- 1Faculty of Health Sciences, UiT The Arctic University of Norway, Tromsø, Norway
- 2Institute of Clinical Medicine, University of Oslo, Oslo, Norway
- 3The Research Centre, Akershus University Hospital, Lørenskog, Norway
- 4Department of Neurology, Akershus University Hospital, Lørenskog, Norway
- 5Department of Medicine, Nordland Hospital Trust, Bodø, Norway
Effective communication is essential for understanding and recall of hospital discharge information. This study aimed to explore discharge information, patient recall and patient involvement in discharge encounters. We conducted an explorative observational study at a secondary care level, observational ward. Patients discharged to their home were asked to participate. 34 patients were assessed for eligibility, of which 13 were included in the analysis. Multiple sources of data were collected: videotapes of discharge encounters, questionnaires to patients and physicians, and semi-structured interviews with patients 2 weeks after discharge. All patients were satisfied with the information received. Five of the eight patients discharged with more than one change in medication had only partial or no recall of these changes. In seven of the 13 encounters the patients and physicians did not agree on the main message most important information item. The patients were to a small extent involved in decision-making. Our findings highlight the gaps in the information exchange at discharge encounters and the resulting poor information recall among patients. Patients do not seem aware of these gaps. Greater provider awareness of patient involvement in the encounter and inclusion of the patient’s perspective may improve communication, and consequently understanding and recall.
Introduction
Hospital discharge encounters are a crucial point of information exchange between patients and healthcare providers. The transition of care and responsibility from the healthcare system to the individual patient can be difficult and make patients feel vulnerable. Failure in this process, such as insufficient discharge information, misunderstanding or lack of information uptake due to individual limitations, can lead to deterioration of health conditions and unnecessary readmissions (Services NMoHaC, 2009; DeLia et al., 2014; Lorentzen et al., 2020). This process depends on how well the patient has been educated at the hospital, and not only that they have received information or that they are satisfied with the information (Horwitz et al., 2013). Involving the patients can improve patient satisfaction and patient-physician communication (Roodbeen et al., 2020; Luo et al., 2021). Shared decision-making (SDM) is one method to involve the patient in decisions. A systematic review on the use of SDM concluded that the method can improve patient knowledge and satisfaction, in addition to engagement in decision-making (Flynn et al., 2012).
The Norwegian Institute of Public Health annually performs user surveys of patients’ experiences of the Norwegian healthcare. The three latest national reports of inpatient experiences with Norwegian hospitals found that approximately 30% of those surveyed expressed that they had received little or no information to prepare them for period after discharge (Bjerkan et al., 2014; Holmboe and Bjertnæs, 2015; Holmboe and Bjertnæs, 2016). The surveys found that approximately 10% of the patients had low or no understanding of having the responsibility for their own health, and 14% had some or limited understanding of their own medical treatment.
Discharge instructions are a critical part of patient care. How the information is communicated, is as important as the content of the information (Asnani, 2009). Several studies have assessed different aspects of discharge information. A research group in Basel have carried out several studies, where they have focused on content, structuring and use of time (Ackermann et al., 2012; Langewitz et al., 2015; Ackermann et al., 2016; Ackermann et al., 2017). They have concluded that the amount of information should be limited, and the information should be structured. Structured information improves recall, especially among patients with low levels of medical knowledge. The same group of researchers also found that physicians often overestimate patients’ recall capacity. Furthermore, it has been shown that there is a negative correlation between the amount of information and recall, and a positive correlation between health literacy and recall (Anderson et al., 1979; McCarthy et al., 2012).
Recall may be affected by misunderstandings of the information given. A study found that less than half of hospitalized patients remembered their diagnosis and treatment plan at discharge (Makaryus and Friedman, 2005). Engel et al. (2009) assessed the understanding of discharge information in the emergency department, and found that four out of five patients had incomplete understanding of the information given. This lack of comprehension can affect both satisfaction and compliance. Furthermore, most patients with recall deficits are not aware of it. Two studies have found that almost half of the information remembered by patients was incorrect (Anderson et al., 1979; Engel et al., 2009). Overall, research shows huge variations in the ability to recall; a systematic review of 51 articles found a variation of 8–94% of recall in verbal information and 23–92% in recall of written information (Hoek et al., 2020).
The degree of recall depends on the amount of information provided and the length of the recall period (Kjellsson et al., 2014). A systematic review concluded that there is no single optimal recall period (Stull et al., 2009). A study on the role of length of recall periods in recall different recall periods ranging from 1 month to a year found that the overall recall decreased with the length of the recall period (Kjellsson et al., 2014). Even though the results showed that the overall recall decreased with the length of the recall period, they concluded that the recall period should be adjusted to individual factors and study objective.
To our knowledge, no study has included both video of actual encounters and subsequent interviews of participants in order to identify 1) information communicated, and 2) strategies utilized to include patient perspectives during discharge encounters. The purpose of this study was to describe the following three aspects of information at discharge: contents, quality (in terms of patient involvement) and physicians’ and patients’ priorities about the information. In addition to explore links with patient recall and perceived information process. information process.
More precisely, the study aimed to answer the following four research questions:
• What information do patients receive in discharge encounters, and how do they assess the information they received?
• When asked 2 weeks after discharge, what do patients remember of the discharge information?
• When asked directly after the discharge encounter, what is the most important discharge information item according to the patient and the physician, respectively, and do physicians and patients agree on this item?
• How and to what degree are the patients’ perspectives included in the encounter?
