- Department of Psychiatry, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
Introduction: Breastfeeding is a natural and universal practice across countries and cultures. It is estimated that several thousand lives could be saved per year if optimal breastfeeding practices were adopted across countries. In addition, breastfeeding has numerous health, emotional and developmental benefits for both the mother and her infant. Despite widespread awareness of these benefits, rates of breastfeeding initiation and maintenance remain suboptimal, both in high- and in low- and middle-income countries. Unfavorable breastfeeding outcomes are related to several factors, including variations in cultural values and the occurrence of common mental disorders in women during pregnancy and in the postnatal period. However, the relative contributions of culture and mental health to variations in national breastfeeding rates have not been examined to date.
Methods: In the current study, recent United Nations International Children's Emergency Fund (UNICEF) data on lifetime breastfeeding rates is analyzed in two stages, to first explore and then confirm the impact of cultural values and maternal mental health status at a cross-national level.
Results: It was found that the estimated prevalence of both depression and anxiety disorders in women of childbearing age was negatively correlated with breastfeeding rates. Significant associations were also observed for the cultural dimensions of individualism-collectivism and masculinity-femininity. The association between anxiety disorders and breastfeeding outcomes remained significant in multivariate analysis incorporating demographic and health variables that could exert a confounding effect.
Discussion: These results suggest that both cultural values and the assessment and treatment of maternal mental illness should be components of any programme aimed at communicating the benefits of breastfeeding or at improving breastfeeding outcomes. The inclusion of these components could help promote the values of cultural sensitivity, inclusiveness and equity in breastfeeding from a global perspective.
Introduction
Breastfeeding is a universally practiced and natural form of infant nutrition that is normative in most countries and cultures. There is extensive evidence from the scientific literature that breastfeeding confers numerous medical and psychological benefits on the developing infant and toddler, and that these benefits may extend even to later childhood or adulthood (Kramer and Kakuma, 2012; Bar et al., 2016; Aryeetey and Dykes, 2018). Moreover, the benefits of breastfeeding are not confined to the child; there are substantial short- and long-term beneficial effects of breastfeeding on maternal physical and mental health (Del Ciampo and Del Ciampo, 2018). It is estimated that if optimal breastfeeding practices could be ensured at a global level, this would lead to a decrease in 200,000–800,000 infant and child deaths per year (North et al., 2022). This has led to large-scale attempts to promote breastfeeding and to increase awareness of its benefits, such as the Baby-Friendly Hospital Initiative (BFHI), a joint initiative of the World Health Organization (WHO) and United Nations International Children's Emergency Fund (UNICEF) (Gomez-Pomer and Blubaugh, 2018). Despite such initiatives at both the national and international levels, the available data suggests that both the initiation and the maintenance of breastfeeding are suboptimal, even in developed countries: for example, it is estimated that exclusive breastfeeding in the first 6 months of life is practiced in only 33% of children at a global level (Philipp and Radford, 2006; Ip et al., 2007; Amoo et al., 2022).
The existence of this significant gap between ideal standards and real-world practices has led to the development and testing of several interventions aimed at promoting the initiation and maintenance of breastfeeding, particularly in the first 6 months after birth (Beake et al., 2012; Gómez et al., 2021). However, the evidence for the efficacy of these programmes has been mixed. A review of research from low- and middle-income countries suggested that structured interventions aimed at improving exclusive breastfeeding were generally effective (Olufunlayo et al., 2019); on the other hand, reviews of interventional studies in developed countries found that less than half of these interventions had a significant impact on breastfeeding outcomes (Skouteris et al., 2014, 2017).
One of the important reasons for the variable success of these interventions is the confounding effect of psychological and social factors. As noted by Kumar et al. (2015), the inability to understand health-related behaviors in the context of local family and community practices has limited the efficacy of interventions aimed at improving maternal and child health, despite their basis in scientific evidence. Moreover, many mothers experience significant mental health problems, both pre- and post-natally, and these factors may act as a significant barrier to successful breastfeeding (Bascom and Napolitano, 2016; Hoff et al., 2019). Breastfeeding is not a mechanical process: it involves a human interaction between a mother and her child (van Wijlen, 2019), and successful breastfeeding depends crucially on both the mother's emotional state and the support and advice provided by those in her immediate social circle (Russell et al., 2022). There is substantial evidence that maternal depression (Butler et al., 2013; Grigoriadis et al., 2013; Hedberg, 2013; Dias and Figueiredo, 2015; Slomian et al., 2019; Dadi et al., 2020; Woldeyohannes et al., 2021; Kim et al., 2022), anxiety (de Jager et al., 2013; Grigoriadis et al., 2013; Fallon et al., 2016a,b; Grigoriadis et al., 2019; Hoff et al., 2019) and post-traumatic stress disorder (Cook et al., 2018; Van Sieleghem et al., 2022) can all reduce the likelihood of both the initiation and the successful maintenance of breastfeeding.
Culture has been defined as “the collective programming of the mind distinguishing the members of one group or category of people from others” (Hofstede et al., 2010). It includes the attitudes, beliefs and practices particular to a given community, which are not genetically predetermined but evolve in a manner contingent on environmental and historical factors. Each culture can be understood as an attempt to solve the problems of human existence, while maintaining the wellbeing the individual and stability of the community as a whole (Hofstede et al., 2010; Moya and Henrich, 2016). There are several methods of describing a nation's culture in terms of more or less orthogonal dimensions (Hsu et al., 2013). Perhaps the most frequently cited and replicated cultural dimension is individualism-collectivism, which reflects the degree to which a given society privileges the rights of the individual as opposed to the rights of the community (Pelham et al., 2022). The influence of culture upon human behavior is pervasive, and it can exert a significant influence on both parenting and feeding practices (LeCuyer and Zhang, 2015; Enriquez and Archila-Godinez, 2022). The difficulties faced in promoting a desirable, health-related behavior at a global level may reflect differences in cultural values (Hopkins et al., 2021). Culture can also influence the relationships between women and their families at various stages of their life cycle. Insecurity in these relationships can lead to psychological distress and reduce the likelihood of successful breastfeeding (Scharfe, 2012), while culturally conditioned supportive relationships lead to positive breastfeeding outcomes (Ni and Lin, 2011). Therefore, exploring the associations between culture, maternal mental health and breastfeeding outcomes may yield valuable information on how these factors could be incorporated into programmes aimed at communicating the benefits of breastfeeding to mothers, and thereby enhancing the initiation and maintenance of breastfeeding in varied cultural settings.
This study is a preliminary investigation of the associations between cultural values, common mental disorders in women of childbearing age, and the likelihood of ever having breastfed at a cross-national level, while correcting for known confounding factors. These confounding factors, which have been highlighted in earlier systematic reviews (Cohen et al., 2018; Santana et al., 2018; Hashemi-Nazari et al., 2020; Normann et al., 2020), include sociodemographic variables (age, urban residence, income and education), maternal factors (age at childbirth, parity, tobacco use and obesity), and relational factors (marital status, mother-infant bonding, and experience of violence in intimate relationships). Some of these factors, such as obesity, interact with psychosocial factors in a complex manner to influence breastfeeding outcomes (Lyons et al., 2018).
Methodology
The current study is an ecological association study, carried out in two stages. In the first stage, a preliminary investigation of the associations between cultural values, the prevalence of common mental disorders, and global breastfeeding statistics was carried out based on Hofstede's model of national cultural values (Hofstede et al., 2010). This analysis included 74 countries, and was exploratory, with no examination of potential confounding factors. In the second stage, an attempt was made to replicate the findings of the initial study in a larger data set of 122 countries, using an independent and more recently calculated measure of cultural individualism-collectivism known as the Global Collectivism Index (Pelham et al., 2022). At this stage, an attempt was made to correct for confounding factors known to influence the initiation and maintenance of breastfeeding.
Data sources
Breastfeeding
The primary source of data on breastfeeding for both stages of the study was UNICEF's 2018 report entitled “Breastfeeding: A Mother's Gift, for Every Child” (UNICEF, 2018). This report provides statistics on the percentage of mothers who have ever breastfed their child, arranged according to four income groups—high, high middle, low middle and low. This publication contains data on a total of 122 countries.
Cultural dimensions
Though various dimensional models of national culture exist, each of them has its own inherent limitations (Hsu et al., 2013). For the purpose of this study, Hofstede's dimensional classification of national cultural values was used as it provides data for a larger number of countries than competing models, and has been associated with several health-related behaviors in prior research (Mansyur et al., 2009; Masood et al., 2019; Matus, 2021). In the first stage of the study, data on national cultural values based on Hofstede's model was obtained via queries from the Hofstede Insights database (Hofstede Insights, 2022). This database provides estimates of national cultural values along six independent dimensions: power distance, individualism-collectivism, masculinity-femininity, uncertainty avoidance, long-term orientation, and indulgence-restraint. Each dimension is assigned a score ranging from 0 to 100. Higher or lower scores indicate that cultural values are closer to one end of a bipolar spectrum. For example, an individualism-collectivism score of 20 indicates high cultural individualism (closeness to the individualism “pole”), while a score of 90 denotes high cultural collectivism (closeness to the collectivism “pole”) (Hofstede Insights, 2022). A description of these six dimensions and their potential influence on breastfeeding is provided in Table 1. Scores on the various dimensions of this model have been significantly associated with other health-related factors at a national level, such as obesity, prescription patterns for specific medications, and interactions between patients and the healthcare system (Borg, 2012; Borisova et al., 2017; Tekeş et al., 2019). The Hofstede Insights database contains data on 115 countries. Breastfeeding data from the UNICEF report was available for 74 of these 115 countries, and these were included in the first-stage analysis.
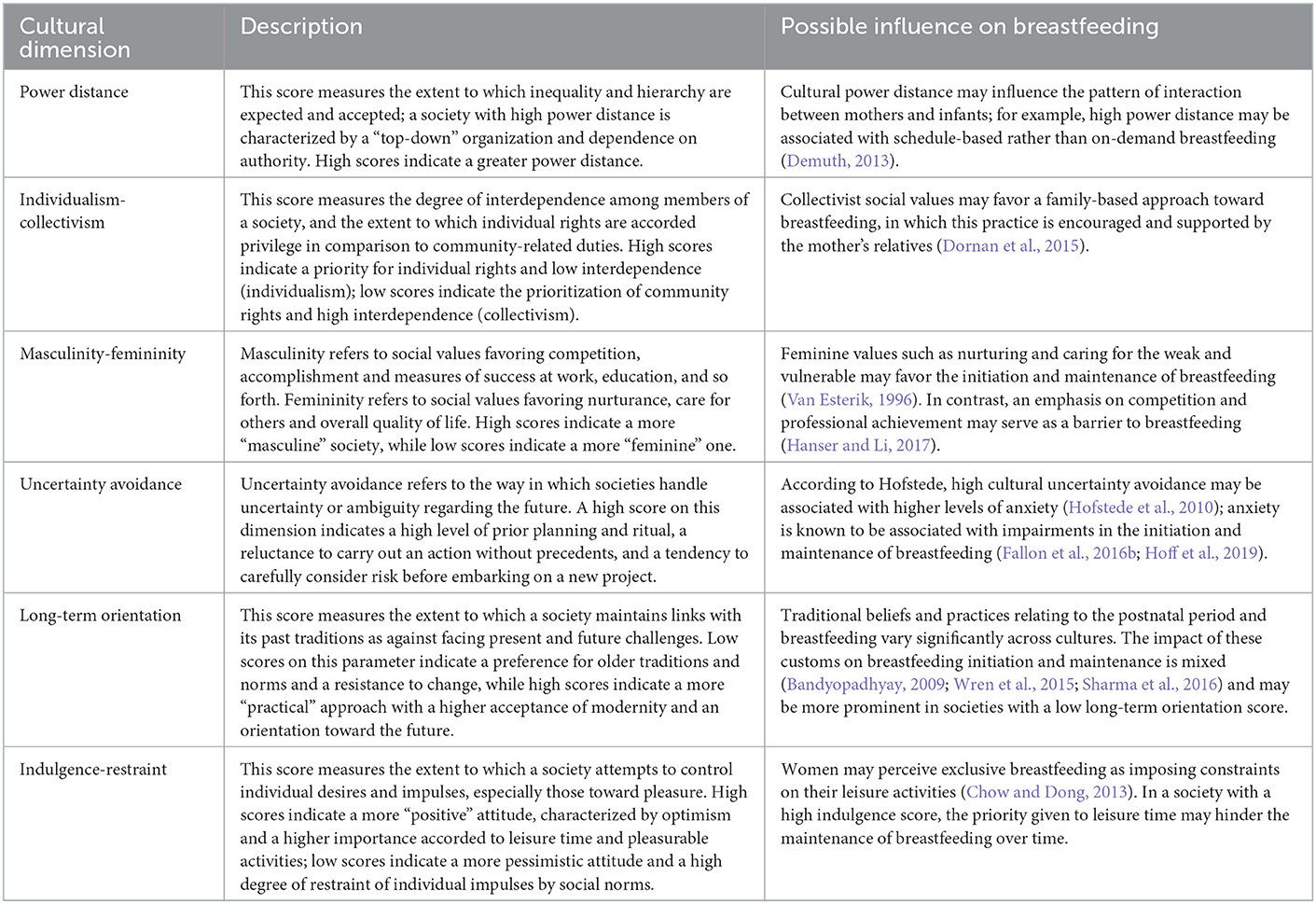
Table 1. Description of Hofstede's cultural value dimensions and their potential relevance to breastfeeding initiation and maintenance.
