- 1Department of Neurology, Tianjin Medical University General Hospital, Tianjin, China
- 2Laboratory of Epidemiology, Tianjin Neurological Institute, Tianjin, China
- 3Tianjin Neurological Institute, Key Laboratory of Post-Neuroinjury Neuro-Repair and Regeneration in Central Nervous System, Ministry of Education and Tianjin City, Tianjin, China
- 4Department of General Medicine, Tianjin Medical University General Hospital, Tianjin Neurological Institute, Tianjin, China
Worldwide, the stroke burden remains severe, especially for people in low socioeconomic groups. Atherosclerosis is a leading cause of stroke that is attracting increasingly greater attention. Blood pressure, including pulse pressure (PP) and systolic (SBP) and diastolic (DBP) blood pressures, is a traditional risk factor for atherosclerosis; its association with carotid intima-media thickness (CIMT) has also been widely studied. However, published studies have not reported on the relationship between PP and CIMT in low-income adults. Thus, this study investigated the relationship between PP and CIMT in a low-income population, in China. A total of 3,789 people, aged ≥45 years and without histories of stroke or cardiovascular disease, were recruited into this study. B-mode ultrasonography was performed to determine CIMTs. Demographic characteristics, physical examination data, previous medical histories, and laboratory test results were collected for each study participant. Multiple linear regression models were used to analyze the association between CIMT and PP. The mean CIMT was 567.1 μm (males, 583.5 μm; females, 555.7 μm). The SBP, DBP, PP, and mean arterial pressure (MAP) values were all positively correlated with CIMT, in the univariate analysis; PP and MAP showed the strongest correlations. In addition, in three multiple linear regression models, PP was shown to be significantly associated with CIMT; each 1-mm Hg increase in PP resulted in a CIMT increase of ≥0.41 μm (all P < 0.001). Our results demonstrated that, when compared with SBP, DBP, and MAP, PP may be the best predictor of CIMT. Thus, controlling blood pressure, especially PP levels, is vital to decreasing the prevalence of atherosclerosis, especially in this low socioeconomic status population in China.
Introduction
Stroke is the main cause of death and disability, worldwide (1), and is the leading cause of death in China (2). Each year, in China, the absolute costs of medical treatments for stroke surpass those reported for the United States in 2013; annually, China is estimated to spend $7.87 billion on stroke-related medical treatment, mostly for post-stroke care and rehabilitation (3). As the leading cause of stroke, atherosclerosis causes 10–20% of cerebral infarction events (4) and 20–30% of ischemic stroke events (5)Carotid intima-media thickness (CIMT) is a useful measure for detecting early atherosclerotic changes (6), and previous studies have demonstrated that an increased CIMT is a marker of atherosclerosis (7, 8). Thus, early detection of CIMT risk factors and their early modification may significantly impact the prevention of atherosclerotic disease.
Blood pressure is known to play a major role in the occurrence and progression of atherosclerosis. In the Young Finns cohort, adolescent systolic blood pressure (SBP) was shown to predict CIMT in adulthood (9). In women with coronary artery disease, followed for 3.2 years, high baseline pulse pressures (PPs) were associated with coronary atherosclerosis progression (10). In fact, studies have shown a direct association between PP and CIMT (11, 12). A previous study of adults with hypertension demonstrated that diastolic blood pressure (DBP) was lower in the group with increased CIMTs than it was in the group with normal CIMTs; PPs and the PP index [(SBP-DBP)/DBP] were significantly higher in the group with increased CIMTs (13).
Presently, China is a developing country and its low-income population accounts for a large proportion of the national population. Because of their lower incomes and poorer medical care, people in this socioeconomic class have greater risks of stroke and cardiovascular disease; however, they are unable to access timely medical assistance. To our knowledge, few other studies have examined this relationship, especially among low-income populations with low levels of educational attainment and living in rural areas of China. This study, therefore, investigated the association between PP and CIMT in such a population.
