- 1A.Q. Miller School of Journalism and Mass Communications, Kansas State University, Manhattan, KS, USA
- 2Food, Nutrition, Dietetics and Health, Kansas State University, Manhattan, KS, USA
- 3Health and Nutritional Sciences, South Dakota State University, Brookings, SD, USA
- 4College of Food, Agricultural and Environmental Sciences, Ohio State University, Bowling Green, OH, USA
- 5Department of Food Science & Technology, University of Georgia, Griffin, GA, USA
Background: Self-efficacy is a crucial component in effective health communication and health promotion interventions and serves as a moderator for behavior change. Although awareness and risk perception are important in the behavior change process, self-efficacy gives people the necessary confidence in their ability to engage in advocated health behaviors. In addressing childhood obesity, self-efficacy plays a crucial role in dietary decisions. Informed by the social cognitive theory, this study examines the personal and environmental factors that determine self-efficacy for healthy food choices and healthy eating among adolescents in low-income communities.
Methods: A survey was administered among adolescents in sixth to eighth grades from three U.S. States – Kansas, Ohio, and South Dakota (N = 410).
Results: Results show a correlation between efficacy for healthy food choice and the adolescent’s perceptions of behavioral control or sense of empowerment. Attitudes toward overall health predict efficacy for healthy eating and for healthy food choice. Other predictors for healthy eating include perceptions of peers’ health concerns and perceptions on healthy food availability, whereas perceived control influences efficacy for healthy food choice. Gender played a significant role in adolescents’ perceptions of peers’ health concerns, whereas geographical location/state played a role in their in adolescents’ attitudes toward health. Ethnicity was a more significant factor in their perceived barriers for healthy eating, and perceptions for healthy food availability and in attitudes toward health.
Conclusion: The study suggests ethnic-specific nutrition education that focuses on attitudes toward health and community partnerships that would support a healthy food environment to enhance self-efficacy and healthy dietary behaviors among adolescents.
Self-efficacy, which is gained through knowledge, understanding, and skills development, is a crucial component in effective health communication and disease prevention interventions. Defined as the belief that one can perform a specified behavior in a specific situation (Bandura, 1998), self-efficacy has been exonerated as one of the prerequisites for behavior change and maintenance of newly adopted behavior. It gives those at health risk the confidence in their ability to exert personal control and the conviction of being able to master specific activities, situations, or aspects of his or her own psychological and social functioning (Bas and Donmez, 2009). In public health promotion and disease prevention, awareness and risk perception are important, but self-efficacy gives people the necessary confidence in their ability to engage in advocated health behaviors.
Childhood obesity is one of the serious public health problems in the U.S. where self-efficacy is critical. About one-third of all children and adolescents were categorized as overweight or obese in 2010, an increase in prevalence from 15% in the 1970s to 30% in overweight and from 5% to almost 17% in obesity in the same time frame (Ogden et al., 2012). Racial and ethnic subgroups are disproportionately burdened, with Hispanic children accounting for 25% of obesity compared to Caucasian children (19%) and African-American children (19%) (Crespo et al., 2012; Wang et al., 2012). This high prevalence mandates identification of customized and effective interventions to address the associated health disparities (Kumanyika et al., 2008).
The rapid rise in obesity across age groups has created a need to identify effective prevention interventions that would address inappropriate weight gain (Ogden et al., 2012) while motivating change in risky behaviors and lifestyles among vulnerable populations. Scholars have advocated for knowledge transition and knowledge sharing in nutrition education and communication (Gavaravarapu, 2013) to increase understanding of health risks while promoting behavior change. There are, however, limited, well-established, and long-term nutrition education interventions that focus on adolescents. In a systematic review of existing literature on programs that focus on childhood obesity, Sharma (2006) found 11 studies that focused on school-based interventions in the U.S. and the UK, and only 3 of them targeted adolescents. The key finding indicates that low-income communities have become more vulnerable to increases in obesity and schools have become important avenues for delivery of prevention programs.
Role of Health Communication in Behavior Change
As a fast-growing discipline, health communication seeks to inform, educate target populations about health risks, increase risk perception, motivate behavior change, and demonstrate the benefits of newly adopted behavior or lifestyles. This is achieved through the use of various strategies that lead to effective health decision-making among individuals, institutions, and communities to improve and enhance people’s quality of life (U.S. Department of Health and Human Services, 2008; Ahmed and Bates, 2013). A key element in health communication interventions is careful segmentation of the target audience, which is necessary in messages tailoring (Atkin and Rice, 2013). This segmentation is particularly important in strategic communication where programs target vulnerable groups with culturally appropriate health campaigns (Kreps and Sparks, 2008).
In addressing childhood obesity and related health problems, health communication has been a key focus in recent studies. Extant literature has specifically underscored the role of nutritionists and dietitians in communicating and interpreting nutritional sciences in the language and lifestyles of people to benefit their health, which includes communication activities such as counseling, consultation, teaching, and community outreach (Gavaravarapu, 2013). Government-sponsored media health campaigns have also been implemented at a national level to address childhood obesity across the U.S. states with the goal of creating awareness and providing nutrition knowledge and motivation for healthier dietary and physical activity behaviors (Andrews et al., 2009).
Despite such communication efforts, a persistent gap exists between risk perception and adoption of self-protective behavior, which continues to attract researchers’ attention (Rimal, 2001). In obesity-related interventions, suggestions have been made to focus on self-efficacy in weight management as a better estimate for effectiveness in behavior change, especially for the obese population, and this would include incorporating self-regulatory strategies into their daily program to enhance self-efficacy (Bas and Donmez, 2009). Gavaravarapu et al. (2015) have identified three adolescent traits, namely, responsive, avoidance, and indifference that may be useful in developing nutrition communication programs. This article examines self-efficacy for healthy food choice and eating among adolescents. It is drawn from a tristate school-based project entitled “Ignite: Sparking Youth to Create Healthy Communities,” which focuses on obesity reduction among adolescents in middle school, grades six through eight, in low-income communities (Kumar et al., 2014, 2016; Comstock et al., 2016; Kidd et al., 2016).
