
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
METHODS article
Front. Commun. , 12 January 2022
Sec. Psychology of Language
Volume 6 - 2021 | https://doi.org/10.3389/fcomm.2021.689439
This article is part of the Research Topic Simple and Simplified Languages View all 11 articles
Caregivers find it difficult to interact with people with dementia who have lost the capacity for speech. Adaptive Interaction is a simplified approach that uses the nonverbal fundamentals of communication to connect with people who can no longer speak. Here we present Adaptive Interaction as a method for equipping caregivers with these nonverbal skills to increase communication with the people they care for. Six caregivers were each paired with one individual with dementia and trained in Adaptive Interaction. After receiving training in Adaptive Interaction, caregivers identified more communicative behaviours in their interactions partners and engaged in more frequent positive social behaviours and meaningful actions during interactions. These findings suggest that it is possible to equip staff to use simplified communication based on nonverbal fundamentals to connect with people with dementia who can no longer speak.
Dementia is a neurodegenerative condition characterised by progressive impairments in cognition that ultimately impact all aspects of an individual’s life. There are multiple causes of dementia, of which Alzheimer’s disease is the most common and age the biggest risk factor (Alzheimer’s Association, 2021). As dementia advances, communication is increasingly affected until people retain little or no speech, relying instead on sounds or vocalizations (Frank, 1994). It has long been established that loss of speech can increase communication difficulties between individuals with dementia and their caregivers, such that the only interactions that take place are during personal care (Bowie and Mountain, 1993).
Lack of meaningful interactions and communication contributes to the increasing social isolation and exclusion of people living with dementia as their illness progresses (Bunn, et al., 2018). Despite being unable to communicate verbally, individuals with dementia retain the “urge to communicate” (Ellis and Astell, 2004; Hughes et al., 2019). Kitwood (1997) as part of his influential work on person-centred dementia care, suggested that when people with dementia are no longer able to communicate with speech, the “fundamentals of communication” that typically act as precursors to the development of speech, can be used. These fundamentals include shared attention, turn taking, eye contact and using and understanding non-verbal communication (Hewitt, 2011; Intensive Interaction Institute, 2021). Using these non-speech-based behaviours to improve communication between people with dementia, their families and caregivers could be crucial in improving their quality of life and well-being (Hughes, et al., 2019), particularly in the later stages of the illness.
Adaptive Interaction (AI: Ellis and Astell, 2011, 2017) is one such approach to communicating with people living with dementia who can no longer speak. AI was developed from Intensive Interaction (Hewett, 1996; Hewett, 2011; Nind, 1996), a teaching/learning approach developed in the UK in the 1980s for people considered “difficult to reach” (Firth et al., 2013). Specifically, these are children and adults with profound and multiple intellectual disabilities who do not develop speech. Intensive Interaction (II) emphasizes the use of these pre-verbal fundamentals of communication that are present in infant-parent interactions (these foundations of II are typically attributed to the work of Ephraim, 1982). II was developed for promoting communication between people born with profound and multiple intellectual disabilities and teachers or classroom assistants.
Developed initially within an educational context, the application and role of II has expanded beyond the classroom to day centres (Clegg et al., 2020), community living (Samuel et al., 2008) and residential (Firth et al., 2007) settings for people with severe developmental disabilities and autism spectrum disorder (ASD; Fraser, 2011). Additionally, training and use of II has extended to speech and language therapists, clinical psychologists (Firth et al., 2004), and care home staff (Firth, et al., 2007).
In considering the utility and application of II, (Firth, 2009) identified two distinct but related approaches that he termed a “social inclusion process model” and “developmental process model” respectively. He argued that the social inclusion model aims primarily at “inclusively responding to a learning disabled person’s communication, however it is expressed. Such social inclusion is seen as being unconditional and at the most personal level” (page 45, Firth, 2009). This is exemplified by practitioners, such as (Caldwell and Jane Horwood 2007) who speak of “connecting” with individuals through a “shared language” and typically describes the increased awareness of the individual’s (nonverbal) communication repertoire. The developmental process model regards II as a means to progressive acquisition of communicative skills (Firth, 2009). Here the focus is on II as “a process with the primary aims of increased sociability and communicative skill development through extended experience of Intensive Interaction” (page 45, ibid). Essentially the aim is to connect with individuals and support acquisition of a greater range of communication skills. From the perspective of dementia as a progressive irreversible neurocognitive disorder, the social process model fits very well with the needs of this population.
One of the key principles of Intensive Interaction is to view all behaviour—such as sounds, movements and facial expressions—from the nonverbal communicator as intentionally communicative. During interactions, communication partners use the fundamentals of communication to uncover aspects of their partner’s communicative repertoire. This uncovering is based primarily on observation of the occurrence of sounds, movements, eye contact, etc, made by the nonverbal partner, to develop an understanding of the ways in which individuals communicate. Close observation means that communication partners can ““be with” this person as they are at present, using their initiatives, gestures, rhythms and sounds to respond in a way that has meaning for them” (Caldwell, 2011). As communicative behaviours are uncovered, the communication partner reflects these back through imitation or repeating a sound or rhythm, building up over time into “wordless conversations” (Barber, 2007). In accordance with the social process model, the intention of learning and adopting the language of the disadvantaged communicator is for the interaction to become shared and meaningful, rather than a list of activities that are carried out with the nonverbal individual (Caldwell, 2011).
The effectiveness of Intensive Interaction is examined through changes in communicative behaviours including elicitations of new behaviours, and increases or reductions in the type, frequency and/or duration of communicative behaviour by both partners. For example, increased contingent smiling (e.g., Argyropoulou and Papoudi, 2012), increased levels of eye contact (e.g., Fraser, 2011) and improved levels of joint attention (e.g., Kellett, 2005). To identify these behaviours, microanalytic observation and coding of video recordings are the major tools for training and implementation of Intensive Interaction (2; Anderson, 2006; Firth, 2021).
Using these methods Watson and Fisher (1997) found increased social behaviours such as “smiling”, “vocalizing”, “initiation” and “direct eye contact” when compared to other classroom activities where Intensive Interaction was not used, leading them to conclude that II was effective in enhancing the level of engagement. In addition to increased communicative behaviours, Nind (2006) found improved ability to maintain and initiate social contact among people with severe developmental disabilities and ritualistic behaviour using a combination of real-time observation, video analysis and informant measures.
In terms of implementation of II as a communication approach in services for people with severe intellectual disabilities and ASD, there are overall positive findings for clients and staff (Berridge and Hutchinson, 2020). For example, staff can gain increased satisfaction in their relationships with clients, residents or service users (Clegg, et al., 2020). However, some challenges with adoption of II have been encountered among care staff, including reluctance to fully engage with the approach (Firth, 2007). In their evaluation of a large-scale II implementation, Clegg et al. (2020) identified “personal discordance, doubt and discomfort” and the importance of organizational support for “implementation at all levels”. These findings have direct relevance for training staff and implementing a non-speech-based approach for people living with advanced dementia.
In adapting II for dementia, Ellis and Astell (2008) conducted a case study with an 81 year old lady—Edie—a care home resident for 5 years. As Edie had gradually ceased being able to use speech, family members and care staff had found communicative interactions with her increasingly difficult. Using the fundamentals of communication, Ellis and Astell uncovered Edie’s communication repertoire which included a range of communicative behaviours. In particular, Edie’s use of vocalizations stood out as a distinctive behaviour. By using imitation to reflect this and other behaviours back to Edie, the communication partner was able to engage in an initial interaction lasting 10 min, in which both partners initiated and took turns (Ellis and Astell, 2008). By uncovering Edie’s communicative repertoire, Adaptive Interactions was able to enhance quality of communication, demonstrated by developing a “shared language” and “meaningful interactions”. A similar study with three individuals living in long-term care reported signs of engagement and interaction and highlighted the opportunity for active participation often denied to bedbound people such as Edie (Harris and Wolverson, 2014).
