- 1Simon Business School, University of Rochester, Rochester, NY, United States
- 2Department of Communication Studies, School of Communication, University of Miami, Coral Gables, FL, United States
Introduction: Type 1 diabetes is a chronic illness requiring immense lifestyle changes to reduce the chance of life-threatening complications, which can be especially challenging during the time of transition to college. This study applies a communication design perspective to explore how students with type 1 diabetes interpret their experiences in college and what meanings they attribute to those experiences. Specifically, this study sheds light on physical and social environmental components affecting students' diabetes management.
Methods: Study participants were recruited from the College Diabetes Network (CDN). A total of twenty students with type 1 diabetes participated in the study. A qualitative descriptive study design with an ethnographic interview approach was applied.
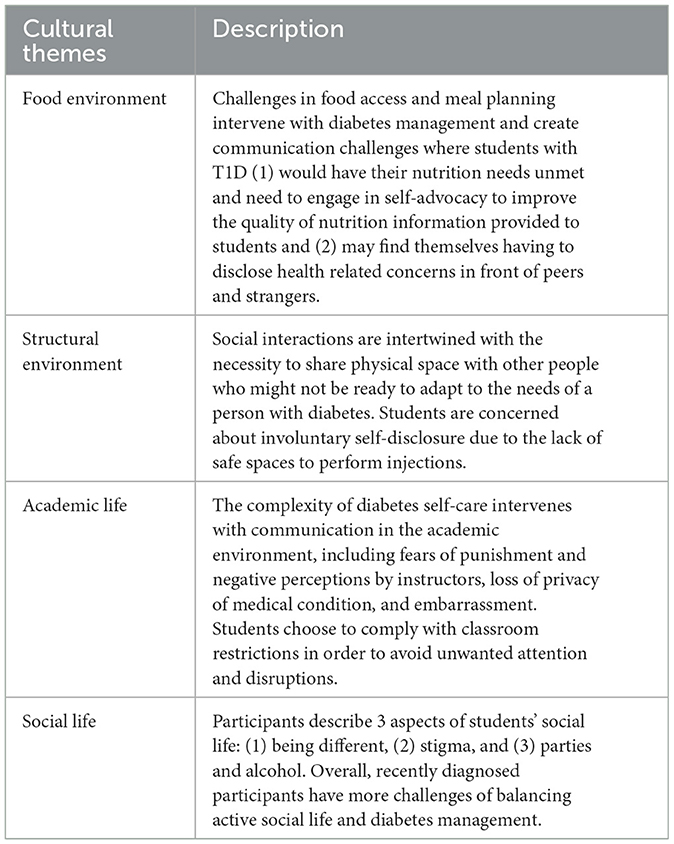
Results: Four cultural themes emerged from the analysis: (1) Food environment, (2) Structural environment, (3) Academic life, and (4) Social life. The findings illustrate how food outlets and food accessibility, safe spaces for insulin injections, comfortable living spaces, availability of health support services, and diabetes-friendly classroom regulations constitute a higher-level environmental system affecting students' wellbeing. They also highlight a complex relationship between structural barriers to diabetes management, health disclosure, and public stigma.
Discussion: Results from this study advance scholarship on diabetes care in the population of emerging adults by offering insights into how college students with T1D transition to college and manage type 1 diabetes. Overall, students with T1D have specific needs beyond those of the general student population. Thus, necessary modifications in the designs of existing structures should be introduced to facilitate students' assimilation into new organizational environments.
Introduction
Type 1 diabetes (T1D) is an invisible disability and a chronic condition typically diagnosed during childhood. It is characterized by the destruction of insulin-producing cells, which prevents the pancreas from producing insulin (Atkinson et al., 2014). Given that insulin helps the body convert glucose into energy, this condition results in extremely high glucose levels and lifelong dependency on exogenous insulin. The failure to adequately control T1D may cause chronic hyperglycemia that leads to lifetime damage and failure of body organs (Atkinson et al., 2014; Chiang et al., 2014). In 2021, there were about 8.4 million individuals worldwide with type 1 diabetes: 1.5 million (18%) were younger than 20 years, 5.4 million (64%) were aged 20–59 years, and 1.6 million (19%) were aged 60 years or older (Gregory et al., 2022). T1D requires immense lifestyle changes, including diet modification, constant blood glucose monitoring, and insulin administration, to reduce the chance of life-threatening complications (Gannoni and Shute, 2010). Longitudinal research shows that clinical and psychiatric outcomes are especially low for young adults with T1D, including the development of diabetes-related complications such as retinopathy, renal disease, and neuropathy (Bryden et al., 2003). Thus, it can be especially challenging to maintain during the time of transition (Balfe, 2009).
Emerging adulthood is a time of major transitions for most adolescents, but it brings additional challenges to those with T1D. First, while pediatric care practices a family-centered approach, adult care employs a more individualistic approach that pays less attention to the issues of social support and family involvement (Peters et al., 2011). Research shows that this transition from pediatric to adult care strongly predicts an increased risk of poor glycemic control (Helgeson et al., 2013; Lotstein et al., 2013). Specifically, this transition was associated with a 2.5-fold increase in the likelihood of maintaining poor glycemic control in young adults with T1D. Second, given the complexity of the diabetes regimen, parents are usually the most involved in helping children manage T1D (Helgeson et al., 2008). However, with the transition to college, emerging adults' social and physical environments change drastically. It can be overwhelming (Hanna, 2012) and contribute to the fact that emerging young adults remain one of the age groups with the highest hemoglobin levels and poorest diabetes control (Miller et al., 2015; Monaghan et al., 2015).
Moving out of the parental home and enrolling in a college far from home may be the first time a young adult with T1D takes responsibility for all the aspects of complex diabetes care. Thus, this period is associated with psychosocial and emotional challenges when diabetes care omissions may occur (Peters et al., 2011; Kapellen et al., 2018). Research involving emerging adults with T1D is limited in the literature, with most studies exploring the challenges of children and adolescents with T1D. Moreover, despite potential severe health risks caused by the lack of proper diabetes self-care (Balfe and Jackson, 2007), little is known about emerging adults embarking on a new higher education journey. This study applies a communication design perspective to fill the gap in research by exploring the challenges of a built and social environment that students with T1D face in college in relation to diabetes self-management.
Communication design
Design has the power to invent something that does not exist and make it appear in the real world (Nelson and Stolterman, 2003). Given that it approaches reality intending to produce a particular result and not a universal solution (Nelson and Stolterman, 2003), it is useful for initiating change, creating new things, and modifying existing ones. Thus, design is a process by which communication can be changed to make the impossible possible (Aakhus, 2007). In a sense, all people are communication designers. Every day, we design different aspects of our experienced world on an individual, group, organizational, and community levels, making choices on how and when to engage in communication (Aakhus and Jackson, 2005). Intervening in our communication, we create possibilities to change situations we do not like and move toward desired outcomes. Communication design is a special way of thinking to examine the environment, find opportunities for improvement, and redesign existing systems by applying relevant theoretical knowledge to a specific context (Harrison, 2014).