Materials and Methods
Study Design
We conducted an explorative observational study with multiple sources of data of patients discharged to their home from the observational ward. The study was presented to the Regional Ethical Committee for Research Ethics and was deemed to be outside requirements of the Norwegian Health Research Law (decision 2019/735). The study was presented to and approved by the Data Protection Officer at the study hospital (Nordland Hospital Trust, Bodø). All participants received oral and written information about the study, and written consent was obtained before enrollment.
Study Setting and Selection of Participants
Nordland Hospital Trust is the second largest hospital in Northern Norway. In the first inclusion period, 2 weeks in August 2019, patients older than 18 years who were to be discharged from the observation ward to their home, were invited to participate in the study. Patients were excluded if they were unwilling to participate, did not speak Norwegian, had a psychiatric diagnosis or cognitive deficit (information obtained from the physician), or if they were influenced by alcohol or other drugs at discharge. If the patient’s physician did not want to participate, the patient was not included in the study.
After the first period of data collection, we conducted preliminary analyses and based on preliminary results, we added a second inclusion period in September/October 2019. The principle of “information power” guided the recruitment and sample size evaluations (saturation of data is usually reached with 10–20 individual interviews, and multiple data increase information power and reduce the number of participants needed) (Malterud et al., 2016). Recruitment of patients endured until the structure of relevant themes became repetitive among the informants and no new themes surfaced. Lastly, participants who had been readmitted in the period from discharge until the follow-up interview were excluded, as their follow-up interview might be biased from information given during the later admission(s).
Procedure and Data Collection
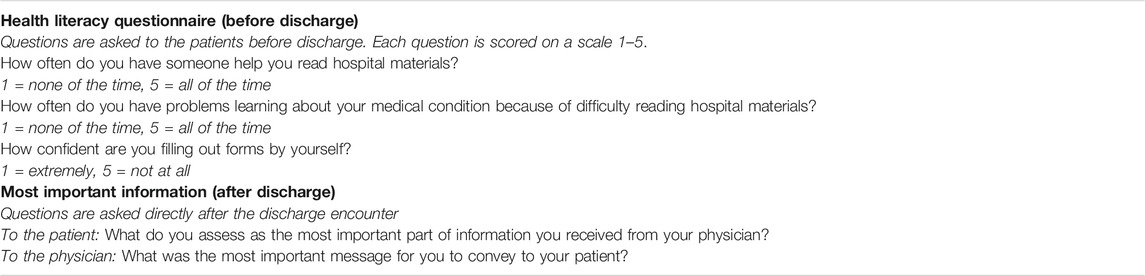
The discharge encounters were conducted and videotaped in a suitable room in or adjacent to the observation ward. One researcher (K.Ø) was in the room during the encounter to do the videotaping. Patients’ health literacy was assessed before or after the discharge encounter by using a short self-report questionnaire from Chew et al. (2008) and translated to Norwegian by the first author (K.Ø.) (see Table 1). Back-translation was performed (by E. O). The minor discrepancies between the original and back-translated version of the questionnaire were deemed acceptable and not requiring revisions; major changes were discussed among the two authors until a satisfactory wording of labels was reached.
Immediately after the encounter, the patient and the physician were separately asked to identify the most important information item in the encounters (see Table 1). In addition, 2 weeks after discharge the patients participated in a semi-structured interview via telephone, following an interview track addressing three components: free, unprompted recall of discharge information, understanding and satisfaction. Minor modifications and improvements to the track were made after the first few interviews. The interviews were all conducted by the same interviewer (K.Ø.), and they were recorded using a digital audio recorder.
Data Analysis
The goal of our analysis was to combine multiple sources of data to better understand the complex process of information exchange in discharge encounters and how it affects satisfaction, recall, degree of agreement between patient and physician and level of patient involvement. Our qualitative analysis is therefore explorative, with the aim of identifying important themes relevant to the entire material. Our quantitative analysis is, because of the number of participants also, explorative and does not aim to describe frequencies of, and associations between the identified themes, at a population level. The results merely describe patterns of variations and similarities in a small sample material.
The videotapes of the discharge encounters and the audiotapes of the interviews were transcribed verbatim. First, the videotapes were inductively analyzed to identify and categorize information items, defined as specific pieces of information exchanged during the encounter, and to categorize physicians’ and patients’ responses to the most important information item discussed at the encounter. Transcripts of videotapes of discharge encounters and of physicians and patients interviews afterwards were thus used as a single corpus to analyze “information items” and derive categories, with videotapes and interviews complementing and informing each other. Pieces of information were grouped and condensed into categories perceived as salient. First, codes and categories were derived by K.Ø. discussed with E.O. refined and cross-checked with data, and final categories agreed upon through consensus. Furthermore, for each encounter the responses from the physician and patient grouped in the “information items” categories, were compared and concordance was assessed.
The resulting “information items” categories were also used to organize and interpret the patients’ recall answers in the interviews. Patient recall was rated on a 3-point scale, based on the proportion of information items provided and recalled by each patient: no recall (not recalled at all or wrong), partial recall (including all from a little to a lot) and complete recall. The category partial recall was not further divided into subgroups e.g. little-mediocre-a lot, because of the low frequency of “information items” pertaining to the partial recall category. A detailed thematic analysis (Braun and Clarke, 2006) of each videotape was done with continuous discussion of themes and interpretations by two researchers (K.Ø. and E.O) to explore aspects concerning patient involvement in the encounter and in decision-making. The presence of recall-promoting techniques (i.e. physicians’ encouragement to ask questions during the encounter) was the main focus of the analysis.
