- Department of Gastroenterology and Hepatology, Shenzhen University General Hospital, Shenzhen, China
With the development of endoscopic technology, an increasing number of patients with esophageal disease are being diagnosed, although the underlying pathogenesis of many esophageal diseases remains unclear. In recent years, a large number of studies have demonstrated that the occurrence and development of various intestinal diseases were related to intestinal flora. As a result, researchers have shifted their focus towards investigating esophageal flora to better understand the pathogenesis, early diagnosis, and treatment of esophageal diseases. This paper reviewed the normal esophageal flora and the changes of esophageal flora under different esophageal disease states. It was observed that there are distinct differences in the composition of esophageal microflora among Gastroesophageal Reflux, Barrett’s esophagus, eosinophilic esophagitis and normal esophagus. The normal esophageal flora was dominated by gram-positive bacteria, particularly Streptococcus, while the esophageal flora under esophagitis was dominated by gram-negative bacteria. Furthermore, the diversity of esophageal flora is significantly decreased in patients with esophageal cancer. Several potential microbial biomarkers for esophageal cancer have been identified, among which Fusobacterium nucleatum showed a close association with esophageal squamous cell carcinoma’s pathological stage and clinical stage.
Introduction
In recent years, there has been increasing interest in studying human microorganisms, and it is now widely recognized that these microorganisms are closely linked to various human diseases (Team NIHHMPA, 2019). However, compared to other parts of the body, the esophageal microflora has received limited attention and keep understudied. Moreover, the correlation between esophageal microflora and esophageal diseases is still largely unclear. Fortunately, with the improvement of sampling technology and the rapid progress of high-throughput sequencing technology, researches on esophageal microflora have gradually increased. Through these studies, we now have a preliminary understanding of the common microflora in a healthy esophagus (Pei et al., 2004; Yang et al., 2009). Furthermore, studies have shown that esophageal diseases such as gastroesophageal reflux disease (GERD), Barrett’s esophagus (BE), Eosinophilic esophagitis (EoE) and esophageal carcinoma (EC) all have their own unique microflora profiles (Paull and Yardley, 1988; Tian et al., 2015; Nardone et al., 2017; Polyzos et al., 2018). Here, we will review the changes of esophageal microflora table under healthy esophagus and different esophageal disease states, aiming to enhance the understanding of the differences of esophageal microflora under different esophageal disease states. This will help to elucidate the correlation between esophageal microflora and esophageal diseases, and may provide new avenues to prevent or treat esophageal diseases.
Esophageal microflora of the normal esophagus
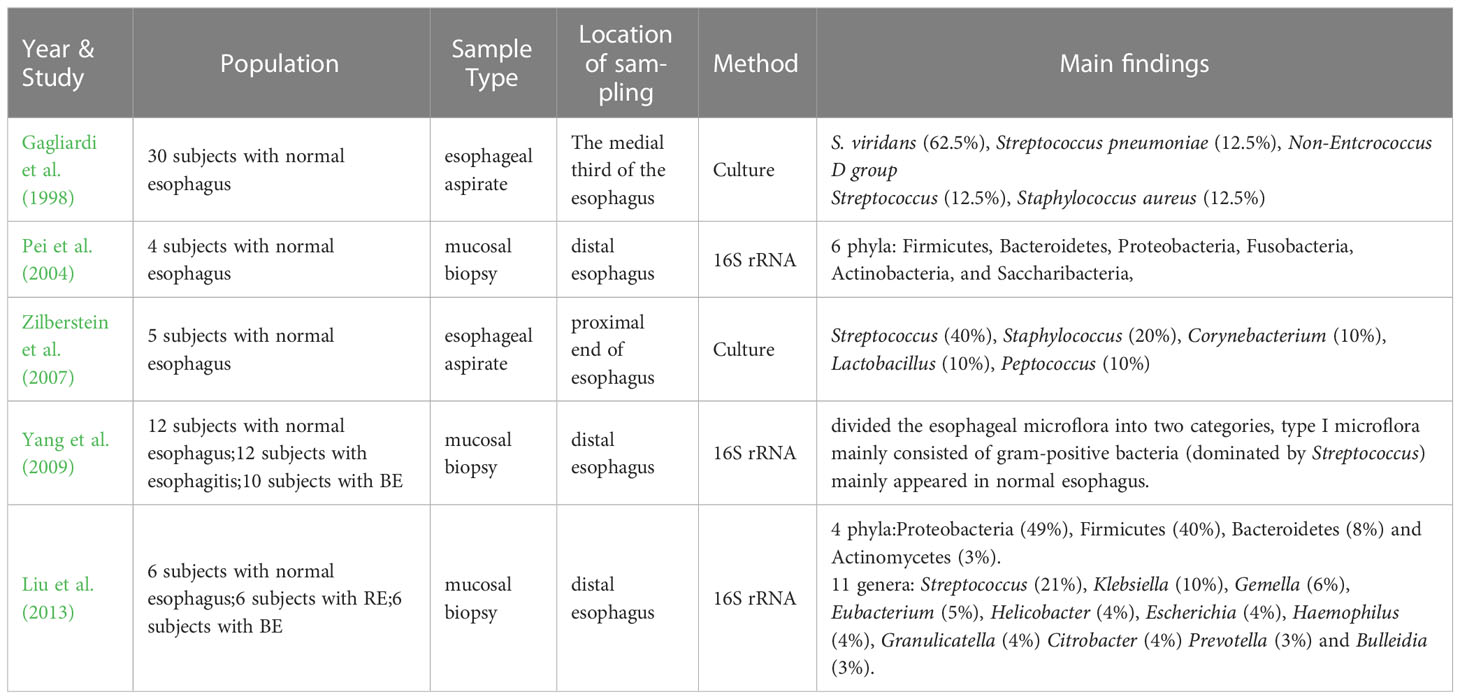
The human microflora has been a hot topic of research in recent years, the studies on intestinal microflora emerge endlessly and a lot of remarkable results have been achieved. However, studies on the esophageal microflora have been limited due to the constraints in sampling techniques, isolation and culture methods. Even after a long time, there is no definitive answer on whether there are long-term colonized microorganisms in the esophagus. Many scientists even believe that the esophagus is an environment for asepsis or the transient passage of bacteria. It was not until the early 1980s that the esophagus was confirmed for the first time that it was not a completely sterile environment through the traditional isolation