- 1Department of Primary Care, Rocky Vista University College of Osteopathic Medicine, Ivins, UT, United States
- 2Department of Biomedical Sciences, Rocky Vista University College of Osteopathic Medicine, Parker, CO, United States
Introduction
Medical education is an ever-changing field fraught with uncertainty for students. Events over the 4 years determine the majority of their careers, which makes the task daunting and stressful. When a pandemic that hinders their learning experience enters the mix, many feel lost and left behind (Ferrel and Ryan, 2020). The recent pandemic has placed a significant strain on education systems across the world. Medical students had licensing examinations cancelled, clinical experiences cut short, and lab time put on hold. Clinical experiences help medical students develop their professional identities (Cullum et al., 2020), yet this opportunity has been stripped from many or hindered at best. For those who remained involved in clinical experiences, it was for a limited period of time. Telehealth became the new norm, personal protective equipment was scarce, and occupancy limits were decreased leaving students to stand in the background (Rose, 2020). These constraints altered many aspects of medical education and, as researchers, we were interested in learning more about how our community was impacted. The purpose of this data set is to provide the basis of an exploratory study to understand the evolution of medical student and university staff perceptions of COVID-19 over the course of 3 months during the pandemic. We investigate both staff and students in order to identify if there is a disparity in effects on mental health.
Current research explores the root cause of the increasing anxiety experienced by medical students during the pandemic. A study done at King Saud University College of Medicine aimed to understand the impact of quarantine on medical student well-being. The results of their online survey showed a significant increase in feelings of distress and depression. Students felt detached from family and friends, and they felt that the pandemic significantly decreased their overall performance (Meo et al., 2020). Another article by Huckins et al. (2020) reported on the behavior of college students before and during the COVID-19 pandemic. Behavior was analyzed using a Student Life mobile application. Depression and anxiety were assessed weekly through self-reporting. Results showed that students were more sedentary and reported increased depression and anxiety during the Winter 2020 academic term when compared to earlier academic terms (Huckins et al., 2020). For university staff the story is likely to be similar to students although there are some additional concerns since medical school staff often have clinical and classroom duties. A recent study in Saudi Arabia showed how the anxiety levels of health care providers working in an academic care center increased 41% with the recent pandemic (Temsah et al., 2020a), similar observations we made in s study in China (Cai et al., 2020), however their compliance to use protective equipment and to adhere to hygienic practices was affected by previous experiences with other infectious agents (Temsah et al., 2020b) Administrative duties that university staff add additional concerns for effective leadership during a continuously changing situation in this pandemic this situation is common across all people involved in leadership (Papadimos et al., 2020). It is important to mention that academic professionals have shown to display lower anxiety and depression levels associated with the COVID-19pandemic than the regular population (Rakhmanov et al., 2020).
A common theme of the articles we reviewed about medical education during the pandemic was communication. Communication plays a vital role in the sense of comradery and wellness essential to a successful medical education. Reassurance is a key part of an institutional response regarding educational changes in response to the pandemic and should be given the highest priority, even more so than learning new technology or focusing on the actual content of study (Rose, 2020) this is highly relevant to both students and staff. It is recommended to have frequent communications even if there are educational uncertainties. A study by Byrnes et al. (2020) found that one-fifth of medical students who took part in a national survey are concerned that their choice of specialty in the future will be directly affected by COVID-19. Without the chance to fully participate in clinical rotations, students are not only losing exposure to potential fields of interest, but they are also missing opportunities to network and obtain the all-important letters of recommendation required for residency applications (Byrnes et al., 2020). Medical student success is an important concern for university staff regardless of the pandemic (Newble and Entwistle, 1986) and is likely to be exacerbated by all the limitations COVID restrictions have imposed in their mission.
As COVID-19 continues to surge in our society and anxiety about their futures persist, communication from medical institutions, including from national governing bodies for medical education, must be a priority. There are essential gaps in the explanation for the mental health effects felt specifically by medical students and university staff during this pandemic, including the evolution of their reactions over time. Future pathways of research should focus on the development of clear operational indicators that will allow for gauging effective communication methods and counseling efforts to alleviate the anxiety felt by medical students and university staff during this trying time.
