
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Commun., 15 December 2023
Sec. Language Communication
Volume 8 - 2023 | https://doi.org/10.3389/fcomm.2023.1176473
This article is part of the Research TopicDigital Participation and Communication Disorders across the LifespanView all 15 articles
Introduction: In speech-language pathology, there is a constant need to make evidence-based decisions based on the patient's needs and goals, speech-language pathologist's clinical expertise, and external evidence. During the COVID-19 pandemic, it was possible for the first time in Germany to implement video-based telepractice in the outpatient care of speech-language pathology. This study aimed to find out how evidence-based decisions are made in video-based telepractice and what forms of evidence are used.
Methods: Speech-language pathologists who were working in outpatient services recorded their video-based telepractices for the research project. Five recorded video-based telepractices were transcribed using a simple transcription system and video interaction analysis was used to analyze the video recordings based on grounded theory methodology.
Results: Interactions between patients and speech-language pathologists are characterized by evidence-based decisions that can be observed. Speech-language pathologists make decisions based on their clinical expertise, patient-related experiences, and patient self-assessments. There is little evidence of negotiation between patients and speech-language pathologists to make joint decisions. Results showed that speech-language pathologists do not explicitly name external evidence to justify their decisions to patients. Shared decision-making is encouraged by a participative interaction between patients and speech-language pathologists. However, there was a predominant paternalistic interaction in which the speech-language pathologists made decisions on their own. To represent the decision-based interactions between patients and speech-language pathologists in a video-based therapy session, a process model was developed.
Discussion: Evidence-based and shared decision-making are important in speech-language pathology to provide patient-centered treatments. The exchange of information between the patient and the speech-language pathologist is important in order to make joint decisions based on these different levels of knowledge. In this way, the patient becomes an active participant in the digital treatment, in the video-based telepractice. As a result, the quality of care can be improved. Further research should reconstruct the implicit (possible) use of external evidence.
During the COVID-19 pandemic, video-based telepractice was allowed to be provided as a telemedical service in an outpatient speech-language pathology (SLP) service for the first time in Germany. The implementation of video-based telepractice was an opportunity to maintain access to SLP service and thus reduce gaps in therapy due to reduce in-person contact. SLPs and patients needed to decide whether continuing therapy via video-based telepractice was feasible with the available technical resources and privacy considerations.
Video-based telepractice as a telehealth service (Gemeinsamer Bundesausschuss, 2020) is a synchronous form of therapy. It is delivered in real time via an audio and video connection, creating an immediate personal contact similar to in-person therapy (ASHA, n.d.). Video-based telepractice can be delivered to individuals with different types of disorders (e.g., aphasia, dysphagia, dysphonia, stuttering) and clinical conditions (e.g., Parkinson's disease, autism spectrum disorder) of different ages. Research findings have shown that there is high satisfaction and broad patient acceptance of patients of different ages in the use of video-based telepractice (e.g., Coleman et al., 2015; Rangarathnam et al., 2015; Wales et al., 2017; Sutherland et al., 2018; McGill et al., 2019; Theodoros et al., 2019; Weidner and Lowman, 2020).
Video-based telepractice is a digital form of therapy in which patients can digitally participate in health care (Neuhaus, 2022). Digital participation is defined in terms of having access to technical equipment (e.g., notebook, mobile phone) and a stable internet connection as well as the ability to use digital applications. Digital participation enables individuals to perform individually relevant activities in various areas of life and to become involved in their own life situation (Neuhaus, 2022; Steiner, 2023). To use video-based telepractice in outpatient speech-language pathology, patients and speech-language pathologists need the necessary hardware (e.g., laptop, PC, mobile phone, camera) and software (e.g., videoconferencing system, online therapy platform) and must be able to use them (Bilda et al., 2020; Lauer, 2020; Barthel et al., 2021b). However, financial, structural and personal difficulties (e.g., unreliable internet connection, limited financial resources, low digital literacy) can limit access and skills and make digital participation in healthcare difficult (Neuhaus, 2022; Steiner, 2023).
This article examines how decision-making occurs in patient-clinician interactions with patients of different ages and clinical indications in video-based telepractice to examine the possibilities of a successful digital participation for people with special needs. It focuses on how patients and clinicians are involved in decision-making and what components characterize a decision-making process.
Decision-making processes in SLP should involve multiple forms of evidence to make informed decisions in patient care.
Evidence-based practice (EBP) “is the conscientious use of current best evidence in making decisions about the care of individual patients or the delivery of health services” (Cochrane, 2011). EBP in SLP has been described as being guided by three core components (ASHA, 2004, 2023; Dodd, 2007; Dollaghan, 2007):
1. The best available evidence from systematic research is called external evidence, current best evidence or external scientific evidence.
2. The knowledge and experience of SLPs and their professional and communication skills needed in the therapy process to make shared decisions is referred to as clinical expertise.
3. Patient interests, needs, circumstances, priorities, expectations are called client value, evidence concerning the preferences of a fully informed patient, client preferences or client perspectives.
Higginbotham and Satchidanand (2019) criticized this understanding of EBP for not distinguishing between clinical expertise and patient-specific evidence. They argued that internal evidence— systematically generated data from patients in the therapy process—should be considered separately, to emphasize its importance in decision-making during the therapy process. They also propose combining clinical expertise and clinical opinion as one expression (Higginbotham and Satchidanand, 2019). Fissel Brannick et al. (2022) noted in their scoping review that there is still no consistent distinction or conflation of internal evidence, clinical expertise, clinical opinion, or evidence internal to clinical practice in the literature, which can lead to uncertainty for therapists in evidence-based decision-making.
Therefore, the advanced EBP model (ASHA, 2023) defines three components. Firstly, the “patient's and caregiver's perspective”, which includes the patient's values, individual circumstances, perspective of the caregivers. Secondly, it includes “evidence (external and internal)”, where external evidence refers to best current scientific literature and internal evidence refers to information from subjective observations or objective measurements about patients gathered during the treatment process. Thirdly, the “clinical expertise” refers to e.g., knowledge from education or critical thinking from professional experience.
Decision-making processes should be based on EBP. Decisions must be made throughout the therapy process (e.g., diagnosis, intervention, counseling). There are two well-known concepts of decision-making: evidence-based decision-making and shared decision-making.
Evidence-based decisions should be based on external and internal evidence, clinical expertise, and the perspectives of patients and their caregivers (ASHA, 2023). As a result, they can provide quality services that reflect people's values and needs. Evidence-informed decision-making in clinical care and health systems has evolved from EBDM. This development focuses on the fact that other factors (e.g., institutional context, equity, feasibility, affordability, sustainability) should be included in the decision-making process; this is in addition to the forms of evidence mentioned so far [World Health Organization (WHO), 2021]. Emphasis is on a reflective approach to the sources of information (e.g., clinical care, health systems) on which decisions are made.
SDM involves clinicians and patients making decisions together based on the best available evidence. Patients are encouraged to think about treatment options, the benefits and limitations of each option, and to communicate their preferences. Patients' autonomy is respected and their involvement is enhanced (Elwyn et al., 2010; Elwyn, 2020). Key components of SDM are (1) understanding what constitutes a decision and acknowledging decisions, (2) communication and collaboration among all involved persons, and (3) existing power and dependencies (e.g., professional role, status, knowledge) between patients and clinicians (Elwyn, 2020). Thus, SDM focuses on the social interaction among all parties involved in the decision and all the associated knowledge bases and forms of interaction.
Both concepts, EBDM and SDM, serve to ensure that patients receive high quality care that is based on the best available evidence. While EBDM focuses on the incorporation of diverse evidence into decisions (ASHA, 2023), SDM aims to ensure that patients are fully informed so that they can share decisions with professionals (Elwyn et al., 2010, 2012). In a systematic review, Stacey et al. (2017) show that SDM results in, e.g., patients becoming more knowledgeable, more confident in their decisions, and more actively involved in the decision-making and care process.
In person-centered health services for children and adults, the International Classification of Functioning, Disability and Health (ICF) can be used as a classification of health and health-related conditions. The ICF is an international framework for organizing and documenting information on functioning and disability. This model provides a multi-perspective, biopsychosocial approach that describes (1) functioning and disability in terms of the body (=body functions and structures) and activities and participation, and (2) contextual factors (=environmental, personal) (World Health Organization (WHO), 2013).
Using the ICF model, SLPs can systematically gather and link information from the different levels of the ICF model with information from external evidence, clinical expertise, and patient preferences in decision-making processes, e.g., when determining therapy goals, to measure patient-reported outcomes (Threats, 2008, 2012). This practice in decision-making can support striving for independent living and social participation for patients and thus pursue the fundamental goal of speech-language pathology (Threats, 2008, 2012).
In addition to the two concepts of decision-making and the ICF model, it is also interesting to consider whether and how EBP and other factors influence the clinical decision making of SLPs. In SLP, clinical decisions should be made with the patient and, when appropriate, the family member. This is intended to increase patient participation in SLP and ensure therapeutic success (Günther, 2013; Furlong et al., 2018). This goes far beyond the mere provision of information by patients and the naming of their ideas as forms of participation. In ICF-oriented and evidence-based therapy orientation and goal setting, as well as in complex disease manifestations, the continuous inclusion of patients' needs and their involvement in decision-making is required in order to do justice to the individuality of the patient (Günther, 2013). Furlong et al. (2018) also emphasize that clinical decision-making processes in in-person services with children with speech and language disorders must be deeply individualized. As EBP is a patient-centered approach, evidence from research and clinical evidence must be continuously related to the needs of individual patients (e.g., values, preferences, living environment). This dynamic process enables individualized and evidence-based healthcare (ASHA, 2004).
