
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Commun., 25 January 2023
Sec. Health Communication
Volume 8 - 2023 | https://doi.org/10.3389/fcomm.2023.995538
This article is part of the Research TopicThe Role of Media and Communications in Vaccine Hesitancy during the COVID-19 PandemicView all 4 articles
 Berhaun Fesshaye1*
Berhaun Fesshaye1* Clarice Lee1,2*
Clarice Lee1,2* Alicia M. Paul1,2,3
Alicia M. Paul1,2,3 Eleonor Zavala1
Eleonor Zavala1 Prachi Singh2
Prachi Singh2 Ruth A. Karron1,4
Ruth A. Karron1,4 Rupali J. Limaye1,2,3,5*
Rupali J. Limaye1,2,3,5*COVID-19 vaccine rollout in Kenya has been challenged by both the supply of and demand for vaccines. With a third of the adult population classifying as vaccine hesitant, reaching vaccination targets requires an understanding of how people make decisions regarding vaccines. Globally, pregnant and lactating women have especially low uptake rates, which could be attributed to the “infodemic,” or constant rush of new information, as this group is vulnerable to misinformation and uncertainty. While presentation of COVID-19 vaccines in the media allows for easy access, these sources are also susceptible to misinformation. Negative and unfounded claims surrounding SARS-CoV-2 infection and COVID-19 vaccines contribute to vaccine hesitancy. Given the influence that the media may have on people's attitudes toward vaccines, this study examines the relationship between the media and the vaccine decision-making process among pregnant and lactating women, healthcare workers, community members (male relatives, male neighbors, and gatekeepers), and policymakers in Kenya. Data were collected through in-depth interviews in urban and rural counties in Kenya to understand how media information was utilized and consumed. While healthcare workers were the most frequently cited information source for pregnant and lactating women, other healthcare workers, and community members, findings also show that the media (traditional, social, and Internet) is an important source for obtaining COVID-19 information for these groups. Policymakers obtained their information most frequently from traditional media. Ensuring that information circulating throughout these media channels is accurate and accessible is vital to reduce vaccine hesitancy and ultimately, meet COVID-19 vaccination goals in Kenya.
On March 12, 2020, Kenya confirmed its first COVID-19 case in its capital, Nairobi. As of January, 2023, Kenya has reported more than 342,507 confirmed cases and more than 5,660 deaths (World Health Organization, 2022). The Ministry of Health has implemented several public health interventions to combat the pandemic, including a COVID-19 vaccine program initiated in March 2021 aiming to vaccinate 26 million citizens by the end of 2022 (Kenya Ministry of Health, 2021). As of December 2022, ~10 million adults in Kenya have been fully vaccinated for COVID-19, defined as two doses of AstraZeneca, Pfizer, Moderna or Sinopharm vaccines, or one dose of the Johnson & Johnson vaccine (Kenya Ministry of Health., 2022).
In 2021, COVID-19 vaccine rollout in Kenya was slowed by obstacles in both vaccine supply and demand. On the supply side, Kenya has faced challenges with vaccine procurement, having received approximately one-quarter of their allocated doses for phase one rollout from COVAX in March 2021 (Kenya Ministry of Health, 2021). Additionally, the country has reported challenges with implementing health worker training, communication to support effective vaccine rollout, and capacity-building for COVID-19 vaccine rollout due to inadequate budgets (Kenya Ministry of Health., 2022). On the demand side, vaccine hesitancy threatens vaccine acceptance in Kenya, with estimates of more than a third of the adult population classified as vaccine hesitant, limiting vaccine uptake (Orangi et al., 2021).
Further hindering Kenya's COVID-19 vaccination goals is low vaccine uptake among pregnant and lactating women (Ceulemans et al., 2021; Mohan et al., 2021; Oluklu et al., 2021; Galanis et al., 2022; Schaal et al., 2022; Shamshirsaz et al., 2022). Use of the COVID-19 vaccine in pregnancy and lactation has been recommended by national and global public health authorities (Kenya Ministry of Health, 2021; Kenya Ministry of Health., 2022) based on a combination of post-authorization evidence demonstrating the safety of the vaccine among this population (Shimabukuro et al., 2021; Blakeway et al., 2022) and epidemiological data establishing the association between COVID-19 during pregnancy and increased risks for severe disease and poor birth outcomes (Liu et al., 2020; Karimi et al., 2021; Nachega et al., 2022). Despite the evidence and these recommendations, pregnant women continue to be one of the highest COVID-19 risk groups with the lowest vaccine uptake globally (Galanis et al., 2022; Shamshirsaz et al., 2022). For example, in a systematic review and meta-analysis of 11 studies measuring COVID-19 vaccine uptake among more than 700,000 pregnant women, Galanis et al. (2022) found that the overall proportion of vaccine uptake was 27.5% (95% CI: 18.8–37.0%). Although data are limited in low-income countries, research conducted in Europe and the Middle East suggest similarly low rates of COVID-19 vaccine intent among lactating people (Ceulemans et al., 2021; Mohan et al., 2021; Oluklu et al., 2021; Schaal et al., 2022).
