- 1Department of Spine Surgery, Heze Municipal Hospital, Heze, China
- 2Department of Anesthesiology, Women’s and Children's Hospital Affiliated to Qingdao University, Qingdao, China
- 3Department of Orthopedics, Affiliated Hospital of Shandong Second Medical University, Weifang, China
Objective: The aim of this study was to investigate the effect of vacuum sealing drainage (VSD) treatment on surgical indicators, inflammatory factors, and functional recovery in patients with chronic osteomyelitis secondary to open tibial fractures.
Methods: In total, 87 patients with secondary bone infection after internal fixation of tibial fracture treated in the Affiliated Hospital of Shandong Second Medical University from December 2020 to June 2022 were selected, all of whom were tibial shaft fractures. Of these, 55 cases of primary open fracture were sutured in the first stage; 32 cases underwent internal fixation after primary debridement at the time of trauma. The patients were treated with surgical debridement, removal of internal fixation, and fixation with an external fixation frame. After debridement, those with local wounds that could not be completely closed and were complicated with exposed bone were randomly selected for either VSD covering treatment (study group, n=46) or bone cement covering treatment (control group, n=41. The distribution of pathogenic bacteria, surgical indicators, inflammatory factors [tumor necrosis factor⁃α(TNF⁃α), interleukin⁃6 (IL⁃6), and C⁃reactive protein (CRP) levels], functional recovery [knee, ankle, and limb function recovery], and complications were summarized.