Self-Efficacy and Behavior Change
The role self-efficacy plays in health care and as a reliable predictor of behavior change for better health outcomes has been evidenced in many studies [e.g., Bandura (1977, 2004), Janz and Becker (1984), Rimal (2001), Schwarzer and Luszczynska (2006), and Rutkowski and Connelly (2012)]. Self-efficacy is a key component in Bandura’s social cognitive theory that posits a causal relationship where personal, behavioral, and environmental determinants interact with each other in predicting health risks and behaviors (Bandura, 1986). Personal factors include knowledge, values, beliefs, attitudes, and self-efficacy that relates to a certain behavior. Research shows health knowledge and behavior to be moderately correlated, whereas self-efficacy, involvement, and interpersonal communication are moderating variables in the behavior change process (Rimal, 2001). In Bandura’s theory, self-efficacy beliefs operate together with knowledge of health risks, goals, outcome expectations, and perceived environmental impediments and facilitators in the regulation of human motivation, behavior, and well-being (Bandura, 2004).
Self-efficacy beliefs define an individual’s capacity to carry out actions and make decisions that are part of success in progressing to positive outcomes, and therefore, beliefs influence motivation, affect, and behavior (Bandura, 1977). Efficacious people who also tend to be optimistic about performing behaviors, rather than focusing on negative thoughts about their inability to achieve a goal (Turner et al., 2006), are more likely to take on challenges easily, have a greater sense of commitment, and cope better with unexpected events or disappointment (Bandura, 1994). On the contrary, non-efficacious people will avoid challenges and fail at tasks perceived to be beyond their abilities, and they have little incentive to act or to persevere in the face of difficulties (Caprara et al., 1998). As Bandura argues, self-efficacy is concerned on the belief that one can do with what he or she has under a variety of circumstances and therefore makes a difference in how people feel, think, and act (Caprara et al., 1998). For instance, in a food desert environment where healthy foods are not readily available or in obesogenic environments, target populations must believe that they can adopt and maintain a healthier diet and lifestyle to reduce childhood obesity.
Studies have reported an association between weight-related self-efficacy and the completion of behavioral weight-loss programs (Bas and Donmez, 2009). There is also evidence on the role of self-efficacy in preventing risk-taking behavior in general among adolescents. For example, self-efficacy has been found to be a significant factor in preventing HIV/AIDS among female adolescents, especially in refusing sexual intercourse, increasing condom use and questioning potential sexual partners (Lee et al., 2016), and preventing alcohol and drug use (Coffman et al., 2011), whereas low self-efficacy has been associated with lower adherence to diabetes regimen among adolescents (Littlefield et al., 1992).
Self-Efficacy in Obesity Reduction among Adolescents
Adolescence is a time of rapid growth and development with biological, psychosocial, and emotional changes, and this places increased nutritional demands on adolescents that lead to engaging in dietary behaviors that may contribute to nutritional deficits (Spear, 2002; Jenkins and Horner, 2005). For instance, during adolescence, there is an increase in the consumption of energy-dense foods that are high in fat, a decrease in the consumption of fruits, vegetables, and calcium-rich foods, and an increase in skipping meals, especially among girls (Story et al., 2002). In the absence of physical activity, this puts adolescents at a higher risk of obesity and related health problems.
Self-efficacy plays a crucial role as a predictor for one’s engagement and performance in weight control behaviors (Linde et al., 2006; Ames et al., 2012). Studies show a correlation between self-efficacy and increasing physical activity among adolescent girls (Dishman et al., 2004; Verloigne et al., 2016) and, with proper planning of interventions, it impacts one’s intake of fruit and vegetables and reduces one’s intake of energy-dense food (Luszczynska et al., 2016). Establishing healthy habits during adolescence is important, given that eating behavior that is likely to cause fatness is actively adopted during this age (Lytle et al., 2000), while consumption of fruits and vegetables, which has immediate and long-term health-protective benefits, is likely to decline (Neumark-Sztainer et al., 2003; Pearson et al., 2011). Instilling self-efficacy is important in ensuring healthier food choices and dietary intake among adolescents since, as Pearson et al. (2011) argue, eating behaviors and habits established during adolescence are likely to persist into adulthood.
Observational learning is a key element in the social cognitive theory and is the most effective way to improve self-efficacy through mastery experiences and social modeling (Bandura, 1986, 1994; Lassetter et al., 2015). If people vicariously perceive others’ success relative to performing a behavior, for instance, healthy eating or engaging in physical activity, they are likely to show increases in self-efficacy (Bandura, 2004). Atkin and Rice (2013) have addressed the role of personal influencers in behavior formation and change. For adolescents, such influencers may include, but are not limited to, parents, teachers, peers, and other community members with whom they interact. The social environment and support they may receive from their environment both directly and indirectly influences their dietary behavior in the presence of personal factors such as self-efficacy (Fitzgerald et al., 2013). Adolescents also engage in weight-reduction interventions, which may include healthier eating, for social identity and in-group inclusion purposes or based on the influence of their peers (Oyserman et al., 2007). In nutrition decisions, self-efficacy empowers youth, giving them a sense of control of their dietary choices. This is because people, regardless of age, are self-organizing, proactive, and self-regulating agents in their own development, rather than just recipients of socialized influences (Bandura, 1986).
Using the lens of the social cognitive theory, this article focuses on the following research questions: (1) What are the individual factors that influence self-efficacy for healthy eating and healthy food choice? (2) Does food environment determine efficacy for healthy eating and food choice among adolescents? Individual perceptions include adolescents’ attitudes toward health, their perceived control or a sense of empowerment, and perceived barriers to healthy eating. Environmental factors include their perceptions of healthy food availability within their home and school environment. Demographic factors, including age, gender, grade level, ethnicity, and state/geographical region, are also examined regarding adolescents’ self-efficacy for healthy food choice and healthy eating.
