- 1Department of Family and Preventive Medicine, Emory University School of Medicine, Atlanta, GA, United States
- 2Center for Contemplative Science and Compassion-Based Ethics, Emory University, Atlanta, GA, United States
- 3Department of Human Development and Family Studies, School of Human Ecology, University of Wisconsin-Madison, Madison, WI, United States
- 4Department of Anesthesiology, Emory University School of Medicine, Atlanta, GA, United States
- 5Department of Biology and Institute for the Liberal Arts, Emory University, Atlanta, GA, United States
Background: Depression is the largest source of global medical disability, highlighting the importance of translating and validating depression screening instruments to improve our understanding of differences in the prevalence of depression in divergent cultures around the world. The aim of this study was to translate and evaluate a widely used depression screening and diagnostic instrument, the Patient Health Questionnaire-9 (PHQ-9), for use with Tibetan populations. A secondary aim was to use the Tibetan-PHQ-9 (T-PHQ-9) to estimate the prevalence of depression symptoms in a population of Tibetan-speaking Buddhist monastic scholars engaging in a 6-year science curriculum in India, the Emory Tibet Science Initiative (ETSI).
Methods: Three-hundred-eighty-four monastics (363 monks, 21 nuns) completed the T-PHQ-9. We computed measures of internal consistency and conducted factor analysis to evaluate scale performance. Following this, we evaluated the prevalence of depressive symptoms among the monastic population. We also conducted cognitive interviews with six monastics to explore their thought processes when completing the instrument and when thinking about depression symptoms.
Results: The T-PHQ-9 had acceptable reliability and demonstrated a single-factor structure. While having low energy was the most commonly endorsed symptom, monastics did not have overall higher endorsement rates of other somatic symptoms when compared with endorsement rates of emotional symptoms. Over 10% of the monastics scored in the moderately severe to severe range and met criteria for major depressive disorder using standard diagnostic criteria cut-offs. First year monks had the highest mean score, and there was not a significant difference between monks and nuns. Cognitive interviews revealed some variation in the cognitive processes used to complete the instrument, particularly with symptoms related to energy and concentration.
Conclusion: These preliminary findings indicate that the Tibetan PHQ-9 is a reliable instrument for assessing depressive symptoms, as evidenced by its ability to inform how symptoms are experienced, interpreted, and communicated among Buddhist monastics. Results from the cognitive interviews may be important for further refining the instrument.
Background
Over 350 million people worldwide suffer from depression, making it the most common mental health disorder and the largest contributor to global disability (Smith, 2014; Vos et al., 2017; James et al., 2018; Salleh, 2018). Typified by persistent sadness and a lack of interest or pleasure in previously rewarding activities, the causes of depression are multifactorial, just as its effects can be both wide-ranging and long lasting. Given this global impact and burden of suffering, it is critical to understand cross-cultural variance in depressive symptoms, as well as the factors that influence these symptoms across time and place. Vital to this understanding is the development of screening and diagnostic instruments adapted and validated for use among diverse populations.
An estimated 150,000 Tibetan refugees live in exile, having left Tibet due to political and cultural oppression1. Previous work has documented elevated levels of trauma, post-traumatic stress disorder, and anxiety among these Tibetan humanitarian migrants (Mills et al., 2005; Evans et al., 2008). The Tibetan diaspora began in 1959 with the escape of the 14th Dalai Lama to India to avoid persecution by the Chinese People’s Liberation Army (Conway, 1975). While Tibetan refugees still travel to Dharamsala - the current residence of the Dalai Lama in India - the number has dropped over the last decade, due in part to economic and cultural uncertainty in India (Purohit, 2019). Many Tibetans from both Tibet and India are traveling to other countries, particularly Canada, Switzerland, the United States, and Germany (Purohit, 2019). With this history of persecution and oppression and elevated risk for mental health concerns, and given the dynamic insecurities experienced by Tibetans living in diaspora communities, it is crucial to translate, adapt, and evaluate psychometric instruments for screening depression among Tibetans and Tibetans in exile.
Among the almost 40,000 Tibetan Buddhist monastics living in India and nearby countries (Sonam, 2019), a growing number participate in a novel science curriculum, the Emory-Tibet Science Initiative (ETSI). First created in 2006 at the behest of His Holiness the Dalai Lama, ETSI is a collaboration between Emory University and the Library of Tibetan Works and Archives to establish a bidirectional convergence of science and spirituality. The program aims to innovate and implement a comprehensive and rigorous educational curriculum built on shared systems of knowledge to teach contemporary scientific knowledge to Tibetan monks and nuns. International science faculty collaborate with Tibetan translators and teachers to provide continuous English-Tibetan translation during classes. As of 2018, over 1,500 monastics have engaged with what is now a 6-year ETSI science curriculum in neuroscience, biology, physics, and epistemology, which includes a summer science intensive program (Gray and Eisen, 2019). Beginning in 2018, scientific concepts taught during ETSI are now included in the examination for the Geshe Lharam degree, the monastic equivalent to a western doctorate. For several reasons, the ETSI program is a salutary venue for the process of translating a depression questionnaire into Tibetan. First, Tibetan interpreters have been essential to ETSI throughout the project, and the process and theory of translating scientific concepts into Tibetan has been foundational to every part of ETSI (Gray et al., 2020). Translators and monastics alike are extraordinarily adept at the iterative and dynamic process of cross-cultural and cross-linguistic scientific dialogue. Second, monks and nuns enrolled in ETSI are highly educated in Buddhist logic, philosophy, and models of mind, making them thoughtful reporters of the phenomenology of mental health symptoms (Gray and Eisen, 2019).
In addition to the importance of constructing tools for evaluating depression symptoms in Tibetan communities, exploring depressive symptoms among Tibetan Buddhist monastics presents an opportunity to understand the proximate outcome of the complex interaction of factors that enact both risk for, and buffering against, depression. On the one hand, growing research highlights the deleterious impact to mental health that can result from becoming a humanitarian migrant (Fazel et al., 2005; Chen et al., 2017). On the other hand, many monastics maintain a lifestyle that may buffer them from developing depression. For example, the interconnected community of a monastery likely reduces loneliness and economic stress, both of which increase the risk for mental illness during post-migration resettlement (Laban et al., 2008; Chen et al., 2017). Monastics often primarily consume a vegetarian diet, which has been associated with a reduced prevalence of depression (Jin et al., 2019). Moreover, some - though not all - Tibetan Buddhist monastics maintain regular contemplative practices, which have positive effects on mental health and well-being (Verma and Araya, 2010). In addition to contemplative practices, Buddhist belief systems may buffer monastics from the harmful effects of stress or trauma, and may provide a mental framework that shapes symptoms of depression and mental distress (Holtz, 1998; Hussain and Bhushan, 2013; Lewis, 2013; 2018). In sum, the lived experience of monastics likely includes both risk and buffering factors, and examining mental health and illness in this context will enrich our overall understanding.