In the second stage of the study, data on the cultural dimension of individualism-collectivism was obtained from a recent publication on the Global Collectivism Index (GCI). The CGI was developed to address certain limitations with earlier measures of individualism-collectivism, most notably (a) a bias toward data from industrialized, high-income “Western” countries in earlier estimates, (b) a relative underrepresentation of African countries, and (c) cultural changes in certain countries previously considered “collectivistic,” such as China and Japan, which impair the validity of earlier measures (Gerlach and Eriksson, 2021; Pelham et al., 2022). Estimates of the GCI are available for 188 countries. Breastfeeding data from the UNICEF report was available for 122 of these 188 countries, and these were included in the second-stage analysis.
Common mental disorders
Anxiety disorders and depression are commonly referred to as “common mental disorders” because of their high prevalence across populations and cultures (Steel et al., 2014). Both these conditions are often present during pregnancy and in the post-partum period, though they often go undiagnosed (Falana and Carrington, 2019). There is no existing data source on the prevalence of depression or anxiety disorders in pregnant or lactating women at a cross-national level. As an approximation to this variable, the prevalence of these disorders in women of child-bearing age (15–49 years) for the year 2018, based on estimates from the Global Burden of Disease Study, was used as an indirect measure of maternal mental health. This data was retrieved through a query from the Global Burden of Disease Collaborative Network database, which provides estimates of global and national prevalence for all major physical and mental disorders for the period 1990–2019 (Global Burden of Disease Collaborative Network, 2020).
Confounding factors
A number of factors have been found to significantly influence the initiation and maintenance of breastfeeding. For the purposes of this study, confounding factors were selected based on two considerations: (a) replicated evidence of an association between the concerned factor and breastfeeding outcomes, reported in a systematic review or meta-analysis, and (b) availability of a reliable data source for the concerned factor at a cross-national level. Based on examination of relevant systematic reviews and meta-analyses, the following factors satisfied criterion (a): maternal age, marital status, urban residence, maternal education, income, parity, maternal smoking, maternal body mass index, intimate partner violence, and mother-infant bonding (Cohen et al., 2018; Santana et al., 2018; Hashemi-Nazari et al., 2020). While mother-infant bonding cannot be easily quantified at a national level, and no reliable source of cross-national data was found for maternal marital status/single motherhood, information on the other variables was obtained from various sources. These are summarized in Table 2.
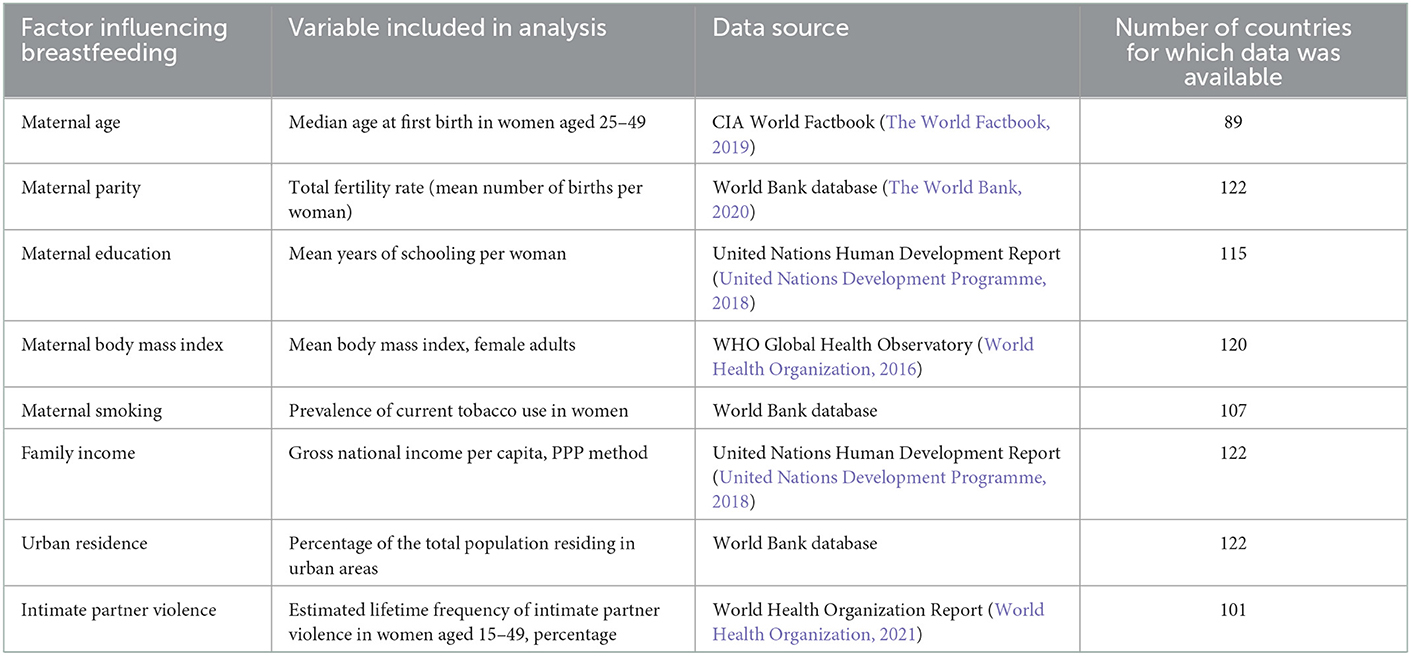
Table 2. Confounding factors influencing breastfeeding initiation and maintenance examined in this study, with their data sources.
Data analysis
In the first, exploratory analysis, all study variables were tested for normality using the Shapiro-Wilk test. As none of the variables conformed to a Gaussian distribution (p < 0.05 for all variables, Shapiro-Wilk test), a cube root transformation was used prior to data analysis. Bivariate (Pearson's r) correlations were used to examine the following associations: (a) correlations between cultural dimensions and breastfeeding, (b) correlations between the prevalence of common mental disorders and breastfeeding, and (c) correlations between cultural dimensions and the prevalence of anxiety and depression. The threshold for significance was set at p < 0.05. In view of the exploratory nature of this analysis, corrections for multiple comparisons were not carried out at this stage. In the event of significant correlations being identified in (c), partial correlation analyses were carried out to examine the relative strength of the associations with cultural dimensions and common mental disorders.
In the second, confirmatory analysis, study variables were tested for normality using the same procedure. As a non-normal distribution was again observed for study variables (p < 0.05 for all variables, Shapiro-Wilk test), a cube root transformation was used prior to data analysis. Bivariate correlations were carried out as described above; in addition, correlations with the confounding factors listed in Table 2 were also examined. As this was a confirmatory analysis, corrections for multiple comparisons were applied at this stage. Following this, a stepwise multivariate linear regression analysis was carried out to identify variables significantly associated with breastfeeding rates. In this analysis, the lifetime breastfeeding rate was the independent variable, and all factors significantly associated with this variable at p < 0.05 or lower in bivariate analyses were included as independent variables. In the event of significant multicollinearity between confounding factors, the factor most significantly associated with the independent variable in bivariate analyses was included in the model.
Results
Exploratory analysis
The first stage of the analysis included data on 74 countries. Reported rates of lifetime breastfeeding by mothers in these countries ranged from a maximum of 99.4% in Sri Lanka to a minimum of 55% in Ireland, with a median of 95.8% and an inter-quartile range (IQR) of 4.4.
Bivariate correlations
A complete correlation matrix is presented in Table 3 and significant findings are illustrated graphically in Figures 1A–C. Lifetime rates of breastfeeding were positively correlated with the cultural dimension of power distance (r = 0.39, p < 0.01) and negatively correlated with the cultural dimensions of individualism-collectivism (r = −0.53, p < 0.01) and masculinity-femininity (r = −0.26, p = 0.028). Breastfeeding rates were negatively correlated with the prevalence of both depression (r = −0.28, p = 0.017) and anxiety disorders (r = −0.40, p < 0.01) in women of childbearing age.
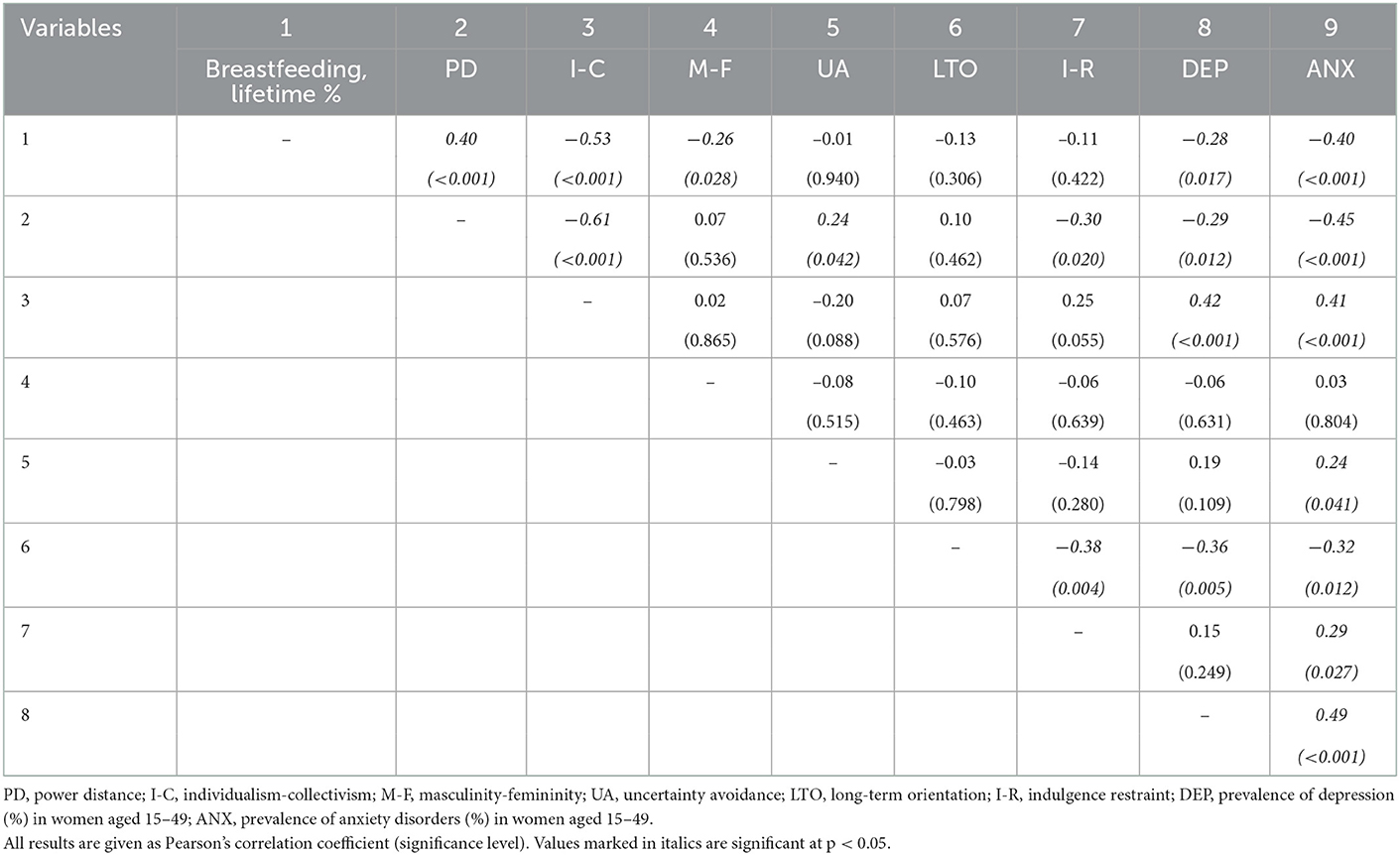
Table 3. Exploratory correlations between national lifetime breastfeeding rates, Hofstede's cultural values, and the prevalence of anxiety and depression in women aged 15–49.
