CAD) after percutaneous coronary intervention (PCI) or surgical revascularization (1–3). Coronary chronic total occlusions (CTOs), as a special type of CAD, are observed in 10–30% of all diagnostic coronary angiography and remain a challenging obstacle in coronary intervention (4–6). The number of CTO patients with renal insufficiency was huge (7, 8). Renal insufficiency was identified as an important high-risk factor for adverse outcomes or death in patients with CTOs (9, 10). Successful CTO procedures have been reported to improve left ventricular function and reduce adverse clinical events (11–13). However, data on the impact of renal insufficiency on clinical outcomes in CTO patients are scarce. Further, the optimal treatment strategy for these high-risk subjects is unknown.
Therefore, this study aimed to investigate clinical outcomes of CTO PCI vs. medical therapy (MT) in CTO patients according to baseline renal function.
Materials and Methods
Study Population
From a total of 27,231 patients undergoing coronary angiography at our institution between January 2007 and December 2018, we identified 2,980 (10.9%) patients who had at least one CTO lesion. Patients who underwent coronary artery bypass grafting (CABG) and those with acute ST-segment elevation myocardial infarction (MI) within the preceding 2 days, history of CABG, missing renal function data, cardiogenic shock, or malignant tumor were excluded from the study (13), leaving a final population of 2,497 patients, treated either by PCI or by MT. Patients referred for revascularization had presence of angina symptoms, or myocardial viability or inducible ischemia based on non-invasive imaging, including dimensional echocardiography, cardiac magnetic resonance imaging, or myocardial perfusion scintigraphy (14, 15). Baseline demographics and angiographic and procedural characteristics were collected and recorded. Patients were followed by telephone contacts or outpatient visits. The present study was approved by the review board of our institution and complied with the principles laid down in the Declaration of Helsinki.
Definitions and End Points
Coronary CTO was defined as a true total occlusion with Thrombolysis In Myocardial Infarction (TIMI) 0 flow for >3 months (16). Duration was estimated according to clinical history or prior angiogram. Renal function was assessed according to the estimated glomerular filtration rate (eGFR) based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (17). Patients were divided into four groups according to baseline eGFR: group 1 (eGFR ≥ 90 ml/min/1.73 m2), group 2 (60 ≤ eGFR <90 ml/min/1.73 m2), group 3 (30 ≤ eGFR <60 ml/min/1.73 m2), and group 4 (eGFR <30 ml/min/1.73 m2). Chronic kidney disease (CKD) was defined as eGFR <60 ml/min/1.73 m2. Angiographic success of the CTO PCI was defined as <30% residual stenosis with TIMI grade ≥ 3 flow and no occlusion of a significant side branch, flow-limiting dissection, distal embolization, or angiographic thrombus (18). The primary end point for this study was major adverse cardiac event (MACE), which was defined as a composite of cardiac mortality, MI, or target-vessel revascularization (TVR). The secondary outcome was cardiac death. Definitions of cardiac death, MI, or TVR were described previously according to Standardized Definitions (8).
Medical and Invasive Treatment
MT included statins, antiplatelet medication, β-blockers, nitrate, and renin–angiotensin system blockade. PCIs were performed in a standard manner. The patients received aspirin (100 mg) and clopidogrel (75 mg) daily before the intervention. After PCI, dual-antiplatelet medication was prescribed for at least 12 months. Patients with CKD received hydration to prevent the occurrence of acute kidney injury before and after the CTO procedure.
Statistical Analysis
Data are presented as mean ± SD or as percentages. Kruskal–Wallis test was performed for comparison of continuous data, and chi-square test analysis or Fisher's exact test was used for categorical variables comparison. Long-term outcomes were determined by using Kaplan–Meier survival curves and compared by the log-rank test. A multivariate Cox regression model was used to identify the independent predictors of MACE at follow-up. Covariates that were with p < 0.05 on univariate analysis were considered candidate variables including age (per year increment), gender, heart failure, diabetes mellitus, left ventricular ejection fraction (LVEF) ≤ 40%, right coronary artery (RCA) CTO, multivessel disease, and MT. All statistical tests were two-sided and considered significant at p < 0.05. All analyses were conducted using IBM SPSS Statistics v24.0 (Chicago, IL) and Stata v15.1 (StataCorp LLC, TX).
