- 1Faculty of Medical Sciences, The University of the West Indies, Cave Hill Campus, Cave Hill, Barbados
- 2Faculty of Medical Sciences, The University of the West Indies, St Augustine Campus, St Augustine, Trinidad and Tobago
Background: Smartphones and medical education apps are popular with and are widely used by medical students to facilitate peer interactions, communication and collaboration in addition to their “learn anywhere” advantage. Smartphone use by medical students has not been studied in the English-speaking Caribbean. Study objectives were to assess in preclinical students attending the University of the West Indies in Barbados, smartphone ownership, usage and attitudes toward use in medical education.
Methods: First and second year preclinical medical students completed a self-administered paper-based questionnaire during the 2018–2019 academic year. Survey questions included sections on smartphone ownership, medical apps used, phone usage for education related tasks, and the perception on the usefulness of smartphones in medical education.
Results: Of 112 participants (response rate 67.4%), 43% considered using the smartphone for medical education when acquiring it but 92% were currently using it for this purpose, with 80.3% (p < 0.01) specifically using it for learning anatomy. The majority of the students felt that the use of smartphones would improve their educational experiences (89.1%) (p < 0.01), be beneficial to medical faculty for teaching (84.8%) (p < 0.01), and could be more effectively used in medical education (50.9%) (p < 0.01). For information resources students used Medscape (67.9%) and Mayo Clinic (57.1%) and the most frequently used search engine was Google (95.5%). Most students (67.9%) used medical apps and 79.5% would buy more useful apps provided they were affordable. The popular apps were: ‘Teach me Anatomy’ (11.9%), ‘UpToDate’ (10.3%) and ‘Medscape’ (8.8%). Most students (66.1%) felt a Smart Campus should ensure e-learning platforms were compatible with smartphones and university policies regarding smartphone usage for academic purposes were needed.
Conclusion: Findings show that smartphones and related medical education apps are widely used by medical students and improve their educational experiences. Universities should develop a policy regarding smartphone usage for academic purposes.
Introduction
Smartphones and medical education apps have become popular and are widely used by medical students because they facilitate peer interactions, communication and collaboration in addition to their “learn anywhere” advantage (Valle et al., 2017). Mobile learning (m-Learning), an extension of e-learning (Ventola, 2014), utilizes mobile devices such as mobile phones, smartphones, personal digital assistants (PDAs), netbooks, tablets, e-readers, and gaming devices (Gavali et al., 2017). Smartphones, a combination of mobile phone and handheld computer, allow web browsing and use of online applications (Apps) (Ventola, 2014). Due to their versatility, educators are integrating smartphone use in curriculum delivery, with an emphasis on the advantages and with amendments to curtail disadvantages (Darko-Adjei, 2019).
It is well-established that learning is most effective and efficient when it is situational (tied to actual activity), continuous, and life-long (Sung et al., 2016; Kim, 2020). Instruction models informed by constructivist theories to integrate mobile technology are widely advocated in higher education settings (Sung et al., 2016). Social media when used for educational activities encourages greater engagement of students in learning and facilitates peer interactions, communication and collaboration (Latif et al., 2019). The concept of situated learning by Lave and Wenger (Lave and Wenger, 1991), emphasizes the need for contextualization of knowledge. Smartphones being portable devices allow ready access to information during clinical encounters (Lave and Wenger, 1991). Knowledge acquired via a smartphone device and its reflection facilitate learning (Davies et al., 2012). Honey and Mumford (2006) classified learning preferences into four broad styles - activists, pragmatists, theorists, and reflectors. The activists learn by doing things (e.g. group discussions and problem-solving), pragmatists learn by practical application of acquired information in the real world (e.g. experiment with theories and ideas), theorists strive to interpret a theory behind any action (e.g. reading stories and quotes), and reflectors learn best by making observations and collecting data (Honey and Mumford, 1992). Taking these learning styles into account can lead to more effective teaching and medical teaching apps can be tailored to the varied learning needs of individuals (Honey and Mumford, 2006). It is suggested that to be successful learning must be based on contemporary practices matching a social-constructivist approach that is active as well as learner, knowledge, assessment and community centered (Shaples, 2016).
The constructivist learning is considered as ‘a holistic approach’ which is purposely tailored to the curricular goals and students’ needs to offer learning experiences related to their personal and professional development (McGrath, 2007). Learners construct their knowledge through a process of active enquiry and engagement and take responsibility for their own learning. Constructivists believe that assessment should be used as a tool to enhance both the student’s learning and the teacher’s understanding of student’s progress i.e. assessment for learning (Rahman and Majumder, 2014). Social constructivists believe in collaborative approach that knowledge is constructed through interaction with others which facilitate life-long learning (Akpan et al., 2020). Information and communication technologies need to integrate with social constructivist approaches in order to assist and facilitate the construction of knowledge. Contemporary learning approaches and e-learning systems need to include cultural and behavioral aspects to integrate pedagogical issues (Louvigne et al., 2018). In traditional teacher-centered classroom teaching, students are passive learners, work primarily alone, and teachers disseminate information to students (Lord, 1999). Teacher’s role is directive, rooted in authority an assessment is focused on through testing and correct answers. Traditional method ignores the students’ psychological level of interest and motivation of the students (Singh et al., 2019). In constructivist learning, ‘interaction is perceived to be one of the most important components of the learning experience’, and ‘students are given sufficient opportunities to express themselves and to share their own experiences with others’ (Alt, 2016).