Methods and Measures
Data Collection Method
Data for this school-based study were gathered from six low-income communities in the U.S. in Kansas, Ohio, and South Dakota. Low-income communities were defined as those with a household income that averaged below 185% federal poverty level, had a community poverty level higher than state average, and where the community percentage of those who qualified for free or reduced-price school lunches was higher than state average or the majority (51% or more) qualified for free or reduced-price school lunches (Kidd et al., 2016). The researchers randomly selected two schools in each state for their control and intervention communities and administered a baseline survey to the intervention community. Except for Ohio, where a random selection of the school was performed, Kansas and South Dakota has only one middle school in each of the selected communities. The sampling frame was composed of the overall population of middle school students, sixth to eighth grades in the selected schools. Data were gathered following approval from Institutional Review Boards in the three states. Parental consent was required due to participants’ age, in addition to participants’ assent prior to involvement.
The survey had 31 items that gathered information on their fruit and vegetable intake, perceptions and self-efficacy for healthy eating and food choice, and one question on demographics (age, gender, grade level, and ethnicity). Focus group discussions conducted prior to the survey were used to guide researchers in the selection of instruments to capture the adolescents’ health and nutrition behaviors, including their perceptions, barriers, and facilitators (Kidd et al., 2016). Although questions were adapted from validated instruments, cognitive testing was performed to ensure that appropriate language was used in the survey. Paper and pencil method was then used in completing the survey. In addition, questions were read out loud by the researchers and clarified wherever necessary, and examples were used to give participants an estimate of fruits, vegetables, and drinks consumed.
Measures
Efficacy for healthy eating was measured with four items (Neumark-Sztainer et al., 2002) that required participants to indicate their confidence in selecting healthy food in certain situations, for example, when hungry after school, with friends, at a fast food restaurant, or while eating dinner with family. The items were measured on a 5-point Likert scale with 1 (not at all sure) to 5 (extremely sure). The scale had a reliable internal consistency (Cronbach α = 0.74).
Efficacy for healthy food choice was measured differently with four items (Dewar et al., 2012) and measured with a 5-point Likert scale with 1 (not at all agree) to 5 (strongly agree) (Cronbach α = 0.60). The scale included statements that examined their ease in choosing to eat healthy meals, e.g., “at least 1½ to 2 cups of fruit each day” and “at least 2 to 3 cups of vegetables each day.”
Attitudes toward healthy eating were measured with six items that asked students to rate how much they cared about various aspects that contributed to physical health (Neumark-Sztainer et al., 2002), such as how much they cared about “eating healthy foods,” “controlling your weight,” or “staying in shape.” The items measured on the 5-point Likert scale with 1 (do not care at all) to 5 (care very much) had a reliable internal consistency (Cronbach α = 0.85).
To measure their perceptions of peers’ health concerns, participants were asked to rate their agreement on statements that measured the extent to which their friends “cared about eating healthy foods” and “cared about staying in shape and exercising.” Both items were adopted from Neumark-Sztainer et al. (2002) and measured on a scale of 1 (do not agree) to 5 (strongly agree), which also had a reliable internal consistency (Cronbach α = 0.77).
Perceived control was measured with six items that addressed adolescents’ sense of control of their future and perceptions of their societal contribution, such as “I often feel that my future is out of control” and “I have some control in my future.” Items in the scale were measured on a 5-point Likert scale with 1 (not at all agree) to 5 (strongly agree). After reverse-coding the first item, the scale had a reliable internal consistency (Cronbach α = 0.70). Perceived barriers for healthy eating were measured with three items that required participants to agree to statements that examined their concerns for healthier eating, such as “I’m too busy to eat healthily” and “Kids my age don’t need to be concerned about their eating habits.” The items were measured on a 5-point Likert scale with 1 (not at all agree) to 5 (strongly agree) (Cronbach α = 0.60).
In examining environmental factors, adolescents’ perceptions of healthy food availability were measured with six items. The items examined their perceptions of availability of fruits and vegetables at home and school, as well as the availability of healthy foods at local grocery stores. The six items were adopted from Neumark-Sztainer et al. (2002) and measured on a 5-point Likert scale with 1 (never) to 5 (always) with reliable internal consistency (Cronbach α = 0.78).
Data were analyzed using the statistical package science statistical (SPSS); analysis included descriptives for demographic characteristics and scales used, and t-tests and one-way ANOVA to examine differences between gender, among states/geographical region, and ethnicity, with Bonferroni post hoc analysis to show specific differences. Correlations and multiple linear regressions were performed to examine relationships between variables. All scales were measured on 5-point Likert scale, and analyses were done at 5% level of significance, with an acceptable Cronbach alpha of 0.60.
Results
Sample Characteristics
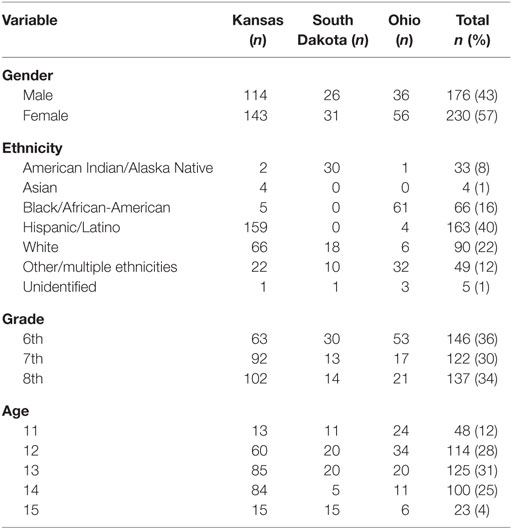
The sample was composed of 410 adolescents with 43% males (n = 176) and 1% (n = 4) who did not reveal his or her gender. Ethnically, the overall sample was diverse, although the majority was Hispanic or Latino (4%) followed by African-Americans (16%) and only four Asians (1%). Table 1 shows the distribution of demographics by state/geographical region.