Additional aspects considered in the analysis to interpret emerging findings, were the duration of the encounter, the number of information items discussed, and the use of written information.
Results
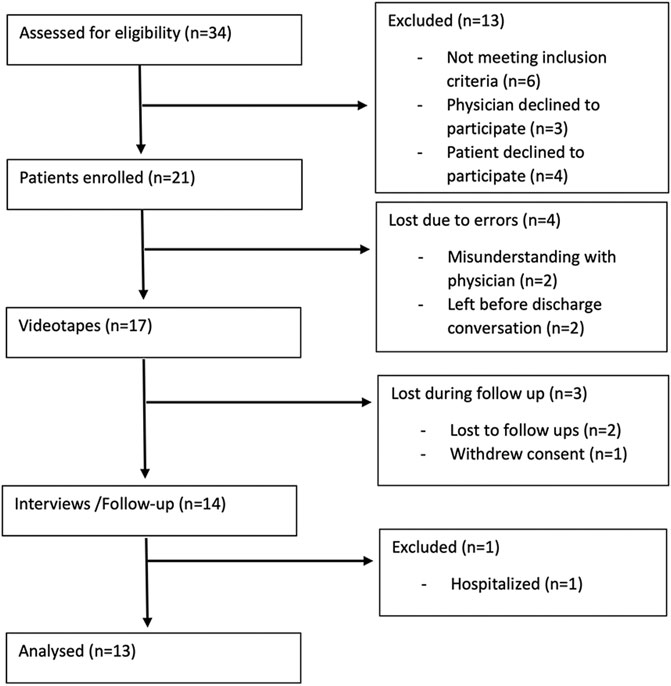
During the study period, a total of 34 patients were assessed for eligibility and a final sample of 13 patients was included in the analysis. Seven patients and physicians declined to participate, four patients were lost due to misunderstandings (the discharge encounters were not videotaped) and three were lost in follow up (they were unreachable by phone on several attempts). Figure 1 summarizes the recruitment and enrolment process.
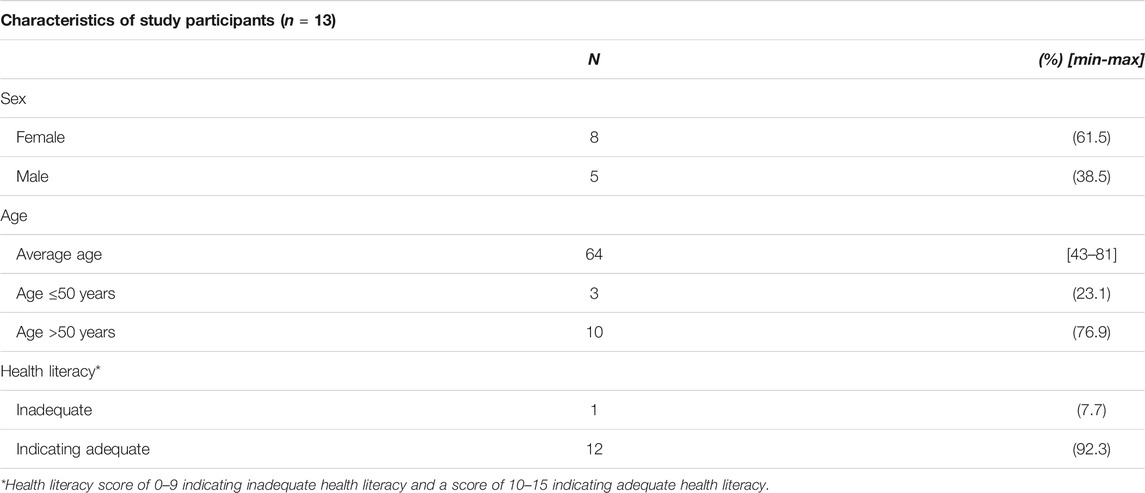
Demographic and health literacy information for the final group of patients is provided in Table 2. The median age of the 13 patients was 64 years and 61.5% were female. One patient had a score of ≤9 on the health literacy screening, indicating inadequate health literacy. Atrial fibrillation (n = 5), chest pain (n = 2), severe hypertension, vertigo, syncope, dyspnea, hyperglycemia, and skin infection (n = 1, respectively) were the different health issues presented at hospitalization. In none of the 13 encounters did the patient have a caregiver or family member present.
Information provided, Recalled, and Perceived
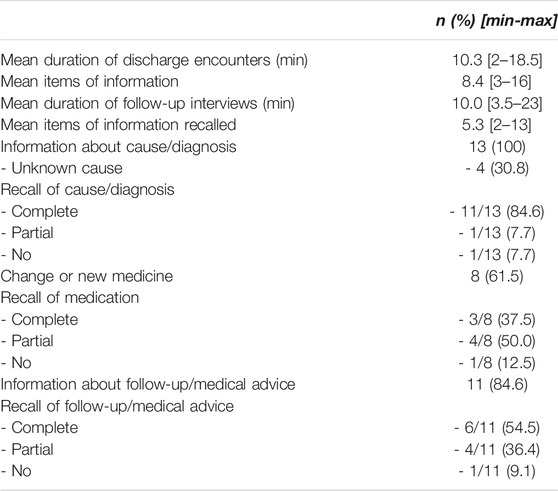
The encounters lasted from 2 to 18.5 min, with a mean of 10.3 min. Patients received a mean of 8.4 items of information during this discharge time. The information provided where relatively the same in amount and type of information. Four patients had a known medical condition with prior hospitalizations, and two of these received brief and limited information at their own request. In all the encounters, the information provided orally was complemented with written discharge instructions; in eight encounters the written papers were actively used during the discharge encounter (six physicians reviewed the paper with the patients and two asked the patient to read the paper and ask questions if there were any). None of the patients wrote down any information during the encounters.
