- 1Department for Social and Health Care Sciences, Regensburg University of Applied Sciences, Technical University of Applied Sciences, Regensburg, Germany
- 2Department for Health Care and Nursing, Catholic University of Applied Sciences, Mainz, Germany
Background: People with aphasia (PWA) often suffer from reduced participation and quality of life. Nevertheless, there are currently only a few specific interventions that respond to this problem. Participation and quality of life could be increased by interacting with peers who have similar experiences. Digital social networks could stimulate an autonomous interaction. However, digital social networks need to be adapted to the specific needs of PWA. Therefore, a participatory, agile process involving the target group should be chosen to develop such a solution, i.e., an app. The research project consists of a total of three phases. In the first phase—app development—the app was developed and programmed including the target group. In the second phase—app testing—the usability and user-friendliness of the app were evaluated with four PWA. In the third phase—feasibility and preliminary efficacy—that will be described in the article, the impact of the app on PWA will be evaluated.
Aims: The overarching aim of our study is to provide preliminary efficacy of the intervention. Digital social interaction with other PWA can lead to increased social integration. In addition to digital interaction, personal encounters between PWA should be encouraged. As a result, we expect an improvement in quality of life of PWA. Additionally, we focus on identification of the most appropriate measurements to discover changes associated with the intervention.
Methods: The evaluation, which is described in this paper, takes place in a pre-test - post-test design with a total of n = 48 PWA. Participants will be recruited in regional clusters to facilitate face-to-face meetings. Half of the participants will be assigned to the delayed intervention group and the other half to the immediate intervention group. Participants in the delayed intervention group will go through a 3-month waiting period before using the app, while the participants of the immediate intervention group will start using the app for 3 months right away. Inclusion criteria are the presence of chronic aphasia (at least 6 months) and possession of a smartphone with internet access. Questionnaires on quality of life (SAQOL-39, GHQ-12), depression (GDS, DISCs), communicative participation (CPIB), and social support (F-SozU) will be conducted at inclusion (t0), after 3 months of app use (t1), and after another 3 months for follow-up (t2). Participants in the delayed intervention group will be assessed twice before the intervention, before the 3-month waiting period (t0a) and after the waiting period (t0b). In addition to the quantitative measures, interviews will take place with 6 to 8 selected participants after 3 months of app use. Responses will be analysed using Thematic Analysis.
Discussion: The app will be the first social network tool that is systematically developed with PWA. Initial indications from the first phases are that the app can be used by PWA, so that the evaluation of this app version can take place in the third phase. Results of this study can provide an initial indication of whether social network support is a suitable intervention. Findings will help provide information on the feasibility of digital connectivity for PWA. Preliminary findings on its impact on the participation and quality of life of PWA could be made available.
1. Background
1.1. Introduction
Aphasia is an acquired language disorder due to brain damage. People with aphasia (PWA) show difficulties in producing or comprehending spoken or written language (Orchardson, 2012). Aphasia is a common consequence of stroke. It occurs in about 30% of all stroke patients (Engelter et al., 2006; Flowers et al., 2016). It is caused by cerebral insult in up to 80% of cases (Kolominsky-Rabas and Heuschmann, 2002). Every year around 270,000 people in Germany suffer a stroke (Stiftung Deutsche Schlaganfallhilfe, 2021). The prevalence of aphasia is around 100,000. It will continue to rise due to demographic change and increasing survival rates because of improved medical care (Rothwell et al., 2004).
1.2. Aphasia impacts quality of life and social connectedness
The World Health Organization defines quality of life (QoL) as the perception of the individual's life situation in the context of their environment and value systems (WHO, 2012). Following Hilari et al. (2021), we refer to the construct of health-related QoL in the following. Health-related QoL describes the impact of a perceived health state on the ability to lead a fulfilling life (Bullinger et al., 1993). Health-related QoL comprises the subjective assessment of several components, e.g., physical, mental, emotional, family, and social functioning (Berzon et al., 1993).
Aphasia impacts QoL significantly (Hilari and Byng, 2009) and is associated with difficulties performing everyday activities (Nätterlund, 2010; Alary Gauvreau and Le Dorze, 2022). For example, up to 80% of PWA do not return to work due to the impact of aphasia on their ability to perform vocational activities (Doucet et al., 2012; Musser et al., 2015) and PWA are often unable to maintain hobbies and life roles (Pike et al., 2017; Taubner et al., 2020). Consequently, PWA suffer worse health-related QoL than people living with cancer or Alzheimer's Disease (Lam and Wodchis, 2010).
QoL can be further impacted by a reduced social participation up to social isolation (Hilari et al., 2010; Lee et al., 2015; Santo Pietro et al., 2019). Social participation can be defined as “a person's involvement in activities that provide interaction with others in society or the community” (Levasseur et al., 2010, p. 2148). Social isolation is defined as having a limited network of people to interact with regularly (NIH, 2021). Due to the language impairments, PWA take part in fewer social activities (Cruice et al., 2006; Vickers, 2010). As a result, they are also exposed to the risk of losing contact with friends and their wider social network (Vickers, 2010; Northcott and Hilari, 2011; Fotiadou et al., 2014; Ellis et al., 2019). Consequently, PWA can experience loss of autonomy and social withdrawal (Cruice et al., 2006; Vickers, 2010; Northcott and Hilari, 2011; Le Dorze et al., 2014; Winkler et al., 2014; Musser et al., 2015; Jones, 2017; Konnerup, 2018), which is associated with psychosocial changes including depression. Up to 62% of PWA show signs of depression 12 months after stroke (Kauhanen et al., 2000).
Additionally, PWA often experience mobility issues due to stroke, which further restrict participation and QoL (Lee et al., 2015). In summary, social isolation, psychosocial changes, and mobility issues caused by stroke and aphasia contribute to significantly reduced QoL.
1.3. Peer support for PWA
A distinction can be made between peer-to-peer support within an entire group (typically, e.g., within aphasia self-help groups) and peer-befriending between two peers, i.e., one-to-one peer support. The focus of this study is peer-befriending. Peer-befriending means a social and emotional support through an exchange of experiences between people with similar life circumstances (e.g., living with the same health condition; Solomon, 2004). Support from peers who are experiencing similar life circumstances can be beneficial also in case of aphasia, as PWA can empathise better and share their concerns, fears, and hardships with each other (NHS Improvement - Stroke, 2011). This shared basis of experience and exchange can lead to a deep relationship of trust between PWA.
Increased participation in meaningful activities and greater involvement with family, friends or support groups can have a positive impact on QoL and living well with aphasia (Brown et al., 2012). Brown et al. (2012) conducted a meta-analysis of data from three studies to examine the role of participation on QoL in PWA. They explored the perspectives of PWA, speech-language pathologists, and family members on living successfully with aphasia. According to the data, PWA participated in a wide range of meaningful activities including communication-based activities such as reading the newspaper and non-verbal activities such as gardening. Engagement in meaningful activities was associated with improved QoL.
