- 1Department of Public Relations and Advertising, Ric Edelman College of Communication and Creative Arts, Rowan University, Glassboro, NJ, United States
- 2Department of Mathematics, Saint Joseph's University, Philadelphia, PA, United States
Introduction: This study explores associations among adult vaccination, ethnicity, gender, and socioeconomic variables such as educational attainment and income, as well as neighborhood factors.
Methods: A telephone quota sample of New Jersey adults (N = 1,984) was used to text associations among proposed predictors of vaccination behaviors.
Results: Our multivariate logistic regression analyses found that certain races/ethnicity, respondents' household income, and perceived safety of one's community were the strongest predictors of COVID-19 vaccination. The odds of COVID-19 vaccination were 52% lower for Black/African American respondents compared to white/Caucasian respondents (p = 0.001) and 44% lower for Hispanic/Latino respondents compared to white/Caucasian respondents (p = 0.001).
Discussion: The results add new insights to public health communication research and suggest careful interventions across racial groups, considering existing racial disparities in vaccination.
Introduction
The COVID-19 pandemic (hereafter “pandemic”) has become a global health disaster. During the pandemic, reducing and preventing the spread of coronavirus disease 2019 (COVID-19) is a main priority for government officials and individuals. Thus, COVID-19 vaccines have become more critical to effectively control the virus together and possibly bring an end to the pandemic (Wakefield and Khauser, 2021).
Yet, vaccination rates in the United States and around the world are still much lower than what is planned and needed (Zampetakis and Melas, 2021). As of 22 October 2021, 189.9 persons (57% of the total population) are fully vaccinated to prevent COVID-19 in the US (CDC, 2021). There is also a delay in the acceptance to get the vaccine around the world due to availability (Freeman et al., 2022). Understanding individual and social determinants of COVID-19 vaccination is critical to population health as vaccination that is apparent in a particular community could be influenced by both individual, socioeconomic status and unique society and neighborhood conditions (Burdette et al., 2014; Alberts et al., 2017; Thompson et al., 2019). Thus, it comes as no surprise that understanding what socio-demographic and community factors significantly influence adults' COVID-19 vaccination is crucial to health and medical professionals and policymakers.
Research that measures vaccine hesitancy tends to adopt the WHO Vaccine Hesitancy Determinants Matrix (MacDonald, 2015; Willis et al., 2021) or intent to receive vaccines (Cohen and Legg, 2014; Budhwani and De, 2016; Cho et al., 2020; Zampetakis and Melas, 2021). Certainly, there is a need to recognize and utilize actual vaccine inoculation rates in a sample that might better inform socioeconomic factor-related health disparities. Therefore, the objectives of the present study are to determine the association of neighborhood factors with actual vaccination by (1) controlling for individual-level demographics and household income; and (2) testing whether the association of neighborhood factors with vaccination was modified by individual demographic factors.
To encapsulate, this study explores how neighborhood factors (i.e., a neighborhood and built environment factor, perceived safety of a township he or she lives in, a healthcare access factor, and proximity to hospitals) as well as critical socio-demographic variables (ethnicity, gender, educational attainment, and income) impact on adults' vaccination during the global pandemic. To address the proposed hypotheses and research questions, we conducted a telephone quota survey with adults in New Jersey (N = 1,984). Our multivariate logistic regression analyses will offer meaningful and generalizable implications to public health communication research and interventions to the population, as effective promotion of health behaviors (e.g., vaccination) are of utmost importance during the pandemic.
Literature review
COVID-19 pandemic and determinants of vaccination
National polls conducted before vaccine distribution began suggested that many people were hesitant to receive COVID-19 vaccination (Nguyen et al., 2021). According to a report from the CDC, younger adults, women, non-Hispanic Black adults, adults living in nonmetropolitan areas, and adults with less education and income, and without health insurance continue to be less likely to receive COVID-19 vaccination, despite overall increased intent to receive the vaccine from 39.4 to 49.1% among adults and across all priority groups (Nguyen et al., 2021).
Prior studies in vaccination behaviors research argue that there are two main factors that might determine or influence vaccine hesitancy: individual psychological influences such as one's beliefs, perceived risk of a new vaccine and worry about a vaccine itself, and contextual and socio-demographic factors such as gender, ethnicity, and other socioeconomic statuses (Alabdulla et al., 2021). For instance, a survey of 1,205 Arkansas adults explored whether and how both individual psychological factors (i.e., COVID-19 health literacy, fear of COVID-19 infection, general trust in vaccines) and group/socio-demographic factors would affect COVID-19 vaccine hesitancy (Willis et al., 2021). In short, the prevalence of COVID-19 vaccine hesitancy was highest among Black/African Americans compared to white respondents; some college/technical degree holders compared to respondents with a 4-year degree; respondents with lower household income (<$25K); and those who reported low trust in vaccines in general (Willis et al., 2021). Freeman et al. (2022) also confirm the two important factors that lead to a willingness to receive a COVID-19 vaccine. That is, not only individual psychological factors such as conspiracy beliefs, negative views of doctors, and positive healthcare experience were related to vaccination but also vaccine hesitancy meaningfully associated with socio-demographic factors, such as younger age, female gender, lower income, and ethnicity (Freeman et al., 2022).