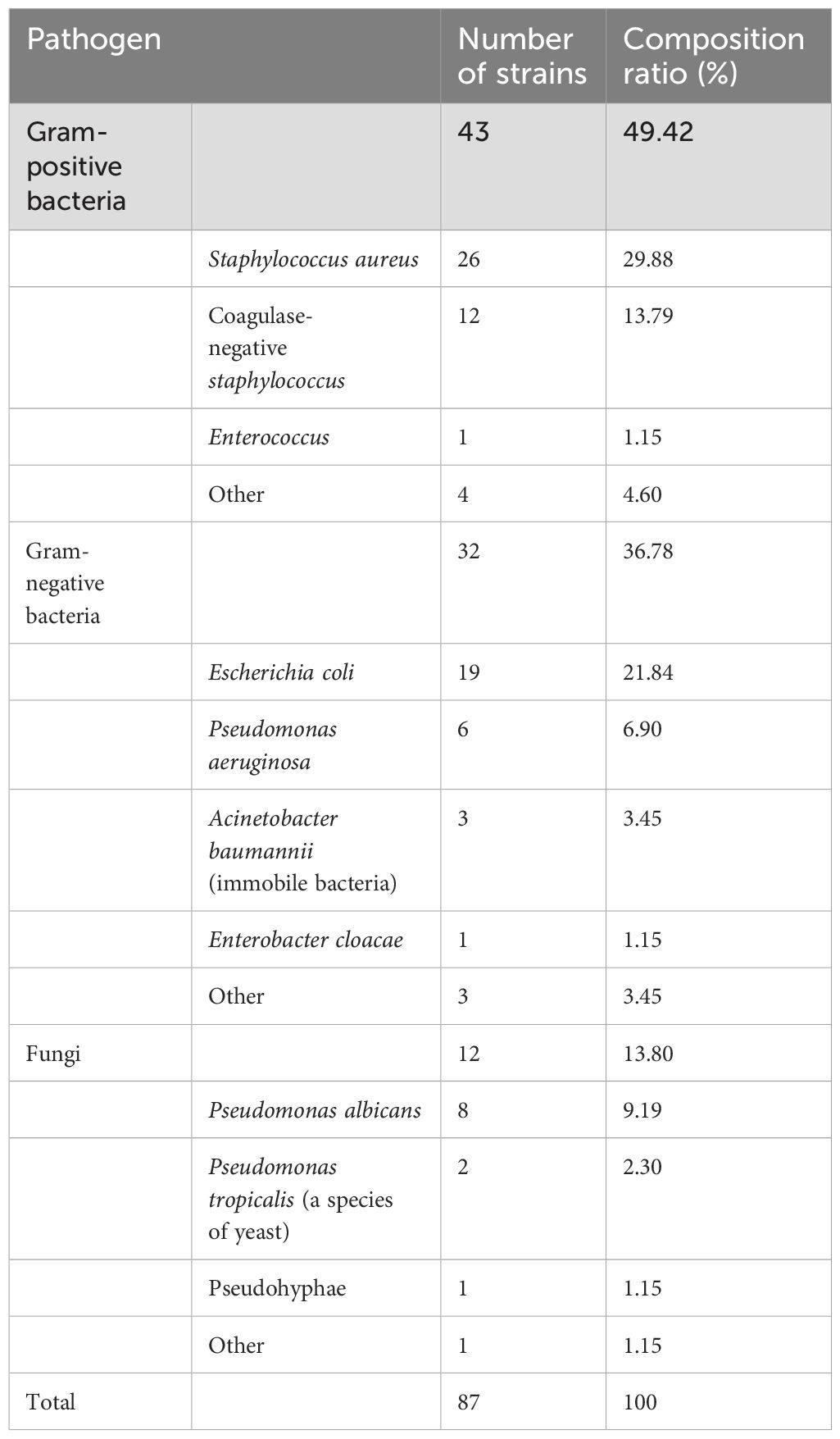
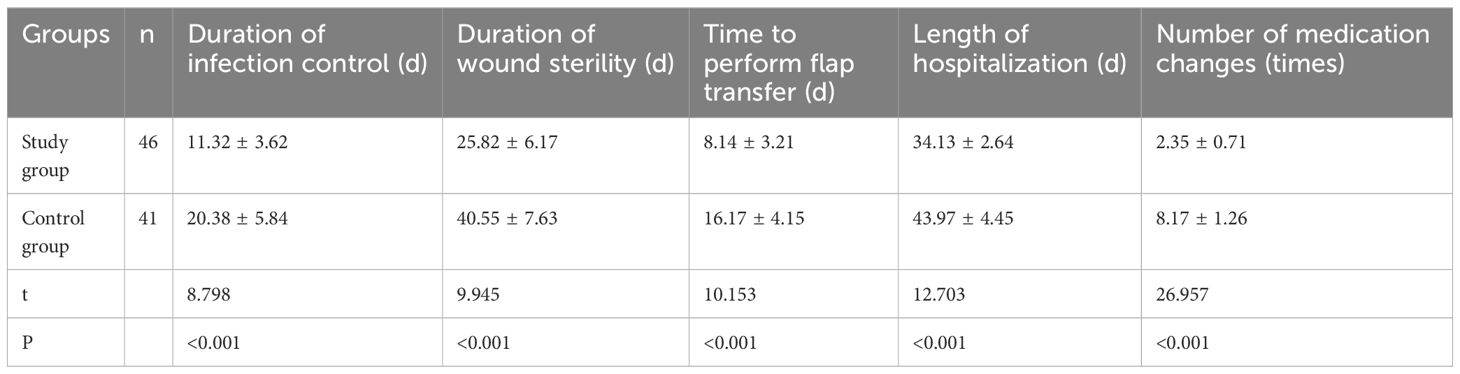
Results: There were 87 pathogenic bacteria strains in 87 patients, including 43 Gram⁃positive bacteria strains (49.42%), 32 Gram⁃negative bacteria strains (36.78%), and 12 fungi strains (13.80%). The number of dressing changes in the study group was less than that in the control group. The infection control time, wound sterility time, hospitalization time, and skin flap transfer operation time in the study group were shorter than those in the control group and the difference was statistically significant (P<0.05). After treatment, the levels of TNF⁃α, IL⁃6, and CRP in the two groups decreased, among which the change in the study group was the most significant and the difference between the two groups was statistically significant (P<0.05). After treatment, the Hospital for Special Surgery Knee Score and Baird–Jackson score of the two groups increased, among which the change in the study group was the most significant and the difference between the two groups was statistically significant (P<0.05). The excellent and good rate of the study group (95.65%) was higher than the excellent and good rate of the control group (80.49%) and the difference was statistically significant (P<0.05).
Conclusion: When a wound cannot be closed, VSD treatment of patients with secondary bone infection after internal fixation of tibial fracture can improve the level of surgical indicators and inflammatory factor levels in patients, and promote the recovery of patients’ limb function, and is thus worthy of clinical promotion and application.