Adaptive Interaction (AI) was developed specifically to improve communication when people living with dementia can no longer speak (Ellis and Astell, 2011). In a mixed baseline study with five individuals, Adaptive Interaction (AI) techniques were compared with standard interaction (SI) approaches (Ellis and Astell, 2017). In the SI sessions, the communication partner used speech and during the AI sessions used nonverbal channels based on the fundamentals of communication. Each interaction session between the individual with dementia and their conversation partner was video-recorded to allow for a comparison of the two communicative methods. Results of microanalysis indicated an increase in the frequency and duration of communicative behaviours in AI sessions compared to SI sessions. For example, there was an increase in “smiling”, “imitation” and “vocalizations” in AI sessions when compared with SI sessions, in which there were longer durations of “neutral” facial expressions, which is something that could indicate lack of engagement or emotion. Crucially, this study confirmed that each person with dementia possessed their own individual communicative repertoire, and that AI methods were able to uncover these repertoires, which could then be used to build up communication with a conversation partner (Ellis and Astell, 2017).
Communication between caregivers and people living with dementia, can be improved through training along with awareness raising and support to improve their wellbeing and quality of life (Surr, et al., 2017). In a feasibility study Ellis and Astell (2011) extended the AI approach to caregivers in a nursing home in order to assess the potential for AI in improving communication between caregivers and people with dementia. The researchers taught three caregivers theoretical and practical elements of the fundamentals of communication, how communication develops, and aspects of verbal and non-verbal behaviours (Ellis and Astell, 2011) over the course of four sessions. Between training sessions, the caregivers were requested to practice a specific AI task each week, such as imitation or focus of eye gaze. Each interaction was observed and video-recorded to understand the impact of the training and support learning. At follow-up, the caregivers reported that they felt “more equipped” to identify communicative behaviours in people with dementia (Ellis and Astell, 2011). This study demonstrated the potential for caregivers to use a simplified nonverbal approach to enhance their communication with people living with dementia.
The present study builds on the previous feasibility study to develop AI as a method to equip caregivers to identify the communicative repertoires of their communication partners. The effectiveness will be explored by examining the impact on the communication behaviour of both parties in the interactions. To achieve this, the study compares the communication repertoires of six caregivers paired with six people with advanced dementia during a baseline interaction and three subsequent interactions recorded whilst the caregivers receive training in AI. The communication behaviour for both partners and their dyadic behaviour is observed for changes during the course of the training that indicate increased engagement and enhanced communication.
The following questions guide the study:
1) Are there changes in the types and/or frequency and/or duration of communicative behaviours across training sessions?
2) Are any new behaviours elicited during training sessions?
3) In order to explore the individuality of each person’s communicative repertoire, are there behaviours that differ between pairs of participants in response to AI techniques?
Six people with dementia (two male) were recruited plus six care staff (two male). The six people with dementia were aged between 78–92 years, mean age 84.3 and all had either no use of words or occasional use of single words. All participants came from the same care home in the South of England. Relatives of the six people with dementia gave their consent for them to participate and for their interactions with care staff to be video recorded in accordance with the (Mental Capacity Act 2005) (England and Wales). Each participating caregiver was matched to one individual with dementia who was to be their communication partner throughout the study. The Assistant Manager from the care home also attended the training sessions. The study received ethical approval from the NRES Committee London—Camberwell, St. Giles (Ref: 12/LO/0818) and also the University Teaching and Research Ethics committee (UTREC) at the University of St Andrews.
A descriptive-qualitative study was conducted in which Adaptive Interaction training was delivered to staff in the care home over a 3-day period. Interactions between the participating staff and their communication partners were recorded prior to training (baseline condition) and in three further sessions during the training. A microanalysis of communicative behaviours was carried out on the video recordings using the Observer 10.5XT software programme by an independent rate who was not part of the training (second author).
The training was delivered over 3 days—2 days together then one further day a month later. The training was interactive and designed to engage participants in a range of activities in pairs and small groups as well as whole group sessions. The training used a range of methods including Powerpoint™ presentations, videos, case studies and peer teaching. Each participant received a folder of teaching materials and guidance in the use of reflective learning techniques. Each training day included practical activities for participants to carry out either before or during the sessions.
The initial session included exploring the difficulties of communicating with people with dementia and sharing their experiences of recording videos. The fundamentals of communication were also introduced. In the second session, Adaptive Interaction was introduced with a video example. The initial baseline videos were then examined in turn to identify one communicative behaviour for each individual with dementia which the caregivers then attempted to use in a new recorded interaction with their conversation partner. Day 2 commenced with examining the videoclips from the day before with the caregivers sharing their experiences of their first attempt to use Adaptive Interaction. They applied the fundamentals of communication to the new clips and then discussed how to use what they observed to further develop the interaction. They then conducted another interaction using a further identified behaviour. After recording this interaction, the caregivers discussed more ways they could develop the interactions. They also further discussed their continued experiences of using videos. In the final part of Day 2 the caregivers applied the fundamentals to the latest videoclip to plan how to extend the interaction. They also set goals for the following month by developing an interaction package for each of the six individuals with dementia. Before the follow up session each caregiver was asked to produce a fourth recording of interaction with their conversation partner. At the follow up day the first part focused on reviewing the video-recordings and consolidating the plan for each individual resident. The rest of the day was spent developing a strategy to assess communication in the home to identify residents who could benefit from AI and discussing how to disseminate the AI technique to other caregivers and family members of the nonverbal residents.
The six staff were provided with information about the study and a consent form to participate and consent to be videorecorded. They each chose a resident with dementia to work with and were asked to work in pairs to record each other interacting with their resident for 5–10 min. These baseline recordings were reviewed as part of the first AI training activity to identify a single communicative behaviour that could be used in the next session as the basis of nonverbal communication.
The training comprised teaching about the principals of AI and the fundamentals of communication as described above interspersed with practical experience using AI over the three training days. Each day lasted approximately 7 hours resulting in 21 h of training. The final session also included an exercise looking at how to maintain AI for the residents with dementia who cannot speak and identifying potential barriers to be overcome.