In this study, our first aim was to translate one of the most widely used depression diagnostic and screening instruments (Tam et al., 2019), the Patient Health Questionnaire (PHQ), for use with Tibetan populations. The PHQ-9 depression diagnostic instrument is a well-validated measure for detecting depression and reflects current criteria for major depression (Kroenke et al., 2010; Blackwell and McDermott, 2014), but to our knowledge it has not been translated for use with Tibetan populations. Our second aim was to evaluate the Tibetan PHQ-9 (T-PHQ-9) using quantitative (factor analysis and psychometric evaluation) and qualitative (cognitive interviewing) methods. A final exploratory aim was to use the T-PHQ-9 to estimate the prevalence of depressive symptoms in a population of Tibetan-speaking Buddhist monks and nuns enrolled in ETSI.
Methods
Overview: The Emory University Institutional Review Board approved the study, and all work was conducted in accordance with the Declaration of Helsinki. As described in more detail below, we first created a Tibetan translation of the widely used depression screening and diagnostic instrument, the Patient Health Questionnaire (PHQ). Next, we administered the T-PHQ-9 to participating monks and nuns during implementation of the summer curriculum in 2019. Finally, we conducted cognitive interviews with a separate group of monks (n = 6) to examine the cognitive processes involved in completing the T-PHQ-9. For the quantitative portion of the study, we obtained signed, informed consent from 453 monastic participants (419 monks, 34 nuns) after a full description (in Tibetan) of study procedures, risks, and potential benefits prior to conducting any study procedures. For the cognitive interviews, we obtained informed consent from six monks after a full description (in Tibetan) of study procedures, risks, and benefits.
Participants: Participants in the quantitative study were Tibetan monastics from five monasteries and four nunneries in India who attend classes to study science with the Emory-Tibet Science Initiative (ETSI), held at the Science Center at the Drepung Losel Ling Monastery in South India. We recruited monastics via an optional face-to-face presentation. There were no exclusion criteria. Because we were interested in item performance, we omitted participants who failed to complete all T-PHQ-9 items (n = 69) and thus the final dataset was composed of 384 monastics (363 monks, 21 nuns). Participants in the cognitive interviewing component of the study were six monks enrolled in ETSI and in residence at Emory University.
Measure: The Patient Health Questionnaire depression module (PHQ-9) is a measure of depression severity that scores each of nine Diagnostic and Statistical Manual of Mental Disorders (DSM 5) symptom criteria according to how often the symptom bothered the person during the previous 2 weeks: 0 = “not at all”; 1 = “several days”; 2 = “more than half the days”; 3 = “nearly every day” (Kroenke et al., 2001). The nine symptoms assessed are: anhedonia, depressed mood, insomnia or hypersomnia, fatigue or loss of energy, appetite disturbances, guilt, diminished ability to think or concentrate, psychomotor agitation, and suicidal ideation. A 10th item rates how the depression symptoms impact daily function, but it is not used in scoring and is not included here. We used conventional categories of symptom severity: 0–4 = Minimal depression severity; 5–9 = Mild; 10–14 = Moderate; 15–19 = Moderately severe; 20–27 = Severe. In addition, we used the conventional cut-off score of 10 or more for major depressive disorder (MDD); (Kroenke et al., 2001).
Measure translation: In the first phase, one translator proficient in English and Tibetan translated the PHQ-9 into Tibetan. Translation and back translation of the Tibetan version of the PHQ-9 was repeated by a group of five translators who provided feedback on the original version until they believed that the Tibetan version accurately corresponded with the English version.
Prior to administering the survey, the research coordinator explained the purpose of the study through an experienced English to Tibetan interpreter employed as an educator by ETSI. After consent, monastics completed the survey with no time restrictions, and they were able to ask questions of the research team via the translator.
Statistical Analysis: All data were double entered to ensure accuracy. To address our first aim of evaluating individual T-PHQ-9 items and scale performance, we examined the internal consistency by computing the Cronbach’s alpha coefficient. To evaluate construct validity, we conducted a factor analysis to evaluate whether a single factor model could be generated for the nine items of the Tibetan PHQ-9, as has been reported in previous studies (e.g., Cameron et al., 2008; Liu et al., 2011; Kocalevent et al., 2013; Dadfar et al., 2018), or whether a two- or three-factor model was a better fit. First, we assessed whether the data were suitable for conducting a factor analysis and found that it was appropriate to proceed using Bartlett’s test of sphericity [p < 0.001] (Bartlett, 1954; Hair, 2009), and the Kaiser-Meyer-Olkin measure of sample adequacy = 0.83 (Kaiser, 1960; Hair, 2009). Next, we conducted a principal component analysis, excluding cases listwise.
To describe the prevalence of depressive symptoms in the monastic population, we generated descriptive statistics (mean, standard deviation, and endorsement frequency) for single items and the median and interquartile range for the sum score of the measure. In addition, we describe monastic participants’ scores according to PHQ-9 diagnostic categories, separated by year in the ETSI program and sex for comparison. We also calculated the prevalence of depression with 95% confidence interval, using the cut-off score of 10 for MDD. To examine whether depression scores differed by ETSI year, we conducted one-way ANOVA followed by Games-Howell post-hoc multiple comparisons tests. To examine whether scores differed between monks and nuns, we conducted a Mann-Whitney test. All statistical analyses were conducted using SPSS (version 26.0 for Windows, SPSS, Inc., Chicago, IL).
Cognitive Interviews: To explore the cross-cultural equivalence of the T-PHQ-9 and to learn about the cognitive processes involved in comprehension of and response to each survey item, we conducted cognitive interviews with six monastic scholars enrolled in ETSI and in residence at Emory. Cognitive interviewing (CI) is a method commonly used to understand how survey items are understood and answered, and it can help identify problems in item translation and interpretation as well as in survey design, organization, and instruction (Collins, 2003; Beatty and Willis, 2007; Campanelli et al., 2015; Meadows, 2021). In general and in practice for the current study, CI involves the administration of survey items, interspersed with the collection of additional information about the accompanying response to each item.
Two researchers (W.K., M.W.) and the translator (T.S.) conducted the cognitive interviews via Zoom using the following procedure. First, we provided the monk with the T-PHQ-9. Next, the translator read each item. After the interviewer read each item, the interviewer asked the monk a series of four questions. First, they asked the participant to describe what the item means in their own words. Next, they asked them to describe their thought process if they were to answer the question. The interviewer used probing prompts to elicit more detail, including asking the monks to describe a situation in which someone might feel or experience the symptom or to think of an example in which someone might experience the symptom. Third, they asked the participant if they know anyone experiencing this symptom. Finally, they asked the participant how they think people would feel saying they experience the symptom. After asking these four questions about each of the 9 T-PHQ-9 items, the interviewer asked the participants two final questions: “What do you think is missing from this questionnaire that would be helpful to evaluate depression?” and “Can you think of any idioms, sayings, phrases, or expressions that you or others use to refer to depression?”
Results
Reliability and item analysis: Cronbach’s alpha for the total scale was 0.71, which is considered acceptable. The mean scores for all T- PHQ-9 items are shown in Table 1. All items, if deleted, would decrease the total alpha, although the alpha would be essentially the same if item 9 (suicidal ideation) was deleted. Item nine also had the lowest item-total correlation and was endorsed far less frequently than all other items (see Table 2). Item-total correlations ranged from 0.30 to 0.46 (Table 1).