Results
Baseline Characteristics
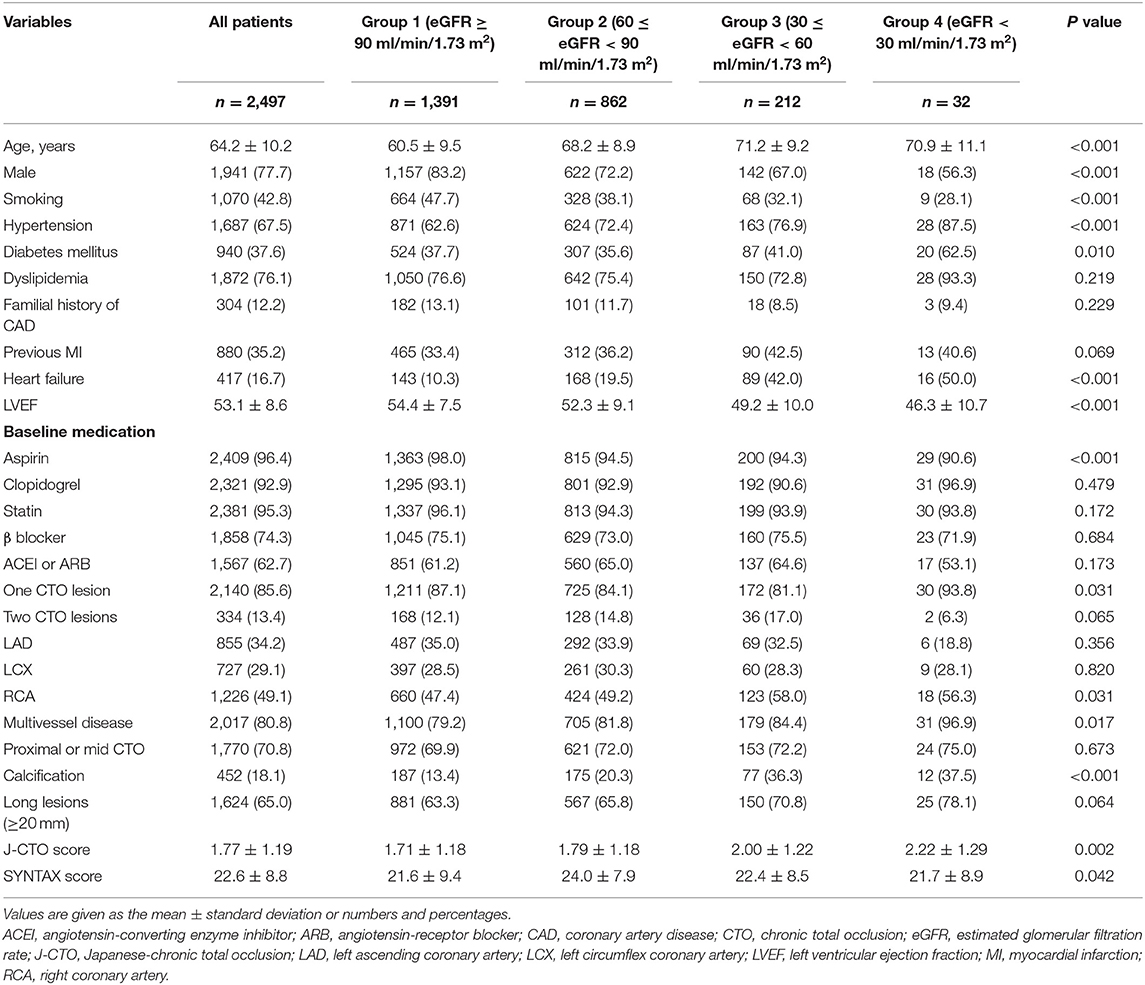
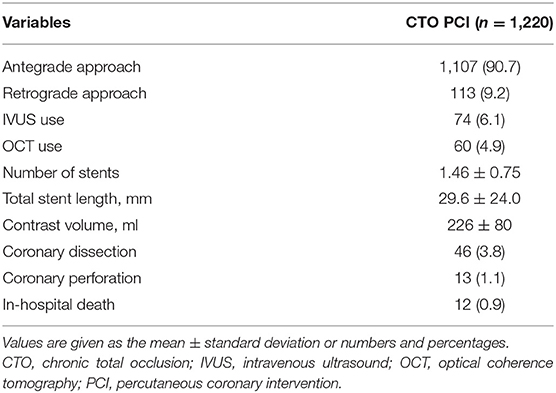
The prevalence of CTO was 10.9% in the present study. After exclusion, in the study population of 2,497, 1,220 patients underwent CTO PCI (710 patients had successful PCI and 510 patients had a failed PCI, and the success rate was 58.2%) and 1,277 patients received MT. Among this population, 1,391 (55.7%), 862 (34.5%), 212 (8.5%), and 32 (1.3%) patients were classified into groups 1–4, respectively. There were five patients with eGFR <15 ml/min/1.73 m2. The baseline clinical and angiographic characteristics are listed in Table 1. With decreasing renal function, patients tended to be older and had higher percentage of female, hypertension, and heart failure, but had a lower prevalence of smoker and lower LVEF. In angiographic characteristics, calcification, multivessel disease, and high Japanese-chronic total occlusion (J-CTO) score were more prevalent in patients with renal impairment. However, dyslipidemia, previous MI, familial history of CAD, the usage of medication except for aspirin, 2 CTO lesions, and LAD CTO were similar between the four groups. Procedural details and in-hospital death are present in Table 2.