A coding scheme was developed based on the fundamentals of communication to microanalyse the communicative behaviours of individuals with dementia and their caregivers from the video-recordings. The coding scheme was based on the elements of verbal and nonverbal behaviour found to comprise the communication repertoires of people with advanced dementia in the previous studies (Astell and Ellis, 2008; Ellis and Astell, 2017). This consisted of thirty-seven behaviours, which were grouped under eight overarching categories, consisting of verbal and nonverbal behaviours: Eye gaze, facial expression, vocalization, physical contact, joint movement, imitation, gestures and body position. The communicative behaviours of individuals with dementia and their caregivers were coded across all four sessions using the following operational definitions (Table 1):
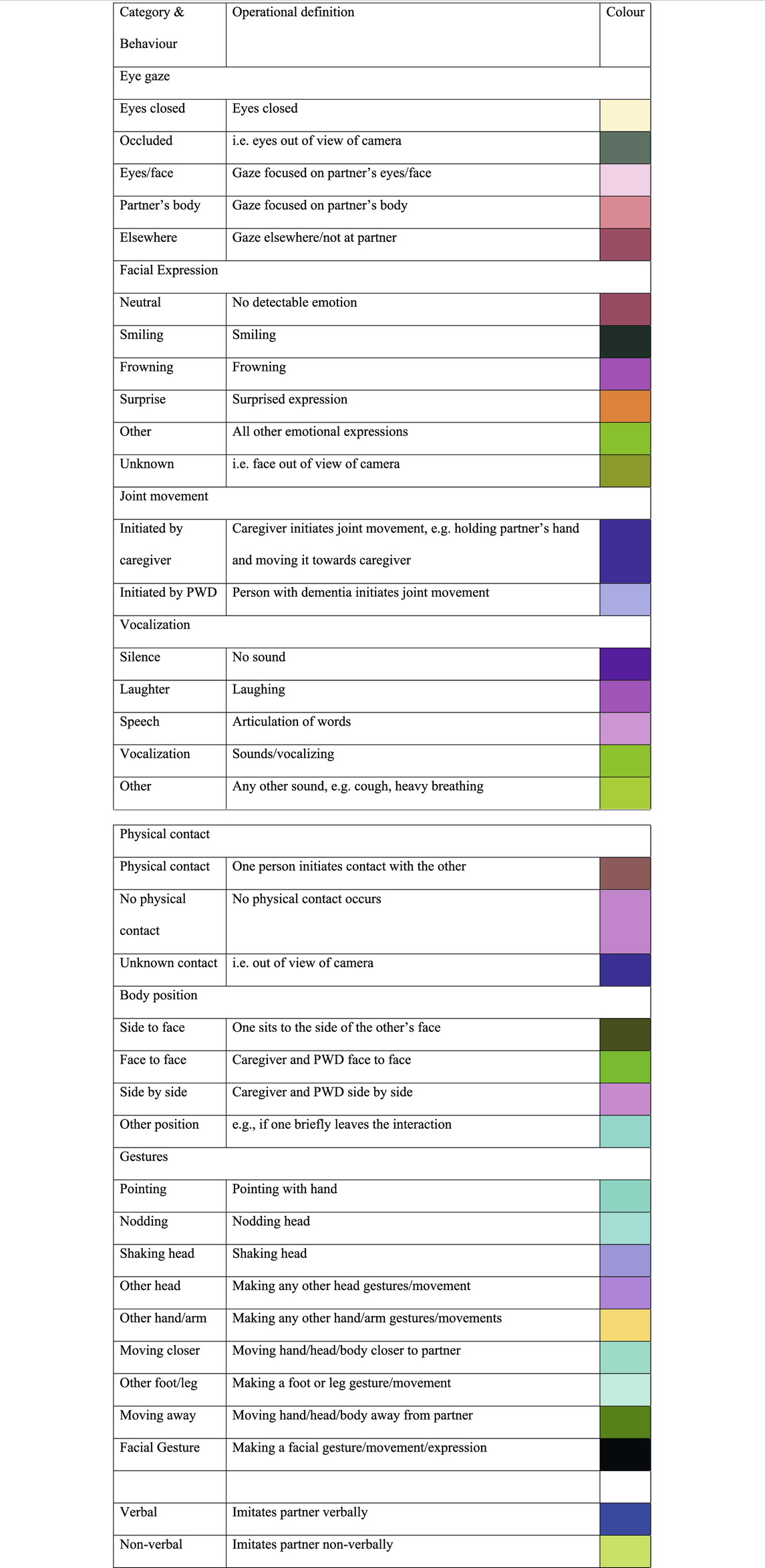
TABLE 1. Coding categories and their operational definitions for both caregiver and person with dementia (PWD).
Each dyad of participants was recorded across four sessions resulting in twenty-four video recordings, ranging from 72 s to 29 min. The Observer 10.5XT software programme was used to code and analyse communicative behaviours for the first 3 min of each session, where possible. The occurrence of behaviours was coded for frequency of occurrence or duration as appropriate. For example, hand movements were recorded for frequency of occurrence, whereas the duration of hand-holding was measured. Visualizations of the coded behaviour were generated from Observer to display the data.
One rater, who was independent of the training, coded each of the twenty-four sessions for communicative behaviours. Three sessions (12%) were selected at random and coded by a second rater, thus allowing kappa values to be calculated. The Cohen’s kappa values were as follows: Inter-rater video A (Diane and Derek session 3)—0.67; inter-rater video B (Graham and Marie session 1)—0.58; inter-rater video C (Karen and Jane session 2)—0.66. As such, the inter-rater reliability can be said to range from fair to moderate agreement (Landis and Koch, 1977). The areas of discrepancy were discussed by the two raters, to further clarify the behavioural coding definitions.
The primary purpose of this study was to explore the potential for training caregivers to use AI to identify, learn and use the communicative repertoires of individuals with dementia for whom speech is no longer functional. Changes in the types and/or number of communicative behaviours across sessions for caregivers and people with dementia would indicate that the Adaptive Interaction method impacts communication.
The communicative behaviour of the dyads at baseline and over the course of practicing AI are displayed in visualizations generated by the Observer video analysis software. The communicative behaviours are grouped into eight domains presented in the same order for all participants: eye gaze, facial expression, joint movement, vocalisation, physical contact, bodily position, gestures and imitation (Table 1). Each behaviour is represented by a colour on the visualization generated by the software. Table 1 contains the key for the visualization labelling.
In the visualizations, the behavioural codes recorded in an event log are plotted horizontally against a time axis—each segment is the first 3 minutes of the interaction. The length of a horizontal bar demonstrates the duration of a “state event” behaviour (e.g., direction of eye gaze). The number of occurrences of a vertical segment demonstrates the frequency of a “point event” behaviour (e.g., smiling) (Zhou, et al., 2013).
Each individual repertoire comprises different combinations of communicative behaviours and therefore not all behaviours occur in each visualization. For example, Figure 3B Jen’s communicative behaviours at baseline fall into five categories—eye gaze (mainly looking elsewhere), facial expression (mainly neutral), vocalization (alternating vocalizing with silence), physical contact (none), and bodily position (side to face). In the fourth interaction (third AI session; Figure 3D) gestures and imitation are also observed. Compared to the baseline visualization Jen and Lorraine are sitting side by side, Jen’s eye gaze is split between looking at Lorraine and looking elsewhere, her facial expression is expanded to include smiling and looking surprised. She also makes physical contact with Lorraine, gestures and imitates Lorraine, none of which were observed in the baseline recording (Figure 3B).
The pattern of change in communicative behaviour across AI sessions provides insight into the point at which the caregiver has identified key components of their partner’s repertoire, and how the caregiver then introduces these components into their own communication approach. The findings are discussed in terms of changes in communicative behaviour from baseline across the AI sessions by looking at key behaviours in the dyads. The data are presented as six dyadic case studies where the first named of each pair the caregiver: Dyad 1: Elena and Renee, Dyad 2: Diane and Derek, Dyad 3: Lorraine and Jen, Dyad 4: Karen and Jane, Dyad 5: Jake and Ernie, and Dyad 6: Graham and Marie (all names have been changed to protect identities).
In the baseline condition, much of Elena’s communicative behaviour was verbal (44.3%), with speech occurring consistently throughout the session (Figure 1A). Elena’s eye gaze shifted between Renee’s eyes/face to looking elsewhere, with much of the interaction spent looking elsewhere (50%). There was some attempt at initiating physical contact with Renee, with the single brown line indicating the short duration of this contact (4.2%).
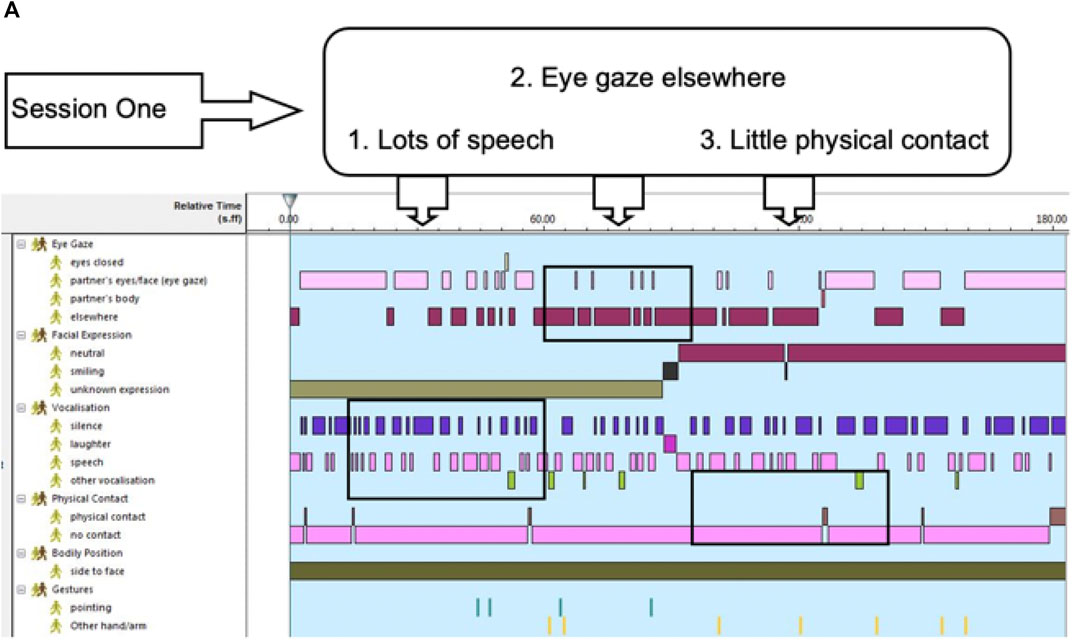
FIGURE 1A. (A) Elena’s Baseline (Session 1) communication. (B) Renee’s Baseline (Session 1) communication. (C) Elena’s First AI (Session 2) communication. (D) Renee’s First AI (Session 2) communication. (E) Elena’s Second AI (Session 3) communication. (F) Renee’s Second AI (Session 3) communication. (G) Elena’s Third AI (Session 4) communication. (H) Renee’s Third AI (Session 4) communication.