Three main categories emerged from the analysis of “information items”: 1) cause/diagnosis, containing information about the disease and the diagnosis - or, if the cause was unknown, about the symptoms and the diagnosis - and main conclusion of the medical investigation, 2) medication, with information about a change in the existing medication plan or about a new prescription, including details about the type, dosage, use and indications for the changed/new medication, and 3) follow-up/medical advice, about information on further medical investigations, follow up, or special considerations/limitations and advices on e.g. lifestyle changes, physical activity, symptoms that require to contact the physician.
All patients received information about the medical conclusion of the hospitalization. Four of the 13 patients were discharged without a known cause of their symptoms. They were admitted with symptoms or signs of hypertension, dyspnea, chest pain and dizziness, respectively, and the physician addressed the lack of a concrete diagnosis and the exclusion of serious causes in all these encounters. Eight patients had a change in medication or got prescribed a new medicine during their stay at the hospital. Information about follow-up/medical advice was the most commonly provided content at discharge, featuring 11 of 13 encounters.
The duration of follow-up interviews 2 weeks after discharge were 3.5–23 min, with a mean of 10 min. Overall, the average of the recalled (partial or complete) information items at the 2 weeks follow up was 5.3. Eleven of the 13 patients had complete recall of information about the cause of their symptoms. Of the eight patients having had a change in medications, five had partial or no recall of the details concerning the new medication. Finally, five of 11 patients had partial or lack of recall of the information provided about follow-up/medical advice. Table 3 summarizes the results of the information provided and recalled.
When patients were asked to express their perception and satisfaction (i.e. comprehensibility, understanding, and unmet needs) about the information they received, all thought the information was comprehensible, all felt they had good understanding of what the physician said, and none felt a need for further information from the physician.
Physicians’ and Patients’ Information Priorities, and Concordance With Patient Recall
As shown in Figure 2, most of the physicians stated that the information about follow-up/medical advice was the most important information they provided. The minority of patients stated this category as the most important.
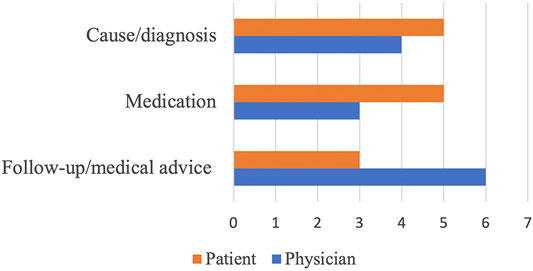
FIGURE 2. Patients’ and physicians’ responses of most important information items, divided in categories.
Figure 3 illustrates the accordance in responses of most important information item, and concordance between patient’s response and patient recall of this information. In six of the 13 encounters, the patient and the physician agreed on the same information category as the main message (marked with an arrow). Among the seven cases of discordance, five had the physician thinking that the information on follow-up/medical advice was the main message while patients’ responses were divided among the two other categories Patient recall of this information is illustrated with a traffic light after the degree of recall.
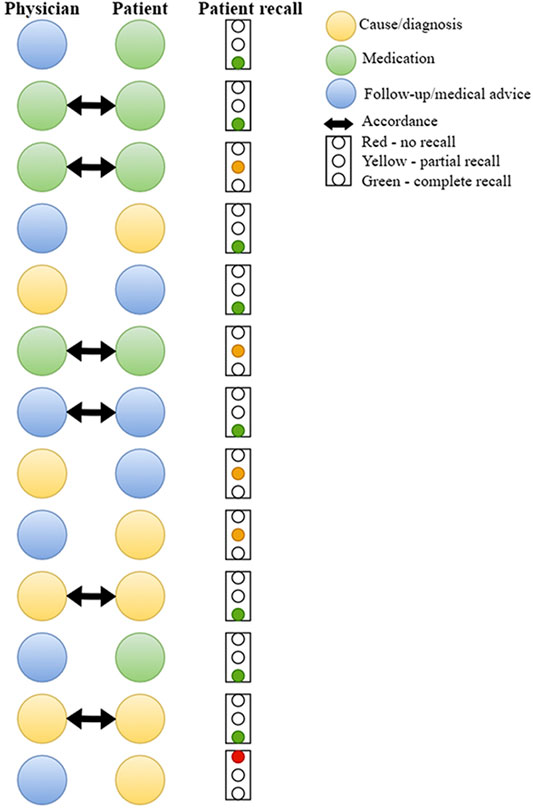
FIGURE 3. Accordance in responses of most important information item, and concordance between patient’s response and patient recall of this information. Note: accordance in responses is marked with an arrow. Degree of patient recall of their response of most important
Patient Involvement During Discharge
When looking at what happened in the information exchange and decision-making process during the discharge encounters, it was possible to observe that, in general, the patients only to a small extent were involved in the decision-making. Three main themes of actions that the physician took during the encounters to involve patients in the decision making emerged from the analysis: 1) encouraging to ask questions, 2) exploring thoughts and opinions and 3) discussing decisions.