1 Introduction
Tibial fractures, especially in the middle and lower segments, are common orthopedic issues with treatment and recovery challenges. Limited soft tissue cover makes the tibia prone to fracture upon trauma, potentially causing open fractures. Treatment is prolonged, complex, and risky due to the tibia’s proximity to the skin and poor blood supply (Li and Wang, 2018). The management of tibial fractures typically involves a two-stage approach. In the initial phase, the risk of infection is controlled through appropriate wound care and antibiotic therapy. Once the infection risk has been mitigated, internal fixation surgery is performed to stabilize the fracture and facilitate healing. However, despite meticulous care and surgical intervention, local infections can still arise due to systemic or local factors post-surgery, leading to refractory bone infections (Wang et al., 2017).
Bone infections, primarily caused by bacteria such as Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa, infect bone tissues such as bone marrow and periosteum, leading to inflammation and symptoms including wound pus, redness, swelling, pain, fever, and bone necrosis. In tibial fracture patients, these infections can have severe consequences, impeding wound healing and fracture union, and potentially causing physical dysfunction and disability. Prompt and effective clinical intervention is crucial to prevent complications such as osteomyelitis or septic arthritis, which can profoundly impact patients’ quality of life, physical health, and mental well-being. The primary treatment involves surgical intervention, including debridement, irrigation, and antibiotic therapy. However, some patients may not fully recover post-surgery and face a higher risk of complications or recurrence. Recently, vacuum sealing drainage (VSD) has shown promise in treating complex wounds, including those associated with bone infections, by creating a sealed environment that removes exudate, reduces edema, and stimulates granulation tissue formation (Jiang et al., 2020; Deng et al., 2023).
In this comprehensive study, we aim to delve into the effects of VSD treatment on surgical indicators, inflammatory factors, and functional recovery in patients who have developed postoperative bone infections secondary to tibial fracture. By comparing the outcomes of patients treated with VSD to those treated with traditional surgical methods, we hope to gain insights into the potential benefits of VSD in managing this challenging condition. The findings of this study will contribute to the evidence base for the use of VSD in the treatment of postoperative bone infections and may ultimately lead to improved patient outcomes and quality of life.
2 Information and methodology
2.1 General information
In total, 87 patients with bone infection secondary to internal fixation of tibia fracture admitted to the Affiliated Hospital of Shandong Second Medical University from December 2015 to June 2024 were selected, all of them were tibial stem fracture; among them, 55 were cases of original open fracture, all of which were sutured in one stage, and 32 cases were cleared in one stage at the time of traumatic injuries and were then subjected to internal fixation. The patients were treated with surgical debridement, removal of internal fixation, and fixation with an external fixation frame, and, after debridement, there were cases in which the wound could not be closed completely and the bone was exposed. These patients were randomly selected to be treated with VSD cover (study group, n=46) or cement cover (control group, n=41), and their indexes were summarized and analyzed. In the study group, there were 25 men and 21 women, with an average age of 35.28 ± 3.26 years; in the control group, there were 23 men and 18 women, with an average age of 34.37 ± 4.49 years. There was no statistically significant difference between the general information of the two groups (P>0.05).
Inclusion criteria: ① in an imaging examination, meet the diagnostic criteria of bone infection (Chastain and Davis, 2019) of local sinus tract formation; ② bone infection after debridement to form a trauma, skin defects, and bone exposure; ③ after one debridement treatment, the trauma surface is clean and the local flap transfer is healing (i.e., infection control); ④ in the hospital and complete clinical data with no defects or loss; ⑤ the patients and their families gave informed consent to the study. The study was approved by the ethics committee of the hospital and the patients and their families were informed and agreed to the study.
Exclusion criteria: (1) people with intact skin and soft tissues; (2) people who had one debridement surgery and the infection was not controlled; (3) people who had necrosis of the flap or the as was not healing for more than 3 weeks after the flap transfer (the infection was not controlled); (4) people who dropped out of the study; (5) people who had systemic acute toxicity symptoms, such as fever, and could not undergo the operation, or people who have a weak body and could not tolerate the operation; (6) people who could not cooperate with this study because of mental illness or related family history.