A professionally guided, peer-befriending approach aiming at depression prevention was planned in a study protocol for PWA (Hilari et al., 2019). In the randomised controlled feasibility study conducted with 56 PWA, Hilari et al. (2021) demonstrated that peer-befriending for PWA resulted in significant long-term improvements in wellbeing. Participants with aphasia were recruited in the acute phase of stroke recovery. They were randomly allocated to receive usual care (control) or usual care plus peer-befriending (intervention). In the intervention arm, participants were age-matched to a peer-befriender (person with chronic mild-moderate aphasia). Participants received six 1-hour peer-befriending visits over 3 months. Wellbeing was measured before and after the intervention with the GHQ-12 (General Health Questionnaire). The intervention group demonstrated greater improvement in GHQ-12 score at the post-test time point providing preliminary efficacy of this peer-befriending intervention. The authors note that PWA who experience low levels of distress in the acute phase of stroke recovery may benefit from this peer-befriending approach in the long term (Hilari et al., 2021).
In another study, patients in the acute phase after a stroke, not all suffering from aphasia, were offered supportive conversations by peers. Semi-structured interviews post-intervention were conducted. Most of the participants perceived the support and peer conversations as emotionally relieving as they gave them hope, provided a sense of validation and reduced feelings of isolation (Kessler et al., 2014).
1.4. Digital solutions
Structural restrictions could make it difficult to participate in peer-befriending approaches. Barriers like reduced mobility, lack of speech therapy provision, especially in rural or underserved areas (Lanyon et al., 2018; Hilari et al., 2021) could be remedied using digital solutions. Digital media can increase autonomous, social participation in the case of health impairments, as Moorhead et al. (2013) found in a review. In this way, contacts and friendships could even be made over distance. This could be helpful especially for people in socially problematic situations. Existing social media platforms such as Facebook are, however, too complex for PWA (Buhr et al., 2017). Moreover, adapted services for PWA so far relate primarily to exchanges via email (e.g., Mahmud and Martens, 2013, 2016; Thiel et al., 2017; Menger et al., 2020). Until now, digital media in aphasia rehabilitation have concentrated mostly on augmented communication in analogue situations and language-specific training as a videoconference (Brandenburg et al., 2013; Bilda et al., 2017; Asghar et al., 2021). Apart from that, there have only been few attempts to develop social networks for PWA. Buhr et al. (2017) found in a feasibility study that an adapted social media tool used for the asynchronous exchange between PWA facilitated interaction among PWA. The social network AphasiaWeb has a linguistically and visually simplified layout and multimodality input/output features (Buhr et al., 2017). However, no activities can be planned. It also lacks the mediating function of “matching” PWA with regard to similar interests, and similar requirements for emotional and psychological support (see Hilari et al., 2021). In addition, chat functions and a platform for appointments, activities, and exchanges are missing. Preliminary concepts use virtual environments to practise specific language skills (Egaji et al., 2019), but also social participation in groups e.g., EVA Park (Galliers et al., 2017; Marshall et al., 2020). In Australia, an app for PWA is also being developed in a participatory approach with the target group (Rose, 2023). As one component of the platform for post-inpatient care, patients with language disorders receive peer support according to the same pattern as in our research project (Communication Connect; Rose, 2023). Thus, this project follows a similar concept as we do. However, digital, autonomous peer-to-peer support for PWA to increase social participation has not yet been investigated.
In summary, there is a pressing need to develop digital interventions to improve QoL of PWA (Hilari et al., 2019). It must be noted that aphasia is often associated with other neurological deficits such as hemiparesis or hemianopia (Fisher, 2009). Furthermore, as aphasia is more common among older adults, digital skills are often lacking (Menger et al., 2020). Possible neurological comorbidities and the advanced age of the target group must be considered when designing a digital solution. Based on the findings from the feasibility study by Buhr et al. (2017) and the insights of Hilari et al. (2021), a digital social network should additionally include a peer-matching function as well as enable activity scheduling.
1.5. Introducing PeerPAL
The project “Peer-to-peer support: digital networking in aphasia to improve quality of life (PeerPAL)” involves the development and evaluation of a social network as a smartphone app. A co-design process was used to incorporate the expertise of speech and language therapists and PWA in the app development, i.e., we aimed at a catalogue of requirements for an app solution in collaboration with PWA. To capture the requirements and needs of the target group, a design thinking workshop and focus group meetings took place in Phase 1 of the research project—the app development. The six focus group meetings included the project staff and four PWA. The group meetings took place digitally at monthly intervals. In an iterative process the content, design, and layout of the app went through repeated reviews, tests, and corrections. It was a constant alternating process between focus group discussions and revisions of the app. In addition to the implementation of important functions such as the chat function or text input, it became apparent that a matching function would help the target group identifying participants with similar interests. The app was then programmed for use on mobile devices (iOS and Android). During Phase 2—app testing—the app was checked for usage difficulties and problems. Again, four PWA, but different from those who were part of the focus group, tested the app over 2 months. In this paper, we describe the study design of Phase 3—feasibility and preliminary efficacy—in which we evaluate the revised app based on findings from Phase 2.
2. Aims
The PeerPAL project aims at:
1) Facilitating digital social networking to prevent depression and social withdrawal, while overcoming physical distances.
2) Encouraging face-to-face meetings and social activities with peers to improve social inclusion.
3) Promoting independent use of the app by PWA.
4) Gaining insights into digital learning under the condition of language limitations to help facilitate digital inclusion of PWA.
5) Identifying the most appropriate outcome measures for evaluating the effects of a digital social networking intervention, which have not been established.
3. Hypotheses
Despite the preliminary nature of our study, we have attempted to formulate initial ideas as hypotheses.
1. We anticipate that the intervention will result in significant improvements in measures of QoL, communication participation, and social participation relative to pre-intervention measures for both the immediate and delayed intervention groups (Babbitt and Cherney, 2010; Hilari et al., 2021).
2. We hypothesise no significant change in measures of QoL, communication participation, and social participation prior to the PeerPAL intervention for the delayed intervention group.
3. We expect approximately constant stable values in the waiting period for the delayed intervention group and significant improvement in QoL, communication participation, and social participation following the intervention period.
4. We hypothesise no significant differences between the immediate and delayed intervention groups on measures of QoL, communication participation, and social participation after the PeerPAL intervention.
5. We expect improvements in measures of QoL, communication participation, and social participation will remain stable for 3 months after the intervention for both groups (Hilari et al., 2021).
6. We expect the level of depression will remain stable in all participants after the intervention until at least follow-up (Hilari et al., 2021).