The increasing use of advanced technologies, especially smartphones (Mohapatra et al., 2015) is reported in the literature (Payne et al., 2012; Wallace et al., 2012). Medical students accept, adapt, and utilize high-quality electronic information resources much more than clinicians (Pedro et al., 2018). Students who use smartphones and medical apps agree that smartphones have a positive effect on their education (Zhao et al., 2018; Maudsley et al., 2019). Moreover, an association between smartphone use and academic performance among medical students is reported in the literature (Craig and Van Lom, 2009; Sheikhtaheri and Kermani, 2018). Many tertiary level medical institutions have implemented m-Learning in order to provide flexibility in learning. For instance Standford University provides students with iPads in place of textbooks (Quant et al., 2016). Smartphone-related medical education apps have also witnessed increased usage among medical students (Zhao et al., 2018), since students find them helpful for their education (Green et al., 2015; Alhazmi et al., 2018). Medical school surveys have shown that approximately 80% of health care professionals and students used their mobile devices for patient care communication (e-mail, telephone and text messages) and 85% reported using them at least once daily for information and time management or communication (Wallace et al., 2012; Ventola 2014). Smartphones offer many advantages including portability, fast access to online information, efficient use of time, flexible communications, applications and access to multimedia resources (Chase et al., 2018). Medical students use smartphones for accessing diverse resources such as learning anatomy, drug information, clinical scoring systems, and eBooks. Increased usage is observed during the transition from preclinical to clinical years (Chase et al., 2018). Clinical students find that with a smarthphone, downtime between clinical activities can be converted into learning opportunities (Chase et al., 2018).
Smartphone use also has limitations which may include superficial learning, use of unreliable information sources, worsened psychological well-being, insomnia, poor sleep quality, anxiety, depression, low self-esteem, higher cognitive distraction, smartphone addiction, poorer academic outcomes and concerns related to privacy and professionalism (Chen et al., 2017; Chase et al., 2018; Loredo e Silva et al., 2018; Maudsley et al., 2019; Goh and Sandars, 2020; Kim, 2020). Medical students are potentially vulnerable to smartphone addiction due to heavy use (Chen et al., 2017; Alhazmi et al., 2018). Loredo e Silva et al. recommend that faculty members “advise and educate their students about conscientious use of this tool to avoid detrimental impact on the learning process” (Loredo e Silva et al., 2018). It is imperative that educational institutions, medical students, and clinicians realize the potential impacts and limitations of m-Learning.
The smart campus, a recent trend in higher education, uses innovative technologies to create a digitally connected campus, thus enhancing the student experience and connecting to a wider audience (Fortes et al., 2019). The Cave Hill Campus of The University of the West Indies (UWI), Barbados undertook a Smart Campus initiative as a part of the major reorientation of the campus’ model of delivering higher education (The University of the West Indies, 2020). There is an ongoing emphasis on smart-learning, through delivery and expansion of online learning using the University’s eLearning Moodle Platform and outfitting the campus to create smart classrooms (UWI, 2020). There are very few publications on smartphone use by undergraduate university students in the Caribbean (Ahmad, 2018; 2019), and to date none on the use by medical students from this region. Against this background, the authors conducted this study to assess the utilization of smartphones and commonly used medical education apps as educational aids by the preclinical medical students of the Faculty of Medical, Sciences (FMS), Cave Hill Campus.
Materials and Methods
A cross-sectional survey was conducted from September 2018 to april 2019 amongst all Year 1 (n = 68) and Year 2 (n = 98) Bachelor of Medicine and Bachelor of Surgery (MBBS) students of FMS, UWI, Cave Hill Campus, Barbados. Ethical approval was obtained from the joint Institutional Review Board of Cave Hill campus and the Ministry of Health (Approval no: 180210-B). Participation was anonymous and voluntary with informed verbal consent. Students who did not give consent or were absent during the survey period were excluded from the study.
A paper-based self-administrated questionnaire developed by Wallace et al. (2012) was adapted for use. Approval to use the instrument was obtained from the authors. The questionnaire was reviewed by the research team and medical educationists and pretested with 15 students to check the clarity, validity, and suitability of the questionnaire. Modifications were done to include the latest development in the field (e.g., the latest iPhone models, WhatsApp communication for smartphone utility, a list of latest medical references to choose from, etc). Survey questions included sections on smartphone ownership, medical apps used, education related tasks the phone was used for, and the perception on the usefulness of the phones in medical education.
The frequency of usage of smartphones for academic and communication purposes was rated on a 6-point Likert scale, ranging from never (a score of 1) to more than once a day (a score of 6). Responses on general use, limitations, and improved future use of smartphones in medical education were rated using a 5-point-Likert scale, ranging from strongly agree (a score of 1) to strongly disagree (a score of 5).
The questionnaire was distributed to students at the end of scheduled lectures, as evidence suggests, it provides a better response rate than with online questionnaires (Wallace et al., 2012), and this allowed for the contents and purpose to be explained by one of the authors (KS). Participants were assured that their responses would be kept strictly confidential. Students were given 20 min to complete the questionnaire.
Statistical Analysis
SPSS version 25.01 was used to analyse data. Data are presented as frequencies and percentages. The Pearson’s Chi-square test was performed to determine the significance of differences in the frequencies of responses.
Results
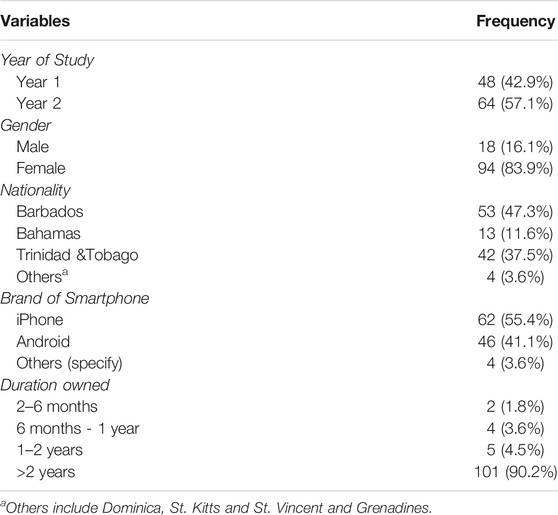
Of 166 eligible students, 112 completed the survey giving a response rate of 67.5% (Table 1). Of the respondents 57.1% were year-2 students, 83.9% female and 47.3% Barbadian. All participants possessed a smartphone. Apple’s iPhone was the most owned brand (55.4%) followed by Google android phones (43.8%). More than 90% had a smartphone for more than 2 years and the mean age of the current smartphone owned was 1.5 years.