Methods
We looked more closely at how the COVID-19 pandemic affected the behaviors and perceptions regarding educational/career success and the gravity of the pandemic. This was investigated by conducting an emailed survey gauging student and staff experiences during this pandemic. The survey was designed as the basis of an exploratory study of a group conceptualization construct that is likely to be multidimensional and which may include as suggested by the literature dimensions such as anxiety level, compliance and perception. Our survey was designed to explore the student and staff body as a group with the intention of further developing a pertinent course of action where the pertinent dimensions can be defined. The questionnaire was based on the recommendations put forth by the CDC during the emergence of the pandemic, such as social distancing, restricting travel, and wearing masks (US Center for Disease Control, 2020). We included questions regarding public behavior, such as panic buying, and shared sentiments among our community, including study/work habits and feelings of isolation. Questions were measured each using a nominal scale with two responses (Agree/Disagree) with the exception of Question 11 which had three responses and each was evaluated using a nominal scale with two responses (Yes/No). Three months later in June of 2020, the original survey was followed up with a second survey that included the same items. The goal of these surveys was to determine if a shift in behavior occurred from the beginning of the pandemic to several months later, and if there were any differences between medical students and university staff.
We collected a total of 600 responses using an online Google survey disseminated via institutional email, of which 52.5% responded to the initial survey deployment and 47.5% to the follow-up. 476 of the 600 identified themselves as either staff or students. Based on those responses, 72% were students and 28% were university staff, including faculty, administrators, and general university staff. All responses were voluntary and anonymous. Respondents were able to answer with either a “disagree” or “agree” response. A copy of the questionnaire is available as Supplementary Material. The collection of this dataset was reviewed and approved by the RVU Institutional Review Board #2020-0036. All participants were provided with informed consent to participate in this study. Our most important limitation in this dataset was the lack of ability to match survey responses between initial and follow-up surveys due to the restrictions on identifiers put in place by our IRB.
Dataset
The dataset and questionnaire presented in this study can be found in the Mendeley Data repository and are freely accessed through the following link: http://dx.doi.org/10.17632/xzwnpjyzwj.1. The dataset is contained in a Microsoft Excel v.2016 format and contains no identifiable information, while the questionnaire is available in PDF form.
Descriptive Analysis of the Data
We evaluated descriptively our data using Generalized Linear Models with a binary response (log-linear), where we evaluated the effects of the time point and the participant’s role, either student or university staff as main effects. Cronbach’s alpha of our exploratory study was of 61% which can be raised to 65% with the deletion of questions 2 and 10, 69% when deleting both questions. Linear model estimates of our analysis are presented in Table 1. The descriptive results from our survey showed that panic buying and plan cancellation were reduced significantly as time progressed (questions 5, 7, 9 and 10); we also observed a more extensive impact on students compared to university staff. COVID-19 closed down the medical school campus. Students were affected in their motivation to study and work when away from campus (questions 17 and 18). While university staff were also significantly concerned about the lack of face-to-face communication in question 19, they were less likely to lose motivation (question 17). Students felt that their performance in school would decline with lack of face-to-face contact with peers (question 19). University staff were less likely to believe their overall work performance would decline without face-to-face interaction. Most importantly, students felt that COVID-19 would negatively impact their medical school education. An important theme we observed was an apparent student concern about institutional communication efforts (questions 12–14). However, this view was not shared by their university staff counterparts. The discrepancy highlights how students’ perceptions and confidence about their medical education is affected dramatically by the degree of effective communication between students and administrators.