2.2 Methods
2.2.1 Pre-operative
The patients were admitted to the hospital for a routine pre-operative examination, and at the same time, blood sedimentation, C-reactive protein (CRP), tumor necrosis factor⁃α (TNF⁃α), and interleukin⁃6 (IL-6) laboratory tests were performed, bacterial cultures and drug sensitivity tests were conducted, and sensitive antibiotics were administered according to the results.
VSD operation process: First, the dressing matching the size of the wound was cut according to the size and shape of the wound. A small hole was cut in the central position of the dressing, and the side hole end of the drainage tube was embedded in it. Then, the foam dressing with a drainage catheter was filled in the wound of the patient. The strength of the filling was measured to avoid secondary trauma to the wound of the patient and reduce the pain and discomfort of the patient during the operation. At the same time, the foam dressing was filled completely to minimize the residual cavity and dead angle in the wound. Second, whether to place an irrigation catheter was determined according to the cleanliness of the wound. If there were more viscous secretions and necrotic tissue in the wound, an irrigation catheter was placed. The catheter was placed between the wound and the dressing, and it established a good circulation state. In addition, the patient’s wound was closed with a transparent 3M film so that the patient’s wound formed a closed system isolated from the external environment. Finally, the successful operation of the VSD device was confirmed when the negative pressure suction device was connected to the other end of the drainage catheter and the negative pressure was turned on. If the foam dressing and the sealing film were slightly deflated, the VSD device was successfully operated.
2.2.2 Study group
The bone surface was covered with petroleum jelly gauze, and according to the patient’s trauma, the VSD was pre-trimmed to cover and fill the bone defect area and all the skin of the surgical incision. After cleaning the skin around the trauma, the trauma was closed with biofilm, and the negative pressure drainage was carried out for 1 week, and then the dressing was taken out, and the trauma infection control was observed.
2.2.3 Control group
The wound is covered with bone cement and bandaged with a sterile dressing. After the oozing around the bone cement was reduced and basically dry, the dressing was removed and the wound was observed.
2.2.4 End of the study node
Local flap transfer was carried out after infection control through comprehensive judgment utilizing wound observation, secretion cultures, laboratory indexes, and clinical experience, and the flap was healed without necrosis within 3 weeks.
2.3 Observation indicators
2.3.1 Distribution of pathogen composition
Before treatment, 87 patients underwent bacterial culture and drug sensitivity tests. Each patient had two specimens collected within 3 hours, and was routinely cultured. Pure colonies were selected and identified by a bacterial identifier (VITEK 2 Compact, BioMérieux, France), and the common bacterial groups obtained from the two specimens were localized to the pathogens, and the culture of the specimens was carried out in accordance with the National Clinical Laboratory Practice Guidelines (Tudan, 2023). The isolation and identification of pathogenic bacteria and drug sensitivity experiments were carried out using the French NEW and ATB analyzers, and the quality control strains were S. aureus (ATCC29213), E. coli (ATCC25922) and P. aeruginosa (ATCC27853).
2.3.2 Surgical indicators
The surgical indicators included time to control infection, length of wound asepsis, number of dressing changes, time to perform flap transfer, and length of hospitalization.
2.3.3 Inflammatory factor
Before the patients were admitted to the hospital for surgical treatment and 1 week after the operation (VSD time was removed), 5 mL of morning fasting venous blood was collected from all the participants, and the serum was separated by centrifugation at 3,000 r/min, with a centrifugation radius of 9 cm, and taken out after 10 min for cryopreservation. Tumor necrosis factor⁃α, interleukin⁃6, and C-reactive protein levels were measured using enzyme-linked immunoluminescence.
2.3.4 Body function
The Hospital for Special Surgery Knee Score (HSS) and the Baird–Jackson Functional Score were used to score the patients’ knee and ankle joints, and the higher the score, the better the recovery of joint function (Mora-Zúñiga et al., 2021). The patients were scored according to Paley’s criteria, which included four grades: excellent, good, acceptable, and poor, and the excellent rate = [(excellent+good)/total number of cases]×100%. Paley’s criteria for functional recovery evaluation are as follows: ① obvious claudication; ② ankle stiffness with a horseshoe shape; ③ soft tissue dystrophy; ④ limb pain; ⑤ limb motor dysfunction. Level 1: none of the symptoms mentioned above, good range of motion of limbs; Level 2: ① to ④ 1-2 symptoms, good physical activity; Grade 3: ① to ④ symptoms of 3-4, good physical activity; Level 4: the fifth symptom is satisfied.