Selin et al. (2019) present that various clinical factors of children (e.g., using verb tenses, forming complex sentences) influenced SLPs' decision-making process when diagnosing and treating children with specific language disorders. Thus, the characteristics of the children influenced the decision-making process more than the characteristics of the SLPs. Nevertheless, practice-based evidence as a characteristic of SLPs (e.g., clinical experience, qualifications, colleague opinion) strongly influences the clinical decision-making process (McCurtin and Clifford, 2015; Selin et al., 2019). Similarly, the interpretation of diagnostic results and the interpretation of clinical symptoms influence the decision-making process (Selin et al., 2019). McCurtin and Clifford (2015) illustrate that SLPs with additional qualifications and long-standing professional experience made treatment decisions based on scientific knowledge and paid less attention to patient preferences.
In addition to external evidence and patient and clinician characteristics, workplace conditions influence the decision-making processes of SLPs. Time pressure, task density, guidelines, prescribed treatment pathways, ethical and financial considerations, etc. influence clinical decision making in the diagnostic and therapeutic process (McCurtin and Clifford, 2015; Furlong et al., 2018; Selin et al., 2019). McCurtin and Clifford (2015, p. 1179) assume that “pragmatic and contextual reasoning” emerges from workplace conditions and influences decision-making processes.
The aforementioned literature focus on the various components of EBP and factors that influence clinical decision making in in-person service. In March 2020, it became possible for the first time in Germany to offer and perform video-based therapy in outpatient SLP. Due to the COVID-19 pandemic, a temporary special permit was granted to offer video-based telepractice to people with certain disorders (e.g., voice disorders, orofacial myofunctional disorders, stuttering, aphasia). Because (evidence-based) decision making in SLP is a relevant topic in literature and research, it is relevant to investigate how different forms of EBP and other factors influence SLPs' decision-making processes in video-based telepractice. The research question of the study was: how do decision-making processes occur between patients and SLPs in video-based telepractice in outpatient service, and what components of evidence do they take? The aim of the study was to conduct the first analysis of video-based telepractice in outpatient SLP services during the COVID-19 pandemic in Germany. Of particular interest was how evidence-based decision-making was realized.
Therefore, a qualitative research design was chosen to answer the research question in a methodological appropriate manner.
This paper reports on data collected within the research project “Videotherapie in der ambulanten logopädischen Versorgung” (ViTaL). The research ethics committee of the University of Applied Sciences and Arts Hildesheim/Holzminden/Göttingen (HAWK) approved this study. The data represented in this study are based on a video interaction analysis (Tuma et al., 2013). Here, five recorded video-based telepractices were analyzed to describe how evidence-based practice, specifically decision making, occurs in video-based SLP.
Qualitative research is used to explore issues or phenomena and to describe their characteristics, complex relationships, contextual conditions, and subjective experiences and meanings in order to understand the issue or phenomenon (Creswell, 2007; Maxwell, 2013). In qualitative social research, there are various methodological approaches (e.g., ethnography, phenomenology, grounded theory, narrative research), which are well known in the social, behavior, and health science literature. Each approach offers a systematic procedure based on methods described in the literature, so that data collection and data analysis are not carried out arbitrarily, but comprehensibly and according to criteria for qualitative social research (e.g., inherent openness, flexibility, adequacy) (Creswell, 2007; Maxwell, 2013). The research process is framed by a theoretical paradigm (e.g., constructivism, hermeneutics). The selection of the theoretical paradigm is based on the research topic and forms the methodological framework of the research process. From this, research strategies (e.g., ethnography, phenomenology, participation observation) and methods of data collection and analysis (e.g., interviewing, observation, focus group, textual analysis, visual analysis) are determined (Creswell, 2007).
Ethnographic research as an approach of qualitative-interpretive research observes social interactions and describes the commonly developed and shared patterns of behavior, values, language, beliefs, etc. of people or groups. The meaning of these patterns in the respective context is examined (Creswell, 2007; Knoblauch and Schnettler, 2012). There are different types of ethnography, e.g., realistic ethnography, autoethnography, confessional ethnography, visual ethnography (photography, video) (Creswell, 2007). The methodology of interpretive video analysis is influenced by the ethnomethodological tradition of conversation analysis. It reconstructs the practices that people use in their everyday lives to make themselves understood by other people. Through these familiar practices, through interaction and reflection on actions, people generate a construction of social reality. The social structures of this reality have to be considered in their situational context (Knoblauch and Schnettler, 2012; Tuma, 2018).
Ethnographic research methods are described in the literature on speech-language pathology care, such as the ethnographic interview (Westby et al., 2003) or the qualitative and/or quantitative analysis of video recordings of in-person therapy with people with aphasia (Merlino, 2021) or home-based video recordings of typical everyday situations of children with language development disorders (Overby et al., 2019) or of children with or without autism (Watson et al., 2013). However, video recordings are also used in seminars for SLPs to strengthen their observation and reflection skills through retrospective analysis (Stokes, 2013).
Outpatient SLPs were recruited by newsletter, social media, homepage, etc. of the Deutscher Bundesverband für Logopädie e.V. (dbl) (the official national professional association of logopedics in Germany) and other research networks (e.g., working groups, students, alumni) (Figure 1). SLPs were asked to record their video-based telepractices.
In May 2020, nine interested SLPs were introduced to the entire project and its requirements, during an online video conference. They were given a written description of the project, the informed consent form, and the privacy policy to participate in the project. For all documents, there was a version for the SLPs and a version for the patients. As the purpose of the study was to explore the decision-making process in video-based telepractice in outpatient service, the only criterion for recruiting patients was that their synchronous therapy had to be video-based. No other inclusion criteria were communicated to SLPs to recruit patients. The reason for this is that it was not possible to assess whether SLPs and patients would be willing to record the video-based telepractice because it was a new medium and some of the use of it was still uncertain.
Since no recordings of video-based telepractices had been made up to that point, recordings of all disturbance patterns, symptoms, therapy phases, etc. were considered relevant for the initial collection and analysis of this data material. Furthermore, the infrastructure (e.g., low internet capacity, software without recording mode), the additional organizational effort for the SLPs and the insight into the privacy of the patients could have argued against recording. Eight SLPs agreed to record video-based telepractice for one to seven patients each. From May 28, 2020, to July 30, 2020, the participating SLPs recorded 23 video-based telepractice sessions, which were provided to the researchers: one video recording of one patient at a time (SLP1, SLP3, SLP6, and SLP7), two video recording of one patient at a time (SLP5, SLP8), three video recordings from two patients (one from one patient and two from another) (SLP2) and 12 video recordings of seven patients (one to four recordings per patient) (SLP4). In addition, the SLPs completed a short questionnaire with sociodemographic questions about themselves as therapists and about their patients (Table 1).
SLP1 and SLP3 are students in their 6th semester of seven semesters of studying at a university. From the beginning of their studies, they observe SLP services and increasingly assume the role of therapist or co-therapist under the supervision of their teachers. The combination of professional knowledge, practical experience and critical reflection takes place from the beginning of the study in order to obtain their state license to work as a SLP at the end of the 6th semester. Thus, it can be assumed that the selected students are novices in the learning process of developing an understanding of EBP and skills for implementation of evidence-based decision making.
The SLPs recorded the video-based telepractices either with the videoconferencing software they used (ZOOM: SLP1, SLP3, SLP4, SLP6, SLP7, and SLP8) or with the free software OBS (www.obsproject.com/de) if the telepractice could not be recorded with the videoconferencing software (e.g., RED connect: SLP2, Sprechstunde online: SLP5).
Each SLP received a link and password e.g., to upload the video files to the HAWK's password-protected cloud. One SLP (SLP4) was unable to upload the video files to the cloud because of a very weak Internet connection. These video files were encrypted on a USB flash drive and were sent by postal service. MB received the USB flash drive and uploaded the video files to the cloud. All video files were stored in the HAWK cloud by MB under anonymized labels.
As more video recordings were provided than could be analyzed, 5 video recordings from different SLPs and patients were selected. Consideration was given to the principle of qualitative research to select cases for data analysis that represent the diversity of individuals, settings, or behaviors (Maxwell, 2013). Purposeful case selection was also guided by identifying variations in the typical population and then systematically selecting cases that represented the most important variations. Minimum and maximum variations were also considered.
Breidenstein et al. (2013) recommend and justify five case selection criteria in ethnographic research to select appropriate cases for analysis when faced with large amounts of fieldwork data. In the study, these criteria were followed to select SLPs and their patients for data analysis. Cases were selected at the level of individuals, specifically SLPs, because it was assumed that decisions in the therapy process are primarily made by SLPs and that decision-making processes are initiated by SLPs. The key criteria for this study were that the spectrum of the research field be represented by SLPs and patients, and that the data show decisions and decision-making processes in great detail. This approach followed an iterative process, using the five selection criteria in a circular rather than linear way (Breidenstein et al., 2013). This was in accordance with the basic principle of minimum and maximum contrast in qualitative research (Glaser and Strauss, 1998).
The selected cases (e.g., interview passages, video recordings) must be particularly rich in detail (Breidenstein et al., 2013).