Several factors may influence pregnant and lactating women's decisions to get the COVID-19 vaccine. From a socioecological perspective, factors may range from the individual level (e.g., attitudes toward vaccines, fear of side effects, awareness of vaccine benefits) to the policy level (e.g., eligibility criteria, prioritization of at-risk groups, vaccine procurement and distribution). One key decision-making factor is access to trusted sources of information (Larson Williams et al., 2019; Kilich et al., 2020; Fauzia Malik et al., 2021; Karafillakis et al., 2021). As the pandemic has evolved, new information has emerged, creating an “infodemic,” or constant rush of information, ranging from new vaccine guidelines to vaccine misinformation (Okereke et al., 2020). As a result, many have experienced oversaturation of COVID-19 updates, which has contributed to heightened confusion and frustration among the general public (Mbae, 2020; Lau et al., 2021). Subsequently, many are losing trust in public health decision-makers (Kithiia et al., 2020) and simultaneously experiencing caution fatigue, reducing their willingness to participate in COVID-19 preventative interventions (Mwenje et al., 2021). Pregnant and lactating women are one group that has been particularly affected by the infodemic. Despite being at higher risk for adverse outcomes from COVID-19, they have been disproportionately impacted by misinformation, uncertainty, changing guidance, and lack of data on COVID-19 outcomes and vaccine safety relevant to pregnancy and lactation (Goldbort et al., 2021; Izhar et al., 2021; Zavala et al., 2022). In response to the growing levels of vaccine hesitancy in the country, the Kenya Ministry of Health bolstered its already far-reaching communication campaign, leveraging mainstream media, social media, and community avenues to reduce misinformation regarding COVID-19 vaccines (Adebisi et al., 2021).
This study aims to identify and compare health information sources used by pregnant and lactating women, healthcare workers, community members, and policymakers during the COVID-19 pandemic to explore how these sources influence vaccine decision-making among pregnant and lactating women in Kenya.
We conducted in-depth interviews with audience types that are likely to influence the vaccine decision-making process of pregnant and lactating women. This included pregnant and lactating women, male family members and neighbors of pregnant or lactating women, community gatekeepers (community leaders, faith-based leaders), policymakers and healthcare workers. Participants were recruited from three diverse counties in Kenya: Garissa (rural), Kakamega (rural and urban), and Nairobi (urban). Within each county, we recruited from two communities.
In-depth interview guides were developed using an iterative process, including pre-testing the guides with pregnant women in Kenya. Interview guides were revised prior to data collection based on feedback. We included questions related to vaccine knowledge, attitudes, decision-making, and intentions, including perceptions related to vaccine effectiveness and vaccine safety. To understand how vaccine knowledge, attitudes, and intentions were informed, we also asked where participants obtain health information, both generally and about vaccines specifically, and which sources they trust to inform their health decisions. Prior to data collection, data collectors participated in a 3-day training exercise, after completing an online human subjects ethics training. Participants were recruited at various health clinics across the six communities, had to be at least 18 years of age, and had to be able to give consent. If a participant met the inclusion criteria and agreed to participate, oral consent was obtained. Interviews were conducted in either English, Swahili, or other local languages as necessary in a semi-private setting or via Zoom and were audio recorded. Members of the study team transcribed and translated the transcripts into English. Members fluent in local languages and English validated a subset of transcriptions. We strived to obtain adequate sample sizes for each participant category. We reached saturation across all participant types and continued to sample for further insights.
Using a grounded theory approach, seven researchers analyzed the data. Three rounds of open coding occurred to develop, refine, and finalize the code list. Team members then coded 24 transcripts and subsequently discussed emerging themes. The remaining transcripts were coded, and two members of the team conducted inter-rater reliability with ~10% of the transcripts that neither of them had coded previously. Reliability was >90%. Themes and sub-themes were then identified and discussed. Data were managed using Atlas.ti. This study received ethical approval from Johns Hopkins Bloomberg School of Public Health and Kenya Medical Research Institute.