In order to ensure high and equitable vaccination coverage among all populations around the world, it is important to understand the aforementioned determining socioeconomic/socio-demographic factors and other contextual factors that lead to vaccine hesitancy or actual vaccination behavior. The following section, thus, will review the aforementioned critical factors in more detail.
Racial- and gender disparities in COVID-19 vaccination
Noteworthy, race/ethnicity is considered a meaningful group factor that influences vaccination likelihood and behaviors, as one study argues being African American/Black or Latino/Hispanic had a greater chance of having limited health resources (Stormacq et al., 2019). Many studies showed empirical evidence of ethnic differences and their behavioral diversities in getting vaccinated against flu influenza (Cohen and Legg, 2014; Budhwani and De, 2016) and/or HPV (Cohen and Legg, 2014; Cho et al., 2020). This stream of research, however, comes to somewhat contradictory findings in terms of which ethnic group would show health disparities in vaccination behaviors. For example, one study showed that “Asian Indians” had higher proportions of college graduation rates (i.e., higher socioeconomic status) than other ethnic groups; and they were more likely to receive the influenza vaccine than white Americans (Budhwani and De, 2016). One thing to note, health insurance status would diminish the effects of race and ethnicity on vaccine uptake rates (Budhwani and De, 2016). On the other hand, a large-scale survey done by the National College Health Assessment (N = 67,762) differently demonstrated that “non-Hispanic whites” had a higher percentage of getting the HPV vaccine over other racial races and ethnicities (e.g., Black/non-Hispanic, Hispanic/Latino, Asian/Pacific Islander, and American Indian/Alaskan Native/Native Hawaiian; Cohen and Legg, 2014). Cohen and Legg (2014) argued that “Black, Hispanic” and “Asian” college women aged 18–26 years, as a minority group, were less likely to receive the HPV vaccine when compared to white women, which is consistent with some previous studies (Stormacq et al., 2019) but not with Budhwani and De (2016). Another study confirms racial and ethnic differences in getting a vaccination for HPV (i.e., the human papillomavirus), but shows that “Hispanic” women were more likely to be vaccinated than non-Hispanic white women, and a total of minority students who were less likely to be vaccinated than white Hispanic women (Cho et al., 2020).
Gender
Noteworthy, female gender and ethnic minority status were associated with more vaccine hesitancy (Fisher et al., 2020; Lazarus et al., 2020; Taylor et al., 2020; Freeman et al., 2022). One study found that women are more skeptical of COVID-19 vaccinations, while they are an important demographic group influencing vaccine opinions as they have more influence over vaccination decisions for children (Alabdulla et al., 2021). Furthermore, there is a strong correlation between the country of origin, socioeconomic status, age, gender, and familial background and the likelihood to be vaccine-hesitant: higher vaccine hesitancy was associated with female gender, being a native, and being over 65 years of age (Alabdulla et al., 2021).
Ethnicity
African Americans and Latinos were less likely to be vaccinated than white American as the survey shows (Chen et al., 2007). Specifically, Latinos cited access and cost barriers as the main reason they were not vaccinated, while African Americans were most likely to be distrustful of the medical system or negative vaccine effects (Chen et al., 2007). Several studies also bolster racial diversities in receiving the COVID-19 vaccines, and conclude, female gender, certain ethnic groups such as non-Hispanic Black/African Americans or Hispanic, and adults with less education and income were less likely to receive the vaccines (Nguyen et al., 2021; Willis et al., 2021; Freeman et al., 2022). Considering the aforementioned arguments, the following hypothesis testing the COVID-19 vaccination by gender and race/ethnicity is proposed:
Hypothesis 1. COVID-19 vaccination will be significantly associated with one's (a) gender and (b) race/ethnicity.
Education and income as meaningful socioeconomic factors about vaccination
Many studies raise concerns about the socioeconomic differences in COVID-19 vaccine hesitancy, leading to widening existing health disparities in COVID-19-related infections (Willis et al., 2021). Socioeconomic disparities, traditionally measured through levels of education, income, and/or occupation, are considered the most fundamental causes of health disparities (Adler and Newman, 2002). Socioeconomic status (SES) indicators are regarded to determine poor health outcomes such as poor environmental conditions, poor living or working conditions, and low health literacy (Evans and Kantrowitz, 2002). In addition, an integrative literature review of 16 scholarly articles about health disparities concluded that the main socioeconomic factors that seem to influence health disparities are educational attainment, income, and race/ethnicity (Stormacq et al., 2019). Indeed, household income proved to be a high influence on whether someone was vaccinated for flu vaccines or not (Chen et al., 2007).
Educational level is one of the most frequently cited variables of health disparities in previous research (Stormacq et al., 2019). A study of 2,668 adults supports that SES are determinants of health disparities: lower educational attainment and certain ethnicity (Blacks and Hispanics) are associated with poor preventive health behaviors (e.g., lower influenza vaccination rates, mammography, or dental care services) and poorer self-rated health status (Bennett et al., 2009). From a systematic review of existing peer-reviewed literature (N = 42), Lucyk et al. (2019) also confirm that higher levels of SES resulted in higher levels of influenza vaccination. Specifically, 18 prior studies used two variables to measure SES, using either a combination of education and income (n = 12), education and poverty (n = 3), education and employment (n = 2), or income and poverty (n = 1), indicating income and education are two determining factors that possibly affect the COVID-19 vaccination. Concerning the review of literature, the second hypothesis is submitted as follows:
Hypothesis 2. COVID-19 vaccination will be significantly associated with one's socioeconomic status such as (a) educational attainment or (b) income.