In this study, the video recordings provide a detailed account of the therapy that took place and the interactions between patient and therapist. For data analysis, video recordings were selected in which decision-making processes (e.g., agreeing on the exercise modification, demonstrating different exercise options) or decisions made (e.g., determining the next exercise, determining the exercise modification) were evident. In the selected video recordings, the results of making decisions with or without giving reasons (SLP1 to SLP8) and of negotiating and deciding together (SLP1, SLP3, SLP5) were identifiable. Due to existing shared decision-making processes, the records of SLP1, SLP3 and SLP5 were selected for analysis. The video recording of SLP6/P6 was selected for maximum contrast. It did not show any negotiation and decision making processes between the patient and the SLP.
SLP7 (female, 22 years old, student/6th semester) was excluded from the data analysis because the video-based telepractice was recorded with an external camera, which severely limited the sound quality and thus the intelligibility of the patient's verbal communication. In addition, the external camera focused the patient's image on the screen, so that the therapist's nonverbal communication was barely visible and thus could only be analyzed to a limited extent.
The transcripts were as detailed as necessary to address the research question and objectives of the study. Pauses, symptoms, repetitions, volume, gestures, and interruptions etc. were used in the transcription to represent social interaction, especially in the decision-making process. In addition, technical difficulties (e.g., delayed audio and video transmission) and the reactions of the SLP and patients were transcribed. No video recordings were excluded from data analysis due to technical difficulties (e.g., delayed audio transmission, interrupted internet connection).
The selection of cases follows the principle of contrast. The cases represent the spectrum of possibilities by showing as much variance as possible (Breidenstein et al., 2013).
In this study, the cases are intended to represent the spectrum of speech and language therapy. The principle of minimum and maximum contrast is the guiding principle. In order to represent the investigation field as broadly as possible, similar cases and very different cases were selected. Information from patients and therapists sociodemographic questionnaires was used. Based on available sociodemographic data of patients and SLPs, 5 individual cases were selected to represent the heterogeneity of patients and SLPs. Among SLPs (SLP1 to SLP8), e.g., work experience ranged from academic training (3 years) to 29 years, and working focus ranged from no focus in academic training to a focus in, e.g., pediatric or neurological work area. The 15 patients e.g., ranged in age from 6 to 82 years, and symptoms included fluency disorders (stuttering, cluttering), developmental language disorders, orofacial myofunctional disorders, aphasia, dysarthria, and voice disorders. The video recording of the youngest patient (P3) was chosen so that the age contrast with P2 (60 years old) and P4 (78 years old) would be maximum. Selection criteria included patients' symptoms to reflect the numerous symptoms and treatment methods, and the number of previous video-based telepractices to reflect the frequency of use and experience with video-based telepractice.
SLP1 and SLP3, both students with little professional experience and both treating a patient (P1, P3) with stuttering, form a minimal contrast to each other. The maximum contrast is SLP2, SLP4 and SLP5 with more professional experience, different professional status and adults with language disorder (P2), neurogenic speech disorder (P4) and voice disorder (P5). SLP6 (female, 47 years, working focus: voice disorders, stuttering, children with speech and language disorders) was excluded because, like SLP1 and SLP3, she treated a patient with stuttering and, like SLP4 and SLP5, she is a practice owner with a similar working experience (18 years). SLP8 was excluded because she worked in an outpatient practice, had a bachelor's degree, was of the same age and had the same work experience (as SLP2), and had a working focus on developmental language disorders (as SLP5). She also had a child with a total number of previous telepractice of 10 (similar to P1 and P3).
Events (e.g., situations, people) that the participants themselves identified as particularly important (Breidenstein et al., 2013).
In this study, participants were informed through the study information and online study presentation that decision making and decisions made during the delivery of video therapy would be analyzed. They made their own decisions about which video-based telepractice to record with which patients, and then they decided which video recordings to make available to researchers. This was not influenced by the researchers. In this way, the SLPs were able to select the video-based telepractices of the patients that they considered to be most relevant. The reasons given by the participants for the selection of the patients and their recorded video-based telepractice were the consent of the patients or their relatives, the symptoms of the patients, or the own working focus. Based on the research question and the purpose of the study, sequences were selected and analyzed by the researchers in which explicit decision-making by SLPs and patients and the negotiation of decisions in video-based telepractice were evident.
Criterions such as representativeness, frequency, and everydayness can also be used to select cases (Breidenstein et al., 2013).
In this study, no recorded video-based telepractices of SLPs and patients were excluded based on this criterion. The five selected cases (Table 2) illustrate typical symptoms of disorders in SLP, the age range of patients, and the known methods of treatment in SLP. In the case of the SLPs, the professional field is represented by different levels of professional experience, the existence of the working focus, and the beginning of the offering of video-based telepractice. Table 2 lists the information obtained from the sociodemographic questionnaires of the patients and the SLPs who were selected for the data analysis.
Case selection can also focus on the unusual, the unexpected, and the misunderstood. Analyzing situations that cause confusion makes it possible to focus on the differences between the culture of the participants and the cultural self-evidence of the observer (Breidenstein et al., 2013).
The researchers' assumption that SLPs give reasons for their decisions led to a search for sequences of decisions in which no reasons were given. It turned out that all the video recordings showed sequences in which the SLPs did not give reasons for their decisions. Therefore, this did not become a criterion for case selection. In one recording (SP2/P2), a decision made by the SLP to perform the exercise was corrected by her after P2 asked several times. Because of this, this video recording was selected for analysis. Other sequences, such as patients disagreeing with the SLP's decisions, or a negotiation process not being completed due to technical difficulties, did not occur in any of the 23 video recordings.
All of the recorded telepractice sessions are equivalent to a 45-min therapy session, which is most common in Germany. During the video-based telepractice, all patients were at home (e.g., in the kitchen, living room, or workroom at home). The SLPs were located in a therapy room in the outpatient clinical practice (SLP1, SLP3, and SLP5) or in their home office (SLP2, SLP4). Within this study, the start of the video-based telepractices was defined when the SLPs enter the digital space of the videoconferencing software. The end was defined when the patients and SLPs say goodbye (SLP1, SLP2, SLP3, SLP4) or when they are interrupted due to technical problems (SLP5). Based on the therapy process, all video-based telepractices demonstrated treatment sessions.
The participating SLPs used various hardware (e.g., computer, laptop, tablet, etc.) and software (e.g., ZOOM, Red Connect) for video-based telepractice. The synchronous therapies were always performed using audio and video transmission. Various features of the videoconferencing software (e.g., screen transfer, screen sharing) were used to show digitally recorded home practices or videos. The video feature was often used to display therapy materials in front of the camera for the other person to see. Due to the limited capacity of the internet, technical problems, such as audio and video transmission interruption occurred. To handle this, therapists and patients agreed to use the chat function of the videoconferencing system if the audio transmission was severely delayed and they could no longer understand each other, or to ignore the poor video transmission and concentrate on the audio transmission. Another way of handling technical malfunctions was for therapists and/or patients to log back into the videoconferencing system.
It is important to note that the patients and SLPs were largely familiar with the technical use of videoconferencing software at the time the video-based therapies were recorded. However, social interaction via a videoconferencing system was unfamiliar to the SLPs as well as to the patients and their families compared with social interaction in in-person therapies. It should also be noted that all patients were in the “intervention” phase of therapy and were receiving individual therapies.
The data were analyzed based on the interpretive video interaction analysis (Tuma et al., 2013). A distinctive feature of video interaction analysis is that it analyzes video recordings that document social actions and practices in natural, everyday situations (Knoblauch and Vollmer, 2018; Tuma, 2018). Thus, these situations were not produced specifically for the research project. They would have occurred even if the researchers had not commissioned the recording. The task and goal of video interaction analysis is to analyze the audiovisually perceptible practices and actions of the actors as a process. Consequently, it is not still images from video recordings that are analyzed, but always sequences of nonverbal and verbal interactions in order to reconstruct social action as a process (Tuma et al., 2013; Tuma, 2018). The video recordings are used as a research medium, to study nonverbal and verbal communicative interactions between all persons in social situations. The purpose is to sequentially analyze and interpret interactive practices in situationally produced social reality (Knoblauch and Schnettler, 2012; Tuma, 2018). The ethnomethodologically based video interaction analysis reconstructs the order of social interactions in the situation and focuses on both spoken language and nonverbal modalities. Depending on the research question and the topic of the research project, e.g., mimic, gestures, symbols, sounds, language, body posture are analyzed as elements of nonverbal and verbal interaction (Moritz, 2018)
Within this study, the social interaction between patients, relatives and SLPs were studied to analyze the clinical decision-making processes that are routinely used in video-based telepractice in outpatient services. The various phases of data analysis were initially carried out by MB (first author). The results were then discussed in ongoing meetings of the research team (MB, SW, BB, and JL) in an analytical and critical-constructive exchange of expertise. Discussions included e. g. the marked sequences per analysis protocol, code naming, assignment of overarching themes, criteria for minimum and maximum contrasts for comparing cases (SLP/P) and sequences. This was done by constantly alternating between analyzing and discussing in order to secure the analysis process and the results. Thus, there was a constant comparison of sequences with similar and varying sequences (e.g., transition to a new exercise, repetition of an action) within and between cases. In this way, the principles of credibility and dependability (Yadav, 2022) for qualitative research were observed.
The interpretive video interaction analysis was realized in two steps: within-case analysis and cross-case analysis.
The first step was to analyze the social interactions of each case individually in the video recording. In this way, the social decision-making processes in different sequences of video-based telepractices will be described. The video recordings were analyzed in terms of how decisions are made during and within the interaction between the patient and the SLP and which elements indicate decision-making processes. An analysis protocol was used for transcription and analysis (Figure 2).