Data were obtained through open ended questions about where participants sought information about general health, COVID-19, and non-COVID-19 vaccines. Within the information sources, codes for traditional media, social media, and the Internet emerged. Quotes were coded as “Internet” if respondents referenced general search engines such as Google, and social media was coded for platforms such as Facebook and Twitter. Each mention of a source was counted individually, allowing for multiple mentions of cited sources in a single interview. Information sources were grouped into the following categories: media (traditional, social, and Internet) health providers, community members, public health agencies, community leaders, sensitization, scientific sources, and no source. Content received from these sources was categorized as follows: general health, COVID-19 vaccine, non-pharmaceutical COVID-19 prevention, COVID-19 (general), and any vaccine.
A total of 94 individuals were interviewed, including 29 pregnant or lactating women, 20 healthcare workers, 35 community members (male relatives or neighbors of pregnant or lactating women and gatekeepers), and 10 policymakers, from August to September 2021.
Overall, healthcare workers were identified as the most common vaccine information source among healthcare workers, pregnant and lactating women, and community members (male relatives, male neighbors, and gatekeepers) in our sample. In comparison, policymakers obtained information most frequently from traditional media. Although we collected data on other sources of information outside of the media, the following results specifically report on sources of information within the media (traditional, social media, and the Internet), from which all participant groups sought health information, including the COVID-19 vaccine (Figure 1; Table 1). Regarding content, most information sought was related to COVID-19 vaccines, followed by any vaccine, COVID-19, general health, and COVID-19 prevention (Figure 2).
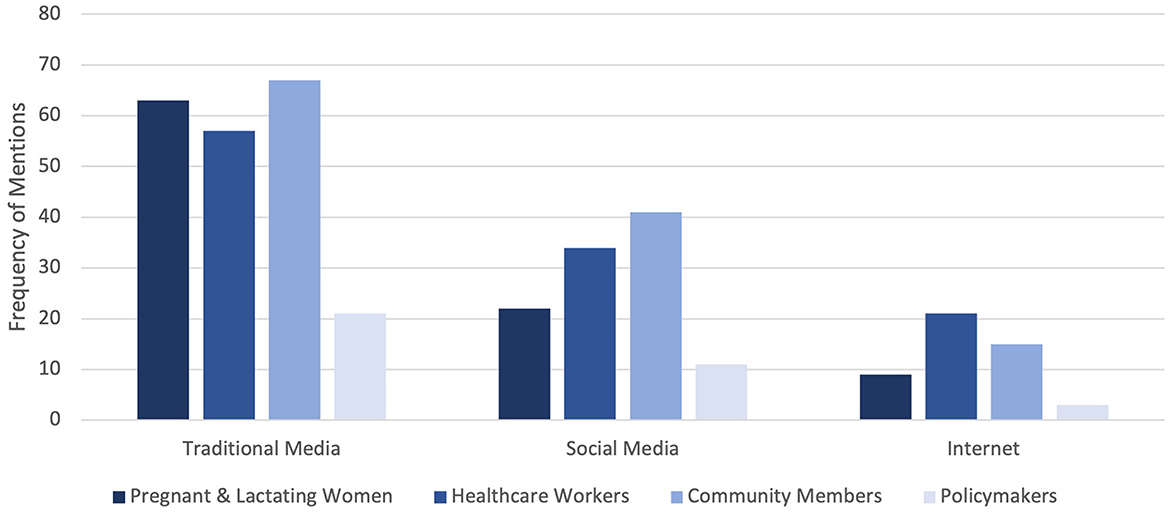
Figure 1. Health information sources in media by audience type. Frequency of mentions for media types (traditional, social, and Internet) among each participant group.

Table 1. Ranking of media-based information sources (traditional media includes TV, radio, newspaper, etc; social media includes Twitter, Facebook, Youtube, etc; and Internet includes Google, etc.) among participants groups.
Traditional media was one of the top information sources for pregnant and lactating women, followed by social media and the Internet more broadly. Across the 31 interviews with pregnant and lactating women, traditional media was mentioned 63 times, while social media and the Internet were cited 22 and 9 times, respectively.
Pregnant and lactating women most often obtained information about COVID-19, including COVID-19 vaccines, from both traditional and social media. As this pregnant woman in Nairobi stated: “I heard about [the vaccine] from the television and just recently they announced in the church that there is a vaccine and people need to go get it.” Some pregnant and lactating women reported getting more specific information regarding vaccine eligibility and prioritization via traditional media. This pregnant woman in rural Kakamega said she “heard about [the vaccine] over the radio, on TV” and “that [the vaccine] is in Kakamega when they had selected groups to go for it, they were specific about it, and then from there that is when it spread out to the sub-county hospital where anybody could go for it.” Related to social media, Facebook and WhatsApp were the platforms most often cited by this group. When asked if she gets information from social media, a pregnant woman in Garissa answered “Yeah, because most of the people when they hear about something they share it. So, you get to hear it from the media like that.” The types of information pregnant and lactating women obtained from the Internet were related to COVID-19, general health, and vaccines. A pregnant woman in rural Kakamega stated “personally, I mostly use Google” to get health information “because, you know, you might be having a problem that is very private, and as I go to ask somebody, the person will again move with that information, especially the health workers, they have that tendency.” Pregnant and lactating women described how the media also played a role in their vaccine decision-making, as highlighted by this lactating mother from rural Kakamega, who mentioned that before deciding to get a COVID-19 vaccine, she “[would go] to Google” and “read more about it to make decisions.”