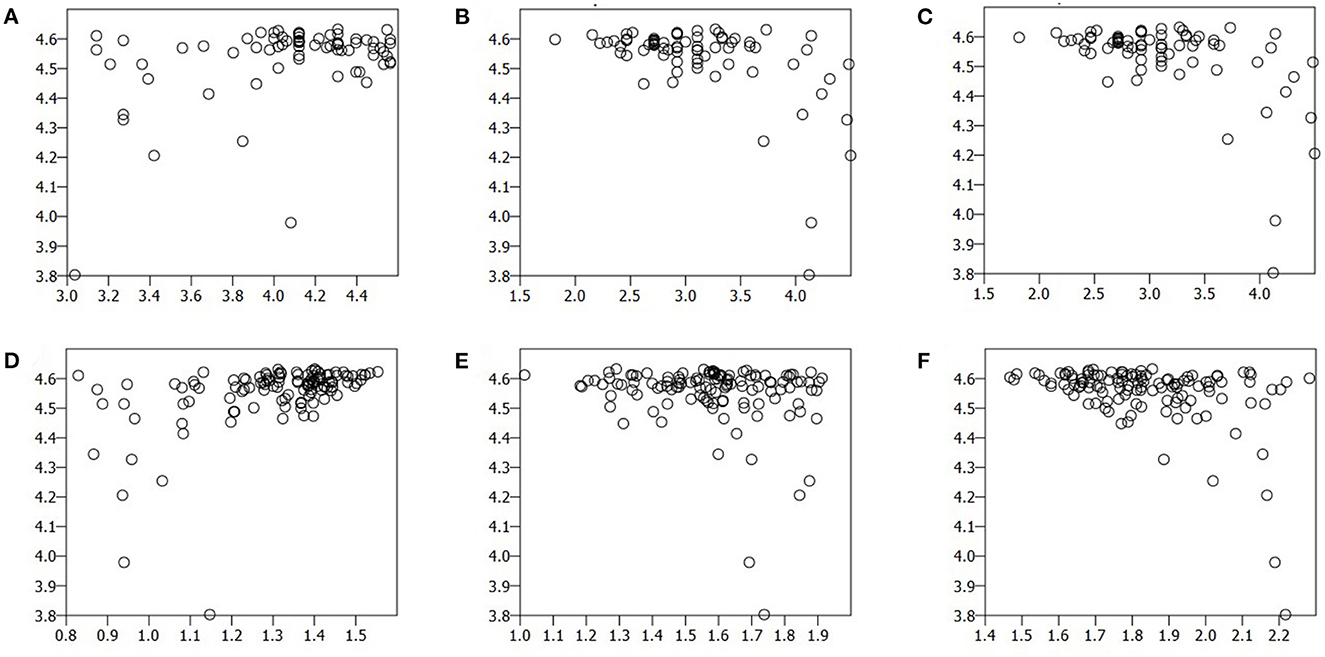
Figure 1. Scatterplots of lifetime national breastfeeding rates (Y-axis) plotted against (A) Hofstede's power distance index, (B) Hofstede's individualism-collectivism index, (C) Hofstede's masculinity-femininity index, (D) Global collectivism index, (E) prevalence of depression in women aged 15–49, and (F) prevalence of anxiety disorders in women aged 15–49 (X-axis). See the text for details of variable transformation prior to analysis.
Examinations of correlations between independent variables revealed that the prevalence of both depression and anxiety disorders were negatively correlated with power distance and long-term orientation, and positively correlated with individualism-collectivism. In addition, anxiety was positively correlated with uncertainty avoidance and indulgence-restraint. The prevalence of depression and anxiety were modestly and positively correlated with each other (r = 0.49, p < 0.01).
Partial correlation analyses
When conditioned on the prevalence of depression and anxiety disorders, lifetime breastfeeding rates remained positively correlated with power distance (partial r = 0.26, p = 0.03) and negatively correlated with individualism-collectivism (partial r = −0.43, p < 0.01) and masculinity-femininity (partial r = −0.28, p = 0.018); though there was some attenuation of the strength of the associations with power distance and individualism-collectivism, these remained statistically significant. On the other hand, when conditioned on scores for power distance and individualism-collectivism, the associations between lifetime breastfeeding rates and the prevalence of depression (partial r = −0.07, p = 0.569) and anxiety disorders (partial r = −0.22, p = 0.063) were no longer significant, though there was a trend toward a negative association with anxiety disorders.
Confirmatory analysis
The second stage of the analysis included data on 122 countries. The maximum and minimum reported values for lifetime breastfeeding were the same as those noted above, while the median (IQR) for the larger sample was 96.3 (4.2). When breastfeeding rates were compared between high-, high middle-, low middle- and low-income countries, a significant difference was noted across groups overall (Kruskal–Wallis H = 30.1, p < 0.01). Post-hoc examination of the data revealed that between-group differences were significant only between high-income countries and the other three groups (p < 0.001 for all comparisons); no significant difference could be identified between the high middle, low middle and low-income countries.
Bivariate correlations
A complete correlation matrix is presented in Table 4 and significant associations are depicted graphically in Figures 1D–F. Breastfeeding rates were positively correlated with the GCI (r = 0.47, p < 0.01) and negatively correlated with the prevalence of anxiety disorders (r = −0.40, p < 0.01) and depression (r = −0.19, p = 0.035); however, the association with depression was weak and did not survive correction for multiple comparisons. The prevalence of anxiety disorders was negatively correlated with the GCI (r = −0.33, p < 0.01), but no significant association between the GCI and the prevalence of depression was noted (r = −0.02, p = 0.810). The prevalence of anxiety and depression were correlated positively, with a strength similar to that observed in the exploratory analysis (r = 0.39, p < 0.01).
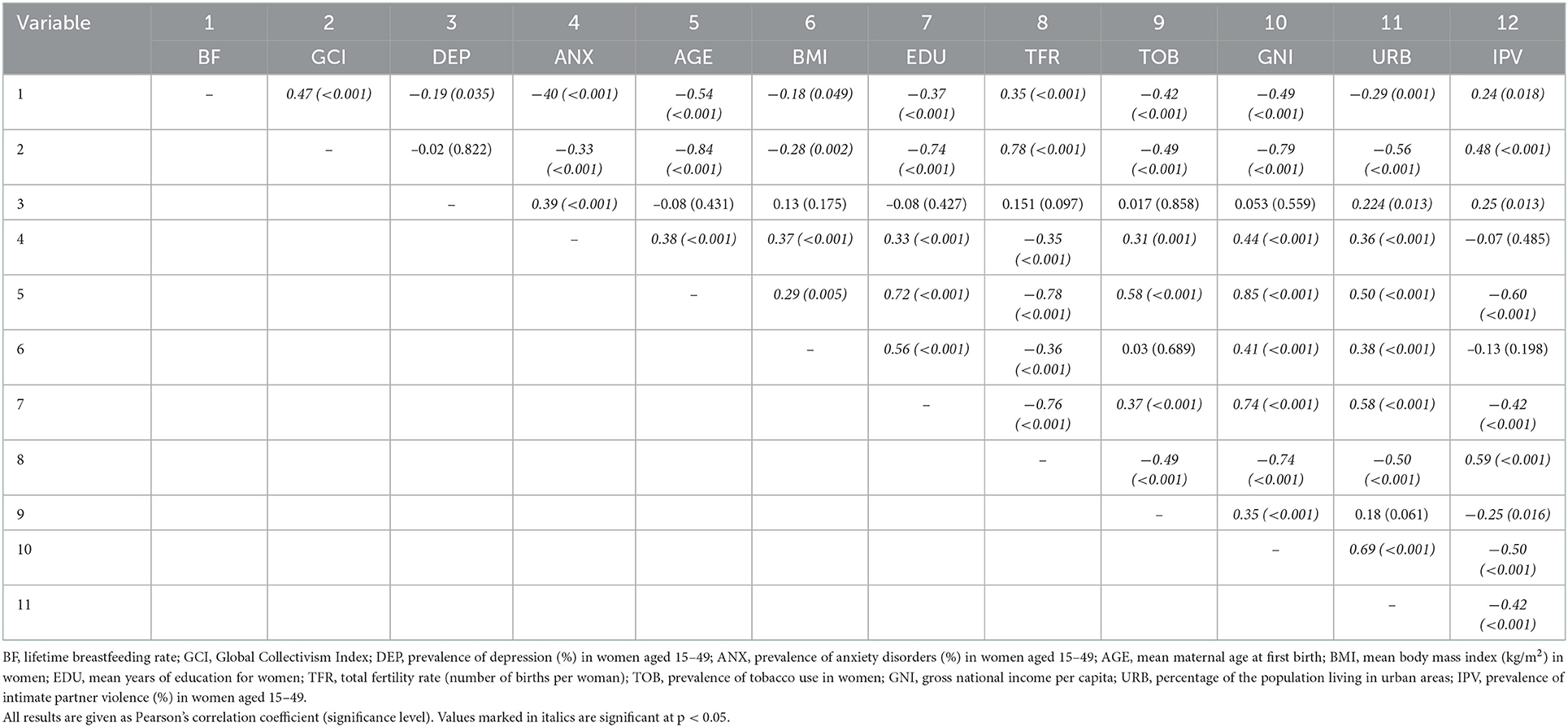
Table 4. Confirmatory correlations between national lifetime breastfeeding rates, individualism-collectivism, the prevalence of anxiety and depression in women aged 15–49, and confounding factors.
All the confounding factors examined in this stage of the study were significantly correlated with breastfeeding rates. Moderate negative correlations with the breastfeeding rate were observed for maternal age at first birth (r = −0.54, p < 0.01), per capita income (r = −0.49, p < 0.01) and tobacco use in women (r = −0.42, p < 0.01), whereas weak negative correlations were observed for mean years of education in women (r = −0.37, p < 0.01), urbanization (r = −0.29, p < 0.01) and mean body mass index in women (r = −0.18, p = 0.049). Weak positive correlation between the total fertility rate and the breastfeeding rate (r = 0.35, p < 0.01), and between the prevalence of intimate partner violence and the breastfeeding rate (r = 0.24, p = 0.018), were observed. All these correlations, except the associations with body mass index, urbanization, and intimate partner violence, remained significant after correction for multiple comparisons.
When examining correlations between the GCI, the prevalence of common mental disorders, and these confounding factors, it was noted that the GCI was positively correlated with the total fertility rate (r = 0.78, p < 0.01) and negatively correlated with all other confounders, with particularly strong associations noted for age at first birth (r = −0.84, p < 0.01), per capita income (r = −0.79, p < 0.01) and women's education (r = −0.74, p < 0.01). The prevalence of depression in women of childbearing age was significantly but weakly correlated with urbanization (r = 0.22, p = 0.013). On the other hand, the prevalence of anxiety disorders in this population was moderately and positively correlated with per capital income, weakly positively correlated with urbanization, age at first birth, mean female body mass index, women's education and tobacco use, and weakly negatively correlated with the total fertility rate. The prevalence of intimate partner violence was positively correlated with the GCI, the prevalence of depression, and the total fertility rate, and negatively correlated with age at first birth, women's education, urbanization and tobacco use.
Partial correlation analyses
When conditioned on the GCI, lifetime breastfeeding rates remained negatively associated with the prevalence of anxiety disorders (r = −0.29, p < 0.01); similarly, when conditioned on the prevalence of anxiety disorders, the GCI remained positively correlated with the breastfeeding rate (r = 0.39, p < 0.01). No such analysis was attempted for the prevalence of depression, as it was not significantly correlated with the GCI.
