- 1Department of Medical Laboratory Technology, Kohat University of Science and Technology, Kohat, Pakistan
- 2Department of Cell Biology, School of Life Sciences, Central South University, Changsha, China
- 3Key Laboratory of Imaging Diagnosis and Minimally Invasive Intervention Research, Zhejiang Engineering Research Center of Interventional Medicine Engineering and Biotechnology, Key Laboratory of Precision Medicine of Lishui City, Lishui Hospital of Zhejiang University, Lishui, China
- 4School of Computing Sciences, Pak-Austria Fachhochschule: Institute of Applied Sciences and Technology, Haripur, KPK, Pakistan
- 5Department of Microbiology University of Swabi, Swabi, Pakistan
- 6School of Pharmacy and Biomolecular Sciences, Royal College of Surgeons (RCSI) University of Medicine and Health Sciences, Dublin, Ireland
- 7Department of Zoology, College of Science, King Saud University, Riyadh, Saudi Arabia
- 8Department of Stomatology, Ditmanson Medical Foundation Chia Yi Christian Hospital, Chiayi, Taiwan
- 9Department of Pathology, Ditmanson Medical Foundation Chia-Yi Christian Hospital, Chiayi, Taiwan
- 10Department of Cosmetic Science, Chia Nan University of Pharmacy and Science, Tainan, Taiwan
- 11Doctoral Program in Translational Medicine, National Chung Hsing University, Taichung, Taiwan
- 12Department of Biotechnology and Bioindustry Sciences, College of Bioscience and Biotechnology, National Cheng Kung University, Tainan, Taiwan
Objective: The reappearance of monkeypox in non-endemic countries has preceded critical public health concerns. The public’s adherence to preventative measures is influenced by their understanding of the infectious monkeypox virus (Mpox), attitude toward it, and perceptions of it. We conducted this study to evaluate the general population’s knowledge, attitude, and perceptions of Mpox in Pakistan.
Methods: From August 15 to August 30, 2022, 3465 participants in this cross-sectional study provided information via an online survey. The survey has 37 questions divided into four categories: sociodemographic, knowledge, attitude, and perceptions of Mpox. Statistical analyses were performed in Jupyter Notebook using Python 3 and the Pandas, Matplotlib, and stats libraries.
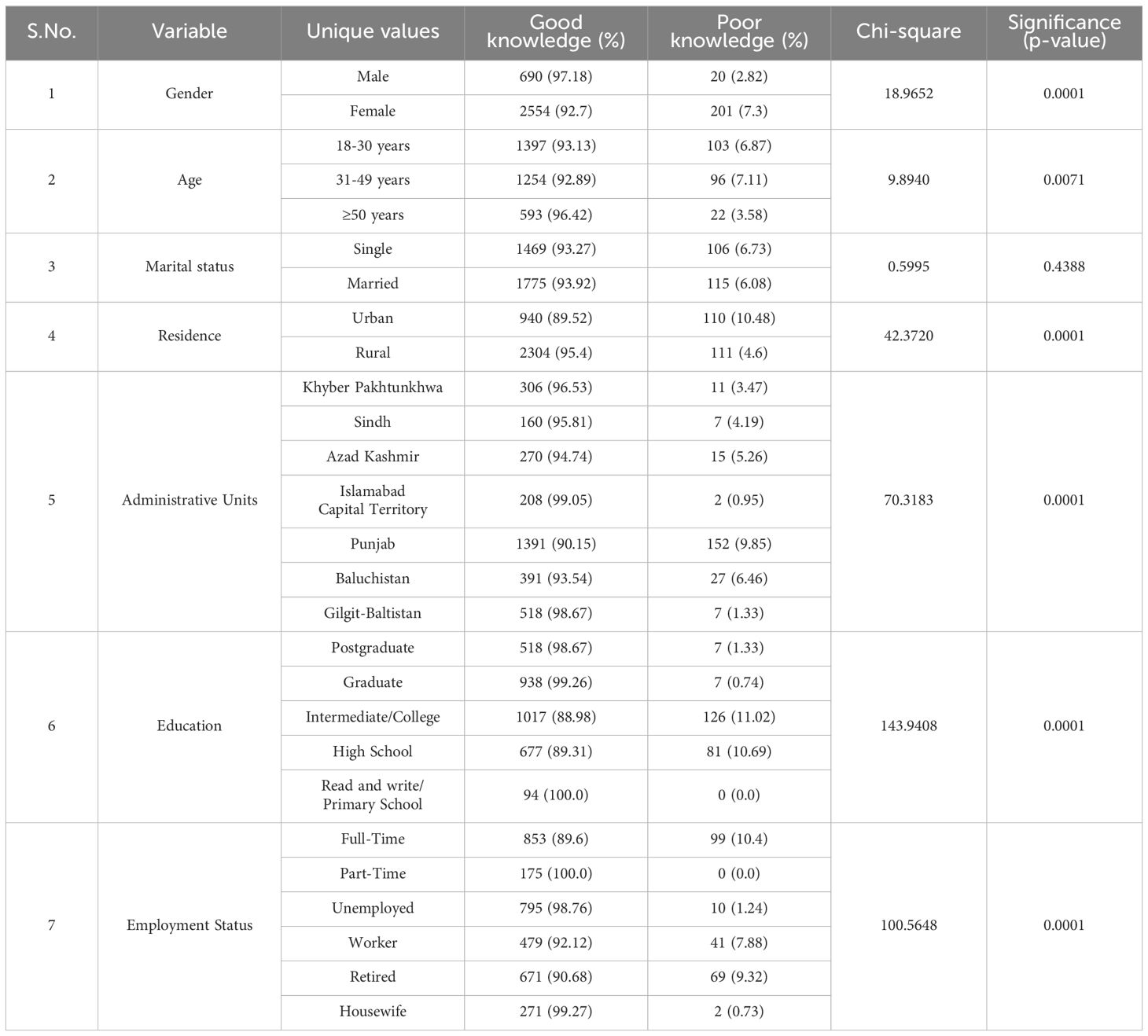
Results: The chi-square test and regression analysis evaluated factors related to Mpox knowledge, attitude, and perception of three thousand four hundred sixty-five participants. Among the participants, about 79.51% (2755) were male, and 32.99% (1143) had post-graduation level education. About 521(99.24) participants with post-graduation education have positive knowledge with a p-value of 0.0001. Approximately 66.78% (2314) of participants answered that Mpox is prevalent in African countries. Almost 85.69% (2969) stated that a virus causes Mpox, and more than 72.18% (2501) said that Mpox spreads through contaminated surfaces. About 60.52% (2097) of participants answered that antivirals are required in treating Mpox patients. Around more than half of the participants, 52.64% (1824), believe that those who receive the chickenpox vaccination are protected against Mpox. It’s interesting to note that most research participants felt favorably about Mpox. Around 90.22% (3126) of participants believed Mpox would be effectively eradicated. Most participants, 86.7% (3004), believe that people should care more about one another nowadays, and 81.36% (2819) believe visiting areas with a Mpox outbreak is risky. About 83.95% (2909) answered that during interaction with the Mpox patient, they’d dress in the appropriate personal protective clothing, like masks, gloves, and gowns. At the same time, 77.66% (2691) responded that they would perform hand hygiene after touching the patients’ surroundings, like beds, tables, doors, etc.
Conclusions: Maximum research participants showed good attitudes and knowledge about Mpox. However, it is essential to start and execute a planned planning framework for public health awareness to avoid the occurrence and spread of Mpox in Pakistan.
1 Introduction
Mpox, formerly known as monkeypox, is a zoonotic viral infection that has gained international attention due to its rising incidence and potential to spread globally. Initially identified in 1958, Mpox is primarily found in tropical rainforest regions of Central and West Africa, with occasional outbreaks outside these areas due to international travel and global interconnectedness (Di Giulio and Eckburg, 2004; Kaler et al., 2022; Shafaati et al., 2022; Khattak et al., 2023a; Ali et al., 2024). The recent surge in cases worldwide has raised concerns about the disease’s potential to become a significant public health threat, particularly in regions where it has not been documented, such as South Asia (Bunge et al., 2022). Mpox is similar to the smallpox virus, sharing many clinical features, including fever, lymphadenopathy, and a characteristic rash. However, Mpox has distinct transmission modes, primarily spreading through close contact with infected individuals, contaminated materials, or animal vectors (Anwar et al., 2023; Khattak et al., 2023a; Khattak et al., 2023b; Zandi et al., 2023). While Mpox is generally less severe than smallpox, the absence of widespread immunity due to the cessation of smallpox vaccination programs increases susceptibility among younger populations. With no specific treatment currently available, prevention through awareness and behavioral modification remains critical to managing the spread of Mpox (Reynolds et al., 2006; Anwar et al., 2023).