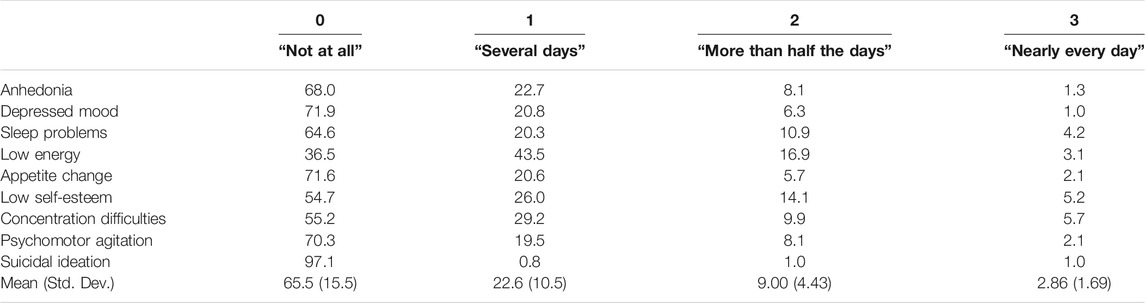
TABLE 2. T-PHQ-9 item responses listed as percent monastics endorsing each response option. Each of the items is scored with the following 4-point response options: 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day).
Construct validity: A principal components factor analysis yielded a single-factor structure, which accounted for 31.1% of the variance in item responses and yielded a total eigenvalue of 2.80. The factor-pattern coefficients ranged from 0.45–0.63 (Table 1).
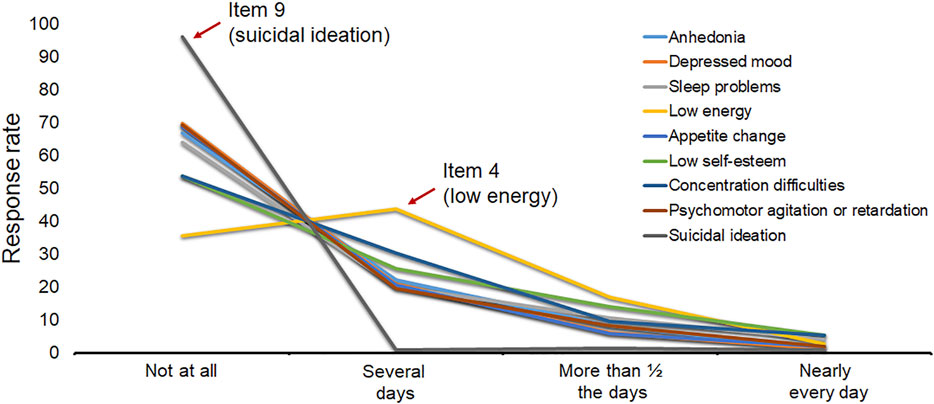
Prevalence of symptoms and participant characteristics: Item response frequencies are detailed in Table 2 and visualized in Figure 1. The majority of monastics chose “not at all” for all items except “low energy”, for which the majority (43.5%) chose “several days”. T-PHQ-9 sum scores are detailed in Table 3.
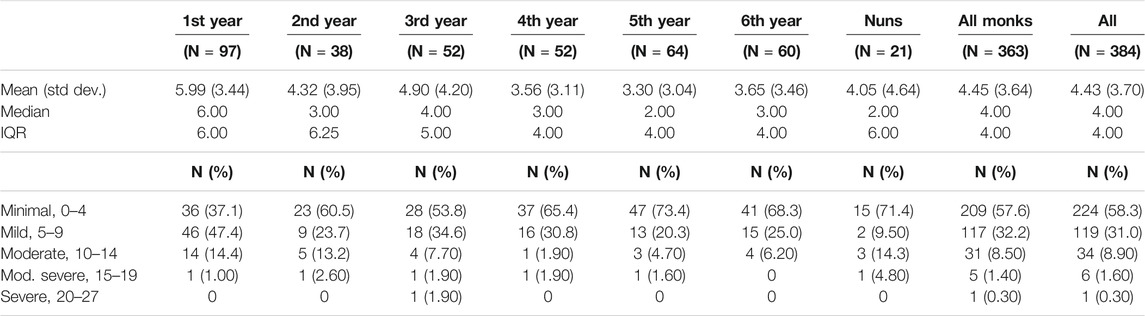
TABLE 3. Mean, standard deviation, median, interquartile range (IQR) of T-PHQ-9 sum scores, as well as frequency (number and percentage) of monastics falling within each of the diagnostic categories. All scores are reported 1) according to monastic year for monks, 2) for nuns, 3) for all monks, and 4) for all monastics combined (monks and nuns).
Participant sum scores were non-normally distributed, with skewness of 1.08 (S.E. = 0.13) and kurtosis of 1.14 (S.E. 0.25). The mean sum score for all monastics was 4.43 (Std. Dev. = 3.70). First year monks had the highest mean score (M = 5.99, SD = 3.44), which was significantly higher than the mean score for other years (F (6, 377) = 5.34, p < 0.001). Post-hoc analyses using Games-Howell tests indicated that first year monks reported higher levels of depression than monks in their fourth (p = 0.001), fifth (p < 0.001), and sixth (p = 0.001) years. There was not a significant difference between the monks and nuns (U = 3,185, p = 0.20). Using diagnostic criteria from previous reports, 244 (58.3%) monastics were in the minimal severity range (0–4), 119 (31.0%) in the mild severity range (5–9), 34 (8.90%) in the moderate severity range (10–14), 6 (1.60%) in the moderately severe range (15–19), and 1 (0.30%) in the severe range (20–27) (Table 3). The prevalence of MDD based on the traditional cutoff score of 10 was 10.7% (95% CI 7.77, 14.2).
Cognitive Interviews: Overall, the monks tended to indicate that they were thinking of specific examples or contextual factors in their efforts to answer each of the items. For example, with respect to answering item 3 (“Trouble falling or staying asleep, or sleeping too much?”), one monk stated, “So, this could happen when one is occupied by some important things perhaps an important task that one had to-one has to finish … because of which, you know, one is not able to sleep … this could also happen when one has too much stress or pressure and with the excessive sleep one is not able to you know wake up uh or stay awake even if one has to finish a task.” In answering item 5 (“Feeling bad about yourself—or that you are a failure or have let yourself or your family down?”), one monk noted, “So this question is not very clear to my mind, I would be thinking about things that I couldn’t achieve. Mmm, and I would also be thinking about the time when I left Tibet … that action, or my decision to leave Tibet could have repercussions for my family, especially my immediate families. So I would be, you know, I’d be thinking about those.”
