- 1Division of Healthcare Engineering, Department of Radiation Oncology, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 2Department of Population Health Sciences, Duke University, Durham, NC, United States
- 3University of Utah, Huntsman Cancer Institute, Salt Lake City, UT, United States
- 4Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC, United States
Introduction: The purpose of this study was to assess whether varying input communication factors impacted participants’ perceived confidence, motivation, and likelihood to act (i.e., share or discuss their preferences and values with their clinician or family/caregiver) when receiving tailored communication from a values-clarification tool.
Methods: This study was conducted over a two-month period at the North Carolina Basnight Cancer Hospital. Patients with hematologic malignancies participated in evaluating three distinct messages that varied on three input communication factors.
Results: Results from this study indicate that most study participants preferred messages that were moderately direct, contained succinct question prompts, and that were empowering. Results also indicate that diverse perspectives and external influences may impact confidence and motivation toward discussing preferences with their clinicians.
Discussion: Our findings suggest the importance of validating the input communication factors within values-clarification tools before presenting results to patients and the need to evaluate potential disparities in patients’ participation toward discussing their preferences. Evidence from this study provides direction for future research efforts focused on improving shared decision-making among older adults.
1 Introduction
The National Academy of Medicine has a longstanding framework that includes six core principles, one of which focuses on patient-centered care, asserting that patients’ preferences, needs, and values should guide clinical decisions (Institute of Medicine, 2001). This principle is often aligned with shared decision-making (SDM), that is, patients and clinicians working together to decide on a treatment in the patients’ best interest (Institute of Medicine, 2001; Agency for Healthcare Research and Quality, 2023). Unfortunately, the SDM process among older adults with cancer is often poorly executed (LeBlanc et al., 2017; Rood et al., 2017; Bories et al., 2018; Loh et al., 2021; Sorror et al., 2021). For patients diagnosed with cancer, SDM has become increasingly complicated. In recent years, the number of cancer treatment options has increased substantially, fundamentally changing treatment paradigms in many contexts (Sochacka-Ćwikła et al., 2021). However, desired care pathways are heterogenous among older patients (≥ 60 years) diagnosed with cancer (Richardson et al., 2020; Sorror et al., 2021). These patients often feel a lack of involvement in the decisions made about which pathway is best for them (Rood et al., 2017; Mohile et al., 2018).
Supporting patients in sharing their preferences and values may improve their involvement in SDM. Effective methods to elicit and quantify patient preferences and values have been developed using best-worst scaling (BWS), a simple yet robust survey method which can help guide treatment decisions and inform SDM between patients and clinicians (Hunter et al., 2015; Smith et al., 2016; Rocque et al., 2019; Sekeres et al., 2020; Cures Act Congress, 2021; Wicker, 2021). Our study team conducted previous research to convert a BWS paper assessment to a digital health tool, referred to as “PRIME” (Preference Reporting to Improve Management and Experience) (Cole et al., 2022). Developing assessments using digital health platforms is an efficient method for eliciting preferences, quantitatively analyzing responses, and delivering tailored messages to patients in real-time. Results from our early study indicate patients found PRIME to be acceptable and user-friendly (Cole et al., 2022), and that they prefer information to be individualized to their particular situation (Kwong et al., 2022). Presenting patients with individualized or tailored messages based on their personalized results may impact affective-cognitive or behavioral outcomes and support patients in communicating their preferences and values with their clinicians (Kreuter et al., 1999; Kreuter and Wray, 2003; Hawkins et al., 2008; Lafata et al., 2017). No study has analyzed the use of tailored messaging regarding patient preferences to inform SDM among older adults with blood cancers.
The primary objective of this study was to assess whether varying input communication factors (Rice and Atkin, 2013) of tailored messages within PRIME are associated with participants’ perceived affective-cognitive (confidence and motivation) and behavior outcomes (likelihood to act). A secondary objective was to evaluate participants’ perception of message effectiveness, relevance, and purpose. We anticipate preliminary evidence from this study will lead to a better understanding of the input communication factors that should be used when developing tailored messages for this population.
2 Materials and methods
The primary outcome of this study is patients’ perception of their confidence, motivation and likelihood to act (i.e., share or discuss their preferences and values with their clinician or family/caregiver) when varying input communication factors of tailored messages within a digital health tool based on BWS results. The secondary outcomes of this study are participants’ (i) perceived message effectiveness, (ii) perceived message relevance, (iii) perceived message purpose, and (iv) preferred communication channels for completing BWS assessments and viewing messages based on BWS results.
2.1 Participants
Eligible patients included those ≥60 years of age with a confirmed diagnosis of a hematologic malignancy including leukemia, lymphoma, or myeloma. We chose this population as treatment decisions for older adults with blood cancers are increasingly becoming preference sensitive (Richardson, 2022). Patients were sequentially approached to be recruited for this study. Patients engaged in one-hour semi-structured interviews facilitated by a study team member with expertise in human factors.
2.2 Study design
Eligible patients were approached by study team members either during their in-patient stay at the North Carolina Basnight Cancer Hospital or via phone. Participating patients gave written consent and agreed to meet with the study team member in either the patient’s hospital room, a hospital meeting room, or via Zoom.
An exploratory mixed-methods design was used to evaluate participants’ perception of tailored messages through qualitative feedback (semi-structured interviews) and quantitative feedback (questionnaires). We used Lafata et al. (2017) patient-clinician communication model to inform our interview guide, which included both validated and open-ended questions. The patient-clinician communication model focuses on patient characteristics and the patient-clinician communication exchange (e.g., adaptations, channels), as well as affective, cognitive, and behavioral outcomes (Lafata et al., 2017).
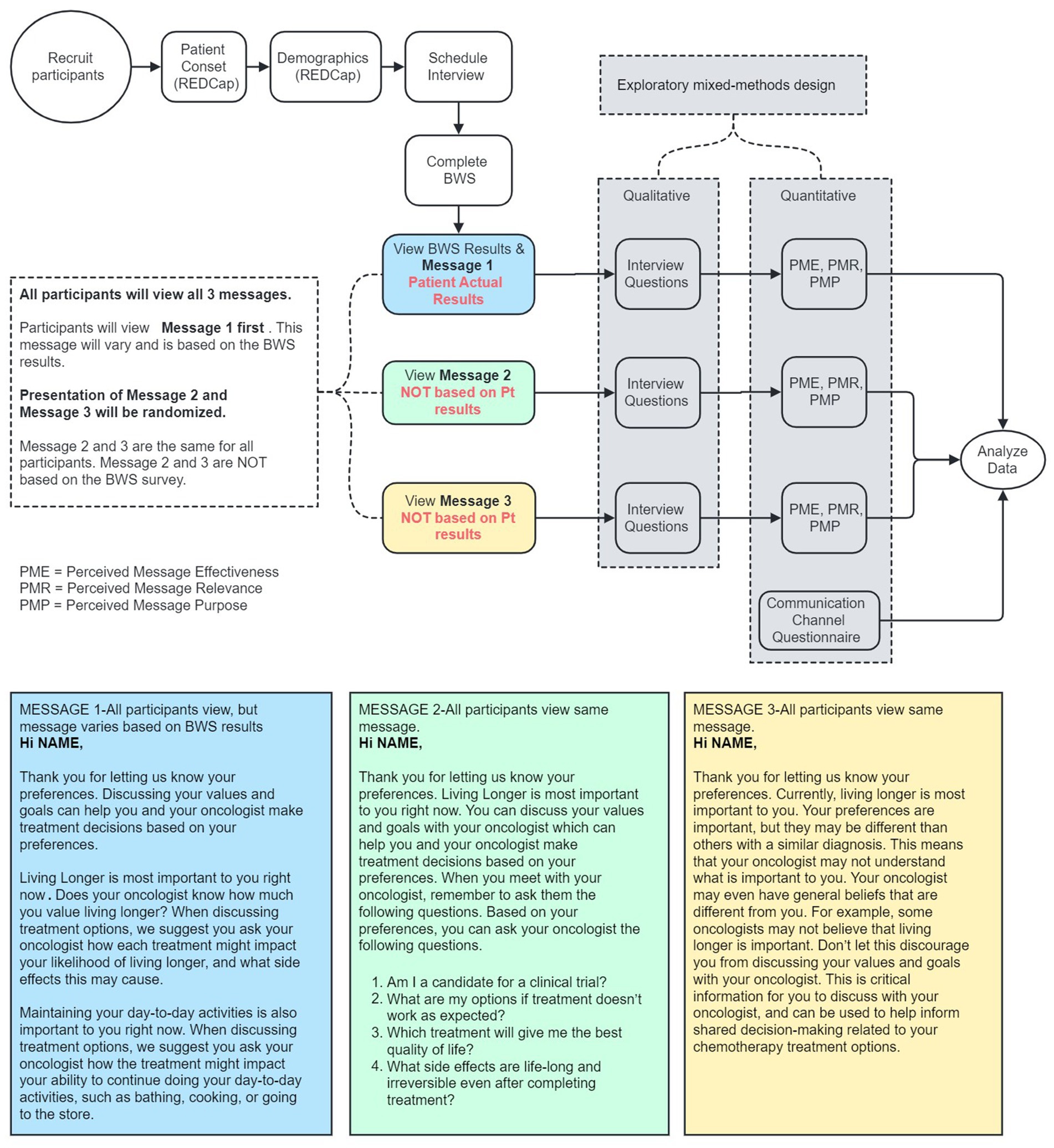
Participants initially completed a brief demographics questionnaire and then completed the BWS assessment. After completing the BWS assessment participants viewed three distinct messages (See Figure 1). After viewing each message, participants provided feedback on affective-cognitive outcomes by evaluating perceived confidence and motivation. Participants also provided feedback on behavioral outcomes by evaluating their perceived likelihood to act (i.e., share or discuss their preferences and values with their clinician or family/caregiver) based on the message they just reviewed. Participants were assessed on the communication exchange (adaptations) by evaluating the effectiveness, relevance, and purpose of each message. Lastly, participants provided feedback on channels of communication exchange by answering questions about how they prefer to complete the BWS assessment and view messages based on BWS results.