The impact of neighborhood factors on vaccination
Often in public health research, more attention has been paid to individual-level factors to health behavior change (e.g., vaccination), which does ignore the social- and community-level factors that impact health behavior. Examining societal factors is important because research has indicated that the quality of community environments, including facilities and amenities, may hamper or enhance residents' health behavior change (Thompson et al., 2019).
The US Department of Health Human Services (2014) identified a framework entitled, Social Determinants of Health (SDOH), of which societal-level conditions may indirectly influence health behaviors. Social determinants of health can be divided into five categories, all of which affect the health of individuals: education, economic stability, social and community context, neighborhood and built environment, and health and healthcare. The five elements of SDOH have often been included in vaccination studies as part of demographic information or along with other individual determinants of health behaviors (Burdette et al., 2014; Alberts et al., 2017; Thompson et al., 2019). For instance, a recent survey with young adults (i.e., those aged 18–26; n = 3,593) showed that SDOH variables were significantly associated with HPV vaccination (Thompson et al., 2019).
The COVID-19 pandemic has been especially difficult for those who live in vulnerable communities without protective equipment and pandemic resources. As one study argues, there are communities that are much more vulnerable to the spread of COVID-19 and experience more fatal effects from contracting the virus than others (Arcadepani et al., 2021). A study of Brazil's “Cracolândia,” having approximately 500 residents and 2000 regular visitors buying, selling, and using drugs, confirms the possible impact of community conditions on vaccine acceptance, and argues that such neighborhood factors are critical to controlling the pandemic and reducing community spread (Arcadepani et al., 2021).
Given that the first two categories of SDOH (i.e., education and economic stability) are well addressed or overlapped by our aforementioned socioeconomic factors, this study adopts the following two community factors that may better explain vaccine disparities in populations at risk: neighborhood and built environment, and health and healthcare. Specifically, literature in SDOH operationalized neighborhood and built environment include items that measure perceived crime and violence in the neighborhood (e.g., people in the neighborhood can be trusted), while health and healthcare focus more on one's access to healthcare and/or primary care physicians (The US Department of Health Human Services, 2014; Thompson et al., 2019).
Given that studies have rarely used the two social and neighborhood factors as a basis for examining potential associations with vaccination (Burdette et al., 2014), the current study seeks to examine relationships between neighborhood environmental factors and adults' vaccination:
Hypothesis 3. COVID-19 vaccine behavior will be significantly associated with neighborhood factors such as (a) the perceived safety of a township and (b) proximity to hospitals.
Research question 1. What is the relative importance of gender, ethnicity, income, education, and neighborhood factors in predicting adults' vaccination?
Methods
The current study used quota sampling with a telephone survey (50% land and 50% cell phone that applied both random digits dialing and list-only methods in the state of New Jersey). This location is a proper example to demonstrate the aforementioned hypotheses due to a huge disparity between cities and townships and its group-to-group comparison being significantly meaningful. A survey company was hired to recruit a population-representative sample. The average length of the telephone survey was 23 min and the response rate was 4.7%. Out of 42,045 calls made, 1,984 individuals have agreed to participate in our survey.
Measures
Vaccination is measured by an item that asks whether he or she did get a vaccine (e.g., for the coronavirus): yes/no (Cohen and Legg, 2014). Income, or total earnings last year, was based on a person's estimate of their earnings for the last year (Lucyk et al., 2019; Willis et al., 2021). Education: Participants reported their highest level of education at the time of the survey. This was operationalized as no school completed, less than a high school degree, high school graduate or GED, some college or college degree, Master's degree, or Doctoral degree (Budhwani and De, 2016; Friis et al., 2016). For health and healthcare access, participants reported their proximity to primary physicians or hospitals; and their perceived safety of the township they live in, as identified as a neighborhood factor from previous studies (The US Department of Health Human Services, 2014; Thompson et al., 2019).
Results
To test the proposed hypotheses, we used multiple logistic regression to predict adults' COVID-19 vaccination and tested hypothesized associations using the R program version 4.4.1, and the R package glm was used to deal with the data. The logistic regression model is suitable if a dependent variable consists of binary outcomes such as success/failure, win/lose, yes/no, or infected/not infected. Logistic regression does not require key assumptions required in linear models such as linearity, normality, and homoscedasticity, but the dependent variable must be a binary variable and observations must be independent of each other.
Multiple logistic regression models
We consider a logistic regression for vaccination which is a binary outcome (0 = no vaccination or 1 = at least one vaccination) with six independent variables: gender, ethnicity, education, income, perceived safety of a township, and distance to hospitals. Gender, ethnicity, and education are categorical variables, but income, perceived safety of a township, and distance to hospitals are continuous variables. The logistic regression model is as follows:
Where,
• Y: Vaccination status: 1 for vaccinated and 0 for not vaccinated;
• p = Pr(Y = 1);
• X1: Gender (two levels);
• X2: Ethnicity (five levels);
• X3: Education (seven levels);
• X4 : Income;
• X5 : Perceived safety of a township;
• X6: Distance to hospitals.