In the first column of the table, the timecode is entered to mark the time of the sequence. In the “SLP” and “Patient” columns, all verbal utterances, nonverbal elements (e.g., facial expressions, gestures, direction of view, posture, showing pictures), and technical features (e.g., beginning and end of screen transmission) were transcribed. Furthermore, paralinguistic elements were included in the transcription (e.g., duration of a break: (3)–break of 3 seconds; intonation: emphasized word–“That was much louder! very good.”). For this purpose, the simple transcription system of Dresing and Pehl (2015) was used. Transcribing was done by MB. Within this study,
First, MB marked the sequences in the transcripts in which she identified decisions made and decision-making processes. In constant comparison with the video recording, the transcript of each individual case was divided into sequences, and sequence markers were set in relation to the research questions (internal sampling) according to the interpretative video interaction analysis (Tuma et al., 2013). Verbal elements of explanation (e.g., because, in order to, due to) and nonverbal elements (e.g., head shake, shoulder shrug) that could indicate agreement, disagreement, or indecision were used to determine the sequences. New verbal and nonverbal elements were continuously compared with the previously analyzed elements from the other analysis protocols to identify similarities and differences and to further develop the results (Glaser and Strauss, 1998). For instance, reflection of self-perception and perception of others, completion of an exercise or instruction of a new exercise were categorized as nonverbal and verbal communication. In this way, minimum and maximum contrast sequence comparisons could be determined during the course of the video-based telepractice for subsequent fine analysis. Maximum contrast sequences include e.g., sequences with decisions with and without explanation, or sequences in which a decision is negotiated between the patient and the SLP vs. sequences in which a decision is predetermined by the SLP. Minimal contrast sequences are, e.g., sequences in which decisions are negotiated between the patient and the SLP, but the patients are of different ages, or sequences in which the SLP explains a decision and the explanations are based on the therapist's experience or on the approach of the therapy method. These marked sequences were then reviewed and discussed with the other members of the team (SW, BB, and JL). As a result of all five within-case analyses, four sequences with decision processes (negotiation, weighing arguments) and 26 sequences with explanations and 61 with decisions without explanations were identified as relevant for further analysis. The sequences ranged in length from 1:24 min to 9:37 min. A blank line was inserted after each sequence in the analysis protocol. This separates the sequences from each other.
The purpose of the detailed analysis was to analyze and compare different sequences of a single case. In addition to analyzing the multiple occurrences of similar actions by one person in a sequence (e.g., asking a question, shaking one's head, interrupting the practicing verbally or nonverbally), special attention was paid to identifying the specifics of the interaction between the patient and the SLP in that sequence were identified (e.g., verbal and nonverbal responses (SLP) to shaking one's head (P) or, after asking a question (SLP) waiting for the response or providing response options). The qualitative analysis was documented in the fourth and fifth columns. Following the grounded theory, the coding process and category formation were conducted (Strauss and Corbin, 1996; Glaser and Strauss, 1998; Dietrich and Mey, 2018). For the nonverbal and verbal elements that were present in these sequences, short labels were noted as initial codes in the fourth column in order to reconstruct the meaning of the segment. In this phase of coding the first case (SLP1/P1), four overarching coding themes emerged to which initial codes could be assigned: (1) default vs. negotiation (SLP), (2) nonverbal/verbal element of interaction, (3) action-related phenomenon, and (4) form of evidence/influencing factors. Consequently, the fourth column of the analysis protocol was divided into these four themes. Table 3 illustrates two examples.
The coding themes were used in the initial coding of the other four cases. During this inductive procedure, the coding themes were confirmed. In doing so, the qualitative principle of the inductive procedure was followed. Therefore, there was no list of expected, known from literature interactions that were deductively searched for in the transcript. At this stage, any notion that arose while analyzing the material was allowed to flow. Categories were then formed from the overarching themes that emerged from the initial coding and were noted in the fifth column (Table 3).
This also took place in the comparative approach of the grounded theory methodology (Strauss and Corbin, 1996; Glaser and Strauss, 1998; Dietrich and Mey, 2018).
On the one side, actions and interactions in which decisions or decision-making were analyzed in individual cases and which were similar in content were now compared across cases. The similarity of content referred, e.g., to the request for self-assessment (SLP), the verbal and nonverbal response (P), and the subsequent reaction (SLP), or specifying the target action with or without reasoning (SLP), performing the exercise (P), and receiving feedback the SLP. The contrast was in the different contexts (e.g., symptoms, presence/absence of relatives, number of previous therapies). Typical courses of interaction were reconstructed in a differentiated way.
On the other side, sequences of interactions with a similar context were compared (e.g., involvement of relatives, teaching self-awareness to patients who had never received in-person therapy, consolidation of speech modification techniques).
The cross-case analysis of similar interactions aimed to describe the temporal sequence and structure of the interaction between the patients and the SLPs. This was to reconstruct across cases how decisions are made or how decision-making occurs in video-based telepractice.
The results indicated that SLPs maintain strategies for a common basis of interaction during video-based telepractice. Nonverbal and verbal communication as part of social practices was limited by the resulting delays in audio or video transmission. To overcome these difficulties, SLPs and patients used various technical interaction strategies. For instance, at the beginning of the treatment, they agreed to use the chat function, to focus on the sound transmission, or to ignore the limited image transmission. In this way, they re-established a common basis for interaction.
In addition, pragmatic practices (e.g., gesture, including head shaking, nodding, hand gestures; pauses in fluent speech) that SLPs and patients used to maintain their interactions were demonstrated. It was noticeable that patients and SLPs sometimes could not see each other. It was not maintained when practice materials were held in front of the video camera, or when patients looked down while writing or reading and talking to the SLP, or when the SLP explained something to them.
By analyzing the data, it could be reconstructed that the decision-making process is strongly influenced by the social interaction between the patient and the SLP. A paternalistic interaction or participative interaction between patients and SLPs characterizes decision making in video-based telepractice (Figure 3). The descriptive characterization of the two styles of interaction applies to the social interactions in video-based telepractice in outpatient SLP services analyzed in this qualitative study.
A paternalistic interaction by the SLP was most evident when structured treatment (e.g., LSVT LOUD®) were used. A more participative interacting was observed in the video-based telepractice, where different individual exercises were combined (e.g., symptomatic voice therapy). The analysis showed that the patient's age, symptoms, total treatment time, etc. had less influence on the decision-making than the style of interaction. In the cross-case analysis, it became clear that negotiation to decide how to perform the next exercise (Case 3: 2 sequences; Case 5: 1 sequence) occurred in both Case 3 (SLP: 22 years/P3: 6 years) and Case 5 (SLP5: 53 years, P5: 49 years). Similarly, both SLPs give a similar number of decisions without giving reasons (SLP3: 11; SLP5: 12) and decisions with giving reasons (SLP3: 2; SLP5: 5). Although both cases are maximum contrasts in terms of age, no difference in decision making could be found. The cross-case analysis also revealed that in all cases there were more decisions without reasoning given (SLP1: 14, SLP2: 13, SLP3: 11, SLP4: 11, SLP5: 12) than decisions with reasoning given (SLP1: 8, SLP2: 3, SLP3: 2, SLP4: 8, SLP5: 5). This is done in patients with different symptoms (e.g. stuttering, aphasia, voice disorder) and with different total treatment time: from 1 month (P2) to 6.5 years (P1).
The SLP's paternalistic interaction characterized social interactions, e.g., by “determine target action” within a therapy sequence or by “determine home practice.”
SLP2: (holds an image card in front of the camera) “What is important to me today is that you also tell me the generic term. it's still a bit difficult (removes image card, looks at screen) to find a generic term for everything in this category. the generic term is especially important to me today. that you find that for the, uh, the pictures that we have now. (holds an image card in front of the camera, SLP2 is not visible (3) SLP2 removes image card, looks at screen)
P2: “This is (2) uh one (3) u::ch”
SLP2: (holds an image card in front of the camera, is not visible)
P2: (looks left, looks at screen) “That is always so difficult to find the (1) the generic term.”
SLP2: “That's what I explained to you before, that everything got a bit mixed up because of the stroke (2) and we're trying to sort it out now. (1) and this categorizing, which you also have to do as home practice from time to time, or now you find these generic terms, that just helps you. (3) and that's why we do/
In quote 1, it can be seen how the SLP2 determines the target action without asking the patient how relevant the goal of the exercise is for him, and whether, and if so, how, the exercise could be performed. She does not respond to his nonverbal and verbal signals (e.g. looking away from the screen, expressing displeasure), but justifies why this target action is necessary based on the cause and symptoms of the disease. The target action and goal are predetermined by the SLP and there is no negotiation or modification of the exercise.
SLP also mentioned their clinical expertise and experience. The focus was on the correct execution of the actions, and the clinical expertise of the SLPs determined the therapeutic approach, i.e., SLP1 asks for the patient's self-assessment of his use of speaking technique using specific criteria and also self-assesses his use of speaking technique using the same specific criteria (quote 2).
P1: “Yes. (1) subtract” [applies speaking technique] (laughs)
SLP1: (laughs) “Oh, you have chosen some difficult words! wow! (laughs)
P1: “Yes.” (laughs)
SLP1: “I'm going to ask you again for the criteria and you can just give a thumbs up (shows it) or thumbs down (shows it). okay?”
P1: “Yes.”
SLP1: “Was it long enough?”
P1: “Yes.” (he stretches up his right thumb)
SLP1: “Yes! it was long enough. (1) was it loud enough?”
