- 1Department of Obstetrics and Gynecology, University of Rochester, Rochester, NY, United States
- 2Department of Pharmacology and Physiology, University of Rochester, Rochester, NY, United States
Editorial on the Research Topic
Vulvodynia and beyond: innate immune sensing, microbes, inflammation, and chronic pain
Although it is inevitable that every person with a vulva will experience pain or discomfort in this area at some point in their life, vulvar disease remains inadequately understood (Damsted-Petersen et al., 2009; Bohm-Starke, 2010; Reed et al., 2014; Akopians and Rapkin, 2015; Bornstein et al., 2016; Falsetta et al., 2017; Stenson, 2017; Bergeron et al., 2020; Graziottin et al., 2020; Vasileva et al., 2020; Bekauri et al., 2023; Falsetta et al., 2023). Patients with vulvodynia, or chronic vulvar pain, suffer from burning, stabbing, or “knife-like” pain that is poorly explained and recalcitrant to treatment (Haefner et al., 2005; Stockdale and Lawson, 2014). This pain occurs in the absence of any obvious disease pathology, making it a diagnosis of exclusion. Thus, patients will suffer, at minimum, months and most often, years before they are diagnosed. Treatment requires an escalation of interventions, starting with changes to hygiene practices, progressing to topical lidocaine and oral therapies such as gabapentin, eventually resulting in surgical removal of the vestibule (ring of tissue surrounding the vaginal opening) (Fischer, 2004; Danby and Margesson, 2010; Nunns et al., 2010; Tieu and MacGregor, 2011; Stockdale and Lawson, 2014; Eppsteiner et al., 2014; Sadownik, 2014; Goldstein et al., 2016; Falsetta et al., 2017; Brown et al., 2018; Vasileva et al., 2020; Bohm-Starke et al., 2022; Falsetta et al., 2023). However, some patients experience generalized pain affecting the whole vulva, such that surgical intervention is not possible.
Patients with vulvar pain have a low quality of life, and disease is often accompanied by depression, pelvic floor dysfunction, relationship issues, and other comorbidities (Arnold et al., 2006; Reed et al., 2012; Reed et al., 2014; Sadownik, 2014; Vasileva et al., 2020; Rubal et al., 2023). While it is socially acceptable to discuss pain in other parts of the body, there is significant stigma associated with vulvar pain or “woman troubles” (Nguyen et al., 2013). Patients often feel isolated, invalidated, or even that they are being “gaslighted” by the medical community and that their experiences are not being taken seriously (Bergeron et al., 2014; Niedenfuehr et al., 2023). It has been recognized that screening, diagnosis, and intervention must be improved for vulvar disease, yet women’s health research as a whole has been chronically underfunded (Reporter, 2023; Smith, 2023).
Advances in the field, roughly within the last decade, have led to the creation of rodent and cell culture models that have facilitated greater mechanistic understanding of disease, while enabling screening of new therapies and therapeutic targets (Gordon et al., 2003; Gerber et al., 2008; Farmer et al., 2011; Leclair et al., 2011; Leclair et al., 2013; Martinov et al., 2013; Leclair et al., 2014; Akopians and Rapkin, 2015; Ali et al., 2015; Falsetta et al., 2015; Foster et al., 2015; Tommola et al., 2015; Akbar et al., 2016; Chalmers et al., 2016; Falsetta et al., 2016; Tommola et al., 2016; Falsetta et al., 2017; Harlow et al., 2017; Falsetta et al., 2018; Zanotta et al., 2018; Arriaga-Gomez et al., 2019; Barry et al., 2019; Bedford et al., 2020; Bergeron et al., 2020; Falsetta et al., 2021; Rangappa et al., 2021; Awad-Igbaria et al., 2022; Falsetta et al., 2023). However, it is still not clear if vulvodynia is a singular disease with different manifestations or multiple related diseases that are grouped simply because they involve otherwise unexplained pain in the vulva. Vulvodynia may present as primary or secondary, appearing before or after a period of “pain-free intercourse” or provoked or unprovoked, meaning pain is elicited upon touch or presents randomly (Haefner et al., 2005; Stockdale and Lawson, 2014). Vulvodynia may also be localized to the vulvar vestibule or generalized (Haefner et al., 2005; Stockdale and Lawson, 2014). These medical terminologies, based on clinical presentation alone, may not translate to clear biological divisions of disease. Therapies that are effective for localized disease, may not work for generalized disease, and so forth. Therefore, it is imperative that studies are carefully designed with this information in mind.