and culture method (Lau et al., 1981; Finlay et al., 1982; Mannell et al., 1983). In 1998, Gagliardi et al. (1998) used the esophageal aspirate to obtain and culture the esophageal microflora, which showed that the most common bacteria in the esophagus was Streptococcus viridans. Because S. viridans was also grown in the oropharynx, the researchers thought that there might be some correlations between the esophageal microflora and the oropharyngeal microflora. Further investigations by Zilberstein et al. (2007) tested the esophageal microflora of 5 healthy adults with esophageal aspirate and culture, and the main bacteria they detected were Streptococcus, Staphylococcus, Corynebacterium, Lactobacillus, Peptococcus, among which Streptococcus is the most prevalent, with a percentage of 40%. However, although the above studies have helped people understand that the esophagus is not sterile, studies based on the above methods have seriously underestimated the complexity of the esophageal microflora due to the close adhesion of some bacteria to the mucosa and the challenges in culturing certain bacteria. In 2004, Pei et al. (2004) determined the colonized microflora in the normal distal esophagus by mucosal biopsy and 16S rRNA gene sequencing for the first time. They revealed that the normal esophageal microflora mainly consisted of six phyla: Firmicutes (mainly Streptococcus, veillonella, Megasphaera, Granulicatella, Gemella, Clostridium and Bulleidia), Bacteroidetes (mainly Prevotella and Bacteroides), Proteobacteria (mainly Haemophilus), Fusobacteria, Actinobacteria (mainly Rothia and Actinomyces), and Saccharibacteria. Among these phyla, the dominant phylum is Firmicutes (specifically Streptococcus mitis). This method of obtaining tissue through mucosal biopsy and then measuring microflora through gene sequencing opened another door to study the esophageal microflora. After that, 16S rRNA gene sequencing technology has become increasingly popular with the continuous progress of molecular technology, allowing for cost-effective large sample detection and quantitative characterization of microflora in complex biological mixtures, or even the entire community and its components (Metzker, 2010; Cox et al., 2013). In 2009, Yang et al. (2009) conducted distal esophageal biopsy sampling and 16S rRNA gene sequencing on 34 subjects, and finally divided the esophageal microflora into two categories, among which type I microflora mainly consisted of gram-positive bacteria predominantly belonging to Streptococcus, and was commonly found in normal esophagus. This finding was later verified by many research results. In 2013, Liu et al. (2013) took mucosal biopsy samples from the distal esophagus of 6 healthy subjects, and analyzed 147 cloned 16S rRNA sequences, they found that there were four phyla in the distal of normal esophagus of Japanese individuals: Proteobacteria (49%), Firmicutes (40%), Bacteroidetes (8%) and Actinomycetes (3%). There were eleven genera (≥3%) detected, including Streptococcus (21%), Klebsiella (10%), Gemella (6%), Eubacterium (5%), Helicobacter (4%), Escherichia (4%), Haemophilus (4%), Granulicatella (4%) Citrobacter (4%) Prevotella (3%) and Bulleidia (3%), with Streptococcus being the most prevalent. In summary, although there are limited studies on the healthy esophageal microflora, and most of them have been used as controls in esophageal diseases research with variations in sampling methods, detection techniques and even sampling sites, it is generally accepted that there is resident microflora in normal esophagus, mainly gram-positive bacteria. Among them, Firmicutes (Streptococcus) is the most common. Proteobacteria, Bacteroidetes and Actinobacteria are also mentioned. They play an important role in maintaining the normal environment of the esophagus (Table 1).