The media similarly played a key role for healthcare workers. Across the 20 interviews conducted with healthcare workers, traditional media was mentioned 45 times, while social media and the Internet were mentioned 24 and 12 times, respectively.
A healthcare worker from Nairobi discussed how traditional media was their source for new information about the COVID-19 vaccine, “It [information] came from the government through the news, I was reading magazines for a while and read that there was a breakthrough that there is a COVID vaccine.” For many healthcare workers, social media was an important source, with the Internet being cited less frequently. Social media was used to obtain information from trusted public health sources as a healthcare worker from Nairobi described, “The most common platform I use is Twitter, that is where I get most of my information. [On Twitter] WHO, we also have Dr. Anthony Fauci's Twitter handle. Those are the common ones I use.” Perceptions of information obtained from social media sources varied, with one Nairobi-based healthcare worker stating “There is also social media which has informed us about the [COVID-19] vaccine. Some are good that give you hope, but some are so scary.” Another Nairobi healthcare worker went into more detail about the negative influence of social media by saying, “At first [the community] never took [the COVID-19 vaccine] positively, they were so negative about it because obviously of what they were hearing in the social media platforms, because you hear people died when they got the vaccine, somebody reacted so badly.”
A healthcare worker from rural Kakamega captured the “infodemic” for vaccine information: “We have the media; we have the magazines, the gazettes, the newspapers that is…and also with the Internet we have a lot of information flying around.” Another healthcare worker from urban Kakamega expressed hesitancy to receive information from the Internet, “For COVID, I don't think that I will rely on the Internet, I think that for COVID it is a bit different, I will try to engage my colleagues of which if something is also not clear, we can seek clarification from a higher authority because there is protocol.” A healthcare worker from Garissa noted the Internet as a source of verifying information received from other media types when making decisions about vaccine acceptance, “We first receive from the television and then you Google to get more verified information.”
Similar to pregnant and lactating women, community members, including male family members and neighbors of pregnant and lactating women as well as gatekeepers, also obtained COVID-19 information primarily from traditional media compared to social media and the Internet. Among community members, across the 33 interviews conducted, traditional media was mentioned 67 times, while social media 41 times and the Internet 15 times. Many community members heard about COVID-19 vaccines through the radio, TV, or the newspaper. As one community member in Nairobi put it, “COVID-19 information is everywhere in radios, newspapers, and media.” A male family member also pointed out that they were broadcasting COVID-19 vaccine administrations on TV, stating that he “saw it on TV that doctors were coming to Jacaranda grounds to administer the corona vaccine.” Information on COVID-19 prevention was also obtained from social media platforms. Another community member in rural Kakamega stated “there are many [social media platforms] when you read there you get to know about the healthcare workers and how you can prevent the disease or whatever has happened.” Social media also helped community members access information from global organizations, like UNICEF. One gatekeeper from Nairobi explained how “if you use Facebook, you find things on the UNICEF page, there you get many things about COVID-19.” Another gatekeeper from Garissa even expressed gratitude for the information available on social media. “We get a lot of information on social media. I am grateful for these platforms. They provide this information repeatedly… This information is available day and night on TV … how to prevent COVID-19 and where to get the vaccinations.” However, some individuals acknowledged that while information is readily available on social media, it may not always be factual. For example, this community member in rural Kakamega stated that they got information on Facebook and WhatsApp but that “mostly what is there is 50/50. 50% is true, 50% is [myths].” A family member in Nairobi echoed this concern saying, “you can get [information from Facebook] but it is not authenticated, you won't know if that is the right information.”
The media also played a central role for policymakers. Among the 10 interviews conducted with policymakers, traditional media was the most cited source, with 21 mentions, followed by social media and Internet with 11 and 3 mentions, respectively. The role of the media on vaccine decision-making was outlined by a Garissa policymaker who stated, “Media plays a role in awareness and focus on attitude change toward any vaccines.” Other policymakers discussed that the media could have both positive and negative influences on vaccine acceptance depending on the information. As one policymaker from Nairobi described “Well the media, if they report negatively, like maybe they report vaccines in a negative light on adverse events or such, it could actually lead to a decrease in vaccine uptake and of course if they are able to report positively about a vaccine and about its benefit, that could lead to an increased uptake.”