2.3 Message development
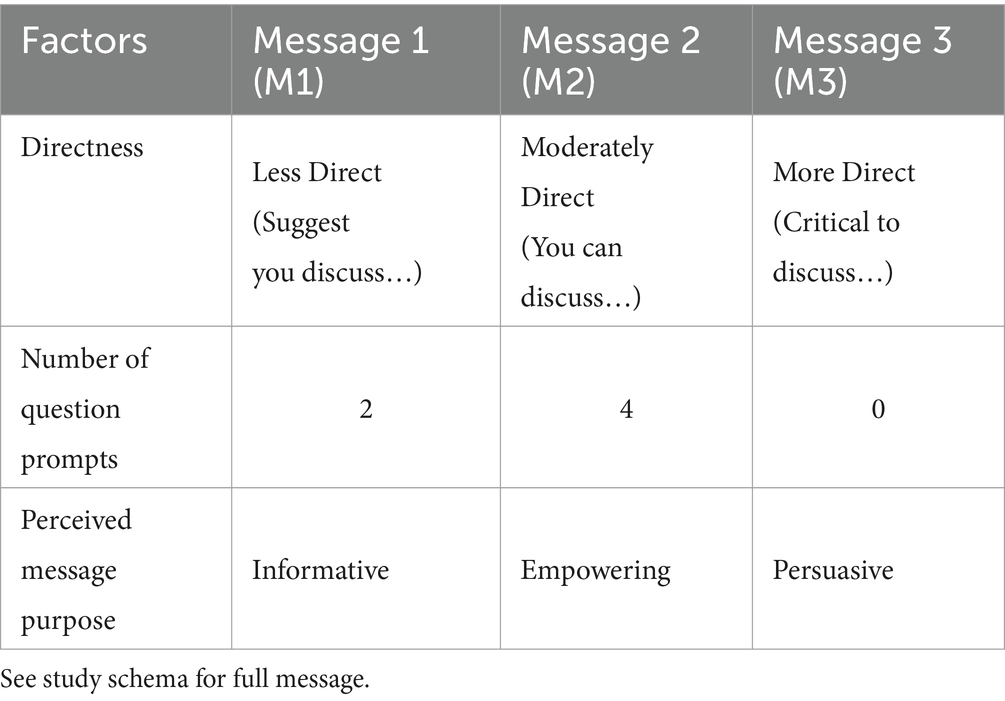
We developed three distinct messages (referred to as M1, M2, and M3) that vary on three input communication factors: (i) directness of the message, (ii) number of question prompts, and (iii) perceived message purpose (see Table 1). Each message was developed with a particular purpose; M1: Informative, M2: Empowering, M3: Persuasive. We made our message design choices based on past research and theorizing on tailoring and persuasion (Rimer and Kreuter, 2006; Rice and Atkin, 2013). The BWS assessment was administered through the Qualtrics platform to present real-time tailored results for M1 (using JavaScript), and a randomization algorithm to present the corresponding M2 and M3 (see Table 1). All participants evaluated all three messages in a sequential, but randomized order. M1, which displayed tailored results based on participants’ responses from the BWS assessment, was always presented first. Then, M2 and M3, which were not based on participants’ BWS results, were presented in random order next. (See Figure 1 for study schema, and Supplementary Table SA for all message responses.)
2.4 Primary measures
2.4.1 Affective-cognitive (confidence and motivation) and behavior (likelihood to act) outcomes
Participants provided subjective feedback according to the interview guide to assess perceived impacts on both affective-cognitive outcomes (confidence and motivation to discuss preferences and values with clinicians) and behavioral outcomes (likelihood of discussing preference and values with clinicians or family/caregivers) (Lafata et al., 2017). After reading each message, participants were asked how they felt about discussing their preferences with their clinician. Follow up questions included how the message impacted their confidence and motivation in talking with their clinicians about their preferences. Participants were also asked how the message impacted their likelihood to discuss their preferences with their clinician and with family members or caregivers. All interview questions were open-ended, however, the framing of “likelihood to discuss either with clinicians or family/caregivers” provided participants with the option to respond based on the scale from very likely to very unlikely. (See Supplementary Table SB for the full interview guide.)
2.5 Secondary measures
2.5.1 Perceived message effectiveness
Evaluation of perceived message effectiveness (PME) was quantified objectively using a modified PME scale (Baig et al., 2019). The original PME scale was validated to evaluate the effectiveness of health messages among diverse populations to prevent smoking (Baig et al., 2019). The brief three-item assessment was developed so the wording of each question could be adapted to other health behaviors (Baig et al., 2019), therefore is an appropriate measure for assessing the message effectiveness for encouraging older adults to discuss their values with their clinician. The PME has been used to evaluate message effectiveness in avoiding a behavior, using three main variables within the three-item assessment (‘worry’, ‘bad idea’, and ‘discourage’) (Noar et al., 2023). For this study, the three-item assessment will evaluate engaging rather than avoiding a behavior, therefore the variables have been reversed to (i) How much does this message make you believe that sharing your preferences with your oncologist will ‘benefit’ you?, (ii) How much does this message make you think that sharing your preferences is a ‘good idea’?, and (iii) How much does this message ‘encourage’ you to discuss your preferences with your oncologist? The PME scale ranges from (1) not at all, to (5) a great deal.
2.5.2 Perceived message relevance
Evaluation of perceived message relevance (PMR) was quantified objectively with a previously used non-validated 4-item Likert-type PMR scale (Jensen et al., 2012). Two items are presented in the positive, including (i) The message seemed to be written personally for me, and (ii) The message was relevant to my situation. To avoid response bias, two items were presented to be framed negatively regarding relevance, including (i) The message was primarily general information that wasn’t applicable to me, and (ii) The message was not customized at all (see PMR Results for excluding the reverse code questions from data analysis). The PMR scale ranges from (1) strongly disagree to (5) strongly agree. The PMR is an appropriate measure for assessing the relevance of tailored messages for older adults to discuss their values with their clinicians.
2.5.3 Perceived message purpose
McGuire’s “Classic Input–Output Framework” was used to define the communication factors of each message, including the perceived message purpose (Rimer and Kreuter, 2006; Rice and Atkin, 2013). Evaluation of perceived message purpose; whether they perceived each message to be informative, empowering, or persuasive, was quantified objectively using a 3-item Likert-type scale. Response options for all items ranged from (1) strongly disagree to (5) strongly agree. Assessing the input factor of ‘perceived message purpose’ provided preliminary evidence on whether a specific purpose (informative, empowering, or persuasive) resonated with the participants and influenced the output (likelihood to discuss preferences with their clinician or family member).
2.5.4 Channels of communication exchange
Participants provided subjective feedback regarding their perceptions of the channels of communication exchange used to disseminate, as well as display, messages related to their values. Items about channels of communication exchange included: (i) who they prefer to be present while taking assessments and viewing results, (ii) preferred location and device-type for taking assessments and viewing results, (iii) comfort with receiving assessment and results through MyChart (i.e., patient portal to access health information), (iv) feelings about taking BWS assessments multiple times (e.g., every 3 months), (v) whether it is valuable to see if their preferences and values change over time, and (vi) how they prefer to share results with either clinicians or family/caregivers.
2.6 Data analysis
Descriptive statistics were used to summarize participants’ demographic characteristics and comfort level with technology. Three members of our research team (AC, EK, and CM) were involved in the primary qualitative thematic analysis. AC performed quantitative analyses for all primary and secondary outcome measures. Qualitative and quantitative analyses were performed in Microsoft Excel.
2.6.1 Primary - qualitative
Semi-structured interview data were analyzed subjectively using a hybrid approach to thematic analysis, including three phases of analysis in which data were refined to assess the meaningfulness of themes related to M1, M2, and M3 (Swain, 2018). In phase 1 of the thematic analysis, data from interviews were categorized by a priori themes from the interview questions (motivation, confidence, likelihood to act). In phase 2, one researcher (AC) created the initial a posteriori codes and applied frequency counts for each time the code appeared in the transcripts. This was followed by independent reviews from two researchers (EK and CM) who looked for meanings and patterns in the interviews, assessing initial codes and creating new codes where necessary. Discrepancies were then collectively addressed, leading to final consensus on the codes. In phase 3, we combined the a priori and a posteriori codes into family codes to structure the findings from the interviews (Swain, 2018). All codes underwent a comprehensive review and were systematically clustered into overarching themes through collaborative discussion and consensus-building among the three researchers (AC, EK, and CM). Individual responses to each message were also subjectively analyzed to assess whether there was variability in how participants responded to each message.