P1: “Yes.” (he stretches up his right thumb)
SLP1: (nods) “Yeah, I think so too. so, with the “s” I think you can be much louder than with the “m”. it's really less of an issue. (1) and how was the transition to the vowel?
P1: (looks down, yawns with mouth closed, looks at screen, smiles) “That was very good. yes.” (he stretches up his right thumb)
SLP1: (nods) “Yes, I thought so too. (nods) was fine. great! (1) then try again. again, stretch long enough, but just long enough so that you still have enough air for the rest of the word. okay? so you can memorize it well. (1) here we go.”
She does not link the evaluation of his speaking to his wishes for therapy. SLP partly justified their decisions by referring to the patient's therapy goal or to previous successes or difficulties in practicing. The SLPs often did not explain to the patients and the continuously present (P3: mother) or partially present (P2: wife) relatives why a target action had to be repeated, or they decided to start a “new target action.”
A participative style of interaction was evident in the video-based telepractice when the SLPs asked the patients to rate their perception of the vocal quality or their effort during “perform target action” (quote 3).
P5: (1) “Ni(.)ha ni(.)ho. (.) ni(.)ha ni(.)ho. (.) ni(.)ha ni(.)ho. (.) ni(.)ha ni(.)ho. (.) ni(.)ha ni(.)ho.” (.)
SLP5: “OK. let it go. feel, sense. is the feeling still here now? (hand on chest) has it increased? has it decreased? (2) is the breathing more stimulated than before?”
P5: “It is mainly that it sticks so much here (the left hand to the lower right costal arches) (.) yes, such a sticky feeling is (.) it's almost like that, yes, like when so layers stick together. and if I do that a few times, it will unstick. (.) and now it's good. so it's less here (.) in the abdomen (.) the further feeling is than so more back here, which I feel is very pleasant.” (both hands are in the lumbar region)
SLP5: “Yes, okay. then let's do a little stretching exercise one more time. (.) you can see me, can't you?”
During voice training, SLP5 asks the patient how she assesses her breathing (quote 3). This requires the patient to be able to perceive, describe and assess herself and her breathing. SLP5 confirms the patient's self-assessment and, based on this, provides a new target action that relates to the patient's self-awareness. She uses the patient's self-awareness to continue voice therapy.
Based on the self-assessment, but also on the patient's needs, negotiations took place between the patients and the SLPs about, e.g. “repeat action” or “extended practice.” In these more participative interactions, patients' self-assessments were used as starting points for modified action or new target actions. When interacting with patients in this way, SLPs brought their clinical expertise and experience, as well as specific knowledge from previous therapy sessions with each patient. The shared dialogues and patient self-assessments allowed the SLPs to flexibly adapt interventions to the current needs, everyday communication situations and the individual living environments of the patients on a situation-specific basis.
Shared decision-making processes took place, e.g. after the self-assessment of the previous implementation and documentation of homework by the patient (P1) or by the mother (P3). Afterwards, the patient respectively the mother and the SLP discussed and decided how to implement home practice more often in the future (P1) and how to use popular and existing games at home (P3). With P3 and P5, further exercise actions were discussed together, taking into account preferences (P3) and physical self-awareness (P5) in the decision-making process. Negotiations in the decision-making process took place in participative interactions.
The data analysis revealed that SLPs rarely explicate their internal decision-making process and thus rarely explain or justify their decisions to patients and relatives. As a result, it is not clear to others on what professional basis the decisions were made, e.g. to “correct” the patient's target actions or to “finish action” and “determine new target action.” When SLPs justified their decisions, they referred to their expertise (e.g., on the symptoms of the disease, on the implementation of the therapy method) and to previous experience with the patient (e.g., progress in the course of therapy, self-assessment skills). The SLPs justified their decisions in participative and paternalistic interactions with the patients and relatives. The internal evidence and the client perspectives were expressed in different degrees of explicitness. No explicit inclusion of current external evidence (e.g., guidelines, scientific evidence) could be reconstructed when analyzing video-based telepractice.
Based on the results of the within-case and of the cross-case analyses, a process model was developed which illustrated how patients and SLPs interact during a video-based telepractice session (Barthel et al., 2021a). Three phases characterize video-based telepractice sessions: (1) situational, content-based arriving, (2) interactive, process-based treatment, and (3) situational, content-based closure (Figure 4).
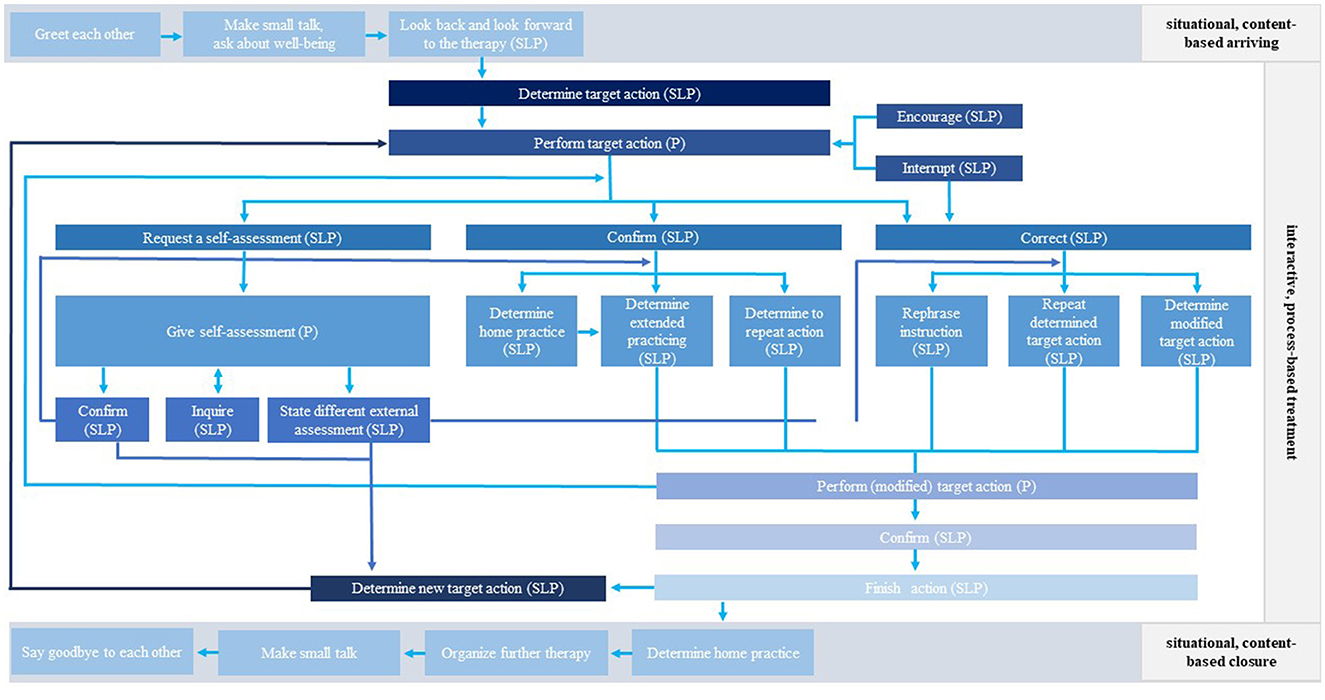
Figure 4. Process model of patient-therapist interactions (P: patient, SLP: speech-language pathologist) (Barthel et al., 2021a).
The visible and audible interactions in each phase and the resulting interaction process throughout the therapy session are based on decisions made by the SLP and the patient. On the one hand, decisions relate to content related structural aspects of speech and language therapy, such as the therapy method or the transfer of practice as the next therapy step. On the other hand, decisions refer to the concrete interactionist situation, such as “determine target action,” “confirm target action,” “request self-assessment,” and “determine home practice. The various decisions all lead to continuous practicing in the “interactive, process-based treatment” phase. They maintain the process-based interaction between patient and SLP.
With the introduction of video-based telepractice during the COVID-19 pandemic, SLPs needed to rapidly transition their outpatient service from in-person to video-based therapy. The study examined the decision-making that occurs in the interactions between patients and SLPs in a video-based telepractice. It focused on the components that characterize a decision-making process.
A common basis for social interactions in video-based telepractice is of fundamental importance for decision-making processes. Social interactions between patients and SLPs are characterized by verbal and nonverbal elements. This enables patients and SLPs to relate to each other and processual interaction can take place. The results of the study show that processual interaction is possible in video-based telepractice for people with communication disorders of different ages. Of course, powerful technical equipment (e.g., hardware, software and internet connection) is required for patients and SLPs to interact in video-based therapy (Bilda et al., 2020; Lauer, 2020; Barthel et al., 2021b). The availability of technical equipment (e.g., laptops, computers, cameras) among patients and SLPs, the availability of videoconferencing systems (e.g., Red Connect, Zoom) among SLPs, and the existing skills to use the technical equipment and functions of the digital applications enabled patient's digital participation in health care. In this way, the health care in outpatient SLP services could continue without interruption due to restrictions during the COVID-19 pandemic.