4. Methods
4.1. Design
The project consists of three phases: App development (Phase 1), app testing (Phase 2), and evaluation of feasibility, acceptability and preliminary efficacy (Phase 3). The first two phases of the study have already been completed, as explained in the background information. Phase 3 uses a pre-post waitlist-controlled comparison design (Figure 1). Participants will be allocated to either the immediate intervention group or the delayed intervention group (3-month waiting period). This allows all PWA to participate in the intervention and still allows any effects found, to be compared with the control period. We will compare the changes during the intervention period with the changes during the waiting period, i.e., our control period. The assessment time points will be at study inclusion (t0), after the intervention (t1) and after follow-up (t2). The delayed intervention group will be tested at study inclusion (t0a) and again after the 3-month waiting period (t0b). They will start the intervention after the second assessment time point t0b. The intervention will consist of two parts. In the first 6 weeks, the participants will receive intensive support in using the app. In the second 6 weeks, only technical support will be provided. Figure 1 shows the study design.
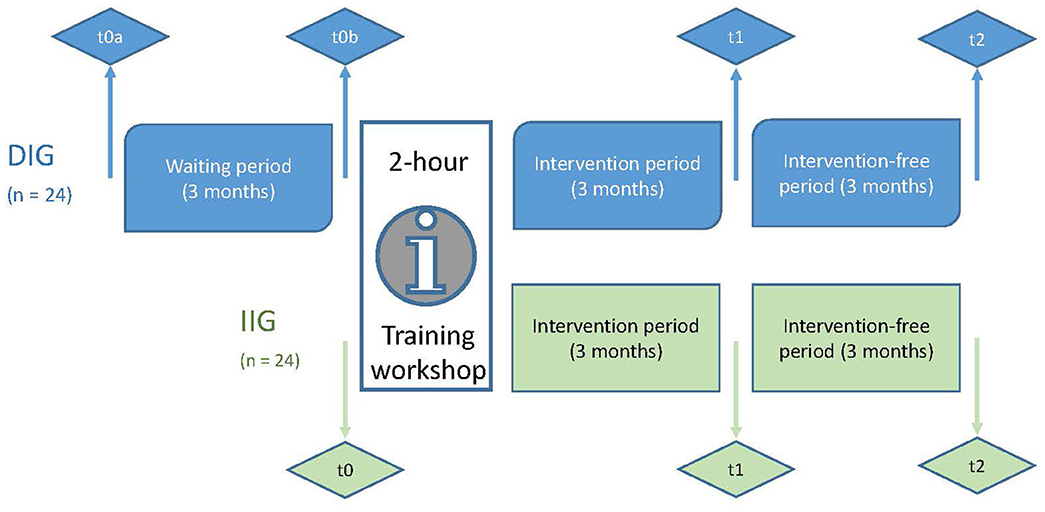
Figure 1. Study design. IIG, Immediate intervention group; DIG, Delayed intervention group; Measurement times: t0(a&b), baseline; t1, post-test; t2, follow-up-survey.
A total of 48 PWA will be enrolled in the main study, 24 in each group. The targeted number of participants was calculated and determined using a power calculation (see Section 4.8.1).
The Template for Intervention Description and Replication (TIDieR) guide (Hoffmann et al., 2014) was used to describe the study interventions (Appendix 1).
Ethical approval to conduct this study with the described study design was sought and received from the Ethics Committee of the German Society for Nursing Science (DGP; 20-032).
4.2. Recruitment
Eligible PWA will be recruited in Germany through various cooperation partners like clinics and language therapy specialist practises as well as regional associations and self-help groups. We will hand out flyers and information material to the cooperation partners describing the inclusion criteria and contact details of the project. PWA, therapists or relatives of PWA could use the material to get in touch if a PWA is interested. By allowing all participants to go through the intervention and thus use the app, we expect that more PWA will be interested in the study resulting in a positive impact on the recruitment rate. When PWA or their relatives or therapists contact us, the project team will check during a phone call if all inclusion criteria are likely to be met (see Section 4.3).
As part of the recruitment strategy, participants are sought in regional clusters. The intervention includes personal meetings. Therefore, it will be necessary to recruit participants in regional proximity so they can meet in person. It is planned that at least six participants per regional cluster will be included and thus it is assumed that about 6 to 8 regional clusters will be needed. For organisational reasons, not all 48 participants can be tested at the same time. However, the participants of a single regional cluster should start the intervention period at the same time so that participants can find as many other participants from their own region as possible in the app. It is planned that the regional clusters will start the intervention one after the other at intervals of 1 month. In the process, the 3-month waiting period will be completed in advance for the first regional clusters. When 24 participants have been found for the delayed intervention group, the following clusters will be recruited for the immediate intervention group. Thus, randomised group assignment will not be used so that participants can use the app in parallel as much as possible. On the one hand, this may lead to differences between groups at baseline, limiting replication and generalisation of this study. On the other hand, non-random group allocation reflects real-world heterogeneity of people with aphasia and the potential impact of heterogeneity on the delivery of this intervention.
4.3. Inclusion criteria for participants
The inclusion criteria for participants are as follows:
• People with chronic aphasia due to a stroke or other injury to the brain (6 months post onset): determined by the Screening of the Aachen Aphasia Test (AAT; Huber et al., 1983). We recruit PWA only from the chronic stage of aphasia onwards, as people in earlier stages of aphasia are more distressed (Hilari et al., 2010). Our method could be used in earlier stages of aphasia, but adaptation to acute aphasia might be required, as PWA in an early stage of aphasia may not yet have realised the impact of the language deficit on their daily lives (Grohn et al., 2012). In addition, social support becomes more important at an advanced stage of adjustment to life after stroke (Hilari et al., 2010).
• Low levels of emotional distress: This is to ensure that participants do not require more complex psychological interventions. To assess depression, the Geriatric Depression Scale (GDS) will be used even if it is not an aphasia-specific measurement tool [such as the Stroke and Aphasia Depression Questionnaire (SADQ; Sutcliffe and Lincoln, 1998)] but it has been successfully used in other studies with PWA previously (Corsten et al., 2015; Lee et al., 2015). As the present intervention is preventive, participants should show only minor signs of depression, operationalised with a score ≤ 8 on the GDS (Sheikh and Yesavage, 1986). For values between five and eight, psychological support is recommended. This will be discussed with the participants in a personal meeting. This conversation is conducted by one of the research assistants with the participants. Both research assistants are qualified speech and language therapists and have therefore also completed several psychology modules. If desired by the participants, relatives may also attend the appointment. If the GDS results in more than eight points, the recruited person must be excluded from the intervention. In this case, one of the research assistants initiates a meeting with the person and his/her relatives and strongly recommends seeking psychological support. Among other things, the participant is strongly advised to go to the general practitioner (GP), who in the German health care system can refer the person to a psychologist or psychiatrist. The GDS test results should be taken to the GP appointment so that the GP can make further decisions based on them.
• Participants should have a smartphone with internet access (WiFi and/or mobile data).
• Vision (with aids) should be sufficient for smartphone use.