Policymakers asserted that social media is considered an easy way to exchange and gain information, especially for those that may not have access to scientific sources. A policymaker from Nairobi noted “[social media] does play a role; the social media plays a very big role because it goes viral very quickly…that's why I am saying the media can play a negative or positive role.” Another policymaker from urban Kakamega noted: “You don't have to have a textbook, you just need a smartphone, and it has made [gaining knowledge about vaccines] easier. Google is your friend.” A Nairobi-based policymaker discussed the importance of accurate information on social media platforms and the Internet generally: “Somebody should be looking at what Dr. Google is telling people—having the correct information on general media and social media to give [people] correct information.” The importance of the media in shaping attitudes and beliefs is described by a policymaker from Nairobi who stated, “If the media says something is bad, people tend to listen to the media.”
Maternal immunization is a powerful public health strategy that can reduce global neonatal, infant, and maternal morbidity and mortality (Larson Williams et al., 2019). The benefits of maternal immunization can only be harnessed if pregnant women and new mothers are willing and able to accept recommended vaccines. The purpose of this research was to gain insight into the influence of the media as a source of COVID-19 information, especially COVID-19 vaccines, in Kenya. While all media types were identified as important sources, traditional media was cited most frequently. Pregnant and lactating women, healthcare workers, community members, and policymakers referenced the use of different media types for various COVID-19 information, including vaccines.
Over the course of the COVID-19 pandemic, pregnant and lactating women, especially in African countries, have exhibited lower levels of COVID-19 vaccine acceptance (Shamshirsaz et al., 2022). These persistent high levels of hesitancy are concerning given pregnant women are more vulnerable to the known risks of COVID-19 infection (Galanis et al., 2022). While vaccine hesitancy is not a new issue, it has been pervasive throughout the COVID-19 pandemic due, in part, to the inundation of information with large amounts of misinformation and unfounded claims (Mheidly and Fares, 2020). Labeled the “infodemic,” this constant onslaught of misleading information has contributed to vaccine hesitancy, particularly in vulnerable groups such as pregnant women in African countries (Garett and Young, 2021; Ennab et al., 2022).
Understanding knowledge, attitudes, and beliefs about vaccines is vital to addressing vaccine hesitancy in the pregnant and lactating population (Larson Williams et al., 2019). In addition to healthcare worker recommendations, which have been shown to influence vaccine uptake in previous literature, mainstream media has also been identified as a central source of information for vaccine hesitant individuals (Getman et al., 2018; Kilich et al., 2020). With the widespread global use of smartphones, access to different media channels allows for more convenient access to health information that may influence vaccine decision-making (Machingaidze and Wiysonge, 2021). The media, though, can also act as a catalyst for the spread of misinformation and mistrust related to vaccination and has proven to be a central factor in settings with high levels of vaccine hesitancy (Zhou et al., 2022). The media acts as a link between government entities, health institutions, and the public (Mheidly and Fares, 2020). People look to media sources for reputable information and utilize it to shape their own attitudes and behaviors (Mheidly and Fares, 2020). Therefore, correctly harnessing the power of media on vaccine decision-making is crucial in improving uptake.
Previous research has also highlighted the importance of the media in Kenya, showing healthcare workers and media as the top trusted sources for government and faith-based organizations (Shah et al., 2022). The information received from media sources consisted mainly of COVID-19 vaccine availability and eligibility. Given that many participants did not receive their information solely from one media channel, but rather through multiple channels, focusing on ensuring accurate information is circulated through all media types may promote positive vaccine attitudes. This could be implemented by the combined effort of government bodies and public health agencies working with the media to reduce the presence of misinformation on platforms, and to ensure that accurate and reliable information is always available (Garett and Young, 2021; Ennab et al., 2022). Increased presence and engagement of public health professionals and policymakers throughout media, especially social media, may assist in reducing misinformation (Garett and Young, 2021; Zhou et al., 2022).
Since the media is a central information source for COVID-19 vaccines, ensuring that positive and truthful messages are presented is paramount. Positive COVID-19 media coverage has been shown to increase vaccine acceptance, while negative coverage can lead to decreased acceptance (Zhou et al., 2022). Digital social networks such as social media permit rapid spread of information (Garett and Young, 2021). Access to trusted information sources is an important decision-making factor; therefore, ensuring that reliable information is easily accessible may influence vaccine decision making (Larson Williams et al., 2019; Kilich et al., 2020; Fauzia Malik et al., 2021; Karafillakis et al., 2021). Increasing access will, once again, likely come from the collaboration between authoritative governmental bodies and media companies (Garett and Young, 2021, Ennab et al., 2022; Zhou et al., 2022). Kenya has been working toward reducing misinformation on social media platforms with investments in fact-checking organizations that locate and mitigate circulating false information (Tully, 2022). However, social media sites are owned and operated by private companies, ultimately leaving it up to those companies to decide what is and is not permitted (Gallo and Cho, 2021). Additionally, non-English African languages are susceptible to the challenge of lacking relevant data to inform natural language processing applications that are used for the detection of misinformation (Gereme et al., 2021).