In testing Hypotheses 1–3, multilevel logistic regression models using the above formula were conducted. The distributions of gender, race, income, and perceived safety of 1,984 individuals in the population representative sample with coefficients are shown in Table 1. As the results of logistic regression models were identified as odds ratios and their confidence intervals, the parameter estimates and p-values are also listed.
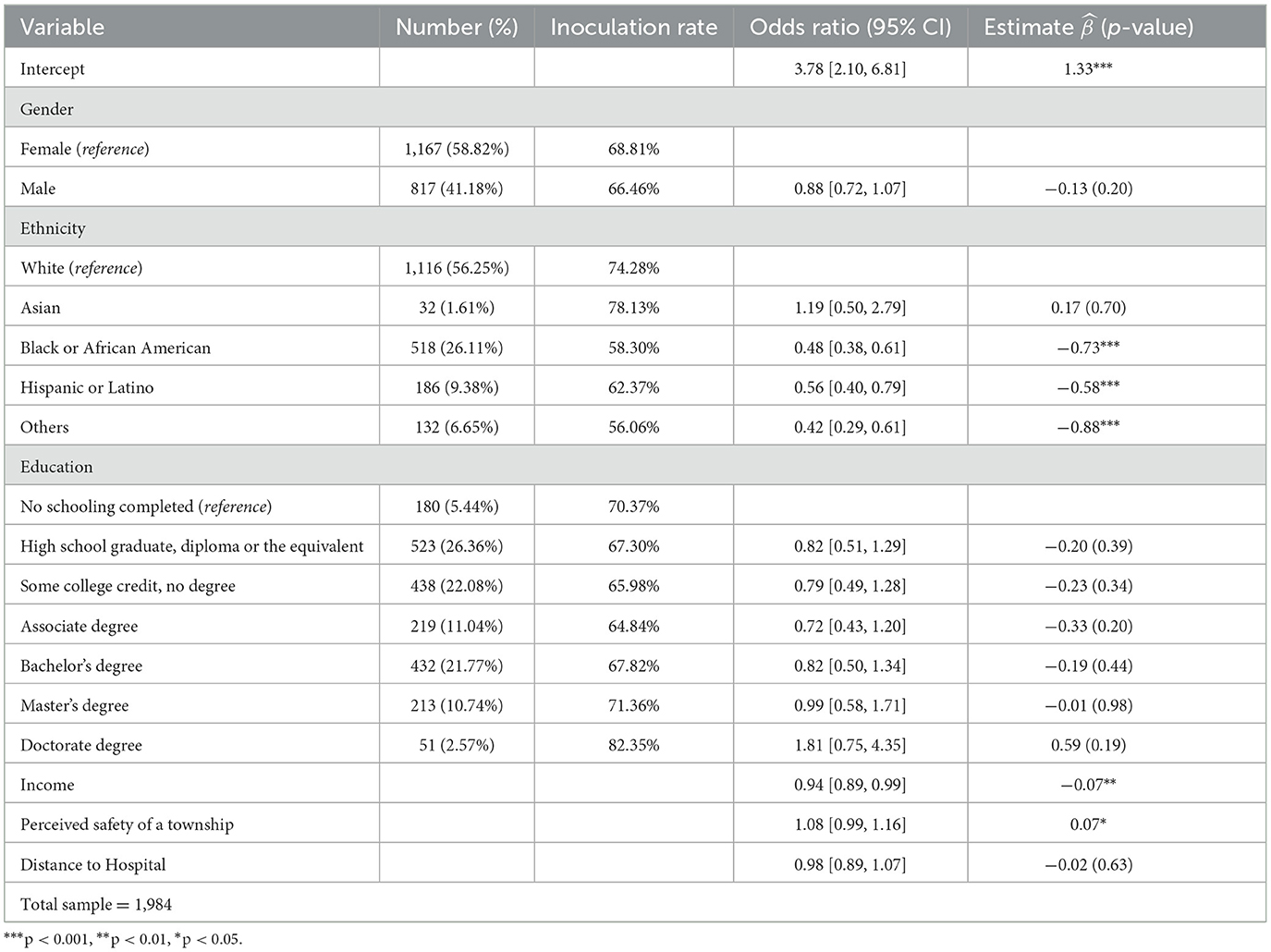
Table 1. The demographic distribution and odds ratios of the vaccine inoculation rate for all variables.
For Hypothesis 1, the results show a significant association between ethnicity and vaccination, partially supporting H1. Specifically, the odds of vaccination in the Black/African American group decreased by 52% ( = 0.48) assuming that the other variables remain fixed while the white group is a reference. The odds of vaccination in Hispanic or Latino groups and the other groups also decreased by 44 and 58%, respectively, compared to the white group. The odds of vaccination in the Asian group increased by 19% compared to the white group, but the difference is not statistically significant. Gender was not a significant indicator in this analysis, rejecting H1b (p = 0.20).