There were no differences in gender distribution by state/geographical region among study participants, but a significant difference was found in their ethnicity across the three states (χ2 = 461.26, df = 12, p < 0.001). The sample was predominantly ethnic, with the majority of Kansas participants being Hispanic, Latino, or Spanish, the majority of Ohio participants being Black or African-Americans, and the majority of South Dakota participants being American Indians or Alaska Natives. This is reflective of ethnicity distribution in the selected communities across the three states. For analysis purposes, the sample was recoded as White/Caucasian (22%) and ethnic minorities (77%).
Scale Descriptives
Results from the 4-item scale show a moderate efficacy for healthy eating among adolescents (M = 3.20, SD = 0.91). A t-test shows no significant differences based on gender. There was also no difference based on the state/geographical region where they reside (p > 0.05). On the other hand, grade level played a significant role in the variation in adolescents’ efficacy for healthy eating [F(2,393) = 10.022, p < 0.001]. A Bonferroni post hoc analysis shows differences between sixth and seventh grades and between sixth and eighth grades but not between seventh and eighth grades.
Efficacy for healthy food choice was also moderate among adolescents in the three states (M = 3.31, SD = 0.76). No significant gender differences were observed (p > 0.05). An ANOVA test also shows no significant differences in their efficacy for healthy food choice based on their grade level or state (p > 0.05). Ethnicity also did not contribute to the variance in their efficacy for healthy food choice.
Participants indicated having relatively positive attitudes toward health (M = 4.30, SD = 0.71), but no gender differences were observed across the states. Their grade level played a significant role in the variation in participants’ attitudes [F(2,395) = 4.273, p < 0.05] but only between sixth and eighth grades. There were also differences in attitudes based on their state/geographical region [F(2,400) = 3.951, p = 0.020]. Specific differences were observed between Kansas and South Dakota (p = 0.02) but not between Kansas and Ohio or between Ohio and South Dakota. Ethnicity was also a significant factor in the variation in adolescents’ attitudes toward health [F(6,391) = 2.242, p = 0.039]. A Pearson correlation test shows that attitudes toward health to be positively correlated with efficacy for healthy food choice (r = 0.477, p < 0.01) and with efficacy for healthy eating (r = 0.317, p < 0.01), which means that those with more positive attitude were more likely to report higher efficacy.
Peers’ perception of health concerns was moderate (M = 3.60, SD = 1.07), with significant gender differences observed (t = 3.352, df = 395, p = 0.001). Males indicated higher perceptions on peers’ health concerns (M = 3.79, SD = 0.97) compared to females (M = 3.43, SD = 1.12). Grade level also contributed to the variation in their perceptions of others’ health concerns [F(2,393) = 6.695, p = 0.001]. A Bonferroni post hoc analysis shows differences between sixth and seventh grades and between sixth and eighth grades but not between seventh and eighth grades. There were no differences in their perceptions based on their ethnicity or state/geographical region.
Results also show a relatively high perception of control among adolescents (mean = 4.0, SD = 0.78), with no significant differences based on gender or grade level (p > 0.05). There was variation in their perceptions [F(2,406) = 7.472, p < 0.01], where a significant difference was observed between Kansas and Ohio and between Ohio and South Dakota but not between Kansas and South Dakota. Ethnicity also contributed to their perceived control [F(6,398) = 3.064, p = 0.006], specifically between Black/African-Americans and Hispanic/Latino adolescents. There was a positive correlation between perceived control and their efficacy for healthy eating (r = 0.212, p < 0.001) and with their efficacy for healthy food choice (r = 0.317, p < 0.001), which means that adolescents who perceived themselves in control of their own lives were more likely to make healthier food choices and eat healthily.
On the other hand, perceived barriers for healthy eating were relatively low among adolescents (mean = 1.85, SD = 0.93). There were differences based on gender, grade level, or state/geographical region on their perceived barriers (p > 0.05), but ethnicity played a significant role [F(6,392) = 2.403, p = 0.027]. A Bonferroni post hoc analysis shows no specific difference between any two ethnicities in their perceived barriers for healthy eating. However, when categorized as ethnic minorities and White/Caucasian, a t-test (t = 3.568, df = 397, p = 0.000) shows that ethnic minorities perceived more barriers (M = 2.27, SD = 0.83) compared to their White counterparts (M = 1.98, SD = 0.60). Perceived barriers were also negatively correlated with efficacy for healthy food choice (r = −0.145, p = 0.003), but no significant correlation was found between barriers and efficacy for healthy eating.
In examining environmental factors, adolescents’ perceptions of healthy food availability indicated high perceptions of a healthy food environment (M = 4.37, SD = 0.63). There were no gender differences in their perceptions of healthy food availability (p > 0.05). State/geographical region also did not play a role in their perceptions. Ethnic differences were observed [F(6,392) = 2.335, p = 0.032], especially between those categorized as Other and Black/African-American, as well as between Other and Hispanic/Latinos (p < 0.05).
Individual Perceptions Associated With Efficacy for Healthy Food Choice
Healthy food choice was measured by four items that examined the ease at which adolescents chose to eat fruits and vegetables and low-fat foods. Respondents reported finding it easy to choose at least one and a half to two cups of fruit each day (M = 3.80, median = 4, SD = 1.192). However, they reported less ease in choosing low-fat foods (M = 2.89, median = 3.0, SD = 1.056) and eating at least two to three cups of vegetables each day (M = 2.99, median = 3.0, SD = 1.23). An ANOVA test was performed to examine differences in each item by state/geographical region, but it found no significant differences. There were differences in the ease to eat fruits and vegetable based on grade level [F(2,397) = 5.466, p = 0.005], but the significant results were only between sixth and eighth grades (p = 0.022).