Initially, vulvodynia was named vestibulitis, implying the involvement of inflammation. Tissue from affected areas clearly showed the presence of infiltrating immune cells, consistent with an inflammatory response (Prayson et al., 1995; Chaim et al., 1996; Chadha et al., 1998). However, tissue from patients without disease also showed the presence of immune cells (Halperin et al., 2005). Therefore, this disease was reclassified as vulvodynia, focusing on the characteristic of pain (Haefner et al., 2005; Bornstein et al., 2016). However, it has since been demonstrated that although the hallmarks of inflammation are present in both patients with and without vulvodynia, the relative numbers and organizations of these cells differ between cases and controls (Leclair et al., 2011; Leclair et al., 2013; Leclair et al., 2014; Falsetta et al., 2015; Foster et al., 2015; Tommola et al., 2015; Falsetta et al., 2016; Tommola et al., 2016; Falsetta et al., 2017; Falsetta et al., 2018; Zanotta et al., 2018; Falsetta et al., 2021; Falsetta et al., 2023). The painful site in patients with localized disease shows a unique inflammatory profile compared to non-painful areas of the vulva from the same patient and matched sites from controls that do not have vulvar disease (Falsetta et al., 2015; Foster et al., 2015; Falsetta et al., 2016; Falsetta et al., 2017; Falsetta et al., 2018; Falsetta et al., 2021; Bekauri et al., 2023; Falsetta et al., 2023). In essence, the vestibule of patients with vulvodynia is exquisitely sensitive to inflammatory stimuli (e.g. microbes, pathogen-associated molecular patterns), setting off a series of events that culminates in chronic pain.
Inflammation and pain are often associated. However, it was unclear how these were associated in vulvodynia until recently (Falsetta et al., 2017; Bekauri et al., 2023; Falsetta et al., 2023). Inflammation induces changes in the vulvar lipidome, specifically at painful sites, that favor inflammation and help to generate or preserve lipid signals that initiate pain signaling through transient receptor potential cation channels (TRPs), specifically subfamily V (TRPVs) (Falsetta et al., 2021; Bekauri et al., 2023; Falsetta et al., 2023). At the same time, the painful vulvar vestibule exhibits a deficiency in the production of lipids that help to abate inflammation, known as special pro-resolving mediators (SPMs). SPMs, unlike non-steroidal anti-inflammatory drugs (NSAIDs), do not impede inflammation (Serhan et al., 2015; Serhan, 2017). They are naturally produced from dietary sources of polyunsaturated fatty acids (PUFAs), and their role is to help to resolve inflammation faster and more efficiently to prevent the unintended side effects of unchecked inflammation. In localized provoked vulvodynia, there appears to be a “perfect storm” where inflammatory stimuli, potentially even the resident microflora, trigger an exaggerated immune response that results in activation of pain signaling, while sustaining inflammation to perpetuate a “never-ending” cycle of pain and inflammation (Falsetta et al., 2021; Bekauri et al., 2023; Falsetta et al., 2023) (Figure 1). Although more work is needed to fully understand the “key players” at a cellular level, there is now evidence of a neuro-inflammatory mechanism of disease that represents a reasonable target for the development of new therapeutics.