2.6.2 Primary - quantitative
Semi-structured interview data were summarized through two-way frequency tables to report perceived confidence, motivation, and likelihood to act (i.e., share or discuss their preferences and values with their clinician or family/caregiver) for each message. Perceived confidence, motivation and likelihood to act were objectively summarized by whether participants indicated the messages increased, somewhat increased, decreased, had no change effect or were uncertain of the messages impact, revealing the distribution across the three messages. Individual variability in response to each message were objectively quantified to assess the percentage of participants that found differences within each message. Perceived confidence, motivation and likelihood to act were evaluated by order of presentation by reporting mean and standard error to objectively assess potential carryover effect and observable trends in the data. Each message was also ranked by the frequency count for whether the message increased or somewhat increased participants’ perceived confidence, motivation, and likelihood to act.
2.6.3 Secondary - quantitative
Descriptive statistics were used to report the mean and standard deviation for the PME, PMR, and perceived message purpose scores. The PME and PMR total mean scores for each message were calculated by averaging three and two subscales, respectively. PME and PMR were also analyzed by assessing whether the total mean score for each message was above the midpoint score (3.0) of the scale, as well as the deviation from the standardized scores (Z-scores) of participants. Total mean scores above the PME midpoint score (3.0) indicate participants, on average, perceived the messages to be effective for (i) making them feel that sharing their preferences will benefit them, (ii) sharing their preferences is a good idea and (iii) feeling encouraged to discuss their preferences. Total mean scores above the PMR midpoint score indicate participants, on average, perceived messages to be (i) written personally for them, and (ii) relevant to their situation. Positive PME and PMR scores (above the study mean) indicate a participant perceived the messages as more effective or relevant than the sample mean. Negative PME and PMR scores indicate a participant perceived the messages as less effective or relevant than the sample mean. Individual variability in response to each message were objectively quantified to assess the percentage of participants that found differences in PME and PMR within each message. Perceived message purpose was evaluated by order of presentation by reporting mean and standard error to objectively assess potential carryover effect and observable trends in the data. Each message was subjectively ranked using the mean value of perceived message purpose to evaluate which messages were considered the most informative, empowering and persuasive.
Descriptive statistics were used to summarize channels of communication exchange (i.e., how participants prefer to complete the BWS assessment and review their results). Each variable for channel of communication exchange were counted and analyzed through frequency tables, revealing the distribution among participants.
2.7 Ethics statement
This study was approved by the UNC Lineberger Comprehensive Cancer Center Protocol Review Committee and the University of North Carolina IRB.
3 Results
3.1 Participant characteristics
Thirty-five patients were approached to participate in the study between August 1, 2023, and September 29, 2023. Eligible patients were approached by study team members either during their in-patient stay at the North Carolina Basnight Cancer Hospital (n = 22) or via phone (n = 13). Sixteen chose to enroll in the study (46% participation rate), but one withdrew after completing the best-worst scaling (BWS) assessment, stating they were unable to concentrate. Another participant completed the quantitative part of the study, but not qualitative portion due to exhaustion. As such, the sample size for analysis was 15 patients for most quantitative measures and 14 for qualitative items. All participants reviewed M1 first, then were randomized to receive M2, then M3 (n = 5/15) or M3, then M2 (n = 10/15). Participants were interviewed either in their inpatient room at the North Carolina Basnight Cancer Hospital (n = 10/15), via Zoom (n = 3/15), or in a meeting room at the North Carolina Basnight Cancer Hospital (n = 2/15).
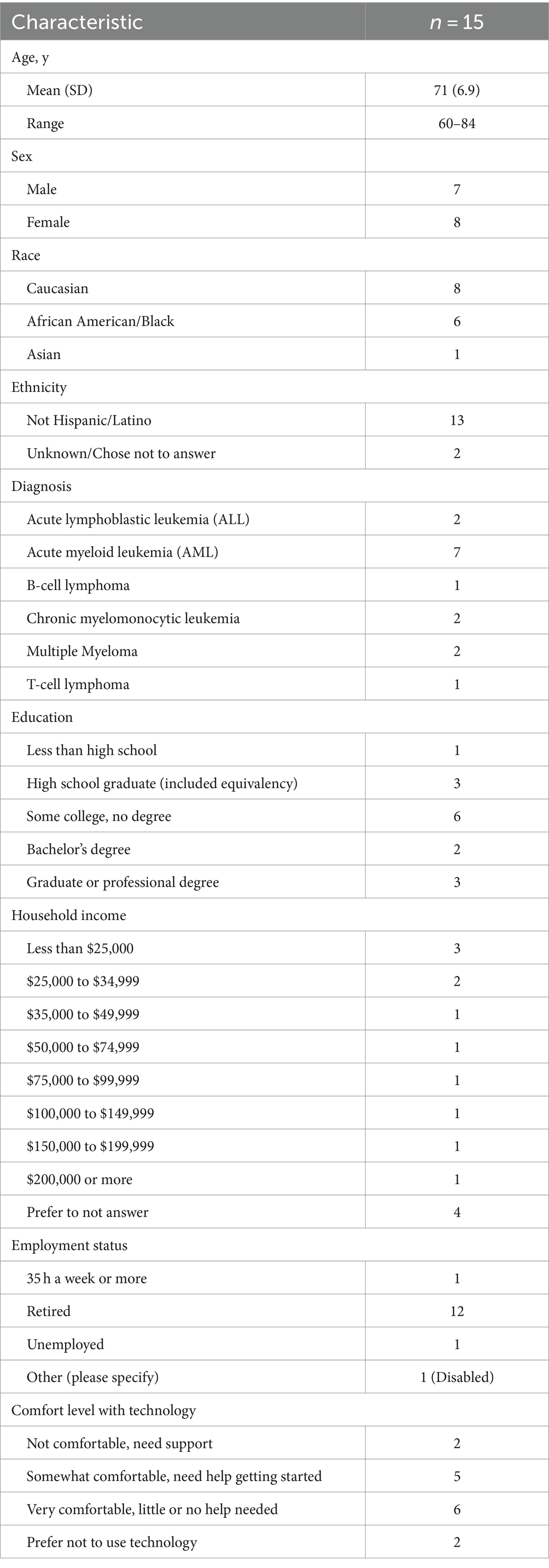
Table 2 summarizes demographic information and comfort level with technology for all participants.
The median age of all participants was 71 years (range: 60–84). All participants had a confirmed diagnosis of hematologic malignancy including leukemia (n = 11/15), lymphoma (n = 2/15), and myeloma (n = 2/15). In our participant population, 53% (n = 8) were female, and 47% (n = 7) were male. Participants identified as Caucasian (n = 8/15), African American/Black (n = 6/15), and Asian (n = 1/15). Participants ranged in level of education, with the majority having some college, but no degree (n = 8/15), and others identifying as a high school graduate (n = 3/15), having a graduate or professional degree (n = 3/15) or a bachelor’s degree (n = 2/15), and not completing high school (n = 1/15). The median household income was $35,000 to $49,999. Most participants were either very comfortable (n = 6/15) or somewhat comfortable (n = 5/15) with technology, however 13% (n = 2/15) were not comfortable and needed support and 13% (n = 2/15) preferred not to use technology at all.
3.2 Primary outcomes
3.2.1 Affective-cognitive (confidence and motivation) and behavior (likelihood to act) outcomes
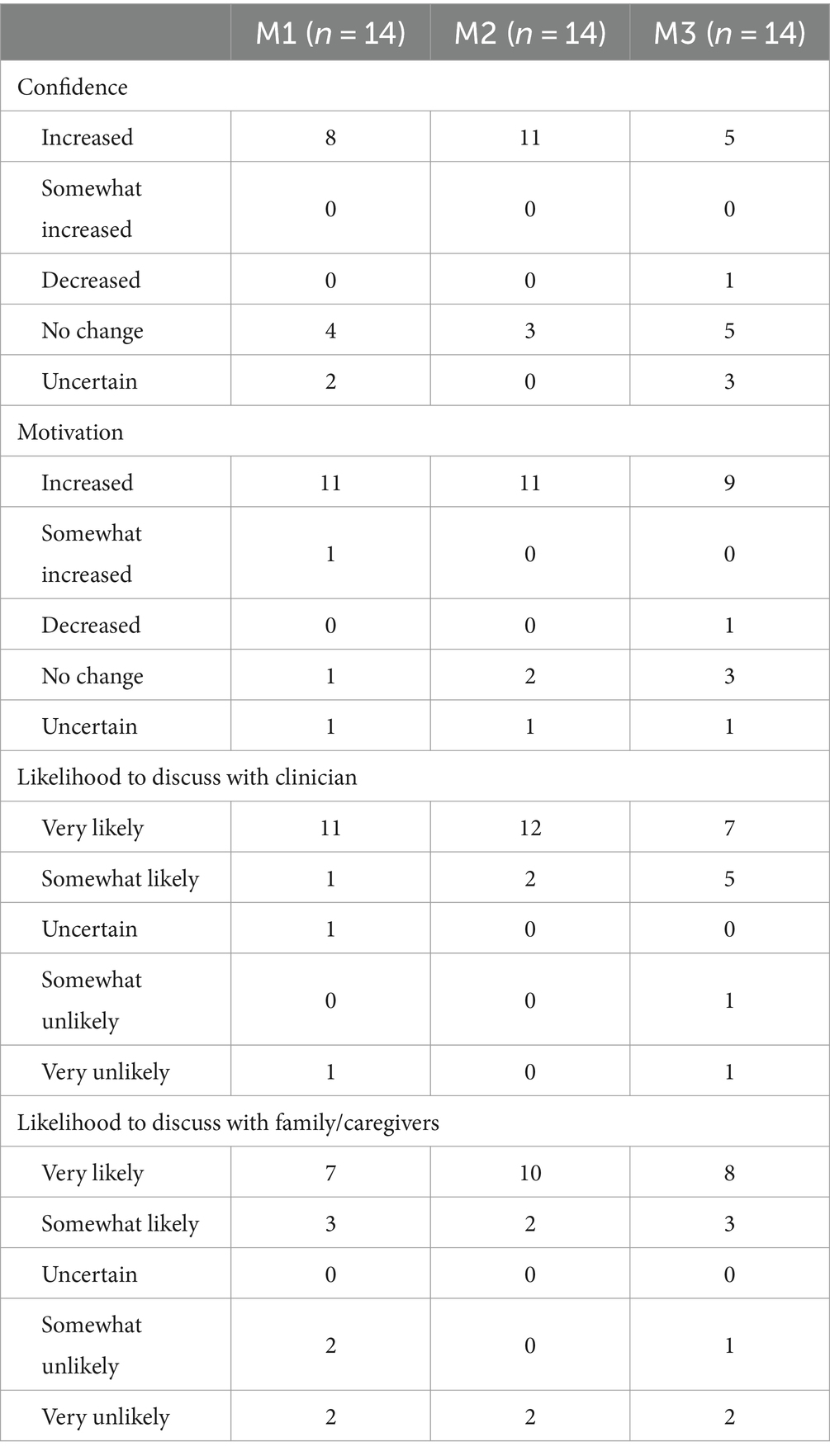
Table 3 summarizes the qualitative responses related to confidence, motivation, and likelihood to act for M1, M2 and M3. Supplementary Table SC reports data trends in perceived confidence, motivation, and likelihood to act, based on order of message presentation.