Multivariate analysis
All variables significantly associated with the lifetime breastfeeding rate at p < 0.05 were included in this model. As there was significant multicollinearity between the gross national income and the age at first childbirth (r = 0.85, p < 0.01), the latter variable was included in the model as it was more significantly correlated with the breastfeeding rate. The final model is presented in Table 5 and included only two variables: maternal age at first birth (β = −0.39, p < 0.001) and prevalence of anxiety disorders in women aged 15–49 (β = −0.34, p = 0.002). This model attained statistical significance overall (F = 20.41, p < 0.001), and explained around 36% of the variance in national breastfeeding rates (R2 = 0.38, adjusted R2 = 0.36).
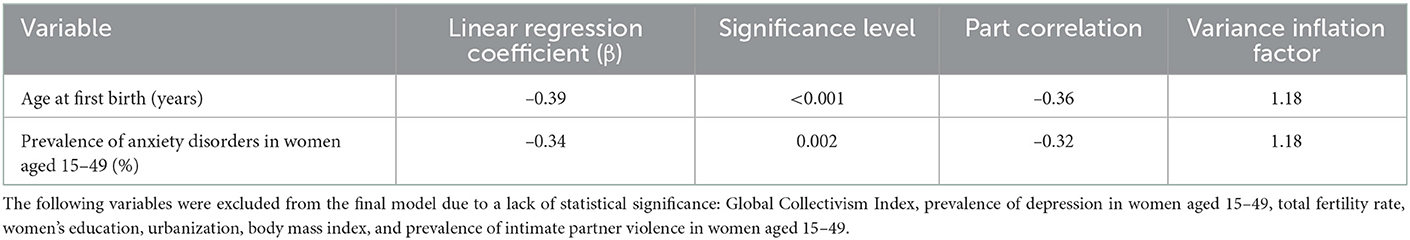
Table 5. Stepwise multivariate linear regression analysis of variables significantly associated with national lifetime breastfeeding rates.
Similar results were obtained when the regression analysis was carried out using alternate methods (“enter,” forward and backward): age at first birth and prevalence of anxiety disorders remained significantly associated with breastfeeding rates.
Discussion
In the current study, the exploratory analysis found support for the hypotheses that both cultural factors and maternal mental health were associated with cross-national variations in breastfeeding rates. While the confirmatory analysis was able to replicate the association between mental health factors—particularly anxiety—and breastfeeding rates, even after controlling for several confounding factors, a direct association with cultural dimensions could not be established. These findings and their implications are discussed below.
Relationships between culture and breastfeeding
In the current study, lifetime breastfeeding rates were found to be associated with three cultural dimensions in the initial analysis: power distance, individualism-collectivism and masculinity-femininity. Countries with higher breastfeeding rates tended to be characterized by a higher power distance, greater collectivism and more feminine values. In the confirmatory analysis, cultural collectivism remained associated with breastfeeding rates in the bivariate analysis, but was excluded from the final regression model. However, cultural collectivism was strongly correlated with both the variables in this model—age at first birth and the prevalence of anxiety disorders in women—suggesting that it may have influenced breastfeeding rates through its influence on these intermediate variables.
There are several mechanisms through which cultural values may influence breastfeeding rates. A collectivist cultural orientation may privilege the mother-infant dyad, and may be associated with greater family support for the initiation and maintenance of breastfeeding. Moreover, collectivist cultural values are associated with a greater fertility rate (Levine et al., 1995; Basabe and Ros, 2005; Pelham et al., 2022), which may be associated with more successful breastfeeding outcomes. On the other hand, a woman in an individualist culture may feel pressured to resume academic or professional duties soon after the birth of her child, and may receive less social support (Corrigan et al., 2015). There is also some evidence that pro-social values are positively associated with mother-infant bonding, while values centered on personal financial success impair the mother-infant bond (Jin et al., 2012; Obikane et al., 2020). Likewise, it is logical to assume that cultures with a more feminine orientation would be more oriented toward successful breastfeeding, as this cultural orientation is associated with values such as nurturance, care for the weak and the maintenance of stable and secure relationships. Feminine cultures may be associated with greater levels of responsiveness and support in childcare activities from husbands (Hofstede et al., 2010), which can also lead to better breastfeeding outcomes (Davidson and Ollerton, 2020). When correcting for other cultural values associated with breastfeeding, the link with a feminine cultural orientation was strengthened rather than attenuated (partial r = 0.30, p = 0.009), suggesting that this association may merit further investigation.
It is not immediately clear why power distance should be associated with breastfeeding rates, as this cultural value may be associated with a less flexible and less infant-centered approach to breastfeeding (Demuth, 2013). However, it should be noted that in the dataset analyzed in this study, power distance was strongly correlated with individualism-collectivism as well as with the prevalence of depression and of anxiety disorders (Table 3). When these associations were accounted for, the link between power distance and breastfeeding rates was weak and not statistically significant (partial r = 0.08, p = 0.494).
Despite the plausibility of these associations, it should be emphasized that a significant association between cultural values and breastfeeding was not established in the second phase of this study. It is therefore likely that these associations—if genuine and not due to chance—may be mediated by intermediate social and demographic factors, or by the effects of culture of mental health.
Relationship between mental health variables and breastfeeding
Maternal mental health has sometimes been described as the “neglected” component of maternal and child health (Rahman et al., 2008). Despite the availability of extensive data on the relationship between maternal maternal health and infant outcomes, this aspect of maternal health tends to be neglected, particularly in low- and middle-income countries where there are already significant constraints on the availability of manpower and infrastructure (Nakku et al., 2016). Though it was formerly assumed that depression and anxiety were rare during pregnancy, current evidence suggests that this is not the case; it is estimated that the prevalence of antepartum depression is around 15–16%, which is comparable to the estimated prevalence (18%) of post-partum depression (Hahn-Holbrook et al., 2018; Okagbue et al., 2019). Maternal depression or anxiety can interfere with successful bonding between a mother and her child (Tolja et al., 2020; Höflich et al., 2022), leading to difficulties in the dyadic interactions that are an essential part of breastfeeding. The neuroendocrine changes associated with these disorders, such as altered patterns of cortisol secretion, may also interfere with successful breastfeeding (Spratt et al., 2016; Bublitz et al., 2019). Women with depression may also be more likely to cease breastfeeding prematurely if they perceive themselves as being overwhelmed by other duties (Bascom and Napolitano, 2016).
In both stages of this study, breastfeeding rates were inversely correlated with the prevalence of depression and anxiety disorders in women aged 15–49. This association was stronger for anxiety disorders than for depression, and remained significant even after correcting for other variables strongly associated with breastfeeding outcomes. A meta-analytic review of 28 studies found that around 20.7% of women fulfilled criteria for an anxiety disorder either during pregnancy or in the post-partum period (Fawcett et al., 2019). A more recent meta-analysis, focused on low- and middle-income countries, replicated these findings, with 25–30% of women experiencing significant anxiety symptoms during this period, 8% receiving an anxiety disorder diagnosis during pregnancy, and 16% receiving such a diagnosis post-natally (Nielsen-Scott et al., 2022). It can be seen from these results that anxiety disorders during and after childbirth occur at a frequency comparable to that of post-partum depression.
From a mechanistic perspective, anxiety may interfere with milk production and ejection via elevations in cortisol, increased insulin resistance and reduced oxytocin release (Nagel et al., 2022), and can also impair a mother's sense of self-efficacy, leading to a loss of confidence in her ability to sustain breastfeeding over time (Corby et al., 2021; Melo et al., 2021). Anxiety during pregnancy has been linked to a lower likelihood of initiating breastfeeding (English et al., 2020), a shorter duration of breastfeeding (Riedstra and Aubuchon-Endsley, 2019; Stuebe et al., 2019), and an earlier introduction of formula feeds (Stuebe et al., 2019). Anxiety in the post-natal period has been associated with a shorter duration of exclusive breastfeeding (Davies et al., 2022), a lower likelihood of colostrum feeding (Sun et al., 2020), increased rates of bottle feeding (Sun et al., 2020), and reduced rates of exclusive breastfeeding at 3 months after delivery (Coo et al., 2020). Thus, the association found in this study between the prevalence and anxiety of disorders and lower breastfeeding rates is both biologically plausible and supported by the results of studies in individual mother-infant dyads.
Relationships between breastfeeding and other demographic or health-related variables
In the confirmatory component of this study, the association between breastfeeding rates and all the variables listed in Table 2 was replicated. The strengths of these associations were comparable to those identified for cultural or mental health variables. These findings suggest that the variables associated with the initiation or maintenance of breastfeeding in individuals also show a similar relationship at a population level. While the prevalence of depression was not significantly correlated with any of these variables except urbanization, both cultural individualism-collectivism and the prevalence of anxiety were significantly correlated with several of these variables. The relationship between demographic variables and cultural values is complex (Hofstede et al., 2010; Pelham et al., 2022). On multivariate analysis, the only demographic variable significantly associated with breastfeeding was the age at first birth; a lower age was associated with higher breastfeeding rates. This result should be interpreted with caution given that some authors have found a positive association between higher maternal age and breastfeeding continuation in large samples of mother-infant dyads (Tracz and Gajewska, 2020; Chooniedass et al., 2021), while others have reported results in line with this study's findings (Ballesta-Castillejos et al., 2021; Dong et al., 2022). There is also some evidence to suggest that breastfeeding may be optimal in mothers aged 26–35—in other words, both maternity at a very early age and advanced maternal age may be associated with reduced breastfeeding rates (Moshi et al., 2021). Moreover, age at first birth was significantly collinear with variables such as individualism-collectivism (r = −0.84), total fertility rate (r = −0.78) and gross national income (r = 0.85). Thus, it is not clear to what extent this finding can inform strategies aimed at improving breast feeding.
The interaction between culture, intimate partner violence, and mental health
Recent literature has drawn attention to the role of intimate partner violence, whether physical, psychological or sexual in nature, as a significant barrier to breastfeeding (Normann et al., 2020). In the current study, the prevalence of IPV was weakly but positively correlated with national breastfeeding rates (R2 = 0.006, Bonferroni adjusted p > 0.2). At first glance, this finding seems paradoxical. However, it should be noted that in the Normann et al. meta-analysis, no significant association between IPV and breastfeeding initiation could be found in 5 of the 6 studies reviewed; more significant effects of IPV were observed for the maintenance of breastfeeding and exclusive breastfeeding. Thus, it is possible that the noxious effects of IPV may be observed more clearly when examining rates of continuous breastfeeding. In the current study, IPV was positively correlated with both the prevalence of depression and the Global Collectivism Index. Prior research has identified cultural collectivism as contributing to IPV through its emphasis on family and group cohesiveness and “saving face” at the expense of the health and wellbeing individual women (Do et al., 2013; Sears, 2021; Natal, 2022), particularly in low- and middle-income countries. Thus, the overall impact of collectivism on breastfeeding may be complex, involving a combination of positive effects (mediated through social support and reduced depression or anxiety) and negative effects (mediated through intimate partner violence and the enforcement of strict gender-related norms) (Jackson et al., 2022). The current data supports this contention: when taking IPV into consideration, the apparent positive association between cultural collectivism and breastfeeding reduces in significance (unadjusted r = 0.47, adjusted r = 0.38). Such findings can be seen as supporting an ecological systems approach to understanding breastfeeding, in which both large- and small-scale systemic factors interact to determine long-term outcomes (Jackson et al., 2022). Further examination of the effects of IPV on mental health and breastfeeding outcomes is certainly warranted on the basis of the current results.
Implications of the study findings for the communication of breastfeeding benefits
Cultural sensitivity
The study findings suggest the possibility of a direct or indirect link between cultural values and breastfeeding rates. As noted by earlier authors, attempts to modify health-related behaviors are likely to be ineffective if they are not adapted to specific cultures and settings. Without the involvement of local social networks and communities, the dissemination of information on the benefits of breastfeeding for a mother and her child is likely to have limited efficacy (Contractor and DeChurch, 2014; Kumar et al., 2015). This was illustrated in a recent study of online breastfeeding information provided to Aboriginal women in Australia, which found that only 4 of 31 of the reviewed sites provided information and advice in a culturally appropriate manner (Hopkins et al., 2021).