The recent outbreak started because of the West African clade (Ogoina et al., 2019) when the United Kingdom Health Security Agency recorded the first case of Mpox on May 7, 2022. Since then, a steady stream of Mpox cases has been reported to the World Health Organization (WHO) (Sah et al., 2022a; Zumla et al., 2022). On July 23, 2022, WHO classified Mpox as a public health emergency of worldwide concern (W.H.O, 2022). As of 1st December 2022, there were more than 81,000 Mpox cases worldwide, an increase from the previous year (W.H.O.a.o.D.A).
Despite Mpox being recorded in several Southeast Asian nations (India, Thailand, and Indonesia) (World Health Organization; REUTERS, 2022), there has been no confirmed Mpox in Pakistan. The National Institute of Health debunked the rumor of Mpox cases in Pakistan on May 24, 2022, despite reports of two uncommon instances of the zoonotic Mpox (c.N.D.n.R.o.M.A.D, 2022). The lack of awareness among the general population of the WHO is one obstacle to preventing the re-emergence of Mpox (World Health Organization, 2022), with most people, doctors, and politicians in impoverished nations unaware of Mpox (EMA, 2022). As a preventive measure, it is crucial to spread “knowledge” to limit the rapid spread of the disease. The scientific and media communities should be engaged to drive the “attitude” of every section of the community. While the world is already facing one pandemic, the goal is to contain the disease with appropriate “practices” based on the “Knowledge, Attitudes and Perceptions” regarding this infectious disease. A community’s collective knowledge, attitudes, and perceptions significantly determine how far a virus may spread within a given area (Ahmed et al., 2021; Tahir et al., 2021; Khattak et al., 2022a). There is a lack of knowledge about fundamental health rights because of ignorance and illiteracy. General populations should be better equipped to alert the public if a pandemic occurs. Targeting this general population is done mainly for this purpose.
Another significant difficulty is the health system’s reactivity, exacerbated by the fact that we typically uncover issues after they have become complicated and take a reactive rather than proactive approach. If Mpox spreads, an already creaking healthcare system will be at the point of disaster. There is no viral diagnostic facility in Pakistan. Still, the health department has proclaimed that in an emergency, samples may be sent outside for testing, which increases the possibility of the virus spreading. To deal with this circumstance, it is necessary to understand the disease’s presenting signs and symptoms to guarantee the prompt quarantine of suspected patients rather than symptomatic therapies. Hospitals should also have well-equipped isolation facilities ready to place patients under quarantine immediately to stop the spread of the dangerous virus.
This study aims to assess the knowledge, attitudes, and perceptions of the Pakistani population regarding Mpox to inform public health strategies. By identifying current knowledge levels and misconceptions, the study seeks to provide insights to guide the development of targeted educational campaigns, improve community engagement, and enhance preventive measures against Mpox in Pakistan. Understanding these factors is crucial to ensuring that public health interventions are effectively designed and implemented, ultimately contributing to the broader goal of safeguarding public health in the face of emerging infectious diseases.
2 Materials and Methods
2.1 Study design
From August 15 to August 30, 2022, we performed cross-sectional web-based research with the general Pakistani population. According to the most recent census, Pakistan’s population is 207.07 million (Pakistan., B.o.S.G.o, 2017). The study was open to all Pakistanis aged 18 and older who could understand English. The required sample was determined using the Raosoft sample size calculator. The estimated minimum sample size needed was 385. A 50% response distribution was considered for the sample estimate, along with a 5% margin of error and a 95% confidence level. To get more exact and accurate results, we gathered 3465 respondents for the survey.
2.2 Data collection tool
To collect data, we conducted an online survey. Cronbach’s Alpha test was utilized to evaluate the reliability of the knowledge attitude and perceptions questions independently. The value of Cronbach’s Alpha for knowledge is 0.81, and attitude is 0.77 and 0.69 for perception. It shows that Knowledge questions are more strongly consistent than Attitude and Perception. Recruitment was conducted using convenience sampling combined with a simplified snowball sampling technique. The survey was configured to accept only one response per participant, verified through their email addresses. Participants could complete and submit the survey using a computer or a mobile device. The questionnaire was divided into four sections: Data on sociodemographic characteristics were included in the first part, in addition to gender, age, Marital status, Residence, Administrative Units, education, and employment status. The second section contained twenty-three multiple-choice questions designed to measure knowledge. The third had nine attitude-testing questions, while the fourth contained six developed perception-testing questions on the Mpox. The study’s instruments were modified from previous studies (Harapan et al., 2017; Harapan et al., 2018; Harapan et al., 2019; Harapan et al., 2020; Khattak et al., 2021; Alshahrani et al., 2022; Khattak et al., 2022a; Khattak et al., 2022b). “Yes,” “No,” and “Not sure” were the only options given to respondents for each question. The survey was written in English.
2.3 Data collection procedure
No personal information was required in the survey, like a person’s name, address, or any other information that may be used to identify them. Using a specific platform Google Forms link, participants were invited to complete a structured questionnaire (see Supplementary Materials 1). We circulated it through social media sites like Twitter, Facebook, and WhatsApp. The survey link was shared with different groups on WhatsApp and Facebook, and the admin and members of these groups were requested to share the link to get enough responses. Before starting the replies, each respondent was asked to confirm they had informed permission by clicking the consent declaration. “I do with this, after reading the aims of the study, engage in the survey supplying my information by answering questions rationally and willingly,” was the informed consent statement offered to the respondents. Respondents filled out the survey and clicked the “submit” button to send it to our platform for data collection. To confirm the authenticity of the responses, all questions were compulsory to be answered.
2.4 Study variables
A total of 23 knowledge questions with “Yes,” “No,” and “Not Sure” response options were used to gauge how well-informed the Pakistani people were about Mpox. The knowledge score was 0 (lowest) to 23 (highest). Age, which was divided into groups of 18 to 30 years, 31 to 49 years, and more or equal ≥50 years; gender (male or female); marital status (single or married); participants’ residency area of Pakistan (Khyber Pakhtunkhwa, Sindh, Azad Kashmir, Islamabad Capital Territory, Punjab, Baluchistan, and Gilgit-Baltistan); and urban or rural area. Furthermore, participants were asked about employment status, and education was divided into five levels: postgraduate, graduate, college, high school, read and write,/primary school. Six questions focused on perception, and nine on attitude and practice in anticipating the disease.
2.5 Statistical analysis
The responses collected via Google Forms were exported to Microsoft Excel. Statistical analysis was conducted in Jupyter Notebook using Python 3 and the Pandas, Matplotlib, and stats libraries. Factors linked with Mpox knowledge, attitude, and perception were discovered using chi-square and Multiple regression analysis. Descriptive statistics such as frequency and percentage were employed to demonstrate the demographic features of the research participants. The chi-square test and Multiple regression analysis were conducted to evaluate response variables and explanatory factors. A P-value of 0.05 was set to determine statistical significance.
2.6 Ethical consideration
The methods utilized in this investigation follow the Helsinki Declaration and the ethical guidelines of relevant national and institutional committees on human experimentation. The Ethical Research Committee of the Department of Microbiology approved the study at the University of Swabi, Pakistan (F.No.1(3)-Micro-8/UOS/2022/1878).