Methods
Participants and Study Design
This cross-sectional survey included 18 villages in rural areas of Tianjin, China, and involved participants from the previously described Tianjin Brain Study (14–16), conducted between April 2014 and January 2015. In short, about 95% of the total area population (14,251 people) were low-income farmers, with 2014 per capita disposable incomes of <1,600 USD (17). In 2011, the average length of formal education for the population was 5.26 years. From this population, 3,789 residents (≥45 years old) were recruited into this study. Individuals with previous histories of or current symptomatic cardiovascular (including myocardial infarctions, angina, and asymptomatic myocardial ischemia) or cerebrovascular (including ischemic and hemorrhagic strokes) diseases were excluded.
The surveys were approved by the ethics committee of Tianjin Medical University General Hospital. The study was conducted according to approved guidelines and written informed consent was obtained from each participant.
Risk Factors and Physical Examinations
This study involved face-to-face interviews conducted by trained researchers. The name, sex, date of birth, education level, individual and family medical histories [including the presence or occurrence of hypertension, stroke, diabetes mellitus (DM), transient ischemic attacks, and coronary heart disease], and lifestyle factors (including cigarette smoking, defined as smoking ≥1 cigarette/day for ≥1 year; passive smoking, defined as ≥1 person smoking in the room; and alcohol consumption, defined as drinking ≥500 g of alcohol/week for ≥1 year).
Each participant underwent a physical examination to measure blood pressure, height, and weight; the body mass index (BMI) was calculated by dividing the weight (kg) by the square of height (m). Fasting blood glucose (FBG), triglyceride (TG), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) levels were measured. Carotid ultrasound examinations were also conducted.
Ultrasonography Measurements
All ultrasound examinations and measurements were performed by one trained technician who was blinded to participant details. Each patient was placed in a supine position, and was examined using B-mode ultrasonography (Terason 3000; Burlington, Massachusetts, MA, US) with a 5–12-MHz linear array transducer. Two extracranial carotid trees (i.e., the common carotid artery, bifurcation, internal carotid artery, and the internal and external carotid arteries) were measured to obtain the CIMT; the vessels were also screened for the presence of plaque. CIMTs of the proximal and distal walls of the common carotid artery were measured on the left and right sides, and the maximum, minimum, and average CIMT values were obtained. Carotid plaques were defined as local structural invasions into the arterial lumen of at least 0.5 mm or 50% of the surrounding CIMT value, or when the distance between the intima-lumen interface and the media adventitia interface was >1.5 mm (18); the longitudinal and transverse dynamic images of each plaque were digitally stored, according to the standard protocol (19). Regardless of the measured carotid plaque values, participants with carotid plaques were included in the carotid plaque group if >1 lesion was found. The ranges of inter- and intra-observer correlation coefficients for the CIMT measurements were 0.88–0.94 and 0.80–0.95, respectively.
Survey Procedure
Local village doctors visited all eligible residents, in accordance with pre-determined procedures, 1 day before the physical examination. Between April 15, 2014 and June 30, 2014, the physical examinations (including blood pressure, weight, height, carotid ultrasound, and 12-lead echocardiography) and blood sample collections were performed in the local clinics. All blood samples were sent to the Central Laboratory of Tianjin Medical University General Hospital for determination of TC, TG, HDL-C, and LDL-C levels within 12 h of collection; FBG levels were determined at the Central Laboratory of Tianjin Ji County People's Hospital within 2 h of sample collection. Between July 1, 2014 and January 8, 2015, carotid plaque and CIMT measurements were determined by one practiced technician.
Definitions of Risk Factors
Mean arterial pressure (MAP) was calculated as (SBP + 2 × DBP)/3 and PP was calculated as SBP – DBP. Hypertension was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg (20). DM was defined as a FBG concentration ≥7.0 mmol/L. Obesity was defined as a BMI ≥ 30.0 kg/m2 and overweight was defined as a BMI of 25.0–29.9 kg/m2.