2.4 Statistical methods
SPSS 22.0 statistical software was used for statistical analysis. The measurement data were described by mean ± standard deviation (x ± s) and analyzed by t-test. Count data were expressed by n (%) and χ2 test was performed. P<0.05 was regarded as the difference of statistical significance.
3 Results
3.1 Distribution of pathogen composition
A total of 87 strains of pathogenic bacteria were found in 87 patients, including 43 (49.42%) Gram-positive, 32 (36.78%) Gram-negative, and 12 (13.80%) fungal strains, as shown in Table 1.
3.2 Surgical indicators
The number of dressing changes in the study group was lower than that in the control group, and the time taken for infection control, wound asepsis, hospitalization, and flap transfer surgery was shorter than those in the control group, with statistically significant differences (P<0.05), as shown in Table 2.
3.3 Inflammatory factor
The levels of TNF⁃α, IL⁃6, and CRP decreased in both groups after treatment, with the most significant changes in the study group (P<0.05).
In the study group, the most significant change was found, and the difference was statistically significant (P<0.05), as shown in Table 3.
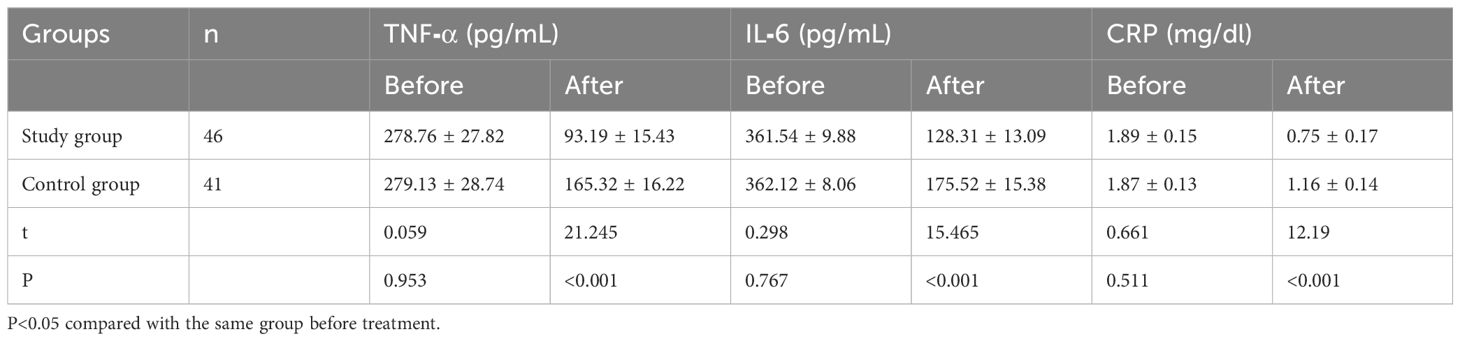
Table 3. Comparison of inflammatory indicators between the two groups before and after treatment (x ± s).
3.4 Body function
The HSS and Baird–Jackson score increased in both groups after treatment, with the most significant change in the study group, and the difference was statistically significant (P<0.05). The good rate of the study group was higher than that of the control group (95.65%), and the difference was statistically significant (P<0.05), as shown in Table 4.