3 Result
3.1 Characteristics of respondents
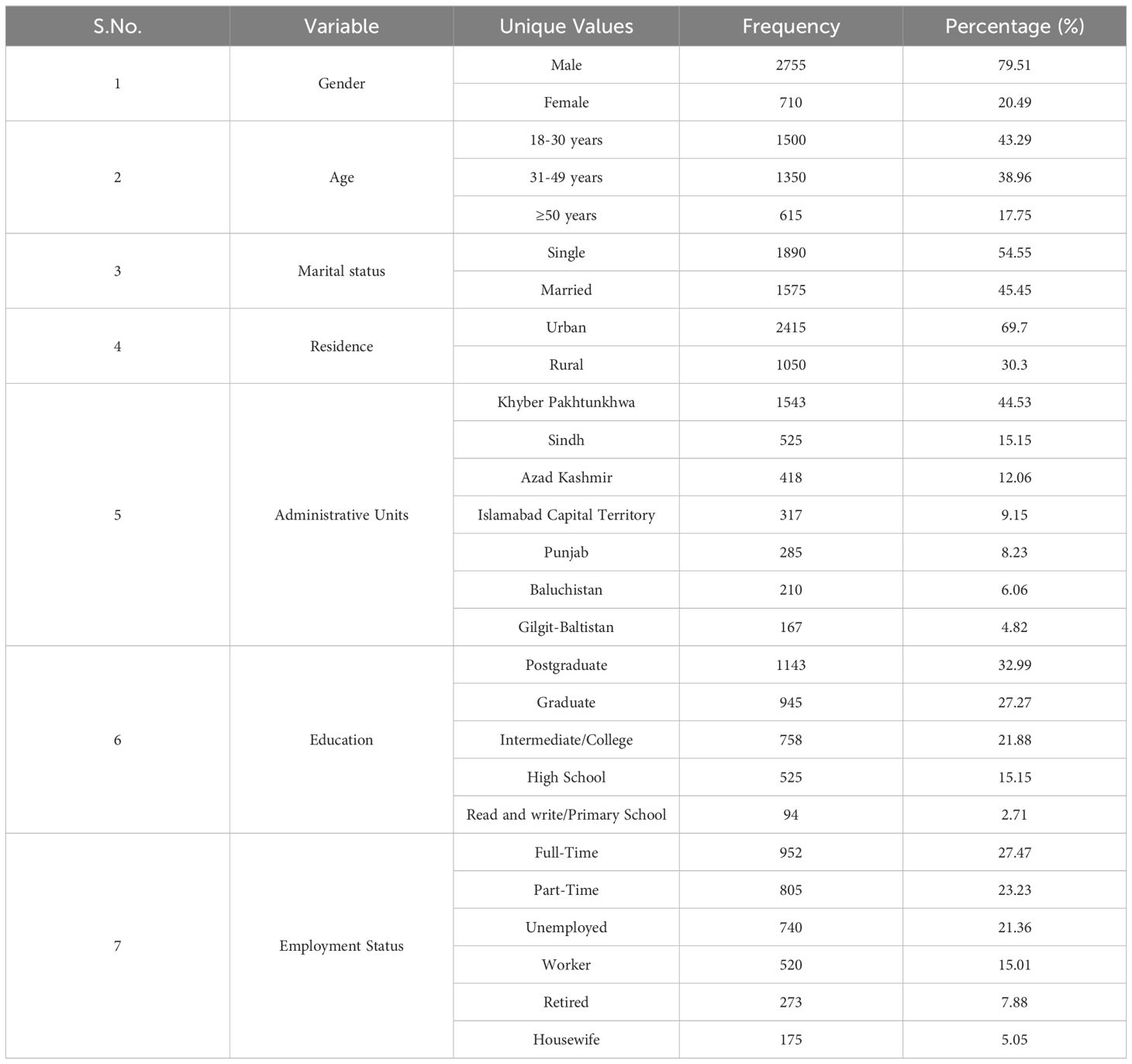
In the final analysis, 3465 research participants were recruited, with 79.51% being men, just 20.49% being females, and 44.53% being Khyber Pakhtunkhwa citizens. Most respondents were 18–30 (43.29%) and from Urban areas (69.7%). 32.99% of participants have a postgraduate level of education. According to the marital status findings, most participants (54.55%) were single, and 27.47% worked full-time. Table 1 provides a summary of the research participants’ demographic characteristics.
3.2 Knowledge
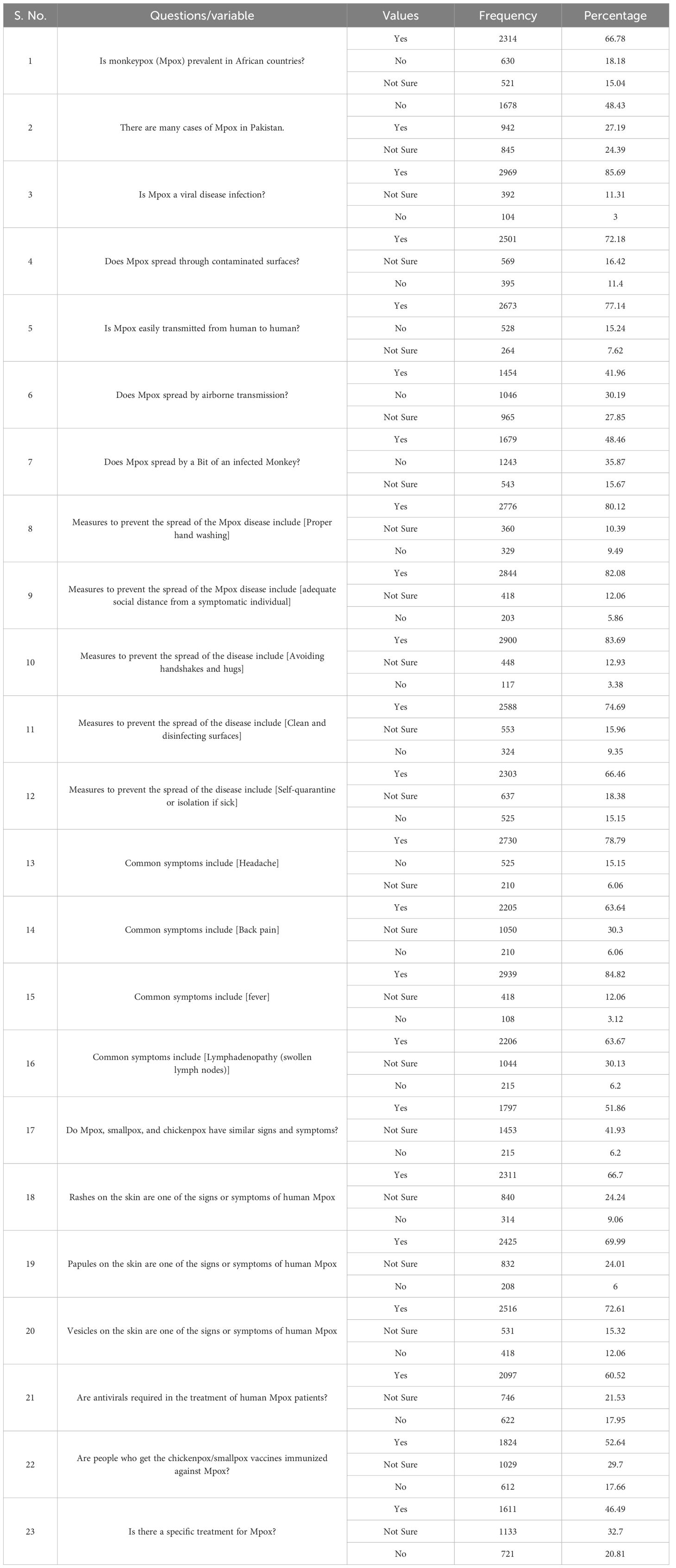
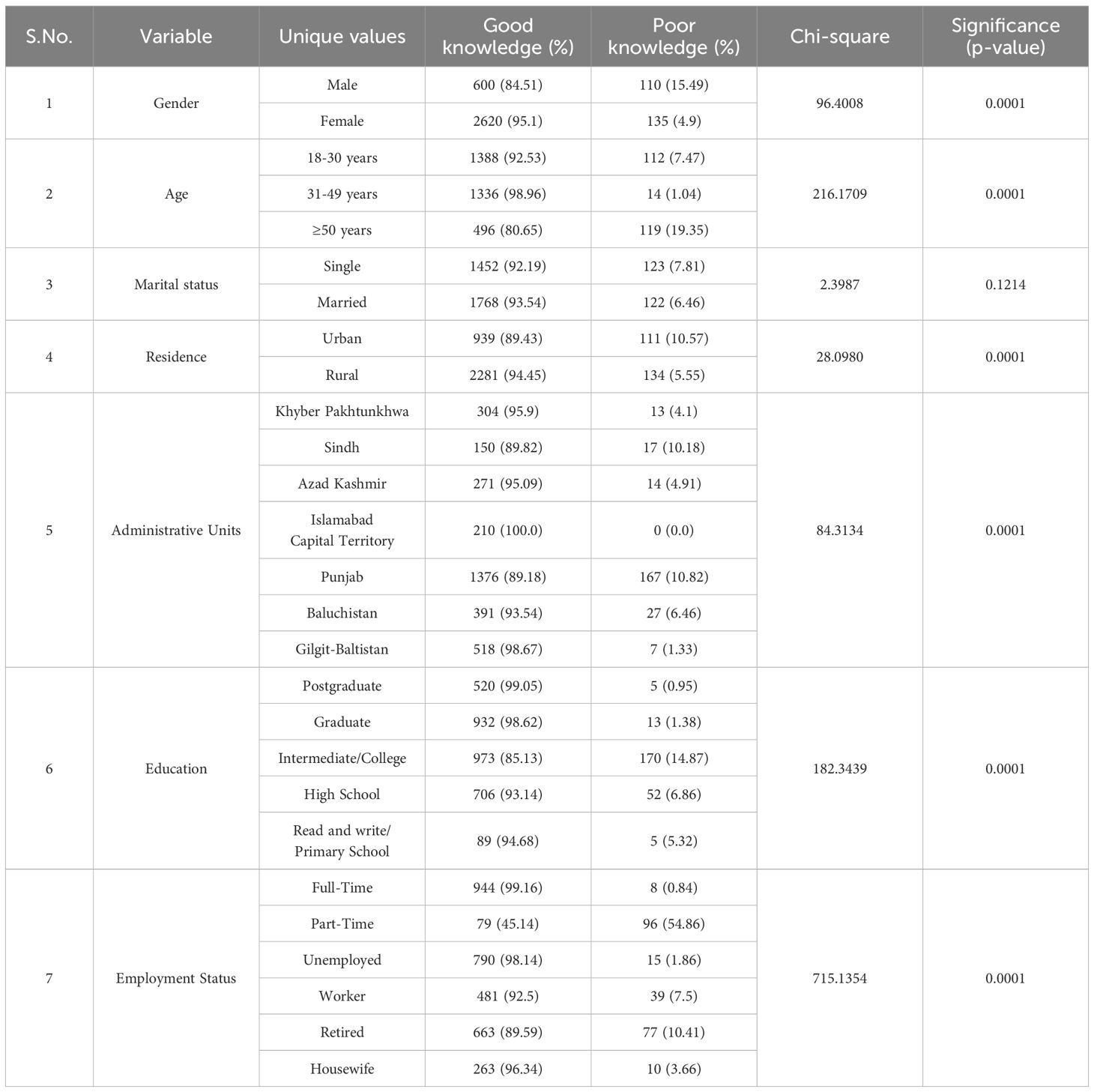
Tables 2, 3; Supplementary Material S2 display the replies to inquiries testing participants’ knowledge of Mpox. Of the male participants, 79.58% (565) have high positive knowledge about Mpox compared to female participants. The 18-29 participants have more positive knowledge than others, with a p-value of 0.0001. Same in marital status, 78.94% (1492) married participants have high positive knowledge related to single participants with a p-value of 0.0008. Approximately 48.43% (1678) affirmed that there had not been any reports of Mpox in humans in Pakistan. Nevertheless, several queries received incorrect responses, such as, A human Mpox case has been confirmed in Pakistan, according to around 27.19% (942) of respondents. Almost 85.69% (2969) stated that a virus causes Mpox, and about 72.18% (2501) said that Mpox spreads through contaminated surfaces. At the same time, approximately 77.14% (2673) of the participants believed that Mpox is easily transmitted from human to human, 48.46% (1679) by Bit of an