The potential influence of other individuals on vaccine uptake of pregnant and lactating women should also be considered when understanding how vaccine attitudes and beliefs are shaped. Male family members, community gatekeepers, policymakers, and healthcare workers were all identified as key stakeholders in the vaccine decision-making process of pregnant and lactating women. Ensuring that these groups are also receiving accurate information from trusted sources, especially the media, should be of interest. Healthcare professionals are of particular interest as one of the most crucial influences for vaccine uptake, especially among pregnant and lactating women (Kilich et al., 2020). Moreover, encouraging healthcare worker engagement in the media could act as the bridge between these two central information sources.
The importance of the media cannot be ignored while addressing COVID-19 vaccine hesitancy. The key to addressing vaccine hesitancy in vulnerable groups, such as pregnant and lactating women, may lie in ensuring that the information they consume is accurate and timely. Key stakeholders in Kenya recognized and discussed the importance of the media in the formation of vaccine attitudes and acceptance. However, misinformation has spread widely through the media. Therefore, ensuring that media channels share up-to-date and accurate information is crucial, along with developing effective communication strategies, to increase vaccine confidence in vulnerable groups and the population overall. The findings from our study will inform the development of such communication strategies to improve trust in media sources and vaccine uptake.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Johns Hopkins Bloomberg School of Public Health (no. 14893; approved 9 July 2021) and Scientific and Ethics Review Unit of the Kenya Medical Research Institute (no. 4211; approved 24 May 2021). The patients/participants provided their written informed consent to participate in this study.
Conceptualization: BF, CL, AP, PS, and RL. Methodology: RL. Validation: AP and RL. Formal analysis: BF, CL, AP, and EZ. Writing—original draft preparation: BF, CL, AP, EZ, PS, and RL. Writing—review and editing: BF, PS, RK, EZ, and RL. Supervision and funding acquisition: RK and RL. All authors have read and agreed to the published version of the manuscript.
This research was funded by the Bill and Melinda Gates Foundation, grant number INV-016977.
We thank Garissa, Kakamega, and Nairobi Counties and their participating health facilities for their collaboration. We also thank Jhpiego Headquarters and their team in Kenya for their partnership and role in conducting this research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2023.995538/full#supplementary-material
Adebisi, Y. A., Rabe, A., and Lucero-Prisno Iii, D. E. (2021). Risk communication and community engagement strategies for COVID-19 in 13 African countries. Health Promot. Perspect. 11, 137–147. doi: 10.34172/hpp.2021.18
Blakeway, H., Prasad, S., Kalafat, E., Heath, P. T., Ladhani, S. N., Le Doare, K., et al. (2022). COVID-19 vaccination during pregnancy: coverage and safety. Am. J. Obstet. Gynecol. 226, 236.e1–236.e14. doi: 10.1016/j.ajog.2021.08.007
Ceulemans, M., Foulon, V., Panchaud, A., Winterfeld, U., Pomar, L., Lambelet, V., et al. (2021). Vaccine Willingness and Impact of the COVID-19 pandemic on women's perinatal experiences and practices: a multinational, cross-sectional study covering the first wave of the pandemic. Int. J. Environ. Res. Public Health 18, 367. doi: 10.3390/ijerph18073367
Ennab, F., Babar, M. S., Khan, A. R., Mittal, R. J., Nawaz, F. A., Essar, M. Y., et al. (2022). Implications of social media misinformation on COVID-19 vaccine confidence among pregnant women in Africa. Clin. Epidemiol. Global Health 14, 100981. doi: 10.1016/j.cegh.2022.100981
Fauzia Malik, A., Belizan, M., Gutierrez, M., Vilajeliu, A., Sanclemente, L. N., Gonzalez Casanova, I., et al. (2021). Pregnant women's perspectives about maternal immunization in Latin America. Vaccine 39, B44–B49. doi: 10.1016/j.vaccine.2020.09.009
Galanis, P., Vraka, I., Siskou, O., Konstantakopoulou, O., Katsiroumpa, A., and Kaitelidou, D. (2022). Uptake of COVID-19 vaccines among pregnant women: a systematic review and meta-analysis. Vaccines 10, 766. doi: 10.3390/vaccines10050766
Gallo, J. A., and Cho, C. Y. (2021). Social Media: Misinformation and Content Moderation Issues for Congress. Washington D.C.: Congressional Research Service.