Esophageal microflora of the gastroesophageal reflux and Barrett’s esophagus
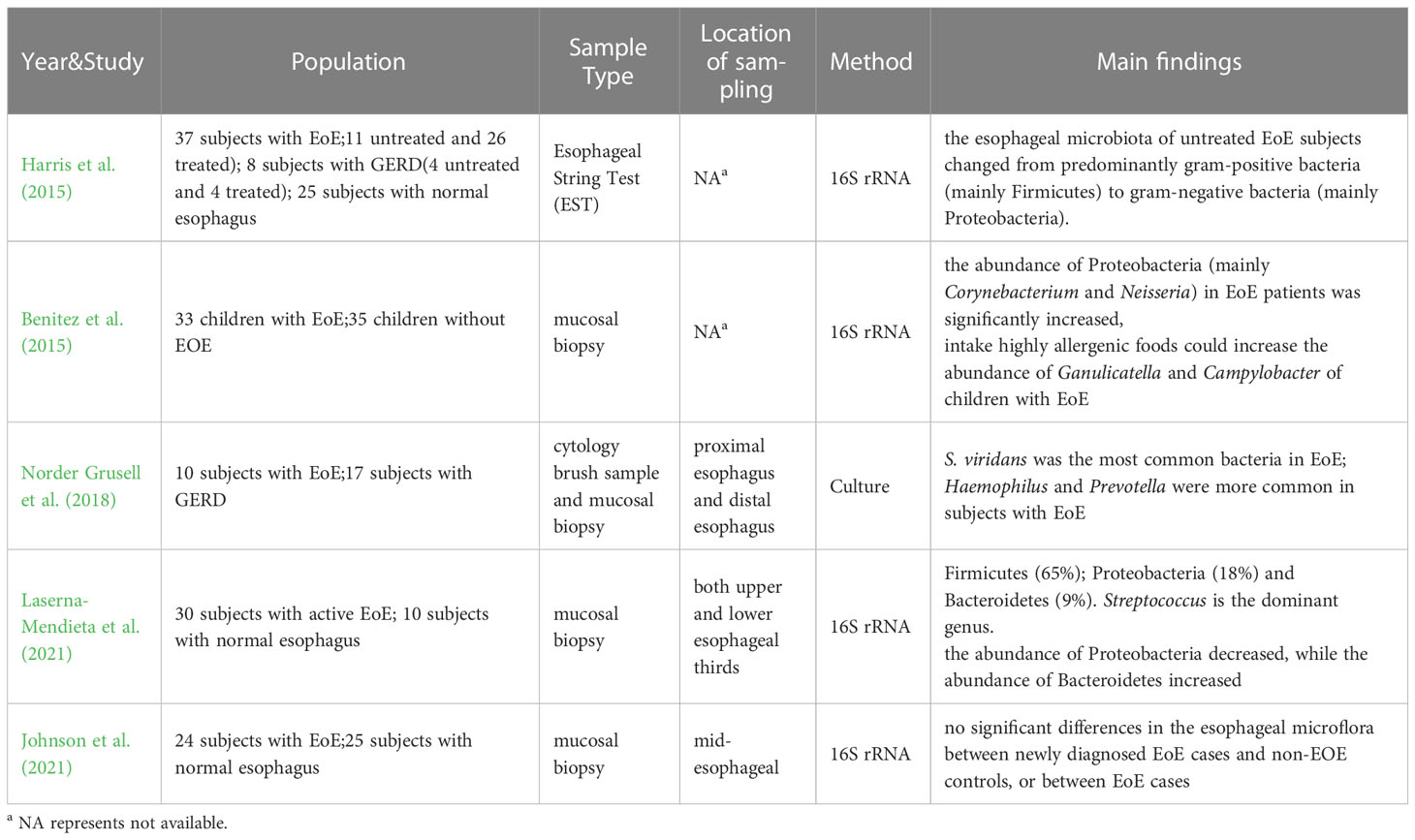
Gastroesophageal reflux (GERD) is characterized by distressing symptoms such as acid reflux and heartburn, as well as complications including bleeding and esophageal stenosis caused by the reflux of gastric contents into the esophagus. Furthermore, chronic gastroesophageal reflux can cause the stratified squamous epithelium that covers in the distal esophagus to be replaced by columnar epithelium, leading to the development of Barrett’s esophagus (BE). Barrett’s esophagus is recognized as a precancerous disease associated with esophageal adenocarcinoma. Therefore, many scientists hope to find strategies to prevent the occurrence of esophageal adenocarcinoma by studying the pathogenesis of GERD and Barrett’s esophagus. In the past, it was believed that GERD and Barrett’s esophagus were triggered by the inflammation of the esophageal mucosa due to exposure to gastric acid or bile. Consequently, the clinical treatment of GERD and Barrett’s esophagus mainly focused on inhibiting gastric acid, protecting esophageal mucosa and promoting peristalsis of esophagus and stomach. However, in 2009, a study linked esophagitis to changes in the esophageal microflora. Yang et al. (2009) divided the esophageal microflora into two types, and they believed that the type II microflora, composed mainly of gram-negative or anaerobic bacteria such as Veillonella, Prevotella, Haemophilus, Campylobacter, Porphyromonas, Neisseria, Granulicatella, Fusobacterium, Rothia and Actinomyces, was closely associated with esophageal diseases such as GERD and Barrett’s esophagus, However, based on current data, it is impossible to determine whether the type II microflora plays a pathogenic role in GERD or Barrett’s esophagus, or whether acid reflux changes the esophageal microflora by affecting acid-sensitive bacteria in the esophagus. In 2013, Liu et al. (2013) studied the esophageal microflora of 6 patients with reflux esophagitis through 16S rRNA gene sequencing. They found that Proteobacteria (43%) was the most prevalent phylum in reflux esophagitis, followed by Firmicutes (33%), Fusobacteria (10%), Bacteroidetes (10%), Saccharibacteria (2%) and Actinomyces (2%). Eleven genera (≥3%) were detected in patients with reflux esophagitis, mainly including Streptococcus (20%), Pasteurella (10%), Haemophilus (9%), Fusobacterium (9%), Klebsiella (9%), Prevotella (5%), Neisseria (4%), Veillonella (3%), Bacillus (3%) and Helicobacter (3%). The researchers also investigated the esophageal microflora of 6 patients with