The manner in which this information is conveyed to mothers and their families, as well as the source providing this information, can both influence health outcomes. Educational interventions aimed at improving breastfeeding outcomes can positively impact a mother's self-efficacy, but these should be delivered in a manner that is adapted to local cultural values (Chipojola et al., 2020). Similar considerations apply to individual or group counseling approaches. For example, in a collectivist society, the involvement of extended family members or older women in a local community as “peer educators” may favorably affect health-related outcomes (Martin et al., 2015). On the other hand, in a society with individualistic values, such a method may be seen as interfering with a mother's self-efficacy and autonomy. In such a setting, the provision of “responsive support” by a woman's husband or partner, intended to promote her sense of self-efficacy in breastfeeding, may be a more appropriate strategy (Davidson and Ollerton, 2020), as would. individual or group interventions aimed at improving breastfeeding self-efficacy (Leahy-Warren et al., 2017; Galipeau et al., 2018; Leeming et al., 2022). In collectivist societies, individual and family attitudes toward breastfeeding may be shaped by traditional beliefs and practices, and it is important that healthcare workers address these in a non-confrontational manner, even when these appear to be in opposition with scientific evidence (Bandyopadhyay, 2009; Newbrander et al., 2014). At the same time, these beliefs should not be accepted unquestioningly, and mothers should be involved in the decision-making process regarding their own feeding plans and practices (Sharma and Byrne, 2016). Those involved in providing breastfeeding support should ensure that unsupportive or hostile attitudes and beliefs are discarded, whether these arise from family members or from healthcare workers unfamiliar with the sensitive nature of this work (Sharma and Byrne, 2016; Pezley et al., 2022). Finally, it is essential that those seeking to provide help to breastfeeding mothers familiarize themselves with the unique social, cultural and economic contexts of women from specific communities, particularly if they face other forms of discrimination or marginalization (Gyamfi et al., 2021).
Similar considerations arise when considering the masculinity-femininity dimension, which was also found to be associated with breastfeeding rates in this study. Countries with masculine values place a strong emphasis on competitiveness and achievement; in such settings, communicating the benefits of breastfeeding for a child's cognitive and educational achievement may be beneficial when advising mothers (LeWinn et al., 2020; Plunkett et al., 2021). Cultural masculinity is also associated with a stricter segregation of gender roles in the family, in which “fathers deal with facts, and mothers deal with feelings” (Hofstede et al., 2010). In such settings, attempting to leverage emotional support from a husband or partner may be unsuccessful; instead, peer groups involving mothers facing common challenges, who are able to support each other emotionally, may be more beneficial (Leahy-Warren et al., 2017). On the other hand, countries with feminine values place a greater emphasis on social bonds, cooperation and nurturing, and parental responsibilities are more equally shared in households. In such cultures, involving a husband or partner in efforts to support breastfeeding may be more effective (Grandahl et al., 2020), and communicating the benefits of breastfeeding in terms of mother-child bonds (Linde et al., 2020; Roth et al., 2021) and child social behavior (Reynolds et al., 2014) may be a more optimal strategy.
In developed countries, a special problem is posed by migrant women who experience a clash between the values of their country or culture of origin, and those of their “new” country, when initiating or continuing breastfeeding (Gallegos et al., 2015; Hohl et al., 2016). In such cases, those involved in providing maternal and health care should be aware of the beliefs and practices associated with breastfeeding in both cultures, and provide advice and guidance in a culturally sensitive manner.
Recognition and management of maternal anxiety and depression
Anxiety disorders and depression are common and occur at roughly equal rates both during pregnancy and in the postpartum period. Evidence from studies in general population samples suggests that these disorders co-occur frequently (Saha et al., 2021), and a meta-analysis of studies involving pregnant and post-natal women found that ~9% of women qualified for both diagnoses during pregnancy, and 4% in the post-partum period (Falah-Hassani et al., 2017). In addition to diagnosed or “syndromal” disorders, many mothers experience “sub-threshold” symptoms of anxiety or depression, which cause significant distress but do not fulfill the criteria for a psychiatric diagnosis (Andersson et al., 2006; Meaney, 2018; Rizzo et al., 2022). The impact of peripartum mental health on breastfeeding practices appears to remain significant even after correcting for demographic factors (Wouk et al., 2017).
Effective screening tools for the diagnosis of these conditions exist, and they can be managed effectively through individual or group psychological interventions, as well as through integrated interventions aimed at improving physical health and nutritional status (Kroska and Stowe, 2020; Yahya et al., 2021). However, diagnostic tools require adaptation to be understandable in non-Western cultural contexts (Green et al., 2018), and significant barriers in terms of budgetary allocation, infrastructure and manpower may compromise the provision of maternal mental health care in low- and middle-income countries (Hanlon et al., 2016). The acceptability of specific forms of treatment, particularly pharmacological therapies, may be low in certain cultures (Azale et al., 2016; Simhi et al., 2019). Cultural values can also influence the stigma associated with mental illness: in collectivist cultures, having a family member with a mental illness may be associated with shame a loss of “face,” leading to social stigma. On the other hand, in individualist cultures, a depressed or anxious individual's inability to achieve certain goals or perform certain tasks may lead to a sense of guilt and self-stigma. In both cases, the result is reduced help-seeking, though the causal mechanisms differ (Abdullah and Brown, 2011; Ran et al., 2021).
These considerations suggest that the incorporation of a mental health component into programmes aimed at communicating the benefits of breastfeeding would be beneficial for both the mother and her child. In settings where formal visits to a health center are difficult, or where formal resources are limited, community-based psychological interventions, delivered at home by non-specialists, may be equally effective (Brock et al., 2017). Group-based approaches may also be helpful in reducing both perinatal anxiety and its endocrine correlates, and is cost-effective in low-income settings (Urizar et al., 2019). Components of these interventions could fruitfully be incorporated into broader programmes aimed at optimizing maternal and child health outcomes, and adapted to the needs of specific cultures (George et al., 2020). It is also essential to screen for the possibility of intimate partner violence in breastfeeding mothers with significant anxiety and depression, but this must be done with sensitivity and in a manner acceptable to them. In many non-Western cultures, women are reluctant to report IPV spontaneously, even when it has a significant impact on their physical and mental health (Ting and Panchanadeswaran, 2009; Sears, 2021). Given the existing evidence on the links between IPV, maternal mental health, and breastfeeding outcomes (Normann et al., 2020; Tran et al., 2020), it is crucial not to neglect this aspect of assessment when women present with difficulties in initiating or maintaining breastfeeding.
Limitations
This study is subject to certain important limitations. First, it is based on analyses of survey data and estimates of disease burden, which are subject to error related to the sampling strategies and statistical methods used. Second, as it is based on a cross-sectional analysis of data, the study findings cannot be used to draw any firm conclusions regarding causality (for example, the association between breastfeeding and mental health disorder may indicate a beneficial effect of the former on the latter, a deleterious effect of the latter on the former, or a combination of both). Third, as it is based on population-level data, the study findings cannot be directly extrapolated to individuals; population-level findings are subject to the “ecological fallacy” (Roumeliotis et al., 2021) and cannot be translated directly into individual-level recommendations. Fourth, it is highly likely that breastfeeding outcomes may be influenced by other variables that were not included in this study, but exert a significant effect at an individual level: these include maternal employment and workplace policies (Vilar-Compte et al., 2021), marital and family discord (Ahmed et al., 2022), intimate partner violence (Miller-Graff et al., 2018; Da Thi Tran et al., 2022), and health literacy, which is distinct from educational attainment (Haaland and Sitaraman, 2022). Fifth, the outcome variable used in this study was the rate of “ever having breastfed;” thus, this study cannot distinguish between factors associated with the initiation of breastfeeding and those associated with its maintenance over a period of 6 months. Sixth, caution must be exercised when interpreting findings related to culture. Though cultural dimensions are useful constructs when making country-level comparisons, they are abstract entities and should not be “reified” for the purpose of generalizations (such as “individualistic values are a barrier to breastfeeding” or “femininity is better than masculinity in the context of breastfeeding”). Rather, the various beliefs and behaviors contained within each dimension should be examined in a more fine-grained manner, to obtain a more balanced view of the impact of culture on individual mother-infant dyads (Van Esterik, 1996). Seventh, certain other variables that could interfere with the initiation of breastfeeding, such as childhood adversity and traumatic birth experiences, could not be examined as there was no cross-national data available. Eighth, it was possible to carry out a confirmatory analysis only for individualism-collectivism, as there is no other larger or more recent data source for power distance or masculinity-femininity. Finally, increased industrialization, economic development and urbanization has led to cultural changes in several countries (Pelham et al., 2022). This should be taken into account when examining the effect of culture on breastfeeding practices and outcomes.
Conclusions
Despite certain limitations inherent in the methodology adopted, the current study is consistent with existing evidence on the relationships between culture, mental health and breastfeeding. This study also extends the results of prior studies by highlighting the potential contributions of specific cultural values (such as individualism-collectivism and masculinity-femininity) and the role of maternal anxiety as a barrier to successful breastfeeding. These findings provide valuable leads for further cross-national, individual-level research on the socio-cultural and psychological factors influencing the initiation and maintenance of breastfeeding, which could be extended through both quantitative and qualitative research across nations and cultures (Leeming et al., 2017). More importantly, these findings can also be used to improve existing information, education and communication strategies to improve breastfeeding outcomes, and to develop innovative approaches to addressing cultural concerns and maternal mental health in a sensitive and inclusive manner. The incorporation of cross-cultural and mental health components into such programmes, if done correctly, could lead to a “socially sensitive” approach to breastfeeding (Leeming et al., 2013) which would entail “listening to women's voices” across diverse cultures (Ting and Panchanadeswaran, 2009). Such an approach could lead to greater equity in breastfeeding practices at a global level (Gyamfi et al., 2021; Vilar-Compte et al., 2021; North et al., 2022), leading to better health outcomes for both mothers and their children.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the author, without undue reservation.