One of the most straightforward ways to engage in communication design is to shape and structure discourse (Jackson, 1998). However, it can also be applied to different levels of communication, including message design (O'Keefe, 2015), argumentation (Jacobs and Jackson, 2006), the design of work and its temporality (Ballard and McVey, 2014), interventions (Morgan et al., 2010; Harrison et al., 2011, 2020), and systems (Barbour and Gill, 2014; Real et al., 2017). While these are some examples of communication design at micro and macro levels, Barbour and Gill (2014) highlight a deficit of communication design at a system level and a critical lack of communication studies examining the influence of the built environment on individuals' health and wellness. As (Nelson and Stolterman, 2003) suggest, “imagination is not only needed as a way to create the unexpected but also in the process of interpreting the present (p. 179).” Thus, the current study interpreted the reality of college students with T1D in regard to build and social environments, diabetes self-management, and quality of life.
Built environment
Material objects in our environment provide a background in terms of what they communicate about the attitudes of various actors in the design process and the university as an organization (Rapoport, 1990). In this regard, the built environment, which is a context for all human interactions, is the focus of this study. It is often treated as invisible in communication research, but its influence can be crucial in communication within complex organizational systems and predicting individual health outcomes (Real et al., 2017). From a design perspective on human health, communication is not limited to interactions about physical health but is also intertwined with different domains of disease, such as environmental conditions that may lead to adverse health outcomes (Burns, 2014). The focus of the system on illness (pathogenesis) rather than wellness (salutogenesis) undermines attributions of people's environment, such as peer and family connections, comfortable living space, safe neighborhoods, and access to medications and insurance (Burns, 2014). Thus, people with chronic illnesses can maintain a high quality of life when the environment allows it. In contrast, improper political and economic arrangements create a form of “structural violence” (Farmer, 2004), putting people at risk and preventing them from accessing basic care that hinders individual wellbeing. Looking at systemwide changes to improve community health, built environment is one area that can be targeted. It can be broadly defined as a “human-made space in which people live, work and recreate on a day-to-day basis.” (Roof and Oleru, 2008, p. 24). Certain health threats, like mental health issues (Galea et al., 2005), have been connected to the built environment in research. Therefore, an interaction between people and their environment is a link in understanding health.
Individual health is defined by physical, mental, and social wellbeing and not simply by the absence of disease (WHO, 2020). Thus, health-related quality of life is strongly affected by psychosocial factors in addition to proper diabetes management. People with diabetes learn to deal with fluctuating blood sugar levels. However, it often takes a psychosocial toll on their quality of life as medical diabetes management (i.e., insulin treatment) is closely intertwined with physical and social environment posing additional challenges for everyday lives (Hanna, 2012). Overall, quality of life can be defined as an individual's subjective perception of physical, emotional, and social wellbeing (Rubin and Peyrot, 1999). For college students with T1D, such perceptions may be heavily affected by communication with peers, professors, admissions, student groups and so are shaped by universities as organizations that design communication (Barbour et al., 2018). As a result, the health and wellbeing of students with T1D may be affected by the college-designed environment. A college environment constitutes a system designed to provide high-quality education and safe physical and social environment without discrimination based on medical conditions. In reality, students' experiences vary based on their individual characteristics and needs (Wilson, 2010). Perceptions of students with T1D about college built and social structures may include the quality of communication with official university systems and its representatives (such as offices and policies related to disability services) and the degree to which a college environment is physically safe and comfortable for maintaining proper diabetes self-care (including food options and safe injection sites) while succeeding academically. These components constitute a university designed physical and social support system for students and are worth exploring from a communication design perspective.
RQ1: How does a perceived built environment on campus shape students' diabetes self-management and quality of life?
Social environment
Research shows that college students not only have difficulties establishing diabetes routines due to the demanding nature of college life (Balfe, 2009) but also due to the necessity of managing relationships with family members, peers, health providers, and professors (Edwards et al., 2014). Although social environment can encompass a much larger range of life aspects (e.g., Yen and Syme, 1999), in this study it is defined as relationships that students with T1D have with people, groups, and organizations in college. Although effective diabetes self-management allows people to avoid health complications and maintain a quality of life similar to those without diabetes (Atkinson et al., 2014), it shows the best results when performed in an environment rich in social capital (Helgeson et al., 2014). Relationships matter because they form an environment where people pursue their goals (Lin, 1999). From a communication standpoint, such an environment can either be an obstacle or a facilitator to the desired outcomes. In everyday lives, people provide help to each other on different levels, including practical (e.g., money borrowing), informational (e.g., news about a job-opening), and emotional (e.g., discussing problems and comforting) aid (House et al., 1988). Such access to benefits from relationships with other people and access to resources provided by them is the basis of the social capital phenomenon (Lin, 1999). The availability of social support resources and the level of their involvement differ depending on the individual's life stage. However, their presence may be particularly important during the major transition to adulthood (Hanna, 2012). Family involvement is essential to optimal diabetes care through an individual's childhood and adolescence (Chiang et al., 2014). However, relationships with parents change when adolescents approach the age of emerging adulthood. Diabetes self-management routines, such as glucose measurements, diet and exercise, and insulin administration become emerging adults' responsibilities. In contrast, other diabetes-related tasks, such as scheduling appointments and filling prescriptions, may remain under parents' control (Hanna et al., 2014).
However, with the transition to emerging adulthood and college, parents become less involved while new relationships with peers and romantic partners evolve. The existing research on the effect of T1D on relationships with peers and romantic partners showed that emerging adults with T1D had less support from friends than those without T1D (Helgeson et al., 2015). Moreover, some individuals with T1D experience trouble maintaining proper diabetes care in social contexts because they anticipate peer pressure and are afraid to become socially isolated (Wysocki et al., 2001). In addition, peers and professors may feel uncomfortable seeing students with T1D performing diabetes care. For example, some professors use a risk of infection by bloodborne pathogens as an excuse to restrict classroom blood glucose testing (Gordon et al., 2011). Lastly, avoidance of diabetes self-management may occur when students with T1D cannot come to terms with the disease that separates them from their peers. Social contexts that call for activities congruent with peer acceptance but violate the norms of diabetes care, such as excessive alcohol use, may result in avoidance of diabetes care due to shame (Turland, 2016). Thus, the following research question explores students' perspectives on a college social environment.