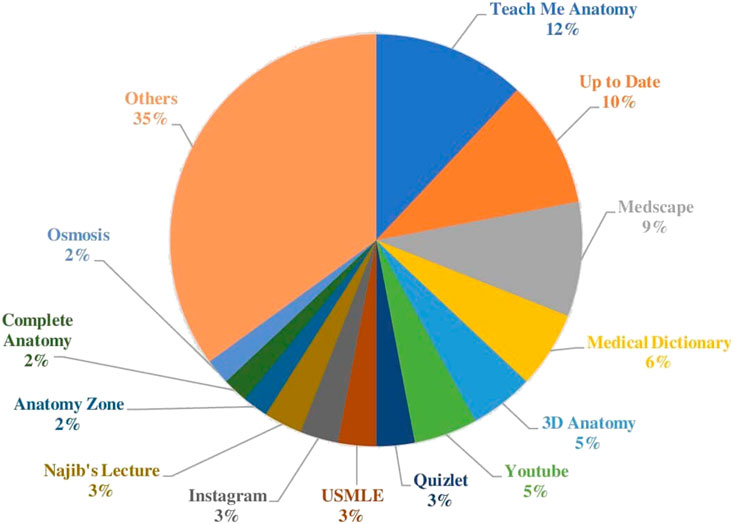
Google (95.5%) was the most popular search engine used by respondents for researching unfamiliar terms or concepts. Medscape (67.9%), and Mayo Clinic (57.1%) were commonly used as information resources. Medical apps were used by 67.9 and 79.5% were willing to buy more useful apps for learning purposes if they were affordable. The most preferred and most often used apps as reported by each student were: ‘Teach me Anatomy’ (11.9%), ‘UpToDate’ (10.3%), and ‘Medscape’ (8.8%) (Figure 1).
Scale used: Never, More than once a month, Once a month, Once a week, Several times a week, Once a day, and More than once a day.
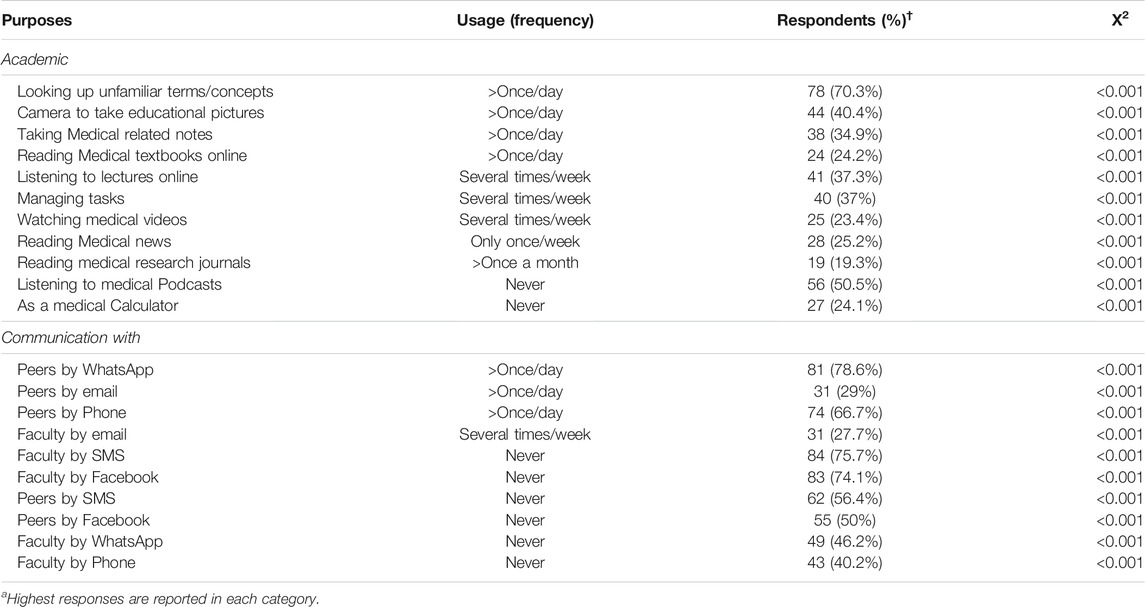
Students utilized smartphones mainly for academic and communication purposes. More than 65% of the students used their smartphone to search the meaning of unfamiliar terms/concepts and communicate with peers by WhatsApp and/or phone. The majority of the students never used smartphones for listening to medical podcasts (50.5%), communicating with faculty by SMS (75.7%) or by Facebook (74.1%), and peers by SMS (56.4%) or Phone (40.2%). All X2 values in Table 2 were found to be statistically significant (p < 0.001).