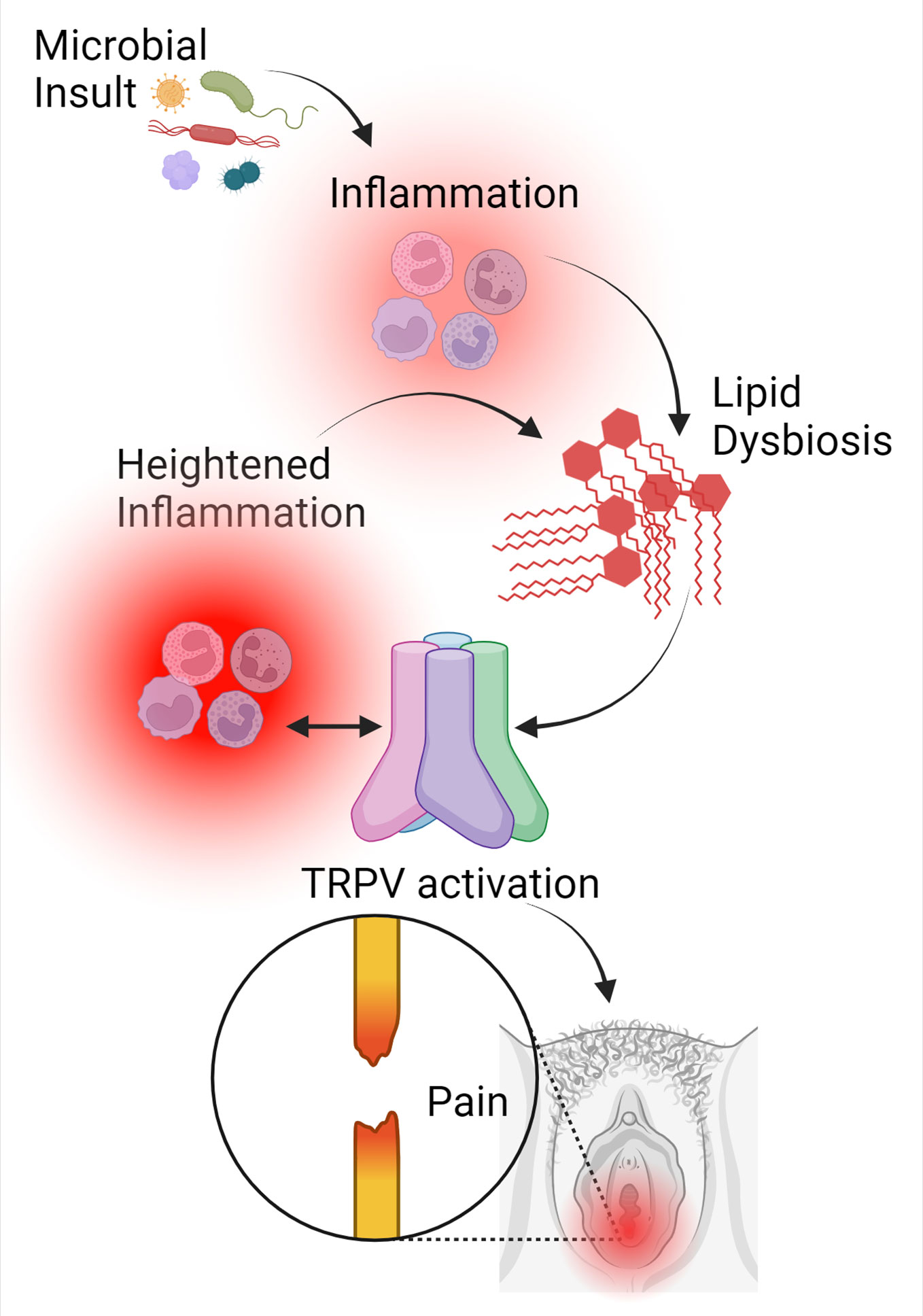
Figure 1 Inflammation is a catalyst for pain signaling in vulvodynia. In patients with localized provoked vulvodynia, an actual or perceived microbial insult triggers an inflammatory response at the site of pain that causes lipid dysbiosis, which favors inflammation and reduces the ability to resolve that inflammation. At the same time, levels of lipids that activate pain signaling through TRPV channels are sustained. When TRPV is activated, inflammation is further heightened, continuing to trigger lipid dysbiosis. Inflammation is both necessary and sufficient for TRPV signaling, while TRPV activation further increases inflammation. This creates a feed-forward loop where inflammation and lipid dysbiosis fuel one another, leading to chronic pain and inflammation. This figure was created using BioRender.com.