3.2.1.1 Confidence
Participants’ responses to whether the message impacted their confidence in discussing their preferences with their clinician indicate that M2, (developed to be moderately direct) had the largest impact on increasing participants’ confidence (n = 11/15), followed by M1 (n = 8/15), then M3 (n = 5/15), regardless of order of presentation (M1-M2-M3 vs.M1-M3-M2). After reviewing M1, some participants (n = 6/15) indicated they were already prone to discuss their preferences, and/or the content of the message would not impact their confidence in discussing their preferences with their clinician. However, through qualitative analysis, we did find variation in individual responses after participants reviewed all messages. For example, one participant stated they already felt confident, and that M1 or M2 would not impact whether they discussed their preferences. M1: “No, I am already confident.” M2: “No, my confidence is already high. I’d talk to him [clinician] anyway. He [clinician] always asks me what I want.” However, after reviewing M3, they stated they felt “Less confident. Having a difference in opinion would change my confidence.” (Female [F], 69 years old [y]).
3.2.1.2 Motivation
Participants’ responses to whether the message impacted their motivation in discussing their preferences with their clinician indicate that M1 had the largest impact on increasing participants’ motivation (n = 12/15), followed by M2 (n = 11/15), then M3 (n = 9/15), regardless of order of presentation. After reviewing M1, 80% (n = 12/15) of participants indicated the message would positively impact their motivation. However, through qualitative analysis, we did find variation in individual responses after participants reviewed all messages. For example, one participant indicated, “Yes, It [M1] makes it front and center to the extent that I would feel it was important [to discuss preferences].” After reviewing M2, they indicated “yes, more [motivating] than first message” and “It makes me feel like I am better equipped.” After reviewing M3, his motivation was decreased in discussing his preferences with his clinician, stating “No, it would probably decrease it. I do not know why I would bother, this does not help, it’s more like a disclaimer than something you would want to talk to him about.” (M 64y).
3.2.1.3 Likelihood to discuss preferences with clinician
Participants responses to whether each message impacted their likelihood of discussing preferences with their clinician indicated they were very likely to discuss based on M2 (n = 12/15), M1 (n = 11/15), and M3 (n = 7/15), with mean results varying slightly with the order of presentation. One participant indicated they were uncertain if they would discuss their preferences, stating “Whoever is my clinician should know just as much as I do or more, about myself. So why should I discuss it with them?” (M 79y).
3.2.1.4 Likelihood to discuss preferences with family/caregiver
Participants responses to whether the message impacted their likelihood of discussing preferences with their family member or caregiver indicated they were very likely to discuss based on M2 (n = 10/15), M3 (n = 8/15), and M1 (n = 7/15), with mean results varying slightly with the order of presentation. Participants who indicated they were somewhat or very unlikely to discuss with their family members or caregivers mentioned that conversations related to their cancer are too difficult for family members, they do not want to burden or make their family worry about them, or they feel they need answers from their clinician before talking to their family. One participant stated they were unlikely to discuss with his family (after reviewing M1 & M2), but after reviewing M3, he stated he would be somewhat likely to discuss with his family because it made him “realize that there are other perspectives than mine.” (M 75y).
3.3 Secondary outcomes
3.3.1 Perceived message effectiveness
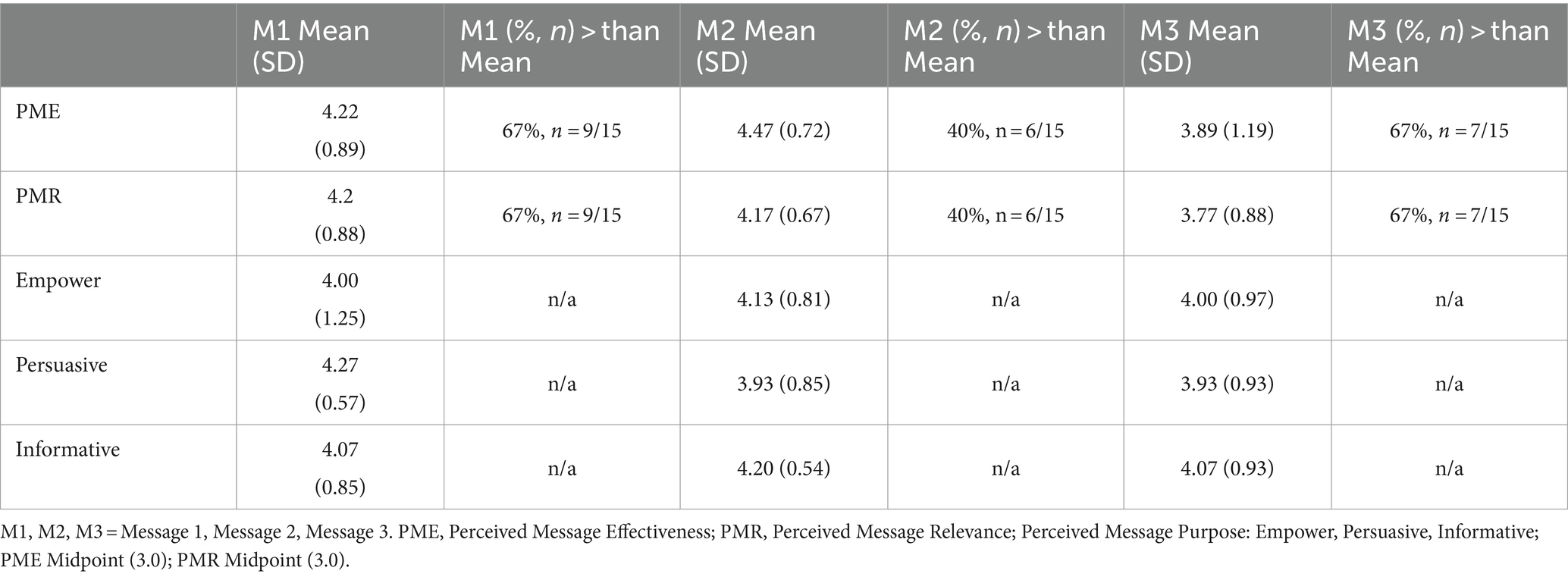
The total mean value of the PME for M1, M2, and M3 were all greater than the midpoint (3.0) of the PME scale, and deviations from the sample means varied per message (Table 4). The mean values indicate that participants, on average, perceived the messages to be effective for (i) making them feel that sharing their preferences will benefit them, (ii) sharing their preferences is a good idea and (iii) feeling encouraged to discuss their preferences. Seventy-three percent of participants reported individual differences between messages.
3.3.2 Perceived message relevance
We observed that many participants found it challenging to answer the two reverse coded PMR questions. At least half of the participants asked for help on understanding what the reverse coded question was asking. After providing assistance, they were still unable to answer the question confidently. Therefore, only the two PMR questions that were framed in the positive were used for data analysis.
The total mean value of the PMR for M1, M2, and M3 were all greater than the midpoint (3.0) of the PMR scale, and deviations from the sample means varied per message (Table 4). The mean values indicate that participants, on average, perceived messages to be (i) written personally for them, and (ii) relevant to their situation. Eighty percent of participants reported individual differences between messages.