It was common for monks to have difficulty thinking of a person they know who experienced a given symptom. For example, the majority (4) of the monks reported that they could not think of anyone they know who has experienced feeling like a failure or having low self-esteem (item 5). However, for other symptoms, monks were able to call to mind someone they know who has experienced that symptom. For example, with reference to sleep difficulty (item 3), one monk stated, “I could think of one monk from my monastery, you know, who was-who was very old, and he had so much trouble, you know, sleeping, difficulty in falling asleep. And it might be because of his health or because of his age. He would often, you know, cry all throughout the night, so I know of that person.”
The interviewees’ ability to think of someone they know who experienced each symptom may be related to the degree of stigma surrounding the disclosure of each of the depressive symptoms. There were several symptoms that the monks felt would carry stigma and for which people might feel embarrassed to discuss, particularly eating too much (4 monks noted that people would feel embarrassed to admit this) and thoughts of suicide (all the monks indicated that people may feel uncomfortable sharing thoughts of suicide). Half of the monastics reported that people might feel uncomfortable disclosing that they have trouble concentrating on their studies. One monk explained an inherent tension involved in answering the questionnaire: “So [I] think it will be-people may struggle depending on their, you know, their outlook. For instance, the monastics are encouraged to, you know, speak truth and be honest. So, you know, even if you are not-feeling even if you are feeling hopeless and, you know, feeling down, you might be tempted to answer in the opposite but, you know, that ethically that will be wrong. So, there would be this tension. On the other hand, you know, people might feel a little embarrassed or uncomfortable, you know, revealing that they are feeling down or hopeless.”
The cognitive interviews also revealed that there appear to be differences in the ways in which monks interpreted the items than are generally intended for the PHQ-9. For example, with respect to item four about low energy, two of the monks noted the distinction between mental and physical energy, and reported that this distinction would be important for answering the item. Several monks appeared to reflect on item 6 (“Trouble concentrating on things, such as reading the newspaper or watching television?”) with reference to interest level, rather than as a general difficulty with concentration. For example, one monk noted, “…this to me seems to be asking about one’s interest or related to one’s interest. So, for me, … I’m interested in reading and I’m also interested in watching … I would think about, you know, where my interest lies and so on.” Similarly, other monks discussed situations in which they have difficulty concentrating on something that does not interest them. When asked if they know anyone experiencing this symptom, most monks talked about classmates or friends who are bored by a particular topic or activity. For example, one monk stated, “Uh yes, my classmates, you know, when we were young, and we were made to read books, you know, they would be completely bored and couldn’t focus. And similarly, you know, watching-when we were made to watch documentary shows, we couldn’t- or they couldn’t concentrate.” Only one of the monks referenced difficulty concentrating due to mood: “So, this could happen because one is not well, or that one is feeling unhappy. Or that something else is occupying, you know, the person’s mind, such as work or tasks that one has to finish.”
With respect to what they thought is missing from the survey, half of the monks mentioned the relationship between stress and depression. For example, one monk stated, “You know, depression and other mental problems, such as, you know, mental health such as, you know, stress … often, these two, tend to have many similar symptoms. And as such, you know, it’s a little hard for [me] to kind of distinguish between the two.” A second stated, “Uh well [I] think that depression could be initiated or started by feeling too much pressure. And so, therefore, it could be started by one’s custom or culture or habits. So, perhaps questions about these might be helpful.”
Discussion
Here, we examined a Tibetan translation of the PHQ-9, which will be important for screening and understanding the prevalence of depression symptoms among Tibetans and Tibetan refugees faced with dynamic globalization and economic and cultural insecurity. The PHQ-9 reflects current criteria for major depression and has been translated into various languages, but to our knowledge, this is the first translation into Tibetan. The quantitative data collected from monastics enrolled in ETSI indicate that the T-PHQ-9 has acceptable reliability and holds promise as a clinical instrument. Our exploratory factor analysis indicates that the T-PHQ-9 has a single factor structure, as is consistent with many previous studies (Cameron et al., 2008; Liu et al., 2011; Kocalevent et al., 2013; Dadfar et al., 2018). While other studies have supported a two-factor model, corresponding to somatic (e.g., sleep, appetite, and fatigue items) and non-somatic or affective symptoms (e.g., mood, suicidal thought items) (Krause et al., 2010; Elhai et al., 2012; Petersen et al., 2015; Guo et al., 2017), our data do not support such a model. Although the T-PHQ-9 demonstrates acceptable reliability, it has a lower alpha than has been found in other studies, many of which have yielded alpha levels above 0.80 (e.g., Kroenke et al., 2001; Cameron et al., 2008; Liu et al., 2011; Wang et al., 2014; Rancans et al., 2018; Kim and Lee, 2019). The lower reliability may reflect something about the current translation, or it may reflect true differences in the way that symptoms are interpreted, experienced, or reported by this unique study population.
With respect to individual item performance, these data indicate that all items were important to the overall construct. However, there was variance in item endorsement. Consistent with other studies, very few monastics endorsed experiencing suicidal ideation (Huang et al., 2006). The most commonly endorsed item, on the other hand, was “Low energy”, and the majority of the monastics (>60%) reported experiencing this symptom at least several days per week. Several studies conducted among Asian populations have found higher rates of somatic symptoms (sleep problems, low energy, and appetite change) [for example, (Kleinman and Kleinman, 1985; Yen et al., 2000; Huang et al., 2006; Lotrakul et al., 2008)]. While the monastics in this study had relatively higher rates of endorsement of “Low energy”, they did not have higher rates of other somatic symptoms compared with endorsement rates of emotional symptoms (e.g., anhedonia). Taken with the single-factor model identified with these data, this study is not consistent with the characterization of Asian racial/ethnic groups as more likely to experience somatic symptoms of depression and it highlights the importance of moving beyond simple east-west essentialism (Kirmayer, 2001; Boiger et al., 2018).
While the PHQ-9 is among the most widely used measures of depression and has proven important as a diagnostic and screening tool in disparate clinical contexts and among diverse populations, the diagnostic utility of the current translation will require further evaluation. Previous research has indicated that diagnostic cutoff scores of 10 are clinically meaningful and have high levels of sensitivity (88%) and specificity (88%), as individuals with major depression seldom score below that range (Kroenke et al., 2001; Kroenke et al., 2010). We used this conventional diagnostic scoring criteria to interpret the current data; however, future research should examine the diagnostic validity of the T-PHQ-9. Responses in the current study indicate that 89.3% of monastics fall in the minimal and mild range for depression. Interestingly over 10% of the monastics fell in the moderate and above range, with 2% categorized as experiencing moderately severe or severe depression.
Rates of MDD in the current sample are lower than those reported in other refugee and exiled populations. For example, the PHQ-9 was used to detect MDD in 44% of Syrian asylum seekers in Greece (Poole et al., 2018), in 27% of Syrian refugees in Germany (Borho et al., 2020), and in 50% of a heterogeneous population of refugees living in refugee housing in Sweden (Leiler et al., 2019). Among Tibetan adolescents and young adults living in India, 79% scored above the cut-off score of 1.75 on the Hopkins Symptom Checklist-25, indicating significant emotional distress (Evans et al., 2008). Interestingly, that study found that rates of distress were higher among young adults born in Tibet who escaped to India, compared to ethnic Tibetans born in exile. Monastics in our sample were a mix of monks and nuns born in Tibet and those of both Tibetan and Indian descent born in India; unfortunately, we did not collect birth or migration histories from the monastics in our study and are unable to examine whether the same trend was observed. Regardless, rates observed in our study were much lower than prevalence rates observed in the study of adolescents, consistent with the overall indication that monastics have lower rates of depression symptoms than other comparable refugee populations. Moreover, while clinical interpretations of these data warrant great caution, our preliminary findings indicate that the T-PHQ-9 is sensitive to variation in depression symptoms and that it appears to be operating similarly to other population studies that evaluate the point prevalence of depression.