Mouse models have been optimized to test a variety of a promising new therapeutics and to further dissect these disease mechanisms (Farmer et al., 2011; Martinov et al., 2013; Arriaga-Gomez et al., 2019; Boo et al., 2019; Falsetta et al., 2021; Rangappa et al., 2021; Awad-Igbaria et al., 2022). While inflammation clearly serves a key role in at least the localized provoked disease subtype (Falsetta et al., 2015; Foster et al., 2015; Falsetta et al., 2016; Falsetta et al., 2017; Falsetta et al., 2018; Falsetta et al., 2021; Bekauri et al., 2023; Falsetta et al., 2023), there are many other factors at play that may cause, exacerbate, or sustain disease. Some of the most promising therapeutic options under investigation thus far involve modulation of this immune response, potentially through the addition of exogenous SPMs or PUFAs (Falsetta et al., 2021; Bekauri et al., 2023; Falsetta et al., 2023). However, further investigation of the underlying disease mechanisms, particularly the biological distinctions between disease subtypes, is critical for development and optimization of new therapeutic strategies. Even if an ideal therapy is on the horizon in the coming decade, it will only be useful to patients that receive a diagnosis. Prompter diagnosis is likely to reduce the incidence and impact of comorbidities, such as depression. Characterizing and harnessing the inflammatory and lipid signatures of disease could be translated to improved and objective diagnostic measures that will help alleviate the feelings of isolation and powerlessness that patients often experience. The overarching goal is to treat the disease and not simply the symptoms of that disease, while minimizing the length and extent of suffering each patient must first face.
Author contributions
MF: Writing – original draft.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Akbar, S., Subhan, F., Karim, N., Shahid, M., Ahmad, N., Ali, G., et al. (2016). 6-Methoxyflavanone attenuates mechanical allodynia and vulvodynia in the streptozotocin-induced diabetic neuropathic pain. BioMed. Pharmacother. 84, 962–971. doi: 10.1016/j.biopha.2016.10.017
Akopians, A. L., Rapkin, A. J. (2015). Vulvodynia: the role of inflammation in the etiology of localized provoked pain of the vulvar vestibule (Vestibulodynia). Semin. Reprod. Med. 33 (4), 239–245. doi: 10.1055/s-0035-1554919
Ali, G., Subhan, F., Abbas, M., Zeb, J., Shahid, M., Sewell, R.D. (2015). A streptozotocin-induced diabetic neuropathic pain model for static or dynamic mechanical allodynia and vulvodynia: validation using topical and systemic gabapentin. Naunyn Schmiedebergs Arch. Pharmacol. 388 (11), 1129–1140. doi: 10.1007/s00210-015-1145-y
Arnold, L. D., Bachmann, G.A., Rosen, R., Kelly, S., Rhoads, G.G. (2006). Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet. Gynecol. 107 (3), 617–624. doi: 10.1097/01.AOG.0000199951.26822.27
Arriaga-Gomez, E., Kline, J., Emanuel, E., Neamonitaki, N., Yangdon, T., Zacheis, H., et al. (2019). Repeated vaginal exposures to the common cosmetic and household preservative methylisothiazolinone induce persistent, mast cell-dependent genital pain in ND4 mice. Int. J. Mol. Sci. 20 (21). doi: 10.3390/ijms20215361
Reporter, N. (2023) Vulvar pain [Internet]2000-2023. Available at: https://reporter.nih.gov/.