infected Monkey, and 41.96% (1454) by airborne transmission. The majority of participants thought the section on measures to stop disease transmission was that proper handwashing 80.12% (2776), adequate social distance 82.08% (2844), avoiding handshakes and hugs 83.69% (2900), and cleaning and disinfecting surfaces 74.69% (2588) were utterly essential. Furthermore, 66.46% (2303) of participants said that quarantining sick people alone was a preventative process to stop the spread of disease.
3.3 Attitudes
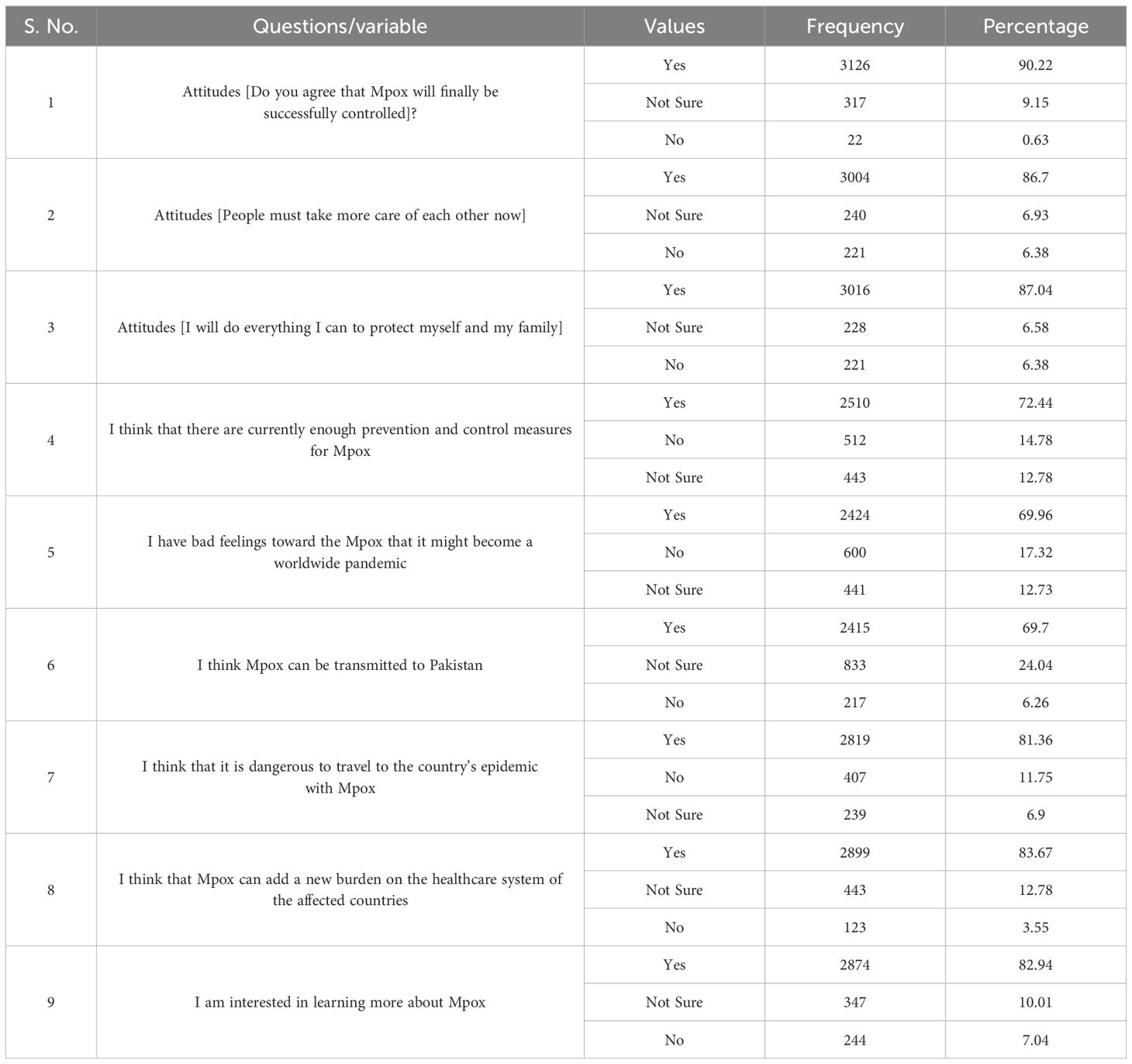
Tables 4, 5; Supplementary Material S2 depict the participants’ attitudes toward Mpox. Remarkably, most research participants had a positive attitude toward Mpox. Most participants, 90.22% (3126), believed Mpox could be managed effectively. Around 86.7% (3004) of participants said that individuals should show more concern for one another nowadays. Furthermore, responding that they would go above and beyond to take care of themselves and their family members was 87.04% (3016) of the participants. There are now sufficient preventative and control methods for Mpox, according to about 72.44% (2510) of respondents. Around approximately 69.96% (2424) of participants have bad feelings toward Mpox; considering the possibility that it may spread globally, 69.7% (2415) think Mpox can be transmitted to Pakistan, and 81.36% (2819) believe that visiting the region where the Mpox pandemic is prevalent is risky. Also, 83.67% (2899) of participants think Mpox might burden the impacted nations’ medical systems. While 82.94% (2874) of participants are concerned with learning more about Mpox, Tables 4, 5 provide the details of these sections.