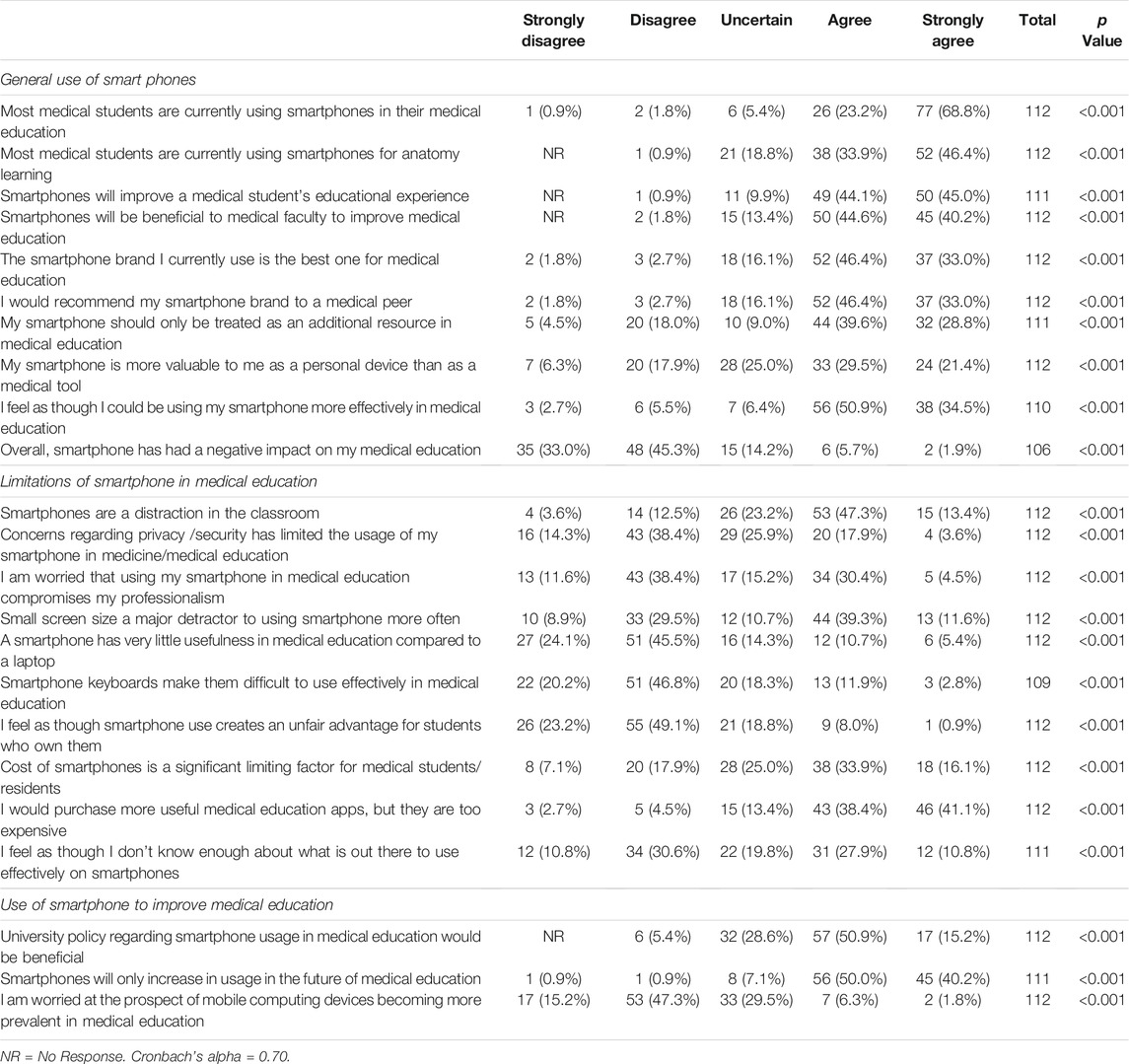
Forty three percent of respondents considered ‘using smartphones in medical education’ when they first bought/received their current smartphones. Ultimately, 92% were now using their smartphone for learning purposes, with 80.3% (p < 0.01) for learning anatomy. The majority of the students felt that the use of smartphones would improve their educational experiences (89.1%), be beneficial to medical faculty for teaching (84.8%), and could be more effectively used in medical education (50.9%) (Table 3). Approximately, three-quarters of the respondents disagreed when asked whether a smartphone has very little usefulness in medical education compared to a laptop. Most students (78.3%) however did not agree that their smartphones had a negative impact on their learning. All X2 values in Table 3 were found to be statistically significant (p < 0.001).
Discussion
The authors report to the best of their knowledge, this is the first study from the English speaking Caribbean, exploring smartphone and medical education apps use as educational aids by preclinical medical students. The study found that all respondents possessed a smartphone and used the device mainly for academic and communication purposes. More than 90% were using a smartphone for learning purposes, 89.1% said that it improved the educational experience and 80.3% used it for anatomy. Apple’s iPhone was found to be the most owned smartphone brand; Google, the most widely used search engine; and Medscape and Mayo Clinic were commonly used educational resources. Among the medical education apps, ‘Teach me Anatomy’ and ‘UpToDate’ were mostly used. Students recommended that the university should adopt online learning platforms for mobile learning and a policy should be put in place for better learning experiences.
The response rate in this study was 67.5% which is similar to a study conducted among the medical students in India (Rohilla et al., 2016). This may be due to the use of an in-person paper-based questionnaire for the collection of responses. However, it was higher than a study conducted amongst medical students, residents and faculty in Canada (14%) (Wallace et al., 2012) and Australia (32.3%) (Wynter et al., 2019) who used online questionnaires. Online surveys particularly recorded low responses in most published studies due to ‘non-response’ and ‘voluntary response’ biases (Payne et al., 2012) or ‘survey fatigue’ (Ahmad, 2019). To improve the survey response rate in medical education, Brown and Watson suggested using the ‘captive audience’ technique supported by technology devices (e.g. iPad) online survey tools (e.g. Survey Monkey) (Brown and Watson, 2016).
In our study all students owned a smartphone with over half owning iPhones. The mean age of the phones was one and a half years and approximately three-quarters used medical apps on their phones. In other studies the phones used by medical students were older, being on average 4 years old or more (Gavali et al., 2017; Chase et al., 2018; Clarke et al., 2019) and medical apps usage was similar (Payne et al., 2012; Latif et al., 2019). Previous surveys report that smartphones and medical apps were a great help to medical students (Brown and Watson, 2016; Alhazmi et al., 2018; Loredo e Silva et al., 2018; Sheikhtaheri and Kermani, 2018).