Statistical Analyses
Continuous variables are reported as means and standard deviations; Student's t-test was used to analyze between-group differences in TC, TG, HDL-C, and LDL-C levels. Categorical variables are expressed as frequencies and 95% confidence intervals (CIs) and between-group comparisons were made using chi-square tests. The participants were divided into four age groups (45–54, 55–64, 65–74, and ≥75 years old) and into three educational groups, based on the length of formal education (0, 1–6, and ≥7 years). Logistic regression analyses were used to evaluate the CIMT risk factors in both males and females.
The univariate analysis results are shown as unadjusted B-values and 95% CIs; the multivariate analysis results are shown as adjusted B-values and 95% CIs, after adjusting for covariates. The age (45–54 years old) and educational (≥7 years) groups were analyzed as categorical variables; hypertension, DM, obesity, current smoking, passive smoking, drinking, high TC, high TG, low HDL-C, and high LDL-C levels were analyzed as dichotomous variables. P-values of statistically significant were considered to be <0.05 for the dichotomous variables, P < 0.0166 for three groups of categorical variables, and P < 0.0125 for four groups of categorical variables.
A linear regression model was used to examine the association of PP and MAP with CIMT. Three models were developed. Model 1 involved adjusting for age (continuous variable), sex (male or female), and education (continuous variable). Model 2 included the Model 1 variables plus hypertension (categorical variable), DM (categorical variable), smoking (categorical variable), and drinking (categorical variable); Model 3 included the Model 2 variables plus FBG, TG, HDL-C, LDL-C, and the HDL-C/LDL-C ratio (all continuous variables). SPSS for Windows (version 19.0; SPSS, Chicago, IL, USA) was used for the analyses.
Results
Participant Characteristics
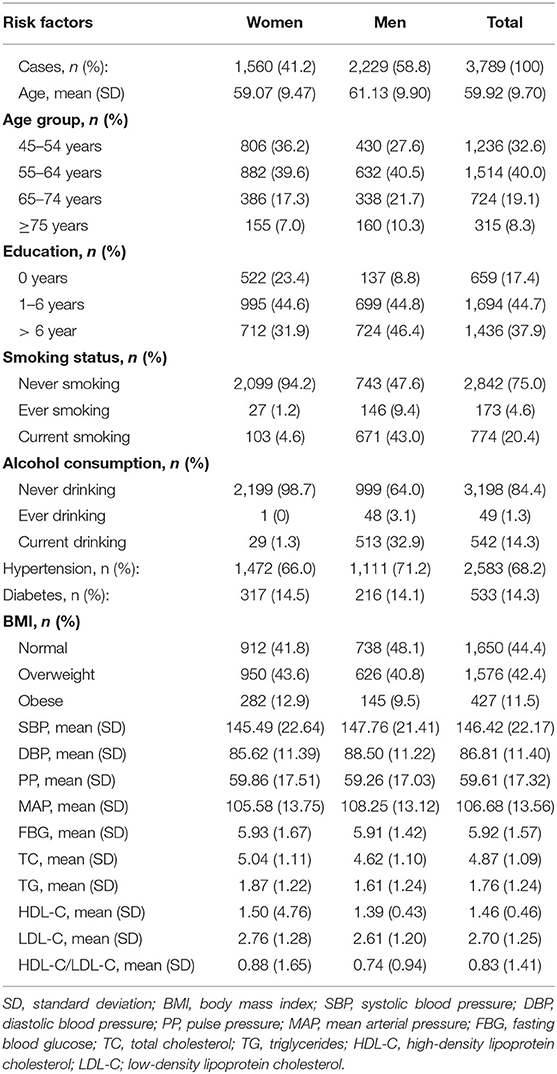
This study recruited 3,789 individuals, aged ≥45 years (mean age, 59.92 years), including 1,560 (41.2%) men and 2,229 (58.8%) women. For these participants, the average length of formal education was 5.48 years, and 17.4% of the participants had never received any formal education (8.8% of men and 23.4% of women); however, 37.9% of the participants had received formal educations lasting ≥6 years. The average SBP and DBP levels were high in this population, with mean values of 146.42 mmHg and 86.81 mmHg, respectively. The mean PP and MAP values were 59.61 mmHg and 106.68 mmHg, respectively (Table 1).