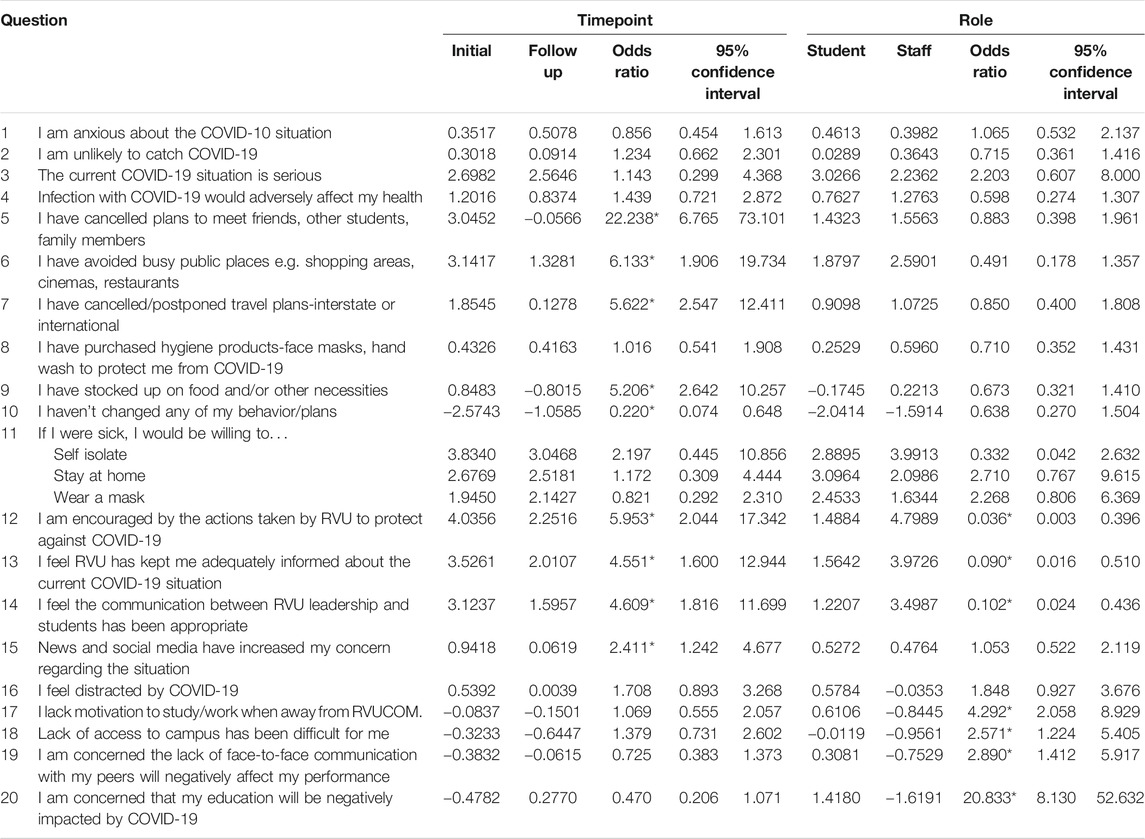
TABLE 1. COVID pandemic survey descriptive data analysis. Total sample included 600 responses, from which 315 were initial and 285 were follow up responses, 343 came from students while 133 came from university staff. Estimates are presented for itemized questions where confidence intervals were estimated using a Bonferroni threshold (0.05/44 = 0.00113636). The total number of responses was 600. Significant tests are labeled with an asterisk (*).
Based on our descriptive analysis of the data, students felt that the communications they received from the institution were not effective in easing their fears and anxieties about education in the COVID-19 era, as compared to university staff (questions 12–14). We suspect the fear that students are experiencing has to do with their belief that they have more at stake than university staff. Students depend on their educational experiences, during both the didactic years and clinical years, to reach the career goals they have invested so much time and money into achieving. University staff mainly worry about job security due to added challenges, whether that means working from home or adapting curriculum. Students will not have the same opportunities to partake in the traditional aspects of medical education, such as in-person anatomy labs using cadavers, regular clinical rotations without significant restrictions, or other hands-on experiences designed to help mold them into competent physicians.