Figure 1B illustrates the pattern of Renee’s communicative behaviour during the baseline interaction. Renee’s eyes were closed for 80% of the videoclip, suggesting a lack of engagement with her caregiver partner. Renee frowned 3 times as a response to being touched by Elena, which accounted for 4% of the time. Renee’s extensive use of facial gestures was evident in this session (55 times) and is something that Elena could potentially reflect back to Renee in subsequent sessions.
Figure 1C presents Elena’s first session with Renee after basic training in Adaptive Interaction. Elena was encouraged to uncover one communicative behaviour in Renee’s repertoire using the fundamentals of communication. Elena’s eye gaze was focused on Renee for most of the video clip (84.8%), in comparison to the 50% elsewhere in the baseline interaction. Elena also attempted to imitate Renee’s facial gestures three times. Furthermore, Elena’s speech decreased from the baseline condition—down from 44 to 11.8%, suggesting a move towards focusing on the non-verbal elements of Renee’s communicative repertoire.
Figure 1D illustrates the pattern of Renee’s communicative behaviour during session 2. In a marked change to the baseline condition, Renee’s eyes were closed only for a very short duration (2.3%) in this session, and she looked elsewhere for the majority of the interaction (83.4%). The frequency of Renee’s facial gestures decreased in comparison to the baseline (9 times) however, the amount of frowning increased (27%). Renee moved away from Elena on two occasions during this session in a response to Elena’s initiation of physical contact.
Figure 1E illustrates the turning point of Elena’s communicative behaviour towards and with Renee as it occurred during session 3. Elena was mostly silent in this session, as she spoke briefly only at the beginning (4%). The amount of time spent looking elsewhere decreased (14%), and the majority of the time was spent looking at Renee’s eyes (67.7%) or her hand movements (18.4%). Physical contact was initiated towards the beginning of the session as Elena began to understand Renee’s communicative behaviours, and what she liked and disliked. Elena had been using materials to brush against Renee’s skin. After a while, she was able to understand that Renee did not enjoy being touched in this way and so, she ceased physical contact. Later in the video, Elena initiates physical contact with Renee by touching her skirt. The generally unbroken brown bar in Figure 1E indicates that Renee engaged in physical contact with Elena, so that physical contact occurred for 31.8% of the interaction. Elena practiced imitative behaviour during this session and spent much time imitating Renee’s hand movements on the side of the chair and imitating Renee’s finger movements on her skirt (27 times in total).
Figure 1F illustrates the pattern of Renee’s communicative behaviour during session 3. A greater percentage of time is spent looking at Elena’s body (34.3%), compared to previous sessions pink line, Figure 1F). Renee introduced hand/arm movements into this session (4 times; yellow line), a behaviour that was not apparent during previous sessions. During this session, Renee moved away and towards Elena in a way that was similar to game-playing, suggesting a desire to interact. Towards the end of the session, Renee initiated physical contact with Elena for the first time (7.8%). This is a marked change from previous sessions.
Figure 1G illustrates Elena’s communicative behaviour during the third AI interaction. At this point, Elena has been able to uncover several aspects of Renee’s communicative repertoire. Elena was silent throughout this session (100%; purple bar) and focused entirely on the non-verbal elements of communication. There was only one occasion during the interaction in which Elena directed her eye gaze elsewhere (0.5%), suggesting close attentiveness to Renee. Physical contact occurred for the vast majority of this video (91.5%), suggesting that Elena had become more comfortable with Renee and also that Renee had become more comfortable with Elena. In previous videos, Renee would move away when Elena attempted physical contact. This suggests that a connection had developed between both caregiver and person with dementia. Elena also imitated Renee’s hand movements during this video (9 times). This imitation differed to that in session 3 in that Elena focused more on Renee’s responses as she imitated her. As we will see when we consider Renee’s behaviour during this session, there is a great deal of turn-taking in terms of hand movement and imitative behaviour.
Figure 1H illustrates the pattern of Renee’s communicative behaviour during session 4. Renee spent the majority of the interaction looking at Elena’s body/hands (93%), and only looked elsewhere for short durations (5.2%). This is a marked change from all three previous sessions and indicates an increase in Renee’s engagement with and attentiveness towards Elena. Renee had not previously engaged in imitation, yet she imitated Elena’s hand movements on 9 occasions during this session (light green bar, Figure 1H). The percentage of time Renee spent initiating physical contact with Elena (23.6%) increased from previous sessions, as did the frequency of moving closer 6) and moving away 5) from Elena, suggesting a willingness and desire to “play” with and interact with her partner.
For space reasons we present the communication behaviour at baseline (session 1) and the third AI (session 4) of the other five dyad cases for comparison. The coding scheme and colours are the same as in the first dyadic case study of Elena and Renee.
During the baseline condition, Diane used speech to try to engage Derek, spending 31.2% of the interaction speaking (Figure 2A; second pink line). Often, Diane’s use of speech would provoke Derek to vocalize (Figure 2B, short light green bars). Her gaze was mostly directed at Derek’s face or body, here facial expression was neutral and there was no physical contact (Figure 2A).

FIGURE 2A. (A) Diane’s Baseline (Session 1) communication. (B) Derek’s Baseline (Session 1) communication. (C) Diane’s Third AI (Session 4) communication. (D) Derek’s Third AI (Session 4) communication.
Derek’s vocalizations, which were often very loud, were a key communicative behaviour in his repertoire at baseline (Figure 2B). Derek’s use of hand/arm gestures was also extensive, gesturing 19 times during the initial baseline condition (Figure 2B, dark green line). Derek’s engagement in “vocalizations” and “other hand/arm” gestures (yellow lines) was often erratic and gave the impression of him being agitated, which the staff reported that they felt made it difficult to engage in interactions with Derek. As a result, he experienced most interactions during care activities at the start of the study and was often on his own as the staff feared he would injure other residents or staff through his unpredictable arm waving and gesturing.
After AI training, Diane’s use of speech reduced to 10.4% in session 4 (Figure 2C, darker pink lines). The percentage of time Diane spent looking at Derek’s eyes/face increased from 59.4% in session 1 (Figure 2A) to 82.3% in session 4 (Figure 2C). In the final session, Dian moved to sit by Derek\s side and initiated some physical contact and nonverbal imitation (Figure 2C).
Over the sessions as Diane’s use of speech changed Derek’s vocalizations also decreased and were of shorter duration and intensity (5.9% in session 4: Figure 2D, light green bar). Derek’s unpredictable movement had also reduced to only 1 hand/arm gesture during the final session (Figure 2D, yellow bar). In the final session the dyad moved part way through to sit side by side and some nonverbal imitation took place between them which was a new component of the interaction (bottom Figures 2C,D).
Diane’s reduced use of speech and increase in eye contact appeared to calm Derek, as indicated by reduced vocalizing and gesturing. Through spending time getting to know Derek’s communication repertoire and in particular how he responded to different communicative bids from others, Diane reported that she felt better equipped for initiating interactions with Derek. She was also keen to upskill other staff on how best to engage with him to provide more opportunities for social interaction.
Lorraine speaks a lot during the baseline session (Figure 3A, second pink bar) and also laughs a few times, but this is not reciprocated by Jen (Figure 3B). As she is speaking Lorraine looks at Jen, moving between the face and body, although quite a lot of time she is looking elsewhere (Figure 3A, first dark red line).