When SLPs explicitly name their decisions, they use their clinical expertise and specific knowledge to reason their decisions. Conspicuously, this knowledge is used in paternalistic interactions to ensure that e.g., the structured performance of LSVT LOUD® is done correctly. The structured performance refers, e.g., to the frequency and duration of practicing, as well as the order and repetition of practice sessions (LSVT Global, 2023). This did not take into account the individual living environment of the patients, their self-assessment and their needs. In more participative interactions, although specific patient-related knowledge and clinical expertise are also used to justify further action in therapy, the focus is on the patient's self-assessment (=client perspectives), available resources, and individual lifeworld. Higginbotham and Satchidanand (2019) suggest differentiating internal evidence into clinical expertise and internal evidence based on data-based knowledge of patient performance. Alternatively, the diamond model (Higginbotham and Satchidanand, 2019) can explain the different reasons for the decisions made by the SLPs very well. In a review, Fissel Brannick et al. (2022) pointed out the difference in terms and definitions for clinical evidence. They argue that clinical opinion, clinical expertise, and practice-based evidence should be clearly defined and used unambiguously in professional and interprofessional communication and in discussions with patients and their families (Fissel Brannick et al., 2022). The clinical evidence provided by the SLPs in the present study can be described as clinical expertise. In the cross-case analysis, it was found that the SLPs used different types of knowledge (e.g., previous experience with the patient, the patient's self-perception, knowledge of the therapy method) to make decisions such as “determine to repeat action,” “determine modified target action,” or “determine new target action.” Two essential attributes of good clinical decision-making are the use of multiple sources of knowledge and the needs of the patients (Fissel Brannick et al., 2022). However, it was not possible to reconstruct whether consensus recommendations, research findings or clinical expertise from other SLPs were used in the decision-making process. These are three more important aspects of clinical expertise in decision-making (Fissel Brannick et al., 2022).
In the paternalistic interactions and the participative interactions, decisions in the therapy process are made predominantly on the basis of the results of previous decisions. Thus, therapists and/or patients assume effects with respect to the previous course of action. All of the studies included in the scoping review by Fissel Brannick et al. (2022) were of interventions delivered in in-person settings. Although this review did not include a study that examined the use of clinical evidence in video-based telepractice, it is reasonable to assume that the use of multiple sources of knowledge is also relevant to video-based telepractice. It is important to examine what sources of knowledge SLPs use in addition to patient needs and their clinical expertise and interne evidence. As the use of video-based telepractice had only been available to all SLPs in Germany for a few weeks at the time of the study and social interaction via videoconferencing software was new to them, there was little expert advice from colleagues or professional associations. How SLPs acquired the knowledge to carry out video-based telepractice and what decisions that led to, e.g., implementing therapy methods in a modified manner or using familiar implementation from in-person therapy is currently not described in the literature. Differential knowledge of influences on clinical evidence may be relevant not only to in-person therapy (Higginbotham and Satchidanand, 2019; Fissel Brannick et al., 2022) but also to video-based telepractice, e.g., to distinguish between clinical opinion and clinical expertise and to understand their influence on the clinical decision-making process.
For paternalistic interactions and for participative interactions the external evidence (ASHA, 2004; Dollaghan, 2007) or external scientific evidence (Higginbotham and Satchidanand, 2019) could not be explicitly reconstructed in the analysis. The results of research or guidelines (=external evidence) were not an explicitly mentioned point of reference for decision-making. Greenwell and Walsh (2021) reported that SLPs use different sources of evidence. Client perspectives and external evidence were the most commonly named (Greenwell and Walsh, 2021). It would be interesting to know how the external evidence and client perspectives from patients and relatives, and the internal evidence from SLPs influence the decision-making and how they interact with each other. How patient-related clinical experience, clinical expertise, and current external evidence combine to lead to the best possible decision and treatment cannot be shown by video interaction analysis. However, different forms of evidence do influence decision-making in in-person therapy (Dollaghan, 2007; Higginbotham and Satchidanand, 2019; Greenwell and Walsh, 2021; Fissel Brannick et al., 2022).
However, the results of the video interaction analysis of this study emphasized that EBDM and interacting must be understood as a process. SDM as a social interaction is present, even if it is not always explicit in nonverbal and verbal communication. The participative approach of decision-making is evident both in asking for patients' self-assessment and needs for treatment and home practice, and in the communicative negotiation of therapy content and procedures. This promotes the digital participation of patients in the video-based telepractice. The results thus demonstrate two core elements of SDM: at least two people are involved and they share information (Elwyn, 2020). The other two core elements of SDM—focusing together on the further course of treatment and reaching consensus (Elwyn, 2020)—could only be reconstructed in short negotiation processes. There was no evidence of patient refusal or questioning of the clinical process during the participative interactions in video-based telepractice. However, this could lead to more content and goal-related justifications by SLPs and more communicative negotiation processes between patients and SLPs. Why patients did not inquire about the content of the practice, did not question it, or even reject it, could be due to the fact that only practices they were already familiar with were performed, that the explanations and the nonverbal and verbal specification of the target action were understandable, or that this pattern of interaction had consciously or unconsciously developed due to the previous number of therapy sessions.
Numerous reviews have shown that video-based telepractice is effective in a great many areas: adults with various communication disorders (e.g., chronic aphasia, dysphagia, primary progressive aphasia) (Weidner and Lowman, 2020), adults with Parkinson's disease (Theodoros et al., 2019), children and adults who stutter (McGill et al., 2019), parents of children and children with autism spectrum disorders (Neely et al., 2017; Sutherland et al., 2018), primary school children (4–12 years) with speech or language impairments (Wales et al., 2017), individuals with a recommendation for voice therapy (Rangarathnam et al., 2015), and individuals with acquired brain injury (traumatic brain injury or stroke) (Coleman et al., 2015) have all shown effective application of video-based telepractice. Due to the complexity of the diseases and various symptoms, it is important to consider the extent to which patients can digital participate in video-based telepractice, the role they are assigned, or the role they take on. Consequently, it is necessary to reflect on how digital participation and SDM can be realized in video-based telepractice. Special attention must be paid to the personal competencies of patients and their physical, linguistic, and cognitive abilities (Steiner, 2023) in order to enable digital participation in SLP services via video-based telepractice for patients of all ages and with different communication disorders. If necessary, technical and structural adaptations and changes in treatment performance must be made in order to provide digital health care (Steiner, 2023).
The role of the SLP also changes in video-based telepractice. Because video-based telepractice occurs at a physical distance (ASHA, 2020), the patient's physical self-awareness and self-evaluation (=client perspectives) seems to be more necessary than in in-person sessions. The SLP becomes a “verbal guide” for the patient. The patient must be able to tactilely and aurally perceive and verbally express himself or herself. Based on self-assessment and the reported needs, the SLP must be situationally flexible in deciding how to proceed with the video-based practicing. Incorporating client perspectives as a feature of participative interactions challenges the SLP to be able to quickly combine client perspectives and clinical expertise. In addition to client perspectives, participative interactions also take into account the individual's lifeworld. SLPs ask about the patients' material and social resources. Patients use materials that they have at home and also use for home practice. As a result, SLPs are better able to support the transfer of practice content to the patient's everyday life because the SLP can see where the patient lives, how he or she practices at home, and what he or she uses to do so. Video-based telepractice allows SLPs to incorporate individual resources and the patient's home and living environment into decisions. This can be an opportunity to increase patient adherence to treatment and goals, and to promote transfer (Barthel et al., 2021b).
The results of the present study are consistent with international findings (e.g., Coleman et al., 2015; Rangarathnam et al., 2015; Wales et al., 2017; Sutherland et al., 2018; McGill et al., 2019; Theodoros et al., 2019; Weidner and Lowman, 2020) that show video-based telepractice can be delivered to individuals with different communication disorders (e.g., aphasia, stuttering, voice disorders) and clinical conditions (e.g., Parkinson's disease) of different ages. One way that people with communication disorders across the lifespan can digitally participate in healthcare is via video-based telepractice as a digital form of outpatient SLP service. Speech and language telepractice is considered necessary in the German health care system, among other things, to counteract physical distances and limited mobility, to integrate the evidence-based transfer of therapy content more strongly into the patients' lives. Video-based telepractice is necessary to meet the advancing digital healthcare.
The small sample size imposes restrictions on the generalizability of the findings. Further studies with higher sample sizes are warranted. Furthermore, it must be critically noted that students with little professional experience and SLPs with many years of professional experience have very different knowledge and experiences of EBP. Therefore, it can be assumed that their understanding of EBP and its implementation in speech-language pathology and audiology practice are different. Nevertheless, the cross-case analysis identified typical interaction patterns and typical communicative actions that shape decision-making processes in video-based telepractice (Barthel et al., 2021a). In addition, the theoretical sampling in the selection of individual cases, the sequencing of the video recordings based on the research questions, and the coding process, among other things, provided the methodological and analytical potential to conceptually reconstruct the multifaceted subject area through the individual case analysis and the following cross-case analysis (Dietrich and Mey, 2018; Strübing, 2021).
The process model focuses on the social interactions between patient and SLP and their decisions in video-based telepractice. A limitation is that continuously or partially present relatives are not explicitly listed in the phases of the process model (Figure 4) and in the styles of interaction (Figure 3), and their role is not differentiated. Since relatives are an important resource in SLP, the involvement of relatives should be focused on in order to describe their role in decision-making processes in a more differentiated way, e.g., in all phases of therapy and depending on the age of the patients. Their interactions could be mapped in an extended model to concretize decisions related to how relatives are guided for “home practice” or how they are integrated into “perform target action.” This could reveal similar or different decision-making processes as well as styles of interaction of the SLPs.