For Hypothesis 2, the results from logistic regression show that increasing income by 1 unit results in a 6% decrease in the odds of vaccination (p = 0.02), again partially supporting H2 in the opposite direction. Education status was not a significant factor for all groups (Highschool diploma, p = 0.39; Associate degree, p = 0.20; bachelor's degree, p = 0.44; Master's degree, p = 0.98; Doctorate degree, p = 0.19).
For Hypothesis 3, there is a significant and positive relationship between perceived safety and vaccination. For instance, increasing the perceived safety of a township by 1 unit results in an 8% increase in the odds of vaccination, supporting H3a. Proximity to the hospital was not a significant factor in predicting vaccination (p = 0.63).
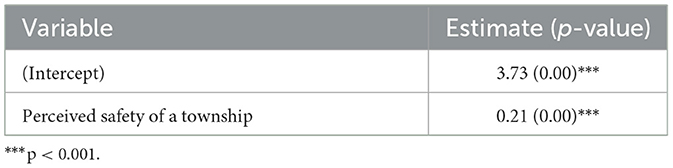
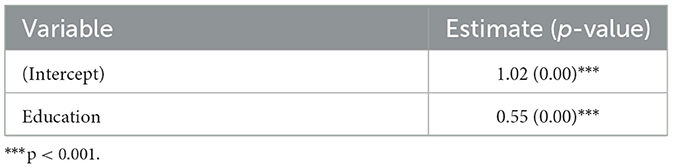
Simple linear regression models
We also consider two simple linear models. In the first simple linear model, we examined the impact of the perceived safety of a township on education. Table 2 shows that a positive linear relationship between the perceived safety of a township and education is strongly significant. The second linear model was used to find out a linear relationship between income and education, and Table 3 indicates that a positive linear relationship exists and it is strongly significant.
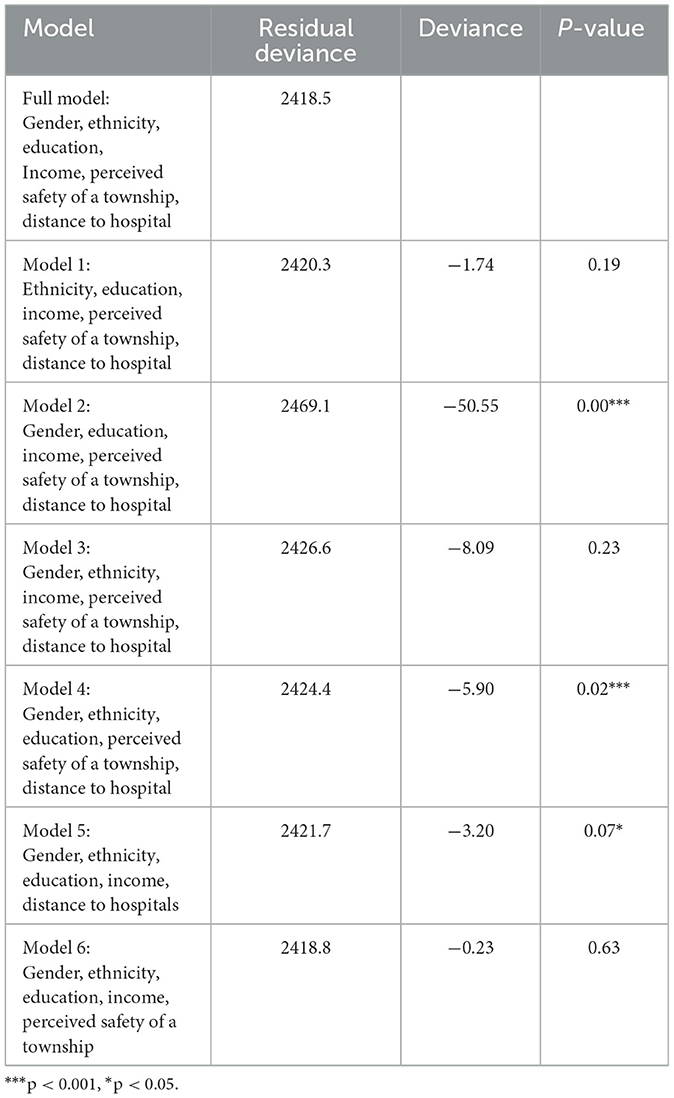
To test our first research question, we measure deviances between candidate models (i.e., each model eliminates one variable from the full model) and a perfect model of all six variables (saturated model). The deviance is always nonnegative, and this becomes zero only if the fit of the model is perfect. Theoretically, deviance is defined as the difference in the log-likelihoods between a fitted model and a perfect model. Table 4 shows that ethnicity and income are statistically significant at a 0.05 level of significance. The perceived safety of a township is significant at a 0.1 level of significance. Model 2 shows the largest difference in deviance from the full model. It tells us that adding race/ethnicity to the model substantially improves our model accuracy given the other variables are already included in Model 2 (p < 0.001). This analysis also shows that adding respondents' income (see Model 4) and perceived safety of a township (see Model 5) also significantly improve the model accuracy. In short, deviance tests compare our full model of six determinants (i.e., gender, ethnicity, education, income, perceived safety of a township, distance to hospitals) of adults' vaccination to all other possible six models, and conclude that ethnicity is the strongest predictor of respondents' vaccine inoculation rate, followed by income and perceived safety of a town.