Possible Research Paths
The COVID pandemic has had an important impact on medical education. The development of professional identity in medicine, or “how someone perceives himself as a physician” (Cullum et al., 2020) has traditionally evolved during a student’s time on clinical rotations. Without the opportunity to partake in clinical rotations, students may not form a strong professional identity. With our data, we hope to provide the basis to evaluate anxiety, compliance and perceptions of medical students and university staff as they may be involved in the development of a professional identity. Per Cullum et al. (2020), “a robust professional identity allows physicians to practice with confidence and professionalism”, which are keys to being successful in the field of medicine (Cullum et al., 2020). Interestingly, a study by Choi et al. (2020) refutes the idea that hands-on experiences are necessary to produce confident future physicians. This study found that fourth-year medical students in the United Kingdom felt significantly less prepared to start their medical careers due to disruptions in clinical rotations. However, despite feeling unprepared, many felt confident entering the physician workforce during the COVID-19 pandemic (Choi et al., 2020). Although this shows that medical students are adaptable and ready to fulfill the oath they took to serve their patients, and that university staff are resourceful and creative to bypass the hurdles imposed by this pandemic; it is the responsibility of medical education to ensure that students are properly trained before having to enter the workforce. Having data available, will facilitate an objective evaluation and quantification of the COVID-19 impact. It is imperative that during COVID-19, communications from students’ institutions provide a sense of reassurance to lessen anxieties that students feel about their futures. Further research is required to explore the best way to navigate medical education in uncertain times. Our research is limited to one institution; however, we suspect that medical education will be forever changed and more investigation is needed across multiple institutions to assess the impact of COVID-19. There may need to be a shift in perspective by students and university staff to understand that even during a typical year of medical education, “no medical student will ever feel prepared enough to be a doctor after graduation” (Tan et al., 2020). Improving communications and focusing on reassurance will help students understand that a sense of uncertainty is normal during medical education and is not unique to a pandemic. This sense of reassurance will help them move forward in their careers with an increased level of confidence.
Based on our preliminary descriptive analysis of our exploratory study, the COVID-19 pandemic has greatly impacted medical students, seemingly more so than university staff. The field of medicine has always relied on the ability to learn, adapt, and innovate, and there is no doubt that medical education will continue to evolve during this pandemic. Students are facing increased anxiety, depression, stress, and apprehension about their education and marketability in the future. The anxiety students feel stems from concerns about lost opportunities during both didactic and clinical years and is shared by the university staff who teaches them. Both students and staff fear that they will not be able to be prepared or to provide the preparation that is necessary to our future physicians. It is essential that medical institutions communicate to provide reassurance to university staff and especially to students in an effort to ease anxieties and increase confidence surrounding medical education in the face of COVID-19.
Data Availability Statement
The raw data supporting the conclusions of this article is available at http://dx.doi.org/10.17632/xzwnpjyzwj.1.
Ethics Statement
The studies involving human participants were reviewed and approved by Rocky Vista University IRB. All participants provided their written informed consent to participate in this study.
Author Contributions
RM, MR, ZS and MW conceptualized the research, drafted the survey, collected the data, interpreted findings, wrote, edited and reviewed the manuscript. IZ analyzed, prepared tables, interpreted findings, wrote, edited and reviewed the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge Andrew Fisher and Steven Howell from RVU for their contributions to the development of this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcomm.2021.665314/full#supplementary-material