RQ2: How does a social environment on campus shape students' diabetes self-management and quality of life?
In sum, this research aims not to provide a universal account of the college system regarding students with T1D but rather to identify specific elements of the system's design that pose communication challenges and affect students' diabetes management and wellbeing.
Method
Participants
Study participants were recruited from the College Diabetes Network (CDN). The CDN is a non-profit organization helping young adults with T1D with their life-changing transition to college by building social capital and resource platforms and seeking to achieve positive health outcomes through information sharing, resources, and social support. The inclusion criteria for this study were (1) diagnosed with T1D, (2) an emerging adult (age of 18–25 years), and (3) a student residing on campus or living independently/with roommates. A total of twenty students with T1D participated in the study. The participants reported age ranged from 19 to 25 years. The reported time with diabetes ranged from 8 months to 16 years. Most participants self-identified as female (n = 17), followed by male (n = 2) and transgender female (n = 1). All participants were from different areas of the United States. Regarding ethnicity, most participants self-identified as White (n = 16), followed by Hispanic (n = 2), Black (n = 1), and Indian American (n = 1). Most participants were sophomores (n = 8), followed by juniors (n = 6), seniors (3), freshmen (n = 2), and graduate students (n = 1).
Procedures
A qualitative descriptive study design with an ethnographic interview approach (Spradley, 1979) was employed to explore how students with T1D interpreted their experiences in college and what meanings they attributed to those experiences.
The interview guide for this study was developed based on Spradley (1979) directions on conducting ethnographic interviews. Several types of questions were used to elicit information. First, by expressing cultural ignorance, the researcher placed themself in the position of acknowledging the population of students with T1D but not knowing what their lives were like. Next, descriptive questions were a big part of the interview. For example, “Being a student and living on campus, you interact with different people daily. I am interested in learning more about how to talk to people about diabetes.” They also included a special kind of descriptive question, called “grand tour,” expanding on the basic questions and giving the informant time to prepare the answer. For example, “Could you start at the beginning of a day. Your typical day in college. And describe to me what goes on in terms of your student life and diabetes routine?” Lastly, the interviewer introduced structural questions by restating the list of things mentioned by the informant that created a certain domain. As Spradley (1979) explains, “any symbolic category that includes other categories is a domain (p. 100)”. All the terms of a domain share at least one feature of meaning. The goal is to look for existing similarities that help us form a certain category, which we call a “domain”. Researchers aimed to elicit a full list of the terms in each domain, so the question sequence started with a verification question. Then, after the informant agreed, the structural question was introduced (Spradley, 1979, p. 121). For example, “I am interested in getting a list of all such places/structures. You have mentioned several things you have experienced (repeating things the participant mentioned). Would you say that these are all the challenges of the college environment that intervene with your diabetes routine? Can you think of any other things?” All interviews were conducted online via Zoom. The average time for completing the interview was 52 min (42–75 range).
Analysis
Interview video recordings and audio transcripts were uploaded into NVivo for coding and analysis. The analysis started by identifying semantic relationships and the number of domains. First, transcribed interviews were examined for terms that have a semantic relationship to develop domains—categories of cultural meanings. As Spradley (1979) explains, it means “to read with a question in mind: ‘Which terms could be a kind of something?' (p. 114)”. For example, a domain “being different” would consist of terms like “less social,” “quiet,” “hide,” and “embarrassing.” Next, larger cultural themes recurrent in several domains were identified to present a holistic view of a cultural scene. A useful strategy for developing cultural themes is to select an organizing domain for intensive analysis (Spradley, 1979, p. 197). Thus, the domain coded in NVivo as “stages in a typical day” was selected as a major organizing domain and examined in relation to others. This stage aims to identify the elements that constitute culture and describe what members believe and recognize as real. This process also takes the qualitative inquiry beyond single-level analysis by identifying specific conditions under which the experiences occur and linking them to larger socio-cultural realms (Spradley, 1979, p. 189). In sum, the analysis explored: (1) the components of a culture, (2) the relationship among components, and (3) the relationship of the components to a larger cultural system (Spradley, 1979, p. 189).
Results
Research questions 1 and 2 explored how the roles of the built and social environment on campus impact students with T1D. The interviews yielded insights into the college environment's role in T1D self-management in different life areas reflected by four cultural themes: (1) Food environment, (2) Structural environment, (3) Academic life, and (4) Social life (see Table 1).
Food environment
This cultural theme addressed how the built environment of campus food services (social challenges related to food are reported in a later section) could affect the quality of diabetes self-care and quality of life. Students reported that each of these cause challenges for health, anxiety, and wellbeing, and created communicative challenges around advocacy as well. The food environment label here mainly refers to food access and communication of nutrition information.
Overall, the major reason for frustration was feeling overwhelmed by meal planning. This included preparing meals independently, eating at dining halls, and planning grocery shopping ahead of time. The “school-diabetes balance” challenge and “lack of control over a diet” were mentioned by 13 participants. Specifically, those living off campus dealt with major challenges during the adaptation period.
Food is definitely a challenge when I was learning to navigate my schedule and grocery shopping. Sometimes I just would not have time and kind of running out of food, just putting butter and jelly for four days in a row till you have time to get to the grocery store.
For newly diagnosed students, it was harder to remember to always carry food for snacking and other supplies. As one participant noted, “I know it should be like an instinct, but sometimes it is difficult because I forget it. It is a human error. It happens.” The analysis shows that the built environment on campus hinders the process of meal planning in three specific ways which created communication challenges negatively affected students' psychological states. First, a total of 13 students reported finding healthy options, “so it is not all carbs all the time”, was a challenge. Students living on campus heavily relied on the services provided by the university even more and were limited in their choices. As Jenna (age 21; sophomore) states: “I do live on campus, so I don't really have access to a kitchen or pots and pans and stuff like that to make my own food.”
Second, eight participants living on campus reported frustration in regard to dining halls' hours of operation, including “closing at random times in the afternoon”. For example, Andrea (age 18; freshman), diagnosed with T1D at the age of 5 and being “one hundred percent on top of diabetes” before enrolling in college, noted that “small organizational moments cause some real troubles:”
I eat at the dining halls, so that was a struggle for me because the dining halls opened up at 8:30 am maybe, and the first class is 8:50 am. There is no time to go, so you have to kind of have breakfast in a dorm room.
Similarly, other students who were “at the mercy of dining halls hours”, reported adjusting their schedule to accommodate mealtimes (n = 7). Given that T1D self-care routine requires an immense amount of planning, the worry about meal planning was described by participants as “additional anxiety”.