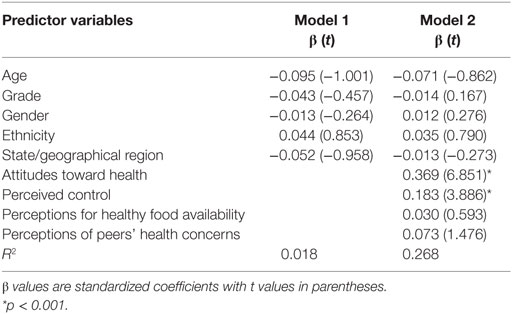
To determine factors that influence healthy food choice among adolescents, a multiple linear regression shows that demographic factors (gender, grade level, ethnicity, and state/geographical region) explained about 2% of model variance (R2 = 0.018) but did not produce a significant model. No demographic factors played a significant role in determining food choice among adolescents. Other factors including attitudes toward health, perceptions on food availability, perceived control, and perception of peers’ health concerns produced a significant equation [F(9,381) = 15.496, p = 0.000] and increased the model explanatory power to about 27% (R2 = 0.268). As Table 2 shows, significant factors in the model included attitudes toward health (β = 0.369, t = 6.851, p < 0.001) and perceived control (β = 0.183, t = 3.886, p < 0.000). Adolescents who believe they are in control of their own lives also indicated higher efficacy for healthy food choice.
Factors That Influence Efficacy for Healthy Eating
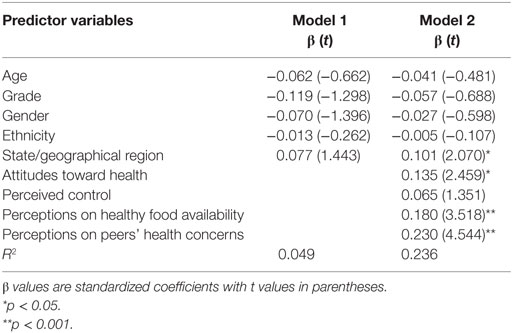
Efficacy for healthy eating was predicted by various factors. Results from a hierarchical multiple regression show that demographic factors accounted for about 5% (R2 = 0.049) and produced a significant model [F(5,385) = 3.979, p = 0.002]. However, like in efficacy for healthy food choice, no demographic factors (age, grade level, gender, ethnicity, and state/geographical region) had a significant contribution by itself, although together they played a role in determining adolescents’ efficacy for healthy eating. Other factors including attitudes toward health, perceptions on healthy food availability, perceived control, and perceptions on peer health concerns increased the model explanatory power to 24% (R2 = 0.236) and produced a significant model equation as well [F(9,381) = 13.072, p = 0.000]. As shown in Table 3, the most significant determinants of healthy eating after controlling for demographics were perceptions of peers’ health concerns, attitudes toward health, and perceptions of healthy food availability. The state/geographical region gained significance in the second model (p < 0.05) after adding other predicting factors.
Discussion
Results show moderate efficacy for healthy food choices and for healthy eating among adolescents across all three states with no significant differences based on their geographical location. Their efficacy for healthy food choice was correlated with a variety of personal and environmental factors, including attitudes toward health, perceptions of the healthy food environment, perceived control, and perceptions of peers’ concerns about health. Similarly, efficacy for healthy eating was correlated with attitudes toward health, perceived healthy food availability, and perceived control. These findings are in line with previous studies that have found a relationship between personal factors with behaviors, where self-efficacy plays the moderating role in advocated health behavior (Bandura, 1977, 2004; Janz and Becker, 1984; Rimal, 2001).
An examination of personal factors that influence adolescents’ self-efficacy for healthy food choice and healthy eating shows both attitudes and perceived control as statistically significant. Attitudes toward health are specifically important in predicting behavior (Janz and Becker, 1984), and results show a significant correlation with self-efficacy. Perceived control or a sense of empowerment among adolescents also has significance in determining adolescents’ dietary decisions, where adolescents with a higher sense of control are more likely to make healthier food choices. This implies the need to focus on youth empowerment and to value their voices and program interventions that seek to promote healthier dietary behaviors. Furthermore, perceptions of peer concerns about health played a significant role in adolescents’ efficacy for healthy eating, which confirms previous studies’ assertion on interpersonal influencers on health behavior. The current study adds a different perspective by virtue of examining how their perception of those influencers’ health concerns relates to their own nutrition decisions.
In examining environmental factors that influence food choice, adolescents indicated relatively positive perceptions of healthy food availability within their environment. These perceptions also played a role in their efficacy for healthy eating but did not play a role in their efficacy for healthy food choice. This discrepancy may be associated with the unhealthy food environment where the samples were drawn – low-income communities. Previous studies have shown that low-income communities face unhealthier food environments, with reduced access to supermarkets, a plethora of convenience stores, fast food outlets, and environmental factors such as crime and lack of access to physical activity resources, all of which contribute to ethnic disparities in weight among children (Rossen, 2014). The discrepancy may also be due to low nutrition literacy or knowledge about a healthy food environment among adolescents, which was not measured in the current study. The fact that adolescents are not food purchasers for home and school meals may also have played a role in their perceptions.
Ethnic-based differences were evident in adolescents’ perceived barriers for healthy eating, attitudes toward health, and perceptions of healthy food availability. This means that although the sample was drawn from low-income communities, adolescents in these communities perceive dietary-related barriers differently and have different attitudes toward health in general based on their ethnicity. Specific differences were observed among Hispanics/Latinos and Blacks/African-Americans in their perceptions of healthy food availability and barriers to healthy eating. Significant differences were also observed in adolescents’ perceived barriers to healthy eating, specifically between American Indians and White/Caucasians. Previous studies have shown ethnic minorities, in general, to be disproportionately impacted (Crespo et al., 2012; Wang et al., 2012; Skinner et al., 2016), but self-efficacy would empower them to overcome those barriers to healthy dietary behaviors. This would, however, be more effective if accompanied by a healthy food environment, including strategic placement of healthy foods at home, schools, and grocery stores.