Garett, R., and Young, S. D. (2021). Online misinformation and vaccine hesitancy. Transl. Behav. Med. 11, 2194–2199. doi: 10.1093/tbm/ibab128
Gereme, F., Zhu, W., Ayall, T., and Alemu, D. (2021). Combating fake news in “low-resource” languages: Amharic fake news detection accompanied by resource crafting. Information 12, 20. doi: 10.3390/info12010020
Getman, R., Helmi, M., Roberts, H., Yansane, A., Cutler, D., and Seymour, B. (2018). Vaccine hesitancy and online information: the influence of digital networks. Health Educ. Behav. 45, 599–606. doi: 10.1177/1090198117739673
Goldbort, J., Zhuang, J., Bogdan-Lovis, E., Bresnahan, M., and Frasher, B. (2021). Navigating uncertain times: information management about pregnancy and breastfeeding during the COVID-19 pandemic. J. Health Commun. 26, 473–479. doi: 10.1080/10810730.2021.1954731
Izhar, R., Husain, S., Tahir, M. A., Husain, S., and Hussain, S. (2021). Pregnant during the COVID-19 pandemic: knowledge, concerns, attitudes and practices of Pakistani women. Eur. J. Midwifery 5, 54. doi: 10.18332/ejm/142818
Karafillakis, E., Francis, M. R., Paterson, P., and Larson, H. J. (2021). Trust, emotions and risks: pregnant women's perceptions, confidence and decision-making practices around maternal vaccination in France. Vaccine 39, 4117–4125. doi: 10.1016/j.vaccine.2021.05.096
Karimi, L., Makvandi, S., Vahedian-Azimi, A., Sathyapalan, T., and Sahebkar, A. (2021). Effect of COVID-19 on mortality of pregnant and postpartum women: a systematic review and meta-analysis. J. Pregn. 2021, 8870129. doi: 10.1155/2021/8870129
Kenya Ministry of Health (2021). National COVID-19 Vaccine Deployment Plan, 2021. Nairobi: Kenya Ministry of Health.
Kenya Ministry of Health. (2022). Kenya COVID-19 Vaccination Program- Daily Situation Report. Nairobi: Kenya Ministry of Health. Available online at: https://www.health.go.ke/#1621663315215-d6245403-4901 (accessed July 10, 2022).
Kilich, E., Dada, S., Francis, M. R., Tazare, J., Chico, R. M., Paterson, P., et al. (2020). Factors that influence vaccination decision-making among pregnant women: a systematic review and meta-analysis. PLoS ONE 15, e0234827. doi: 10.1371/journal.pone.0234827
Kithiia, J., Wanyonyi, I., Maina, J., Jefwa, T., and Gamoyo, M. (2020). The socio-economic impacts of COVID-19 restrictions: data from the coastal city of Mombasa, Kenya. Data Brief 33, 106317. doi: 10.1016/j.dib.2020.106317
Larson Williams, A., Mitrovich, R., Mwananyanda, L., and Gill, C. (2019). Maternal vaccine knowledge in low- and middle-income countries-and why it matters. Hum. Vacc. Immunother. 15, 283–286. doi: 10.1080/21645515.2018.1526589
Lau, J., Sutcliffe, S., Barnes, M., Mbaru, E., Muly, I., Muthiga, N., et al. (2021). COVID-19 impacts on coastal communities in Kenya. Mar. Policy 134, 104803. doi: 10.1016/j.marpol.2021.104803
Liu, W., Zhou, P., Chen, K., Ye, Z., Liu, F., Li, X., et al. (2020). Efficacy and safety of antiviral treatment for COVID-19 from evidence in studies of SARS-CoV-2 and other acute viral infections: a systematic review and meta-analysis. CMAJ 192, E734–E744. doi: 10.1503/cmaj.200647
Machingaidze, S., and Wiysonge, C. S. (2021). Understanding COVID-19 vaccine hesitancy. Nat. Med. 27, 1338–1339. doi: 10.1038/s41591-021-01459-7
Mheidly, N., and Fares, J. (2020). Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J. Public Health Policy 41, 410–420. doi: 10.1057/s41271-020-00247-w
Mohan, S., Reagu, S., Lindow, S., and Alabdulla, M. (2021). COVID-19 vaccine hesitancy in perinatal women: a cross sectional survey. J. Perinat. Med. 49, 678–685. doi: 10.1515/jpm-2021-0069
Mwenje, M., Githui, P., Kamunyu, R., Wanjau-Maseno, M., and University, C. (2021). Prevalence of caution fatigue in relation to adherence to COVID-19 pandemic safety guidelines in Kenya. Int. J. Sci. Res. 10, 1–10. doi: 10.21275/SR211006132641