3.3.3 Perceived message purpose
Each message was developed with a particular purpose; M1: Informative, M2: Empowering, M3: Persuasive (Table 1). The mean value and standard deviation for each perceived message purpose is reported in Table 4. Participants felt that M1 was informative, but also found M2 and M3 to be similarly informative. M1 contained 2 question prompts, but only one participant mentioned these questions when providing feedback. Participants felt that M2 was the most empowering and was ranked higher than M1 or M3. M2 contained 4 question prompts, with qualitative analysis revealing that 80% (n = 12/15) of participants perceived the question prompts would be helpful in discussing their preferences with their clinician. Participants perceived M3 to be persuasive, but less persuasive than M1 or M2, regardless of order of presentation. The ranking of each message by purpose are as follows: Informative (M2, M1, and M3), Empowering (M2, M1, and M3), and Persuasive (M1, M2, and M3). Data trends based on order of message presentation suggest that the ordering of messages was not highly influential on perceived message purpose though sample size was insufficient to adequately determine this relationship (see Supplementary Table SC).
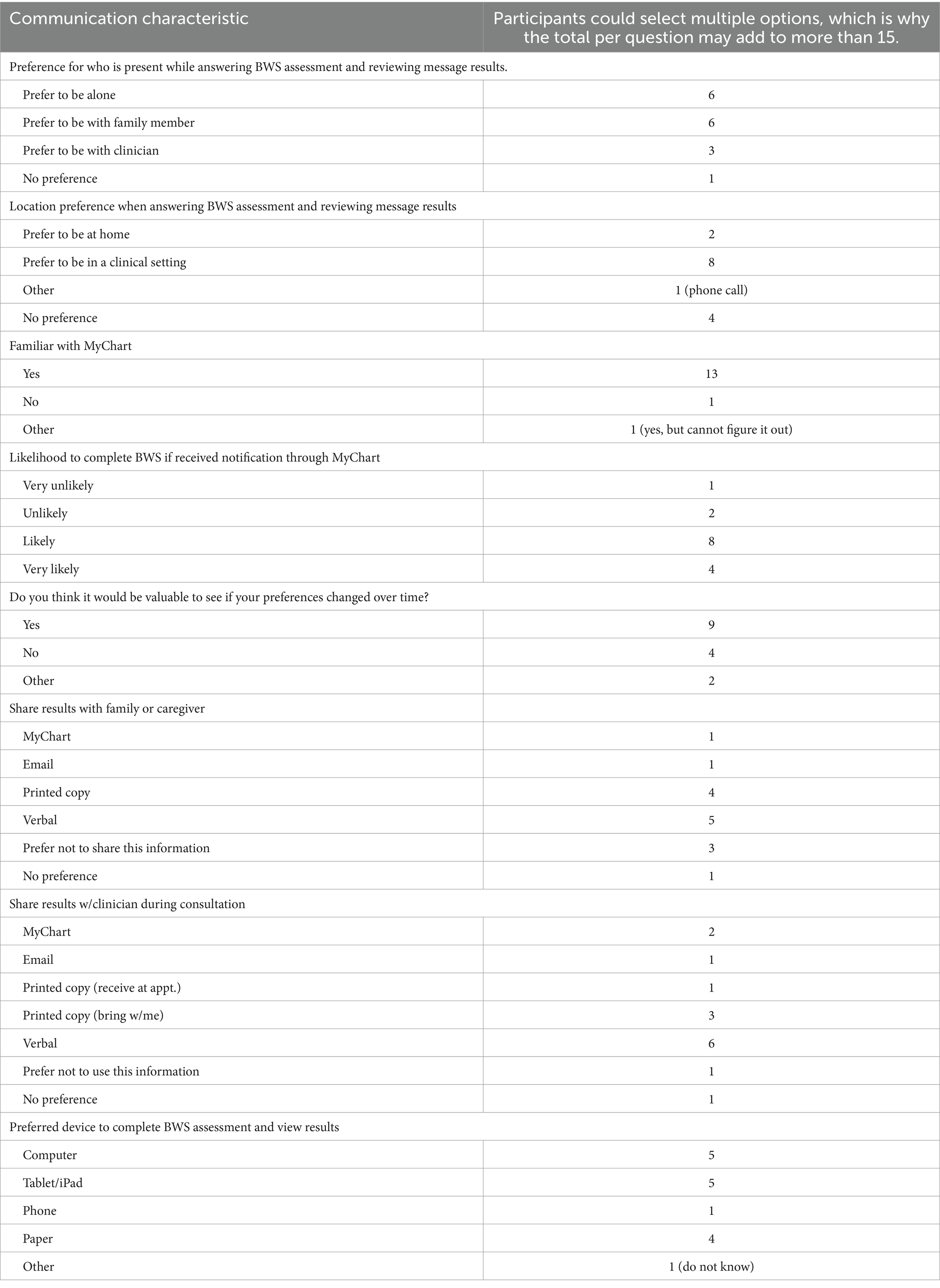
3.3.4 Channels of communication exchange
Participants preferred to be in a clinical setting (n = 8/15), alone (n = 6/15), or with a family member (n = 6/15) to complete the BWS assessment and review the results (Table 5). Ninety-three percent (n = 14/15) of participants were familiar with MyChart, although one participant indicated they were aware of MyChart, but were unable to figure it out. Of those 14 participants, 86% (n = 12/14) indicated they would be likely or very likely to complete the BWS if they received a notification through MyChart. Sixty percent (n = 9/15) of participants thought it would be valuable to take the BWS assessment multiple times; the remaining did not believe their preferences would change. Most participants who indicated they would share this information with their clinician preferred to share the information verbally (n = 6/15), or via a printed copy (n = 4/15). One participant did not want to share this information, as they believed that if their clinician knew their preferences, it may negatively impact their treatment. Most participants who indicated they would share this information with their family member or caregiver preferred to share the information verbally (n = 5/15), or via a printed copy (n = 4/15). Participants indicated they preferred using an electronic method [computer (n = 5/15), tablet/iPad (n = 5/15)] to complete the BWS and view results as opposed to on paper (n = 4/15), or over the phone (n = 1/15).
3.4 Thematic analysis
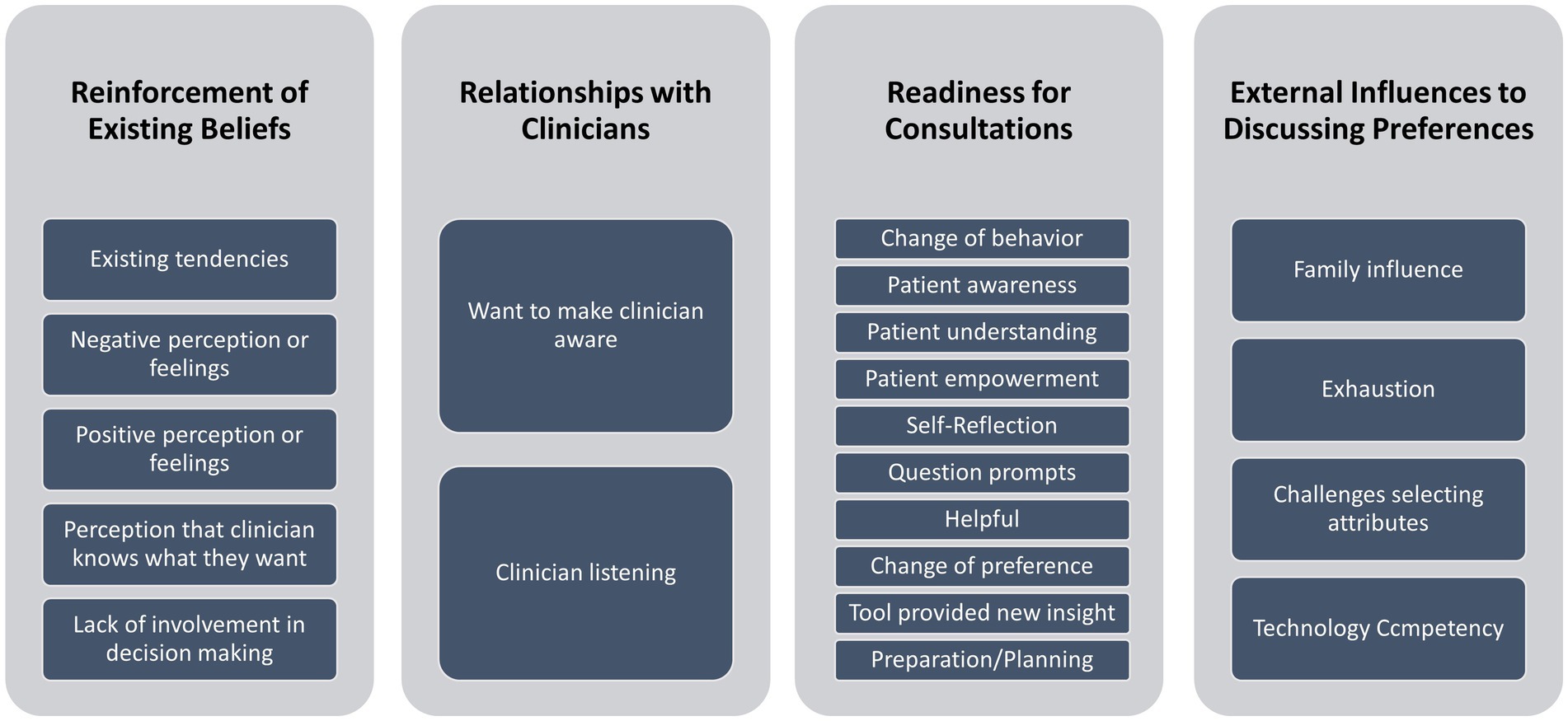
Twenty-one a posteriori codes were developed after reviewing each transcribed interview. We summarized the interviews, then combined the a priori and a posteriori codes resulting in four major themes: (i) readiness for consultations, (ii) relationships with clinicians, (iii) reinforcement of existing beliefs, and (iv) external influences to discussing preferences. (see Figure 2 – Thematic Analysis).