3.4 Perception
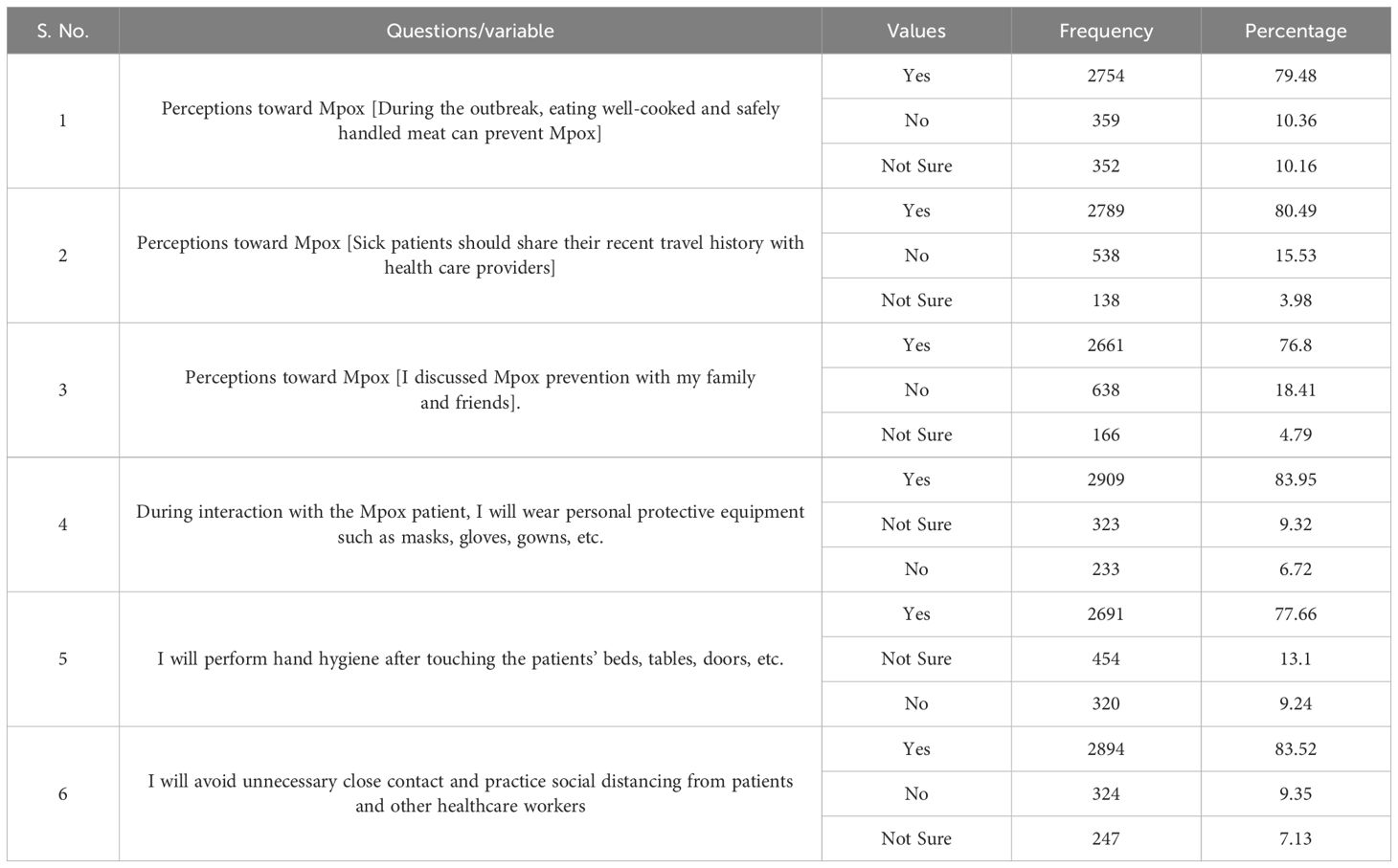
Tables 6, 7; Supplementary Material S2 include the results of the perception questionnaire evaluating participants’ perceptions of several characteristics of Mpox. In total, 79.48% (2754) stated “handling and eating adequately cooked meat might help avoid disease, 80.49% (2789) said that medical professionals should be informed of sick patients’ recent travel history, and 76.8% (2661) participants discussed Mpox prevention with family and friends. About 83.95% (2909) answered that during interaction with the Mpox patient, they would wear the proper personal protective clothing, like masks, gloves, and gowns. At the same time, 77.66% (2691) of the participants answered that they would wash their hands after contacting the patients’ surroundings, such as beds, tables, doors, etc. However, 83.52% (2894) of participants said they would avoid inappropriate close contact and practice social distancing from patients and other healthcare professionals.
4 Discussion
As global cases of Mpox continue to rise, Pakistan needs to enhance its preparedness. While public health officials focus on prevention and epidemic management, success depends heavily on public engagement. Understanding the Pakistani population’s knowledge, attitudes, and perceptions towards Mpox is essential for developing effective public health interventions, including educational campaigns and community participation in management, prevention, and care efforts.
This study reveals a high awareness of Mpox among the Pakistani public, with 85.69% of respondents correctly identifying it as a viral infection. These findings highlight a notable difference compared to previous studies that have reported significant knowledge gaps between healthcare workers and the public regarding other infectious diseases, such as measles and dengue (Ahmed et al., 2022; Alsanafi et al., 2022; Nath et al., 2022; Sallam et al., 2022). This lack of information is unsurprising given that Mpox is a reemerging infectious disease with no documented cases in Pakistan or South Asia. Our results are consistent with findings from a Malaysian study that reported over 95% of respondents were aware of dengue fever during an outbreak despite limited knowledge about its transmission and treatment (Naing et al., 2011). Similarly, a pilot study among hospital visitors in Karachi, Pakistan, found that only 38.5% of participants had adequate knowledge of viral diseases, even though 90% knew their existence (Itrat et al., 2008). Another study from Pakistan noted that only 35% of individuals, regardless of socioeconomic status, had sufficient awareness of dengue during the epidemic, paralleling data on public awareness of the COVID-19 pandemic (Syed et al., 2010).
This consistency in public awareness of infectious disease symptoms and preventive measures reflects an encouraging baseline for future public health campaigns targeting emerging threats like Mpox. For instance, studies on COVID-19 indicated that 90-96% of Pakistani participants were knowledgeable about its symptoms, transmission routes, and prevention (Khattak et al., 2022b). However, further research has shown that approximately 90% of individuals were familiar with various infectious diseases’ clinical manifestations and symptoms (Khattak et al., 2021). This underscores the importance of enhancing public understanding of Mpox, especially as an emerging viral threat (Cheema et al., 2017). The relative absence of Mpox awareness in Pakistan is partly due to the country’s climate and the historical lack of outbreaks, as Mpox is primarily endemic to tropical rainforest regions (Damon, 2011; Durski et al., 2018). For travelers to endemic areas, such as the Democratic Republic of Congo (DRC) and China, raising awareness about Mpox and related diseases is essential for encouraging preventive measures (Nolen et al., 2016; Hadi et al., 2020).
Our study found that participants were well informed about the causes of Mpox, with notable awareness of its transmission through contaminated surfaces (72.18%), human-to-human contact (77.14%), airborne exposure (41.96%), and animal bites (48.46%). Key preventive measures recognized by participants included proper hand washing (80.12%), social distancing (82.08%), avoiding physical contact (83.69%), disinfecting surfaces (74.69%), and self-quarantine if sick (66.46%). The most well-known symptoms included fever (84.82%), headache (78.79%), rash (66.7%), and vesicles on the skin (72.61%). These findings are consistent with previous studies that reported high public knowledge of disease prevention and common symptoms (Jamil et al., 2022). Given the similarities between smallpox and Mpox regarding symptoms, transmission, and prevention strategies, the widespread recognition of Mpox symptoms may be partially attributed to public familiarity with smallpox (Petersen and Damon, 2015; Bunge et al., 2022; Kmiec and Kirchhoff, 2022). However, only 52.64% of participants knew that the smallpox vaccine also offers protection against Mpox, suggesting the need for more education on this aspect of prevention (Earl et al., 2004; Edghill-Smith et al., 2005).
Most participants displayed positive attitudes towards prevention, agreeing that isolating infected individuals and adopting protective measures, such as face masks and hand hygiene, could help control the spread. This is likely influenced by recent experiences during the COVID-19 pandemic, when preventive measures were the primary defense before vaccines were available (Hemati et al., 2022). Moreover, the guidance from global health authorities like the CDC and WHO may have contributed to the public’s adherence to recommended practices.