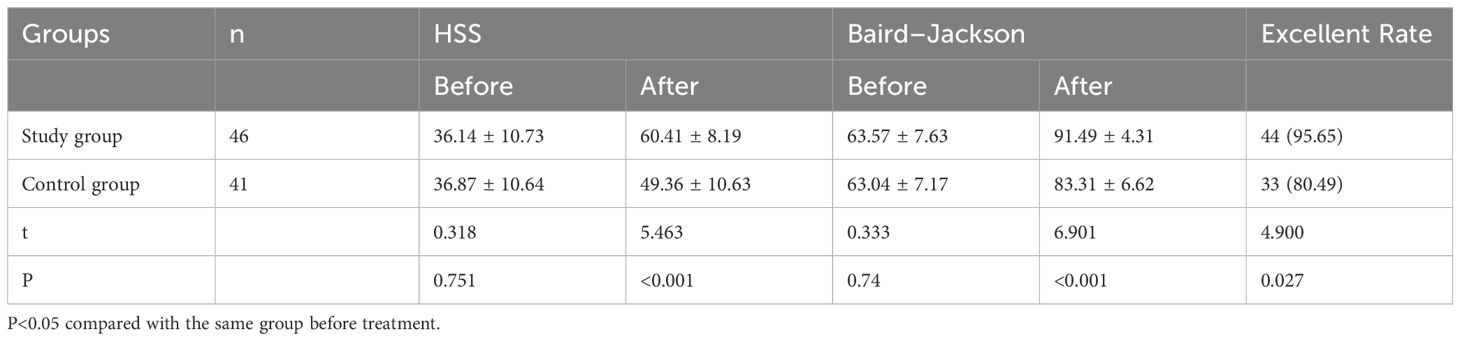
Table 4. Comparison of limb function between the two groups before and after treatment [(x ± s), n(%)].
4 Discussion
The tibia, a crucial long bone, is prone to open fractures from an external force, leading to clinical treatment challenges and a high risk of bone infections. Open fractures often result in poor soft tissue conditions, joint stiffness, and ligament contraction, affecting recovery (Yisireyili et al., 2017). Postoperative bone infections are a critical issue in orthopedic clinics due to long treatment times, high disability rates, and poor outcomes. Antibiotic bone cement can locally prevent and treat infections, but its effectiveness is limited in tibial fracture patients with secondary bone infections due to soft tissue defects and biofilm-protected bacteria (Christersson et al., 2018; Ma et al., 2022). This study found similar pathogen distributions as previous research, with Gram-positive bacteria (49.42%), Gram-negative bacteria (36.78%), and fungi (13.80%). Advances like the VSD technique have improved bone infection cure rates by creating a sealed negative pressure environment that promotes wound healing, reduces secondary infections, and enhances microcirculation (Krappinger et al., 2015). The study showed significant improvements in inflammatory levels and limb function in the VSD group, consistent with prior research (Ma et al., 2018). VSD reduced surgery and treatment times, enhanced recovery, and minimized drug side effects and patient pain. However, limitations include a small sample size (87 patients), potential bias from random group assignment and a single-center location, short follow-up time, and diverse pathogen distribution. Future research should expand sample sizes, include multi-center studies, and conduct long-term follow-ups to fully evaluate VSD’s efficacy and safety, especially in patients with specific pathogens (Huang et al., 2021).
To reduce potential bias, future studies should further optimize randomization and blinding design. For example, a double-blind or triple-blind design could be used to ensure objectivity and accuracy of the results. Future studies should extend the follow-up period to fully evaluate the long-term efficacy of VSD techniques. At the same time, we should pay attention to the quality of life of patients, the incidence of complications, and other indicators to understand the clinical value of VSD technology more comprehensively. Future studies could focus on the efficacy and safety of VSD in patients infected with specific pathogens, such as drug-resistant bacteria. More effective treatment options could be developed for these patients through subgroup analysis or specialized studies. Future studies could explore the combination of VSD technology with other treatment methods (such as antibiotic bone cement, and membrane induction technology). By optimizing the treatment plan, the efficacy and safety of patients with secondary bone infection after tibial fracture surgery can be further improved. In conclusion, if the wound cannot be closed, VSD can improve the surgical index and inflammatory factor level of the patients, and promote the recovery of limb function after internal fixation of tibial fracture, and is thus worth popularizing and applying in the clinic.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Affiliated Hospital of Shandong SecondMedical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SC: Writing – original draft, Writing – review & editing. YW: Writing – original draft, Writing – review & editing. ZZ: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Chastain, D. B., Davis, A. (2019). Treatment of chronic osteomyelitis with multidose oritavancin: A case series and literature review. Int. J. Antimicrob. Agents 53, 429–434. doi: 10.1016/j.ijantimicag.2018.11.023
Christersson, A., Larsson, S., Sörensen, J. (2018). Presurgical localization of infected avascular bone segments in chronic complicated posttraumatic osteomyelitis in the lower extremity using dual-tracer PET/CT. EJNMMI Res. 8, 65. doi: 10.1186/s13550-018-0426-0
Deng, Y., Wang, L., Zhang, Y., Sun, D., Min, H., Zhou, H., et al. (2023). HBx promotes hepatocellular carcinoma progression by repressing the transcription level of miR-187-5p. Aging (Albany NY) 15, 7533–7550. doi: 10.18632/aging.204921
Huang, K., Lin, B. Y., Ren, H. Y., Liu, Y. Y., Zhang, Z., Zhai, L. F., et al. (2021). Surgical treatment of traumatic osteomyelitis of extremities with MRSA infection. Zhongguo Gu Shang 34, 550–553.