Nachega, J. B., Sam-Agudu, N. A., Machekano, R. N., Rosenthal, P. J., Schell, S., de Waard, L., et al. (2022). Severe acute respiratory syndrome coronavirus 2 infection and pregnancy in sub-Saharan Africa: a 6-country retrospective cohort analysis. Clin. Infect. Dis. 75, 1950–1961. doi: 10.1093/cid/ciac294
Okereke, M., Ukor, N. A., Ngaruiya, L. M., Mwansa, C., Alhaj, S. M., Ogunkola, I. O., et al. (2020). COVID-19 misinformation and infodemic in rural Africa. Am. J. Trop. Med. Hyg. 104, 453. doi: 10.4269/ajtmh.20-1488
Oluklu, D., Goncu Ayhan, S., Menekse Beser, D., Uyan Hendem, D., Ozden Tokalioglu, E., Turgut, E., et al. (2021). Factors affecting the acceptability of COVID-19 vaccine in the postpartum period. Hum. Vaccin. Immunother. 17, 4043–4047. doi: 10.1080/21645515.2021.1972710
Orangi, S., Pinchoff, J., Mwanga, D., Abuya, T., Hamaluba, M., Warimwe, G., et al. (2021). Assessing the level and determinants of COVID-19 vaccine confidence in Kenya. Vaccines 9, 936. doi: 10.3390/vaccines9080936
Schaal, N. K., Zöllkau, J., Hepp, P., Fehm, T., and Hagenbeck, C. (2022). Pregnant and breastfeeding women's attitudes and fears regarding the COVID-19 vaccination. Arch. Gynecol. Obstet. 306, 365–372. doi: 10.1007/s00404-021-06297-z
Shah, J., Abeid, A., Sharma, K., Manji, S., Nambafu, J., Korom, R., et al. (2022). Perceptions and Knowledge towards COVID-19 Vaccine Hesitancy among a Subpopulation of Adults in Kenya: an English Survey at Six Healthcare Facilities. Vaccines 10, 705. doi: 10.3390/vaccines10050705
Shamshirsaz, A. A., Hessami, K., Morain, S., Afshar, Y., Nassr, A. A., Arian, S. E., et al. (2022). Intention to receive COVID-19 vaccine during pregnancy: a systematic review and meta-analysis. Am. J. Perinatol. 39, 492–500. doi: 10.1055/a-1674-6120
Shimabukuro, T. T., Kim, S. Y., Myers, T. R., Moro, P. L., Oduyebo, T., Panagiotakopoulos, L., et al. (2021). Preliminary findings of mRNA Covid-19 vaccine safety in pregnant persons. N. Engl. J. Med. 384, 2273–2282. doi: 10.1056/NEJMoa2104983
Tully, M. (2022). “Responses to misinformation: examining the Kenyan context,” in Disinformation in the Global South, eds H. Wasserman, and D. Madrid-Morales (Amsterdam: Wiley), 179–192. doi: 10.1002/9781119714491.ch12
World Health Organization (2022). Kenya: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Geneva: World Health Organization. Available online at: https://covid19.who.int/region/afro/country/ke (accessed December 5, 2022).
Zavala, E., Krubiner, C. B., Jaffe, E. F., Nicklin, A., Gur-Arie, R., Wonodi, C., et al. (2022). Global disparities in public health guidance for the use of COVID-19 vaccines in pregnancy. BMJ Glob Health 7, 7730. doi: 10.1136/bmjgh-2021-007730
Keywords: COVID-19, media, vaccine hesitancy, maternal health, qualitative, Kenya
Citation: Fesshaye B, Lee C, Paul AM, Zavala E, Singh P, Karron RA and Limaye RJ (2023) A qualitative inquiry in understanding trusted media sources to reduce vaccine hesitancy among Kenyans. Front. Commun. 8:995538. doi: 10.3389/fcomm.2023.995538
Received: 16 July 2022; Accepted: 09 January 2023;
Published: 25 January 2023.
Edited by:
Ruobing Li, Stony Brook University, United StatesReviewed by:
Douglas Ashwell, Massey University Business School, New ZealandCopyright © 2023 Fesshaye, Lee, Paul, Zavala, Singh, Karron and Limaye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Berhaun Fesshaye,  YmZlc3NoYTFAamh1LmVkdQ==; Clarice Lee,
YmZlc3NoYTFAamh1LmVkdQ==; Clarice Lee,  Y2xhcmljZWxlZUBqaHUuZWR1; Rupali J. Limaye,
Y2xhcmljZWxlZUBqaHUuZWR1; Rupali J. Limaye,  cmxpbWF5ZUBqaHUuZWR1
cmxpbWF5ZUBqaHUuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.