Barrett’s esophagus. The most prevalent phylum in Barrett’s esophagus was Firmicutes (55%), followed by Proteobacteria (20%), Bacteroidetes (14%), Fusobacteria (9%) and Actinobacteria (2%). Similarly, 11 genera (≥3%) were detected in patients with Barrett’s esophagus, mainly including Veillonella (19%), Prevotella (12%), Streptococcus (11%), Fusobacterium (9%), Lactobacillus (4%), Actinobacillus (4%), Neisseria (4%), Helicobacter (4%), Gemella (4%), Achromobacter (3%) and Dialister (3%). Notably, patients with Barrett’s esophagus had a lower proportion of Streptococcus compared to patients with reflux esophagitis and normal esophagus. In addition, Fusobacterium, Neisseria and Veilonella were commonly detected in patients with reflux esophagitis and Barrett’s esophagus, but not in subjects with normal esophagus, indicating differences in microflora among these esophageal conditions. Furthermore, Harris et al. (2015) studied the esophageal microflora of 8 subjects with GERD (4 treated and 4 untreated), and found that the average amount of bacteria in GERD patients was significantly increased compared to normal esophageal subjects. This increase was mainly represented by an increase in Firmicutes and a decrease in Proteobacteria. Similarly, Park et al. (2020) analyzed the esophageal microflora of 18 Non-erosive Gastrooesophageal Reflux Disease (NERD) patients through 16S rRNA gene sequencing, and found that the most common bacterial groups at the phylum level were Firmicutes, Proteobacteria and Bacteroidetes. At the level of genus, Streptococcus, Haemophilus, Prevotella, Veillonella, Neisseria and Granulicatella were more prevalent. This is consistent with the fingdings of Yang et al. (2009). In addition, Okereke et al. (2021) compared the esophageal microflora of 24 patients with Barrett’s esophagus and 40 GERD patients without Barrett’s esophagus, and found that there was a dramatic difference between the Barrett’s esophagus group and the GERD group in a variety of microorganisms (Actinomyces, Prevotellapallens, Dialister, Streptococcus salivarius, Prevotella unspecified, Streptococcus unspecified). With the increase of the length of Barrett’s column, the possibility of detecting various bacteria in the distal esophagus decreased, especially the possibility of detecting Streptococcus, Neisseria, Leptotrichia, Dialister, Gemella, Veillonella, Corynebacterium, Rothia, Haemophilus and Prevotella. The study of Zhou et al. (2020) showed that compared to the normal esophagus group, which had a higher level of gram-positive Firmicutes and Actinomyces, the composition of the NERD microflora has shifted from