Gender and education levels were significant factors influencing knowledge and perceptions. Similar to earlier research, our study found that male participants were more aware of Mpox (Nath et al., 2022). This may be linked to the higher prevalence of Mpox cases among men who have sex with men, as noted in recent outbreaks (Seang et al., 2022; Bragazzi et al., 2023). A pooled meta-analysis showed that over 91% of recent Mpox cases involved sexual contact (Sah et al., 2022b), and a UK health center reported that all detected Mpox cases were among men who have sex with men (Girometti et al., 2022). Participants with higher education levels demonstrated better knowledge than those with only primary or secondary education, consistent with previous findings that associate higher education with greater health awareness and protective behaviors (Li et al., 2020; Raghupathi and Raghupathi, 2020). This may be attributed to increased access to information through the media, the internet, and educational resources.
Geographic and socio-economic disparities also played a role, with urban residents showing greater awareness than those in rural areas, reflecting findings from similar studies in other developing nations (Wen et al., 2020). This discrepancy can be attributed to greater access to mainstream media, the Internet, and educational resources in urban settings (Ahdab, 2020). Limited resources for health education in rural areas and insufficient support for medical professionals may contribute to lower awareness levels in these communities.
Mpox, as an emerging infectious disease, poses a significant threat to global public health (Kmiec and Kirchhoff, 2022; Shafaati and Zandi, 2022). Preventive measures are crucial in mitigating the spread of Mpox, especially without a dedicated vaccine. Raising awareness through targeted campaigns and educational initiatives can prevent outbreaks of contagious diseases like Mpox, COVID-19, influenza, and dengue from escalating into pandemics (Ismail and Ahmed, 2010; Tahir et al., 2020; Mahmood et al., 2022). Public engagement is critical; without widespread cooperation, efforts to enhance public health interventions through studies evaluating knowledge and attitudes are less effective (Tomar et al., 2021; Riccò et al., 2022).
Given Pakistan’s diverse population and varying access to information, knowledge levels about Mpox are likely to differ. Those without internet access or living in areas with limited outreach may have lower awareness, emphasizing the need for targeted education programs. Our study highlights the importance of multifaceted interventions, such as community engagement and media campaigns, which have been successful in the past and can be adapted to improve Mpox awareness and prevention (Ahinkorah et al., 2020; Geoffrion et al., 2020; Ali et al., 2022).
Healthcare professionals, social workers, and community partners should cooperate with multi-sectoral organizations to gather resources for Mpox awareness. Combining situational data into local and national studies can guide efficient practices and update policy. A national data dashboard for real-time decision-making would further support public health works. Taking the initiative measures, informed via lessons from COVID-19 and other epidemics, is essential for strengthening Pakistan’s response approaches.
5 Study limitations and strengths
Numerous limitations should be considered when assessing the outcomes of this research. Firstly, the use of a convenience sampling method leads to the potential for selection bias. Secondly, the survey was circulated online through various social media platforms, which could lead to bias, as individuals from lower socioeconomic backgrounds might have been excluded, limiting the capacity to generalize the results to the larger population. Thirdly, since the research relied on previously published studies in English, there could be a language bias in the data, which may have influenced participants’ responses, especially in relation to complex or technical topics. Respondents may have also given socially desirable answers to questions about their attitudes and perceptions, aligning their responses with what they believed was expected of them. Fourth, the survey is subject to recall bias, which could have affected the accuracy of the participants’ responses.
Additionally, since most participants were married and residing in urban areas, any results stratified by these factors should be taken with concern. Also, the sample included 79.51% males, which may affect the generalizability of the outcomes, remarkably in relation to gender-specific trends, and should be admitted as a limitation. Another issue is that the questionnaire was only available in English, which could have excluded less educated individuals, specifically in a developing country, concerning the representativeness of the sample. Yet, the large sample size of the study strengthens its outcomes. Eventually, the insights from this research could be effective for health officials in getting targeted policies to combat the spread of Mpox in Pakistan.
6 Conclusion
Overall, the results of the current study showed that the Pakistani populace has an adequate level of awareness, attitudes, and perception of Mpox. Our findings suggested that excellent information might lead to positive attitudes and views, which is essential for reducing the disease’s escalating effects. Careful epidemiological surveillance is required to prevent the present Mpox outbreak from spreading to other non-endemic nations. Also, there was a strong correlation between participants’ knowledge and their education, gender, age, marital status, place of residence, administrative units, education, and employment status. The results of our study highlight the need to provide more excellent information about Mpox and its preventative strategies. Public awareness campaigns must be launched to increase Mpox’s adherence to preventive advice. They could also highlight the risks to public health posed by this zoonotic illness. Our research may aid in gaining knowledge of the Mpox vaccine and vaccination status among experts, laypeople, and policymakers. To combat this disease, patients must be immunized as soon as possible. Using successful strategies that promote awareness of and combat the spread of Mpox implies the active involvement of global organizations, national health authorities, governments, medical professionals, and the media sectors.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Bioethical Committee of the Department of Microbiology, University of Swabi. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HY: Formal analysis, Investigation, Writing – original draft. AQ: Conceptualization, Methodology, Project administration, Writing – review & editing. MS: Formal analysis, Project administration, Software, Writing – review & editing. MK: Formal analysis, Investigation, Methodology, Software, Writing – review & editing. MF: Formal analysis, Visualization, Writing – original draft. ZK: Formal analysis, Visualization, Writing – review & editing. DF: Funding acquisition, Supervision, Writing – review & editing. Y-CL: Funding acquisition, Validation, Writing – review & editing. C-CC: Funding acquisition, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors extend their appreciation to Researchers Supporting Project number (RSPD2025R965), King Saud University, Riyadh, Saudi Arabia, for funding this work.
Acknowledgments
The authors would like to thank everyone participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2024.1449096/full#supplementary-material
References
Al Ahdab, S. A. (2020). A cross-sectional survey of knowledge, attitude and practice (KAP) towards COVID-19 pandemic among the Syrian residents. BMC Public Health, 21, 1–7. doi: 10.1186/s12889-021-10353-3
Ahinkorah, B. O., Seidu, A.-A., Armah-Ansah, E.K., Budu, E., Ameyaw, E.K., Agbaglo, E., et al. (2020). Drivers of desire for more children among childbearing women in sub-Saharan Africa: implications for fertility control. BMC Pregnancy Childbirth 20, 1–11. doi: 10.1186/s12884-020-03470-1
Ahmed, A., Saqlain, M., Tanveer, M., Tahir, A.H., Ud-Din, F., Shinwari, M.I., et al. (2021). Knowledge, attitude and perceptions about Crimean Congo Hemorrhagic Fever (CCHF) among occupationally high-risk healthcare professionals of Pakistan. BMC Infect. Dis. 21, 1–9. doi: 10.1186/s12879-020-05714-z
Ahmed, S. K., Abdulqadirb, S.O., Omar, R.M., Hussein, S.H., Chandran, D., Sharma, A., et al. (2022). Study of knowledge, attitude and anxiety in Kurdistan-region of Iraqi population during the monkeypox outbreak in 2022: An online cross-sectional study. Research Square. doi: 10.21203/rs.3.rs-1961934/v2
Ali, A., Khaliq, A., Lokeesan, L., Meherali, S., Lassi, Z.S. (2022). Prevalence and predictors of teenage pregnancy in Pakistan: a trend analysis from Pakistan Demographic and Health Survey datasets from 1990 to 2018. Int. Health 14, 176–182. doi: 10.1093/inthealth/ihab025
Ali, Y., Khan, A.A., Alanazi, A.M., Abdikakharovich, S.A., Shah, J.A., Ren, Z.-G., et al. (2024). Identification of the myxobacterial secondary metabolites Aurachin A and Soraphinol A as promising inhibitors of thymidylate kinase of the Monkeypox virus. Mol. Diversity p, 1–14. doi: 10.1007/s11030-023-10764-x
Alsanafi, M., Al-Mahzoum, K., Sallam, M. (2022). Monkeypox knowledge and confidence in diagnosis and management with evaluation of emerging virus infection conspiracies among health professionals in Kuwait. Pathogens 11, 994. doi: 10.3390/pathogens11090994
Alshahrani, N. Z., Alzahrani, F., Alarifi, A.M., Algethami, M.R., Alhumam, M.N., Ayied, H.A.M., et al. (2022). Assessment of knowledge of monkeypox viral infection among the general population in Saudi Arabia. Pathogens 11, 904. doi: 10.3390/pathogens11080904
Anwar, F., Haider, F., Khan, S., Ahmad, I., Ahmed, N., Imran, M., et al. (2023). Clinical manifestation, transmission, pathogenesis, and diagnosis of monkeypox virus: a comprehensive review. Life 13, 522. doi: 10.3390/life13020522
Bragazzi, N. L., Kong, J.D., Mahroum, N., Tsigalou, C., Khamisy-Farah, R., Converti, M., et al. (2023). Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J. Med. Virol. 95, e27931. doi: 10.1002/jmv.27931
Bunge, E. M., Hoet, B., Chen, L., Lienert, F., Weidenthaler, H., Baer, L.R., et al. (2022). The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLoS Negl. Trop. Dis. 16, e0010141. doi: 10.1371/journal.pntd.0010141
Cheema, S., Maisonneuve, P., Weber, I., Fernandez-Luque, L., Abraham, A., Alrouh, H., et al. (2017). Knowledge and perceptions about Zika virus in a Middle East country. BMC Infect. Dis. 17, 1–9. doi: 10.1186/s12879-017-2603-6
c.N.D.n.R.o.M.A.D (2022). No monkeypox case detected in Pakistan yet. Available online at: https://www.dawn.com/news/1691293.