Mean CIMT Differences Grouped by Demographic Characteristics and Risk Factors
Table 2 shows the mean CIMT values for the participants, grouped by demographic characteristics and risk factors. The mean CIMT increased from 536.3 μm (45–54-year-old group) to 609.0 μm (≥75-year-old group). However, the mean CIMT decreased as the group education level increased. The mean CIMT was significantly higher in current smokers than in never smokers, and it was also higher among alcohol consumers than among those who did not consume alcohol (P < 0.001). Compared with the non-hypertensive population, patients with hypertension had a significantly higher mean CIMT (P < 0.001). Similarly, the mean CIMT for patients with DM was higher than that for patients without DM (P < 0.001).
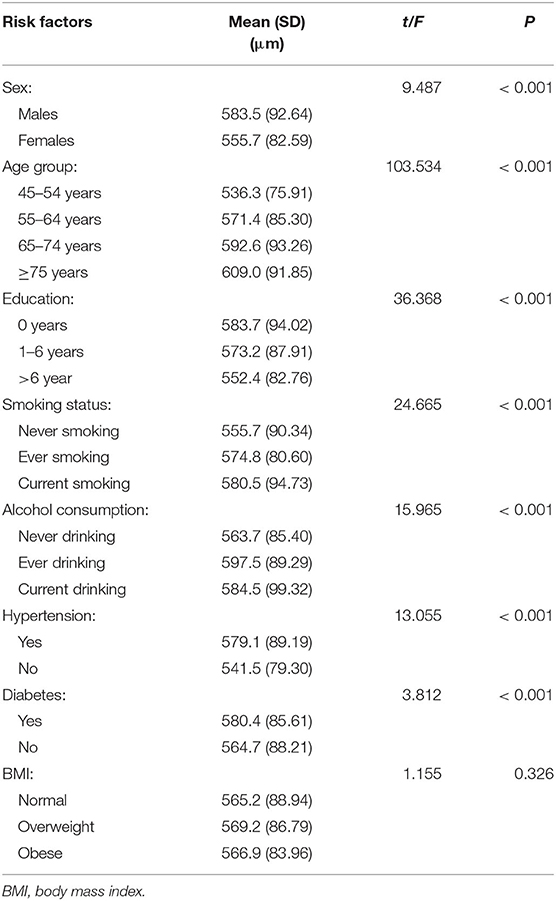
Table 2. Differences in mean carotid intima-media thicknesses, according to demographic characteristics and risk factors groups.
Associations Between the Mean CIMT and Measured Parameters in the Linear Regression Analysis
A linear regression analysis showed that age, PP, MAP, SBP, DBP, FBG, TC, and LDL-C were positively correlated with CIMTs, but education, TG, and HDL-C levels, and the HDL-C/LDL-C ratio were negatively correlated with CIMTs (all, P < 0.05). Each 1-mmHg increase in PP or MAP was associated with mean CIMT increases of 1.16 μm (95% CI, 1.00–1.32; P < 0.001) and 1.02 μm (95% CI, 0.82–1.23; P < 0.001), respectively. Moreover, SBP, DBP, FBG, TC, and LDL-C were positively associated with CIMT in the univariate analysis (β = 0.85, 0.56, 4.65, 3.40, and 6.57, respectively; all P < 0.05; Table 3).