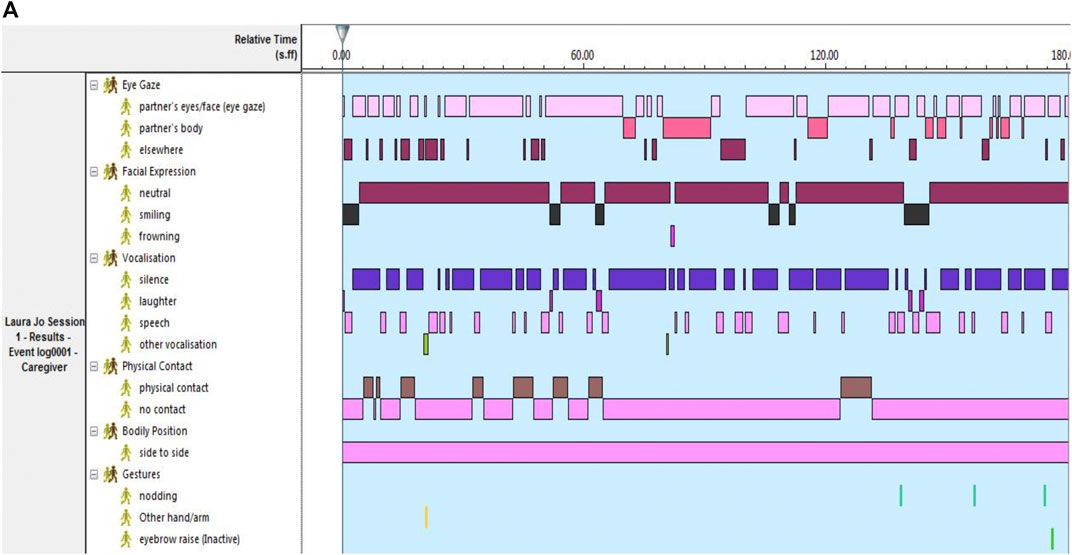
FIGURE 3A. (A) Lorraine’s Baseline (Session 1) communication. (B) Jen’s Baseline (Session 1) communication. (C) Lorraine’s Third AI (Session 4) communication.
A distinct aspect of Jen’s communicative repertoire was “vocalizations”, which were similar to those made by Derek, in respect of being very loud and lengthy in duration. At the start of the project, Jen’s vocalizations were identified as a problem in the care home. Jen did have some residual single words and in the baseline condition (3a), Lorraine commented in response to Jen’s vocalizations: “I don’t understand, use your words”. In the baseline session, Jen spent a lot looking away from Lorraine (Figure 3B, first dark red bar). She did make two single-word utterances, but the majority of her sound-based communication was loud vocalizing which occurred quite frequently (Figure 3B, lower light green bar).
Lorraine continued to use speech during the AI sessions perhaps because she knew that Jen retained one or two individual words (Figure 3C, second pink bar). However, during the AI training and practice, a shift occurred during the second AI interaction (session 3; not shown here for space reasons). In this interaction Lorraine and Jen started building a shared language through imitation, physical contact and turn-taking. Specifically, Lorraine initiated physical contact 81.7% of the time and Jen 31% of the time (not shown here). Jen also initiated joint movement twice in this session whilst Lorraine initiated joint movement 6 times. Here, they would pull each other’s hands/arm towards one another and would touch heads. Jen “moved closer” to Lorraine 11 times during this session.
As the sessions progressed, Lorraine imitated components of Jen’s communicative repertoire including her vocalizations and facial gestures, with the number of imitations increasing steadily from 0 in session 1 (Figure 3A) to 12 in session 4 (Figure 3C). Lorraine’s use of facial gestures increased similarly from 0 in session 1 (Figure 3A) to 15 in session 4 (Figure 3C, bottom row), suggesting that she became more comfortable using nonverbal communication alongside speech.
As occurred with Derek, the percentage of time Jen spent engaging in vocalizations reduced from 28% in session 1 (Figure 3B) to just 1% in session 4 (Figure 3D). The level of contentment and attentiveness in the dyad can be seen in the percentage of smiling which increased from 0% in session 1 (Figure 3B) to 49.6% in session 4 for Jen (Figure 3D), and from 11.2% in session 1 (Figure 3A) to 35.8% in session 4 for Lorraine (Figure 3C). In the final session, the amount of time Jen spent looking at Lorraine’s face (43.4%) was roughly double that in the baseline (22.5%; Figure 3B), even though Jen and Lorraine were engaged in an activity which involved looking at a fish tank. A major change is the physical contact Jen makes in the final session (Figure 3D, brown bar) compared to none in the baseline session (Figure 3B).
During the reflection component of the training, Lorraine was able to share what she had learnt about Jen’s communication and specifically her vocalizing. This empowered the team to develop a plan for reducing the occurrence of loud vocalizing, which was creating difficulties within the care home at the start of the training, whilst increasing opportunities for Jen to engage in social interactions, outside of personal care.
Jane was the only participant with dementia who had retained some ability to use more than single words. However, her verbal language would get very muddled, and it was difficult to understand what she was saying and the meaning of her words. Jane’s use of facial expressions was one way of understanding her communicative repertoire. Her facial expressions would shift rapidly from “neutral” to “smiling” to looking distressed (coded as “other facial expression”). As Karen recognized Jane’s distressed expression, she would often touch and engage in “smiling” to comfort her. In the baseline session, Karen initiated physical contact 8.8% of the time (Figure 4A) and she consistently used gestures, including nodding, and shaking her head.
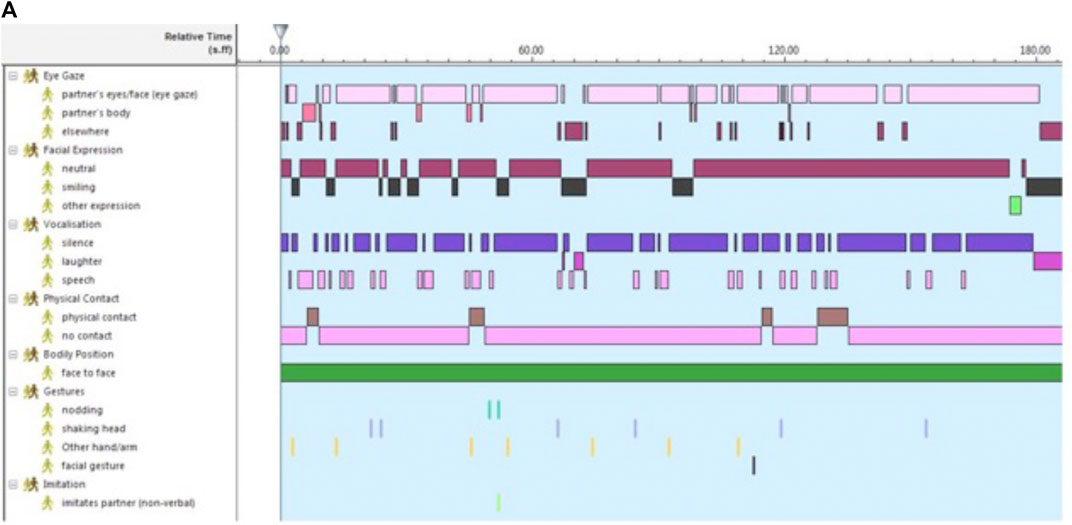
FIGURE 4A. (A) Karen’s Baseline (Session 1) communication. (B) Jane’s Baseline (Session 1) communication. (C) Karen’s Third AI (Session 4) communication. (D) Jane’s Third AI (Session 4) communication.
As Jane had some preserved speech, the turn-taking between her and Karen was more apparent at baselines, with Jane frequently looking at Karen’s face (Figure 4B). Jane did speak during the baseline session, but the interaction was also maintained through nonverbal behaviours such as head nodding and other gestures (Figure 4B). Jane also made notable facial expressions including one which was labelled as distress but was not accompanied by other signs that might indicate she was experiencing pain or discomfort.