Damon, I. K. (2011). Status of human monkeypox: clinical disease, epidemiology and research. Vaccine 29, D54–D59. doi: 10.1016/j.vaccine.2011.04.014
Di Giulio, D. B., Eckburg, P. B. (2004). Human monkeypox: an emerging zoonosis. Lancet Infect. Dis. 4, 15–25. doi: 10.1016/S1473-3099(03)00856-9
Durski, K. N., McCollum, A.M., Nakazawa, Y., Petersen, B.W., Reynolds, M.G., Briand, S., et al. (2018). Emergence of monkeypox—west and central Africa, 1970–2017. Morbidity mortality weekly Rep. 67, 306. doi: 10.15585/mmwr.mm6710a5
Earl, P. L., Americo, J. L., Wyatt, L. S., Eller, L. A., Whitbeck, J. C., Cohen, G. H., et al. (2004). Immunogenicity of a highly attenuated MVA smallpox vaccine and protection against monkeypox. Nature 428, 182–185. doi: 10.1038/nature02331
Edghill-Smith, Y., Golding, H., Manischewitz, J., King, L. R., Scott, D., Bray, M., et al. (2005). Smallpox vaccine–induced antibodies are necessary and sufficient for protection against monkeypox virus. Nat. Med. 11, 740–747. doi: 10.1038/nm1261
EMA (2022). Tecovirimat SIGA. Available online at: https://www.ema.europa.eu/en/medicines/human/EPAR/tecovirimat-siga.
Geoffrion, S., Hills, D. J., Ross, H. M., Pich, J., Hill, A. T., Dalsbø, T. K.v, et al. (2020). Education and training for preventing and minimizing workplace aggression directed toward healthcare workers. Cochrane Database systematic Rev. 9 Art. No.: CD011860. doi: 10.1002/14651858.CD011860.pub2
Girometti, N., Byrne, R., Bracchi, M., Heskin, J., McOwan, A., Tittle, V., et al. (2022). Epidemiological characteristics and clinical features of confirmed human monkeypox virus cases in individuals attending a sexual health Centre in London, United Kingdom. Lancet Infect. Dis 10, S1473–3099.
Hadi, A. G., Kadhom, M., Hairunisa, N., Yousif, E., Mohammed, S. A. (2020). A review on COVID-19: origin, spread, symptoms, treatment, and prevention. Biointerface Res. Appl. Chem. 10, 7234–7242. doi: 10.33263/BRIAC
Harapan, H., Aletta, A., Anwar, S., Setiawan, A. M., Maulana, R., Wahyuniati, N., et al. (2017). Healthcare workers' knowledge towards Zika virus infection in Indonesia: a survey in Aceh. Asian Pacific J. Trop. Med. 10, 189–194. doi: 10.1016/j.apjtm.2017.01.018
Harapan, H., Aletta, A., Anwar, S., Setiawan, A. M., Maulana, R., Wahyuniati, N., et al. (2018). Attitudes towards Zika virus infection among medical doctors in Aceh province, Indonesia. J. infection Public Health 11, 99–104. doi: 10.1016/j.jiph.2017.06.013
Harapan, H., Rajamoorthy, Y., Utomo, P. S., Anwar, S., Setiawan, A. M., Aletta, A., et al. (2019). Knowledge and attitude towards pregnancy-related issues of Zika virus infection among general practitioners in Indonesia. BMC Infect. Dis. 19, 1–12. doi: 10.1186/s12879-019-4297-4
Harapan, H., Setiawan, A. M., Yufika, A., Anwar, S., Wahyuni, S., Asrizal, F. W., et al. (2020). Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog. Global Health 114, 68–75. doi: 10.1080/20477724.2020.1743037
Hemati, S., Farhadkhani, M., Sanami, S., Mohammadi-Moghadam, F.. (2022). A review on insights and lessons from COVID-19 to the prevent of monkeypox pandemic. Travel Med. Infect. Dis. p, 102441. doi: 10.1016/j.tmaid.2022.102441
Ismail, N. A., Ahmed, H. A. (2010). Knowledge, attitudes and practices related to avian influenza among a rural community in Egypt. J. Egypt Public Health Assoc. 85, 73–96.
Itrat, A., Khan, A., Javaid, S., Kamal, M., Khan, H., Javed, S., et al. (2008). Knowledge, awareness and practices regarding dengue fever among the adult population of dengue hit cosmopolitan. PLoS One 3, e2620. doi: 10.1371/journal.pone.0002620
Jamil, H., Idrees, M., Idrees, K., Tariq, W., Sayyeda, Q., Asghar, M. S., et al. (2022). Socio-demographic determinants of monkeypox virus preventive behavior: a cross-sectional study in Pakistan. bioRxiv 12 (8), e0279952. doi: 10.1101/2022.12.20.521248
Kaler, J., Hussain, A., Flores, G., Kheiri, S., Desrosiers, D. (2022). Monkeypox: a comprehensive review of transmission, pathogenesis, and manifestation. Cureus 14 (7), e26531. doi: 10.7759/cureus.26531
Khattak, S., Khan, M., Usman, T., Ali, J., Wu, D.-X., Jahangir, M., et al. (2021). Assessment of general populations knowledge, attitude, and perceptions toward the coronavirus disease (COVID-19): a cross-sectional study from Pakistan. Front. Med. 8, 747819. doi: 10.3389/fmed.2021.747819
Khattak, S., Idrees, M., Iqbal, H. I., Khan, M., Assad, N., Khan, M. N., et al. (2022a). Assessment of attitudes and intentions towards COVID-19 vaccines and associated factors among general populations of Pakistan: A cross-sectional study. Vaccines 10, 1583. doi: 10.3390/vaccines10101583
Khattak, S., Faheem, M., Nawaz, B., Khan, M., Khan, N. H., Ullah, N., et al. (2022b). Knowledge, Attitude, and perception of cancer patients towards COVID-19 in Pakistan: a cross-sectional study. Int. J. Environ. Res. Public Health 19, 7926. doi: 10.3390/ijerph19137926
Khattak, S., Ali, Y., Ren, Z., Ji, X.-Y. (2023a). Monkeypox entry and emergence preparation in Pakistan (MDPI) 13 (12), 2308.