Awad-Igbaria, Y., Dadon, S., Shamir, A., Livoff, A., Shlapobersky, M., Bornstein, J., et al. (2022). Characterization of early inflammatory events leading to provoked vulvodynia development in rats. J. Inflammation Res. 15, 3901–3923. doi: 10.2147/JIR.S367193
Barry, C. M., Matusica, D., Haberberger, R.V. (2019). Emerging evidence of macrophage contribution to hyperinnervation and nociceptor sensitization in vulvodynia. Front. Mol. Neurosci. 12, 186. doi: 10.3389/fnmol.2019.00186
Bedford, L., Parker, S.E., Davis, E., Salzman, E., Hillier, S.L., Foxman, B., et al. (2020). Characteristics of the vaginal microbiome in women with and without clinically confirmed vulvodynia. Am. J. Obstet. Gynecol. 406.e401-406.e416. doi: 10.1016/j.ajog.2020.02.039
Bekauri, T., Fischer, S., Honn, K., Maddipati, K., Love, T., Little, C., et al. (2023). Inflammation, lipid dysregulation, and transient receptor potential cation channel subfamily V member 4 (TRPV4) signaling perpetuate chronic vulvar pain. Pain. doi: 10.1097/j.pain.0000000000003088
Bergeron, S., Likes, W.M., Steben, M. (2014). Psychosexual aspects of vulvovaginal pain. Best Pract. Res. Clin. Obstet. Gynaecol. 28 (7), 991–999. doi: 10.1016/j.bpobgyn.2014.07.007
Bergeron, S., Reed, B.D., Wesselmann, U., Bohm-Starke, N. (2020). Vulvodynia. Nat. Rev. Dis. Primers. 6 (1), 36. doi: 10.1038/s41572-020-0164-2
Bohm-Starke, N. (2010). Medical and physical predictors of localized provoked vulvodynia. Acta Obstet. Gynecol. Scandinavica. 89 (12), 1504–1510.
Bohm-Starke, N., Ramsay, K.W., Lytsy, P., Nordgren, B., Sjoberg, I., Moberg, K., et al. (2022). Treatment of provoked vulvodynia: A systematic review. J. Sexual Med. 19 (5), 789–808. doi: 10.3109/00016349.2010.528368
Boo, B., Kamath, R., Arriaga-Gomez, E., Landry, J., Emanuel, E., Joo, S., et al. (2019). Tetrahydrocannabinol reduces hapten-driven mast cell accumulation and persistent tactile sensitivity in mouse model of allergen-provoked localized vulvodynia. Int. J. Mol. Sci. 20 (9). doi: 10.3390/ijms20092163
Bornstein, J., Goldstein, A.T., Stockdale, C.K., Bergeron, S., Pukall, C., Zolnoun, D., et al. (2016). 2015 ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. J. Sexual Med. 13 (4), 607–612. doi: 10.1016/j.jsxm.2016.02.167
Brown, C. S., Bachmann, G.A., Wan, J., Foster, D.C., Gabapentin Study, G. (2018). Gabapentin for the treatment of vulvodynia: A randomized controlled trial. Obstet. Gynecol. 131 (6), 1000–1007. doi: 10.1097/AOG.0000000000002617
Chadha, S., Gianotten, W.L., Drogendijk, A.C., Weijmar Schultz, W.C., Blindeman, L.A., Van Der Meijden, W.I. (1998). Histopathologic features of vulvar vestibulitis. Int. J. Gynecol. Pathol. 17 (1), 7–11. doi: 10.1097/00004347-199801000-00002
Chaim, W., Meriwether, C., Gonik, B., Qureshi, F., Sobel, J.D. (1996). Vulvar vestibulitis subjects undergoing surgical intervention: a descriptive analysis and histopathological correlates. Eur. J. Obstet. Gynecol. Reprod. Biol. 68 (1-2), 165–168. doi: 10.1016/0301-2115(96)02502-X