Long-Term Outcomes
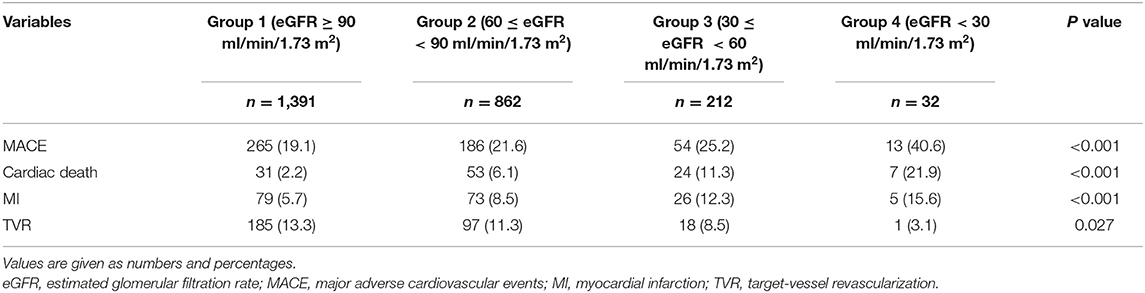
During a median follow-up of 2.6 (interquartile range, 1.2–4.7) years, MACE (p <0.001), cardiac death (p < 0.001), and MI (p < 0.001) were increased with decreasing renal function. However, the incidence of TVR (p < 0.001) was decreased with decreasing renal function (Table 3) (Figure 1).
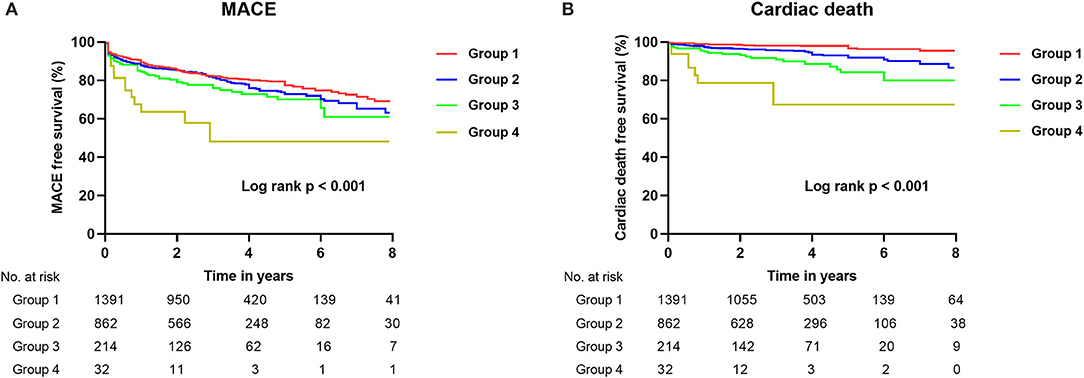
Figure 1. Kaplan–Meier curves for MACE (A) and cardiac death (B) during follow-up in total patients with CTO according to baseline renal function. CTO, chronic total occlusion; MACE, major adverse cardiovascular events; Group 1 [estimated glomerular filtration rate (eGFR) ≥ 90 ml/min/1.73 m2]; Group 2 (60 ≤ eGFR < 90 ml/min/1.73 m2); Group 3 (30 ≤ eGFR < 60 ml/min/1.73 m2); Group 4 (eGFR <30 ml/min/1.73 m2).
The clinical outcomes of the two different strategies (MT and CTO PCI) for CTO patients in the four groups are shown in Table 4. In group 1 and group 2, MACE occurred less frequently in patients with CTO PCI, as compared to patients in the MT group (15.6% vs. 22.8%, p < 0.001; 15.6% vs. 26.5%, p < 0.001, respectively). However, there was no significant difference on MACE between CTO PCI and MT in group 3 (21.1% vs. 28.7%, p = 0.211) and group 4 (28.6% vs. 50.0%, p = 0.289). The differences were not significant on cardiac mortality and MI regarding the two treatment strategies among the four groups (Figure 2).
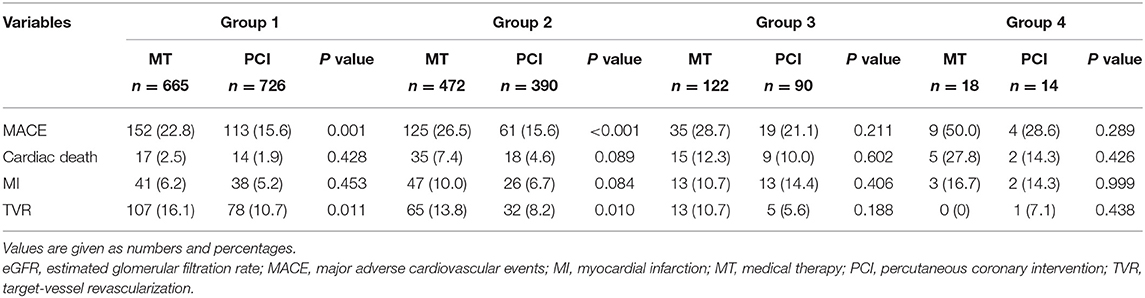
Table 4. Clinical outcomes of all patients stratified by eGFR in the medical therapy and PCI groups.