Smartphones are primarily used for information management in medical education, communication and time management (Mohapatra et al., 2015). The top two uses of smartphones in our study were for communicating with peers by WhatsApp (78.6%) and looking up unfamiliar terms and concepts (70.3%) greater than once a day. Half of the students (50.9%) valued their smartphone more as a personal device than as a medical education tool. It has been found elsewhere that even when smartphones are initially acquired for personal use, their usefulness for study purposes is recognized with time (Latif et al., 2019). Ifeanyi and Chukwuere (2018) reported that smartphone usage fostered better communication between students and tutors but many of our students reported that they do not use their phone to communicate with tutors. Smartphones aid the discussion of concepts with colleagues, sharing facts and illustrations, downloading of study materials including lecture slides, doing assignments and recording of lectures (Ifeanyi and Chukwuere, 2018). A study investigating student preparedness for mobile learning found that smartphones allow better interaction between students and instructors in comparison to face-to-face learning (Corbeil and Valdes-Corbeil, 2007; Kim, 2020). Other studies report that smartphones help students learn at their own pace, retrieve up-to-date information for their assignments without the need to physically visit the library and facilitate reading ahead of class (Corbeil and Valdes-Corbeil, 2007; Subhash and Bapurao, 2015). There are encouraging reports of effective delivery of distance education courses via smartphones with students accessing lecture materials on their phones and interacting with their lecturers (Kim 2020). This is particularly relevant to the current COVID-19 pandemic with the shift to teaching online (Cecilio-Fernandes et al., 2020; Gaur et al., 2020; Goh and Sandars, 2020; Majumder, 2020; Singh et al., 2020).
Medscape and Mayo Clinic were frequently used as information resources in this study while Google was the most frequently used search engine. Studies have found that Medscape (Venkatesh et al., 2017; Smalls et al., 2019), Wikipedia and Google (Ventola, 2014) are the most commonly used and easily accessible reference sources for the medical community. Many default to Google search results due to the usefullness and to avoid the time required logging into library licensed resources or downloading an app (Wang et al., 2012). Most information resources listed by our students were free with easily downloadable apps.
The focus of mobile technology has shifted to “Apps” (Masters et al., 2016). Most students in our study used medical apps (67.9%). The most preferred and most often used apps as reported by each student were ‘Teach me Anatomy’ followed by ‘UpToDate’ and ‘Medscape’ (Figure 1). However, 35% (others) represented a long tail of less frequently used apps which were only mentioned once or twice (Figure 1). Variations in the use of apps has been reported. Medical students prefer drug handbook and medical book apps in the UK, guidelines and dictionary in the United States of America (Golenhofen et al., 2020), Medical Dictionary and Medscape apps in India (Gavali et al., 2017) and UpToDate and PubSearch in Iran (Jebraeily et al., 2017). The usage of anatomy apps was very popular among students (80.3%), as supported by previous studies (Pedro et al., 2018; Pires et al., 2018; Golenhofen et al., 2020). Usage of anatomy apps have been associated with lower failure rates and better exam grades (Golenhofen et al., 2020). However, students expressed the following concerns in using apps for learning and assessment: superficial learning, lack of reliability and accuracy, quality and safety, security and privacy of patient information, medical apps not being developed by professionals appropriately trained in medical education, lack of accreditation of medical apps by recognized health institutions, lack of support and update of apps by their developers, and lack of easy usability of applications (Kim, 2020) (Masters et al., 2016; Jebraeily et al., 2017).
This study showed that WhatsApp or phone calls were the common daily modes of communication with peers and faculty. Studies confirmed that WhatsApp’s online group discussions may provide students with a one-point learning and information source (Latif et al., 2019). Current research highlighted WhatsApp can be effective as a medical learning tool (Salam et al., 2021) to facilitate classroom learning and clinical training (Coleman and O'Connor, 2019). Similarly, instant messaging applications can improve “the way medical education is delivered, by creating communication channels between students and tutors, increasing learning opportunities and providing an overall superior educational experience for medical students” (Coleman and O'Connor, 2019). However, there are reports of adverse effects on academic performance with the use of applications such as WhatsApp, Facebook, and games being addictive and stealing students’ study time (Salam et al., 2021). Thus, smartphone learning also has challenges (Kim, 2020) along with its many benefits, indicative of its effect on academic performance (Ifeanyi and Chukwuere, 2018; Darko-Adjei, 2019).
Smart devices used in smart campuses significantly impact student learning, the most remarkable being significant cost savings and a direct impact in improving student learning (Ahmad, 2018). Smart campuses should have a clear policy to integrate online learning in the curriculum with adequate technology support which was also recommended by the students. Medical educators and policymakers should also take necessary measures to improve the quality of online learning and assessment as the use of emergent technology is likely to continue as an indispensable component of post-COVID medical education (Majumder et al., 2021).
Limitations
The present study has notable limitations. This cross-sectional study involved only Year one and Year two students and had a small sample size; therefore, caution needs to be taken to generalize the data to other settings. Another limitation is of using ‘captive audience’, there is a possibility that respondents felt coerced to participate and so it is less likely that they answered questions honestly. Lastly, this survey looked at only preclinical medical students, therefore does not represent the current practices or needs of clinical or other health science disciplines.
Conclusion
Our study shows that smartphones and related medical education apps are widely used by medical students and majority of the students felt that the use of smartphones would improve their educational experiences, be beneficial to medical faculty for teaching, and could be more effectively used in medical education. Medical schools should take appropriate measures to guide and educate students on the effective use of smartphones and medical apps for learning purposes. Universities should make e-learning platforms compatible with smartphones and develop a policy regarding smartphone usage for academic purposes.
Future Directions
Smartphone learning fosters discussion, communication and collaboration, and assures better student engagement. The millennial learners prefer student-centered, active, and self-directed learning. Smartphone learning has shifted the location of education settings outside of classrooms, demanding a suitable shift in delivery methods. Mobile learning can be integrated into medical education to assess its effectiveness; learning materials should be in a digital format as far as possible to fuel smartphone learning and online education in smart campuses. A faculty guided approach in the selection of suitable and cost-effective medical education apps can be adopted. Universities should have ongoing teaching and learning programs for educators to develop, collaborative, communication-based, interactive, new online teaching skills and assessment methods, thus, shifting the role of educators to facilitators. Smart campuses must develop internet-based, smartphone-compatible learning platforms. Universities should develop policies for staff and students regarding smartphone usage for academic purposes (The University of the West Indies, 2018).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB), UWI, Cave Hill/Barbados Ministry of Health Research Ethics Committee (Approval no: 180210-B). The participants provided their written informed consent to participate in this study.