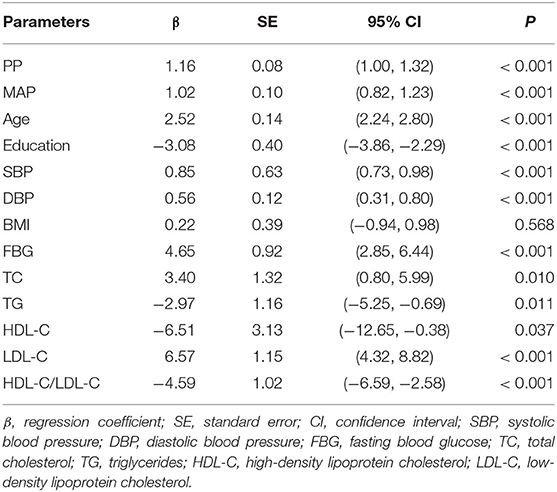
Table 3. Association of mean carotid intima-media thickness with measured parameters in the linear regression analysis.
Associations Between the Mean CIMT and the PP and MAP in the Multivariate Analysis
The associations between the mean CIMT and the PP and MAP, in the multivariate analysis, are shown in Table 4. The association between CIMT and PP remained statistically significant in Model 1. Moreover, PP was an independent risk factor for increased CIMT in Models 2 and 3; each 1-mmHg increase in PP was associated with CIMT increases of 0.42 μm (95% CI, 0.20–0.63; P < 0.001) and 0.41 μm (95% CI, 0.18–0.63; P < 0.001), respectively. However, there was no significant association between MAP and CIMT in Models 2 and 3 (both, P > 0.05).
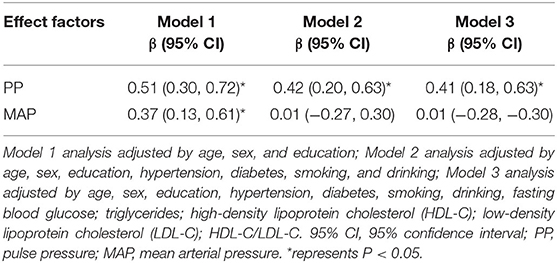
Table 4. Association of mean carotid intima-media thickness (μm) with pulse pressure, according to demographic characteristics and risk factor groups in the multivariate analysis.
Discussion
To our knowledge, this was the first population-based study to explore the relationship between PP and CIMT in a low socioeconomic status study population. All of the included participants were low-income residents of the target area, were ≥45 years old, and had low educational attainment. The results of the multivariate analysis showed that PP was an independent risk factor for increased CIMT. Each 1-mmHg increase in PP was associated with a CIMT increase of at least 0.41 μm. However, there was no association between MAP and CIMT, after adjusting for covariates.
Although the relationship between blood pressure and CIMT has been demonstrated in many studies, few studies have explored the relationship between PP and CIMT, especially in a low socioeconomic status population. PP, a significant independent risk factor for cardiovascular mortality (21), has been shown in some experimental and clinical studies to modulate CIMT (13, 22, 23). After a 4-year follow-up, the Etude du Vieillissement Artériel study demonstrated that elevated PP levels were associated with CIMT progression, and increased CIMT was associated with PP widening (12). The Muscatine Offspring Study reported that, in adolescents, the CIMT increased by 0.232 mm for each 1-mmHg increase in PP (22). A Belgian study reported that each 1-mmHg increase in the 24-h PP resulted in a 139-μm CIMT increase (18). A study from France showed that, after adjusting for confounding variables, an increased CIMT was the only factor significantly and independently associated with high PP, irrespective of the effectiveness of blood pressure control and antihypertensive drug treatments (19). Our previous study showed a positive association between SBP and CIMT and a negative association between DBP and CIMT (16). However, the current study showed different results in the univariate analysis. In view of the collinearity between PP and SBP or DBP, the present study assessed the relationship between CIMT and PP by adjusting for other covariables, including hypertension, using a multivariate analysis. As a result, the current study showed that PP was an independent risk factor for CIMT in this low-income population in China. A continuously elevated blood pressure is well-known to impose a great mechanical burden on the vascular endothelium; subsequently, vascular structures and function gradually become impaired, ultimately resulting in vascular fibrosis, stiffness, and decreased intrinsic compliance (24). In turn, vascular stiffness and decreased compliance are often associated with the early stages of atherosclerosis, when CIMT first increases (25, 26). Pressure pulsation may directly affect atherosclerosis through a variety of mechanisms (27). For example, high pulsation can induce endothelial dysfunction (28), while cyclical strain can enhance monocyte adhesion to endothelial cells and regulate gene expression in smooth muscle cells and monocytes/macrophages (29–31).