Chalmers, K. J., Madden, V.J., Hutchinson, M.R., Moseley, G.L. (2016). Local and systemic inflammation in localized, provoked vestibulodynia: A systematic review. Obstet. Gynecol. 128 (2), 337–347. doi: 10.1097/AOG.0000000000001510
Damsted-Petersen, C., Boyer, S.C., Pukall, C.F. (2009). Current perspectives in vulvodynia. Women’s. Health 5 (4), 423–436. doi: 10.2217/WHE.09.30
Danby, C. S., Margesson, L. J. (2010). Approach to the diagnosis and treatment of vulvar pain. Dermatol. Ther. 23 (5), 485–504. doi: 10.1111/j.1529-8019.2010.01352.x
Eppsteiner, E., Boardman, L., Stockdale, C.K. (2014). Vulvodynia. Best Pract. Res. Clin. Obstet. Gynaecol. 28 (7), 1000–1012. doi: 10.1016/j.bpobgyn.2014.07.009
Falsetta, M. L., Foster, D.C., Bonham, A.D., Phipps, R.P. (2015). Identification of novel mechanisms involved in generating localized vulvodynia pain. Am. J. Obstet. Gynecol. 38.e31-38.e12. doi: 10.1016/j.ajog.2015.02.002
Falsetta, M. L., Foster, D.C., Woeller, C.F., Pollock, S.J., Bonham, A.D., Haidaris, C.G., et al. (2016). A role for bradykinin signaling in chronic vulvar pain. J. Pain. 1183–1197. doi: 10.1016/j.jpain.2016.07.007
Falsetta, M. L., Foster, D.C., Woeller, C.F., Pollock, S.J., Bonham, A.D., Haidaris, C.G., et al. (2017). A review of the available clinical therapies for vulvodynia management and new data implicating proinflammatory mediators in pain elicitation. BJOG.: an Int. J. Obstet. Gynaecol. 124 (2), 210–218. doi: 10.1111/1471-0528.14157
Falsetta, M. L., Foster, D.C., Woeller, C.F., Pollock, S.J., Bonham, A.D., Piekna-Przybylska, D., et al. (2018). Toll-like receptor signaling contributes to proinflammatory mediator production in localized provoked vulvodynia. J. Lower. Genital. Tract. Dis. 22 (1), 52–57. doi: 10.1097/LGT.0000000000000364
Falsetta, M. L., Maddipati, K.R., Honn, K.V. (2021). Specialized pro-resolving mediators reduce pro-nociceptive inflammatory mediator production in models of localized provoked vulvodynia. J. Pain 22 (10), 1195–1209. doi: 10.1016/j.jpain.2021.03.144
Falsetta, M. L., Wood, R.W., Linder, M.A., Bonham, A.D., Honn, K.V., Maddipati, K.R., et al. (2023). Inflammation, lipids, and pain in vulvar disease. Pharmacol. Ther. 248, 108467. doi: 10.1016/j.pharmthera.2023.108467
Farmer, M. A., Taylor, A.M., Bailey, A.L., Tuttle, A.H., Macintyre, L.C., Milagrosa, Z.E., et al. (2011). Repeated vulvovaginal fungal infections cause persistent pain in a mouse model of vulvodynia. Sci. Transl. Med. 3 (101), 101ra91. doi: 10.1126/scitranslmed.3002613
Foster, D., Falsetta, M., Woeller, C., Pollock, S., Song, K., Bonham, A., et al. (2015). Site-specific mesenchymal control of inflammatory pain to yeast challenge in vulvodynia afflicted and pain-free women. Pain 156 (3), 386–396. doi: 10.1097/01.j.pain.0000460320.95267.5d
Gerber, S., Witkin, S.S., Stucki, D. (2008). Immunological and genetic characterization of women with vulvodynia. J. Med. Life. 1 (4), 432–438.