Fusobacteria and Actinobacteria to Proteobacteria and Bacteroidetes. The composition of microflora in reflux esophagitis and Barrett’s esophagus shifted from Firmicutes to gram-negative Fusobacteria and Proteobacteria, as revealed by 16S rRNA gene sequencing. However, it should be noted that bacteria detected through this method may be not viable and could have amplification deviations. As a result, some researchers still employ traditional culture techniques to measure esophageal microflora. Norder et al (Norder Grusell et al., 2018). measured esophageal microflora in 17 GERD subjects by brush sample, mucosal biopsy and AGAR culture. Alpha-Streptococcus was cultured in 71% (brush) and 76% (biopsy) of the distal esophagus, along with other common genera such as Lactobacillus, Prevotella, Haemophilus, Clostridium and Neisseria. However, not all studies demonstrate significant differences in the microflora of patients with esophagitis compared to those with a normal esophagus. Yu et al. (2019) compared the esophageal microflora of 17 healthy subjects and 32 patients with reflux esophagitis, and found no significant differences between two groups. At the phylum level, only Bacteroidetes differed between groups, with relatively low abundance in the reflux esophagitis group. No significant differences were observed at the family and genus levels. Although the findings of microflora measurement in patients with GERD and Barrett’s esophagus between studies are varied, most studies demonstrated that there are differences in esophageal microflora among GERD, Barrett’s esophagus and normal esophagus. Specifically, gram-negative bacteria are more abundant in GERD and Barrett’s esophagus, and the diversity of microflora is lower in Barrett’s esophagus. The proportion of Streptococcus is reduced in Barrett’s esophagus compared to that in GERD and normal esophagus. Furthermore, Fusobacterium, Neisseria and Veilonella were commonly detected in patients with reflux esophagitis and Barrett’s esophagus, but not in subjects with normal esophagus. These findings provide insights for further understanding of the pathological mechanisms of GERD and Barrett’s esophagus and for predicting the transformation of Barrett’s esophagus into esophageal adenocarcinoma through changes in esophageal microflora. Proteobacteria, Bacteroidetes and Actinobacteria are also mentioned as important phyla that play a role in maintaining the normal esophageal environment. (Table 2)
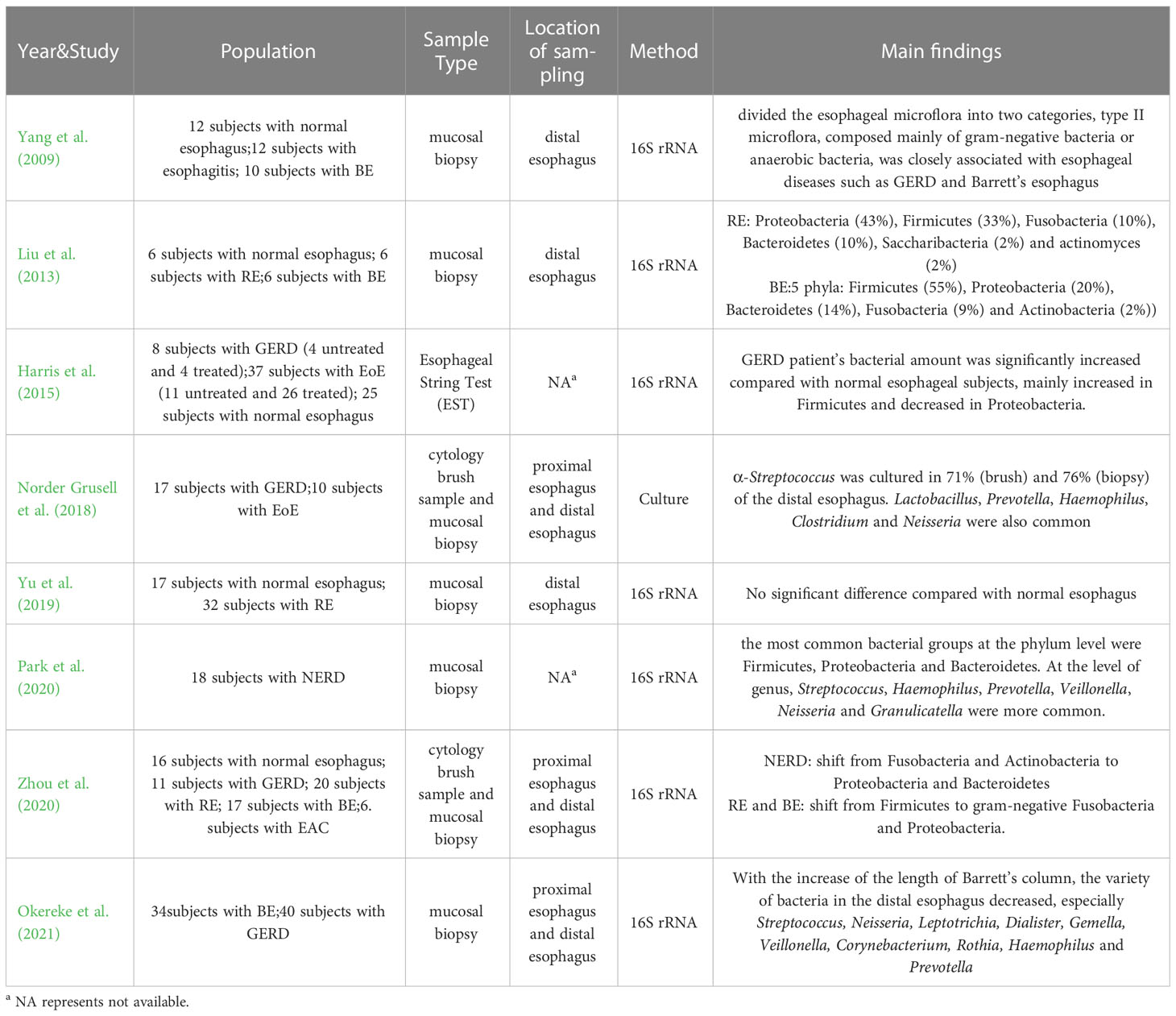
Table 2 Main findings about esophageal microflora of Gastroesophageal reflux (GERD) and Barrett’s esophagus (BE).