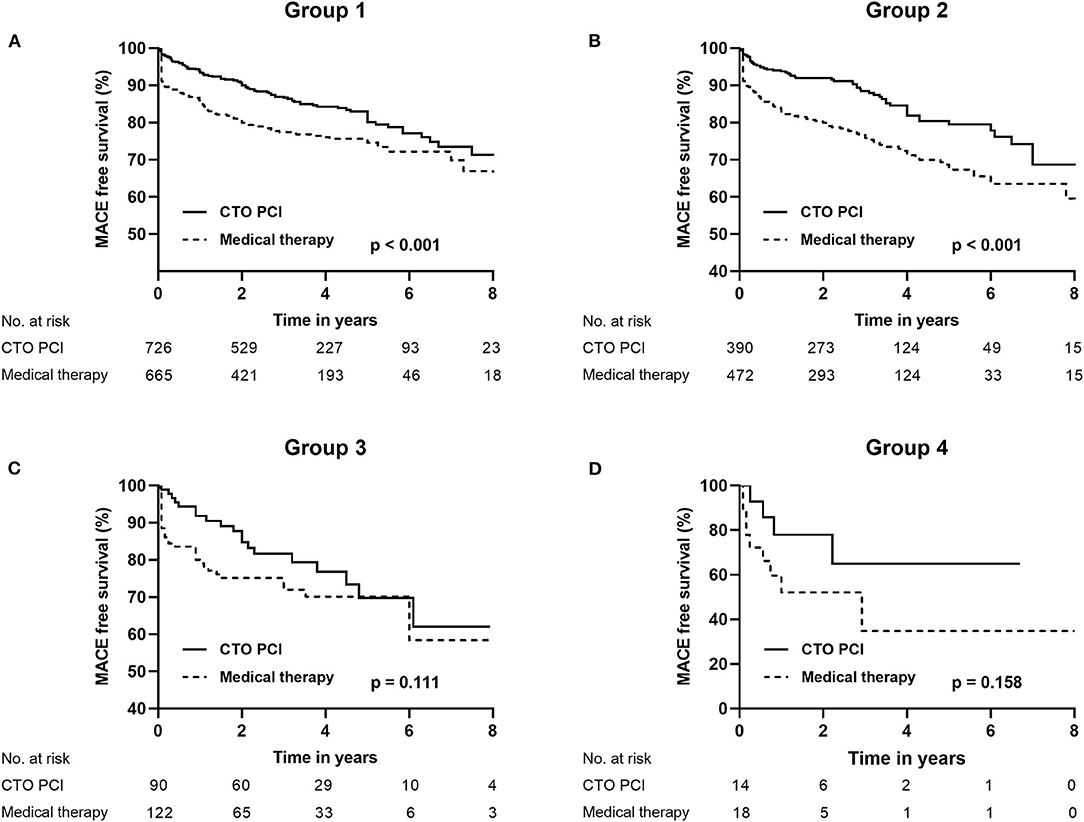
Figure 2. Kaplan–Meier curves for MACE (A–D) during follow-up for CTO PCI vs. medical therapy in CTO patients according to baseline renal function (groups 1, 2, 3, and 4). CTO, chronic total occlusion; MACE, major adverse cardiovascular events; PCI, percutaneous coronary intervention; Group 1 [estimated glomerular filtration rate (eGFR) ≥ 90 ml/min/1.73 m2]; Group 2 (60 ≤ eGFR < 90 ml/min/1.73 m2); Group 3 (30 ≤ eGFR < 60 ml/min/1.73 m2); Group 4 (eGFR <30 ml/min/1.73 m2).
To reduce the impact of failed CTO procedures on outcomes, we compared the clinical outcomes of MT vs. successful CTO PCI in Table 5. In group 1 and group 2, rate of MACE was significantly reduced for patients who received successful CTO PCI compared to patients with MT (16.7% vs. 22.8%, p = 0.006; 16.3% vs. 26.5%, p = 0.003; respectively). However, we did not observe a significant difference on MACE between successful CTO PCI and MT in group 3 (23.3% vs. 28.7%, p = 0.492) and group 4 (37.5% vs. 50.0%, p = 0.683). There were no significant differences in terms of MI and TVR regarding the successful CTO PCI and MT among the four groups.
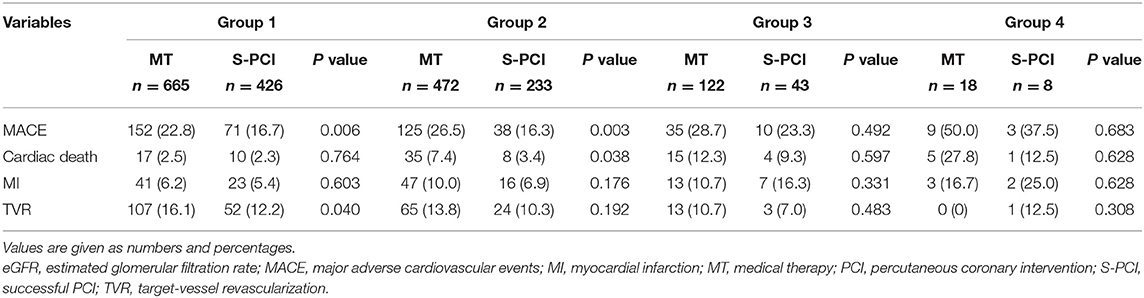
Table 5. Clinical outcomes of all patients stratified by eGFR in the medical therapy and successful PCI groups.