Third, 11 participants living on campus voiced concern over the lack of nutrition information or incorrect nutrition information communicated to the students in the dining halls, which was described as “frustrating” and as Bruce (age 19; sophomore) noted, “having to fend for myself for a whole year, I did not feel like I was able to eat as healthy as I would have wanted to”. The same sentiment was echoed by Rose (age 21; junior).
One of the biggest things for me was my first year and eating in the dining halls. I found they would have nutrition facts, but then it did not match my intuition, so I ended up estimating a lot. I tried to advocate a little bit for them to fix the errors, but really it came down to me bringing measuring cups to the dining hall to figure it out.
In sum, these environmental elements not only intervene with diabetes management but also create communication challenges where students with T1D (1) would have their nutrition needs unmet and need to engage in self-advocacy to improve the quality of nutrition information provided to students and (2) may find themselves having to disclose health related concerns in front of peers and strangers.
Structural environment
This cultural theme addressed how specific elements in the physical space of campus could affect the quality of diabetes self-care and quality of life. The structural environment here is broadly defined as a physical space where students live, study, and interact.
First, participant responses highlighted the influence of living space on communication with roommates. Living in the dorm, they had a fear of “waking everyone up with alarms going off”. For this reason, many (n = 11) tend to turn their continuous glucose monitor alarms off, which creates dangerous health situations.
Joy (age 19; freshman): I think my roommate just did not realize what he was getting into, I mean, living with someone with diabetes. I think that is a very challenging dynamic. As someone with diabetes, you get annoyed by the alarm, so how do you think your roommate feels? But there is nothing you can really do about that. That kind of caused some friction between us because I would feel like she was not sympathetic enough of what I was going through.
The social interaction here is intertwined with the necessity to share physical space with other people who might not be ready to adapt to the needs of a person with diabetes. Thus, students feel more comfortable living with someone who also has diabetes and similar experience managing it. Students who were “matched up” to live with other students with diabetes felt less pressure to not disrupt other peoples' routines.
Second, participants (n = 7) shared concerns about involuntary self-disclosure due to the lack of physical and emotionally safe spaces to perform injections. The lack of these spaces was perceived as not only a threat to their physical health, but a source of stigma that influenced relationships with peers. Amanda (age 22; senior) provides the following example: “When I was on syringes (…), it is really difficult to find places where people don't stare at me.”
Staying in control of diabetes was salient to all participants, and they tried to overcome the stigma related comments and “sidelong glances”. However, 5 respondents shared that they were concerned about bothering people and receiving “dumb jokes about shooting heroin”.
Amely (age 21; junior): I got some really awful stares from giving myself a shot. I would usually do it in the car before going inside, so that people wouldn't look at me and then like in the bathroom, and there is usually no really space for that unless you do it at the sinks. And there is plenty of people that think of doing drugs, and they will see the needles in my bag and be very scared.
The adverse effect of such a situation on diabetes management was also reported by Emma (age 23; senior).
I usually go to the bathroom to inject [insulin]. It is not the most sterile area if you do it in the bathroom, so that is kind of frustrating, but it is better than being stared at by people and asked weird questions. Sometimes I try to avoid it, so I will just wait till I get back to my room to do it. It does affect my health, I know.
The physical environment of a campus impacted students' self-care and communication with peers. However, those who use insulin pumps report less concern, while all students on insulin injections vocalize frustration from the stigmatization of needle use in public spaces. Similarly, the following sections highlight the intersection between physical space (e.g., classroom), health outcomes, and peer communication, including health disclosure.
Academic Life
This cultural theme described the intersection between academic life and the quality of diabetes self-care and quality of life. It taps into the challenges around classroom regulation, classroom disruptions, and communication with professors. According to study participants, when one's blood sugar is high, it feels “like flu”, and the brain is “foggy”. Similarly, when blood sugar goes low, students (n = 11) reported feeling “shaky and miserable” and reported having to “step out and be outside for a while and miss a part of what is going on” as a major limitation. Sam (age 18; freshman) describes it like this: “When I have to leave to either go get candy from the vending machines or go to the bathroom to administer insulin, it can definitely chip away from my experience in class.”
In terms of lectures and tests, students unanimously reported being concerned about an impaired class experience that also partly depended on classroom regulations. Despite the steps that students took to effectively communicate with professors, they only had a limited ability to control classroom regulations. For example, the rules of an engineering lab prevented Carol (age 22; senior) from bringing food and water to class.
It's hard to just get up and leave sometimes. I would illegally sneak sugar in the class. I was always really nervous that the professor would call me out, and I would have to say it was for medical purposes.
In addition, all respondents shared that they were concerned with creating classroom disruptions. The worry of the pump making loud noises and the fear of being accused of the phone going off was reported by all but one participant. Betty (age 21; senior) provides describes her experience as following:
During classes, especially in lectures, this is always a concern that professors do not know that [the ringer] is your insulin pump or your blood sugar, so they usually say something to the class, and that is never really fun to deal with and be like, “oh, that was me, I'm not answering a phone call or anything.” So that is definitely something to kind of navigate. I have always been really open about my diabetes, but people who are quieter or just do not want to disclose can sometimes be forced to in such situations.
Participants (n = 9) described situations when everybody in the room turns around, trying to figure out where the noise is coming from as “stressful” and “embarrassing”.
Bruce (age 19; sophomore): Having proctored exams where you cannot have your phones is really, really difficult. I get anxiety just thinking about it because so much of my diabetes care involves my phone, and the people that are proctoring the exams are not necessarily the professors that I have spoken to about diabetes.
Lastly, while most participants did not report any problems regarding communication with professors about T1D, 3 of them acknowledged the lack of understanding about students' health needs. Specifically, participants mentioned professors' unwillingness to provide additional time during exams or to postpone exams. Although students with T1D are eligible to request such accommodations, students like Rachel (age 18; freshman) feared “making a fuss over it because that brings even more attention. It means I cannot do everything everybody else can do”. To comply with classroom restrictions and in an attempt to avoid unwanted attention, students reported “regularly putting insulin pump on silent so it will not go off in lectures” and “ignoring low and high blood sugar in class”.
Rachel (age 18; freshman): As much as professors will be like, “oh no, eat when you need to and everything,” your peers are looking at you like, “why can she eat, and I can't.” I will try to suppress it long enough because I do not really want to call attention to it, but I do not really have a choice.
Feeling uncomfortable eating in class and avoiding “embarrassing” situations with loud beeps, students reported turning insulin pumps off while admitting that high blood sugar takes a long time to fix and might have a negative long-term effect on their health.
In sum, the complexity of diabetes self-care intervened with communication in the academic environment, including fears of punishment and negative perceptions by instructors, loss of privacy of medical condition, and embarrassment. Overall, the analysis of this cultural theme shows an intertwinement of diabetes self-management routine, academic life, and social interactions. Socially uncomfortable situations can be triggered, and academic experiences can be affected by diabetes care necessity.