No criteria for linguistic abilities are formulated (see Buhr et al., 2017). Thus, the participants could represent a broad spectrum of different levels of aphasia severity. Physical limitations (e.g., hemiplegia) are not an exclusion criteria as long as individuals can operate a smartphone. The aim is to make the app useable for as many PWA as possible. Especially PWA with more severe disabilities, regarding language, mobility, and fine motor skills might benefit from digital inclusion. Persons who do not meet the above inclusion criteria will be excluded from the study.
4.4. Blinding
There is no blinding but there are two rules to improve internal validity. Outcome scorers and assessors are different staff members, but both are involved in the project. Assessors will conduct the quantitative and qualitative outcome measures. Outcome scorers who have experience in administration and evaluation will score the outcome measures. The separation of test administration and test evaluating reduces the risk of individual bias. Participants are not explicitly informed that there is a delayed intervention group and an immediate intervention group. They are only informed about the procedure in their group.
4.5. Training workshop
All participants will attend a 2-h training workshop prior to the intervention period (Figure 1). The training workshop will be based on an action-oriented approach (Pihlanto, 1994). It will take place in a digital setting via Zoom with end-to-end encryption. This is important to protect data privacy of the study participants as best as possible. Small groups of four to eight participants from the same regional cluster will be brought together. Technical and media skills will be trained and knowledge about multimodal communication will be taught. The sections of the app and its functions will be explained in detail and the handling of the app will be practised. Multimodal communication will be explained in more detail and all communication modalities will be tried out in the app. The following communication options are offered in the app: Writing on the keyboard, writing using a dictation function, selection of prepared response options (text modules), emojis and photos.
4.6. Intervention
Following the training workshop, participants will use the PeerPAL-App independently in everyday life over a period of 3 months (Figure 1). The app allows participants to create a profile with name, age, location, interests, and preferred modalities of communication. Using these profiles, PWA can find other users in regional proximity who have similar interests. Contact can be made via text message (chat function) or via phone call. A reduced number of emojis are offered in the chat to not overwhelm with the selection. These are the emojis that are most commonly used by PWA [empirically surveyed and literature-based (Petroi et al., 2014)]. In addition, a selection of text modules is offered, which can be used as response options. Activities can be scheduled. Invitations can be sent to selected friends in the app, or all app users can be invited. All tabs and functions in the app are designed to be as simple and intuitive as possible. Video tutorials explain the functions of the app in plain language and slow speed.
During the first 6 weeks, close support will be provided by the project staff to help users post content and troubleshoot technical issues. The participants will also receive weekly messages via the app's chat from the project team to motivate and remind to use the app. In addition, they will receive individual feedback on their usage behaviour once during this period. This should increase the motivation of the participants to use the app (Zapata et al., 2018). To promote independent use of the app and self-directed learning, participants will be asked in the first 6 weeks of the intervention period to carry out at least two actions in the app each week, e.g., send messages in the chat, schedule activities, or accept an activity invitation. In the second part of the intervention, users will only receive support when having technical problems. Participants will be encouraged to continue using the app after the intervention period has concluded. Technical support will be provided as needed until the follow-up survey.
4.7. Measures
4.7.1. Quantitative outcomes
Based on the aims and hypotheses of the study, the measurements were selected. All tests will be performed at all assessment dates, before intervention (t0), after intervention (t1), and at follow-up (t2). The delayed intervention group will be tested twice before the intervention, once before the waiting period (t0a) and once after the waiting period (t0b). The project staff will conduct the quantitative outcome measures in individual meetings and support participants in case of language difficulties.
As the primary outcome QoL in PWA will be assessed with the SAQOL-39 (Stroke and Aphasia Quality of Life Scale-39; Hilari et al., 2003). The time required for the assessment is manageable, appropriate for the target group and internationally compatible. The test shows good values in internal consistency, test-retest reliability, and construct validity.
GHQ-12 will be used as a second measure for QoL (Goldberg and Williams, 1988). The procedure is the same as that of Hilari et al. (2019). The GHQ-12 was tested in six validity studies and demonstrated high reliability and validity (Goldberg and Williams, 1988).
All other tests are used as secondary outcome measures to learn more about other effects of the intervention and to determine which tests are best suited to detect therapy-specific effects.
Depression will be surveyed with the GDS (Sheikh and Yesavage, 1986). The GDS contains 15 items that are answered with yes or no. The GDS represents a reliable and valid self-rating depression screening scale for elderly populations (Yesavage et al., 1982). Nevertheless, GDS shows good diagnostic sensitivity and specificity even for younger individuals (adults 18 years and older; Guerin et al., 2018).
The intensity of depression will be assessed with the DISCs (Depression Intensity Scale Circles; Turner-Stokes et al., 2005). The DISCs Screening is a simple assessment tool with two questions, specifically for depression in brain injury. It has acceptable convergent validity, reliability, and responsiveness. The research group translated the DISCs from English into German in a scientific translation process ensuring that the internationally used DISCs with a visual scale can be used for this German study with PWA.
Perceived social support and relationships with significant others will be surveyed using the F-SozU (Social Support Questionnaire; Fydrich et al., 2007). The short form of the F-SozU used in this study contains only 14 items and can therefore be completed in a short time. The F-SozU represents a reliable, valid, and economical instrument and can therefore be used effectively in clinical epidemiological studies or related fields (Kliem et al., 2015).
Communicative participation will be assessed with the CPIB (Communicative Participation Item Bank; Baylor et al., 2013). The short form of the CPIB contains 10 items and has been validated for PWA (Baylor et al., 2017). In the study of Baylor et al., the majority of the PWA were able to respond to the CPIB tasks, although most of them needed assistance. PWA, who were unable to complete the CPIB, generally had higher aphasia severity. The research group translated the CPIB from English into German in a scientific translation.
4.7.2. Qualitative outcomes
Semi-structured interviews regarding the social network and living situation will be conducted with seven to eight randomly selected participants immediately after the intervention (t1) and during the follow-up (t2). In order to ensure variance between the clusters and aphasia severity, the participants are divided into the respective groups and randomly drawn from them. On the one hand, this excludes selection bias, but on the other hand, this approach also enables data transferability, by creating variability and gaining different perspectives. Interviews will be held to get a better insight into individually seen advantages and disadvantages of the app, regional cluster dynamics, and perceived effects from app usage, and to learn more about the working mechanism of the intervention. In addition, the interview data will also serve to elicit further suggestions for improving the app. The interviews are based on a guide that includes open-ended narrative-generating questions and specific follow-up questions. This allows the interview to be individually adapted to PWA with different levels of aphasia severity.
4.7.3. Fidelity
To ensure adherence to the protocol and comparability of the implementation, all activities of the participants are recorded in detail (number of posts, number of messages sent, time spent online). This protocol has been developed and defined in advance according to international guidelines.