3.4.1 Readiness for consultations
Participants indicated that after reviewing certain messages they felt a sense of self-awareness or self-reflection of what was important to talk about with their clinicians.
“It made me feel like I was thinking through the process and what it was that was important to me. It was good exercise, to think about that this thing is significant and this thing is not.” (M1: M 64y).
“It has enlightened me to make sure I stay on top of the situation.” (M2: M 64y).
“It would help clear my thoughts about myself, and what he [clinician] thinks. I might get more information about my own thoughts about living longer. I can always give them feedback of what I am doing on my own” (M3: F 77y).
“It makes me think, um, kind of deep, I never thought about it like that. But, those side effects I did not know there was a difference in long or short side effects.” (M1: F 60y).
“Well I would feel good about discussing. It might change my preferences after reading it though. Right now, chemo is not in my game plan. Potential short term discomfort are different than someone going through chemo/radiation. I’m interested in living longer because side effects are minimal. If I had the options of chemo/radiation with serious side effects, I’d have to think about my goals and prospect a lot more.” (M3: M 80 y).
Participants indicated the messages would help prepare them for their consultations, specifically due to the question prompts that were provided to them.
“I did not know about asking these questions. I have talked to him about options, if what I am going through does not work. Never really asked him about side effects. These are important questions to be discussed.” (M2: F 66y).
“I liked it because they had specific questions. When you are going through this, there are so many questions running through your brain and you cannot think of everything. Those questions are important for making a treatment plan. This was more beneficial for me.” (M2: F 66y).
For some participants, providing them with a question prompt list positively impacted their confidence.
“I’d feel good about. I like the questions. Asking the questions is important. I kind of know what side effects are life long and irreversible. It encourages me to ask the questions.” (M2: M 75y).
One participant, after reviewing M1 stated “I do not have a problem discussing anything with my doctor. Actually, it would not increase it [confidence].” Then, after M3 stated, “Like I said, I do not have any problem talking to him about anything. I tell him how I feel and what I think will happen.” When asked whether M2 impacted her confidence, she stated “Yes, more than the message that did not have questions.” She further explained that “It [M2] makes me feel like I really should ask him these questions. A lot of these questions would be helpful to know.” and “this is more specific. I know how to word the questions, and which questions to ask him.” (F 60y).
Participants indicated they felt a sense of empowerment or control over how to engage with their clinicians.
“I would discuss it with my doctor. I would not have known to talk about this [preferences] with him [clinician] before.” (M1: F 60y).
“I could tell him [clinician] that I did take this survey and this is what is most important and not me just talking off the top of my head.” (M1: F 66y).
“I like it better. It makes me feel like I am better equipped. These are specific things that potentially are options or things that benefit me that I’m not aware of. Also, it made me think about quality of life. I had not factored that into it. The first message did not give me extra information. This is a good way to tease things out.” (M2: M 64y).
“I know it is true that they have their general beliefs about what is going to happen and what they need to do. It’s a good statement to have in there about their beliefs may be different. And that you need to communicate if they do not ask you. It’s important for them to treat you as a person first then as a patient.” (M3: F 66y).
3.4.2 Relationships with clinicians
Participants mentioned their existing relationships with their clinicians, and how that has an impact on whether they would discuss preferences during consultations.
For some participants, their clinicians have already engaged them in discussing their preferences, therefore they feel comfortable having these discussions.
“He knows from day 1 what I want and he is that kind of doctor.” (M1: F 66y).
“My confidence is already high. I’d talk to him anyway. He always asks me what I want.” (M2: M 65y).
“I agree with the information. I love traveling, and it’s becoming more of a challenge for me. That’s why the long term effects I am trying to avoid, or I want to fix them. Also, I do not want to be in hospital, unless I do not have any control over myself. My clinician does know how these things are important to me.” (M1: F 77y).
“I was going to discuss anyway. I have been discussing.” (M1: F 73y).
Other participants indicated they had not previously discussed their preferences with their clinicians. Reviewing the messages made them recognize the need to discuss their preferences. They felt having this information was beneficial toward developing a relationship in which they feel comfortable discussing their preferences with their clinician.
“Definitely inclined to discuss my preferences to make sure the clinician is made aware of my expectations and to make sure he is onboard with the same goal.” (M2: M 64y).
“This would make me want to discuss my preferences with them. He is there to help you, but he needs to know what you want, and what your family wants.” (M2: F 66y).
“It makes me feel like he will listen to me.” (M2: F 71y).
3.4.3 Reinforcement of existing beliefs
For some participants, certain messages reinforced their existing beliefs about what they considered most important, and in some cases motivated them to ensure their preferences were discussed.
For example, one participant indicated “Yes, It [M1] has already done that,” referencing an earlier statement that he was definitely going to discuss his preferences. He also indicated M1 motivated him to discuss “long term side effects that I had not considered about, if this was a side effect of age or treatment.” When asked if motivation was impacted after reviewing M2, he indicated “Yes. It’s reinforcing the thoughts that I am having to encourage me [discuss preferences] and that I am not on a limb doing something stupid.” When asked if motivation was impacted after reviewing M3, he indicated “It would increase it. I like that it lays the take on the line. It explains that my clinician may not find living longer important.” (M 80y).
“It would just reinforce my thoughts and what I am looking to achieve by getting all this treatment.” (M1: M 64y).
“It is right on target because from the beginning of my diagnosis, this is what I talked about with my clinician. He asked me what was most important. I wanted to live longer, but I wanted my quality of life to do things. I do not want to be stuck in the hospital.” (M1: F 66y).
“It’s pretty much what my thoughts are. I have 3 kids and want to see them get married and have kids. I want to walk her down the aisle. The message reinforced how I was thinking.” (M1: M 64y).
“It brings in what we discussed about side effects. It reinforces my need to bring up what’s important to me. All worthwhile questions.” (M2: M 75y).
“I feel it reinforces what my feelings are and I want to make sure the provider is made aware of my expectations.” (M3: M 64y).
“I imagine this was supposed to motivate me, but it is more of an affirmation to do so [discuss preferences] than further motivation. It reinforces an original belief.” (M3: M 75y).
3.4.4 External influences to discussing preferences
Participants indicated that aspects such as desire to share preferences with family members, beliefs that clinicians already know what’s most important to patients, or expressing financial concerns have influences on whether patients discuss their preferences with either clinicians or family members.
Some participants felt the information was helpful for conveying their preferences to family members.
“I would share it with my family so they would know what my long-term goals are and for chemotherapy” (M1: F 73y).
“This would make me want to discuss my preferences with them [family]. He [clinician] is there to help you, but he needs to know what you want, and what your family wants.” (M2: F 66y).
Some participants stated that the presence of family members may impact their desire to discuss their preferences with their clinician. For example, one participant indicated he would not have felt comfortable answering these questions if his wife were present. He further explained that it would be too challenging because it is harder to talk about his preferences with her. (M 64y).
Other participants were less encouraged to discuss their preferences, or had pre-existing beliefs that their clinicians were already aware of what was most important to them.
“I would not talk to my doctor or family about it. Certain things you do not tell. I’m a very private person.” (M1: M 79y).
“I figure they [clinicians] should know more than I know.” (M3: F 71y).
Some participants initially thought their clinician knew what was most important to them, but after reviewing the messages, indicated the importance of discussing their preferences with their clinicians.
“I think he knows most of it. But what we think, he may not know. It’s important to discuss.” (M1: M 75y).
“It encourages me more. It hits home to say clinicians are busy people, they have a lot to take in from people, but I do not read their notes they put in. It’s a logical assumption, they now know what I’m interested in. It drives home that he does not know that we feel that way.” (M3: M 75y).
“It would help clear my thoughts about myself, and what he [clinician] thinks. I might get more information about my own thoughts about living longer. I can always give them feedback of what I am doing on my own.” (M3: F 77y).
“It puts it in a frame of reference. It makes you question if they [clinicians] know your preferences.” (M1: M 75y).
One participant did not want her clinician to know that avoiding high financial costs was most important to her. She expressed concerns about letting him know because she felt that if the clinician knew she had financial concerns, she may not receive the best care. (F 84y).
4 Discussion
This study provides new information to suggest that informative and empowering messages with tailored question prompt lists are likely effective at preparing older adults with blood cancers for shared decision-making. Participants found the informative message (M1) and the empowering message (M2) most effective in increasing confidence, motivation, and likelihood to discuss their preferences with their clinician. These messages both contained question prompts which were absent from the persuasive message (M3). Participants reported that these question prompts were very helpful in preparing them for discussion with their clinician. This is consistent with previous studies that found that providing patients with question prompts encourages them to actively participate in their consultations (Clayton et al., 2003; Sansoni et al., 2015; Keinki et al., 2021; Terrasson et al., 2022). M3 was designed to be persuasive and more direct. Although generally participants found the message to be helpful, this message was found to be disconcerting to some and reduced confidence, motivation, and likelihood to discuss preferences in others. This may suggest that such messages are less effective than informative and empowering messages, though larger studies specifically designed to detect statistically significant differences between messages are needed.