Monastic scholars in our sample are not only refugees but are also students, and careful consideration should be given to determining the most appropriate comparison groups to interpret the current data. These monastic science students may have relatively more in common with other student populations than with a more general adult population or with other refugee populations, especially to the Geshe Lharam degree is considered equivalent in rigor to the PhD and likely carries comparable levels of effort and stress, Among studies of students, there appears to be a relatively large amount of variance in PHQ-9 scores and in the prevalence of MDD. For example, in a study of Chinese medical students, the mean PHQ-9 score was 6.02, with 13.5% of respondents reporting scores that reflect MDD (Sobowale et al., 2014). Similarly, a large study of South Korean medical students found that 13.7% of students scored in the moderate to severe range (Yoon et al., 2014) and rates of MDD among medical students in India were found to be over 30% (Patil et al., 2018). A study of medical students in Cameroon found that 30.6% scored in the moderate to severe range (Ngasa et al., 2017). There also appears to be extensive variation in prevalence of depression among university students, with rates of depression ranging from 10 to 85% (Ibrahim et al., 2013). A recent meta-analysis indicates that depression is highly prevalent among PhD students, with a pooled prevalence of clinically significant depression of 24% (Satinsky et al., 2021). Depression levels in the current study were at the bottom-end of what is generally seen in studies of university and post-graduate students.
Taken together, the prevalence of depression symptoms among these monastic scholars is similar to rates found in general populations, but quite a bit lower than is often found in both refugee and student populations. Monastics may experience lifestyle factors or engage in health behaviors that are protective from depression, a possibility that warrants further inquiry. Several large studies point to factors that exert direct effects on risk of major depression, including income, sleep disorders, and chronic diseases (Majidi et al., 2018). Other studies find associations between nutritional status, adiposity, and physical activity and rates of depression (Ngasa et al., 2017; Li et al., 2018; Jin et al., 2019). A large body of research has found that education (Bauldry, 2015; Madden, 2016) and religiosity (Wangmo and Teaster, 2010; Gearing and Alonzo, 2018) are protective against depression, which would suggest that monastics may be relatively buffered from experiencing depression. However, another study of Tibetan refugees living in India found lower prevalence of depression and importantly found no association between monastic status or educational variables and depression levels (Sachs et al., 2008). Future research should examine the relationship between depression symptoms and specific health behaviors among monastic refugees.
However, the findings from this study indicate that the monastic scholars are not free from depression; rather, rates are higher than are found in several population studies (for example, (Kocalevent et al., 2013; Brody et al., 2018)). Monastics in our sample may experience specific burdens that affect their experience of depression symptoms. Tibetan culture and traditions, including the growth and development of monastic universities serve the purpose of maintaining Tibetan culture in the hope of a future repatriation to the ancestral homeland. A community in diaspora navigates the present circumstance with great care. By definition, the aspirations of the community are to return, but the reality requires the laying down of a local foundation. As the years pass, all that may be known is the current reality, and the more settled in place, the weaker the claim becomes for repatriation. Diaspora communities risk adverse mental health as a consequence of state impermanence (Benedict et al., 2009). Previous studies have found high rates of trauma exposure, post-traumatic stress disorder, and depressive and anxiety symptoms among children and adolescent Tibetan refugees (Servan-Schreiber et al., 1998; Evans et al., 2008), findings that are congruent with our own and which highlight the importance of mental health resources for exiled communities. Moreover, during the cognitive interviews several monastics reported on the high rates of stress and pressure involved in their monastic studies, and pointed to this stress as a risk factor for depression.
Although the quantitative data indicated that the T-PHQ-9 is a reliable instrument for quantifying depression symptoms, the cognitive interviews suggest that monks may interpret some items differently than is generally intended by the PHQ-9. This was especially the case for the concentration and low energy items, in which Tibetan Buddhist cultural and linguistic distinctions between interest/concentration and mental/physical energy may be crucial. This knowledge may be used to refine the T-PHQ-9 for future use. Importantly, researchers have identified two disparate objectives of cognitive interviewing in the context of survey development (Willis, 2015; Meadows, 2021). On the one hand, CI can be reparative, with a primary goal of identifying and fixing specific problems in the survey. Alternatively, CI can be used descriptively to gain a better understanding of whether and how the survey is tapping into the construct it is intended to measure. Here, we conceptualized and analyzed our interviews as more aligned with the latter goal. However, we only surveyed the monastics in residence at Emory and thus may not have reached saturation in our dataset. Moreover, these interviews could be used in an iterative way to refine and optimize the T-PHQ-9, an important next step for future research. In addition, the discrepancies in meaning for interest/concentration and mental/physical energy may have influenced the factor analysis. More fine-grained examination of these cultural-linguistic distinctions will be important toward more definitively interpreting the one-factor result and for ruling out a two-factor model that may have arisen with a more precise or concordant translation for those items. Gaining clarity on item 4 (low energy/fatigue) will be particularly crucial since it falls on the somatic factor in two-factor models. Two of the monks noted the distinction between mental and physical energy when thinking about this item and had difficulty answering as a result. A thorough comparison of the cultural/linguistic meaning and cognitive scripts involved in answering this item would help disambiguate the possible interpretations. Moreover, it is possible that the monastics would be more sensitively assessed if that item were split into two items, tapping into mental and physical energy as distinct symptoms.
Limitations and future directions: For several reasons, caution is warranted with diagnostic claims or interpretations of the current data. First, as stated above, we did not conduct any validity estimates within the current study. Future research should examine convergent validity of the T-PHQ-9 and other validated instruments. In addition, we did not conduct clinical diagnostic interviews, and we are unable to determine whether the cut-off score of 10 for MDD that we used is applicable for this study population. Second, while we conducted cognitive interviews with a small number of monks, more thorough qualitative evaluations are warranted to explore how monastics understood and related to the translated items given the complex ways that linguistic and cultural differences will impact how emotions are perceived and interpreted, as well as how distress and symptoms of distress are communicated (Kirmayer, 2001). Related, the monastics are relatively unfamiliar with survey instruments like the PHQ, which may influence the way they thought about the items or answered the survey. In fact, one monk pointed this out in the cognitive interview. This may help explain why a relatively high percentage (15%) of the monastics who took the T-PHQ-9 left at least one of the nine items unanswered. In addition, while we have placed our findings alongside a large body of research examining the prevalence of depression using the PHQ-9, the uniqueness of the population studied here limits the generalizability of the current preliminary results to other Tibetan-speaking populations. The T-PHQ-9 should be evaluated among other populations, an extension of the present research that would help overcome potential translation difficulties and help inform the interpretation of the data presented here.