Training workshop fidelity is monitored by video recordings and with the use of a checklist. The template will be a checklist that was developed and evaluated in the project, “Biography work in long-term residential aged care with tablet support to improve the quality of life and communication” (BaSeTaLK; Corsten and Lauer, 2020). The checklist includes items on observation of the participants and conveyed information on the app. Each training workshop is supervised by an assistant who observes the participants and ensures that the checklist is followed.
4.8. Data analysis
4.8.1. Power calculation
The sample size to detect the efficacy of the intervention was determined based on the research design. Statistical power was calculated using G*Power. With 24 participants each in the immediate intervention group and delayed intervention group, a mean effect size of 0.73 in the primary outcome measure (SAQOL-39) is sufficient to confirm differences between pre- and post-test (for n = 20, a mean effect size of 0.82). This is a high effect size. The outcome variable in the calculations is QoL as measured by the SAQOL-39. The calculations were based on a one-tailed test situation, an alpha error of 0.05, and a beta error of 0.2. However, it is meant as a compromise between an achievable number of participants and an expected effect. If we do not achieve such an effect, we may at least be able to see pre- and post-effects. The t-test for differences between two independent means was used. The input parameters were one-tailed calculation with an alpha error of 0.05 and a power of 0.8 given the exploratory character of the study. For the G*Power calculation, the t-test for two independent samples was again used. The input parameters were one-tailed calculations with an alpha error of 0.05 and a beta error of 0.2, which is common for constructing an RCT.
4.8.2. Statistical methods and qualitative analysis
Inferential statistics of intra-individual changes and inter-individual differences, group differences as well as group differences between the waiting period and intervention period will be evaluated after testing for normal distribution either with non-parametric or parametric procedures (depending on the distribution of the data) with the IBM SPSS 25.0 statistics program. The main objective of the study is to provide evidence of efficacy of the intervention in improving QoL. To prove this, a pre-post analysis will take place. Since we would also like to verify long-term effects, an additional follow-up survey will take place after 3 months. The quantitative outcomes (see Section 4.7.1) will be used as dependent variables. The continuous variables will be analysed according to the distribution characteristics by means of a t-test for connected samples or Wilcoxon test. In addition, regression analyses and the Kruskal-Wallis test will be used. The number of factors will depend on the extent to which the recorded group and study periods differences represent a homogeneous or nonhomogeneous construct. Cluster analyses or latent class analyses can be used to identify the subgroups. For example, influencing factors such as age, gender, morbidity, and aphasia severity can be analysed. An alpha level of 0.05 will be accepted as significant. The results of the statistical models will be presented in the form of regression coefficients, their 95% confidence intervals, and effect sizes. Percentage scores will be determined for the checklists for protocol adherence and Kappa statistics will be calculated to determine inter- and intra-rater reliability.
The study uses descriptive statistics to capture numbers on recruitment, treatment fidelity and reasons for dropping out.
Recruitment and retention rates will be used to aid in the calculation of the sample size of future studies with a similar research interest, and to determine the required number of possible recruitment locations (such as clinics and practises). Adverse incidents such as dropouts will be also documented. The course of study will be evaluated with qualitative interviews of the participants. Thematic analysis will be used to explore the interview material (Braun and Clarke, 2006).
4.8.3. Data management
A data management plan has been created via DMPonline (data management plans online; Digital Curation Center, 2023). DMPonline is a web-based tool that supports researchers to develop data management plans. For secure data exchange between the network universities, Synology Cloud Station Drive will be used, which enables data storage on a server of the Ostbayerische Technische Hochschule Regensburg (OTH Regensburg). Project staff at each university will enter anonymized participant data directly into Synology Cloud Station Drive. Once data collection has commenced, the study's chief investigators will monitor data for completeness and accuracy. They will also continuously monitor the progress of the study, adverse safety events and data accuracy. No formal criteria exist for discontinuing the trial early.
4.9. Trial status
The project started in December 2020 and the first focus group meeting took place in March 2021 (phase 1). A total of six focus group meetings were held by August 2021 to continuously improve the app prototype. The time that followed was all about programming the app, until 4 participants started the app testing in May 2022 (phase 2). In August 2022, the first participants for the main study were enrolled in the delayed intervention group (phase 3). The project is officially registered and can be viewed on the public website of the German Register of Clinical Trials (DRKS00023855) and in the World Health Organization's search portal (http://apps.who.int/trialsearch/). Cooperation agreements have been signed with the following practise partners: “Aphasie Landesverband” (Aphasia National Association) in Bavaria, the “Aphasiker-Zentrum” (Aphasia Center) in Lower Franconia, the Asklepios Klinik Schaufling, the “Berufsfachschule für Logopädie” (Vocational school for speech and language therapy) in Regensburg, the “Logopädische Praxis Brigitte Brauer” (speech and language therapy practise Brigitte Brauer) in Mainz, the “Logopädische Praxis Bruni Zeuner” (speech and language therapy practise Bruni Zeuner) in Idstein and the “Praxis für Logopädie und Neurolinguistik” (practise for speech and language therapy and neurolinguistics) in Regensburg.
5. Discussion
The PeerPAL-App is the first digital social network tailored to the needs and capabilities of PWA. The app is intended to promote social interaction with peers both online and face-to-face, and thereby improve QoL and prevent depression. Consistent and regular use of the app will be facilitated through training, supervision, and support. If effective and integrated into the life of PWA, it may have the potential to improve QoL, communicative participation, and social support, and thereby prevent depression.
App-supported peer-befriending could ease the burden on family members of PWA. Most PWA strengthen ties with immediate family members after stroke, bringing them into focus and making them key contacts (Hilari and Northcott, 2006; Ellis et al., 2019). Interaction with other PWA can improve communication within the family, reduce PWA dependence on family members, and allow family members to have time to themselves (Rotherham et al., 2016).
Future research could more fully implement qualitative outcome measures to better elicit individual factors that contribute to successful intervention such as size of current social circle or personality factors. Transferring the app to other groups, e.g., with neurogenic speech disorders, dysarthria in Parkinson's disease or multiple sclerosis, could be evaluated in following projects. In this way, further benefits can be generated.
5.1. Potential short-term impact
The social network will be open sourced after the end of the project. Thus, the app could be used beyond the end of the project and a continuous, flexible adaptation with low operating costs could take place. In addition, training courses for speech and language therapists, neuropsychologists and social pedagogues are planned to make PWA aware of the app and, if necessary, provide assistance during initial use. Professionals could benefit as PWA will gain more autonomy and rely less on the support of professionals. We are aware that successful use of the app cannot replace personal contacts and professional support. Nevertheless, the interaction with other peers might possibly be an alternative way to get in touch with other people especially for people who live in rural regions with poor infrastructure (Walter and Altgeld, 2000; Keck and Doarn, 2014; WHO, 2016; Roche and Nicholas, 2019), which means e.g., a lack of public transport or reduced speech and language therapy provision. These structural restrictions could make it difficult to keep appointments (without assistance), meet with other people or participate in peer-support approaches such as self-help groups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
CK, MN, and MK elaborated and researched content on the background and hypotheses. Furthermore, they compiled content on the method and wrote the discussion. Significant contributions have been made to the paper as a whole by NL and SC who are both responsible for the research conception design, who contributed to literature search, screening, and editing the paper. DK is responsible for the programming and design of the app. All authors read and approved the final manuscript.