Although the study provides some insights on the determinants for self-efficacy among adolescents, it has some limitations that need to be mentioned. First, the length of the questionnaire may have been an issue among adolescents, particularly those in the sixth grade due to their lower reading skills. The questionnaire was completed with the assistance of the researchers to address this limitation, but it is likely that not all participants across the states or different grade levels had the same level of comprehension. The questionnaires were not pilot-tested since all items were adopted from validated instruments. However, cognitive testing was used to ensure the language used was age appropriate. Additionally, although not examined, it is also likely that nutrition literacy varied by grade level, which could have impacted the scales’ external validity. Second, in spite of the internal consistency of the scales used, the study is likely to have external validity issues due to self-reporting, especially as students attempted to recall their food consumption. Third, the study relied on cross-sectional observation data and therefore did not provide causal inferences.
Conclusion
As a public health problem in the U.S., childhood obesity has been addressed from various perspectives. The current study addresses the issue from a prevention and communication perspective and examined some of the key factors in self-efficacy for food choice and healthy eating among adolescents in low-income communities. The study uses the social cognitive theory (Bandura, 1977, 1986, 2004) to predict the relationships between personal and environmental factors in adolescent obesity in these communities. It also examines differences in these factors based on demographic elements – gender, ethnicity, grade level, and geographical region in which they reside.
A key predictor for self-efficacy for healthy eating was food availability within the home and school environment, where adolescents spend most of their time. If they believe healthy food is available in these environments, they were more likely to have confidence in their capability to eat healthily. This finding has an important practical implication for obesity prevention interventions among adolescents: although nutrition education is important in obesity prevention (Gavaravarapu, 2013; Rosemond et al., 2016), it is equally necessary to focus on enhancing confidence for healthier dietary habits. This confidence may be enhanced through community partnerships that facilitate access to healthier foods within the overall environment, including grocery stores, especially in low-income and rural communities that are characterized as food deserts.
Attitudes toward overall health play an important role in predicting efficacy for food choice and for healthy eating among adolescents. Although health communication campaigns focus on awareness and risk perception with a focus on behavior change, findings from this study suggest incorporating strategies that will enhance adolescents’ attitudes toward health in obesity prevention interventions. Focusing health communication interventions on the bigger picture would include promoting healthier dietary habits, physical activity, and overall physical and social well-being.
It is particularly important for health communication interventions to focus on strategies that will promote and enhance youth empowerment or a sense of control, which may be achieved through listening to their views and giving them an opportunity to contribute in dietary and overall health decision-making. Participatory projects focus on engagement of targets groups that are deemed at health risks in developing strategies to address the problem and design of appropriate solutions. Results from the current study validate that need to empower adolescents as a crucial component in obesity prevention. Such programs are also more likely to be acceptable to adolescents who otherwise might have lower risk perception for overweight and obesity. Additionally, ethnic-based nutrition health communication programing that targets adolescents is crucial. As results have shown, ethnic differences exist for attitudes and perceptions related to health and healthy eating behaviors. It is important to acknowledge that though ethnic minorities are disproportionately impacted by childhood obesity overall, the determinants and barriers may differ ethnically. This implies the need for audience segmentation and design of strategic programs that focus on tailoring information and messages based on not only personal factors (knowledge, attitudes, and perceptions) but also external factors such as intercultural barriers in healthier dietary habits that promote unhealthy nutrition decisions.
Addressing the role of peers and their influence in self-efficacy for dietary habits among adolescents is also necessary. This role of peer influence is documented in previous studies that focus on interpersonal influencers (e.g., Oyserman et al., 2007; Atkin and Rice, 2013). Rather than focus on direct influence, we examined their perceptions of peers’ health concerns and how those perceptions might influence their own self-efficacy for food choice. Based on the social cognitive theory and findings from this study, we suggest promoting positive attitudes and role modeling in the overall health and well-being among adolescents, which is likely to influence dietary habits that will lead to obesity prevention.
Author Contributions
Prof. NM was a co-PI and took the lead in writing the manuscript. Other Co-PIs that made substantial contribution to the conception and design of the project were Dr. TK, Dr. KA, Prof. KK, and Ms. SZ. All co-authors reviewed and provided critical feedback on the manuscript. Ms. TK assisted with literature review and final editing of the manuscript. Ms. EL made critical and intellectual evaluation and contributed in the revisions of the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This article is based upon work that is supported by the National Institute of Food and Agriculture, U.S. Department of Agriculture, under award number 2012-68001-19619.
References
Ahmed, R., and Bates, B. R. (2013). Health Communication and Mass Media: An Integrated Approach to Policy and Practice. New York: Routledge.
Ames, G. E., Heckman, M. G., Grothe, K. B., and Clark, M. M. (2012). Eating self-efficacy: development of a short-form WEL. Eat. Behav. 13, 375–378. doi: 10.1016/j.eatbeh.2012.03.013
Andrews, J. C., Netemeyer, R. G., and Burton, S. (2009). The nutrition elite: do only the highest levels of caloric knowledge, obesity knowledge, and motivation matter in processing nutrition ad claims and disclosures? J. Public Policy Mark. 28, 41–55. doi:10.1509/jppm.28.1.41
Atkin, C. K., and Rice, R. E. (eds). (2013). “Theory and principles of public communication campaigns,” in Public Communication Campaigns, 4th Edn (Thousand Oaks, CA: Sage), 3–20.
Bandura, A. (1977). Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 84, 191. doi:10.1037/0033-295X.84.2.191
Bandura, A. (1994). “Self-efficacy,” in Encyclopedia of Human Behavior, ed. V. S. Ramachandran, Vol. 4 (New York: Academic Press), 71–81.