During the AI training, the percentage of time Karen spent initiating physical contact increased from 8.8% in session 1 (Figure 4A) to 48% in session 4 (Figure 4C). Karen’s use of speech remained at a relatively constant level throughout the sessions (Figure 4A and4c), and she consistently used gestures, including nodding and shaking her head, In session 4 Karen moved closer to Jane (Figure 4C) and she also made some vocalizations.
Jane’s level of contentment and engagement with Karen can be observed in the amount of time spent “smiling” which increased from 7.4% during session 1 (Figure 4B) to 30% in session 4 (Figure 4D). There was also an increase in the percentage of time Jane was looking at Karen’s eyes/face which increased from 44% in session 1 (Figure 4B) to 87% in session 4 (Figure 4D). Jane used less speech in the final AI session and also vocalized, which appeared to be in response to Karen. Her head nodding and shaking also increased (Figure 4D).
Jane and Karen present an interesting example of the familiar situation that occurs when people living with dementia still have some speech, but it is no longer sufficient or functional for supporting interactions. There is usually a tendency to rely on speech, but what emerged during the AI sessions is the importance of attending to and learning an individual’s communicative repertoire even when they have some speech, to identify the nonverbal behaviours that can support continued social interaction.
In the baseline session Jake spoke for around 18% of the time and made no attempts to imitate Ernie (Figure 5A). Jake mostly has a neutral facial expression with occasional smiles (Figures 5A, C). In session 1 Jake attempts physical contact (Figure 5A) which Ernie withdraws from. However, by session 4 this has reduced to almost none (Figure 5C) as he became more familiar with Ernie’s repertoire.
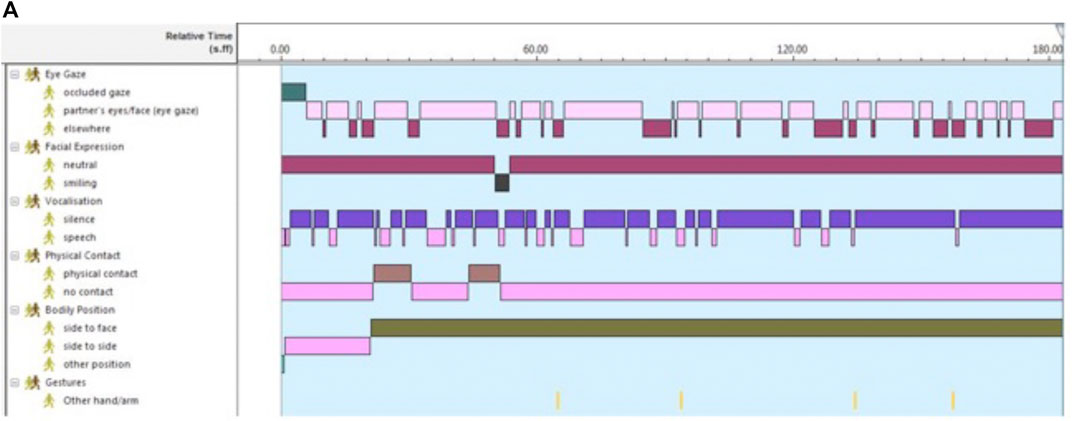
FIGURE 5A. (A) Jake’s Baseline (Session 1) communication. (B) Ernie’s Baseline (Session 1) communication. (C) Jake’s Third AI (Session 4) communication. (D) Ernie’s Third AI (Session 4) communication.
Ernie’s started the first session with his eyes closed (26.3% of time; Figure 5B) and when he opened them, he mostly looked away from Jake. At baseline a small number of communicative behaviours were evident including hand/arm gestures, and facial gestures such as blinking (Figure 5B). He moved away when Jake made physical contact and made no sounds at all (Figure 5B).
Jake’s speech reduced steadily from 17.8% in session 1 (Figure 5A) to 2.2% in session 4 (Figure 5C), where he is almost totally silent. After AI training, Jake attempts to imitate Ernie 7 times in the final session 4 (Figure 5C, light green bar) relative to no attempts in the baseline (Figure 5A). Jake is also more attentive to Ernie in the final session, looking almost constantly at his face (Figure 5C), as opposed to the first session where he gazes towards and away from Ernie throughout (Figure 5A).
In the final session Ernie kept his eyes open pretty much all of the time, which may be the result of efforts by Jake to engage with Ernie. Ernie still spent most of the time looking away from Jake (Figure 5D) Much of this time was spent looking at the camera/researcher, which consistently occurred across the four sessions. Attempts by Jake to touch Ernie would result in Ernie moving away from Jake and/or “frowning”. In the final session Ernie vocalized a couple of times, which was a new behaviour and his facial expressions increased (Figure 5D).
While people living with dementia who make loud vocalizations (such a Derek and Jen) are often considered “problematic” in care settings, people such as Ernie, who make no sounds (baseline) can be overlooked or their silence interpreted as contentment or satisfaction. The small changes that occurred in Ernie’s behaviour suggest that he started to respond to Jake’s attentiveness and imitation, which could lead to increased social opportunities as the caregivers understand how to engage and interact with him.
Marie was in the very late stages of dementia and was limited in her movements. Graham was fairly new to caregiving and paid close attention to Marie during the baseline session, looking at her for long periods (Figure 6A). He spoke briefly and waited to see if she responded and also nodded his head, perhaps to reinforce that he was attending to her (Figure 6A). Graham initiated physical contact once or twice but primarily tried speech to engage Marie.

FIGURE 6A. (A) Graham’s Baseline (Session 1) communication. (B) Marie’s Baseline (Session 1) communication. (C) Graham’s Third AI (Session 4) communication. (D) Marie’s Third Ai (Session 4) communication.
A key component of Marie’s communicative repertoire was her heavy breathing (Figure 6B “other vocalizations”). For most of the time she was silent but there was one instance of laughter in response to Graham laughing (Figures 6A,B dark pink bar). During the baseline session Marie looked at Graham a few times, including when she was laughing, but mostly she looked elsewhere.
Through the AI training, Graham was able to identify Marie’s heavy breathing and imitate this to engage Marie, which resulted in turn-taking during the later sessions. This is evident from the increasing number of instances where Graham imitated Marie from 0 during session 1 (Figure 6A) to 17 times during session 4 (Figure 6C). The percentage of time Graham spent initiating physical contact also increased from 5.8% in session 1 (Figure 6A) to 100% in session 4 (Figure 6C). As Graham learnt more about Marie’s communication repertoire, his use of speech reduced from 28.3% in session 1 (Figure 5A) to 2.6% in session 4 (Figure 6C) as he vocalized with Marie (Figure 6C, light green bar). Graham continued to use head nodding and shaking to support turn taking.
The number of times Marie imitated Graham also increased steadily from 0 during session 1 (Figure 6B) to 13 times during session 4 (Figure 6D), highlighting the “turn-taking” that took place. Marie also engaged in physical contact for 100% of the time in session 4 (Figure 6D), with Graham commenting that she was “holding my fingers”. In the final session Marie had her eyes closed some of the time, during which one of the other staff commented that she looked “blissful”. Indeed, the interactions between Graham and Marie were very calm, with the growing sense of connection apparent to observers.
Marie, like Ernie, was a very quiet resident and due to her mobility restrictions was at risk of social exclusion. The recordings of her sessions with Graham and his reflection on them encouraged the staff as a group to think about how they could spend quality time with Marie, who actually died shortly after the end of the training.
Unsurprisingly the caregivers primarily used speech in the baseline interactions to engage the people living with dementia. When they did not respond to speech, they often used physical contact to try to gain their partner’s attention. They were self-conscious of being recorded and often uncomfortable trying to have an interaction that did not involve a care act, such as supporting the individual to eat. Many of the interactions took place side to face, as the participants were in bed. Only Karen positioned herself face to face with Jane during the baseline session, where she also gestured and smiled unlike most of her colleagues. Karen was also the only caregiver who used imitation in the baseline session, suggesting that she was comfortable with nonverbal means of communication before the AI training.