In considering the process model, it is important to note that the patients, the SLPs, and the family members were using the video-based telepractice for at least six therapy sessions. It is reasonable to assume that during this time, interactions were implicitly and/or explicitly developed that influenced decision-making in video-based telepractice. How social practices of decision-making occur in other phases of the therapy process (e.g., clinical history, diagnosis, counseling, or final session), what patterns of decision-making occur in group therapy, and how little experience with social interactions in video-based telepractice affects decision-making are not answered by the study. Therefore, the process model can only map individual therapy in the treatment phase. In this video-based observational study with a cross-sectional design, it was not possible to reconstruct how nonverbal and verbal pragmatic communication factors (e.g., speech contribution, gestures) depend on the relationship between patients and SLPs, or on symptoms of the communication disorder, and in turn influence decision-making processes.
SLPs can design decision-making processes in participative interactions in video-based telepractice. For this reason, it would be possible that all participants can make shared, evidence-based decisions in the intervention process. In cross-sectional observational studies, decisions in different interaction styles are recognizably shaped by client perspectives and clinical expertise. As it was possible to offer video-based telepractice for the first time in Germany in spring 2020, the study served as a first survey. The results of the present study can be used as a starting point for further research projects on video-based telepractice in Germany. Further research is urgently needed to analyze the differentiation, e.g., between communication disorders, the age of the patients, the professional experience of the therapists, and their influence on the decision-making process in video-based telepractice. This should focus on a differentiated analysis of digital participation in speech and language pathology for people with communication disorders at different ages. On the one hand, the focus should be on the access to digital health care and the competence to use hardware and software, taking into account individual needs and living conditions. On the other hand, active involvement through a participative style of interaction is also important to enable patients to actively participate in the decision making process of digital care. This should also focus on the necessary social and digital skills of SLPs that are needed to ensure the digital participation of people with communication disorders in video-based telepractice in outpatient SLP services (Steiner, 2023). This refers both to the access and use of digital applications and to the participative style of social interactions in digital care.
The use of different qualitative and quantitative methods of data collection and analysis in different research designs can address the complexity of video-based in outpatient SLP service (e.g., heterogeneous patient populations, ICF orientation) and decision-making processes. This can be used to gain further essential insights into the conditions and patterns of interaction in evidence-based decision-making processes in video-based telepractice and also in SLP in general.
The implicit role of client perspectives, internal and external evidence and clinical expertise in interactive decision-making needs to be elicited from the perspectives of SLPs and patients and made explicit for use in treatment.
To concretize the sources of knowledge of SLPs, it would be relevant to know which sources of knowledge influence the interne evidence and clinical expertise. It would be interesting to determine whether and how, e.g., research findings, theory-based knowledge, or the expertise of colleagues are incorporated into clinical decision-making processes.
In future research it would be interesting to find out when decisions in the video-based therapy process are explained and justified, whether and how often they are explained repeatedly, and what this depends on for SLPs. It would also be interesting to know how aware SLPs are of decision-making processes in video-based telepractice and how they might make them explicit. Qualitative research approaches (e.g., stimulated recall interviews) could be used to make decision-making processes—especially cognitive ones—explicit and to reconstruct their relevance (Dempsey, 2010; Vall et al., 2018).
A decision-making process in which the patient ultimately made the decision about how to proceed with practicing was not analyzed in the video interaction analysis. It was not founded that SLPs were asking patients to make a choice between different practice options or intensities. It would be interesting to find out in which situations and for which content patients make the final decision and SLPs leave the final decision to the patients. It would also be interesting to find out what patients and families want to know from their perspective in order to make an informed decision. Qualitative research methods would be appropriate to explore the views, experiences, and wishes of patients and their families.
Additionally, as working conditions have a high impact on decision-making processes in in-person therapy (McCurtin and Clifford, 2015; Furlong et al., 2018; Selin et al., 2019), further research examining how working conditions influence decision-making processes in video-based telepractice are needed to uncover potential workloads that could reduce quality of care. The workplace-related advantages and disadvantages of video-based telepractice (Wittmar et al., 2023) should be compared with the working conditions of in-person therapy in order to decide when which form of care—in-person therapy, video-based synchronous and asynchronous telepractice, hybrid service (ASHA, 2020)—is necessary to improve the quality of care in outpatient SLP.
It would also be interesting to know when and how decisions are influenced when synchronous video and in-person therapies take place during the course of therapy. This could provide knowledge about the role of patients and the competencies of SLPs in order to shape the future of evidence-based and digital SLP in Germany.
The datasets presented in this article are not readily available because it is not possible to anonymize the recorded video-based teletherapies. Due to privacy and ethical concerns, the data cannot be made publicly available. Further inquiries can be directed to the corresponding author. Requests to access the datasets should be directed to MB, bWFyaWEuYmFydGhlbDJAaGF3ay5kZQ==.
MB, SW, BB, and JL contributed to conception and design of the study. MB wrote the first draft of the manuscript. MB and JL contributed to manuscript revision. All authors contributed to the article and approved the submitted version.
The Deutscher Bundesverband für Logopädie e.V. (dbl) (the official national professional association of logopedics in Germany) funded this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor PJ declared a shared committee with the author JL at the time of review.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ASHA (2004). Report of the Joint Coordinating Committee on Evidence-Based Practice. Available online at: https://www.asha.org/siteassets/uploadedfiles/jccebpreport04.pdf (accessed January 24, 2023).
ASHA (2020). Telepractice. Available online at: https://www.asha.org/practice-portal/professional-issues/telepractice/ (accessed November 14, 2020).
ASHA (2023). Evidence-Based Practice (EBP). Available online at: https://www.asha.org/research/ebp/ (accessed January 24, 2023).
Barthel, M., Schwinn, S., Borgetto, B., and Leinweber, J. (2021a). Digitalisierungschancen –Spurensuche nach Evidenz. Ergebnisse der Videointeraktionsanalyse aus dem Forschungsprojekt ViTaL. Forum Logopädie 35, 34–39. doi: 10.2443/skv-s-2021-53020210105
Barthel, M., Schwinn, S., Einfeldt, A., Borgetto, B., and Leinweber, J. (2021b). Digitalisierungschancen nutzen! Kernaussagen und Empfehlungen für die Nutzung von Videotherapie in der ambulanten logopädischen/sprachtherapeutischen Versorgung (Kurzfassung). Forum Logopädie 35, 49–50.
Bilda, K., Dörr, F., Urban, K., and Tschuschke, B. (2020). Digitale logopädische Therapie. Ergebnisse einer Befragung zum aktuellen Ist-Stand aus der Sicht von LogopädInnen. Logos 28, 176–183.
Breidenstein, G., Hirschauer, S., Kalthoff, H., and Nieswand, B. (2013). Ethnografie. Die Praxis der Feldforschung. Konstanz, München: UVK.
Cochrane (2011). Glossary. Available online at: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/SURE-Guides-v2.1/Collectedfiles/source/glossary.html (accessed September 21, 2023).
Coleman, J. J., Frymark, T., Franceschini, N. M., and Theodoros, D. G. (2015). Assessment and treatment of cognition and communication skills in adults with acquired brain injury via telepractice: a systematic review. Am. J. Speech-Lang. Pathol. 24, 2. doi: 10.1044/2015_AJSLP-14-0028
Creswell, J. W. (2007). Qualitative Inquiry and Research Design. Choosing Among Five Approaches. Los Angeles: SAGE.
Dempsey, N. P. (2010). Stimulated recall interviews in ethnography. Qual. Sociol 33, 3. doi: 10.1007/s11133-010-9157-x
Dietrich, M., and Mey, G. (2018). “Grounding Visuals. Annotationen zur Analyse audiovisueller Daten mit der Grounded-Theory-Methodologie,” in Handbuch. Qualitative Videoanalyse, eds. C. Moritz and M. Corsten (Wiesbaden: Springer), 135–152.
Dodd, B. (2007). Evidence-based practice and speech-language pathology: strengths, weaknesses, opportunities and threats. Folia Phoniatr Logop 59, 3. doi: 10.1159/000101770
Dollaghan, C. A. (2007). The Handbook for Evidence-Based Practice In Communication Disorders. Baltimore: Brookes.
Dresing, T., and Pehl, T. (2015). Praxisbuch Interview, Transkription and Analyse. Anleitungen und Regelsysteme für qualitativ Forschende. Marburg: audiotranskription.
Elwyn, G. (2020). Shared decision making: what is the work?. Patient Educ. Counsel. 104, 7. doi: 10.1016/j.pec.2020.11.032
Elwyn, G., Coulter, A., Laitner, S., Walker, E., Watson, P., and Thomson, R. (2010). Implementing shared decision making in the NHS. BMJ. 341, 971–973. doi: 10.1136/bmj.c5146
Elwyn, G., Frosch, D., Thomson, R., Joseph-Williams, N., Lloyd, A., Kinnersley, P., et al. (2012). Shared decision making: a model for clinical practice. J. Gen. Intern. Med. 27, 10. doi: 10.1007/s11606-012-2077-6
Fissel Brannick, S., Wolford, G. W., Wolford, L. L., Effron, K., and Buckler, J. (2022). What is clinical evidence in speech-language pathology? A scoping review. Am. J. Speech-Lang. Pathol. 31, 6. doi: 10.1044/2022_AJSLP-22-00203
Furlong, L., Serry, T., Erickson, S., and Morris, M. E. (2018). Processes and challenges in clinical decision-making for children with speech-sound disorders. Int. J. Lang. Commun. Dis. 53, 6. doi: 10.1111/1460-6984.12426
Gemeinsamer Bundesausschuss (2020). Einleitung des Beratungsverfahrens: Maßnahmen der Heilmitteltherapie als telemedizinische Leistung (Videotherapie). Available online at: https://www.g-ba.de/beschluesse/4521/ (accessed November 02, 2020).