Most participants also reported that having tailored information about their preferences impacted their readiness for their consultations. Participants’ sentiments indicate they felt having this information gave them a sense of self-awareness and self-reflection on what is most important to them, and a sense of empowerment to discuss their preferences. Most frequently, participants focused on the benefits of knowing what questions to ask their clinician and felt having a specific list of questions would best prepare them to discuss their preferences. For some participants, having access to the question list positively impacted their confidence. For those who indicated it did not increase confidence, it was because they felt they already had adequate confidence to discuss their preferences with their clinician. However, participants also reported that while their confidence may not be impacted due to existing perceived tendencies to communicate, their motivation was positively impacted by having a specific list of questions to ask their clinician. Participants also reported the messages reinforced their existing beliefs. For many participants this was an affirmation of what is most important to them, and for others was a motivator to ensure they discuss their preferences with their clinicians.
Participants also reported that external influences including family members, innate trust in clinicians to already know what is most important, and expressing financial concerns, may impact whether they discuss their preferences. This is consistent with previous studies that found external factors to cause higher levels of distress among cancer patients and influenced whether patients actively engaged in their consultations (Cavers et al., 2013; Mead et al., 2013; Carrera et al., 2018; Perez Jolles et al., 2019; Bartlett et al., 2020; Kim and Lee, 2023).
Evidence from this study suggests that participants’ perceptions of confidence, motivation, and likelihood to act changed based on the information presented in the varied messages. This was a critical finding, as the information presented in M2 had a positive change influence, while M3 had mixed influences, and even lowered the confidence of some participants for discussing preferences. Participants provided mixed feedback on whether it is important to know their clinician may have a different opinion about what is most important regarding treatment outcomes. While some participants indicated this may provide more of a reason to discuss their preferences, others found it disconcerting and were not certain they would discuss their preferences. Previous research indicates that cancer patients have varying perspectives on whether their treatment decisions are unduly influenced by knowing their clinicians’ opinions (Ryan et al., 2009). This research suggests that clinicians’ standard communication approaches should be carefully balanced with respecting cancer patients’ diverse opinions (Ryan et al., 2009). This highlights the need to validate the input communication factors within values-clarification tools before presenting results to patients, especially when messages are tailored to patients based on what they identified as the most important treatment outcome.
Participants’ communication channel preferences also varied regarding who should be present when completing and reviewing BWS results, the location of where they would be most comfortable completing and reviewing BWS results, their desire to repeat assessments over time, and preferred device type. This information is important to capture for future research and clinical implementation of tools.
Lastly, while combining the quantitative and qualitative results together, it is important to note that all messages met the minimum scoring thresholds to be considered acceptable, with participants’ sentiments regarding M1 and M2 being generally more positive. Specifically, participants’ sentiments regarding M2 mainly focused on the benefits of having a list of questions to discuss with their clinician. Sentiments regarding M3 were mixed with some participants indicated that M3 may provide more of a reason to discuss their preferences, others found it disconcerting and were not always certain they would discuss their preferences.
4.1 Limitations
Our study had several limitations. First, most interviews took place during a hospitalization. This included patients who were recruited over the phone but asked to hold the interview during their upcoming inpatient stay. This environmental context may have influenced participants responses to the questions, especially for interviews in which participants were actively receiving chemotherapy (feeling tired or expressing they had “chemobrain”), or in which family members were present, as some participants were unlikely to discuss preferences with family members. We sought to evaluate patients in different contexts to provide us the opportunity to better understand these factors and ultimately develop better values-clarification tools (Ryan et al., 2009; Thorne et al., 2013). These contextual factors were valuable to describe, especially since our study participants were demographically diverse, specific to race, gender, education, income and comfort level with technology. Future research should consider the impacts of these factors and whether there are disparities in rates of patient participation between Caucasian and Black/African American patients, as suggested by a recent systematic review (Perez Jolles et al., 2019).
A second limitation is that messages M2 and M3 were not tailored to each participant. Participant responses may have been biased, depending on whether or not the static results aligned with their most important treatment outcome. Presenting all three messages based on their personal BWS results might have resulted in different results. For the patients in which M2 and M3 messages aligned with their preferences, they may have had more of an emotional response and felt the message was more meaningful. Although we did not see differences in perceived message relevance for M2 or M3 based on whether the results aligned with participant preferences, our small sample size limited evaluating this adequately.
Lastly, we recognize that there may have been carryover effects from one message to another that are not accounted for in our analysis. We sought to limit these by randomizing M2 and M3 though carryover from M1 may have influenced outcomes. Data trends (see Supplementary Table SC) reveal that most perceptions were consistent regardless of order of presentation. Likely, other contextual factors that were not captured, such as personality, influenced how these messages are perceived. Further research should explore the specific factors that contribute to these perceptions and how they impact participants’ confidence, motivation, and likelihood to act.
5 Conclusion
We used an exploratory mixed methods design to assess varying input communication factors of three distinct messages to better understand the impacts on participants perceived affective-cognitive (confidence and motivation) and behavior (likelihood to act) outcomes when receiving tailored messages based on personalized values within a digital health tool. Overall, participants preferred messages that were moderately direct, contained succinct question prompts, and that were empowering. The preliminary evidence from this study will lead to future research evaluating how tailoring messages based on best-worst scaling results can improve SDM for older adults diagnosed with cancer.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by UNC Lineberger Comprehensive Cancer Center Protocol Review Committee and the University of North Carolina IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
AC: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Validation, Writing – original draft, Writing – review & editing. EK: Investigation, Writing – review & editing. CM: Writing – review & editing. AK: Writing – review & editing. LM: Funding acquisition, Supervision, Writing – review & editing. DR: Conceptualization, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study is funded in part by the Harry F. Bisel Endowed Young Investigator Award from the Conquer Cancer Foundation, Alexandria, Virginia (principal investigator: DR). We appreciate the financial support from the Integrated Well-Being Program at UNC Healthcare.
Acknowledgments
We would like to thank UNC Health for their ongoing support devoted to our research efforts. We would like to thank Mark Jackson for his help in writing the JavaScript code that was used to associate each tailored message with the corresponding attributes. We would like to thank Mireille Leone for assisting with the investigation for this study. We would like to thank Dorothy Sippo for her thoughtful input and revisions, which improved the quality of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2024.1347310/full#supplementary-material
References
Agency for Healthcare Research and Quality . (2023). About shared decision making Agency for Healthcare Research and Quality. About Shared Decision Making. Available at: https://www.ahrq.gov/sdm/about/index.html. (Accessed July 30, 2023).
Baig, S. A., Noar, S. M., Gottfredson, N. C., Boynton, M. H., Ribisl, K. M., and Brewer, N. T. (2019). UNC perceived message effectiveness: validation of a brief scale. Ann. Behav. Med. 53, 732–742. doi: 10.1093/abm/kay080
Bartlett, S. J., de Leon, E., Orbai, A.-M., Haque, U. J., Manno, R. L., Ruffing, V., et al. (2020). Patient-reported outcomes in RA care improve patient communication, decision-making, satisfaction and confidence: qualitative results. Rheumatology (Oxford) 59, 1662–1670. doi: 10.1093/rheumatology/kez506
Bories, P., Lamy, S., Simand, C., Bertoli, S., Delpierre, C., Malak, S., et al. (2018). Physician uncertainty aversion impacts medical decision making for older patients with acute myeloid leukemia: results of a national survey. Haematologica 103, 2040–2048. doi: 10.3324/haematol.2018.192468
Carrera, P. M., Kantarjian, H. M., and Blinder, V. S. (2018). The financial burden and distress of patients with cancer: understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J. Clin. 68, 153–165. doi: 10.3322/caac.21443
Cavers, D., Hacking, B., Erridge, S. C., Morris, P. G., Kendall, M., and Murray, S. A. (2013). Adjustment and support needs of glioma patients and their relatives: serial interviews. Psychooncology 22, 1299–1305. doi: 10.1002/pon.3136
Clayton, J., Butow, P., Tattersall, M., Chye, R., Noel, M., Davis, J. M., et al. (2003). Asking questions can help: development and preliminary evaluation of a question prompt list for palliative care patients. Br. J. Cancer 89, 2069–2077. doi: 10.1038/sj.bjc.6601380
Cole, A., Khasawneh, A., Adapa, K., Mazur, L., and Richardson, D. R. (2022). “Development of an electronic healthcare tool to elicit patient preferences in older adults diagnosed with hematologic malignancies” in Human aspects of IT for the aged population. Technology in Everyday Living: 8th international conference, ITAP 2022, held as part of the 24th HCI international conference, HCII 2022, virtual event, June 26 – July 1, 2022, proceedings, part II. eds. Q. Gao and J. Zhou, vol. 13331 (Berlin: Lecture Notes in Computer Science. Springer International Publishing), 210–228.
Cures Act Congress . (2021). Text - H.R.34 - 114th Congress (2015–2016): 21st Century Cures Act Congress.gov Library of Congress. Available at: https://www.congress.gov/bill/114th-congress/house-bill/34/text (Accessed October 21, 2021).