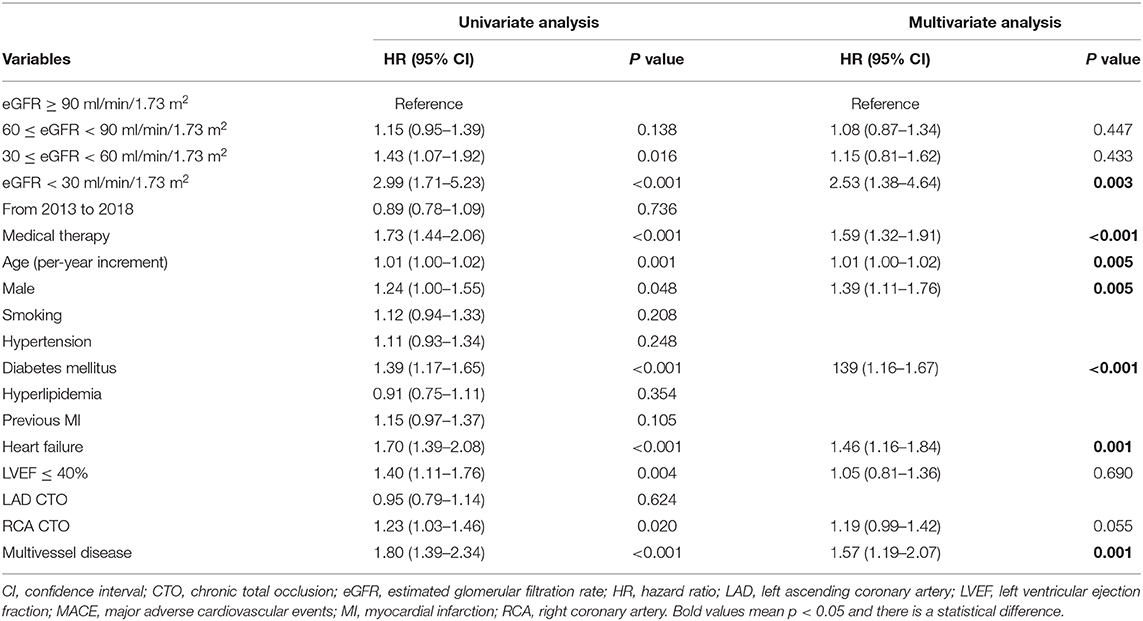
After multivariate analysis, Cox model identified eGFR <30 ml/min/1.73 m2 [hazard ratio (HR) 2.53, 95% confidence interval (CI): 1.38–4.64, p = 0.003], MT (HR 1.59, 95% CI: 1.32–1.91, p < 0.001), age (per-year increment) (HR 1.01, 95% CI: 1.00–1.02, p = 0.005), male gender (HR 1.39, 95% CI: 1.11–1.76, p = 0.005), diabetes mellitus (HR 1.39, 95% CI: 1.16–1.67, p < 0.001), heart failure (HR 1.46, 95% CI: 1.16–1.84, p = 0.001), and multivessel disease (HR 1.57, 95% CI: 1.19–2.07, p = 0.001) as independent predictors for MACE in patients with CTOs. However, 30 ≤ eGFR < 60 ml/min/1.73 m2 (p = 0.433) and LVEF ≤ 40% (p = 0.690) were not associated with MACE in this cohort (Table 6).
Discussion
This study demonstrated three major findings. Firstly, with the decline in renal function, patients tended to be older and had more comorbidities, including hypertension, diabetes mellitus, heart failure, and low LVEF. Secondly, MACE and cardiac death were increased with decreasing renal function. Thirdly, initial CTO PCI procedures were associated with reduced MACE in patients without CKD, but not in patients with CKD. Similar beneficial effects were observed in patients without CKD who underwent successful CTO procedures. To the best of our knowledge, this is the first large cohort study to report the impact of renal function on long-term clinical outcomes in patients with coronary CTOs.
Renal impairment is associated with inflammatory, oxidative stress, and metabolic perturbations and coronary microcirculation disorders (1, 19–22), all of which are associated with accelerated atherosclerosis and endothelial dysfunction and increased incidence of hypertension, diabetes mellitus, dyslipidemia, multivessel disease, and coronary calcified lesions (23, 24). These may be the mechanisms that renal dysfunction contribute to adverse short-term as well as long-term outcomes. In the previous studies, a cardiologist evaluated the outcomes after revascularization in CAD patients with renal impairment, and they found that the presence of renal impairment was associated with lower success rate and increasing complication and cardiac death or other adverse cardiovascular events (3, 25, 26).