Funding
This project was funded by the Federal Ministry of Education and Research (BMBF; grant from 2020–2023, 13FH077SA8, 13FH077SB8).
Acknowledgments
The trial sponsor is the Federal Ministry of Education and Research. Special thanks also go to the participants in the study, their families for their support, and the cooperation partners for finding suitable participants. In addition, we would like to thank our student assistants, Lena Werner, Larisa Malanchev, Viktoria Thedens, Isabell Starke, Franziska Gärtner, and Anna Holzammer for their great support. Our work was also supported by Hannah Casling, who proofread our manuscript and gave us helpful tips on wording. We would especially like to thank the reviewers and editor, whose suggestions contributed significantly to the improvement of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2023.1187233/full#supplementary-material
References
Alary Gauvreau, C., and Le Dorze, G. (2022). Participant reported outcomes of a community of practice about social participation for speech-language pathologists in aphasia rehabilitation. Disabil. Rehabil. 44, 231–242. doi: 10.1080/09638288.2020.1764116
Asghar, I., Egaji, O. A., and Griffiths, M. (2021). An overview of the digital solutions for helping people with aphasia through bibliometric analysis. eNeurologicalSci 22, 100311. doi: 10.1016/j.ensci.2021.100311
Babbitt, E. M., and Cherney, L. R. (2010). Communication confidence in persons with aphasia. Top. Stroke Rehabil. 17, 214–223. doi: 10.1310/tsr1703-214
Baylor, C., Oelke, M., Bamer, A., Hunsaker, E., Off, C., Wallace, S. E., et al. (2017). Validating the Communicative Participation Item Bank (CPIB) for use with people with aphasia: an analysis of Differential Item Function (DIF). Aphasiology 31, 861–878. doi: 10.1080/02687038.2016.1225274
Baylor, C., Yorkston, K., Eadie, T., Kim, J., Chung, H., and Amtmann, D. (2013). The Communicative Participation Item Bank (CPIB): item bank calibration and development of a disorder-generic short form. J. Speech Lang. Hear. Res. 56, 1190–1208. doi: 10.1044/1092-4388(2012/12-0140)
Berzon, R., Hays, R. D., and Shumaker, S. A. (1993). International use, application and performance of health-related quality of life instruments. Q. Life Res. 2, 367–368. doi: 10.1007/BF00422214
Bilda, K., Mühlhaus, J., and Ritterfeld, U. (2017). Neue Technologien in der Sprachtherapie. Stuttgart: Thieme.
Brandenburg, C., Worrall, L., Rodriguez, A. D., and Copland, D. (2013). Mobile computing technology and aphasia: an integrated review of accessibility and potential uses. Aphasiology 27, 444–461. doi: 10.1080/02687038.2013.772293
Braun, V., and Clarke, V. (2006). Using thematic analysis in psychology. Qual. Res. Psychol. 3, 77–101. doi: 10.1191/1478088706qp063oa
Brown, K., Worrall, L., Davidson, B., and Howe, T. (2012). Living successfully with aphasia: a qualitative metaanalysis of the perspectives of individuals with aphasia, family members, and speech-language pathologists. Int. J. Speech Lang. Pathol. 14, 141–155. doi: 10.3109/17549507.2011.632026
Buhr, H. R., Hoepner, J. K., Miller, H., and Johnson, C. (2017). AphasiaWeb: development and evaluation of an aphasia-friendly social networking application. Aphasiology 31, 999–1020. doi: 10.1080/02687038.2016.1232361
Bullinger, M., Anderson, R., Cella, D., and Aaronson, N. (1993). Developing and evaluating cross-cultural instruments from minimum requirements to optimal models. Q. Life Res. 2, 451–459. doi: 10.1007/BF00422219
Corsten, S., and Lauer, N. (2020). Biography work in in long-term residential aged care with tablet support to improve the quality of life and communication – study protocol for app development and evaluation. Int. J. Health Prof. 7, 13–23. doi: 10.2478/ijhp-2020-0002
Corsten, S., Schimpf, E. J., Konradi, J., Keilmann, A., and Hardering, F. (2015). The participants' perspective: how biographic-narrative intervention influences identity negotiation and quality of life in aphasia. Int. J. Lang. Comm. Disord. 50, 788–800. doi: 10.1111/1460-6984.12173
Cruice, M., Worrall, L., and Hickson, L. (2006). Quantifying aphasic people's social lives in the context of non-aphasic peers. Aphasiology 20, 1210–1225. doi: 10.1080/02687030600790136
Doucet, T., Muller, F., Verdun-Esquer, C., Debeillex, X., and Brochard, P. (2012). Returning to work after stroke: a retrospective study at the Physical and Rehabilitation Centre La Tour de Gassies. Ann. Phys. Rehabil. Med. 55, 112–127 doi: 10.1016/j.rehab.2012.01.007
Egaji, O. A., Asghar, I., Griffiths, M., and Warren, W. (2019). “Digital speech therapy for the aphasia patients: challenges, opportunities and solutions,” in International Conference on Information Communication and Management (ICICM), Conference Paper, 08/19 (Pontypridd: The Centre of Excellence in Mobile and Emerging Technologies, University of South Wales), 85–88.
Ellis, C., Phillips, R., Hill, T., and Briley, P. M. (2019). Social network structure in young stroke survivors with aphasia: a case series report. Semin. Speech Lang. 40, 359–369. doi: 10.1055/s-0039-1688695
Engelter, S. T., Gostynski, M., Papa, S., Frei, M., Born, C., Ajdacic-Gross, V., et al. (2006). Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke 37, 1379–1384. doi: 10.1161/01.STR.0000221815.64093.8c
Fisher, M. (2009). Stroke, Part II: Clinical Manifestations and Pathogenesis. Amsterdam: Elsevier Science.
Flowers, H. L., Skoretz, S. A., Silver, F. L., Rochon, E., Fang, J., Flamand-Roze, C., et al. (2016). Poststroke aphasia frequency, recovery, and outcomes: a systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 97, 2188–2201. doi: 10.1016/j.apmr.2016.03.006
Fotiadou, D., Northcott, S., Chatzidaki, A., and Hilari, K. (2014). Aphasia blog talk: how does stroke and aphasia affect a person's social relationships? Aphasiology 28, 1281–1300. doi: 10.1080/02687038.2014.928664
Fydrich, T., Sommer, G., and Brähler, E. (2007). F-SozU: Fragebogen zur Sozialen Unterstützung. Göttingen: Hogrefe.