Author Contributions
KS and MAAM conceived and designed the study and led data collection. All authors (BS, MAAM, KS, OPA, SS, UG, and SG) were involved in analyzing and interpreting the data. The manuscript was drafted by MAAM and KS with notable input from SS, OPA, BS, and SG. All authors reviewed and approved the final version and have agreed to be accountable for all aspects of the work including any issues related to accuracy or integrity. The manuscript has been read and approved by all the authors and authorship has been determined based on ICJME guidelines.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors wish to thank the students who consented to participate in the Smartphone study and gave their valuable opinion. The authors extend their gratitude to Professor R. Clive Landis (Pro Vice-Chancellor and Principal, The University of the West Indies, Cave Hill Campus, Barbados) for providing his valuable advice during manuscript writing and journal selection, Professor Simon Anderson (Director, George Alleyne Chronic Diseases Research Centre, GACDRC, and Professor of Population Health Sciences, Faculty of Medical Sciences, UWI Cave Hill Campus, Barbados) for critical review of the manuscript and Professor Ian Hambleton (Professor of Biostatistics at the George Alleyne Chronic disease Research Centre, GACDRC) for his inputs and expert advice during the preparation of this manuscript and statistical analysis. The authors are grateful to the team of the Author Fellowship Programme at the UWI Cave Hill Campus, Barbados for their support and guidance.
Abbreviations
UWI, The University of the West Indies; COVID-19, Corona Virus disease 2019; PDA, Personal Digital Assistants; FMS, Faculty of Medical Sciences; MBBS, Bachelor of Medicine and Bachelor of Surgery; IRB, Institutional Review Board; CARICOM, Caribbean Community and Common Market
References
Ahmad, T. (2018). Mobile Phones as a Learning Tool: A Lecturer’s Viewpoint. Society and Business Review 13 (3), 132–138. doi:10.1108/SBR-03-2018-0021
Ahmad, T. (2019). Undergraduate mobile Phone Use in the Caribbean. J. Res. Innovative Teach. Learn. 13 (2), 191–210. doi:10.1108/jrit-01-2019-0001
Akpan, V. I. I. A., Mpamah, I. B. I., and Okoro, C. O. (2020). Social Constructivism: Implications on Teaching and Learning. Br. J. Edu. 8, 49–56.
Alhazmi, A. A., Alzahrani, S. H., Baig, M., Salawati, E. M., and Alkatheri, A. (2018). Prevalence and Factors Associated with Smartphone Addiction Among Medical Students at king Abdulaziz university, Jeddah. Pak J. Med. Sci. 34 (4), 984–988. doi:10.12669/pjms.344.15294
Alt, D. (2016). Contemporary Constructivist Practices in Higher Education Settings and Academic Motivational Factors. Aust. J. Adult Learn. 56, 374–399.
Brown, C., and Watson, W. (2016). Techniques for Improving Survey Response Rates in Medical Education. Med. Teach. 38(6):634. doi:10.3109/0142159x.2016.1170787
Cecilio-Fernandes, D., Parisi, M. C. R., Santos, T. M., and Sandars, J. (2020). The Covid-19 Pandemic and the challenge of Using Technology for Medical Education in Low and Middle Income Countries. MedEdPublish 9. doi:10.15694/mep.2020.000074.1
Chase, T. J. G., Julius, A., Chandan, J. S., Powell, E., Hall, C. S., Phillips, B. L., et al. (2018). Mobile Learning in Medicine: An Evaluation of Attitudes and Behaviours of Medical Students. BMC Med. Educ. 18 (1), 152. doi:10.1186/s12909-018-1264-5
Chen, B., Liu, F., Ding, S., Ying, X., Wang, L., and Wen, Y. (2017). Gender Differences in Factors Associated with Smartphone Addiction: A Cross-Sectional Study Among Medical College Students. BMC psychiatry 17 (1), 341. doi:10.1186/s12888-017-1503-z
Clarke, E., Burns, J., Bruen, C., Crehan, M., Smyth, E., and Pawlikowska, T. (2019). The 'connectaholic' behind the Curtain: Medical Student Use of Computer Devices in the Clinical Setting and the Influence of Patients. BMC Med. Educ. 19 (1), 376. doi:10.1186/s12909-019-1811-8
Coleman, E., and O’Connor, E. (2019). The Role of WhatsApp in Medical Education; a Scoping Review and Instructional Design Model. BMC Med. Educ. 19 (1), 279. doi:10.1186/s12909-019-1706-8
Corbeil, J. R., and Valdes-Corbeil, M. E. (2007). Are You Ready for mobile Learning. Educause Q. 30 (2), 51.
Craig, T., and Van Lom, M. (2009). “Impact Constructivist Learning Theory and Mobile Technology Integration,” in Theories of Educational Technology. Editor K. Rice. Available at: https://sites.google.com/a/boisestate.edu/edtech theories/craig_and_vanlom.
Darko-Adjei, N. (2019). The Use and Effect of Smartphones in Students' Learning Activities. Legon: Evidence from the University of Ghana.