CTO remains a challenging obstacle in coronary intervention (27). The benefits from successful revascularization for CTO, such as reduced death and angina, had been proved by several studies (9, 28). The large registry reported that PCI for CTO lesions account for <5% of coronary interventions in clinical practice (29), and most of the patients with CTO lesions still are treated conservatively (10, 30). A prior study reported that the prevalence of CTO in a non-infarct-related artery was 13% in patients with renal insufficiency compared with 7% in those with normal renal function (10). The number of CTO patients with renal insufficiency was huge. Previous studies have mainly focused on the impact of renal insufficiency on clinical outcomes after revascularization among acute coronary syndrome patients or unselected patients. However, patients with significant renal insufficiency are regularly excluded from most studies relevant to CTO, and little data exist on the impact of renal impairment on outcomes in among patients with CTOs. Furthermore, which strategy is optimal in this high-risk population remains unknown. Consequently, evaluating clinical outcomes of CTO PCI vs. MT is crucial for decision making in clinical practice among patients with renal dysfunction.
Our study provides evidence that, with decreasing renal function, the prevalence of MACE and cardiac death was increased, in accordance with the findings of Stähli and coworkers (31). Furthermore, we found that PCI for CTO was associated with reduced MACE compared to MT alone among patients without CKD. Nonetheless, no beneficial effects of CTO PCI were observed in patients with 30 ≤ eGFR <60 ml/min/1.73 m2 and patients with eGFR <30 ml/min/1.73 m2. These findings were supported by recent studies, which showed no decreased adverse outcomes following CTO PCI in patients with CKD (32, 33). Of note, even in the recent ISCHEMIA-CKD trial, revascularization for stable CAD did not improve outcomes among patients with advanced CKD (eGFR <30 ml/min/1.73 m2), as compared with medical treatment (34). Additionally, we found that eGFR <30 ml/min/1.73 m2 was a strong predictor of MACE in CTO patients, which were consistent with findings of previous studies (9, 31).
Of note, failure of CTO PCI was associated with increasing baseline patient and lesion complexity, and therefore, the poorer clinical outcomes were more common among this population (8, 13). To reduce the impact of failed CTO procedures on outcomes, we compared the clinical outcomes of MT vs. successful CTO PCI. We found that successful CTO PCI was associated with reduced MACE compared to MT alone among patients without CKD but not in patients with CKD, which was similar with the results of MT vs. initial CTO PCI.
Up to now, no guideline or widely recognized consensus on treatment strategy of CTO patients with renal insufficiency and the prognosis of this population is unknown. Therefore, our findings strengthen the idea that a careful patient selection is important and suggest that, considering prognosis as well as the multiple comorbidities, operative complications, and high expense, aggressive revascularization should be considered carefully for these high-risk patients with significant renal insufficiency.
Limitations should be taken into consideration. Firstly, the analysis is limited by an observational design and the patients with CKD is relatively small. Secondly, as the time period of the study is long (more than 10 years), the changes of PCI materials and technique or medical treatment may have the impact on the clinical outcomes, though we have considered these factors in our previous study (4). Additionally, the infrequent use of imaging devices, such as IVUS and OCT, due to high cost in the present study may lower the success rate of CTO PCI and affect the outcomes, though our success rate was similar to the National Cardiovascular Data Registry from the US (29). Thirdly, the crossovers of MT and CTO PCI groups may limit conclusions, even though the rate was very low. Despite these limitations, this is the first large cohort study to report different treatment strategies on clinical outcomes in patients with coronary chronic total occlusions according to baseline renal function, and our study provided valuable data among this high-risk population, which may benefit future investigations.
Conclusions
With decreasing renal function, the prevalence of MACE and cardiac death was increased among patients with CTOs. For treatment of CTO, compared with MT alone, CTO PCI may reduce the risk of MACE in patients without CKD. However, reduced MACE from CTO procedures among patients with CKD was not observed. Similar beneficial effects were observed in patients without CKD who underwent successful CTO procedures. Large randomized clinical trials are required to confirm the findings of the present study.
Data Availability Statement
The datasets generated for this study are available on motivated request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by First Affiliated Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LG and HD prepared the manuscript. All authors contributed to data collection and analyses, edited the draft manuscript, and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Anavekar NS, McMurray JJV, Velazquez EJ, Solomon SD, Kober L, Rouleau J-L, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N. Engl. J. Med. (2004) 351:1285–95. doi: 10.1056/NEJMoa041365
2. Sadeghi HM, Stone GW, Grines CL, Mehran R, Dixon SR, Lansky AJ, et al. Impact of renal insufficiency in patients undergoing primary angioplasty for acute myocardial infarction. Circulation. (2003) 108:2769–75. doi: 10.1161/01.CIR.0000103623.63687.21
3. Cooper WA, O'Brien SM, Thourani VH, Guyton RA, Bridges CR, Szczech LA, et al. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the Society of Thoracic Surgeons National Adult Cardiac Database. Circulation. (2006) 113:1063–70. doi: 10.1161/CIRCULATIONAHA.105.580084
4. Guo L, Wu J, Zhong L, Ding HY, Xu JY, Zhou XC, et al. Two-year clinical outcomes of medical therapy vs. revascularization for patients with coronary chronic total occlusion. Hell. J. Cardiol. (2019). doi: 10.1016/j.hjc.2019.03.006. [Epub ahead of print].