Discussion
This study explored associations among vaccination, socioeconomic variables such as race/ethnicity, gender, educational attainment, and income, as well as neighborhood factors (perceived safety of one's community/township and health care access factor) that are widely cited as critical factors of health disparities, in a sample of New Jersey adults surveyed via telephone.
Multiple logistic regression analysis showed that vaccination differed significantly across race/ethnicity, individual income, and perceived safety of one's township. This analysis was applied as the current study has the potential to control for cross-level confounding of an association of a contextual exposure (e.g., neighborhood factors) with an individual-level outcome (e.g., vaccination) that may occur due to omission of individual-level covariates (e.g., individual income) that are also correlated with the contextual exposure (Diez-Roux, 1998). In this regard, we aim to explain the significance of individual factors first, followed by neighborhood factors.
The results showed respondents who were Black/African American or Hispanic/Latino, and those with lower income had a prevalence of vaccination than those who were white or one in higher income brackets. These findings are consistent with prior literature (Stormacq et al., 2019; CDC, 2021; Willis et al., 2021; Freeman et al., 2022), but build new insight, as this study has a large and diverse sample from a state and adds the societal and community factors of consideration (i.e., proximity to hospitals and perceived safety of a township). But we could not find any gender differences in getting vaccinated for the coronavirus, which is consistent with a previous study (Stormacq et al., 2019). This finding is of great concern because Black/African Americans bear a greater burden of COVID-19 hospitalizations and deaths, according to Fisher et al. (2020). African American/Black and Latino/Hispanic have a greater chance of having limited health resources (Stormacq et al., 2019), which in turn, can perpetuate long-term racial health disparities.
In addition, income was significantly associated with whether someone was vaccinated for COVID-19 vaccines or not, which is partially consistent with prior studies (Chen et al., 2007; Jeudin et al., 2014). Although our data supported household income as being a high influence on vaccinations, low-income adults were more likely to get vaccinated than those with high incomes.
Surprisingly, different studies testing an association between vaccination and income have yielded contradictory results. While Freeman et al. (2022) argued that those with less income were less likely to receive the vaccines, one study reviewed relevant literature and concluded that low-income adolescents are equally or more likely to start the HPV vaccination series than those who have a higher income (Jeudin et al., 2014). Concerning the mixed findings, our sample was drawn from the state of New Jersey which is considered a Democratic stronghold with a more liberal population and culture (World Population Review, 2021), as well as the state showing its vaccination rate is among the highest in the country (Laughlin and Goodin-Smith, 2021). Kreps et al. (2020) argued that political partisanship strongly impacted COVID-19 vaccination, and Democratic political partisans would be more likely to receive vaccination than those who are Republicans or independents. Thus, we suggest scholars to further examine a state or town's political identity that could explain the strong relationship between those with low income and their greater vaccine inoculation rate.
Noteworthy, we found that individual assessment of one's community environments and perceived safety was another significant determinant of COVID-19 vaccination. The more he or she perceived his or her township as safe, the more the odds one received a COVID-19 vaccination. More importantly, our sub-analysis showed a significant linear relationship between respondents' educational attainment and perceived safety of community environments (p = 0.00). See more details in Table 2. That is, those who assessed their community as safer are with more advanced education/degrees, possibly leading to an explanation of more prevalence of COVID-19 vaccination among them. In other words, those who have college degrees or higher in our sample are known to be associated with greater health literacy (Stormacq et al., 2019), along with their positive perceptions of community environments, which might explain the greater COVID-19 vaccination rate. Future research, therefore, is needed to further understand which factors are associated with positive perceptions of neighborhood and built environments, leading to COVID-19 vaccination.
Taken together, socio-demographic and neighborhood differences in adults' COVID-19 vaccination raise concerns about the potential of vaccine implementation to widen existing health disparities in a pandemic such as COVID-19. Specifically, racial differences, income, and perceived safety of one's township as the most critical determinants of COVID-19 vaccination call for comprehensive public health policies and campaigns for those facing community health disparities, particularly among African Americans and Hispanics or Latinos.
There are many implications for future research and points to improve the COVID-19 vaccination rates for certain communities and ethnic groups. For a possible explanation of racial disparities in vaccination, vaccine hesitancy is positively associated with less fear of infection by COVID-19, while African Americans reported the highest fearing infection to a great extent across all racial/ethnic groups (Willis et al., 2021). In addition, barriers to COVID-19 vaccination include healthcare access and cost for Hispanics/Latinos, distrust of the medical system, or negative views on vaccine effects for Black/African Americans (Chen et al., 2007). Therefore, further investigation is needed to determine ways in which fear or other psychological factors may or may not explain different vaccine inoculation rates across racial groups. Public health research should also identify and elaborate more on neighborhood/community-level barriers to vaccination.