Galliers, J., Wilson, S., Marshall, J., Talbot, R., Devane, N., Booth, T., et al. (2017). Experiencing EVA park, a multi-user virtual world for people with aphasia. ACM Transact. Access. Comp. 15, 1–24. doi: 10.1145/3134227
Goldberg, D. P., and Williams, P. A. (1988). User's Guide to the General Health Questionnaire (GHQ). Oxford: NFER-Nelson.
Grohn, B., Worrall, L. E., Simmons-Mackie, N., and Brown, K. (2012). The first 3-months post-stroke: what facilitates successfully living with aphasia? Int. J. Speech Lang. Pathol. 14, 390–400. doi: 10.3109/17549507.2012.692813
Guerin, J. M., Copersino, M. L., and Schretlen, D. J. (2018). Clinical utility of the 15-item geriatric depression scale (GDS-15) for use with young and middle-aged adults. J. Affect. Disord. 241, 59–62. doi: 10.1016/j.jad.2018.07.038
Hilari, K., Behn, N., James, K., Northcott, S., Marshall, J., Thomas, S., et al. (2021). Supporting wellbeing through peer-befriending (SUPERB) for people with aphasia: a feasibility randomised controlled trial. Clin. Rehabil. 35, 1151–1163. doi: 10.1177/0269215521995671
Hilari, K., Behn, N., Marshall, J., Simpson, A., Thomas, S., Northcott, S., et al. (2019). Adjustment with aphasia after stroke: study protocol for a pilot feasibility randomised controlled trial for SUpporting wellbeing through PEeR Befriending (SUPERB). Pilot Feas. Stud. 5, 1–16. doi: 10.1186/s40814-019-0397-6
Hilari, K., and Byng, S. (2009). Health-related quality of life in people with severe aphasia. Int. J. Lang. Commun. Disord. 44, 193–205. doi: 10.1080/13682820802008820
Hilari, K., Byng, S., Lamping, D. L., and Smith, S. C. (2003). Stroke and aphasia quality of life scale-39 (SAQOL-39) evaluation of acceptability, reliability, and validity. Stroke 34, 1944–1950. doi: 10.1161/01.STR.0000081987.46660.ED
Hilari, K., and Northcott, S. (2006). Social support in people with chronic aphasia. Aphasiology 20, 17–36. doi: 10.1080/02687030500279982
Hilari, K., Northcott, S., Roy, P., Marshall, J., Wiggins, R. D., Chataway, J., et al. (2010). Psychological distress after stroke and aphasia: the first six months. Clin. Rehabil. 24, 181–190. doi: 10.1177/0269215509346090
Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., et al. (2014). Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 348, g1687. doi: 10.1136/bmj.g1687
Huber, W., Poeck, K., Weniger, D., and Willmes, K. (1983). Aachener Aphasie-Test (AAT). Göttingen; Toronto, ON; Zürich: Verlag für Psychologie.
Jones, B. A. (2017). Comparing Satisfaction With Social Networks of Adults With and Without Aphasia [MA (Master of Arts) thesis], Iowa: University of Iowa.
Kauhanen, M. L., Korpelainen, J. T., Hiltunen, P., Määtt,ä, R., Mononen, H., Brusin, E., et al. (2000). Aphasia, depression and non-verbal cognitive impairment in ischaemic stroke. Cerebrovasc. Dis. 10, 455–461. doi: 10.1159/000016107
Keck, C., and Doarn, C. (2014). Telehealth technology applications in speech–language pathology. Telemed. eHealth 20, 653–659. doi: 10.1089/tmj.2013.0295
Kessler, D., Egan, M., and Kubina, L.-A. (2014). Peer support for stroke survivors: a case study. BMC Health Serv. Res. 14, 1–9. doi: 10.1186/1472-6963-14-256
Kliem, S., Mößle, T., Rehbein, F., Hellmann, D. F., Zenger, M., and Brähler, E. (2015). A brief form of the Perceived Social Support Questionnaire (F-SozU) was developed, validated, and standardized. J. Clin. Epidemiol. 68, 551–562. doi: 10.1016/j.jclinepi.2014.11.003
Kolominsky-Rabas, P. L., and Heuschmann, P. U. (2002). Inzidenz, Ätiologie und Langzeitprognose des Schlaganfalls. Fortschritte Neurol. Psychiatr. 70, 657–662. doi: 10.1055/s-2002-35857
Konnerup, U. (2018). “Inclusive digital technologies for people with communication disabilities,” in The Digital Turn in Higher Education. International Perspectives on Learning and Teaching in a Changing World, eds D. Kergel, B. Heidkamp, P. K. Telléus, T. Rachwal, and S. Nowakowski (Wiesbaden: Springer), 193–208.
Lam, J. M., and Wodchis, W. P. (2010). The relationship of 60 disease diagnoses and 15 conditions to preference-based health-related quality of life in Ontario hospital-based long-term care residents. Med. Care 48, 380–387. doi: 10.1097/MLR.0b013e3181ca2647
Lanyon, L., Worrall, L., and Rose, M. (2018). Exploring participant perspectives of community aphasia group participation: from “I know where I belong now” to “Some people didn't really fit in”. Aphasiology 32, 139–163. doi: 10.1080/02687038.2017.1396574
Le Dorze, G., Salois-Bellerose, É., Alepins, M., Croteau, C., and Hallé, C. (2014). A description of the personal and environmental determinants of participation several years post-stroke according to the views of people who have aphasia. Aphasiology 28, 421–439. doi: 10.1080/02687038.2013.869305
Lee, H., Lee, Y., Choi, H., and Pyun, S. B. (2015). Community integration and quality of life in aphasia after stroke. Yonsei Med. J. 56, 1694–1702. doi: 10.3349/ymj.2015.56.6.1694
Levasseur, M., Richard, L., Gauvin, L., and Ramond, E. (2010). Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Soc. Sci. Med. 71, 2141–2149. doi: 10.1016/j.socscimed.2010.09.041
Mahmud, A. A., and Martens, J.-B. (2013). Amail: design and evaluation of an accessible email tool for persons with aphasia. Interact. Comput. 25, 351–374. doi: 10.1093/iwc/iws025
Mahmud, A. A., and Martens, J.-B. (2016). Social networking through email: studying email usage patterns of persons with aphasia. Aphasiology 30, 186–210. doi: 10.1080/02687038.2015.1109051
Marshall, J., Devane, N., Talbot, R., Caute, A., Cruice, M., Hilari, K., et al. (2020). A randomised trial of social support group intervention for people with aphasia: a novel application of virtual reality. PLoS ONE 15, e0239715. doi: 10.1371/journal.pone.0239715
Menger, F., Morris, J., and Salis, C. (2020). The impact of aphasia on Internet and technology use. Disabil. Rehabil. 42, 2986–2996. doi: 10.1080/09638288.2019.1580320
Moorhead, S. A., Hazlett, D. E., Harrison, L., Carroll, J. K., Irwin, A., and Hoving, C. (2013). A new dimension in health care: systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Int. Res. 15, 85–112. doi: 10.2196/jmir.1933
Musser, B., Wilkinson, J., Gilbert, T., and Bokhour, B. G. (2015). Changes in identity after aphasic stroke: implications for primary care. Int. J. Fam. Med. 2015. doi: 10.1155/2015/970345
Nätterlund, B. S. (2010). A new life with aphasia: everyday activities and social support. Scand. J. Occup. Ther. 17, 117–129. doi: 10.3109/11038120902814416
NHS Improvement - Stroke (2011). Psychological Care After Stroke: Improving Stroke Services for People With Cognitive and Mood Disorders.