Author contributions
RR: design, data collection, data analysis, writing, and editing.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abdullah, T., and Brown, T. L. (2011). Mental illness stigma and ethnocultural beliefs, values, and norms: an integrative review. Clin. Psychol. Rev. 31, 934–948. doi: 10.1016/j.cpr.2011.05.003
Ahmed, F., Malik, N. I., Shahzad, M., Ahmad, M., Shahid, M., Feng, X. L., et al. (2022). Determinants of infant young child feeding among mothers of malnourished children in south Punjab, Pakistan: a qualitative study. Front. Public Health 10, 834089. doi: 10.3389/fpubh.2022.834089
Amoo, T. B., Popoola, T., and Lucas, R. (2022). Promoting the practice of exclusive breastfeeding: a philosophic scoping review. BMC Pregn. Childbirth 22, 380. doi: 10.1186/s12884-022-04689-w
Andersson, L., Sundström-Poromaa, I., Wulff, M., Aström, M., and Bixo, M. (2006). Depression and anxiety during pregnancy and 6 months postpartum: a follow-up study. Acta Obstet. Gynecol. Scand. 85, 937–944. doi: 10.1080/00016340600697652
Aryeetey, R., and Dykes, F. (2018). Global implications of the new WHO and UNICEF implementation guidance on the revised baby-friendly hospital initiative. Matern. Child. Nutr. 14, e12637. doi: 10.1111/mcn.12637
Azale, T., Fekadu, A., and Hanlon, C. (2016). Treatment gap and help-seeking for postpartum depression in a rural African setting. BMC Psychiatry 16, 196. doi: 10.1186/s12888-016-0892-8
Ballesta-Castillejos, A., Gómez-Salgado, J., Rodríguez-Almagro, J., and Hernández-Martínez, A. (2021). Development and validation of a predictive model of exclusive breastfeeding at hospital discharge: retrospective cohort study. Int. J. Nurs. Stud. 117, 103898. doi: 10.1016/j.ijnurstu.2021.103898
Bandyopadhyay, M. (2009). Impact of ritual pollution on lactation and breastfeeding practices in rural West Bengal, India. Int. Breastfeed. J. 4, 2. doi: 10.1186/1746-4358-4-2
Bar, S., Milanaik, R., and Adesman, A. (2016). Long-term neurodevelopmental benefits of breastfeeding. Curr. Opin. Pediatrics 28, 559–566. doi: 10.1097/MOP.0000000000000389
Basabe, N., and Ros, M. (2005). Cultural dimensions and social behavior correlates: individualism-collectivism and power distance. Int. Rev. Soc. Psychol. 18, 189–225. Available online at: https://psycnet.apa.org/record/2005-06455-008
Bascom, E. M., and Napolitano, M. A. (2016). Breastfeeding duration and primary reasons for breastfeeding cessation among women with postpartum depressive symptoms. J. Hum. Lact. 32, 282–291. doi: 10.1177/0890334415619908
Beake, S., Pellowe, C., Dykes, F., Schmied, V., and Bick, D. (2012). A systematic review of structured compared with non-structured breastfeeding programmes to support the initiation of and duration of exclusive and any breastfeeding in acute and primary health care settings. Matern. Child Nutr. 8, 141–161. doi: 10.1111/j.1740-8709.2011.00381.x
Borg, M. A. (2012). National cultural dimensions as drivers of inappropriate ambulatory care consumption of antibiotics in Europe and their relevance to awareness campaigns. J. Antimicrob. Chemother. 67, 763–767. doi: 10.1093/jac/dkr541
Borisova, L. V., Martinussen, P. E., Rydland, H. T., Stornes, P., and Eikemo, T. A. (2017). Public evaluation of health services across 21 European countries: the role of culture. Scand. J. Public Health 45, 132–139. doi: 10.1177/1403494816685920
Brock, R. L., O'Hara, M. W., and Segre, L. S. (2017). Depression treatment by non-mental-health providers: incremental evidence for the effectiveness of listening visits. Am. J. Community Psychol. 59, 172–183. doi: 10.1002/ajcp.12129
Bublitz, M. H., Bourjeilly, G., Bilodeau, C., and Stroud, L. R. (2019). Maternal circadian cortisol mediates the link between prenatal distress and breastfeeding. Stress 22, 53–59. doi: 10.1080/10253890.2018.1501023
Butler, M. S., Young, S. L., and Tuthill, E. L. (2013). Perinatal depressive symptoms and breastfeeding behaviors: a systematic literature review and biosocial research agenda. J. Affect. Disord. 283, 441–471. doi: 10.1016/j.jad.2020.11.080
Chipojola, R., Chiu, H.-Y., Huda, M. H., Lin, Y.-M., and Kuo, S.-Y. (2020). Effectiveness of theory-based educational interventions on breastfeeding self-efficacy and exclusive breastfeeding: a systematic review and meta-analysis. Int. J. Nurs. Stud. 109, 103675. doi: 10.1016/j.ijnurstu.2020.103675
Chooniedass, R., Tarrant, M., Turner, S., Lok Fan, H. S., Del Buono, K., Masina, S., et al. (2021). Factors associated with breast-feeding initiation and continuation in Canadian-born and non-Canadian-born women: a multi-centre study. Public Health Nutr. 3, 1–12. doi: 10.1017/S1368980021004699
Chow, H.-W., and Dong, Y.-H. (2013). Relationship between participation in leisure activities and constraints on Taiwanese breastfeeding mothers during leisure activities. BMC Public Health 13, 410. doi: 10.1186/1471-2458-13-410
Cohen, S. S., Alexander, D. D., Krebs, N. F., Young, B. E., Cabana, M. D., Erdmann, P., et al. (2018). Factors associated with breastfeeding initiation and continuation: A meta-analysis. J. Pediatr. 203, 190–196. doi: 10.1016/j.jpeds.2018.08.008
Contractor, N. S., and DeChurch, L. A. (2014). Integrating social networks and human social motives to achieve social influence at scale. Proc. Natl. Acad. Sci. U. S. A. 111, 13650–13657. doi: 10.1073/pnas.1401211111
Coo, S., García, M. I., Mira, A., and Valdés, V. (2020). The role of perinatal anxiety and depression in breastfeeding practices. Breastfeed. Med. 15, 495–500. doi: 10.1089/bfm.2020.0091
Cook, N., Ayers, S., and Horsch, A. (2018). Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J. Affect. Disord. 225, 18–31. doi: 10.1016/j.jad.2017.07.045
Corby, K., Kane, D., and Dayus, D. (2021). Investigating predictors of prenatal breastfeeding self-efficacy. Can. J. Nurs. Res. 53, 56–63. doi: 10.1177/0844562119888363
Corrigan, C. P., Kwasky, A. N., and Groh, C. J. (2015). Social support, postpartum depression, and professional assistance: a survey of mothers in the Midwestern United States. J. Perinat. Educ. 24, 48–60. doi: 10.1891/1058-1243.24.1.48
Da Thi Tran, T., Murray, L., and Van Vo, T. (2022). Intimate partner violence during pregnancy and maternal and child health outcomes: a scoping review of the literature from low-and-middle income countries from 2016 to 2021. BMC Pregn. Childbirth 22, 315. doi: 10.1186/s12884-022-04604-3
Dadi, A. F., Miller, E. R., and Mwanri, L. (2020). Postnatal depression and its association with adverse infant health outcomes in low- and middle-income countries: a systematic review and meta-analysis. BMC Pregn. Childbirth 20, 416. doi: 10.1186/s12884-020-03092-7
Davidson, E. L., and Ollerton, R. L. (2020). Partner behaviours improving breastfeeding outcomes: an integrative review. Women Birth 33, e15–e23. doi: 10.1016/j.wombi.2019.05.010
Davies, S. M., Todd-Leonida, B. F., Fallon, V. M., and Silverio, S. A. (2022). Exclusive breastfeeding duration and perceptions of infant sleep: the mediating role of postpartum anxiety. Int. J. Environ. Res. Public Health 19, 4494. doi: 10.3390/ijerph19084494
de Jager, E., Skouteris, H., Broadbent, J., Amir, L., and Mellor, K. (2013). Psychosocial correlates of exclusive breastfeeding: a systematic review. Midwifery 29, 506–518. doi: 10.1016/j.midw.2012.04.009
Del Ciampo, L. A., and Del Ciampo, I. R. L. (2018). Breastfeeding and the benefits of lactation for women's health. Rev. Bras. Ginecol. Obstet. 40, 354–359. doi: 10.1055/s-0038-1657766
Demuth, C. (2013). Handling power-asymmetry in interactions with infants: a comparative socio-cultural perspective. Interact. Stud. 14, 212–239. doi: 10.1075/is.14.2.04dem
Dias, C. C., and Figueiredo, B. (2015). Breastfeeding and depression: a systematic review of the literature. J. Affect. Disord. 171, 142–154. doi: 10.1016/j.jad.2014.09.022
Do, K. N., Weiss, B., and Pollack, A. (2013). Cultural beliefs, intimate partner violence and mental health functioning among Vietnamese women. Int. Perspect. Psychol. 2, 4. doi: 10.1037/ipp0000004
Dong, D., Ru, X., Huang, X., Sang, T., Li, S., Wang, Y., et al. (2022). A prospective cohort study on lactation status and breastfeeding challenges in mothers giving birth to preterm infants. Int. Breastfeed. J. 17, 6. doi: 10.1186/s13006-021-00447-4
Dornan, L., Sinclair, M., Kernohan, W. G., Stockdale, J., Khuwuthyakorn, V., and Suppasan, P. (2015). Thai cultural influences on breastfeeding behaviour. Evid. Based Midwifery 13, 84–91. Available online at: https://www.proquest.com/openview/2cc58548b8693cb598c7929b4813fd08/
English, S., Wright, I., Ashburn, V., Ford, G., and Caramaschi, D. (2020). Prenatal anxiety, breastfeeding and child growth and puberty: linking evolutionary models with human cohort studies. Ann. Hum. Biol. 47, 106–115. doi: 10.1080/03014460.2020.1751286
Enriquez, J. P., and Archila-Godinez, J. C. (2022). Social and cultural influences on food choices: a review. Crit. Rev. Food Sci. Nutr. 62, 3698–3704. doi: 10.1080/10408398.2020.1870434
Falah-Hassani, K., Shiri, R., and Dennis, C. L. (2017). The prevalence of antenatal and postnatal co-morbid anxiety and depression: a meta-analysis. Psychol. Med. 47, 2041–2053. doi: 10.1017/S0033291717000617
Falana, S. D., and Carrington, J. M. (2019). Postpartum depression: are you listening? Nurs. Clin. North. Am. 54, 561–567. doi: 10.1016/j.cnur.2019.07.006
Fallon, V., Bennett, M. K., and Harrold, J. A. (2016b). Prenatal anxiety and infant feeding outcomes: a systematic review. J. Hum. Lact. 32, 53–66. doi: 10.1177/0890334415604129
Fallon, V., Groves, R., Halford, J. C., Bennett, K. M., and Harrold, J. A. (2016a). Postpartum anxiety and infant-feeding outcomes. J. Hum. Lact. 32, 740–758. doi: 10.1177/0890334416662241
Fawcett, E. J., Fairbrother, N., Cox, M. L., White, I. R., and Fawcett, J. M. (2019). The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J. Clin. Psychiatry 80, 18r12527. doi: 10.4088/JCP.18r12527
Galipeau, R., Baillot, A., Trottier, A., and Lemire, L. (2018). Effectiveness of interventions on breastfeeding self-efficacy and perceived insufficient milk supply: a systematic review and meta-analysis. Matern. Child Nutr. 14, e12607. doi: 10.1111/mcn.12607
Gallegos, D., Vicca, N., and Steiner, S. (2015). Breastfeeding beliefs and practices of African women living in Brisbane and Perth, Australia. Matern. Child Nutr. 11, 727–736. doi: 10.1111/mcn.12034
George, C., Kumar, V. A., and Girish, N. (2020). Effectiveness of a group intervention led by lay health workers in reducing the incidence of postpartum depression in South India. Asian J. Psychiatr. 47, 101864. doi: 10.1016/j.ajp.2019.101864
Gerlach, P., and Eriksson, K. (2021). Measuring cultural dimensions: external validity and internal consistency of Hofstede's VSM 2013 scales. Front. Psychol. 12, 662604. doi: 10.3389/fpsyg.2021.662604
Global Burden of Disease Collaborative Network (2020). Global Burden of Disease Study 2019 (GBD 2019) Results. Seattle: Institute for Health Metrics and Evaluation (IHME). Available online at: http://ghdx.healthdata.org/gbd-results-tool (accessed June 2, 2022).
Gómez, L., Verd, S., de-la-Banda, G., Cardo, E., Servera, M., Filgueira, A., et al. (2021). Perinatal psychological interventions to promote breastfeeding: a narrative review. Int. Breastfeed. J. 16, 8. doi: 10.1186/s13006-020-00348-y
Gomez-Pomer, E., and Blubaugh, R. (2018). The baby friendly hospital initiative and the ten steps for successful breastfeeding. J. Perinatol. 38, 623–632. doi: 10.1038/s41372-018-0068-0
Grandahl, M., Stern, J., and Funkquist, E. L. (2020). Longer shared parental leave is associated with longer duration of breastfeeding: a cross-sectional study among Swedish mothers and their partners. BMC Pediatr. 20, 159. doi: 10.1186/s12887-020-02065-1
Green, E. P., Tuli, H., Kwobah, E., Menya, D., Chesire, I., and Schmidt, C. (2018). Developing and validating a perinatal depression screening tool in Kenya blending Western criteria with local idioms: a mixed methods study. J. Affect. Disord. 228, 49–59. doi: 10.1016/j.jad.2017.11.027
Grigoriadis, S., Graves, L., Peer, M., Mamisashvili, L., Tomlinson, G., Vigod, S. N., et al. (2019). A systematic review and meta-analysis of the effects of antenatal anxiety on postpartum outcomes. Arch. Womens Ment. Health 22, 543–556. doi: 10.1007/s00737-018-0930-2
Grigoriadis, S., VonderPorten, E. H., Mamisashvili, L., Tomlinson, G., Dennis, C.-L., Koren, G., et al. (2013). The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J. Clin. Psychiatry 74, e321–341. doi: 10.4088/JCP.12r07968
Gyamfi, A., O'Neill, B., Henderson, W. A., and Lucas, R. (2021). Black/African–American breastfeeding experience: cultural, sociological, and health dimensions through an equity lens. Breastfeed. Med. 16, 103–111. doi: 10.1089/bfm.2020.0312
Haaland, K., and Sitaraman, S. (2022). Increased breastfeeding; an educational exchange program between India and Norway improving newborn health in a low- and middle-income hospital population. J. Health Popul. Nutr. 41, 16. doi: 10.1186/s41043-022-00297-8
Hahn-Holbrook, J., Cornwell-Hinrichs, T., and Anaya, I. (2018). Economic and health predictors of national postpartum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Front. Psychiatr. 8, 248. doi: 10.3389/fpsyt.2017.00248
Hanlon, C., Fekadu, A., Jordans, M., Kigozi, F., Petersen, I., Shidhaye, R., et al. (2016). District mental healthcare plans for five low- and middle-income countries: commonalities, variations and evidence gaps. Br. J. Psychiatry 208, s47–s54. doi: 10.1192/bjp.bp.114.153767
Hanser, A., and Li, J. (2017). The hard work of feeding the baby: breastfeeding and intensive mothering in contemporary urban China. J. Chinese Sociol. 4, 18. doi: 10.1186/s40711-017-0065-2
Hashemi-Nazari, S. -S., Hasani, J., Izadi, N., Najafi, F., Rahmani, J., Naseri, P., et al. (2020). The effect of pre-pregnancy body mass index on breastfeeding initiation, intention and duration: a systematic review and dose-response meta-analysis. Heliyon. 6, e05622. doi: 10.1016/j.heliyon.2020.e05622
Hedberg, I. C. (2013). Barriers to breastfeeding in the WIC population. MCN Am. J. Matern. Child Nurs. 38, 244–249. doi: 10.1097/NMC.0b013e3182836ca2
Hoff, C. E., Movva, N., Vollmar, A. K. R., and Perez-Escamilla, R. (2019). Impact of maternal anxiety on breastfeeding outcomes: a systematic review. Adv. Nutr. 10, 816–826. doi: 10.1093/advances/nmy132
Höflich, A., Kautzky, A., Slamanig, R., Kampshoff, J., and Unger, A. (2022). Depressive symptoms as a transdiagnostic mediator of mother-to-infant bonding: results from a psychiatric mother-baby unit. J. Psychiatr. Res. 149, 37–43. doi: 10.1016/j.jpsychires.2022.02.005
Hofstede Insights (2022). Country Comparison. Helsinki: Hofstede Insights. Available online at: https://www.hofstede-insights.com/country-comparison/ (accessed June 2, 2022).