As income and perceived safety of a town are strong determinants of vaccination in our study, COVID-19 vaccination for African Americans or Latinos is to be explained by not only the aforementioned community factors but also other individual psychological determinants. For example, certain gender (female) and race/ethnicity (white) and higher levels of education are significantly associated with better health information recall and a higher level of health literacy, leading to vaccination behaviors (Ayotte et al., 2009). As such, we suggest studying the interplay between race/ethnicity, socioeconomic status (i.e., education or income from the current study), health literacy or health information seeking, and other neighborhood determinants to understand adults' vaccination in a more holistic approach. Governmental agencies should use this data to create a plan that specifically targets the concerns of each group in communities in promoting vaccination.
Limitations and future research
The sample was slightly skewed to women (59%) and college-educated respondents (70%), and the study recruited respondents via telephone who are known to be more exposed and often contacted for research purposes. The high number of respondents having college degrees or at least college credits limits the generalizability of these results to a population. Finally, our measure of the neighborhood factor is limited to the respondents' self-report of how much they perceive their community as safe, and we do not know if that assessment is valid in other contexts. Future researchers might want to adopt more in-depth, yet comprehensive measurements of other Social Determinants of Health (SDOH) variables (The US Department of Health Human Services, 2014; Thompson et al., 2019) to explore a full picture of societal influences on adults' vaccination. Such limitations are offset to some extent by our large and diverse telephone quota sample, which closely mirrored the ethnic composition in the US.
Conclusion
We hope our findings help develop an equitable vaccine distribution plan, as well as public health campaigns that pursue racial/ethnic equality. Whether vaccination will be positively or negatively influenced would depend on how strongly neighborhood factors are associated with individual momentums. While we could not assess the extent of individual and personal motivation toward this health behavior, the current line of study should be extended as more people are exposed to vaccination intervention. In doing so, we are careful to suggest that vaccine advocacy in public policy should accompany a complex, multifaceted perspective that considers subgroup diversities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, upon request.
Ethics statement
The studies involving human participants were reviewed and approved by the IRB Rowan University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adler, N. E., and Newman, K. (2002). Socioeconomic disparities in health: pathways and policies. Health Affairs 21, 60–76. doi: 10.1377/hlthaff.21.2.60
Alabdulla, M., Reagu, S. M., Al-Khal, A., Elzain, M., and Jones, R. M. (2021). COVID-19 vaccine hesitancy and attitudes in Qatar: a national cross-sectional survey of a migrant-majority population. Influenza Resp. Viruses 15, 361–370. doi: 10.1111/irv.12847
Alberts, C. J., van der Loeff, M. F., Hazeveld, Y., Melker, T. G., van der Wal, H. E., Nielen, M. F., et al. (2017). A longitudinal study on determinants of HPV vaccination uptake in parents/guardians from different ethnic backgrounds in Amsterdam, the Netherlands. BMC Public Health 17, 220. doi: 10.1186/s12889-017-4091-4
Arcadepani, F. B., Macedo, D., Tardelli, M. A. C. F., Martins, V. S. S. S., and Fidalgo, T. M. (2021). COVID-19 vaccination among socially vulnerable people who use drugs. Addiction 116, 2590–2591. doi: 10.1111/add.15500
Ayotte, B. J., Allaire, J. C., and Bosworth, H. (2009). The associations of patient demographic characteristics and health information recall: the mediating role of health literacy. Aging Neuropsychol. Cognit. 16, 419–432. doi: 10.1080/13825580902741336
Bennett, I. M., Chen, J., Soroui, J. S., and White, S. (2009). The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Annal. Family Med. 7, 204–211. doi: 10.1370/afm.940
Budhwani, H., and De, P. (2016). Disparities in influenza vaccination across the United States: variability by minority group, asian sub-populations, socio-economic status, and health insurance coverage. Public Health 138, 146–153. doi: 10.1016/j.puhe.2016.04.003
Burdette, A. M., Gordon-Jokinen, H., and Hill, T. D. (2014). (2014). Social determinants of HPV vaccination delay rationales: evidence from the 2011 national immunization survey-teen. Prev. Med. Rep. 1, 21–26. doi: 10.1016/j.pmedr.2014.09.003
CDC (2021). COVID data tracker: COVID-19 vaccinations in the United States. Atlanta, GA: US Department of Health and Human Services. Available online at: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total (accessed October 22, 2021).
Chen, J. Y., Fox, S. A., Cantrell, C. H., Stockdale, S. E., and Kagawa-Singer, M. (2007). Health disparities and prevention: racial/ethnic barriers to flu vaccinations. J. Commun. Health 32, 5–20. doi: 10.1007/s10900-006-9031-7
Cho, D., Ramondetta, L., Garcini, L., and Lu, Q. (2020). HPVs Vaccination among racial/ethnic minority college students: current status and future direction. J. Nat. Med. Assoc. 112, 639–649. doi: 10.1016/j.jnma.2020.06.005
Cohen, T. F., and Legg, J. (2014). Factors associated with HPV vaccine use among hispanic college students. J. Allied Health. 43, 241–246.