As shown in previous studies, the trend toward higher CIMTs in individuals with only primary educations, or less, was more significant than in individuals with secondary or high school educations (32). More than 40% of China's population live in rural areas (17); these people tend to have poor health insurance, low educational attainment, and low incomes (33). Although the prevalence of hypertension in rural adults is similar to that for adults living in urban areas, the detection and medical treatment of hypertension in rural-living adults remains unsatisfactory (34). The unusually large urban-rural gap in hypertension treatment and the expanding trend toward hypertension detection require health policymakers and researchers to pay more attention to rural populations.
There are several limitations in this study. First, with respect to the study design, an inherent limitation of a cross-sectional study is that it cannot determine causal links between significant variables and CIMT; thus, additional longitudinal studies are needed to determine causality. Secondly, the reliance on low-income, poorly educated rural residents in China may limit the study's generalizability. However, this study population may represent other low socioeconomic status populations. Additionally, we did not analyze information regarding medication use among the participants; however, the frequency of medication use is low in this low socioeconomic status population. Thus, the absence of this information may not have had a significant impact on the validity of the present results. Finally, the study did not include a high-income comparator group. Further studies are needed to explore the differences between low- and high-income populations.
Conclusions
This study focused on the relationship between PP and CIMT in low socioeconomic status adults in China. When compared with SBP, DBP, and MAP, PP appears to be the best predictor of CIMT. CIMTs were associated with increasing PP levels, and each 1-mmHg increase in PP resulted in a CIMT increase of at least 0.41 μm, in this low socioeconomic population. These findings suggest the need to both control blood pressure levels and monitor PP levels to decrease the prevalence of atherosclerosis and reduce the burden of cardiovascular disease and stroke, especially among this low-socioeconomic status population, in China.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee of Tianjin Medical University General Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JW, YS, and XN were involved in conception and design and data interpretation for this article. JW was involved in data analysis for this article. JL, QL, and DG was involved in manuscript drafting. JL, QL, DG, YY, XZ, and JT were involved in data collection, case diagnosis and confirmation for this article. JW, YS, and XN were involved critical review for this article. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank all participants of the Tianjin Brain Study, and local medical care professionals for their valuable contributions.
References
1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
2. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
3. Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. (2017) 135:759–71. doi: 10.1161/CIRCULATIONAHA.116.025250
4. Fairhead JF, Rothwell PM. The need for urgency in identification and treatment of symptomatic carotid stenosis is already established. Cerebrovasc Dis. (2005) 19:355–8. doi: 10.1159/000085201
5. Dogan A, Dempsey RJ. Diagnostic modalities for carotid artery disease. Neurosurg Clin N Am. (2000) 11:205–20. doi: 10.1016/S1042-3680(18)30127-X