Hofstede, G., Hofstede, G. J., and Minkov, M. (2010). Cultures and Organizations: Software of the Mind, 3rd Edn. New York: McGraw-Hill.
Hohl, S., Thompson, B., Escareno, M., and Duggan, C. (2016). Cultural norms in conflict: breastfeeding among Hispanic immigrants in Rural Washington State. Matern. Child Health J. 20, 1549–1557. doi: 10.1007/s10995-016-1954-8
Hopkins, M., Meedya, S., Ivers, R., and Charlton, K. (2021). Review of online breastfeeding information for Aboriginal and Torres Strait Islander women. Women Birth 34, 309–315. doi: 10.1016/j.wombi.2020.06.012
Hsu, S.-Y., Woodside, A. G., and Marshall, R. (2013). Critical tests of multiple theories of cultures' consequences: comparing the usefulness of models by Hofstede, Inglehart and Baker, Schwartz, Steenkamp, as well as GDP and distance for explaining overseas tourism behavior. J. Travel Res. 52, 679–704. doi: 10.1177/0047287512475218
Ip, S., Chung, M., Raman, G., Chew, P., Magula, N., DeVine, D., et al. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evid. Rep. Technol. Assess. 153, 1–186.
Jackson, J., Safari, R., and Hallam, J. (2022). A narrative synthesis using the ecological systems theory for understanding a woman's ability to continue breastfeeding. Int. J. Health Promot. Educ. 8, 98162. doi: 10.1080/14635240.2022.2098162
Jin, M. K., Jacobvitz, D., Hazen, N., and Jung, S. H. (2012). Maternal sensitivity and infant attachment security in Korea: Cross-cultural validation of the strange situation. Attach. Hum. Dev. 14, 33–44. doi: 10.1080/14616734.2012.636656
Kim, S., Park, M., and Ahn, S. (2022). The impact of antepartum depression and postpartum depression on exclusive breastfeeding: a systematic review and meta-analysis. Clin. Nurs. Res. 31, 866–880. doi: 10.1177/10547738211053507
Kramer, M. S., and Kakuma, R. (2012). Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012, CD003517. doi: 10.1002/14651858.CD003517.pub2
Kroska, E. B., and Stowe, Z. N. (2020). Postpartum depression: identification and treatment in the clinic setting. Obstet. Gynecol. Clin. North Am. 47, 409–419. doi: 10.1016/j.ogc.2020.05.001
Kumar, V., Kumar, A., Ghosh, A. K., Samphel, R., Yadav, R., Yeung, D., et al. (2015). Enculturating science: community-centric design of behavior change interactions for accelerating health impact. Semin. Perinatol. 39, 393–415. doi: 10.1053/j.semperi.2015.06.010
Leahy-Warren, P., Creedon, M., O'Mahony, A., and Mulcahy, H. (2017). Normalising breastfeeding within a formula feeding culture: an Irish qualitative study. Women Birth. 30, e103–e110. doi: 10.1016/j.wombi.2016.10.002
LeCuyer, E. A., and Zhang, Y. (2015). An integrative review of ethnic and cultural variation in socialization and children's self-regulation. J. Adv. Nurs. 71, 735–750. doi: 10.1111/jan.12526
Leeming, D., Marshall, J., and Hinsliff, S. (2022). Self-conscious emotions and breastfeeding support: a focused synthesis of UK qualitative research. Mat. Child. Nutr.18, e13270. doi: 10.1111/mcn.13270
Leeming, D., Marshall, J., and Locke, A. (2017). Understanding process and context in breastfeeding support interventions: the potential of qualitative research. Matern. Child Nutr. 13, e12407. doi: 10.1111/mcn.12407
Leeming, D., Williamson, I., Lyttle, S., and Johnson, S. (2013). Socially sensitive lactation: exploring the social context of breastfeeding. Psychol. Health 28, 450–468. doi: 10.1080/08870446.2012.737465
Levine, R., Sato, S., Hashimoto, T., and Verma, J. (1995). Love and marriage in eleven cultures. J. Cross Cult. Psychol. 26, 554–571. doi: 10.1177/0022022195265007
LeWinn, K. Z., Bush, N. R., Batra, A., Tylavsky, F., and Rehkopf, D. (2020). Identification of modifiable social and behavioral factors associated with childhood cognitive performance. JAMA Pediatr. 174, 1063–1072. doi: 10.1001/jamapediatrics.2020.2904
Linde, K., Lehnig, F., Nagl, M., and Kersting, A. (2020). The association between breastfeeding and attachment: a systematic review. Midwifery 81, 102592. doi: 10.1016/j.midw.2019.102592
Lyons, S., Currie, S., Peters, S., Lavender, T., and Smith, D. M. (2018). The association between psychological factors and breastfeeding behaviour in women with a body mass index (BMI) ≥30 kg m−2: a systematic review. Obes. Rev. 19, 947–959. doi: 10.1111/obr.12681
Mansyur, C. L., Amick, B. C., Harrist, R. B., Franzini, L., and Roberts, R. E. (2009). The cultural production of health inequalities: a cross-sectional, multilevel examination of 52 countries. Int. J. Health Serv. 39, 301–319. doi: 10.2190/HS.39.2.e
Martin, S. L., Muhomah, T., Thuita, F., Bingham, A., and Mukuria, A. G. (2015). What motivates maternal and child nutrition peer educators? Experiences of fathers and grandmothers in western Kenya. Soc. Sci. Med. 143, 45–53. doi: 10.1016/j.socscimed.2015.08.036
Masood, M., Aggarwal, A., and Reidpath, D. D. (2019). Effect of national culture on BMI: a multilevel analysis of 53 countries. BMC Public Health 19, 1212. doi: 10.1186/s12889-019-7536-0
Matus, J. C. (2021). A comparison of country's cultural dimensions and health outcomes. Healthcare 9, 1654. doi: 10.3390/healthcare9121654
Meaney, M. J. (2018). Perinatal maternal depressive symptoms as an issue for population health. Am. J. Psychiatry 175, 1084–1093. doi: 10.1176/appi.ajp.2018.17091031
Melo, L., Bonelli, M., Lima, R., Gomes-Sponholz, F. A., and Monteiro, J. (2021). Anxiety and its influence on maternal breastfeeding self-efficacy. Rev. Lat. Am. Enfermagem 29, e3485. doi: 10.1590/1518-8345.5104.3485
Miller-Graff, L. E., Ahmed, A. H., and Paulson, J. L. (2018). Intimate partner violence and breastfeeding outcomes in a sample of low-income women. J. Hum. Lact. 34, 494–502. doi: 10.1177/0890334418776217
Moshi, F. V., Akyoo, E. E., and Seif, S. A. (2021). Prevalence and predictor of exclusive breastfeeding among mothers of 0 to 6 months infants from pastoralists and hunters' community in Tanzania: a community based cross-sectional study. East Afr. Health Res. J. 5, 82–90. doi: 10.24248/eahrj.v5i1.654
Moya, C., and Henrich, J. (2016). Culture-gene coevolutionary psychology: cultural learning, language, and ethnic psychology. Curr. Opin. Psychol. 8, 112–118. doi: 10.1016/j.copsyc.2015.10.001
Nagel, E. M., Howland, M. A., Pando, C., Stang, J., Mason, S. M., Fields, D. A., et al. (2022). Maternal psychological distress and lactation and breastfeeding outcomes: a narrative review. Clin. Ther. 44, 215–227. doi: 10.1016/j.clinthera.2021.11.007
Nakku, J. E., Okello, E. S., Kizza, D., Honikman, S., Ssebunnya, J., Ndyanabangi, S., et al. (2016). Perinatal mental health care in a rural African district, Uganda: a qualitative study of barriers, facilitators and needs. BMC Health Serv. Res. 16, 295. doi: 10.1186/s12913-016-1547-7
Natal, M. (2022). Intimate partner violence experiences among Puerto Rican mothers. J. Interpers. Viol. 37, NP2626–NP2651. doi: 10.1177/0886260520944556
Newbrander, W., Natiq, K., Shahim, S., Hamid, N., and Skena, N. B. (2014). Barriers to appropriate care for mothers and infants during the perinatal period in rural Afghanistan: a qualitative assessment. Glob. Public Health 9, S93–S109. doi: 10.1080/17441692.2013.827735
Ni, P. K., and Lin, S. K. S. (2011). The role of family and friends in providing social support towards enhancing the wellbeing of postpartum women: a comprehensive systematic review. JBI Libr. Syst. Rev. 9, 313–370. doi: 10.11124/jbisrir-2011-94
Nielsen-Scott, M., Fellmeth, G., Opondo, C., and Alderdice, F. (2022). Prevalence of perinatal anxiety in low- and middle-income countries: a systematic review and meta-analysis. J. Affect. Disord. 306, 71–79. doi: 10.1016/j.jad.2022.03.032
Normann, A. K., Bakiewicz, A., Madsen, F. K., Khan, K. S., Rasch, V., and Linde, D. S. (2020). Intimate partner violence and breastfeeding: a systematic review. BMJ Open 10, e034153. doi: 10.1136/bmjopen-2019-034153
North, K., Gao, M., Allen, G., and Lee, A. C. (2022). Breastfeeding in a global context: epidemiology, impact, and future directions. Clin. Ther. 44, 228–244. doi: 10.1016/j.clinthera.2021.11.017
Obikane, E., Watanabe, K., Nishi, D., and Kawakami, N. (2020). Association between personal values in adolescence and impaired bonding relationship with children. BMC Psychol. 8, 98. doi: 10.1186/s40359-020-00463-9
Okagbue, H. I., Adamu, P. I., Bishop, S. A., Oguntunde, P. E., Opanuga, A. A., and Akhmetshin, E. M. (2019). Systematic review of prevalence of antepartum depression during the trimesters of pregnancy. Open Access Maced. J. Med. Sci. 7, 1555–1560. doi: 10.3889/oamjms.2019.270
Olufunlayo, T. F., Roberts, A. A., MacArthur, C., Thomas, N., Odeyemi, K. A., Price, M., et al. (2019). Improving exclusive breastfeeding in low and middle-income countries: a systematic review. Matern. Child. Nutr. 15, e12788. doi: 10.1111/mcn.12788
Pelham, B., Hardin, C., Murray, D., Shimizu, M., and Vandello, J. (2022). A truly global, non-WEIRD examination of collectivism: the Global Collectivism Index (GCI). Curr. Res. Ecol. Soc. Psychol. 3, 100030. doi: 10.1016/j.cresp.2021.100030
Pezley, L., Cares, K., Duffecy, J., Koenig, M. D., Maki, P., Odoms-Young, A., et al. (2022). Efficacy of behavioral interventions to improve maternal mental health and breastfeeding outcomes: a systematic review. Int. Breastfeed. J. 17, 67. doi: 10.1186/s13006-022-00501-9
Philipp, B. L., and Radford, A. (2006). Baby-Friendly: snappy slogan or standard of care? Arch. Dis. Child Fetal Neonatal Ed. 91, F145–F149. doi: 10.1136/adc.2005.074443
Plunkett, B. A., Mele, L., Casey, B. M., Varner, M. W., Sorokin, Y., Reddy, U. M., et al. (2021). Association of breastfeeding and child IQ score at age 5 years. Obstet. Gynecol. 137, 561–570. doi: 10.1097/AOG.0000000000004314
Rahman, A., Patel, V., Maselko, J., and Kirkwood, B. (2008). The neglected ‘m' in MCH programmes—why mental health of mothers is important for child nutrition. Trop. Med. Int. Health 13, 579–583. doi: 10.1111/j.1365-3156.2008.02036.x
Ran, M. -S., Hall, B. J., Su, T. T., Prawira, B., Breth-Petersen, M., Li, X. -H., et al. (2021). Stigma of mental illness and cultural factors in Pacific Rim region: a systematic review. BMC Psychiatry 21, 8. doi: 10.1186/s12888-020-02991-5