Goldstein, A. T., Pukall, C.F., Brown, C., Bergeron, S., Stein, A., Kellogg-Spadt, S. (2016). Vulvodynia: assessment and treatment. J. Sexual Med. 13 (4), 572–590. doi: 10.1016/j.jsxm.2016.01.020
Gordon, A. S., Panahian-Jand, M., Mccomb, F., Melegari, C., Sharp, S. (2003). Characteristics of women with vulvar pain disorders: responses to a Web-based survey. J. Sex. Marital. Ther. 29 Suppl 1, 45–58. doi: 10.1080/713847126
Graziottin, A., Murina, F., Gambini, D., Taraborrelli, S., Gardella, B., Campo, M., et al. (2020). Vulvar pain: The revealing scenario of leading comorbidities in 1183 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 252, 50–55. doi: 10.1016/j.ejogrb.2020.05.052
Haefner, H. K., Collins, M.E., Davis, G.D., Edwards, L., Foster, D.C., Hartmann, E.D., et al. (2005). The vulvodynia guideline. J. Lower. Genital. Tract. Dis. 9 (1), 40–51. doi: 10.1097/00128360-200501000-00009
Halperin, R., Zehavi, S., Vaknin, Z., Ben-Ami, I., Pansky, M., Schneider, D. (2005). The major histopathologic characteristics in the vulvar vestibulitis syndrome. Gynecol. Obstet. Invest. 59 (2), 75–79. doi: 10.1159/000082112
Harlow, B. L., Caron, R.E., Parker, S.E., Chatterjea, D., Fox, M.P., Nguyen, R.H.N. (2017). Recurrent yeast infections and vulvodynia: can we believe associations based on self-reported data? J. Women’s. Health 26 (10), 1069–1076. doi: 10.1089/jwh.2016.5777
Leclair, C. M., Goetsch, M.F., Korcheva, V.B., Anderson, R., Peters, D., Morgan, T.K. (2011). Differences in primary compared with secondary vestibulodynia by immunohistochemistry. Obstet. Gynecol. 117 (6), 1307–1313. doi: 10.1097/AOG.0b013e31821c33dc
Leclair, C. M., Goetsch, M.F., Li, H., Morgan, T.K. (2013). Histopathologic characteristics of menopausal vestibulodynia. Obstet. Gynecol. 122 (4), 787–793. doi: 10.1097/AOG.0b013e3182a5f25f
Leclair, C. M., Leeborg, N.J., Jacobson-Dunlop, E., Goetsch, M.F., Morgan, T.K. (2014). CD4-positive T-cell recruitment in primary-provoked localized vulvodynia: potential insights into disease triggers. J. Lower. Genital. Tract. Dis. 18 (2), 195–201. doi: 10.1097/LGT.0b013e3182a55591
Martinov, T., Glenn-Finer, R., Burley, S., Tonc, E., Balsells, E., Ashbaugh, A., et al. (2013). Contact hypersensitivity to oxazolone provokes vulvar mechanical hyperalgesia in mice. PloS One 8 (10), e78673. doi: 10.1371/journal.pone.0078673
Nguyen, R. H., Turner, R.M., Rydell, S.A., Maclehose, R.F., Harlow, B.L. (2013). Perceived stereotyping and seeking care for chronic vulvar pain. Pain Med. 14 (10), 1461–1467. doi: 10.1111/pme.12151
Niedenfuehr, J., Edwards, M., King, L.M. (2023). A scoping review: the psychosocial barriers that exist for people with vulvodynia. J. Sexual Med. 20 (6), 833–858. doi: 10.1093/jsxmed/qdad035
Nunns, D., Mandal, D., Byrne, M., Mclelland, J., Rani, R., Cullimore, J., et al. (2010). Guidelines for the management of vulvodynia. Br. J. Dermatol. 162 (6), 1180–1185. doi: 10.1111/j.1365-2133.2010.09684.x
Prayson, R. A., Stoler, M.H., Hart, W.R. (1995). Vulvar vestibulitis. A histopathologic study of 36 cases, including human papillomavirus in situ hybridization analysis. Am. J. Surg. Pathol. 19 (2), 154–160.