Bandura, A. (1998). Health promotion from the perspective of social cognitive theory. Psychol. Health 13, 623–649. doi:10.1080/08870449808407422
Bandura, A. (2004). Health promotion by social cognitive means. Health Educ. Behav. 31, 143–164. doi:10.1177/1090198104263660
Bas, M., and Donmez, S. (2009). Self-efficacy and restrained eating in relation to weight loss among overweight men and women in Turkey. Appetite 52, 209–216. doi:10.1016/j.appet.2008.09.017
Caprara, G. V., Scabini, E., Barbaranelli, C., Pastorelli, C., Regalia, C., and Bandura, A. (1998). Impact of adolescents’ perceived self-regulatory efficacy on familial communication and antisocial conduct. Eur. Psychol. 3, 125–132. doi:10.1027/1016-9040.3.2.125
Coffman, D. L., Smith, E. A., Flisher, A. J., and Caldwell, L. L. (2011). Effects of health wise South Africa on condom use self-efficacy. Prev. Sci. 12, 162–172. doi:10.1007/s11121-010-0196-z
Comstock, C., Kattelmann, K., Zastrow, M., McCormack, L., Lindshield, E., Li, Y., et al. (2016). Assessing the environment for support of youth physical activity in rural communities. J. Nutr. Educ. Behav. 48, 234–241. doi:10.1016/j.jneb.2015.12.013
Crespo, N. C., Elder, J. P., Ayala, G. X., Slymen, D. J., Campbell, N. R., Sallis, J. F., et al. (2012). Results of a multi-level intervention to prevent and control childhood obesity among Latino children: the Aventuras Para Niños Study. Ann. Behav. Med. 43, 84–100. doi:10.1007/s12160-011-9332-7
Dewar, D. L., Lubans, D. R., Plotnikoff, R. C., and Morgan, P. J. (2012). Development and evaluation of social cognitive measures related to adolescent dietary behaviors. Int. J. Behav. Nutr. Phys. Act. 9, 1. doi:10.1186/1479-5868-9-36
Dishman, R. K., Motl, R. W., Saunders, R., Felton, G., Ward, D. S., Dowda, M., et al. (2004). Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev. Med. 38, 628–636. doi:10.1016/j.ypmed.2003.12.007
Fitzgerald, A., Heary, C., Kelly, C., Nixon, E., and Shevlin, M. (2013). Self-efficacy for healthy eating and peer support for unhealthy eating are associated with adolescents’ food intake patterns. Appetite 63, 48–58. doi:10.1016/j.appet.2012.12.011
Gavaravarapu, S. M. (2013). Knowledge translation – some perspectives for nutrition education and communication. J. Nutr. Educ. Behav. 45, e5. doi:10.1016/j.jneb.2013.04.258
Gavaravarapu, S. M., Rao, K. M., Nagalla, B., and Avula, L. (2015). Assessing differences in risk perceptions about obesity among “normal-weight” and “overweight” adolescents – a qualitative study. J. Nutr. Educ. Behav. 47, 488–497. doi:10.1016/j.jneb.2015.07.001
Janz, N. K., and Becker, M. H. (1984). The health belief model: a decade later. Health Educ. Behav. 11, 1–47. doi:10.1177/109019818401100101
Jenkins, S., and Horner, S. D. (2005). Barriers that influence eating behaviors in adolescents. J. Pediatr. Nurs. 20, 258–267. doi:10.1016/j.pedn.2005.02.014
Kidd, T., Lindshield, E., Kattelmann, K., Adhikari, K., Muturi, N., and Zies, S. (2016). Ignite-sparking youth to create healthy communities: a protocol for a community-centered effort for the prevention of adolescent obesity. Int. J. Nurs. Clin. Pract. 3, 189. doi:10.15344/2394-4978/2016/189
Kreps, G. L., and Sparks, L. (2008). Meeting the health literacy needs of immigrant populations. Patient Educ. Couns. 71, 328–332. doi:10.1016/j.pec.2008.03.001
Kumanyika, S. K., Obarzanek, E., Stettler, N., Bell, R., Field, A. E., Fortmann, S. P., et al. (2008). Population-based prevention of obesity the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American heart association council on epidemiology and prevention, interdisciplinary committee for prevention (formerly the expert panel on population and prevention science). Circulation 118, 428–464. doi:10.1161/CIRCULATIONAHA.108.189702
Kumar, J., Adhikari, K., Li, Y., Lindshield, E., Muturi, N., and Kidd, T. (2016). Identifying barriers, perceptions and motivations related to healthy eating and physical activity among 6th to 8th grade, rural, limited-resource adolescents. Health Educ. 116(2), 123–137. doi:10.1108/HE-03-2014-0035
Kumar, J., Kidd, T., Li, Y., Lindshield, E., Muturi, N., and Adhikari, K. (2014). Using the community-based participatory research (CBPR) approach in childhood obesity prevention. Int. J. Child Health Nutr. 3, 170–178. doi:10.6000/1929-4247.2014.03.04.3
Lassetter, J. H., Ray, G., Driessnack, M., and Williams, M. (2015). Consulting with children in the development of self-efficacy and recall tools related to nutrition and physical activity. J. Spec. Pediatr. Nurs. 20, 21–28. doi:10.1111/jspn.12093
Lee, Y. H., Salman, A., and Cooksey-James, T. (2016). Gender differences in HIV/AIDS preventive self-efficacy among Taiwanese adolescents. AIDS Educ. Prev. 28, 77–89. doi:10.1521/aeap.2016.28.1.77
Linde, J. A., Rothman, A. J., Baldwin, A. S., and Jeffery, R. W. (2006). The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. 25, 282–291. doi:10.1037/0278-6133.25.3.282
Littlefield, C. H., Craven, J. L., Rodin, G. M., Daneman, D., Murray, M. A., and Rydall, A. C. (1992). Relationship of self-efficacy and binging to adherence to diabetes regimen among adolescents. Diabetes Care 15, 90–94. doi:10.2337/diacare.15.1.90