Esophageal microflora of the eosinophilic esophagitis
Eosinophilic esophagitis is a chronic esophagitis characterized by eosinophil infiltration into the esophageal wall. Swallowing obstruction, food incarceration, and reflux symptoms are the most common clinical symptoms. Since eosinophilic esophagitis is an immune-related disease and its pathogenesis is not fully understood, it has been hypothesized that esophageal ecological disorders are the trigger for EoE pathology (Jensen and Dellon, 2018). Additionally, environmental factors related to living conditions may also increase EoE susceptibility by causing changes in the esophageal microflora (Jensen et al., 2018). Therefore, researchers have attempted to explore the diagnosis and treatment of eosinophilic esophagitis by studying the esophageal microflora. In 2015, Harris et al. (2015) measured the esophageal flora of 37 EoE subjects (11 untreated and 26 treated), 8 GERD subjects and 25 normal subjects. The results showed no significant difference in α diversity between EoE subjects and the control group, either in normal subjects. In patients with active or treated EoE, Bacteroidetes, Firmicutes, Fusobacterium, and Proteobacteria were dominant, but the average bacterial load detected in all EoE subjects was significantly higher than in normal subjects. There was a significant increase in Haemophilus in untreated EoE compared to normal control subjects, and the esophageal microflora of untreated EoE subjects shifted from predominantly gram-positive bacteria (mainly Firmicutes) to gram-negative bacteria (mainly Proteobacteria). This is consistent with Yang et al.’s view that TypeI bacteria were more common in the normal esophagus and Type II bacteria were more common in patients with esophagitis (Yang et al., 2009). In another study by Benitez et al. (2015), the esophageal microflora of 33 children with EoE and 35 non-EOE children was analyzed, and the results showed that compared to non-EOE children, the abundance of Proteobacteria (mainly Corynebacterium and Neisseria) in EoE patients was significantly increased, while Firmicutes were more prevalent in non-EOE children. Additionally, they found that the intake of highly allergenic foods could significantly increase the abundance of Ganulicatella and Campylobacter in the esophagus of children with eosinophilic esophagitis. In 2018, a study on GERD and EoE by Norder et al (Norder Grusell et al., 2018). showed that bacteria were present in the distal esophagus of all EoE subjects. Compared to GERD subjects and healthy subjects, patients with EoE exhibited a more diverse esophageal microflora. Through the results, they found that S. viridans was the most common bacteria in EoE patients. The study found an increase in Haemophilus in patients with EoE compared to patients with GERD, and Prevotella was more prevalent in subjects with EoE. Laserna-Mendieta et al. (2021) studies on active EoE, which showed that inflammation in EoE did not significantly alter the α-diversity of esophageal microflora. The dominant phylum in both EoE and non-EoE subjects was Firmicutes (65%), followed by Proteobacteria (18%) and Bacteroidetes (9%). Streptococcus was the dominant genus. Compared to the control group, the abundance of Proteobacteria in EoE patients was slightly decreased, while the abundance of Bacteroidetes was increased. However, not all the research shows that there were significant differences between EoE subjects and controls. In a study of 24 adult EoE and 25 adult non-EOE subjects, Johnson et al. (2021) reported no significant differences in esophageal microflora between newly diagnosed adult EoE cases and non-EOE controls, or between EoE cases. As eosinophilic esophagitis is a relatively rare esophageal disease, there are limited studies on the esophageal microflora of eosinophilic esophagitis. Besides, because the prone population of eosinophilic esophagitis includes both adults and children. There still has no definitive conclusion on the esophageal microflora of eosinophilic esophagitis. However, combined with the existing research results, the microflora of EoE patients demonstrated a shift from gram-positive bacteria to gram-negative bacteria, particularly Proteobacteria. Several studies have reported that Proteobacteria increased significantly in the esophagus of EoE patients, which is more pronounced in untreated EoE patients (Table 3).