Social life
Participants described the intersection between social life and the quality of diabetes self-care and quality of life. Theme 4 covered 3 aspects of students' social life: (1) being different, (2) stigma, and (3) parties and alcohol.
Being different
It was reported that participants' social life and personal relationships in college were also affected by diabetes. Participants (n = 17) described the disadvantages they faced from being a college student with T1D. For example, blood sugar fluctuations were reported to cause disruptions in social settings by “making everyone around you stop what they are doing to find you something to eat because you forgot something”. Similarly, half of students reported ignoring beeping noise from their pumps when they hung out with friends because they did not want to leave to change it. In addition to “doing a lot of math every time I eat”, students acknowledged the challenges of social eating scenarios. Nina (age 19; sophomore) shares her experience: “You are making friends, but then you are at meals, and you have to check your blood sugar under the table. It is hard to navigate by trying to be social.” Also, students described plenty of social situations when they “have eaten something that they really should not have eaten at that point” because they did not want to draw attention to their special needs. Recently diagnosed participants were particularly sensitive to the issues of being “different”. Moreover, some participants' experiences, for example Amy's (age 19; sophomore), were marked by the perception that peers discouraged them from performing diabetes by labeling people with T1D as “less social” and “quiet”.
There are times when everybody is like, “let's go here right now,” and I am like, “wait, I have to test my blood sugar first,” or “I have to change my pump again.” Then everybody is sitting there waiting for me, which is not the most comfortable feeling. It is just I am different. I have to keep thinking about it.
In addition, 4 participants shared life situations when it was difficult “to look professional” because of diabetes. Kelly (age 21; junior) provided a vivid example.
There was one point where my insulin pump, I had my sensor attached to it, was going off because of some sort of sensor error. I was wearing a dress, so I had to get my insulin pump out, acknowledge it, and put it back in my dress. And then, at one point, my professor called on me, and I had to stand up, and I have my pump just like dangling everywhere. It was an embarrassing moment.
Overall, recently diagnosed participants were more sensitive to the issues of being different and found many social and classroom interactions embarrassing. In contrast, students with longer diabetes care experience perceived less pressure and embraced diabetes as a part of their personal identity.
Stigma
Another concern grew out of the fear that “people would not understand”. All participants acknowledged the challenges related to lack of knowledge in the general population on what T1D really is, how it develops and affects the human body, and how it differs from type 2 diabetes. Brianna (age 18; freshman) provided a social stigma example: “when people think of diabetes, and they think of Black people, they automatically assume it's type 2 diabetes and not type 1 diabetes”. Additionally, Brianna reported that most people mix type 1 and type 2 diabetes, which causes misunderstandings and frustration.
I was trying to communicate to people so many times that it is not really my fault that I got type 1 diabetes. It was just that one day my pancreas decided wanting to stop creating insulin.
Other typical messages received by participants from random people in their environment included comments about “taking drugs in the middle of campus,” “eating too many calories,” and “not looking diabetic”.
Parties and alcohol
Participants (n = 9) acknowledged the challenges related to social events. Given that college life is strongly associated with parties and alcohol, many recognized that they had to “take it into their own hands to have good judgment in those scenarios”. Specifically, students needed to know their alcohol limits and when they were supposed to eat and administer insulin. However, half of participants reported struggling with self-control and admitted poor diabetes control when drinking.
Mark (age 22; senior): After a party, I set a temporary basal rate before going to sleep, but I looked at my graph the next morning, and it plummeted for a couple hours and then just miraculously stopped at 100. That could have gone badly. It convinced me that I should not drink a lot because I do not like how I feel the next day, and I do not like what it does to me. I think it is too big of a risk.
All participants acknowledged that scenarios involving alcohol can quickly become dangerous for a person with diabetes, and it is “something that people do not really know or understand”. Specifically, participants described frustration as related to “people's willingness to leave you behind because of your disability and because you are different.” For example, participants experienced pressure to drink at a party and, when refused and explained that they were “high risk”, were labeled by their peers as “not fun”.
Clearly, the importance of social events in college came with an additional burden for students with diabetes. Those who do not consume alcohol and feel confident telling people about it have fewer concerns about public perceptions. In contrast, students who struggle with self-regulation, party a lot, and try to “fit in”, face life-threatening challenges related to extensive alcohol consumption.
Discussion
This study interpreted the reality of college students with T1D and linked it to the built and social environment on campus, diabetes self-management, and quality of life. Previous limited research shows that students with T1D face certain challenges in the college built environment, including the need for extra time between classes or during exams to check glucose levels (Balfe and Jackson, 2007), allowance of food and drink in classrooms (Saylor et al., 2019), challenges of navigating college campuses, and obtaining healthy food (Fredette et al., 2016; Saylor et al., 2019). The current study results extend this knowledge and highlight the complexity of communication in higher education organizations. They illustrate how an ineffectively designed built environment can be intertwined with health stigma, social interactions, and a reduced sense of belonging. The complexity and permanence of diabetes self-care make it invasive into every aspect of students' lives. For example, the results showed that the need to perform insulin injections and the inability to always predict the timing is connected to the absence of a comfortable and hygienic place on campus. Moreover, it may lead to forced self-disclosure when people in public spaces notice students performing diabetes self-care and ask questions. Similarly, sharing a living space with someone unfamiliar with T1D specifics might create a challenging social dynamic for roommates and adversely affect diabetes management and organizational assimilation.
Results from this study advance scholarship on diabetes care in the population of emerging adults by offering insight into how college students with T1D transition to college and assimilate to a new environment. Specifically, this research illustrates that food outlets and accessibility, safe spaces for insulin injections, comfortable living spaces, and diabetes-friendly classroom regulations constitute a higher-level environmental system affecting students' wellbeing. For example, it has been previously highlighted that environment plays an important role in influencing one's dietary patterns (Story et al., 2008). However, for students with T1D, the lack of healthy food options and incorrect nutrition information in dining halls leads to (1) the food routine not matching their diabetes treatment plans and (2) the necessity to self-advocate and disclose health information. Another prominent example is how the built environment of universities often challenges students' insulin administration. Relying on public spaces such as restrooms poses physical contamination threats and increases the stigma of using needles in public spaces. Also, official classroom regulations and university policies pose additional barriers to students' diabetes care. For example, the reliance on technology for diabetes management is often compromised during examinations and in lab settings when students are reluctant to draw attention to their special needs and refrain from communicating their concerns to professors.