Hawkins, R. P., Kreuter, M., Resnicow, K., Fishbein, M., and Dijkstra, A. (2008). Understanding tailoring in communicating about health. Health Educ. Res. 23, 454–466. doi: 10.1093/her/cyn004
Hunter, N. L., O’Callaghan, K. M., and Califf, R. M. (2015). Engaging patients across the spectrum of medical product development: view from the US food and drug administration. JAMA 314, 2499–2500. doi: 10.1001/jama.2015.15818
Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC: The National Academies Press.
Jensen, J. D., King, A. J., Carcioppolo, N., and Davis, L. (2012). Why are tailored messages more effective? A multiple mediation analysis of a breast cancer screening intervention. J. Commun. 62, 851–868. doi: 10.1111/j.1460-2466.2012.01668.x
Keinki, C., Momberg, A., Clauß, K., Bozkurt, G., Hertel, E., Freuding, M., et al. (2021). Effect of question prompt lists for cancer patients on communication and mental health outcomes-a systematic review. Patient Educ. Couns. 104, 1335–1346. doi: 10.1016/j.pec.2021.01.012
Kim, Y. M., and Lee, J. E. (2023). Dyadic effects of psychological health on quality of life in patients with colorectal Cancer and caregivers: a systematic review and Meta-analysis. Semin. Oncol. Nurs. :151477. doi: 10.1016/j.soncn.2023.151477
Kreuter, M. W., Farrell, D. W., Brennan, L. K., and Olevitch, L. R. (1999). Tailoring health messages: Customizing communication with computer technology (Routledge communication series). 1st Edn. London, UK: Routledge, 288.
Kreuter, M. W., and Wray, R. J. (2003). Tailored and targeted health communication: strategies for enhancing information relevance. Am. J. Health Behav. 27, S227–S232. doi: 10.5993/ajhb.27.1.s3.6
Kwong, E., Cole, A., Khasawneh, A., Mhina, C., Mazur, L., Adapa, K., et al. (2022). Evaluation of data visualizations for an electronic patient preferences tool for older adults diagnosed with hematologic malignancies. Workshop on visual analytics in healthcare (VAHC). IEEE; pp. 1–6.
Lafata, J. E., Shay, L. A., and Winship, J. M. (2017). Understanding the influences and impact of patient-clinician communication in cancer care. Health Expect. 20, 1385–1392. doi: 10.1111/hex.12579
LeBlanc, T. W., Fish, L. J., Bloom, C. T., el-Jawahri, A., Davis, D. M., Locke, S. C., et al. (2017). Patient experiences of acute myeloid leukemia: a qualitative study about diagnosis, illness understanding, and treatment decision-making. Psychooncology 26, 2063–2068. doi: 10.1002/pon.4309
Loh, K. P., Abdallah, M., Kadambi, S., Wells, M., Kumar, A. J., Mendler, J. H., et al. (2021). Treatment decision-making in acute myeloid leukemia: a qualitative study of older adults and community oncologists. Leuk. Lymphoma 62, 387–398. doi: 10.1080/10428194.2020.1832662
Mead, E. L., Doorenbos, A. Z., Javid, S. H., Haozous, E. A., Alvord, L. A., Flum, D. R., et al. (2013). Shared decision-making for cancer care among racial and ethnic minorities: a systematic review. Am. J. Public Health 103, e15–e29. doi: 10.2105/AJPH.2013.301631
Mohile, S. G., Dale, W., Somerfield, M. R., Schonberg, M. A., Boyd, C. M., Burhenn, P. S., et al. (2018). Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J. Clin. Oncol. 36, 2326–2347. doi: 10.1200/JCO.2018.78.8687
Noar, S. M., Gottfredson, N., Vereen, R. N., Kurtzman, R., Sheldon, J. M., Adams, E., et al. (2023). Development of the UNC perceived message effectiveness scale for youth. Tob. Control. 32, 553–558. doi: 10.1136/tobaccocontrol-2021-056929
Perez Jolles, M., Richmond, J., and Thomas, K. C. (2019). Minority patient preferences, barriers, and facilitators for shared decision-making with health care providers in the USA: a systematic review. Patient Educ. Couns. 102, 1251–1262. doi: 10.1016/j.pec.2019.02.003
Rice, R. E., and Atkin, C. K. (2013). Public communication campaigns. Thousand Oaks, CA: SAGE Publications, Inc.
Richardson, D. R. (2022). Mproving personalized treatment decision-making for older adults with cancer: the necessity of eliciting patient preferences. J. Geriatr. Oncol. 13, 1–3. doi: 10.1016/j.jgo.2021.06.001
Richardson, D. R., Crossnohere, N. L., Seo, J., Estey, E., O'Donoghue, B., Smith, B. D., et al. (2020). Age at diagnosis and patient preferences for treatment outcomes in AML: a discrete choice experiment to explore meaningful benefits. Cancer Epidemiol. Biomarkers Prev. 29, 942–948. doi: 10.1158/1055-9965.EPI-19-1277
Rimer, B. K., and Kreuter, M. W. (2006). Advancing tailored health communication: a persuasion and message effects perspective. J. Commun. 56, S184–S201. doi: 10.1111/j.1460-2466.2006.00289.x
Rocque, G., Miller-Sonnet, E., Balch, A., Stricker, C., Seidman, J., Stiles, S., et al. (2019). Engaging multidisciplinary stakeholders to drive shared decision-making in oncology. J. Palliat. Care 34, 29–31. doi: 10.1177/0825859718810723
Rood, J. A. J., Nauta, I. H., Witte, B. I., Stam, F., van Zuuren, F. J., Manenschijn, A., et al. (2017). Shared decision-making and providing information among newly diagnosed patients with hematological malignancies and their informal caregivers: not “one-size-fits-all”. Psychooncology 26, 2040–2047. doi: 10.1002/pon.4414
Ryan, M., Watson, V., and Entwistle, V. (2009). Rationalising the “irrational”: a think aloud study of discrete choice experiment responses. Health Econ. 18, 321–336. doi: 10.1002/hec.1369
Sansoni, J. E., Grootemaat, P., and Duncan, C. (2015). Question prompt lists in health consultations: a review. Patient Educ. Couns. 3:15. doi: 10.1016/j.pec.2015.05.015
Sekeres, M. A., Guyatt, G., Abel, G., Alibhai, S., Altman, J. K., Buckstein, R., et al. (2020). American Society of Hematology 2020 guidelines for treating newly diagnosed acute myeloid leukemia in older adults. Blood Adv. 4, 3528–3549. doi: 10.1182/bloodadvances.2020001920
Smith, M. Y., Hammad, T. A., Metcalf, M., Levitan, B., Noel, R., Wolka, A. M., et al. (2016). Patient engagement at a tipping point-the need for cultural change across patient, sponsor, and regulator stakeholders: insights from the DIA conference, “patient engagement in benefit risk assessment throughout the life cycle of medical products”. Ther. Innov. Regul. Sci. 50, 546–553. doi: 10.1177/2168479016662902
Sochacka-Ćwikła, A., Mączyński, M., and Regiec, A. (2021). FDA-approved drugs for hematological malignancies-the last decade review. Cancers (Basel) 14:87. doi: 10.3390/cancers14010087
Sorror, M. L., Storer, B. E., Fathi, A. T., Brunner, A., Gerds, A. T., Sekeres, M. A., et al. (2021). Multisite 11-year experience of less-intensive vs intensive therapies in acute myeloid leukemia. Blood 138, 387–400. doi: 10.1182/blood.2020008812
Swain, J. (2018). A hybrid approach to thematic analysis in qualitative research: Using a practical example. Thousand Oaks, CA: SAGE Publications Ltd.
Terrasson, J., Rault, A., Dolbeault, S., and Brédart, A. (2022). Question prompt lists to improve communication between cancer patients and healthcare professionals. Curr. Opin. Oncol. doi: 10.1097/CCO.0000000000000840
Thorne, S., Oliffe, J. L., and Stajduhar, K. I. (2013). Communicating shared decision-making: cancer patient perspectives. Patient Educ. Couns. 90, 291–296. doi: 10.1016/j.pec.2012.02.018
Wicker, R. F. (2021). Text - S.1597 - 114th Congress (2015–2016): Patient-Focused Impact Assessment Act of 2016 Congress.gov Library of Congress. Available at: https://www.congress.gov/bill/114th-congress/senate-bill/1597/text (Accessed October 21, 2021).
Keywords: values-clarification, patient-centered care, shared decision-making, effective communication, digital health, cancer, tailored health communication
Citation: Cole AC, Kwong E, Mhina C, King AJ, Mazur L and Richardson DR (2024) Perceptions on tailored messages from a values clarification tool: a mixed-methods study of older adults with cancer. Front. Commun. 9:1347310. doi: 10.3389/fcomm.2024.1347310
Edited by:
Sriram Iyengar, University of Arizona, United StatesReviewed by:
Jose Florez Arango, Cornell University, United StatesMary Mays, University of Puerto Rico, Puerto Rico
Copyright © 2024 Cole, Kwong, Mhina, King, Mazur and Richardson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amy C. Cole, YW15X2NvbGVAbWVkLnVuYy5lZHU=
 Amy C. Cole
Amy C. Cole Elizabeth Kwong
Elizabeth Kwong Carl Mhina2
Carl Mhina2 Andy J. King
Andy J. King