Luszczynska, A., Hagger, M. S., Banik, A., Horodyska, K., Knoll, N., and Scholz, U. (2016). Self-efficacy, planning, or a combination of both? A longitudinal experimental study comparing effects of three interventions on adolescents’ body fat. PLoS ONE 11:e0159125. doi:10.1371/journal.pone.0159125
Lytle, L. A., Seifert, S., Greenstein, J., and McGovern, P. (2000). How do children’s eating patterns and food choices change over time? Results from a cohort study. Am. J. Health Promot. 14, 222–228. doi:10.4278/0890-1171-14.4.222
Neumark-Sztainer, D., Story, M., Hannan, P. J., Perry, C. L., and Irving, L. M. (2002). Weight-related concerns and behaviors among overweight and non-overweight adolescents: implications for preventing weight-related disorders. Arch. Pediatr. Adolesc. Med. 156, 171–178. doi:10.1001/archpedi.156.2.171
Neumark-Sztainer, D., Wall, M., Perry, C., and Story, M. (2003). Correlates of fruit and vegetable intake among adolescents: findings from Project EAT. Prev. Med. 37, 198–208. doi:10.1016/S0091-7435(03)00114-2
Ogden, C. L., Carroll, M. D., Kit, B. K., and Flegal, K. M. (2012). Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 307, 483–490. doi:10.1001/jama.2012.40
Oyserman, D., Fryberg, S. A., and Yoder, N. (2007). Identity-based motivation and health. J. Pers. Soc. Psychol. 93, 1011–1027. doi:10.1037/0022-3514.93.6.1011
Pearson, N., Ball, K., and Crawford, D. (2011). Predictors of changes in adolescents’ consumption of fruits, vegetables and energy-dense snacks. Br. J. Nutr. 105, 795–803. doi:10.1017/S0007114510004290
Rimal, R. N. (2001). Perceived risk and self-efficacy as motivators: understanding individuals’ long-term use of health information. J. Commun. 51, 633–654. doi:10.1111/j.1460-2466.2001.tb02900.x
Rosemond, T. N., Blake, C. E., Buff, S. M., Blake, E. W., Dunn, B. L., Browne, T., et al. (2016). Sensitizing future health professionals to determinants of childhood obesity. Am. J. Prev. Med. 51, 106–113. doi:10.1016/j.amepre.2016.01.002
Rossen, L. M. (2014). Neighborhood economic deprivation explains racial/ethnic disparities in overweight and obesity among children and adolescents in the USA. J. Epidemiol. Community Health 68, 123–129. doi:10.1136/jech-2012-202245
Rutkowski, E. M., and Connelly, C. D. (2012). Self-efficacy and physical activity in adolescent and parent dyads. J. Spec. Pediatr. Nurs. 17, 51–60. doi:10.1111/j.1744-6155.2011.00314.x
Schwarzer, R., and Luszczynska, A. (2006). “Self-efficacy, adolescents’ risk-taking behaviors, and health,” in Self-Efficacy Beliefs of Adolescents, eds F. Pajared and T. Urdan, Vol. 5 (Greenwich, CT: Information Age Publishing), 139–159.
Sharma, M. (2006). School-based interventions for childhood and adolescent obesity. Obes. Rev. 7, 261–269. doi:10.1111/j.1467-789X.2006.00227.x
Skinner, A. C., Perrin, E. M., and Skelton, J. A. (2016). Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity 24, 1116–1123. doi:10.1002/oby.21497
Spear, B. A. (2002). Adolescent growth and development. J. Am. Diet. Assoc. 102, S23–S29. doi:10.1016/S0002-8223(02)90418-9
Story, M., Neumark-Sztainer, D., and French, S. (2002). Individual and environmental influences on adolescent eating behaviors. J. Am. Diet. Assoc. 102(Suppl. 3), 40–51. doi:10.1016/S0002-8223(02)90421-9
Turner, M. M., Rimal, R. N., Morrison, D., and Kim, H. (2006). The role of anxiety in seeking and retaining risk information: testing the risk perception attitude framework in two studies. Hum. Commun. Res. 32, 130–156. doi:10.1111/j.1468-2958.2006.00006.x
U.S. Department of Health and Human Services. (2008). Making Health Communication Programs Work: A Planner’s Guide. Bethesda, MD: National Cancer Institute. Available from: http://www.cancer.gov/publications/health-communication/pink-book.pdf
Verloigne, M., Cardon, G., De Craemer, M., D’Haese, S., and De Bourdeaudhuij, I. (2016). Mediating effects of self-efficacy, benefits and barriers on the association between peer and parental factors and physical activity among adolescent girls with a lower educational level. PLoS ONE 11:e0157216. doi:10.1371/journal.pone.0157216
Keywords: adolescence, ethnic minorities, low-income, obesity, self-efficacy, school-based program
Citation: Muturi NW, Kidd T, Khan T, Kattelmann K, Zies S, Lindshield E and Adhikari K (2016) An Examination of Factors Associated With Self-Efficacy for Food Choice and Healthy Eating among Low-Income Adolescents in Three U.S. States. Front. Commun. 1:6. doi: 10.3389/fcomm.2016.00006
Received: 27 June 2016; Accepted: 06 September 2016;
Published: 21 September 2016
Edited by:
Rukhsana Ahmed, University of Ottawa, CanadaReviewed by:
Maria Beatriz Torres, Gustavus Adolphus College, USASubbaRao M. Gavaravarapu, National Institute of Nutrition (Indian Council of Medical Research), India
Copyright: © 2016 Muturi, Kidd, Khan, Kattelmann, Zies, Lindshield and Adhikari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nancy W. Muturi, bm11dHVyaUBrc3UuZWR1
 Nancy W. Muturi
Nancy W. Muturi Tandalayo Kidd2
Tandalayo Kidd2 Tazrin Khan
Tazrin Khan Susan Zies
Susan Zies Erika Lindshield
Erika Lindshield Koushik Adhikari
Koushik Adhikari