Students with T1D often perceive their health condition as disrupting their higher education. Previous research has shown that emerging adults with chronic illnesses struggle to disclose their diagnosis to peers, which leads to social isolation and “abnormal” (Abbott et al., 2008). As a result, emerging adults report high levels of social anxiety (Pinquart and Shen, 2011) and lower levels of life satisfaction and purpose than those without diabetes (Palladino et al., 2013). Desiring to be “normal”, emerging adults with T1D may withhold their diagnosis from others (Habenicht et al., 2021), with the lack of public understanding and fear of being treated differently (Dovey-Pearce et al., 2007) among the major reasons of non-disclosure. This study's results are consistent with and are an extension of research on diabetes-related stigma (Browne et al., 2014) and academic life (Saylor et al., 2019) in the T1D context. Each of the previously described themes comes with specific diabetes-related concerns and adjustments. However, the findings show an overlap between domains. For example, there is a complex relationship between structural barriers to diabetes management on campus, issues of self-disclosure, and public stigma. Future studies should specifically examine diabetes-related self-disclosure in a college setting, where students regularly make choices of disclosure/nondisclosure in classrooms, dorms, and during social events.
In the literature, disability culture is described as a “thriving concept and lived experience in the hearts and minds of many disabled people” (Peters, 2000, p. 584). A unique cultural identity of people living with disabilities, including T1D, has been addressed in the literature, along with the notion of invisible disability, an illness that is not immediately visible, and its impact on relationships and daily lives. In line with previous research, this study findings indicate that students who had had diabetes for many years perceive diabetes as an important part of their identity and feel comfortable disclosing it to other people. In contrast, recently diagnosed participants were particularly sensitive to the issues of being “different”. The preconceived notions that the lay public may hold about T1D and the general lack of understanding of how T1D develops and differs from type 2 diabetes contribute to the stigmatization of illness. In addition, there may be substantial variation in how the lay public views diabetes as an easily controllable disease. As a result, students may feel anxious and uneasy when others' perceptions of control do not correspond with their own.
In sum, students with T1D have specific needs beyond those of the general student population. Thus, necessary modifications in the designs of existing structures should be introduced to facilitate students' assimilation into new organizational environments.
Practical implications and recommendations
A systematic review of interventions to improve outcomes for young adults with T1D (O'Hara et al., 2017) shows a critical need for more high-quality, well-designed interventions to improve young adults' health outcomes. The current analysis of the structural system surrounding students with T1D on campus can inform the design of interventions to address existing constraints. Guided by the communication design approach (Harrison, 2014), future interventions should focus on empowering students to (1) request necessary accommodations, (2) plan for contingencies, (3) take advantage of university services, (4) seek emotional support, and (5) engage in self-advocacy. In addition, there are several possibilities for improving college system design on a higher organizational and policy level. Therefore, college authorities should address previously discussed issues by (1) improving food services on campus, (2) accommodating students' requests regarding living space and classroom regulations, and (3) creating a support system on campus. Lastly, it is important to acknowledge that universities are complex systems embedded in broader designed systems. On a larger scale, the obtained knowledge should be used to create an official college transition system for students with T1D to help them stay in control of disease and successfully adapt to a college environment.
Limitations and future research
This study has several limitations. First, the employed approach does not involve methodological triangulation (Morse, 1991) and cannot specify how the college environment predicts students' diabetes management. Second, convenience sampling was used to recruit participants in the study. Thus, the results may only partially reflect the experiences of all college students living with T1D. Third, the lack of demographic diversity in this research is a limitation. Although some representation of ethnic minority groups and male participants was present, the collected data was skewed toward the experiences of White female students and cannot necessarily be extrapolated to the larger population of ethnic minority and male students diagnosed with T1D. One of the major challenges in this research was recruiting minority young adults, who currently represent the largest growing population with T1D (Mayer-Davis et al., 2017) but rarely participate in research. Collaboration with CDN on participant recruitment was essential in accessing this hard-to-reach population, and all efforts have been made to diversify the pool of participants. For example, the CDN administration sent out multiple additional calls for minority students with T1D promoted via monthly newsletters and social media platforms. Recruiting people with disabilities to serve as both participants and decision-makers should be done by future studies to address systemic inequities in health and organizational settings.
Conclusions
In this study, we apply a communication design approach to identify specific elements of the built and social environment that affect diabetes management and wellbeing of young adults with type 1 diabetes. These findings not only contribute to the limited body of research on this topic but can also help initiate organizational change as they (1) highlight an interplay between the built environment and supportive organizational communication during major life transitions in a chronic illness context and (2) can be used to increase patients' adherence to diabetes treatment, which can be a challenging process for young adults with chronic health conditions. This study findings advance scholarship on diabetes care in the population of emerging adults by offering insight into how college students with T1D transition to college and adapt to a new environment. Specifically, this research illustrates that food outlets and food accessibility, safe spaces for insulin injections, comfortable living spaces, availability of health support services, and diabetes-friendly classroom regulations constitute a higher-level environmental system affecting students' wellbeing. It also highlights a complex relationship between structural barriers to diabetes management, health disclosure, and public stigma. The communication design approach addresses situations where standard communication practices lack efficiency due to environmental constraints (e.g., Harrison, 2014; Real et al., 2017). Thus, the current study provides narrative accounts that voice the specific needs of a vulnerable population and offer a blueprint for future interventions to improve students' diabetes management and quality of life.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Miami IRB. The participants' oral informed consent for participation in the study was documented in the video recordings.
Author contributions
EM and TH: conceptualization of the study and data analysis. EM: data collection and writing. TH: editing. All authors contributed to the article and approved the submitted version.
Funding
This project was partially funded by the School of Communication (Dissertation Award), University of Miami.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aakhus, M. (2007). Communication as design. Commun. Monogr. 74, 112–117. doi: 10.1080/03637750701196383
Aakhus, M., and Jackson, S. (2005). Technology, Interaction, and Design. Handbook of Language and Social Interaction, 411–436. Available online at: https://books.google.com/books?hl=en&lr=&id=uwdREjcZ07cC&oi=fnd&pg=PA411&dq=Aakhus+%26+Jackson,+2005&ots=0nA6lLbts1&sig=7R40S1IGSQof69_dhy5-JHeMLOc (accessed April, 2020).