NIH (2021). Loneliness and Social Isolation — Tips for Staying Connected. National Institute on Aging.
Northcott, S., and Hilari, K. (2011). Why do people lose their friends after a stroke? Int. J. Lang. Commun. Disord. 46, 524–534. doi: 10.1111/j.1460-6984.2011.00079.x
Orchardson, R. (2012). Aphasia - the hidden disability. Dent. Update 39, 173–174. doi: 10.12968/denu.2012.39.3.168
Petroi, D., Koul, R. K., and Corwin, M. (2014). Effect of number of graphic symbols, levels, and listening conditions on symbol identification and latency in persons with aphasia. Augment. Altern. Commun. 30, 40–54. doi: 10.3109/07434618.2014.882984
Pihlanto, P. (1994). The action-oriented approach and case study method in management studies. Scand. J. Manag. 10, 369–382. doi: 10.1016/0956-5221(94)90024-8
Pike, C., Kritzinger, A., and Pillay, B. (2017). Social participation in working-age adults with aphasia: an updated systematic review. Top. Stroke Rehabil. 24, 627–639. doi: 10.1080/10749357.2017.1366012
Roche, A. M., and Nicholas, R. S. (2019). Mental Health and Addictions Workforce Development: Past, Present, and Future. Substance Abuse and Addiction: Breakthroughs in Research and Practice (Hershey: IGI Global), 24–58.
Rose, M. (2023). Communication Connect. Research Project, Duration: 2021–2025. Melbourne, VIC: La Trobe University.
Rotherham, A., Howe, T., and Tillard, G. (2016). Perceived benefits for family members of group participation by their relatives with aphasia. Clin. Arch. Commun. Disord. 1, 62–68. doi: 10.21849/cacd.2016.00059
Rothwell, P. M., Coull, A. J., Giles, M. F., Howard, S. C., Silver, L. E., Bull, L. M., et al. (2004). Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 363, 1925–1933. doi: 10.1016/S0140-6736(04)16405-2
Santo Pietro, M. J., Marks, D. R., and Mullen, A. (2019). When words fail: providing effective psychological treatment for depression in persons with aphasia. J. Clin. Psychol. Med. Sett. 26, 483–494. doi: 10.1007/s10880-019-09608-4
Sheikh, J. I., and Yesavage, J. A. (1986). “Geriatric Depression Scale (GDS). Recent evidence and development of a shorter version,” in Clinical Gerontology: A Guide to Assessment and Intervention, ed T. L. Brink (New York, NY: The Haworth Press, Inc.), 165–173.
Solomon, P. (2004). Peer support/peer provided services underlying processes, benefits, and critical ingredients. Psychiatr. Rehabil. J. 4, 392–401 doi: 10.2975/27.2004.392.401
Sutcliffe, L. M., and Lincoln, N. B. (1998). The assessment of depression in aphasic stroke patients: the development of the Stroke Aphasic Depression Questionnaire. Clin. Rehabil. 12, 506–513. doi: 10.1191/026921598672167702
Taubner, H., Hallén, M., and Wengelin, Å. (2020). Still the same? – Self-identity dilemmas when living with post-stroke aphasia in a digitalised society. Aphasiology 34, 300–318. doi: 10.1080/02687038.2019.1594151
Thiel, J., Sage, K., and Conroy, P. (2017). Promoting linguistic complexity, greater message length and ease of engagement in email writing in people with aphasia: initial evidence from a study utilizing assistive writing software. Int. J. Lang. Commun. Disord. 52, 106–124. doi: 10.1111/1460-6984.12261
Turner-Stokes, L., Kalmus, M., Hirani, D., and Clegg, F. (2005). The depression intensity scale circles (DISCs): a first evaluation of a simple assessment tool for depression in the context of brain injury. J. Neurol. Neurosurg. Psychiatr. 76, 1273–1278. doi: 10.1136/jnnp.2004.050096
Vickers, C. P. (2010). Social networks after the onset of aphasia: the impact of aphasia group attendance. Aphasiology 24, 902–913. doi: 10.1080/02687030903438532
Walter, U., and Altgeld, T. (2000). Altern im ländlichen Raum: Ansätze für eine vorausschauende Alten- und Gesundheitspolitik. Frankfurt: Campus Verlag.
Winkler, M., Bedford, V., Northcott, S., and Hilari, K. (2014). Aphasia blog talk: how does stroke and aphasia affect the carer and their relationship with the person with aphasia? Aphasiology 28, 1301–1319 doi: 10.1080/02687038.2014.928665
Yesavage, J. A., Brink, T. L., Rose, T. L., Lum, O., Huang, V., Adey, M., et al. (1982). Development and validation of a geriatric depression screening scale: a preliminary report. J. Psychiatr. Res. 17, 37–49. doi: 10.1016/0022-3956(82)90033-4
Keywords: aphasia, digital participation, quality of life, social network, peer-to-peer support
Citation: Kurfess C, Corsten S, Nickel MT, Knieriemen M, Kreiter D and Lauer N (2023) Peer-to-peer support: digital networking in aphasia to improve quality of life (PeerPAL). Front. Commun. 8:1187233. doi: 10.3389/fcomm.2023.1187233
Received: 15 March 2023; Accepted: 17 August 2023;
Published: 07 September 2023.
Edited by:
Hendrike Frieg, University of Applied Sciences and Arts Hildesheim, Holzminden, Göttingen, GermanyReviewed by:
Guylaine Le Dorze, Montreal University, CanadaSam Harvey, The University of Queensland, Australia
Copyright © 2023 Kurfess, Corsten, Nickel, Knieriemen, Kreiter and Lauer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christina Kurfess, Y2hyaXN0aW5hLmt1cmZlc3NAb3RoLXJlZ2Vuc2J1cmcuZGU=
 Christina Kurfess
Christina Kurfess Sabine Corsten2
Sabine Corsten2 Maren Tabea Nickel
Maren Tabea Nickel Norina Lauer
Norina Lauer