6. Iglesias del Sol A, Bots ML, Grobbee DE, Hofman A, Witteman JC. Carotid intima-media thickness at different sites: relation to incident myocardial infarction; The Rotterdam Study. Eur Heart J. (2002) 23: 934–40. doi: 10.1053/euhj.2001.2965
7. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. (2007) 115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875
8. Johnson HM, Stein JH. Measurement of carotid intima-media thickness and carotid plaque detection for cardiovascular risk assessment. J Nucl Cardiol. (2011) 18:153–62. doi: 10.1007/s12350-010-9319-y
9. Juonala M, Viikari JS, Kähönen M, Taittonen L, Laitinen T, Hutri-Kähönen N, et al. Life-time risk factors and progression of carotid atherosclerosis in young adults: the cardiovascular risk in young finns study. Eur Heart J. (2010) 31:1745–51. doi: 10.1093/eurheartj/ehq141
10. Nair GV, Waters D, Rogers W, Kowalchuk GJ, Stuckey TD, Herrington DM. Pulse pressure and coronary atherosclerosis progression in postmenopausal women. Hypertension. (2005) 45:53–7. doi: 10.1161/01.HYP.0000149599.99266.44
11. Riley WA, Evans GW, Sharrett AR, Burke GL, Barnes RW. Variation of common carotid artery elasticity with intimal-medial thickness: the ARIC Study. Atherosclerosis Risk in Communities. Ultrasound Med Biol. (1997) 23:157–64. doi: 10.1016/S0301-5629(96)00211-6
12. Zureik M, Touboul PJ, Bonithon-Kopp C, Courbon D, Berr C, Leroux C, et al. Cross-sectional and 4-year longitudinal associations between brachial pulse pressure and common carotid intima-media thickness in a general population. The EVA study. Stroke. (1999) 30:550–5. doi: 10.1161/01.STR.30.3.550
13. Cai A, Mo Y, Zhang Y, Li J, Chen J, Zhou Y, et al. Relationship of pulse pressure index and carotid intima-media thickness in hypertensive adults. Clin Exp Hypertens. (2015) 37:267–70. doi: 10.3109/10641963.2014.954713
14. Zhan C, Shi M, Yang Y, Pang H, Fei S, Bai L, et al. Prevalence and Risk Factors of carotid plaque among middle-aged and elderly adults in rural Tianjin, China. Sci Rep. (2016) 6:23870. doi: 10.1038/srep23870
15. Ren L, Shi M, Wu Y, Ni J, Bai L, Lu H, et al. Correlation between hypertension and common carotid artery intima-media thickness in rural China: a population-based study. J Hum Hypertens. (2018) 32:548–54. doi: 10.1038/s41371-018-0074-x
16. Liu B, Ni J, Shi M, Bai L, Zhan C, Lu H, et al. Carotid intima-media thickness and its association with conventional risk factors in low-income adults: a population-based cross-sectional study in China. Sci Rep. (2017) 7:41500. doi: 10.1038/srep41500
17. China National Bureau of Statistics (2019). Available online at: http://www.stats.gov.cn/tjsj/ndsj/
18. Dechering DG, Wizner B, Adiyaman A, Nawrot T, Jin Y, Richart T, et al. Sphygmomanometric and ambulatory blood pressures as forerunners of carotid and femoral intima-media thickness. J Hypertens. (2009) 27:813–21. doi: 10.1097/HJH.0b013e328324ed6c
19. Tartière JM, Kesri L, Safar H, Girerd X, Bots M, Safar ME, et al. Association between pulse pressure, carotid intima-media thickness and carotid and/or iliofemoral plaque in hypertensive patients. J Hum Hypertens. (2004) 18:325–31. doi: 10.1038/sj.jhh.1001673
20. Unger T, Borghi C, Charchar FJ, Khan NA, Poulter NR, Dorairaj P, et al. International society of hypertension global hypertension practice guidelines. Hypertension. (2020) 75:1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026
21. Niiranen TJ, Kalesan B, Mitchell GF, Vasan RS. Relative contributions of pulse pressure and arterial stiffness to cardiovascular disease. Hypertension. (2019) 73:712–7. doi: 10.1161/HYPERTENSIONAHA.118.12289