Abbott, S., Cairns, L., and Davies, H. (2008). Empowering young people with long-term illness. Paediatr. Nurs. 20, 35–37. doi: 10.7748/paed.20.4.35.s25
Atkinson, M. A., Eisenbarth, G. S., and Michels, A. W. (2014). Type 1 diabetes. Lancet 383, 69–82. doi: 10.1016/S0140-6736(13)60591-7
Balfe, M. (2009). Healthcare routines of university students with Type 1 diabetes. J. Adv. Nurs. 65, 2367–2375. doi: 10.1111/j.1365-2648.2009.05098.x
Balfe, M., and Jackson, P. (2007). Technologies, diabetes and the student body. Health Place 13, 775–787. doi: 10.1016/j.healthplace.2007.01.001
Ballard, D. I., and McVey, T. (2014). Measure twice, cut once: the temporality of communication design. J. Appl. Commun. Res. 42, 190–207. doi: 10.1080/00909882.2013.874571
Barbour, J. B., and Gill, R. (2014). Designing communication for the day-to-day safety oversight of nuclear power plants. J. Appl. Commun. Res. 42, 168–189. doi: 10.1080/00909882.2013.859291
Barbour, J. B., Gill, R., and Barge, J. K. (2018). Organizational communication design logics: a theory of communicative intervention and collective communication design. Commun. Theory 28, 332–353. doi: 10.1093/ct/qtx005
Browne, J. L., Ventura, A., Mosely, K., and Speight, J. (2014). “I”m not a druggie, I'm just a diabetic': a qualitative study of stigma from the perspective of adults with type 1 diabetes. BMJ Open 4, e005625. doi: 10.1136/bmjopen-2014-005625
Bryden, K. S., Dunger, D. B., Mayou, R. A., Peveler, R. C., and Neil, H. A. W. (2003). Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care 26, 1052–1057. doi: 10.2337/diacare.26.4.1052
Burns, H. (2014). What causes health? J. R. Coll. Phys. Edinb. 44, 103–105. doi: 10.4997/JRCPE.2014.202
Chiang, J. L., Kirkman, M. S., Laffel, L. M. B., Peters, A. L., and Type 1 Diabetes Sourcebook Authors (2014). Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care 37, 2034–2054. doi: 10.2337/dc14-1140
Dovey-Pearce, G., Doherty, Y., and May, C. (2007). The influence of diabetes upon adolescent and young adult development: a qualitative study. Br. J. Health Psychol. 12 (Pt 1), 75–91. doi: 10.1348/135910706X98317
Edwards, D., Noyes, J., Lowes, L., Haf Spencer, L., and Gregory, J. W. (2014). An ongoing struggle: a mixed-method systematic review of interventions, barriers and facilitators to achieving optimal self-care by children and young people with type 1 diabetes in educational settings. BMC Pediatr. 14, 228. doi: 10.1186/1471-2431-14-228
Farmer, P. (2004). An anthropology of structural violence. Curr. Anthropol. 45, 305–325. doi: 10.1086/382250
Fredette, J., Mawn, B., Hood, K., and Fain, J. (2016). Quality of life of college students living with type 1 diabetes: a qualitative view. West J. Nurs. Res. 38, 1595–1610. doi: 10.1177/0193945916651265
Galea, S., Freudenberg, N., and Vlahov, D. (2005). Cities and population health. Soc. Sci. Med. 60, 1017–1033.
Gannoni, A. F., and Shute, R. H. (2010). Parental and child perspectives on adaptation to childhood chronic illness: a qualitative study. Clin. Child Psychol. Psychiatry 15, 39–53. doi: 10.1177/1359104509338432
Gordon, K., Rapp, J. A., Dimmick, B. L., and Jackson, C. (2011). Going to College with Diabetes: A Self Advocacy Guide for Students. Denver, CO: American Diabetes Association. Available online at: https://www.herpmed.com/main/dorg/living-with-diabetes/edmats-lawyers/going-to-college-with-diabetes.pdf (accessed April, 2020).
Gregory, G. A., Robinson, T. I. G., Linklater, S. E., Wang, F., Colagiuri, S., de Beaufort, C., et al. (2022). Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diab. Endocrinol. 10, 741–760. doi: 10.1016/S2213-8587(22)00218-2
Habenicht, A. E., Gallagher, S., O'Keeffe, M.-C., and Creaven, A.-M. (2021). Making the leap and finding your feet: a qualitative study of disclosure and social support in university students with type 1 diabetes. J. Health Psychol. 26, 260–269. doi: 10.1177/1359105318810875
Hanna, K. M. (2012). A framework for the youth with type 1 diabetes during the emerging adulthood transition. Nurs. Outlook 60, 401–410. doi: 10.1016/j.outlook.2011.10.005
Hanna, K. M., Weaver, M. T., Stump, T. E., Guthrie, D., and Oruche, U. M. (2014). Emerging adults with type 1 diabetes during the first year post-high school: perceptions of parental behaviors. Emerg. Adulth. 2, 128–137. doi: 10.1177/2167696813512621
Harrison, T. R. (2014). Enhancing communication interventions and evaluations through communication design. J. Appl. Commun. Res. 42, 135–149. doi: 10.1080/00909882.2013.825047
Harrison, T. R., Morgan, S. E., King, A. J., and Williams, E. A. (2011). Saving lives branch by branch: the effectiveness of driver licensing bureau campaigns to promote organ donor registry sign-ups to African Americans in Michigan. J. Health Commun. 16, 805–819. doi: 10.1080/10810730.2011.552001
Harrison, T. R., Williams, E. A., and Reynolds, A. R. (2020). “The intersections of organizations, health, and safety: designing communication for high reliability organizations,” in The Handbook of Applied Communication Research, eds H. Dan O'Hair, M. John O'Hair (John Wiley & Sons, Inc), 279–296. doi: 10.1002/9781119399926.ch17
Helgeson, V. S., Mascatelli, K., Reynolds, K. A., Becker, D., Escobar, O., and Siminerio, L. (2015). Friendship and romantic relationships among emerging adults with and without type 1 diabetes. J. Pediatr. Psychol. 40, 359–372. doi: 10.1093/jpepsy/jsu069
Helgeson, V. S., Palladino, D. K., Reynolds, K. A., Becker, D. J., Escobar, O., and Siminerio, L. (2014). Relationships and health among emerging adults with and without Type 1 diabetes. Health Psychol. 33, 1125–1133. doi: 10.1037/a0033511
Helgeson, V. S., Reynolds, K. A., Siminerio, L., Escobar, O., and Becker, D. (2008). Parent and adolescent distribution of responsibility for diabetes self-care: links to health outcomes. J. Pediatr. Psychol. 33, 497–508. doi: 10.1093/jpepsy/jsm081
Helgeson, V. S., Reynolds, K. A., Snyder, P. R., Palladino, D. K., Becker, D. J., Siminerio, L., et al. (2013). Characterizing the transition from paediatric to adult care among emerging adults with Type 1 diabetes. Diabet. Med. 30, 610–615. doi: 10.1111/dme.12067
House, J. S., Umberson, D., and Landis, K. R. (1988). Structures and processes of social support. Annu. Rev. Sociol. 14, 293–318. doi: 10.1146/annurev.so.14.080188.001453
Jacobs, S., and Jackson, S. (2006). Derailments of Argumentation: It Takes Two to Tango. Considering Pragma-Dialectics, 121–133. Available online at: https://books.google.com/books?hl=en&lr=&id=QGOPAgAAQBAJ&oi=fnd&pg=PA121&dq=jacobs+jackson+argument+2006&ots=GQkMKhaUeF&sig=cPbY50kTxWTEWGy71cT9IoRw7og (accessed April, 2020).