Another important next step in this research is to examine how age and sex impact monastic depression symptoms. While we did not find a significant difference between monks and nuns, we were likely underpowered to examine whether well-described sex-differences in depression (Evans et al., 2008; Brody et al., 2018; Eid et al., 2019) are also evident among this monastic population. Nuns are newly involved with ETSI, and as their representation grows there will be more nuns available to participate in future iterations of this research program. It will also be critical to examine lifestyle risk factors as well as social and cultural influences on monastics’ experience of depression symptoms. Finally, this study raises critical issues related to the ethical obligations and best practices in conducting cross-cultural research at the intersection of mental health.
Conclusion
Preliminary evidence indicates that the T-PHQ-9 is a reliable instrument for future analyses. While we must interpret these data with care, they highlight the importance of diagnostic and clinical resources made available to monastics.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Emory University Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JM helped design the study, analyzed and interpreted the data, and was a major contributor in writing the manuscript; DS helped design the study, helped administer surveys and enter data, and helped with data interpretation and writing the manuscript; WK and MW conducted and transcribed the cognitive interviews; EB helped analyze the cognitive interviews; TS translated the survey, helped administer surveys, and helped with data interpretation and writing the manuscript; HC helped enter data and helped with writing the manuscript, CR contributed to interpretation of the data and writing the manuscript, JZ and AE were major contributors in designing the study and helped with interpretation and writing the manuscript. All authors critically read and approved the final manuscript.
Funding
The cognitive interviews were supported by the Nat C. Robertson Endowment in Science and Society.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
This project is indebted to His Holiness the Dalai Lama, who envisioned and supports, together with Joni Winston, the Emory Tibet Science Initiative. We are grateful to the translators for their expertise and assistance and to all of the monastics for their time and efforts in completing the survey. We are also grateful to Elizabeth Walker and Marcia Ash for their helpful feedback on the cognitive interview guide.
Abbreviations
ETSI, Emory-Tibet Science Initiative; MDD, Major Depressive Disorder; PHQ-9, Patient Health Questionnaire-9; T-PHQ-9, Tibetan Patient Health Questionnaire-9.
Footnotes
1127935 Tibetans living outside Tibet: Tibetan survey. Hindustan Times Dec 04, 2010
References
Bartlett, M. S. (1954). A Note on the Multiplying Factors for Various χ2 Approximations. J. R. Stat. Soc. Ser. B (Methodological) 16, 296–298. doi:10.1111/j.2517-6161.1954.tb00174.x
Bauldry, S. (2015). Variation in the Protective Effect of Higher Education against Depression. Soc. Ment. Health. 5, 145–161. doi:10.1177/2156869314564399
Beatty, P. C., and Willis, G. B. (2007). Research Synthesis: The Practice of Cognitive Interviewing. Public Opin. Q. 71, 287–311. doi:10.1093/poq/nfm006
Benedict, A. L., Mancini, L., and Grodin, M. A. (2009). Struggling to Meditate: Contextualising Integrated Treatment of Traumatised Tibetan Refugee Monks. Ment. Health Religion Cult. 12, 485–499. doi:10.1080/13674670902788908
Blackwell, T. L., and McDermott, A. N. (2014). Review of Patient Health Questionnaire–9 (PHQ-9) [Review of the test Patient Health Questionnaire–9 (phq-9), by R. L. Spitzer, J. B. W. Williams and K. Kroenke]. Rehabil. Couns. Bull. 57 (8), 246–248. doi:10.1177/0034355213515305
Boiger, M., Ceulemans, E., De Leersnyder, J., Uchida, Y., Norasakkunkit, V., and Mesquita, B. (2018). Beyond Essentialism: Cultural Differences in Emotions Revisited. Emotion 18, 1142–1162. doi:10.1037/emo0000390
Borho, A., Viazminsky, A., Morawa, E., Schmitt, G. M., Georgiadou, E., and Erim, Y. (2020). The Prevalence and Risk Factors for Mental Distress Among Syrian Refugees in Germany: a Register-Based Follow-Up Study. BMC psychiatry 20. doi:10.1186/s12888-020-02746-2
Brody, D. J., Pratt, L. A., and Hughes, J. P. (2018). Prevalence of Depression Among Adults Aged 20 and Over: United States, 2013–2016. NCHS Data Brief (303), 1–8.
Cameron, I. M., Crawford, J. R., Lawton, K., and Reid, I. C. (2008). Psychometric Comparison of PHQ-9 and HADS for Measuring Depression Severity in Primary Care. Br. J. Gen. Pract. 58, 32–36. doi:10.3399/bjgp08x263794
Campanelli, P., Blake, M., Mackie, M., and Hope, S. (2015). Mixed Modes and Measurement Error: Using Cognitive Interviewing to Explore the Results of a Mixed Modes experiment. ISER Working Paper Series 2015-18.
Chen, W., Hall, B. J., Ling, L., and Renzaho, A. M. (2017). Pre-migration and post-migration Factors Associated with Mental Health in Humanitarian Migrants in Australia and the Moderation Effect of post-migration Stressors: Findings from the First Wave Data of the BNLA Cohort Study. The Lancet Psychiatry 4, 218–229. doi:10.1016/s2215-0366(17)30032-9
Collins, D. (2003). Pretesting Survey Instruments: an Overview of Cognitive Methods. Qual. Life Res. 12, 229–238. doi:10.1023/a:1023254226592
Dadfar, M., Kalibatseva, Z., and Lester, D. (2018). Reliability and Validity of the Farsi Version of the Patient Health Questionnaire-9 (PHQ-9) with Iranian Psychiatric Outpatients. Trends Psychiatry Psychother. 40, 144–151. doi:10.1590/2237-6089-2017-0116
Eid, R. S., Gobinath, A. R., and Galea, L. A. M. (2019). Sex Differences in Depression: Insights from Clinical and Preclinical Studies. Prog. Neurobiol. 176, 86–102. doi:10.1016/j.pneurobio.2019.01.006
Elhai, J. D., Contractor, A. A., Tamburrino, M., Fine, T. H., Prescott, M. R., Shirley, E., et al. (2012). The Factor Structure of Major Depression Symptoms: a Test of Four Competing Models Using the Patient Health Questionnaire-9. Psychiatry Res. 199, 169–173. doi:10.1016/j.psychres.2012.05.018
Evans, D., Buxton, D. C., Borisov, A., Manatunga, A. K., Ngodup, D., and Raison, C. L. (2008). Shattered Shangri-La: Differences in Depressive and Anxiety Symptoms in Students Born in Tibet Compared to Tibetan Students Born in Exile. Soc. Psychiat Epidemiol. 43, 429–436. doi:10.1007/s00127-008-0346-9
Fazel, M., Wheeler, J., and Danesh, J. (2005). Prevalence of Serious Mental Disorder in 7000 Refugees Resettled in Western Countries: a Systematic Review. The Lancet 365, 1309–1314. doi:10.1016/s0140-6736(05)61027-6
Gearing, R. E., and Alonzo, D. (2018). Religion and Suicide: New Findings. J. Relig Health. 57, 2478–2499. doi:10.1007/s10943-018-0629-8
Gray, K. M., and Eisen, A. (2019). The Emory-Tibet Science Initiative: Rethinking Cross-Cultural Science and Teaching. J. Microbiol. Biol. Educ., 20. doi:10.1128/jmbe.v20i1.1618
Gray, K. M., Namgyal, D., Purcell, J., Samphel, T., Sonam, T., Tenzin, K., et al. (2020). Found in Translation: Collaborative Contemplations of Tibetan Buddhism and Western Science. Front. Commun. 4, 76. doi:10.3389/fcomm.2019.00076
Guo, B., Kaylor-Hughes, C., Garland, A., Nixon, N., Sweeney, T., Simpson, S., et al. (2017). Factor Structure and Longitudinal Measurement Invariance of PHQ-9 for Specialist Mental Health Care Patients with Persistent Major Depressive Disorder: Exploratory Structural Equation Modelling. J. Affective Disord. 219, 1–8. doi:10.1016/j.jad.2017.05.020
Hair, J. F. (2009). Multivariate Data Analysis: A Global Perspective. 7th ed.. Upper Saddle River: Prentice Hall.