Diez-Roux, A. (1998). Bringing context back into epidemiology: variables and fallacies in multilevel analysis. Am. J. Publ. Health, 88, 216–22. doi: 10.2105/AJPH.88.2.216
Evans, G. W., and Kantrowitz, E. (2002). Socioeconomic status and health: the potential role of environmental risk exposure. Ann. Rev. Pub. Health 23, 303–331. doi: 10.1146/annurev.publhealth.23.112001.112349
Fisher, K. A., Bloomstone, S. J., Walder, J., Crawford, S., Fouayzi, H., Mazor, K. M., et al. (2020). Attitudes toward a potential SARS-CoV-2 vaccine : a survey of U.S. adults. Annal. Int. Med. 173, 964–973. doi: 10.7326/M20-3569
Freeman, D., Loe, B. S., Chadwick, A., Vaccari, C., Waite, F., Rosebrock, L., et al. (2022). COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol. Med. 52, 3127–3141. doi: 10.1017./S0033291720005188
Friis, K., Lasgaard, M., Rowlands, G., Osborne, R. H., and Maindal, H. T. (2016). Health literacy mediates the relationship between educational attainment and health behavior: a Danish population-based study. J. Health Commun. 21, 54–60. doi: 10.1080/10810730.2016.1201175
Jeudin, P., Liveright, E., Del Carmen, M. G., and Perkins, R. B. (2014). Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clin. Ther. 36, 24–37. doi: 10.1016/j.clinthera.2013.11.001
Kreps, S., Prasad, S., Brownstein, J. S., Hswen, Y., Garibaldi, B. T., Zhang, B., et al. (2020). Factors associated with US adults' likelihood of accepting COVID-19 vaccination. JAMA Network Open 3, e2025594–e2025594. doi: 10.1001/jamanetworkopen.2020.25594
Laughlin, J., and Goodin-Smith, O. (2021). For many, life edges closer to normal: Vaccination rates are fueling falling COVID-19 case counts, officials say. Philadelphia Daily News, May 22, 2021.
Lazarus, J. V., Ratzan, S., Palayew, A., Billari, F. C., Binagwaho, A., Kimball, S., et al. (2020). COVID-SCORE: A global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10). PloS ONE 15, e0240011–e0240011. doi: 10.1371/journal.pone.0240011
Lucyk, K., Simmonds, K. A., Lorenzetti, D. L., Drews, S. J., Svenson, L. W., Russell, M. L., et al. (2019). The association between influenza vaccination and socioeconomic status in high-income countries varies by the measure used: a systematic review. BMC Med. Res. Methodol. 19, 1–23. doi: 10.1186/s12874-019-0801-1
MacDonald, N. E. (2015). Vaccine hesitancy: definition, scope and determinants. Vaccine 33, 4161. doi: 10.1016/j.vaccine.2015.04.036
Nguyen, K. H., Srivastav, A., Razzaghi, H., Williams, W., Lindley, M. C., Jorgensen, C., et al. (2021). COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination — United States, September and December 2020. Am. J. Transpl. 21, 1650–1656. doi: 10.1111/ajt.16560
Stormacq, C., Van den Broucke, S., and Wosinski, J. (2019). Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot. Int. 34, e1–e17. doi: 10.1093/heapro/day062
Taylor, S., Landry, C. A., Paluszek, M. M., Groenewoud, R., Rachor, G. S., and Asmundson, G. J. (2020). A proactive approach for managing COVID-19: the importance of understanding the motivational roots of vaccination hesitancy for SARS-CoV2. Front. Psychol. 11, 575950–575950. doi: 10.3389/fpsyg.2020.575950
The US Department of Health Human Services (2014). Social Determinants of Health. Available online at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources (accessed September 30, 2021).
Thompson, E. L., Rosen, B. L., and Maness, S. B. (2019). Social determinants of health and human papillomavirus vaccination among young adults, national health interview survey 2016. J. Commun. Health 44, 149–158. doi: 10.1007/s10900-018-0565-2
Wakefield, J. R. H., and Khauser, A. (2021). Doing it for us: community identification predicts willingness to receive a COVID-19 vaccination via perceived sense of duty to the community. J. Commun. Appl. Soc. Psychol. 31, 603–614. doi: 10.1002/casp.2542
Willis, D. E., Andersen, J. A., Bryant-Moore, K., Selig, J. P., Long, C. R., Felix, H. C., et al. (2021). COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin. Transl. Sci. 14, 2200–2207. doi: 10.1111/cts.13077
World Population Review (2021). Most Liberal States 2021. Available online at: https://worldpopulationreview.com/state-rankings/most-liberal-states (accessed October 22, 2021).
Keywords: COVID-19 vaccination, vaccination behavior, gender impact, racial disparities, socio economic status, survey
Citation: Kim B, Hong S and Kim S (2023) Are they still determining? Analysis of associations among ethnicity, gender, socioeconomic status, neighborhood factors, and COVID-19 vaccination. Front. Commun. 8:1040797. doi: 10.3389/fcomm.2023.1040797
Received: 09 September 2022; Accepted: 10 March 2023;
Published: 04 April 2023.
Edited by:
Ruma Sen, Ramapo College, United StatesReviewed by:
Muhammad Khayyam, Southwest Jiaotong University, ChinaLindsey A. Harvell-Bowman, James Madison University, United States
Copyright © 2023 Kim, Hong and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bokyung Kim, a2ltYkByb3dhbi5lZHU=
 Bokyung Kim
Bokyung Kim Seoyeon Hong
Seoyeon Hong Sungwook Kim2
Sungwook Kim2