Esophageal microflora of the esophageal cancer
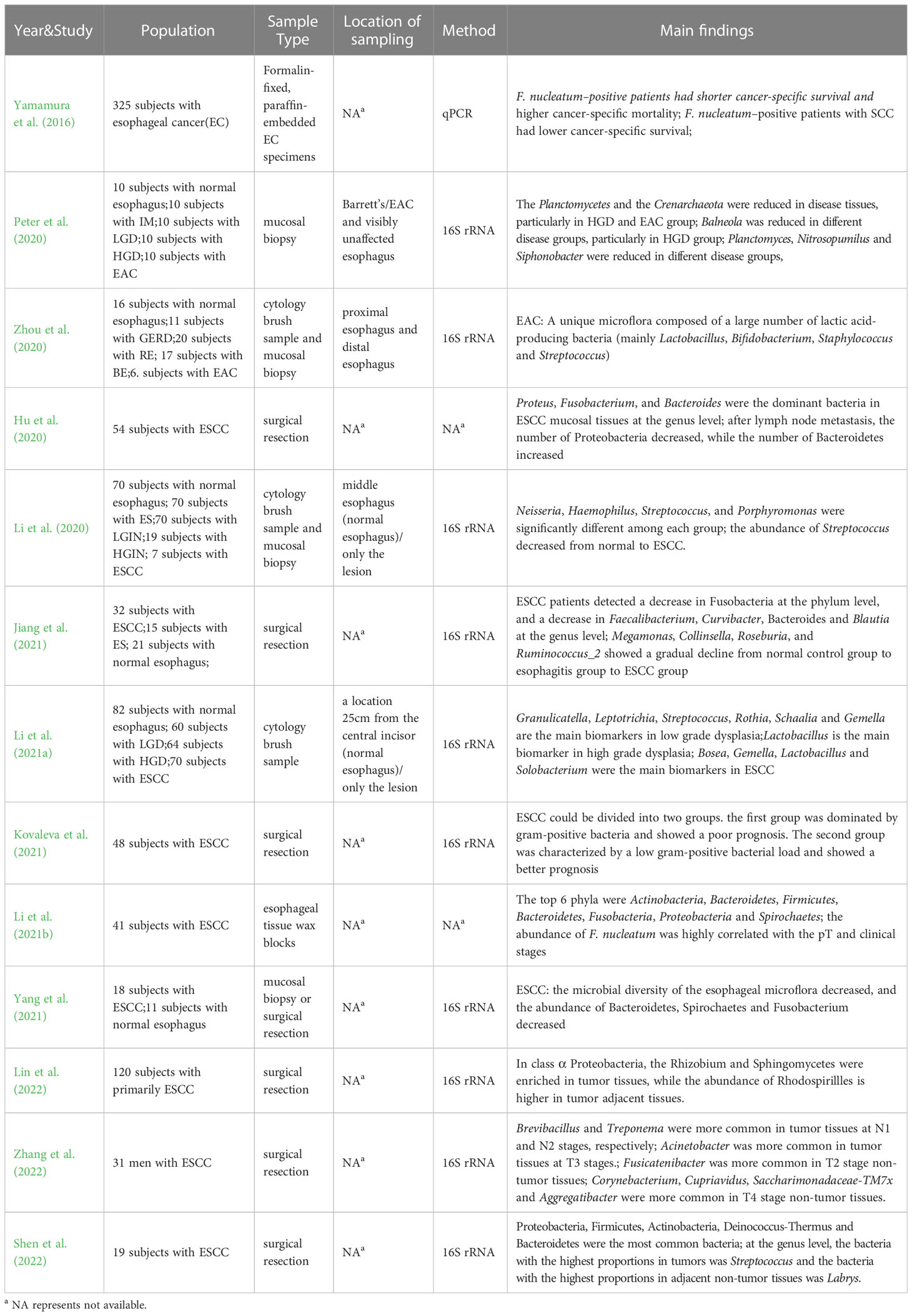
With the rising incidence and mortality rates of esophageal cancer, clinicians and researchers have paid increasing attention to this disease in recent years. However, the early diagnosis and treatment of this disease have remained challenging, with many esophageal cancers cannot be found until they present with symptoms such as dysphagia or odynophagia (Cook et al., 2009; Abnet et al., 2018). The etiology and pathogenesis of esophageal cancer are still not fully understood, making it imperative to uncover potential biomarkers that can be clinically applied. With the deepening of research on human microbes, lots of evidences show that human microbes play a vital role in the occurrence and development of various malignant tumors (Rajagopala et al., 2017; Helmink et al., 2019; Matson et al., 2021; Sepich-Poore et al., 2021). Jiang et al.’s study (Jiang et al., 2021) on Esophageal Squamous Cell Carcinoma (ESCC) found there were significant differences in microbial diversity between ESCC subjects and healthy controls. The species and abundance of the esophageal microflora in patients with ESCC decreased significantly, which means, their bacterial diversity decreased. Specifically, at the phylum level, ESCC patients showed a decrease in Fusobacteria compared to the control group, and at the genus level, they detected a decrease in Faecalibacterium, Curvibacter, Bacteroides and Blautia. In comparison to the esophagitis group, the ESCC group demonstrated fewer Faecalibacterium, Blautia, Bacteroides, but increased Streptococcus. From normal control group to esophagitis group to ESCC group, Megamonas, Collinsella, Roseburia, and Ruminococcus_2 showed a gradual decline. Using multi-level LEfSe analysis, potential microbe biomarkers for ESCC, such as Actinobacillus, Peptostreptococcus, Streptococcus, Prevotella and Fusobacterium were identified. Another study by Lin et al. (2022) found that the relative abundances of Proteobacteria, Fusobacteria, Bacteroidetes and Firmicutes were similar between tumors and adjacent tissues by sequencing the genes of tumor tissues and adjacent tissues of 120 ESCC patients. Within the class α Proteobacteria, Rhizobium and Sphingomycetes were enriched in tumor tissues, while Rhodospirillles was enriched in tumor adjacent tissues. Additionally, Saccharibacteria and its bacterial branches, including H. pylori, were also higher in adjacent tissues of the tumor. The study also revealed decreased esophageal bacterial diversity in ESCC patients. A study by Zhang et al. (2022) on the microflora of ESCC tumors and non-tumor tissues in the esophagus showed that Brevibacillus and Treponema were more commonly present in tumor tissues at N1 and N2 stages, respectively, while Acinetobacter was more common in tumor tissues at T3 stages. Fusicatenibacter was more common in T2 stage non-tumor tissues, while Corynebacterium, Cupriavidus, Saccharimonadaceae-TM7x and Aggregatibacter were more commonly found in T4 stage non-tumor tissues. In addition, more bacteria were associated with base excision repair in tumor tissues, whereas more with nitrotoluene degradation in non-tumor tissues. Different tumor stages can be associated with distinct major bacterial taxa, suggesting the potential involvement of these bacteria in the occurrence and development of ESCC. These findings may contribute to the identification of bacterial markers to predict, diagnose and even treat ESCC. Peter et al. (2020) compared paired samples (disease and non-disease) composed of normal esophagus (n=10), intestinal metaplasia (IM n=10), low-grade dysplasia (LGD n=10), high-grade dysplasia (HGD n=10) and adenocarcinoma (EAC n=10) to analyze the differences in esophageal microflora under different disease states. Results showed that compared to healthy controls, Planctomycetes and Crenarchaeota were significantly decreased in disease tissues, particularly in the HGD group and the adenocarcinoma group, and Balneola was also reduced in different disease