5. Guo L, Zhang XY, Lv HC, Zhong L, Wu J, Ding HY, et al. Long-term outcomes of successful revascularization for patients with coronary chronic total occlusions: a report of 1,655 patients. Front. Cardiovasc. Med. (2020) 7:116. doi: 10.3389/fcvm.2020.00116
6. Grantham JA, Marso SP, Spertus J, House J, Holmes DR, Rutherford BD. Chronic total occlusion angioplasty in the united states. JACC Cardiovasc. Interv. (2009) 2:479–86. doi: 10.1016/j.jcin.2009.02.008
7. Bataille Y, Plourde G, Machaalany J, Abdelaal E, Déry J-P, Larose É, et al. Interaction of chronic total occlusion and chronic kidney disease in patients undergoing primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. Am. J. Cardiol. (2013) 112:194–9. doi: 10.1016/j.amjcard.2013.03.010
8. Guo L, Wang JJ, Ding HY, Meng SK, Zhang XY, Lv HC, et al. Long-term outcomes of medical therapy versus successful recanalisation for coronary chronic total occlusions in patients with and without type 2 diabetes mellitus. Cardiovasc. Diabetol. (2020) 19:100. doi: 10.1186/s12933-020-01087-4
9. George S, Cockburn J, Clayton TC, Ludman P, Cotton J, Spratt J, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: analysis from the U.K. Central Cardiac Audit Database. J. Am. Coll. Cardiol. (2014) 64:235–43. doi: 10.1016/j.jacc.2014.04.040
10. Tomasello SD, Boukhris M, Giubilato S, Marza F, Garbo R, Contegiacomo G, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions. Eur. Heart J. (2015) 36:3189–98. doi: 10.1093/eurheartj/ehv450
11. Guo L, Zhang SF, Wu J, Zhong L, Ding HY, Xu JY, et al. Successful recanalisation of coronary chronic total occlusions is not associated with improved cardiovascular survival compared with initial medical therapy. Scand. Cardiovasc. J. (2019) 53:305–11. doi: 10.1080/14017431.2019.1645351
12. Sirnes PA, Myreng Y, Mølstad P, Bonarjee V, Golf S. Improvement in left ventricular ejection fraction and wall motion after successful recanalization of chronic coronary occlusions. Eur. Heart J. (1998) 19:273–81. doi: 10.1053/euhj.1997.0617
13. Guo L, Zhong L, Chen K, Wu J, Huang RC. Long-term clinical outcomes of optimal medical therapy vs. successful percutaneous coronary intervention for patients with coronary chronic total occlusions. Hell. J. Cardiol. (2018) 59:281–7. doi: 10.1016/j.hjc.2018.03.005
14. Kirschbaum SW, Rossi A, Boersma E, Springeling T, van de Ent M, Krestin GP, et al. Combining magnetic resonance viability variables better predicts improvement of myocardial function prior to percutaneous coronary intervention. Int. J. Cardiol. (2012) 159:192–7. doi: 10.1016/j.ijcard.2011.02.048
15. Tousoulis D. Chronic total occlusion: the puzzle is not yet solved. Hell. J. Cardiol. (2018) 59:251–3. doi: 10.1016/j.hjc.2018.10.010
16. Sianos G, Werner GS, Galassi AR, Papafaklis MI, Escaned J, Hildick-Smith D, et al. Recanalisation of chronic total coronary occlusions: 2012 consensus document from the EuroCTO club. EuroIntervention. (2012) 8:139–45. doi: 10.4244/EIJV8I1A21
17. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF III, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. (2009) 150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006
18. Harold JG, Bass TA, Bashore TM, Brindis RG, Brush JE Jr, Burke JA, et al. ACCF/AHA/SCAI 2013 update of the clinical competence statement on coronary artery interventional procedures: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training (writing committee to revise the 2007 clinical competence statement on cardiac interventional procedures). Circulation. (2013) 128:436–72. doi: 10.1161/CIR.0b013e318299cd8a
19. Hage FG, Venkataraman R, Zoghbi GJ, Perry GJ, DeMattos AM, Iskandrian AE. The scope of coronary heart disease in patients with chronic kidney disease. J. Am. Coll. Cardiol. (2009) 53:2129–40. doi: 10.1016/j.jacc.2009.02.047
20. Severino P, D'Amato A, Netti L, Pucci M, Infusino F, Maestrini V, et al. Myocardial ischemia and diabetes mellitus: role of oxidative stress in the connection between cardiac metabolism and coronary blood flow. J. Diabetes Res. (2019) 2019:9489826. doi: 10.1155/2019/9489826
21. Severino P, D'Amato A, Netti L, Pucci M, Mariani MV, Cimino S, et al. Susceptibility to ischaemic heart disease: focusing on genetic variants for ATP-sensitive potassium channel beyond traditional risk factors. Eur. J. Prev. Cardiol. (2020). doi: 10.1177/2047487320926780. [Epub ahead of print].