“Encouraging to ask questions” was the most frequently observed behavior by physicians to involve patients. With only one exception, all patients were directly encouraged by the physician to ask questions during the encounter. However, only five patients actually asked questions during the discharge encounter. At the follow-up interviews, a few patients emphasized that they did it when something was unclear:
“I think I got good communication with the doctor. It was a two-way communication. As mentioned, the doctor asked if there was anything I wanted to ask about. If there was something I did not understand, I just had to say it” (Female, 31 years-old, skin infection).
Rarely patients were encouraged to share their thoughts and opinions. In three encounters the physicians asked for the patients’ thoughts about starting a new medication, follow-up and about the patients’ perspective for the cause of his symptoms, respectively. None of the patients were asked to repeat the information provided (“teach back”).
Lastly, “Discussing decisions” was an observed action among some of the physicians to involve patients. Different degrees of implementation of this action were observed in the encounters. In most of the encounters, a further plan was already settled by the physician before the discharge encounter; in three encounters the decision was the result of a discussion with the patient. One physician let the patient decide whether to start taking an oral anticoagulant or not: the physician provided information about the reason for starting the medication and related risks and benefits, explained that there was no clear right or wrong decision, and asked the patient to decide themselves. Two other encounters were similar, but the physicians did not ask for the patient’s preference concerning the medication.
Links Between Information in Discharge Encounters and Patient Recall
When exploring possible links between patient recall of information 2 weeks after discharge and what happened and was perceived at discharge, several chains were observed that can explain recall findings in this group of patients. Links are organized based on the no, partial and complete recall scores.
All the patients with complete recall of medications had only one change in medication. Five patients asked questions concerning follow-up/medical advice; four of them had complete recall of information of this category after 2 weeks. Eight patients had complete recall of the category of information they considered the most important at discharge. Of the six cases of accordance between patients’ and physicians’ responses, four patients had complete recall. Two of the patients who were discharged with an unknown cause of their problems stated that information about exclusion of serious causes of their symptoms was the most important for them, and they had both complete recall of it. In the one case of shared decision-making, the patient had complete recall of the medications.
Half of the patients with partial recall of medication dialog had two or three changes in their medications. Four had partial recall of the category of information considered the most important at discharge, and in two of these cases there were accordance between patients’ and physicians’ responses.
The one patient with no recall of information about medications had two changes in medications. In the one case of no recall of diagnosis/cause, the patient had a score indicating inadequate health literacy and the written paper was not used during the discharge encounter. One patient did not recall the information that 2 weeks earlier considered as the most important. There was no difference in recall or satisfaction between those who reviewed in any degree the written paper with the physician during the encounter and those who did not.
Discussion
This study showed that despite high levels of patient satisfaction with communication at discharge, many patients were not able to recall the discharge information in full. The information most patients had problems remembering was information about medication. These findings are in accordance with several other studies (Grover et al., 1994; Engel et al., 2009; McCarthy et al., 2012), e.g. Engel et al. (2009) found that one in three patients had problems comprehending instructions about treatment. Possible explanations mentioned in literature include level of health literacy, focus, concentration, age, motivation and amount of information received (McCarthy et al., 2012; Bol et al., 2018; Laws et al., 2018). Our finding that high levels of satisfaction is not synonymous with high levels of recall also confirms previous literature. Pavlik et al. (2014) reported high patient satisfaction with the information received and low recall of the same information among 272 primary care patients.
Another finding in this study was that physicians and patients often do not share the same opinion about the main message of the discharge encounter. This may be due to inadequate communication and insufficient focus on the patient’s perspective. A study of treatment goals of patients with multiple sclerosis and healthcare providers also had results indicating that patients and health care providers had different focus areas (Col et al., 2018). If patients are not encouraged to share their point of view, physicians may focus on the information they believe is the most relevant. Physicians should involve the patient in order to better understand the patient’s goals, concerns and needs for information, and thereby achieve more efficient communication and a stronger patient-physician relationship. The accordance between patients’ and physicians’ perspective can be seen as an indicator of physicians fine tuning their priorities based on what patients bring in the encounter (and the other way around), which in turn might increase involvement and recall (Watson and McKinstry, 2009; Richard et al., 2017).
In this study, we found that patient involvement is usually encouraged by physicians by asking patients if they have any questions. However, not many patients were actually involved in the encounter by asking questions. It is demonstrated that one effective way to increase patient involvement in decision-making is asking patients not only for their doubts, but for their opinion, ideas and goals (Stiggelbout et al., 2015). Even though some patients may not be used to or feel comfortable with expressing a medical opinion and be involved in medical decisions (Say et al., 2006), it is important that physicians arrange for this to be possible and include questions about patients’ opinions, values and goals in their encounters. Furthermore, we found that in a minority of cases, the decision was actually discussed with the patient and not made by the physician beforehand. This may indicate, on one hand, that the pinnacle of shared decision-making (SDM) can be unpractical in some situations, e.g. where there is a clear road to take, or, on the other hand, that discharge consultations are not easily suited for a full SDM process e.g. because of time constraints. The term SDM is used when the patient and/or family, and the physician cooperate to develop successful therapeutic plans (Beckman et al., 2019). In discharge consultations, even if physicians have already made a decision on a preferred treatment option, identifying the patient’s goals can give a common understanding and grounding of how to proceed, as a starting point of an SDM-like process. Focusing on the patient can increase satisfaction, patient engagement and autonomy, and compliance (Laws et al., 2018). In addition, focus on patients’ perspectives may reveal different views of explanations and misunderstandings, and thereby create a golden opportunity to clarify them. “Teach back” is a strategy to both enhance patient involvement and confirm patient understanding (Yen and Leasure, 2019; Talevski et al., 2020) by asking the patients to repeat the information provided. Thereby creating an opportunity for clarification and prevent bigger chains of misunderstandings. The method has showed to be effective on comprehension and recall, both immediate and short-term, of discharge instructions (Mandhkani et al., 2020).