Holtz, T. H. (1998). Refugee Trauma versus Torture Trauma: a Retrospective Controlled Cohort Study of Tibetan Refugees. J. Nervous Ment. Dis. 186, 24–34. doi:10.1097/00005053-199801000-00005
Huang, F. Y., Chung, H., Kroenke, K., Delucchi, K. L., and Spitzer, R. L. (2006). Using the Patient Health Questionnaire-9 to Measure Depression Among Racially and Ethnically Diverse Primary Care Patients. J. Gen. Intern. Med. 21, 547–552. doi:10.1111/j.1525-1497.2006.00409.x
Hussain, D., and Bhushan, B. (2013). Posttraumatic Growth Experiences Among Tibetan Refugees: A Qualitative Investigation. Qual. Res. Psychol. 10, 204–216. doi:10.1080/14780887.2011.616623
Ibrahim, A. K., Kelly, S. J., Adams, C. E., and Glazebrook, C. (2013). A Systematic Review of Studies of Depression Prevalence in university Students. J. Psychiatr. Res. 47, 391–400. doi:10.1016/j.jpsychires.2012.11.015
James, S. L., Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N., et al. (2018). Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 354 Diseases and Injuries for 195 Countries and Territories, 1990-2017: a Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858. doi:10.1016/S0140-6736(18)32279-7
Jin, Y., Kandula, N. R., Kanaya, A. M., and Talegawkar, S. A. (2019). Vegetarian Diet Is Inversely Associated with Prevalence of Depression in Middle-Older Aged South Asians in the United States. Ethn. Health, 1–8. doi:10.1080/13557858.2019.1606166
Kaiser, H. F. (1960). The Application of Electronic Computers to Factor Analysis. Educ. Psychol. Meas. 20, 141–151. doi:10.1177/001316446002000116
Kim, Y. E., and Lee, B. (2019). The Psychometric Properties of the Patient Health Questionnaire-9 in a Sample of Korean University Students. Psychiatry Investig. 16, 904–910. doi:10.30773/pi.2019.0226
Kirmayer, L. J. (2001). Cultural Variations in the Clinical Presentation of Depression and Anxiety: Implications for Diagnosis and Treatment. J. Clin. Psychiatry 62, 22–30.
Kleinman, A., and Kleinman, J. (1985). 13. Somatization: The Interconnections in Chinese Society Among Culture, Depressive Experiences, and the Meanings of Pain. Cult. Depress. Stud. Anthropol. cross-cultural Psychiatry affect Disord. 16, 429–490. doi:10.1525/9780520340923-018
Kocalevent, R.-D., Hinz, A., and Brähler, E. (2013). Standardization of the Depression Screener Patient Health Questionnaire (PHQ-9) in the General Population. Gen. Hosp. Psychiatry. 35, 551–555. doi:10.1016/j.genhosppsych.2013.04.006
Krause, J. S., Reed, K. S., and Mcardle, J. J. (2010). Factor Structure and Predictive Validity of Somatic and Nonsomatic Symptoms from the Patient Health Questionnaire-9: a Longitudinal Study after Spinal Cord Injury. Arch. Phys. Med. Rehabil. 91, 1218–1224. doi:10.1016/j.apmr.2010.04.015
Kroenke, K., Spitzer, R. L., Williams, J. B. W., and Löwe, B. (2010). The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a Systematic Review. Gen. Hosp. Psychiatry. 32, 345–359. doi:10.1016/j.genhosppsych.2010.03.006
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2001). The PHQ-9. J. Gen. Intern. Med. 16, 606–613. doi:10.1046/j.1525-1497.2001.016009606.x
Laban, C. J., Komproe, I. H., Gernaat, H. B. P. E., and De Jong, J. T. V. M. (2008). The Impact of a Long Asylum Procedure on Quality of Life, Disability and Physical Health in Iraqi Asylum Seekers in the Netherlands. Soc. Psychiat Epidemiol. 43, 507–515. doi:10.1007/s00127-008-0333-1
Leiler, A., Bjärtå, A., Ekdahl, J., and Wasteson, E. (2019). Mental Health and Quality of Life Among Asylum Seekers and Refugees Living in Refugee Housing Facilities in Sweden. Soc. Psychiatry Psychiatr. Epidemiol. 54, 543–551. doi:10.1007/s00127-018-1651-6
Lewis, S. E. (2018). Resilience, Agency, and Everydaylojongin the Tibetan Diaspora. Contemp. Buddhism 19, 342–361. doi:10.1080/14639947.2018.1480153
Lewis, S. E. (2013). Trauma and the Making of Flexible Minds in the Tibetan Exile Community. Ethos 41, 313–336. doi:10.1111/etho.12024
Li, Z., Wang, W., Xin, X., Song, X., and Zhang, D. (2018). Association of Total Zinc, Iron, Copper and Selenium Intakes with Depression in the US Adults. J. affective Disord. 228, 68–74. doi:10.1016/j.jad.2017.12.004
Liu, S.-I., Yeh, Z.-T., Huang, H.-C., Sun, F.-J., Tjung, J.-J., Hwang, L.-C., et al. (2011). Validation of Patient Health Questionnaire for Depression Screening Among Primary Care Patients in Taiwan. Compr. Psychiatry. 52, 96–101. doi:10.1016/j.comppsych.2010.04.013
Lotrakul, M., Sumrithe, S., and Saipanish, R. (2008). Reliability and Validity of the Thai Version of the PHQ-9. BMC psychiatry 8, 46. doi:10.1186/1471-244x-8-46
Madden, D. (2016). Do schooling Reforms Improve Long-Term Health. IZA World of Labor. doi:10.15185/izawol.306
Majidi, M., Khadembashi, N., Etemad, K., Jafari, M., and Khodakarim, S. (2018). Associated Factors with Major Depression: a Path Analysis on NHANES 2013–2014 Study. Int. J. Cult. Ment. Health 11, 763–773. doi:10.1080/17542863.2018.1563623
Meadows, K. (2021). Cognitive Interviewing Methodologies. Clin. Nurs. Res. 30, 375–379. doi:10.1177/10547738211014099
Mills, E. J., Singh, S., Holtz, T. H., Chase, R. M., Dolma, S., Santa-Barbara, J., et al. (2005). Prevalence of Mental Disorders and Torture Among Tibetan Refugees: A Systematic Review. BMC Int. Health Hum. Rights 5, 7. doi:10.1186/1472-698x-5-7