During the AI sessions, the use of speech declined considerably as the caregivers started to attend to and reflect their partner’s nonverbal communicative behaviours. There was a notable shift in the nature of the interactions, with caregivers focusing intently on their partner and the act of communication. As they concentrated on connecting with their partner, they also lost their self-consciousness. In the video review sessions, the caregivers were excited to point out where they noticed a communicative behaviour, how they imitated or expanded a sound or gesture and the reaction of their partner. Playfulness also emerged, such as Renee moving her hand towards and then away from Elena in the final session and Elena following which she described as a “game”.
Two key points emerged from the six dyadic cases. First is that each caregiver was able to learn to use AI to elucidate their partner’s communicative repertoire and identify aspects of it to reflect back. These repertoires ranged from loud vocalizing to complete silence, facial expressions, eye gaze direction, and physical movements. This confirms that each person with advanced dementia retained the urge to communicate and that caregivers were able to recognise this which motivated them to continue the interactions.
The second point is that the nature of the interactions changed over time with different interaction patterns apparent in the final AI session (figures “g” and “h” in Dyad 1 and figure “c” and “d” in Dyads 2–6) relative to the baseline interactions (figures “a” and “b” in all dyads). All of the caregivers reduced the amount of speech they used and increased nonverbal behaviours, such as eye gaze, imitation and reflecting back the communicative behaviours of the individual with advanced dementia. For example, Graham identified Marie’s heavy breathing as a communicative act and reflected this back to make an intense connection. Whilst caregivers often started to use vocalizing to connect with their partners, for example by imitating a sound or breathing pattern, the loud, vocalizations of two residents—Derek and Jen–were substantially reduced over the AI sessions as other communicative behaviours developed within their dyads. This confirms that it is possible to build a communicative relationship with individuals with advanced dementia who can no longer use speech.
In a separate interview conducted by an independent researcher 3 months after the AI training, the caregivers all said that they found the training excellent and did not have any suggestions to improve it (Dampney-Jay, 2015). Three caregivers reported that watching back videos of themselves interacting was a particularly helpful element of the course and two commented that having opportunities to practice the skills as they learn them was beneficial.
This study describes how caregivers can be trained to use Adaptive Interaction, a simplified method, to communicate with people living with dementia who can no longer speak. Introducing the fundamentals of communication to care staff enabled them to identify non speech based communicative behaviours in the residents they care for. Staff learnt how to attend to the individual residents, to identify an initial communicative behaviour and make a connection with them. The training also equipped them to apply AI to identify the communicative repertoires of people living with advanced dementia and use this as the basis for a meaningful interaction. The study also further extended understanding about the individuality of nonverbal communication repertoires (Ellis and Astell, 2017) and how they can be uncovered with AI.
The findings indicate that it is feasible to train staff in long term dementia care settings to use AI to engage with and interact with nonverbal residents. These individuals, who are often also immobile, are completely reliant on caregivers for social interactions either in or out of their bedrooms (Astell and Ellis, 2006). However, staff often feel that without speech, they can no longer connect with residents. The findings that AI can be used to make a connection and maintain this nonverbally suggests that the Social Inclusion Process (SIP) model of Intensive Interaction (Firth, 2009) on which AI is based, can be applied to people living with advanced dementia. the SIP model emphasises making a connection and learning the language of the individual who does not have speech (Caldwell, 2006). This finding presents a hopeful message for people living with dementia and caregivers as it provides a means of keeping them engaged in the social world (Currie, 2020). This can open up new ways of thinking about how to meet the needs of nonverbal individuals and improve their wellbeing. For example, in this study as the staff became more aware of the ways in which their nonverbal residents communicated, this generated discussions about care planning to increase the wellbeing of residents using AI.
Training in communication skills can raise awareness of the needs of people living with dementia and improve their wellbeing and quality of life (Surr, et al., 2017). Equipping care staff to use AI could overcome some of the barriers identified in previous studies regarding communication with people with advanced dementia (Beer et al., 2012). For example, Beer and colleagues (2012) found that communication training provided to nursing aides increased their awareness of the need for meaningful contact with people living with advanced dementia but did not improve their comfort levels or perceive skills for working with this population. The interactive training approach described here combining case examples, hands-on practice, and reflection may be successful at overcoming barriers to staff competence and confidence at using non speech-based communication.
Additionally, this study included two components aimed at implementing and sustaining AI in long-term care. The first was to include someone from the care home management team in the training, in this case the Deputy Manager, in line with the importance identified by Clegg, et al. (2020) for “organizational support”. The second aspect was to include in the training programme a session to develop a strategy 1) to assess communication in the home to identify residents who could benefit from AI and 2) to disseminate AI to other caregivers and family members of the nonverbal residents.
A single rater coded 100% of the videos, which was partially addressed through this rater being independent of the study and having a second rater code a proportion of the videoclips. The small scale and short duration could be regarded as another limitation, although in long-term care settings, freeing up staff to participate in training is a perennial challenge. Interactions recorded over a longer duration of time (e.g., 6 months) could permit the effects of consolidation over time to be measured. To address this, interviews about the training and consolidation were conducted 3 months after the end by a researcher external to the research team.
Adaptive Interaction is a simplified approach to communication that can equip caregivers with the skills to communicate effectively with individuals with dementia who can no longer speak. Caregivers were able to use AI to learn the language of the individuals they care for and adopt nonverbal strategies to connect with them. Each individul living with advanced dementia had their unique communicative repertoire comprising a specific set of nonverbal behaviours. These findings support the utility of AI to elucidate even the most subtle communicative behaviours, whilst looking across the dyads collectively, illustrates the range of such behaviours. The findings also suggest an increase in the quality of communication as indicated by more frequent positive social behaviours and meaningful actions such as eye gaze, turn-taking and initiating physical contact by both partners in the interactions. Adaptive Interaction could be a useful tool for improving the quality of life and wellbeing of people living with advanced dementia who can no longer speak by providing a means of enhancing caregiving relationships. This in turn could improve the job satisfaction and feelings of competence of the people who care for them.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by NRES Committee London—Camberwell, St. Giles (Ref: 12/LO/0818). The ethics committee waived the requirement of written informed consent for participation
AA co-designed the study, delivered the training and prepared the manuscript SS co-developed the video doing scheme, coded the videos and wrote up the results ME co-designed the study, delivered the training, co-developed the video coding scheme.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Alzheimer’s Association (2021). 2021 Alzheimer's disease facts and figures. Alzheimers Dement. 17(3):327-406. Available athttps://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.12328 doi:10.1002/alz.12328
Anderson, C. (2006). Early Communication Strategies: Using Video Analysis to Support Teachers Working with Preverbal Pupils. Br. J. Spec. Education 33 (3), 114–120. doi:10.1111/j.1467-8578.2006.00426.x
Argyropoulou, Z., and Papoudi, D. (2012). The Training of a Child with Autism in a Greek Preschool Inclusive Class through Intensive Interaction: a Case Study. Eur. J. Spec. Needs Education 27 (1), 99–114. doi:10.1080/08856257.2011.640489
Astell, A. J., and Ellis, M. P. (2006). The Social Function of Imitation in Severe Dementia. Inf. Child. Develop. 15, 311–319. doi:10.1002/icd.455
Barber, M. (2007). Imitation, Interaction and Dialogue Using Intensive Interaction: tea Party Rules. Support Learn. 22 (3), 124–130. doi:10.1111/j.1467-9604.2007.00459.x
Beer, L. E., Hutchinson, S. R., and Skala-Cordes, K. K. (2012). Communicating with Patients Who Have Advanced Dementia: Training Nurse Aide Students, Communicating with Patients Who Have Advanced Dementia: Training Nurse Aide Students. Gerontol. Geriatr. Education 33 (4), 402–420. doi:10.1080/02701960.2012.702165
Berridge, S., and Hutchinson, N. (2021). Staff Experience of the Implementation of Intensive Interaction within Their Places of Work with People with Learning Disabilities And/or Autism. J. Appl. Res. Intellect. Disabil. 34, 1–15.