22. Severino P, D'Amato A, Pucci M, Infusino F, Birtolo LI, Mariani MV, et al. Ischemic heart disease and heart failure: role of coronary ion channels. Int. J. Mol. Sci. (2020) 21: 3167. doi: 10.3390/ijms21093167
23. Guo L, Lv H, Zhong L, Wu J, Ding H, Xu J, et al. Gender differences in long-term outcomes of medical therapy and successful percutaneous coronary intervention for coronary chronic total occlusions. J. Interv. Cardiol. (2019) 24:484–8. doi: 10.1155/2019/2017958
24. Guo L, Lv HC, Zhong L, Wu J, Ding HY, Xu JY, et al. Comparison of long-term outcomes of medical therapy and successful recanalisation for coronary chronic total occlusions in elderly patients: a report of 1,294 patients. Cardiovasc. Diagn. Ther. (2019) 9:586–95. doi: 10.21037/cdt.2019.11.01
25. Latif F, Kleiman NS, Cohen DJ, Pencina MJ, Yen CH, Cutlip DE, et al. In-hospital and 1-year outcomes among percutaneous coronary intervention patients with chronic kidney disease in the era of drug-eluting stents: a report from the EVENT (Evaluation of Drug Eluting Stents and Ischemic Events) registry. JACC Cardiovasc. Interv. (2009) 2:37–45. doi: 10.1016/j.jcin.2008.06.012
26. Moroni F, Spangaro A, Carlino M, Baber U, Brilakis ES, Azzalini L. Impact of renal function on the immediate and long-term outcomes of percutaneous recanalization of coronary chronic total occlusions: a systematic review and meta-analysis. Int. J. Cardiol. (2020) 317:200–6. doi: 10.1016/j.ijcard.2020.05.067
27. Guo L, Lv HC, Huang R. Percutaneous coronary intervention in elderly patients with coronary chronic total occlusions: current evidence and future perspectives. Clin. Interv. Aging. (2020) 15:771–81. doi: 10.2147/CIA.S252318
28. Wijeysundera HC, Norris C, Fefer P, Galbraith PD, Knudtson ML, Wolff R, et al. Relationship between initial treatment strategy and quality of life in patients with coronary chronic total occlusions. EuroIntervention. (2014) 9:1165–72. doi: 10.4244/EIJV9I10A197
29. Brilakis ES, Banerjee S, Karmpaliotis D, Lombardi WL, Tsai TT, Shunk KA, et al. Procedural outcomes of chronic total occlusion percutaneous coronary intervention: a report from the NCDR (National CardiovascularData Registry). JACC Cardiovasc. Interv. (2015) 8:245–53. doi: 10.1016/j.jcin.2014.08.014
30. Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions registry. J. Am. Coll. Cardiol. (2012) 59:991–7. doi: 10.1016/j.jacc.2011.12.007
31. Stahli BE, Gebhard C, Gick M, Ferenc M, Mashayekhi K, Buettner HJ, et al. Outcomes after percutaneous coronary intervention for chronic total occlusion according to baseline renal function. Clin. Res. Cardiol. (2018) 107:259–67. doi: 10.1007/s00392-017-1179-x
32. Best PJM, Lennon R, Ting HH, Bell MR, Rihal CS, Holmes DR, et al. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J. Am. Coll. Cardiol. (2002) 39:1113–9. doi: 10.1016/S0735-1097(02)01745-X
33. Kim CH, Yang JH, Park TK, Song YB, Hahn JY, Choi JH, et al. Revascularization vs. medical therapy for coronary chronic total occlusions in patients with chronic kidney disease. Circ. J. (2018) 82:2136–42. doi: 10.1253/circj.CJ-17-1272
Keywords: chronic total occlusions, medical therapy, outcomes, percutaneous coronary intervention, renal function
Citation: Guo L, Ding H, Lv H, Zhang X, Zhong L, Wu J, Xu J, Zhou X and Huang R (2020) Impact of Renal Function on Long-Term Clinical Outcomes in Patients With Coronary Chronic Total Occlusions: Results From an Observational Single-Center Cohort Study During the Last 12 Years. Front. Cardiovasc. Med. 7:550428. doi: 10.3389/fcvm.2020.550428
Received: 09 April 2020; Accepted: 14 October 2020;
Published: 16 November 2020.
Edited by:
Masanori Aikawa, Harvard Medical School, United StatesReviewed by:
Paolo Severino, Sapienza University of Rome, ItalyShunsuke Katsuki, Kyushu University Hospital, Japan
Copyright © 2020 Guo, Ding, Lv, Zhang, Zhong, Wu, Xu, Zhou and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Guo, leiguo@dmu.edu.cn
†These authors have contributed equally to this work and share first authorship
 Lei Guo
Lei Guo Huaiyu Ding1†
Huaiyu Ding1† Haichen Lv
Haichen Lv