References
Byrnes, Y. M., Civantos, A. M., Go, B. C., McWilliams, T. L., and Rajasekaran, K. (2020). Effect of the COVID-19 Pandemic on Medical Student Career Perceptions: A National Survey Study. Med. Educ. Online 25, 1798088. doi:10.1080/10872981.2020.1798088
Cai, W., Lian, B., Song, X., Hou, T., Deng, G., and Li, H. (2020). A Cross-Sectional Study on Mental Health Among Health Care Workers during the Outbreak of Corona Virus Disease 2019. Asian J. Psychiatry 51, 102111. doi:10.1016/j.ajp.2020.102111
Choi, B., Jegatheeswaran, L., Minocha, A., Alhilani, M., Nakhoul, M., and Mutengesa, E. (2020). The Impact of the COVID-19 Pandemic on Final Year Medical Students in the United Kingdom: A National Survey. BMC Med. Educ. 20, 206. doi:10.1186/s12909-020-02117-1
Cullum, R. J., Shaughnessy, A., Mayat, N. Y., and Brown, M. E. (2020). Identity in Lockdown: Supporting Primary Care Professional Identity Development in the COVID-19 Generation. Educ. Prim. Care 31, 200–204. doi:10.1080/14739879.2020.1779616
Ferrel, M. N., and Ryan, J. J. (2020). The Impact of COVID-19 on Medical Education. Cureus 12, e7492. doi:10.7759/cureus.7492
Huckins, J. F., DaSilva, A. W., Wang, W., Hedlund, E., Rogers, C., Nepal, S. K., et al. (2020). Mental Health and Behavior During the Early Phases of the COVID-19 Pandemic: A Longitudinal Mobile Smartphone and Ecological Momentary Assessment Study in College Students (Preprint). J. Med. Internet Res. 22, e20185. doi:10.2196/20185
Meo, S. A., Abukhalaf, D. A. A., Alomar, A. A., Sattar, K., and Klonoff, D. C. (2020). COVID-19 Pandemic: Impact of Quarantine on Medical Students' Mental Wellbeing and Learning Behaviors. Pak J. Med. Sci. 36, S43–S48. doi:10.12669/pjms.36.COVID19-S4.2809
Newble, D. I., and Entwistle, N. J. (1986). Learning Styles and Approaches: Implications for Medical Education. Med. Educ. 20, 162–175. doi:10.1111/j.1365-2923.1986.tb01163.x
Papadimos, T. J., Soghoian, S. E., Nanayakkara, P., Singh, S., Miller, A. C., Saddikuti, V., et al. (2020). COVID-19 Blind Spots: A Consensus Statement on the Importance of Competent Political Leadership and the Need for Public Health Cognizance. J. Glob. Infect. Dis. 12, 167–190. doi:10.4103/jgid.jgid_397_20
Rakhmanov, O., Demir, A., and Dane, S. (2020). A Brief Communication: Anxiety and Depression Levels in the Staff of a Nigerian Private University during COVID 19 Pandemic Outbreak. J. Res. Med. Dent. Sci. 8, 118–122.
Rose, S. (2020). Medical Student Education in the Time of COVID-19. Jama 323, 2131–2132. doi:10.1001/jama.2020.5227
Tan, K., Foo, J., Ang, B., Chua, J., and Teo, D. (2020). Perspectives of Medical Students on Local Medical Education during COVID-19. Singapore Med. J. doi:10.11622/smedj.2020105
Temsah, M.-H., Al-Sohime, F., Alamro, N., Al-Eyadhy, A., Al-Hasan, K., Jamal, A., et al. (2020a). The Psychological Impact of COVID-19 Pandemic on Health Care Workers in a MERS-CoV Endemic Country. J. Infect. Public Health 13, 877–882. doi:10.1016/j.jiph.2020.05.021
Temsah, M. H., Alhuzaimi, A. N., Alamro, N., Alrabiaah, A., Al-Sohime, F., Alhasan, K., et al. (2020b). Knowledge, Attitudes and Practices of Healthcare Workers During the Early COVID-19 Pandemic in a Main, Academic Tertiary Care Centre in Saudi Arabia. Epidemiol. Infect. 148, e203. doi:10.1017/S0950268820001958
US Center for Disease Control (2020). Running Essential Errands. Available at: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/essential-goods-services.html (Accessed January 19, 2021).
Keywords: COVID-19, medical students, perception, survey, faculty
Citation: McCann R, Russell M, Sandhu Z, Zapata I and Wardle M (2021) Exploratory Evaluation of Anxiety, Compliance and Perceptions of the COVID-19 Pandemic of Medical Students and Medical University Staff. Front. Commun. 6:665314. doi: 10.3389/fcomm.2021.665314
Received: 07 February 2021; Accepted: 14 July 2021;
Published: 28 July 2021.
Edited by:
Peter Kruyen, Radboud University Nijmegen, NetherlandsReviewed by:
Veronica Velasco, University of Milano-Bicocca, ItalyMonica Zaharie, Babeş-Bolyai University, Romania
Copyright © 2021 McCann, Russell, Sandhu, Zapata and Wardle. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mark Wardle, bXdhcmRsZUBydnUuZWR1
 Rachel McCann
Rachel McCann Mikala Russell
Mikala Russell Zoya Sandhu
Zoya Sandhu Isain Zapata
Isain Zapata Mark Wardle
Mark Wardle