Finally, written information was frequently used in the discharge encounters. When examining the videotapes, those encounters using the written information seemed easier to follow as it gave more structure. However, the use of written information did not affect patient recall or patient satisfaction of the information and communication. A systematic review and meta-analysis of recall and manners of providing discharge information concluded that using written information in addition to verbal recall improves satisfaction and recall of instructions (Hoek et al., 2020).
In order to increase recall, the physician should, early in the discharge encounter, be curious about the patient’s ideas and concerns. She/he should also explore or be attentive to signs revealing what information the patients would like to receive, and how. In this way information to a larger extent can be tailor-made to the unique patient and a more active role of patients in the information exchange and decision-making can be enabled. Patients may not be aware of the information and communication holes, so attention from researchers, analysts, and clinicians should be paid on what happens in the dialogue rather than on patients’ satisfaction evaluations afterwards.
This study has a number of limitations. First, the small sample of 13 patients does not allow strong conclusions to be driven by findings. Results should be interpreted as explorative indications. The small sample was due to challenges and practicalities in recruitment. Of 34 eligible patients in the study period, only 13 were finally included. Clearer messages and more information about the study may have improved this, which stress the importance of good communication. However, given the explorative nature of the study and the multiple sources of data collected, we think the findings add knowledge to the field. The small sample was skewed towards high health literacy, not providing heterogeneity among participants that could have yielded a larger range of recall responses. At the same time, homogeneity in health literacy scores of participants allowed removing this variable as confounder in interpreting findings on recall: recall was low, even if patients were highly health literate. Furthermore, having the discharge encounter videotaped and having an observer in the same room, may have influenced the discharge encounter in several ways. Both patients and physicians may have modified their behavior in response to their awareness of being observed, a phenomenon known as the Hawthorne effect (McCambridge et al., 2014). The impact of this effect is however limited and unclear (McCambridge et al., 2014).
A final limitation may concern the assessment of recall. We used a common way to assess it, by asking patients to freely recall their overall memories of the information received at discharge (free recall). The way patients are asked to recall can influence their actual recall, e.g. with no (free recall), little (cued recall), or full prompting (recognition). The use of free recall may have provided a more accurate information, though more difficult for the patients to recollect. Indeed, free recall can be different from actual memory: patients with deficient recall may have followed the instructions precisely, but recalled them incorrectly in retrospect.
Conclusion
This study showed that about half of the patients had problems recalling instructions about medication and follow-up/medical advice, and in half of the encounters the patients and physicians did not share the same perspective on the main message of the encounter. However, the patients themselves considered the information understandable, reported no need for further information and they were satisfied with the communication. Even though all patients received written information, only about half of them reviewed it with the physician.
Practice Implications
Physicians can communicate information, but if the patients do not understand it, it is of no use. Therefore, physicians must be aware of the importance of effective communication in discharge encounters. Greater provider awareness of patient involvement in the encounter and including the patient’s perspective may improve communication. Increased focus on simple communication strategies may improve recall and understanding for patients.
Data Availability Statement
The datasets presented in this article are not readily available because by agreement with the participant all videos and audios will be deleted in 2022. In addition, all videos, audios, and transcriptions are in Norwegian. Requests to access the datasets should be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the study was presented to the Regional Ethical Committee for Research Ethics and was deemed to be outside requirements of the Norwegian Health Research Law (decision 2019/735). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed to conceptualization of this study. KØ, JN and EO contributed to methodology. KØ were responsible for data collection, formal analysis, investigation and writing of original draft. All authors contributed to writing with review and editing.
Funding
Financial support for the author KØ was provided by a summer scholarship from the Norwegian Medical Students’ Association. Grant number N/A. The publication charges for this article have been funded by a grant from the publication fund of UiT The Arctic University of Norway. Grant number N/A.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to thank the Oslo Communication in Health Care Education and Research (OCHER) network useful feedback in the planning phase of the study, which was accepted for preliminary discussion at the OCHER workshop 2019.
References
Ackermann, S., Bingisser, M. B., Heierle, A., Langewitz, W., Hertwig, R., and Bingisser, R. (2012). Discharge Communication in the Emergency Department: Physicians Underestimate the Time Needed. Swiss Med. Wkly 142, w13588. doi:10.4414/smw.2012.13588
Ackermann, S., Ghanim, L., Heierle, A., Hertwig, R., Langewitz, W., Mata, R., et al. (2017). Information Structuring Improves Recall of Emergency Discharge Information: a Randomized Clinical Trial. Psychol. Health Med. 22 (6), 646–662. doi:10.1080/13548506.2016.1198816
Ackermann, S., Heierle, A., Bingisser, M.-B., Hertwig, R., Padiyath, R., Nickel, C. H., et al. (2016). Discharge Communication in Patients Presenting to the Emergency Department with Chest Pain: Defining the Ideal Content. Health Commun. 31 (5), 557–565. doi:10.1080/10410236.2014.979115
Anderson, J. L., Dodman, S., Kopelman, M., and Fleming, A. (1979). Patient Information Recall in a Rheumatology Clinic. Rheumatology 18 (1), 18–22. doi:10.1093/rheumatology/18.1.18
Asnani, M. R. (2009). Patient-physician Communication. West. Indian Med. J. 58 (4), 357–361. doi:10.1001/archinternmed.2008.586
Beckman, A., Wendl, M., Cohen, E. S., Bartock, B., and Beckman, J. C. H. (2019). Soliciting Patients Goals for Care on Hospital Discharge the Gateway to Shared Decision-Making. Qual. Prim. Care 27, 1–8.