Reynolds, D., Hennessy, E., and Polek, E. (2014). Is breastfeeding in infancy predictive of child mental well-being and protective against obesity at 9 years of age? Child Care Health Dev. 40, 882–890. doi: 10.1111/cch.12126
Riedstra, J. P., and Aubuchon-Endsley, N. L. (2019). A moderated mediation model of maternal perinatal stress, anxiety, infant perceptions and breastfeeding. Nutrients 11, 2981. doi: 10.3390/nu11122981
Rizzo, A., Bruno, A., Torre, G., Mento, C., Pandolfo, G., Cedro, C., et al. (2022). Subthreshold psychiatric symptoms as potential predictors of postpartum depression. Health Care Women Int. 43, 129–141. doi: 10.1080/07399332.2021.1963730
Roth, M. C., Humphreys, K. L., King, L. S., Gotlib, I. H., and Robakis, T. K. (2021). Breastfeeding difficulties predict mothers' bonding with their infants from birth to age 6 months. Matern. Child Health J. 25, 777–785. doi: 10.1007/s10995-020-03036-9
Roumeliotis, S., Abd ElHafeez, S., Jager, K. J., Dekker, F. W., Stel, V. S., Pitino, A., et al. (2021). Be careful with ecological associations. Nephrology 26, 501–505. doi: 10.1111/nep.13861
Russell, P. S., Smith, D. M., Birtel, M. D., Hart, K. H., and Golding, S. E. (2022). The role of emotions and injunctive norms in breastfeeding: A systematic review and meta-analysis. Health Psychol. Rev. 16, 257–279. doi: 10.1080/17437199.2021.1893783
Saha, S., Lim, C., Cannon, D. L., Burton, L., Bremner, M., Cosgrove, P., et al. (2021). Co-morbidity between mood and anxiety disorders: a systematic review and meta-analysis. Depress. Anxiety 38, 286–306. doi: 10.1002/da.23113
Santana, G. S., Giugliani, E. R. J., de O. Vieira, T., and Vieira, G. O. (2018). Factors associated with breastfeeding maintenance for 12 months or more: a systematic review. J. Pediatr. 94, 104–122. doi: 10.1016/j.jped.2017.06.013
Scharfe, E. (2012). Maternal attachment representations and initiation and duration of breastfeeding. J. Hum. Lact. 28, 218–225. doi: 10.1177/0890334411429111
Sears, K. P. (2021). Cultural beliefs related to intimate partner violence help-seeking among African college women. J. Aggress. Maltreat. Trauma 30, 972–989. doi: 10.1080/10926771.2021.1912874
Sharma, I. K., and Byrne, A. (2016). Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia. Int. Breastfeed. J. 11, 17. doi: 10.1186/s13006-016-0076-7
Sharma, S., van Teijlingen, E., Hundley, V., Angell, C., and Simkhada, P. (2016). Dirty and 40 days in the wilderness: eliciting childbirth and postnatal cultural practices and beliefs in Nepal. BMC Pregn. Childbirth 16, 147. doi: 10.1186/s12884-016-0938-4
Simhi, M., Sarid, O., and Cwikel, J. (2019). Preferences for mental health treatment for post-partum depression among new mothers. Isr. J. Health Policy Res. 8, 84. doi: 10.1186/s13584-019-0354-0
Skouteris, H., Bailey, C., Nagle, C., Hauck, Y., Bruce, L., and Morris, H. (2017). Interventions designed to promote exclusive breastfeeding in high-income countries: a systematic review update. Breastfeed. Med. 12, 604–614. doi: 10.1089/bfm.2017.0065
Skouteris, H., Nagle, C., Fowler, M., Kent, B., Sahota, P., and Morris, H. (2014). Interventions designed to promote exclusive breastfeeding in high-income countries: a systematic review. Breastfeed. Med. 9, 113–127. doi: 10.1089/bfm.2013.0081
Slomian, J., Honvo, G., Emonts, P., Reginster, J.-Y., and Bruyere, O. (2019). Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health 15, 1–55. doi: 10.1177/1745506519844044
Spratt, E. G., Marsh, C., Wahlquist, A. E., Papa, C. E., Nietert, P. J., Brady, K. T., et al. (2016). Biologic effects of stress and bonding in mother-infant pairs. Int. J. Psychiatry Med. 51, 246–257. doi: 10.1177/0091217416652382
Steel, Z., Marnane, C., Iranpour, C., Chey, T., Jackson, J. W., Patel, V., et al. (2014). The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43, 476–493. doi: 10.1093/ije/dyu038
Stuebe, A. M., Meltzer-Brody, S., Propper, C., Pearson, B., Beiler, P., Elam, M., et al. (2019). The mood, mother, and infant study: Associations between maternal mood in pregnancy and breastfeeding outcome. Breastfeed. Med. 14, 551–559. doi: 10.1089/bfm.2019.0079
Sun, J., Zhu, Y., Li, Y., Li, N., Liu, T., Su, X., et al. (2020). Maternal postpartum feeding anxiety was associated with infant feeding practices: results from the mother-infant cohort study of China. BMC Pregn. Childbirth 20, 780. doi: 10.1186/s12884-020-03483-w
Tekeş, B., Üzümcüoglu, Y., Hoe, C., and Özkan, T. (2019). The relationship between Hofstede's cultural dimensions, Schwartz's cultural values, and obesity. Psychol. Rep. 122, 968–987. doi: 10.1177/0033294118777965
The World Bank (2020). Fertility Rate, Total (Births Per Woman). Washington, DC: The World Bank. Available online at: https://data.worldbank.org/indicator/sp.dyn.tfrt.in?most_recent_value_desc=true (accessed June 2, 2022).
The World Factbook (2019). Field Listing: Mother's Mean Age At First Birth. Washington, DC: The World Factbook. Available online at: https://www.cia.gov/the-world-factbook/field/mothers-mean-age-at-first-birth/ (accessed June 2, 2022).
Ting, L., and Panchanadeswaran, S. (2009). Barriers to help-seeking among immigrant African women survivors of partner abuse: listening to women's own voices. J. Aggress. Maltreat. Trauma 8, 817–838. doi: 10.1080/10926770903291795
Tolja, R., Nakić Radoš, S., and Andelinović, M. (2020). The role of maternal mental health, infant temperament, and couple's relationship quality for mother-infant bonding. J. Reprod. Infant Psychol. 38, 395–407. doi: 10.1080/02646838.2020.1733503
Tracz, J., and Gajewska, D. (2020). Factors influencing the duration of breastfeeding among polish women. J. Mother Child. 24, 39–46. doi: 10.34763/jmotherandchild.2020241.2006.000007
Tran, L. M., Nguyen, P. H., Naved, R. T., and Menon, P. (2020). Intimate partner violence is associated with poorer maternal mental health and breastfeeding practices in Bangladesh. Health Policy Plan. 35, i19–i29. doi: 10.1093/heapol/czaa106
UNICEF. (2018). Breastfeeding: A Mother's Gift, for Every Child. New York, NY: UNICEF. Available online at: https://data.unicef.org/resources/breastfeeding-a-mothers-gift-for-every-child/ (accessed January 16, 2023).
United Nations Development Programme (2018). Human Development Indices and Indicators: 2018 Statistical Update. New York, NY: United Nations Development Programme. Available online at: https://hdr.undp.org/en/content/human-development-indices-indicators-2018-statistical-update (accessed June 2, 2022).
Urizar, G. G., Yim, I. S., Rodriguez, A., and Schetter, C. D. (2019). The SMART moms program: a randomized trial of the impact of stress management on perceived stress and cortisol in low-income pregnant women. Psychoneuroendocrinology 104, 174–184. doi: 10.1016/j.psyneuen.2019.02.022
Van Esterik, P. (1996). The cultural context of breastfeeding and breastfeeding policy. Food Nutr. Bull. 17, 1–6. doi: 10.1177/156482659601700425
Van Sieleghem, S., Danckaerts, M., Rieken, R., Okkerse, J. M. E., de Jonge, E., Bramer, W. M., et al. (2022). Childbirth related PTSD and its association with infant outcome: a systematic review. Early Hum. Dev. 174, 105667. doi: 10.1016/j.earlhumdev.2022.105667
van Wijlen, J. E. (2019). Breastfeeding woman or lactating object? A critical philosophical discussion on the influence of Cartesian dualism on breastfeeding in the neonatal intensive care unit. J. Clin. Nurs. 28, 1022–1031. doi: 10.1111/jocn.14686
Vilar-Compte, M., Hernández-Cordero, S., Ancira-Moreno, M., Burrola-Méndez, S., Ferre-Eguiluz, I., Omaña, I., et al. (2021). Breastfeeding at the workplace: a systematic review of interventions to improve workplace environments to facilitate breastfeeding among working women. Int. J. Equity Health 20, 110. doi: 10.1186/s12939-021-01432-3
Woldeyohannes, D., Tekalegn, Y., Sahiledengle, B., Ermias, D., Ejajo, T., and Mwanri, L. (2021). Effect of postpartum depression on exclusive breast-feeding practices in sub-Saharan Africa countries: a systematic review and meta-analysis. BMC Pregn. Childbirth 21, 113. doi: 10.1186/s12884-020-03535-1
World Health Organization (2016). Mean BMI (kg/m2) (Age-Standardized Estimate). Geneva: World Health Organization. Available online at: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/mean-bmi-(kg-m-)-(age-standardized-estimate) (accessed June 2, 2022).
World Health Organization (2021). Violence Against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence Against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence Against Women. Geneva: World Health Organization.
Wouk, K., Stuebe, A. M., and Meltzer-Brody, S. (2017). Postpartum mental health and breastfeeding practices: an analysis using the 2010–2011 pregnancy risk monitoring system. Matern. Child Health J. 21, 636–647. doi: 10.1007/s10995-016-2150-6
Wren, H. M., Solomons, N. W., Chomat, A. M., Scott, M. E., and Koski, K. G. (2015). Cultural determinants of optimal breastfeeding practices among indigenous Mam-Mayan women in the western highlands of Guatemala. J. Hum. Lact. 31, 172–184. doi: 10.1177/0890334414560194
Keywords: breastfeeding, anxiety, depression, obesity, ecological analysis, culture, cultural dimension
Citation: Rajkumar RP (2023) The relationship between national cultural dimensions, maternal anxiety and depression, and national breastfeeding rates: An analysis of data from 122 countries. Front. Commun. 8:966603. doi: 10.3389/fcomm.2023.966603
Received: 11 June 2022; Accepted: 09 January 2023;
Published: 26 January 2023.
Edited by:
Dina Refki, University at Albany, United StatesReviewed by:
Kathleen Ann Kendall-Tackett, Texas Tech University Health Science Center Amarillo, United StatesOlukunmi Omobolanle Balogun, National Center for Child Health and Development (NCCHD), Japan
Copyright © 2023 Rajkumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ravi Philip Rajkumar,  cmF2aS5wc3ljaEBnbWFpbC5jb20=
cmF2aS5wc3ljaEBnbWFpbC5jb20=
 Ravi Philip Rajkumar
Ravi Philip Rajkumar