Kapellen, T. M., Müther, S., Schwandt, A., Grulich-Henn, J., Schenk, B., Schwab, K. O., et al. (2018). Transition to adult diabetes care in Germany—High risk for acute complications and declining metabolic control during the transition phase. Pediatr. Diabetes 19, 1094–1099. doi: 10.1111/pedi.12687
Lotstein, D. S., Seid, M., Klingensmith, G., Case, D., Lawrence, J. M., Pihoker, C., et al. (2013). Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 131, e1062–e1070. doi: 10.1542/peds.2012-1450
Mayer-Davis, E. J., Lawrence, J. M., Dabelea, D., Divers, J., Isom, S., Dolan, L., et al. (2017). Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N. Engl. J. Med. 376, 1419–1429. doi: 10.1056/NEJMoa1610187
Miller, K. M., Foster, N. C., Beck, R. W., Bergenstal, R. M., DuBose, S. N., DiMeglio, L. A., et al. (2015). Current state of type 1 diabetes treatment in the US: updated data from the T1D Exchange clinic registry. Diabetes Care 38, 971–978. doi: 10.2337/dc15-0078
Monaghan, M., Helgeson, V., and Wiebe, D. (2015). Type 1 diabetes in young adulthood. Curr. Diabetes Rev. 11, 239–250. doi: 10.2174/1573399811666150421114957
Morgan, S. E., Harrison, T. R., Chewning, L. V., DiCorcia, M. J., and Davis, L. A. (2010). The effectiveness of high- and low-intensity worksite campaigns to promote organ donation: the workplace partnership for life. Commun. Monogr. 77, 341–356. doi: 10.1080/03637751.2010.495948
Morse, J. M. (1991). Approaches to qualitative-quantitative methodological triangulation. Nurs. Res. 40, 120–123. doi: 10.1097/00006199-199103000-00014
O'Hara, M. C., Hynes, L., O'Donnell, M., Nery, N., Byrne, M., Heller, S. R., et al. (2017). A systematic review of interventions to improve outcomes for young adults with Type 1 diabetes. Diabet. Med. 34, 753–769. doi: 10.1111/dme.13276
O'Keefe, D. J. (2015). Message generalizations that support evidence-based persuasive message design: specifying the evidentiary requirements. Health Commun. 30, 106–113. doi: 10.1080/10410236.2014.974123
Palladino, D. K., Helgeson, V. S., Reynolds, K. A., Becker, D. J., Siminerio, L. M., and Escobar, O. (2013). Emerging adults with type 1 diabetes: a comparison to peers without diabetes. J. Pediatr. Psychol. 38, 506–517. doi: 10.1093/jpepsy/jst002
Peters, A., Laffel, L., and American Diabetes Association Transitions Working Group (2011). Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care 34, 2477–2485. doi: 10.2337/dc11-1723
Peters, S. (2000). Is there a disability culture? A syncretisation of three possible world views. Disabil. Soc. 15, 583–601. doi: 10.1080/09687590050058198
Pinquart, M., and Shen, Y. (2011). Anxiety in children and adolescents with chronic physical illnesses: a meta-analysis. Acta Paediatr. 100, 1069–1076. doi: 10.1111/j.1651-2227.2011.02223.x
Rapoport, A. (1990). The Meaning of the Built Environment: A Nonverbal Communication Approach. University of Arizona Press.
Real, K., Bardach, S. H., and Bardach, D. R. (2017). The role of the built environment: how decentralized nurse stations shape communication, patient care processes, and patient outcomes. Health Commun. 32, 1557–1570. doi: 10.1080/10410236.2016.1239302
Roof, K., and Oleru, N. (2008). Public health: Seattle and King County's push for the built environment. J. Environ. Health 71, 24–27.
Rubin, R. R., and Peyrot, M. (1999). Quality of life and diabetes. Diabetes Metab. Res. Rev. 15, 205–218. doi: 10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O
Saylor, J., Hanna, K. M., and Calamaro, C. J. (2019). Experiences of college students who are newly diagnosed with type 1 diabetes mellitus. J. Pediatr. Nurs. 44, 74–80. doi: 10.1016/j.pedn.2018.10.020
Story, M., Kaphingst, K. M., Robinson-O? Brien, R., and Glanz, K. (2008). Creating healthy food and eating environments: policy and environmental approaches. Ann. Rev. Public Health 29, 253–272. doi: 10.1146/annurev.publhealth.29.020907.090926
Turland, A. H. (2016). Shame, Depression and Self-Care in Emerging Adults With Type 1 Diabetes (Doctoral). University of Surrey. Available online at: http://epubs.surrey.ac.uk/811792/
WHO (2020). Diabetes. World Health Organization. Available online at: https://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf?fbclid=IwAR3bSPmEMO5GR9oP9tFp5lD0BZFJM-fAtc12ogjAp8kFTD2t_fahFbfFeNY (accessed April, 2020).
Wilson, V. (2010). Students' experiences of managing type 1 diabetes. Paediatr. Nurs. 22, 25–28. doi: 10.7748/paed.22.10.25.s26
Wysocki, T., Greco, P., Harris, M. A., Bubb, J., and White, N. H. (2001). Behavior therapy for families of adolescents with diabetes: maintenance of treatment effects. Diabetes Care 24, 441–446. doi: 10.2337/diacare.24.3.441
Keywords: health communication, diabetes, built environment, social capital, quality of life, organizational support
Citation: Malova E and Harrison TR (2023) Environmental characteristics and type 1 diabetes: students' perspectives on diabetes management in college. Front. Commun. 8:1208219. doi: 10.3389/fcomm.2023.1208219
Received: 18 April 2023; Accepted: 16 October 2023;
Published: 13 November 2023.
Edited by:
Vinita Agarwal, Salisbury University, United StatesReviewed by:
Jiawei Liu, Cornell University, United StatesElizabeth Williams, Colorado State University, United States
Copyright © 2023 Malova and Harrison. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ekaterina Malova, ZW1hbG92YUBzaW1vbi5yb2NoZXN0ZXIuZWR1
 Ekaterina Malova
Ekaterina Malova Tyler R. Harrison
Tyler R. Harrison