Bjerkan, A., Holmboe, O., and Skudal, K. (2014). Inpatients’ Experiences with Norwegian Hospitals: National Results in 2013Report No. Oslo: National Knowledge Centre for Health, 2–2014.
Bol, N., Smets, E. M. A., Burgers, J. A., Samii, S. M., De Haes, H. C. J. M., and Van Weert, J. C. M. (2018). Older Patients' Recall of Online Cancer Information: Do Ability and Motivation Matter More Than Chronological Age? J. Health Commun. 23 (1), 9–19. doi:10.1080/10810730.2017.1394400
Braun, V., and Clarke, V. (2006). Using Thematic Analysis in Psychology. Qual. Res. Psychol. 3 (2), 77–101. doi:10.1191/1478088706qp063oa
Chew, L. D., Griffin, J. M., Partin, M. R., Noorbaloochi, S., Grill, J. P., Snyder, A., et al. (2008). Validation of Screening Questions for Limited Health Literacy in a Large VA Outpatient Population. J. Gen. Intern. Med. 23 (5), 561–566. doi:10.1007/s11606-008-0520-5
Col, N. F., Solomon, A. J., Springmann, V., Garbin, C. P., Ionete, C., Pbert, L., et al. (2018). Whose Preferences Matter? A Patient-Centered Approach for Eliciting Treatment Goals. Med. Decis. Making 38 (1), 44–55. doi:10.1177/0272989x17724434
DeLia, D., Tong, J., Gaboda, D., and Casalino, L. P. (2014). Post-discharge Follow-Up Visits and Hospital Utilization by Medicare Patients, 2007-2010. Medicare Medicaid Res. Rev., 4. doi:10.5600/mmrr.004.02.a01
Engel, K. G., Heisler, M., Smith, D. M., Robinson, C. H., Forman, J. H., and Ubel, P. A. (2009). Patient Comprehension of Emergency Department Care and Instructions: Are Patients Aware of when They Do Not Understand? Ann. Emerg. Med. 53 (4), 454–461. doi:10.1016/j.annemergmed.2008.05.016
Flynn, D., Knoedler, M. A., Hess, E. P., Murad, M. H., Erwin, P. J., Montori, V. M., et al. (2012). Engaging Patients in Health Care Decisions in the Emergency Department through Shared Decision-Making: A Systematic Review. Acad. Emerg. Med. 19 (8), 959–967. doi:10.1111/j.1553-2712.2012.01414.x
Grover, G., Berkowitz, C. D., and Lewis, R. J. (1994). Parental Recall after a Visit to the Emergency Department. Clin. Pediatr. (Phila) 33 (4), 194–201. doi:10.1177/000992289403300401
Hoek, A. E., Anker, S. C. P., van Beeck, E. F., Burdorf, A., Rood, P. P. M., and Haagsma, J. A. (2020). Patient Discharge Instructions in the Emergency Department and Their Effects on Comprehension and Recall of Discharge Instructions: A Systematic Review and Meta-Analysis. Ann. Emerg. Med. 75 (3), 435–444. doi:10.1016/j.annemergmed.2019.06.008
Holmboe, O., and Bjertnæs, O. (2015). Inpatients’ Experiences with Somatic Hospitals in 2014: National Results Oslo: National Knowledge Centre for Health. Report No, 2–2015.
Holmboe, O., and Bjertnæs, O. (2016). Inpatients’ Experiences with Somatic Hospitals in 2015: National Results. Oslo: Norwegian Institute of Public Health. Report No.: 147.