Davies, B. S., Rafique, J., Vincent, T. R., Fairclough, J., Packer, M. H., Vincent, R., et al. (2012). Mobile Medical Education (MoMEd) - How mobile Information Resources Contribute to Learning for Undergraduate Clinical Students - a Mixed Methods Study. BMC Med. Educ. 12 (1), 1–11. doi:10.1186/1472-6920-12-1
Fortes, S., Santoyo-Ramón, J., Palacios, D., Baena, E., Mora-García, R., Medina, M., et al. (2019). The Campus as a Smart City: University of Málaga Environmental, Learning, and Research Approaches. Sensors 19 (6), 1349. doi:10.3390/s19061349
Gaur, U., Majumder, M. A. A., Sa, B., Sarkar, S., Williams, A., and Singh, K. (2020). Challenges and Opportunities of Preclinical Medical Education: Covid-19 Crisis and Beyond. Compr. Clin. Med. 2, 1992–1997. doi:10.1007/s42399-020-00528-1
Gavali, M. Y., Khismatrao, D. S., Gavali, Y. V., and Patil, K. B. (2017). Smartphone, the New Learning Aid Amongst Medical Students. J. Clin. Diagn. Res. 11 (5), JC05–JC08. doi:10.7860/JCDR/2017/20948.9826
Goh, P-S., and Sandars, J. (2020). A Vision of the Use of Technology in Medical Education after the Covid-19 Pandemic. MedEdPublish 9 (1), 49. doi:10.15694/mep.2020.000049.1
Golenhofen, N., Heindl, F., Grab‐Kroll, C., Messerer, D. A. C., Böckers, T. M., and Böckers, A. (2020). The Use of a mobile Learning Tool by Medical Students in Undergraduate Anatomy and its Effects on Assessment Outcomes. Anat. Sci. Educ. 13 (1), 8–18. doi:10.1002/ase.1878
Green, B. L., Kennedy, I., Hassanzadeh, H., Sharma, S., Frith, G., and Darling, J. C. (2015). A Semi-quantitative and Thematic Analysis of Medical Student Attitudes towards M-Learning. J. Eval. Clin. Pract. 21 (5), 925–930. doi:10.1111/jep.12400
Honey, P., and Mumford, A. (2006). The Learning Styles Helper’s Guide. Peter Honey Publications Limited, Harlow, England.
Honey, P., and Mumford, A. (1992). The Manual of Learning Styles. Berkshire: Peter Honey Publications.
Ifeanyi, I. P., and Chukwuere, J. E. (2018). The Impact of Using Smartphones on the Academic Performance of Undergraduate Students. Knowledge Manag. E-Learning 10 (3), 290–308. doi:10.34105/j.kmel.2018.10.017
Jebraeily, M., Fazlollahi, Z., and Rahimi, B. (2017). The Most Common Smartphone Applications Used by Medical Students and Barriers of Using Them. Acta Inform. Med. 25 (4), 232. doi:10.5455/aim.2017.25.232-235
Kim, C. (2020). Debating the Role of Smartphones and mobile Applications in Medical Education. Biomed. J. Scientific Tech. Res. 26 (5), 20314–20320. doi:10.26717/bjstr.2020.26.004420
Latif, M., Hussain, I., Saeed, R., Qureshi, M., and Maqsood, U. (2019). Use of Smart Phones and Social media in Medical Education: Trends, Advantages, Challenges and Barriers. Acta Inform. Med. 27 (2), 133–138. doi:10.5455/aim.2019.27.133-138
Lave, J., and Wenger, E. (1991). Situated Learning in Communities of Practice. Cambridge University, Cambridge, United Kingdom.
Lord, T. R. (1999). A Comparison between Traditional and Constructivist Teaching in Environmental Science. J. Environ. Edu. 30 (3), 22–27.
Loredo e Silva, M. P., de Souza Matos, B. D., da Silva Ezequiel, O., Lucchetti, A. L. G., and Lucchetti, G. (2018). The Use of Smartphones in Different Phases of Medical School and its Relationship to Internet Addiction and Learning Approaches. J. Med. Syst. 42 (6), 106. doi:10.1007/s10916-018-0958-x
Louvigne, S. U. M., Kato, Y., and Ishii, T. (2018). Social Constructivist Approach of Motivation: Social media Messages Recommendation System. Behaviormetrika 45 (1), 133–155.
Majumder, M. A. A. (2020). Covid-19 Pandemic: Medical Education Is Clinging on a Knife's Edge!. Adv. Hum. Biol. 10 (3), 83. doi:10.4103/aihb.aihb_88_20
Majumder, M. A. A., Cohall, D., Ojeh, N., Campbell, M. H., Adams, O. P., Sa, B., et al. (2021). Assessing Online Learning Readiness and Perceived Stress Among First Year Medical Students during Covid-19 Pandemic: A Multi-Country Study. Can. Med. Educ. J. 12 (2), e131–e133. doi:10.36834/cmej.71609
Masters, K., Ellaway, R. H., Topps, D., Archibald, D., and Hogue, R. J. (2016). Mobile Technologies in Medical Education: Amee Guide No. 105. Med. Teach. 38 (6), 537–549. doi:10.3109/0142159x.2016.1141190
Maudsley, G., Taylor, D., Allam, O., Garner, J., Calinici, T., and Linkman, K. (2019). A Best Evidence Medical Education (Beme) Systematic Review of: What Works Best for Health Professions Students Using mobile (Hand-held) Devices for Educational Support on Clinical Placements? Beme Guide No. 52. Med. Teach. 41 (2), 125–140. doi:10.1080/0142159x.2018.1508829
McGrath, D-L. (2007). Implementing an Holistic Approach in Vocational Education and Training. Aust. J. Adult Learn. 47, 228–244.
Mohapatra, D., Mohapatra, M., Chittoria, R., Friji, M., and Kumar, S. (2015). The Scope of mobile Devices in Health Care and Medical Education. Int. J. Adv. Med. Health Res. 2 (1), 3. doi:10.4103/2349-4220.159113
Payne, K. F. B., Wharrad, H., and Watts, K. (2012). Smartphone and Medical Related App Use Among Medical Students and Junior Doctors in the united kingdom (uk): A Regional Survey. BMC Med. Inform. Decis. Mak 12 (1), 121. doi:10.1186/1472-6947-12-121
Pedro, L. F. M. G., Barbosa, C. M. M. d. O., and Santos, C. M. d. N. (2018). A Critical Review of mobile Learning Integration in Formal Educational Contexts. Int. J. Educ. Technol. High Educ. 15 (1), 10. doi:10.1186/s41239-018-0091-4
Pires, L., de Oliveira Leite, T., Fonseca Junior, A., Babinski, M., and Chagas, C. (2018). Anatomical Apps and Smartphones: A Pilot Study with 100 Graduation Students. SM J. Clin. Anat. 2 (1), 1007.