Ngasa, S. N., Sama, C.-B., Dzekem, B. S., Nforchu, K. N., Tindong, M., Aroke, D., et al. (2017). Prevalence and Factors Associated with Depression Among Medical Students in Cameroon: a Cross-Sectional Study. BMC psychiatry 17, 216. doi:10.1186/s12888-017-1382-3
Patil, K., Chande, D., Pratinidhi, S., and Bhat, A. (2018). A Study to Assess Depression Levels in MBBS Students. Indian J. Ment. Health 5, 296. doi:10.30877/ijmh.5.3.2018.296-300
Petersen, J. J., Paulitsch, M. A., Hartig, J., Mergenthal, K., Gerlach, F. M., and Gensichen, J. (2015). Factor Structure and Measurement Invariance of the Patient Health Questionnaire-9 for Female and Male Primary Care Patients with Major Depression in Germany. J. affective Disord. 170, 138–142. doi:10.1016/j.jad.2014.08.053
Poole, D. N., Hedt-Gauthier, B., Liao, S., Raymond, N. A., and Bärnighausen, T. (2018). Major Depressive Disorder Prevalence and Risk Factors Among Syrian Asylum Seekers in Greece. BMC public health 18, 908. doi:10.1186/s12889-018-5822-x
Rancans, E., Trapencieris, M., Ivanovs, R., and Vrublevska, J. (2018). Validity of the PHQ-9 and PHQ-2 to Screen for Depression in Nationwide Primary Care Population in Latvia. Ann. Gen. Psychiatry 17, 33. doi:10.1186/s12991-018-0203-5
Sachs, E., Rosenfeld, B., Lhewa, D., Rasmussen, A., and Keller, A. (2008). Entering Exile: Trauma, Mental Health, and Coping Among Tibetan Refugees Arriving in Dharamsala, India. J. Traum. Stress 21, 199–208. doi:10.1002/jts.20324
Salleh, M. R. (2018). The Burden of Mental Illness: An Emerging Global Disaster. Jchs 3, 5–12. doi:10.24191/jchs.v3i1.6150
Satinsky, E. N., Kimura, T., Kiang, M. V., Abebe, R., Cunningham, S., Lee, H., et al. (2021). Systematic Review and Meta-Analysis of Depression, Anxiety, and Suicidal Ideation Among Ph.D. Students. Sci. Rep. 11. doi:10.1038/s41598-021-93687-7
Servan-Schreiber, D., Lin, B. L., and Birmaher, B. (1998). Prevalence of Posttraumatic Stress Disorder and Major Depressive Disorder in Tibetan Refugee Children. J. Am. Acad. Child Adolesc. Psychiatry 37, 874–879. doi:10.1097/00004583-199808000-00018
Sobowale, K., Zhou, A. N., Fan, J., Liu, N., and Sherer, R. (2014). Depression and Suicidal Ideation in Medical Students in China: a Call for Wellness Curricula. Int. J. Med. Educ. 5, 31–36. doi:10.5116/ijme.52e3.a465
Sonam, T. (2019). “Incubating Western Science Education in Tibetan Buddhist Monasteries in India,” in Science Education in India (Singapore: Springer), 27–45.
Spitzer, R., Williams, J., and Kroenke, K. (2014). Test Review: Patient Health Questionnaire–9 (PHQ-9). Rehabil. Couns. Bull. 57, 246–248.
Tam, W., Lo, K., and Pacheco, J. (2019). Prevalence of Depressive Symptoms Among Medical Students: Overview of Systematic Reviews. Med. Educ. 53, 345–354. doi:10.1111/medu.13770
Verma, G., and Araya, R. (2010). The Effect of Meditation on Psychological Distress Among Buddhist Monks and Nuns. Int. J. Psychiatry Med. 40, 461–468. doi:10.2190/pm.40.4.h
Vos, T., Abajobir, A. A., Abate, K. H., Abbafati, C., Abbas, K. M., Abd-Allah, F., et al. (2017). Global, Regional, and National Incidence, Prevalence, and Years Lived with Disability for 328 Diseases and Injuries for 195 Countries, 1990-2016: a Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259. doi:10.1016/S0140-6736(17)32154-2
Wang, W., Bian, Q., Zhao, Y., Li, X., Wang, W., Du, J., et al. (2014). Reliability and Validity of the Chinese Version of the Patient Health Questionnaire (PHQ-9) in the General Population. Gen. Hosp. Psychiatry 36, 539–544. doi:10.1016/j.genhosppsych.2014.05.021
Wangmo, T., and Teaster, P. B. (2010). The Bridge from Then to Now: Tibetan Elders Living in Diaspora. J. Appl. Gerontol. 29, 434–454. doi:10.1177/0733464809341468
Willis, G. B. (2015). Analysis of the Cognitive Interview in Questionnaire Design. Oxford: Oxford University Press.
Yen, S., Robins, C. J., and Lin, N. (2000). A Cross-Cultural Comparison of Depressive Symptom Manifestation: China and the United States. J. consulting Clin. Psychol. 68, 993–999. doi:10.1037/0022-006x.68.6.993
Keywords: depression, patient health questionnaire-9, Tbetan, Buddhist, monastic, translation, cross-cultural psychiatry
Citation: Mascaro JS, Shellman D, Keaton WA, Willson M, Brauer E, Samphel T, Chang H, Raison CL, Zivot J and Eisen A (2021) Mixed-Method Evaluation of the Public Health Questionnaire for Estimating Depression Among Tibetan Buddhist Monastics. Front. Commun. 6:752820. doi: 10.3389/fcomm.2021.752820
Received: 03 August 2021; Accepted: 01 November 2021;
Published: 24 November 2021.
Edited by:
Robin Nusslock, Northwestern University, United StatesReviewed by:
Seth Davin Norrholm, Wayne State University, United StatesJames Glazer, University of Illinois at Chicago, United States
Copyright © 2021 Mascaro, Shellman, Keaton, Willson, Brauer, Samphel, Chang, Raison, Zivot and Eisen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer S. Mascaro, am1hc2NhckBlbW9yeS5lZHU=
 Jennifer S. Mascaro
Jennifer S. Mascaro Danielle Shellman1
Danielle Shellman1 Tsondue Samphel
Tsondue Samphel Hope Chang
Hope Chang Joel Zivot
Joel Zivot Arri Eisen
Arri Eisen