Horwitz, L. I., Moriarty, J. P., Chen, C., Fogerty, R. L., Brewster, U. C., Kanade, S., et al. (2013). Quality of Discharge Practices and Patient Understanding at an Academic Medical Center. JAMA Intern. Med. 173 (18), 1715–1722. doi:10.1001/jamainternmed.2013.9318
Kjellsson, G., Clarke, P., and Gerdtham, U.-G. (2014). Forgetting to Remember or Remembering to Forget: A Study of the Recall Period Length in Health Care Survey Questions. J. Health Econ. 35 (Feb 7), 34–46. doi:10.1016/j.jhealeco.2014.01.007
Langewitz, W., Ackermann, S., Heierle, A., Hertwig, R., Ghanim, L., and Bingisser, R. (2015). Improving Patient Recall of Information: Harnessing the Power of Structure. Patient Edu. Couns. 98 (6), 716–721. doi:10.1016/j.pec.2015.02.003
Laws, M. B., Lee, Y., Taubin, T., Rogers, W. H., and Wilson, I. B. (2018). Factors Associated with Patient Recall of Key Information in Ambulatory Specialty Care Visits: Results of an Innovative Methodology. PLoS One 13 (2), e0191940. doi:10.1371/journal.pone.0191940
Lorentzen, I. C., Larsby, K. E., Bugge, E., and Lindekleiv, H. (2020). Readmissions to a Cardiology Department. Tidsskr Nor Laegeforen 140 (1), 41–45. doi:10.4045/tidsskr.19.0225
Luo, H., Liu, G., Lu, J., and Xue, D. (2021). Association of Shared Decision Making with Inpatient Satisfaction: a Cross-Sectional Study. BMC Med. Inform. Decis. Mak. 21 (1), 25. doi:10.1186/s12911-021-01385-1
Makaryus, A. N., and Friedman, E. A. (2005). Patients' Understanding of Their Treatment Plans and Diagnosis at Discharge. Mayo Clinic Proc. 80 (8), 991–994. doi:10.4065/80.8.991
Malterud, K., Siersma, V. D., and Guassora, A. D. (2016). Sample Size in Qualitative Interview Studies. Qual. Health Res. 26 (13), 1753–1760. doi:10.1177/1049732315617444
Mandhkani, M., Janine Alida, H., Jeroen Joseph Antonius, Z., Margreet, K., Mathilde, F., and Daphne Annika van, R. (2020). The Impact of Teach-Back on Patient Recall and Understanding of Discharge Information in the Emergency Department: the Emergency Teach-Back (EM-TeBa) Study. Int. J. Emerg. Med. 13 (1), 1–8. doi:10.1186/s12245-020-00306-9
McCambridge, J., Witton, J., and Elbourne, D. R. (2014). Systematic Review of the Hawthorne Effect: New Concepts Are Needed to Study Research Participation Effects. J. Clin. Epidemiol. 67 (3), 267–277. doi:10.1016/j.jclinepi.2013.08.015
McCarthy, D. M., Waite, K. R., Curtis, L. M., Engel, K. G., Baker, D. W., and Wolf, M. S. (2012). What Did the Doctor Say? Health Literacy and Recall of Medical Instructions. Med. Care 50 (4), 277–282. doi:10.1097/mlr.0b013e318241e8e1
Pavlik, V., Brown, A. E., Nash, S., and Gossey, J. T. (2014). Association of Patient Recall, Satisfaction, and Adherence to Content of an Electronic Health Record (EHR)-Generated after Visit Summary: A Randomized Clinical Trial. J. Am. Board Fam. Med. 27 (2), 209–218. doi:10.3122/jabfm.2014.02.130137
Richard, C., Glaser, E., and Lussier, M.-T. (2017). Communication and Patient Participation Influencing Patient Recall of Treatment Discussions. Health Expect. 20 (4), 760–770. doi:10.1111/hex.12515
Roodbeen, R., Vreke, A., Boland, G., Rademakers, J., van den Muijsenbergh, M., Noordman, J., et al. (2020). Communication and Shared Decision-Making with Patients with Limited Health Literacy; Helpful Strategies, Barriers and Suggestions for Improvement Reported by Hospital-Based Palliative Care Providers. PloS one 15 (6), e0234926–e. doi:10.1371/journal.pone.0234926
Say, R., Murtagh, M., and Thomson, R. (2006). Patients' Preference for Involvement in Medical Decision Making: a Narrative Review. Patient Edu. Couns. 60 (2), 102–114. doi:10.1016/j.pec.2005.02.003
Services NMoHaC (2009). The Coordination Reform, Proper Treatment – at the Right Place and Right Time. Oslo: Norwegian Ministry of Health and Care Services. Report No.: 47.
Stiggelbout, A. M., Pieterse, A. H., and De Haes, J. C. J. M. (2015). Shared Decision Making: Concepts, Evidence, and Practice. Patient Edu. Couns. 98 (10), 1172–1179. doi:10.1016/j.pec.2015.06.022
Stull, D. E., Leidy, N. K., Parasuraman, B., and Chassany, O. (2009). Optimal Recall Periods for Patient-Reported Outcomes: Challenges and Potential Solutions. Curr. Med. Res. Opin. 25 (4), 929–942. doi:10.1185/03007990902774765
Talevski, J., Wong Shee, A., Rasmussen, B., Kemp, G., and Beauchamp, A. (2020). Teach-back: A Systematic Review of Implementation and Impacts. PLoS One 15 (4), e0231350. doi:10.1371/journal.pone.0231350
Watson, P. W., and McKinstry, B. (2009). A Systematic Review of Interventions to Improve Recall of Medical Advice in Healthcare Consultations. J. R. Soc. Med. 102 (6), 235–243. doi:10.1258/jrsm.2009.090013
Keywords: patient recall, patient perspective, shared decision-making, information exchange, discharge communication
Citation: Østen K, Menichetti J, Nordfalk JM and Ofstad EH (2021) Recall and Understanding of Discharge Information in Observation Ward Patients: An Explorative Observational Study. Front. Commun. 6:736095. doi: 10.3389/fcomm.2021.736095
Received: 04 July 2021; Accepted: 19 August 2021;
Published: 07 September 2021.
Edited by:
Victoria Team, Monash University, AustraliaReviewed by:
Jennifer K. Ptacek, University of Dayton, United StatesJodie Marcantoni, Simmons University, United States
Copyright © 2021 Østen, Menichetti, Nordfalk and Ofstad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kjersti Østen, a29zMDE3QHVpdC5ubw==
 Kjersti Østen
Kjersti Østen Julia Menichetti
Julia Menichetti Jenny M. Nordfalk
Jenny M. Nordfalk Eirik H. Ofstad
Eirik H. Ofstad