Quant, C., Altieri, L., Torres, J., and Craft, N. (2016). The Self-Perception and Usage of Medical Apps Amongst Medical Students in the United States: A Cross-Sectional Survey. Int. J. Telemed. Appl. 2016. doi:10.1155/2016/3929741
Rahman, S., and Majumder, M. A. A. (2014). Is it Assessment of Learning or Assessment for Learning? South East Asia. J. Public Health 4 (1), 72–74.
Rohilla, R., Rohilla, J., Rohilla, A., and Singh, K. (2016). Academic Use and Attitude of the 1styear Medical Students toward Smartphones in a North Indian City. Digit Med. 2 (1), 13. doi:10.4103/2226-8561.182293
Salam, M. A. u., Oyekwe, G. C., Ghani, S. A., and Choudhury, R. I. (2021). How Can WhatsApp Facilitate the Future of Medical Education and Clinical Practice. BMC Med. Educ. 21 (1), 54. doi:10.1186/s12909-020-02440-7
Shaples, M. T. J. V. G. (2016). A Theory of Learning for the mobile Age the Sage Handbook of E-Learning Research. 2nd. SAGE. 63–81.
Sheikhtaheri, A., and Kermani, F. (2018). Use of mobile Apps Among Medical and Nursing Students in Iran. Stud. Health Technol. Inform. 248, 33–39. doi:10.3233/978-1-61499-858-7-33
Singh, K., Gaur, U., Hall, K., Mascoll, K., Cohall, D., and Majumder, M. A. A. (2020). Teaching Anatomy and Dissection in an Era of Social Distancing and Remote Learning. Adv. Hum. Biol. 10 (3), 90.
Singh, K., Bharatha, A., Sa, B., Adams, O. P., and Majumder, M. A. A. (2019). Teaching Anatomy Using an Active and Engaging Learning Strategy. BMC Med. Educ. 19 (1), 149. doi:10.1186/s12909-019-1590-2
Smalls, D., Akaeme, O., Hailemeskel, B., and Maneno, M. (2019). Availability of Various Categories of Drug-Related Infor-Mation Among Free Drug Databases: Survey of First Professional Year Students. Int. J. Pharma Care Health IJPCH 103, 10.
Subhash, T. S., and Bapurao, T. S. (2015). Perception of Medical Students for Utility of mobile Technology Use in Medical Education. Int. J. Med. Public Health 5 (4), 305–311.
Sung, Y.-T., Chang, K.-E., and Liu, T.-C. (2016). The Effects of Integrating mobile Devices with Teaching and Learning on Students' Learning Performance: A Meta-Analysis and Research Synthesis. Comput. Edu. 94, 252–275. doi:10.1016/j.compedu.2015.11.008
The University of the West Indies (2018). Academia in Action. The UWI at 70: The Next Phase. Mona, Jamaica: The University of the West Indies.
The University of the West Indies (2020). Triple a Strategy 2017-2022. Available at: https://www.uwi.edu/uop/sites/uop/files/Booklet.pdf.
Valle, J., Godby, T., Paul, D. P., Smith, H., and Coustasse, A. (2017). Use of Smartphones for Clinical and Medical Education. Health Care Manag. 36 (3), 293–300. doi:10.1097/hcm.0000000000000176
Venkatesh, S., Chandrasekaran, V., Dhandapany, G., Palanisamy, S., and Sadagopan, S. (2017). A Survey on Internet Usage and Online Learning Behaviour Among Medical Undergraduates. Postgrad. Med. J. 93 (1099), 275–279. doi:10.1136/postgradmedj-2016-134164
Ventola, C. L. (2014). Mobile Devices and Apps for Health Care Professionals: Uses and Benefits. P T 39 (5), 356–364.
Wallace, S., Clark, M., and White, J. (2012). 'It's on My iPhone': Attitudes to the Use of mobile Computing Devices in Medical Education, a Mixed-Methods Study. BMJ open 2 (4). doi:10.1136/bmjopen-2012-001099
Wang, L., Wang, J., Wang, M., Li, Y., Liang, Y., and Xu, D. (2012). Using Internet Search Engines to Obtain Medical Information: A Comparative Study. J. Med. Internet Res. 14 (3), e74. doi:10.2196/jmir.1943
Wynter, L., Burgess, A., Kalman, E., Heron, J. E., and Bleasel, J. (2019). Medical Students: What Educational Resources Are They Using. BMC Med. Educ. 19 (1), 36. doi:10.1186/s12909-019-1462-9
Keywords: smartphones, medical education apps, medical education, smart campus, Barbados
Citation: Singh K, Sarkar S, Gaur U, Gupta S, Adams OP, Sa B and Majumder MAA (2021) Smartphones and Educational Apps Use Among Medical Students of a Smart University Campus. Front. Commun. 6:649102. doi: 10.3389/fcomm.2021.649102
Received: 03 January 2021; Accepted: 04 October 2021;
Published: 02 November 2021.
Edited by:
Vinita Agarwal, Salisbury University, United StatesReviewed by:
Heloise Pieterse, Council for Scientific and Industrial Research (CSIR), South AfricaJennifer K. Ptacek, University of Dayton, United States
Copyright © 2021 Singh, Sarkar, Gaur, Gupta, Adams, Sa and Majumder. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. A. A. Majumder, YXppbS5tYWp1bWRlckBjYXZlaGlsbC51d2kuZWR1
 K. Singh
K. Singh S. Sarkar1
S. Sarkar1 O. P. Adams
O. P. Adams B. Sa
B. Sa M. A. A. Majumder
M. A. A. Majumder