22. Dawson JD, Sonka M, Blecha MB, Lin W, Davis PH. Risk factors associated with aortic and carotid intima-media thickness in adolescents and young adults: the Muscatine Offspring Study. J Am Coll Cardiol. (2009) 53:2273–9. doi: 10.1016/j.jacc.2009.03.026
23. Zanchetti A, Hansson L, Dahlöf B, Elmfeldt D, Kjeldsen S, Kolloch R, et al. Effects of individual risk factors on the incidence of cardiovascular events in the treated hypertensive patients of the Hypertension Optimal Treatment Study. HOT Study Group. J Hypertens. (2001) 19:1149–59. doi: 10.1097/00004872-200106000-00021
24. Sarafidis PA, Bakris GL. Early patterns of blood pressure change and future coronary atherosclerosis. JAMA. (2014) 311:471–2. doi: 10.1001/jama.2013.285123
25. Bianchini E, Giannarelli C, Bruno RM, Armenia S, Landini L, Faita F, et al. Functional and structural alterations of large arteries: methodological issues. Curr Pharm Des. (2013) 19:2390–400. doi: 10.2174/1381612811319130007
26. Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. (2013) 34:2159–219. doi: 10.1093/eurheartj/eht151
27. Yamamoto K, Ikeda U, Shimada K. Role of mechanical stress in monocytes/macrophages: implications for atherosclerosis. Curr Vasc Pharmacol. (2003) 1:315–9. doi: 10.2174/1570161033476565
28. Ryan SM, Waack BJ, Weno BL, Heistad DD. Increases in pulse pressure impair acetylcholine-induced vascular relaxation. Am J Physiol. (1995) 268(1 Pt 2):H359–63. doi: 10.1152/ajpheart.1995.268.1.H359
29. Cheng JJ, Wung BS, Chao YJ, Wang DL. Cyclic strain enhances adhesion of monocytes to endothelial cells by increasing intercellular adhesion molecule-1 expression. Hypertension. (1996) 28:386–91. doi: 10.1161/01.HYP.28.3.386
30. Ohki R, Yamamoto K, Mano H, Lee RT, Ikeda U, Shimada K. Identification of mechanically induced genes in human monocytic cells by DNA microarrays. J Hypertens. (2002) 20:685–91. doi: 10.1097/00004872-200204000-00026
31. Sakamoto H, Aikawa M, Hill CC, Weiss D, Taylor WR, Libby P, et al. Biomechanical strain induces class a scavenger receptor expression in human monocyte/macrophages and THP-1 cells: a potential mechanism of increased atherosclerosis in hypertension. Circulation. (2001) 104:109–14. doi: 10.1161/hc2701.091070
32. Wang A, Chen G, Su Z, Liu X, Yuan X, Jiang R, et al. Carotid intima-media thickness and cognitive function in a middle-aged and older adult community: a cross-sectional study. J Neurol. (2016) 263:2097–104. doi: 10.1007/s00415-016-8234-9
Keywords: pulse pressure, carotid intima-media thickness, risk factors, epidemiology, atherosclerosis
Citation: Liu J, Lin Q, Guo D, Yang Y, Zhang X, Tu J, Ning X, Song Y and Wang J (2020) Association Between Pulse Pressure and Carotid Intima-Media Thickness Among Low-Income Adults Aged 45 Years and Older: A Population-Based Cross-Sectional Study in Rural China. Front. Cardiovasc. Med. 7:547365. doi: 10.3389/fcvm.2020.547365
Received: 20 August 2020; Accepted: 21 October 2020;
Published: 12 November 2020.
Edited by:
Isabella Sudano, University Hospital Zürich, SwitzerlandReviewed by:
Michele Ciccarelli, University of Salerno, ItalyJane A. Leopold, Massachusetts General Hospital and Harvard Medical School, United States
Copyright © 2020 Liu, Lin, Guo, Yang, Zhang, Tu, Ning, Song and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianjia Ning, eGpuMDkwNkBnbWFpbC5jb20=; Yijun Song, c29uZ3lpanVuMjAwMEAxMjYuY29t; Jinghua Wang, amh3ODc5OUB5YWhvby5jb20=
†These authors have contributed equally to this work
 Jie Liu
Jie Liu Qiuxing Lin1,2,3†
Qiuxing Lin1,2,3† Dandan Guo
Dandan Guo Xianjia Ning
Xianjia Ning Jinghua Wang
Jinghua Wang