Glaser, B. G., and Strauss, A. L. (1998). Grounded Theory. Strategien qualitativer Forschung. Bern: Hans Huber.
Greenwell, T., and Walsh, B. (2021). Evidence-based practice in speech-language pathology: where are we now? Am. J. Speech-Lang. Pathol. 30, 1. doi: 10.1044/2020_AJSLP-20-00194
Günther, T. (2013). Evidenz-basierte praxis oder praxis-basierte evidenz? Forum Logopädie 27, 26–27.
Higginbotham, J., and Satchidanand, A. (2019). From Triangle to Diamond: Recognizing and Using Data to Inform Our Evidence-Based Practice. Available online at: https://academy.pubs.asha.org/2019/04/from-triangle-to-diamond-recognizing-and-using-data-to-inform-our-evidence-based-practice/ (accessed January 24, 2023).
Knoblauch, H., and Schnettler, B. (2012). Videography: analysing video data as a ‘focused' ethnographic and hermeneutical exercise. Qual. Res. 12, 3. doi: 10.1177/1468794111436147
Knoblauch, H., and Vollmer, T. (2018). “Soziologische Videographie. Fokussierte Ethnographie und Sampling”, in Handbuch. Qualitative Videoanalyse, ed. C. Moritz and M. Corsten (Wiesbaden: Springer), 121–134. doi: 10.1007/978-3-658-15894-1_7
Lauer, N. (2020). Teletherapie – hat die Logopädie eine digitale Zukunft? Ergebnisse eines qualitativen Forschungsprojekts des Studiengangs Logopädie der OTH Regensburg. Forum Logopädie 34, 12-17.
McCurtin, A., and Clifford, A. M. (2015). What are the primary influences on treatment decisions? How does this reflect on evidence-based practice? Indications from the discipline of speech and language therapy. J. Evaluat. Clini. Pract. 21, 6. doi: 10.1111/jep.12385
McGill, M., Noureal, N., and Siegel, J. (2019). Telepractice treatment of stuttering: a systematic review. Telemed. J. e-Health 25, 5. doi: 10.1089/tmj.2017.0319
Merlino, S. (2021). Making sounds visible in speech-language therapy for aphasia. Social Interaction. Video-Based Stud. Human Soc. 4, 3. doi: 10.7146/si.v4i3.128151
Moritz, C. (2018). Well, it depends…“: Die mannigfaltigen Formen der Videoanalyse in der Qualitativen Sozialforschung. Eine Annäherung,” in Handbuch. Qualitative Videoanalyse, eds. C. Moritz and M. Corsten (Wiesbaden: Springer), 3–37.
Neely, L., Rispoli, M., Gerow, S., Hong, E. R., and Hagan-Burke, S. (2017). Fidelity outcomes for autism-focused interventionists coached via telepractice: a systematic literature review. J. Dev. Phys. Disabil. 29, 6. doi: 10.1007/s10882-017-9550-4
Neuhaus, S. (2022). Digitale Teilhabe – Begriffsklärung und Bedeutung für die Praxis der Logopädie mit dem Versuch einer Vision. Available online at: https://zenodo.org/record/6560260/files/BA_2022_003.pdf?download=1 (accessed November 01, 2023).
Overby, M. S., Caspari, S. S., and Schreiber, J. (2019). Volubility, consonant emergence, and syllabic structure in infants and toddlers later diagnosed with childhood apraxia of speech, speech sound disorder, and typical development: a retrospective video analysis. J. Speech Lang. Hear. Res. 62, 6. doi: 10.1044/2019_JSLHR-S-18-0046
Rangarathnam, B., Gilroy, H., and McCullough, G. H. (2015). Do patients treated for voice therapy with telepractice show similar changes in voice outcome measures as patients treated face to face? EBP Briefs 11, 1–6.
Selin, C. M., Rice, M. L., Girolamo, T., and Wang, C. J. (2019). Speech-language pathologists' clinical decision making for children with specific language impairment. Lang. Speech Hear. Serv. Schools 50, 2. doi: 10.1044/2018_LSHSS-18-0017
Stacey, D., Légar,é, F., Lewis, K., Barry, M. J., Bennett, C. L., Eden, K. B., et al. (2017). Decision aids for people facing health treatment or screening decisions (Review). Cochrane Database Syst. Rev. 4, CD001431. doi: 10.1002/14651858.CD001431.pub5
Steiner, J. (2023). Digitale Teilhabe als Auftrag in der Logopädie. Grundlegung, Begriffsklärungen und Befragung von Praktiker*innen. Forum Logopädie 37, 18–23.
Stokes, J. (2013). Video use in reflective practice: experience from educating speech and language therapists. J. Learn. Teach. 4, 7. doi: 10.21100/compass.v4i7.82
Strauss, A. L., and Corbin, J. (1996). Grounded Theory: Grundlagen Qualitativer Sozialforschung. Weinheim: Beltz.
Strübing, J. (2021). Grounded Theory. Zur sozialtheoretischen und epistemologischen Fundierung eines pragmatistischen Forschungsstils. Wiesbaden: Springer. doi: 10.1007/978-3-658-24425-5
Sutherland, R., Trembath, D., and Roberts, J. (2018). Telehealth and autism: a systematic search and review of the literature. Int. J. Speech-Lang. Pathol. 20, 3. doi: 10.1080/17549507.2018.1465123
Theodoros, D., Aldridge, D., Hill, A. J., and Russell, T. (2019). Technology-enabled management of communication and swallowing disorders in Parkinson‘s disease: a systematic scoping review. Int. J. Lang. Commun. Dis. 54, 2. doi: 10.1111/1460-6984.12400
Threats, T. T. (2008). Use of the ICF for guiding patient-reported outcome measures. Int. J. Speech-Lang. Pathol. 10:1–2. doi: 10.1080/14417040701768693
Threats, T. T. (2012). Use of the ICF for guiding patient-reported outcome measures. Perspect. Neurophysiol. Neurogenic Speech Lang. Disord. 22, 4. doi: 10.1044/nnsld22.4.128
Tuma, R. (2018). “Video-Interaktionsanalyse. Zur Feinauswertung von videographisch erhobenen Daten”, in Handbuch. Qualitative Videoanalyse, ed. C. Moritz and M. Corsten (Wiesbaden: Springer), 423–444. doi: 10.1007/978-3-658-15894-1_22
Tuma, R., Schnettler, B., and Knoblauch, H. (2013). Videographie – Einführung in die interpretative Videoanalyse sozialer Situationen. Wiesbaden: Springer.
Vall, B., Laitila, A., Borcsa, M., Kykyri, V.-L., Karvonen, A., Kaartinen, J., et al. (2018). Stimulated recall interviews: How can the research interview contribute to new therapeutic practices? Revista Argentina de Clinica Psicologica 27, 2.
Wales, D., Skinner, L., and Hayman, M. (2017). The efficacy of telehealth-delivered speech and language intervention for primary school-age children: a systematic review. Int. J. Telerehabilitat. 9, 1. doi: 10.5195/ijt.2017.6219
Watson, L. R., Crais, E. R., Baranek, G. T., Dykstra, J. R., and Wilson, K. P. (2013). Communicative gesture use in infants with and without autism: a retrospective home video study. Am. J. Speech-Lang. Pathol. 22, 1. doi: 10.1044/1058-0360(2012/11-0145)
Weidner, K., and Lowman, J. (2020). Telepractice for adult speech-language pathology services: a systematic review. Persp. ASHA Special Int. Groups 5, 1. doi: 10.1044/2019_PERSP-19-00146
Westby, C., Burda, A., and Mehta, Z. (2003). Asking the right questions in the right ways: strategies for ethnographic interviewing. ASHA Leader 8, 8. doi: 10.1044/leader.FTR3.08082003.4
Wittmar, S., Barthel, M., Leinweber, J., and Borgetto, B. (2023). Outpatient speech and language therapy via videoconferencing in Germany during the COVID-19 pandemic: experiences of therapists. Int. J. Health Prof. 10, 1. doi: 10.2478/ijhp-2023-0001
World Health Organization (WHO) (2021). Evidence, Policy, Impact. WHO Guide for Evidence-Informed Decision-Making. Available online at: https://apps.who.int/iris/rest/bitstreams/1405176/retrieve (accessed January 30, 2023).
World Health Organization (WHO) (2013). How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF). Exposure Draft for comment. Geneva: WHO
Keywords: video-based telepractice, decision-making, evidence-based, speech-language pathology, digital participation, qualitative research, video interaction analysis
Citation: Barthel M, Wittmar S, Borgetto B and Leinweber J (2023) Evidence-based decision-making in speech-language pathology via video-based telepractice—A qualitative video interaction analysis. Front. Commun. 8:1176473. doi: 10.3389/fcomm.2023.1176473
Received: 28 February 2023; Accepted: 30 November 2023;
Published: 15 December 2023.
Edited by:
Petra Jaecks, Bielefeld University, GermanyReviewed by:
Elena Theodorou, Cyprus University of Technology, CyprusCopyright © 2023 Barthel, Wittmar, Borgetto and Leinweber. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maria Barthel, bWFyaWEuYmFydGhlbDJAaGF3ay5kZQ==
†ORCID: Maria Barthel orcid.org/0000-0002-3682-6555
Silke Wittmar orcid.org/0000-0003-0886-6872
Bernhard Borgetto orcid.org/0000-0001-7465-3061
Juliane Leinweber orcid.org/0000-0002-5655-7882
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.