Jiang, N., Li, S. Y., Zhang, P., Yu, B. (2020). Clinical characteristics, treatment, and prognosis of squamous cell carcinoma arising from extremity chronic osteomyelitis: a synthesis analysis of one hundred and seventy six reported cases. Int. Orthop 44, 2457–2471. doi: 10.1007/s00264-020-04737-0
Krappinger, D., Lindtner, R. A., Zegg, M., Dal Pont, A., Huber, B. (2015). Masquelet technique for the treatment of large dia- and metaphyseal bone defects. Oper Orthop Traumatol 27, 357–368. doi: 10.1007/s00064-014-0300-9
Li, Y., Wang, L. (2018). Changes in inflammatory factors in patients with osteoporotic vertebral compression fracture and influences of rehabilitation training on postoperative functional recovery and inflammation. J. Musculoskelet Neuronal Interact. 18, 272–279.
Ma, L., Liu, H., Tang, H., Zhang, Z., Zou, L., Yu, H., et al. (2022). Clinical characteristics and outcomes of chronic nonbacterial osteomyelitis in children: a multicenter case series. Pediatr. Rheumatol Online J. 20, 1. doi: 10.1186/s12969-021-00657-4
Ma, X., Han, S., Ma, J., Chen, X., Bai, W., Yan, W., et al. (2018). Epidemiology, microbiology and therapeutic consequences of chronic osteomyelitis in northern China: A retrospective analysis of 255 Patients. Sci. Rep. 8, 14895. doi: 10.1038/s41598-018-33106-6
Mora-Zúñiga, A., Cárdenas-Arellano, F., Cruz-Munguía, J. D., Hernández-Carrillo, J. E. (2021). Chronic osteomyelitis of the tibia; use of bioactive glass as a treatment alternative. Acta Ortop Mex 35, 461–464.
Tudan, C. (2023). Good clinical practices in the bioanalytical laboratory. Bioanalysis 15, 1381–1388. doi: 10.4155/bio-2023-0150
Wang, X., Wang, Z., Fu, J., Huang, K., Xie, Z. (2017). Induced membrane technique for the treatment of chronic hematogenous tibia osteomyelitis. BMC Musculoskelet Disord. 18, 33. doi: 10.1186/s12891-017-1395-6
Keywords: VSD, bone infection secondary to tibial fracture, distribution of pathogenic bacteria, inflammatory factors, bone infection
Citation: Chang S, Wang Y and Zhang Z (2025) Impact of VSD therapy on surgical outcomes, inflammatory markers, and functional rehabilitation in patients with secondary bone infection following tibial fracture surgery. Front. Cell. Infect. Microbiol. 14:1508424. doi: 10.3389/fcimb.2024.1508424
Received: 09 October 2024; Accepted: 17 December 2024;
Published: 17 January 2025.
Edited by:
Martina Maritati, University of Ferrara, ItalyReviewed by:
Anna Benini, University of Verona, ItalyWenqi Luo, Jilin University, China
Rong Liu, Wuhan Puren Hospital, China
Copyright © 2025 Chang, Wang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zengshan Zhang, emVuZ3NoYW4xMDAzQDE2My5jb20=
 Sheng Chang
Sheng Chang Yu Wang2
Yu Wang2