Rangappa, S., Shankar, V.K., Jo, S., Repka, M.A., Murthy, S.N. (2021). Chemotherapeutic agent-induced vulvodynia, an experimental model. AAPS PharmSciTech. 22 (3), 95. doi: 10.1208/s12249-021-01969-0
Reed, B. D., Harlow, S.D., Sen, A., Legocki, L.J., Edwards, R.M., Arato, N., et al. (2012). Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am. J. Obstet. Gynecol. 206 (2), 170 e1–170 e9. doi: 10.1016/j.ajog.2011.08.012
Reed, B. D., Legocki, L.J., Plegue, M.A., Sen, A., Haefner, H.K., Harlow, S.D. (2014). Factors associated with vulvodynia incidence. Obstet. Gynecol. 123 (2 Pt 1), 225–231. doi: 10.1097/AOG.0000000000000066
Rubal, C., Pereira, A., Sastre, L.C., Perez-Cejuela, B.A., Gamiz, S.H., Chaves, P., et al. (2023). Managing vulvodynia with central sensitization: challenges and strategies. J. Clin. Med. 12 (11). doi: 10.3390/jcm12113851
Sadownik, L. A. (2014). Etiology, diagnosis, and clinical management of vulvodynia. Int. J. Womens. Health 6, 437–449. doi: 10.2147/IJWH.S37660
Serhan, C. N. (2017). Discovery of specialized pro-resolving mediators marks the dawn of resolution physiology and pharmacology. Mol. Aspects. Med. 58, 1–11. doi: 10.1016/j.mam.2017.03.001
Serhan, C. N., Chiang, N., Dalli, J. (2015). The resolution code of acute inflammation: Novel pro-resolving lipid mediators in resolution. Semin. Immunol. 200-215. doi: 10.1016/j.smim.2015.03.004
Smith, K. (2023). Women’s health research lacks funding - in a series of charts. Nature 617 (7959), 28–29. doi: 10.1038/d41586-023-01475-2
Stenson, A. L. (2017). Vulvodynia: diagnosis and management. Obstet. Gynecol. Clin. North Am. 44 (3), 493–508. doi: 10.1016/j.ogc.2017.05.008
Stockdale, C. K., Lawson, H. W. (2014). 2013 Vulvodynia guideline update. J. Lower. Genital. Tract. Dis. 18 (2), 93–100. doi: 10.1097/LGT.0000000000000021
Tieu, K. D., MacGregor, J. L. (2011). Successful treatment of vulvodynia with botulinum toxin A. Arch. Dermatol. 147 (2), 251–252. doi: 10.1001/archdermatol.2010.443
Tommola, P., Butzow, R., Unkila-Kallio, L., Paavonen, J., Meri, S. (2015). Activation of vestibule-associated lymphoid tissue in localized provoked vulvodynia. Am. J. Obstet. Gynecol. 212 (4), 476 e1–476 e8. doi: 10.1016/j.ajog.2014.10.1098
Tommola, P., Unkila-Kallio, L., Paetau, A., Meri, S., Kalso, E., Paavonen, J. (2016). Immune activation enhances epithelial nerve growth in provoked vestibulodynia. Am. J. Obstet. Gynecol. 215 (6), 768 e1–768 e8. doi: 10.1016/j.ajog.2016.07.037
Vasileva, P., Strashilov, S.A., Yordanov, A.D. (2020). Aetiology, diagnosis, and clinical management of vulvodynia. Prz. Menopauzalny. 19 (1), 44–48. doi: 10.5114/pm.2020.95337
Keywords: pain, vulva, vestibulitis, vulvodynia, inflammation, TRPV cation channels, lipidome
Citation: Falsetta ML (2023) Editorial: Vulvodynia and beyond: innate immune sensing, microbes, inflammation, and chronic pain. Front. Cell. Infect. Microbiol. 13:1338659. doi: 10.3389/fcimb.2023.1338659
Received: 15 November 2023; Accepted: 17 November 2023;
Published: 08 December 2023.
Edited and Reviewed by:
Annemarie H. Meijer, Leiden University, NetherlandsCopyright © 2023 Falsetta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Megan L. Falsetta, bWVnYW5fd29vZEB1cm1jLnJvY2hlc3Rlci5lZHU=
 Megan L. Falsetta
Megan L. Falsetta