Khattak, S., Rauf, M. A., Ali, Y., Yousaf, M. T., Liu, Z., Wu, D.-D., et al. (2023b). The monkeypox diagnosis, treatments and prevention: A review. Front. Cell. infection Microbiol. 12, 1088471. doi: 10.3389/fcimb.2022.1088471
Kmiec, D., Kirchhoff, F. (2022). Monkeypox: a new threat? Int. J. Mol. Sci. 23, 7866. doi: 10.3390/ijms23147866
Li, Z.-H., Zhang, X.-R., Zhong, W.-F., Song, W.-Q., Wang, Z.-H., Chen, Q., et al. (2020). Knowledge, attitudes, and practices related to Coronavirus disease 2019 during the outbreak among workers in China: A large cross-sectional study. PLoS Negl. Trop. Dis. 14, e0008584. doi: 10.1371/journal.pntd.0008584
Mahmood, M. M., Rehman, J., Arif, B., Rehman, Z., Aasim, M., Saeed, M. T.. (2022). Knowledge, attitudes and practices of patients with chronic illnesses during the COVID-19 pandemic: A cross-sectional survey from Pakistan. Chronic illness 18, 608–619. doi: 10.1177/17423953211023961
Naing, C., Ren, W. Y., Man, C. Y., Fern, K. P., Qiqi, C., Ning, C. N., et al. (2011). Awareness of dengue and practice of dengue control among the semi-urban community: a cross sectional survey. J. Community Health 36, 1044–1049. doi: 10.1007/s10900-011-9407-1
Nath, S. D., Islam, A. K., Majumder, K., Rimti, F. H., Das, J., Tabassum, M. N., et al. (2022). Assessment of knowledge on human mpox virus among general population in Bangladesh. MedRxiv 2022. doi: 10.1101/2022.08.31.22279445
Nolen, L. D., Osadebe, L., Katomba, J., Likofata, J., Mukadi, D., Monroe, B., et al. (2016). Extended human-to-human transmission during a monkeypox outbreak in the Democratic Republic of the Congo. Emerging Infect. Dis. 22, 1014. doi: 10.3201/eid2206.150579
Ogoina, D., Izibewule, J. H., Ogunleye, A., Ederiane, E., Anebonam, U., Neni, A., et al. (2019). The 2017 human monkeypox outbreak in Nigeria—report of outbreak experience and response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS One 14, e0214229. doi: 10.1371/journal.pone.0214229
Pakistan., B.o.S.G.o (2017). Brief on Census. Available online at: https://www.pbs.gov.pk/content/brief-census-2017:~:text=According%20to%20the%20final%20results,males%20and%20101.3%20million%20females.
Petersen, B. W., Damon, I. K. (2015). “Orthopoxviruses: vaccinia (smallpox vaccine), variola (smallpox), monkeypox, and cowpox,” in Mandell, Douglas, and Bennett's principles and practice of infectious diseases (Elsevier), 1694–1702.e3.
Raghupathi, V., Raghupathi, W. (2020). The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health 78, 1–18. doi: 10.1186/s13690-020-00402-5
REUTERS (2022). Indonesia confirms first monkeypox case in citizen returning from abroad. Available Online at: https://www.reuters.com/world/asia-pacific/indonesia-brief-media-first-confirmed-monkeypox-case-2022-08-20/.
Reynolds, M. G., Yorita, K. L., Kuehnert, M. J., Davidson, W. B., Huhn, G. D., Holman, R. C., et al. (2006). Clinical manifestations of human monkeypox influenced by route of infection. J. Infect. Dis. 194, 773–780. doi: 10.1086/jid.2006.194.issue-6
Riccò, M., Ferraro, P., Camisa, V., Satta, E., Zaniboni, A., Ranzieri, S., et al. (2022). When a neglected tropical disease goes global: knowledge, attitudes and practices of Italian physicians towards monkeypox, preliminary results. Trop. Med. Infect. Dis. 7, 135. doi: 10.3390/tropicalmed7070135
Sah, R., Abdelaal, A., Reda, A., Katamesh, B. E., Manirambona, E., Abdelmonem, H., et al. (2022a). Monkeypox reported in India–South East Asia region: health and economic challenges. Lancet Regional Health-Southeast Asia 4, 100063. doi: 10.1016/j.lansea.2022.100063
Sah, R., Mohanty, A., Siddiq, A., Singh, P., Abdelaal, A., Alshahrani, N. Z., et al. (2022b). Monkeypox and its possible sexual transmission: where are we now with its evidence? Pathogens 11, 924. doi: 10.3390/pathogens11080924
Sallam, M., Al-Mahzoum, K., Dardas, L. A., Al-Tammemi, A. A.B., Al-Majali, L., Al-Naimat, H., et al. (2022). Knowledge of human monkeypox and its relation to conspiracy beliefs among students in Jordanian health schools: filling the knowledge gap on emerging zoonotic viruses. Medicina 58, 924. doi: 10.3390/medicina58070924
Seang, S., Burrel, S., Todesco, E., Leducq, V., Monsel, G., Le Pluart, D., et al. (2022). Evidence of human-to-dog transmission of monkeypox virus. Lancet 400, 658–659. doi: 10.1016/S0140-6736(22)01487-8
Shafaati, M., Zandi, M. (2022). Monkeypox virus neurological manifestations in comparison to other orthopoxviruses. Travel Med. Infect. Dis. 49, 102414. doi: 10.1016/j.tmaid.2022.102414
Shafaati, M., Zandi, M., Choudhary, O. P. (2022). Monkeypox virus crosstalk with HIV; where do we stand now? Int. J. Surg. 105, 106897. doi: 10.1016/j.ijsu.2022.106897
Syed, M., Saleem, T., Syeda, U.-R., Habib, M., Zahid, R., Bashir, A., et al. (2010). Knowledge, attitudes and practices regarding dengue fever among adults of high and low socioeconomic groups. J. Pakistan Med. Assoc. 60, 243.
Tahir, M. J., Saqlain, M., Tariq, W., Waheed, S., Tan, S. H., Nasir, S. I., et al. (2020). Devastating urban flooding and dengue outbreak during the COVID-19 pandemic in Pakistan. Med. J. Islamic Republic Iran 34, 169. doi: 10.47176/mjiri.34.169
Tahir, M. J., Siddiqi, A. R., Ullah, I., Ahmed, A., Dujaili, J., Saqlain, M. (2021). Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health 21, 1–12. doi: 10.1186/s12889-021-11814-5
Tomar, B. S., Singh, P., Nathiya, D., Suman, S., Raj, P., Tripathi, S., et al. (2021). Indian community's knowledge, attitude, and practice toward COVID-19. Indian J. Soc. Psychiatry 37, 48–56. doi: 10.4103/ijsp.ijsp_133_20
Wen, F., Meng, Y., Cao, H., Xia, J., Li, H., Qi, H., et al. (2020). Knowledge, attitudes, practices of primary and middle school students at the outbreak of COVID-19 in Beijing: A cross-sectional online study. MedRxiv. doi: 10.1101/2020.06.29.20138628
W.H.O (2022). WHO Director-General declares the ongoing monkeypox outbreak a Public Health Emergency of International Concern. Available online at: https://www.who.int/europe/news/item/23-07-2022-who-director-general-declares-the-ongoing-monkeypox-outbreak-a-public-health-event-of-international-concern.
W.H.O.a.o.D.A Monkeypox Outbreak: Global Trends. Available online at: https://worldhealthorg.shinyapps.io/mpx_global/section-fns2.
World Health Organization Enhance surveillance, p.h.m.f.m.W. Available online at: https://www.who.int/southeastasia/news/detail/24-07-2022-enhancesurveillance–public-health-measures-formonkeypox–who (Accessed Dec 3,2022).
Zandi, M., Shafaati, M., Hosseini, F. (2023). Mechanisms of immune evasion of monkeypox virus. Front. Microbiol. 14, 1106247. doi: 10.3389/fmicb.2023.1106247
Keywords: monkeypox, endemic, knowledge, attitude, perception, Pakistan
Citation: Yousaf H, Qadeer A, Sohail M, Khan M, Farooq M, Khan Z, Fouad D, Liu Y-C and Chen C-C (2025) Knowledge, attitude, and perception of Pakistani populations toward monkeypox: a cross-section study. Front. Cell. Infect. Microbiol. 14:1449096. doi: 10.3389/fcimb.2024.1449096
Received: 14 June 2024; Accepted: 23 December 2024;
Published: 04 February 2025.
Edited by:
Daniel Felmlee, University of Plymouth, United KingdomReviewed by:
Shoaib Ahmad, Punjab Medical College, PakistanTatina Todorova, Medical University of Varna, Bulgaria
Copyright © 2025 Yousaf, Qadeer, Sohail, Khan, Farooq, Khan, Fouad, Liu and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Chia Liu, MDcyMDRAY3ljaC5vcmcudHc=; Chien-Chin Chen, aGxtYXJrY0BnbWFpbC5jb20=; Muhammad Sohail, c29oYWlsc2hhaDExQHlhaG9vLmNvbQ==
 Humayun Yousaf
Humayun Yousaf Abdul Qadeer
Abdul Qadeer Muhammad Sohail
Muhammad Sohail Maqbool Khan4
Maqbool Khan4 Muhammad Farooq
Muhammad Farooq Zakir Khan
Zakir Khan Chien-Chin Chen
Chien-Chin Chen