Bowie, P., and Mountain, G. (1993). Using Direct Observation to Record the Behaviour of Long-Stay Patients with Dementia. Int. J. Geriat. Psychiatry 8, 857–864. doi:10.1002/gps.930081009
Bunn, F., Lynch, J., Goodman, C., Sharpe, R., Walshe, C., Preston, N., et al. (2018). Improving Living and Dying for People with Advanced Dementia Living in Care Homes: a Realist Review of Namaste Care and Other Multisensory Interventions. BMC Geriatr. 18, 303. doi:10.1186/s12877-018-0995-9
Caldwell, P. (2005). Finding You, Finding Me: Using Intensive Interaction to Get in Touch with People with Sever Learning Disabilities Combined with Autistic Spectrum Disorder. London: Jessica Kingsley Publisher.
Caldwell, P. (2011). Intensive Interaction: Using Body Language to Communicate. UK. JODD. Available at http://www.intellectualdisability.info/how-to-guides/articles/intensive-interaction-using-body-language-to-communicate.
Caldwell, P., and Horwood, J. (2007). From Isolation to Intimacy. London: Jessica Kingsley Publisher.
Clegg, J., Black, R., Smith, A., and Brumfitt, S. (2020). Examining the Impact of a City-wide Intensive Interaction Staff Training Program for Adults with Profound and Multiple Learning Disability: a Mixed Methods Evaluation. Disabil. Rehabil. 42 (2), 201–210. doi:10.1080/09638288.2018.1495769
Currie, L. (2020). Adaptive Interaction as a Method of Non-verbal Communication in Individuals with Dementia. Independent Nurse. 29(4):176-180. Feb 11th Available at https://www.independentnurse.co.uk/year-of-the-nurse/adaptive-interaction-as-a-method-of-non-verbal-communication-in-individuals-with-dementia/224051/. doi:10.12968/pnur.2018.29.4.176
Dampney-Jay, G. (2015). Improving Nonverbal Communication between Caregivers and People with Advanced Dementia: the Effect of Staff Training in Intensive Interaction on Quality of Life. Unpublished DClinPsych Thesis. Canterbury, United Kingdom: Canterbury Christchurch University.
Ellis, M., and Astell, A. J. (2004). The Urge to Communicate in Severe Dementia. Brain Lang. 91 (1), 51–52. doi:10.1016/j.bandl.2004.06.028
Ellis, M. P., and Astell, A. J. (2011). Intensive Interaction for People with Dementia: A New Approach to Communication? J. Demen. Care 19 (3), 24–26.
Ellis, M. P., and Astell, A. J. (2008). Promoting Communication with People with Severe Dementia. in Techniques for Promoting Social Engagement in Individuals with Communicative Impairments Editor S. Zeedyk (London: Jessica Kingsley Publishers).
Ellis, M. P., and Astell, A. J. (2017). Communicating with People with Dementia Who Are Nonverbal: the Creation of Adaptive Interaction. PLOS ONE 12 (8), e0180395.
Ephraim, G. W. (1982). Developmental Process in Mental Handicap: A Generative Structure Approach. Unpublished PhD Thesis. Bristol, United Kingdom: Brunel University.
Firth, G. (2021). Connecting with Intensive Interaction. Available at https://connectingwithintensiveinteraction.com/category/research/research-summaries-with-adult-participants/.
Firth, G. (2009). A Dual Aspect Process Model of Intensive Interaction. Br. J. Learn. Disabilities 37 (1), 43–49. doi:10.1111/j.1468-3156.2008.00505.x
Firth, G., Elford, H., Crabbe, M., and Leeming, C. (2007). Intensive Interaction as a Novel Approach in Social Care: Care Staff’s Views on the Practice Change Process. J. Appl. Res. Intellect. Disabil. 21, 58–69. doi:10.1111/j.1468-3148.2007.00369.x
Firth, G., Elford, H., Crabbe, M., and Leeming, C. (2004). Intensive Interaction: Changing Views and Relationships? Draft Final Report. Leeds: Leeds Mental Health NHS Trust.
Firth, G., Poyser, C., and Guthrie, N. (2013). Training Care Staff in Intensive Interactions. Learn. Disabil. Pract. 16 (10), 14–19. doi:10.7748/ldp2013.12.16.10.14.e1499
Frank, E. M. (1994). Effect of Alzheimer’s Disease on Communication Function. J. South Carolina Med. Assoc. 90 (9), 417–423.
Fraser, C. (2011). Can Adults on the Autism Spectrum Be Affected Positively by the Use of Intensive Interaction in Supported Living Services? Good Autism Pract. 12 (2), 37–42.
Harris, C., and Wolverson, E. (2014). Intensive Interaction: to Build Fulfilling Relationships. J. Demen. Care 22 (6), 27–30.
Hewett, D. (1996). “How to Do Intensive Interaction,” in Interactive Approaches to Teaching: A Framework for INSET. Editors M. Collis., and P. Lacey (London: David Fulton).
Hughes, S., Woods, B., Algar-Skaife, K., and Hedd Jones, C. (2019). Understanding Quality of Life and Well-Being for People Living with Advanced Dementia. Nurs. Old. People 31 (2), 18–24. doi:10.7748/nop.2019.e1129
Intensive Interaction Institute (2021). The Fundamentals of Communication. Spring Arbor University. Available at https://www.intensiveinteraction.org/find-out-more/fundamentals-of-communication/.
Kellet, M. (2005). Catherine’s Legacy: Social Communication Development for Individuals With Profound Learning Difficulties and Fragile Life Expectancies. Brit. J. Spec. Edu. 32 (3), 116–122. doi:10.1111/j.0952-3383.2005.00383.x
Kitwood, T. (1997). Dementia Reconsidered. The Person Comes first Maidenhead. Maidenhead, United Kingdom: Open University Press.
Landis, J. R., and Koch, G. G. (1977). The Measurement of Observer Agreement for Categorical Data. Biometrics 33, 159–174. doi:10.2307/2529310
Mental Capacity Act (2005). Available at: https://www.legislation.gov.uk/ukpga/2005/9/contents.
Nind, M. (1996). ‘Efficacy of Intensive Interaction: Developing Sociability and Communication in People with Severe and Complex Learning Difficulties Using an Approach Based on Caregiver-Infant Interaction'. Eur. J. Spec. Educ. Needs 11 (1), 48–66.10.1080/0885625960110104.
Nind, M. (2006). Efficacy of Intensive Interaction: Developing Sociability and Communication in People with Severe and Complex Learning Difficulties Using an Approach Based on Caregiver‐infant Interaction. Eur. J. Spec. Needs Education 11 (1), 48–66. doi:10.1080/0885625960110104
Samuel, J., Nind, M., Volans, A., and Scriven, I. (2008). An Evaluation of Intensive Interaction in Community Living Settings for Adults with Profound Intellectual Disabilities. J. Intellect. Disabil. 12 (2), 111–126. doi:10.1177/1744629508090983
Surr, C. A., Gates, C., Irving, D., Oyebode, J., Smith, S. J., Parveen, S., et al. (2017). Effective Dementia Education and Training for the Health and Social Care Workforce: A Systematic Review of the Literature. Rev. Educ. Res. 87 (5), 966–1002. doi:10.3102/0034654317723305
Watson, J., and Fisher, A. (1997). Research Section: Evaluating the Effectiveness of Intensive Interactive Teaching with Pupils with Profound and Complex Learning Difficulties. Br. J. Spec. Education 24, 80–87. doi:10.1111/1467-8527.00020
Keywords: dementia, nonverbal, interaction, social isolation, training, communication
Citation: Astell AJ, Shoaran S and Ellis MP (2022) Using Adaptive Interaction to Simplify Caregiver’s Communication with People with Dementia Who Cannot Speak. Front. Commun. 6:689439. doi: 10.3389/fcomm.2021.689439
Received: 31 March 2021; Accepted: 15 October 2021;
Published: 12 January 2022.
Edited by:
Andras Kornai, Computer and Automation Research Institute (MTA), HungaryReviewed by:
Eliseo Diez-Itza, University of Oviedo, SpainCopyright © 2022 Astell, Shoaran and Ellis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Arlene J. Astell, YS5hc3RlbGxAcmVhZGluZy5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.