groups, particularly in HGD group. Planctomyces, Nitrosopumilus and Siphonobacter in the diseases were also significantly decreased compared to the healthy control group. Li et al. (2021a) divided 276 subjects into 4 groups according to pathology: normal group (n=82), low-grade dysplasia group (LGD n=60), high-grade dysplasia group (HGD n=64) and esophageal squamous cell carcinoma group (ESCC n=70). They collected saliva and samples of the esophageal chest segment with a sterile brush. The study revealed that bacterial diversity in saliva and sterile brush samples decreased with the progression of disease. Granulicatella, Leptotrichia, Streptococcus, Rothia, Schaalia and Gemella were identified as main biomarkers in low grade dysplasia, while Lactobacillus was identified as the main biomarker in high grade dysplasia. Bosea, Gemella, Lactobacillus and Solobacterium were identified as the main biomarkers in ESCC. Zhou (Zhou et al., 2020) observed a unique esophageal adenocarcinoma (EAC) microflora composed of a high abundance of lactic acid-producing bacteria (mainly Lactobacillus, Bifidobacterium, Staphylococcus and Streptococcus), and they believed that this microflora may promote carcinogenic effects through maladjusted lactic acid metabolism. Hu et al. (2020) found that compared to normal esophageal tissues, the diversity and distribution of bacteria in esophageal cancer tissues were reduced and disordered. Proteus, Fusobacterium, and Bacteroides were the dominant bacteria at the genus level in ESCC mucosal tissues, while Prevotella, Klebsiella, Clostridia, Delftia, Streptococcus and Serratia had high abundance, belonging to the dominant genus in esophageal cancer tissue at the subordinate level. Although no significant correlation was found between different locations and stages of ESCC with esophageal microflora, differences in the type of ESCC and the presence or absence of lymph node metastasis could affect the structure of esophageal microflora. After lymph node metastasis, the number of Proteobacteria in esophagus decreased significantly, while the number of Bacteroidetes increased significantly. Shen et al. (2022) sequenced the tumor tissues and adjacent non-tumor tissues from 19 patients with ESCC, revealing that Proteobacteria, Firmicutes, Actinobacteria, Deinococcus-Thermus, and Bacteroidetes were the most common bacteria found in tumor tissues and adjacent non-tumor tissues. Streptococcus (6.93%) was the most abundant genus in tumor tissues, while Labrys (11.1%) was the most abundant genus in adjacent non-tumor tissues. Notably, the complexity of microbial interactions in adjacent non-tumor tissues is stronger than that in tumor tissues, suggesting that microbial interactions may play an important role in maintaining the normal microenvironment of tissues. Kovaleva et al. (2021) reported a significant correlation between bacterial load and tumor interstitial phenotype, with gram-positive bacteria dominating over gram-negative bacteria in the group with high CD206+ macrophage content. Furthermore, they suggested that ESCC could be divided into two groups, both of the which had a high content of CD206+ macrophages. However, the first group was dominated by gram-positive bacteria and showed a poor prognosis, whereas the second group was characterized by a low gram-positive bacterial load and showed a better prognosis. These findings highlight the association between gram-positive bacterial load and ESCC prognosis, and suggest that combining tumor microflora with other matrix markers may have prognostic significance for ESCC. Li et al. (2020) divided the subjects into five groups: normal group (n=70), esophagitis group (n=70), low-grade intraepithelial neoplasia group (LGIN n=70), high-grade intraepithelial neoplasia group (HGIN n=19) and ESCC group (n=7), and conducted gene sequencing of esophageal specimens from different groups. They found that Neisseria, Haemophilus, Streptococcus, and Porphyromonas were significantly different among the groups, with the abundance of Streptococcus decreased from normal to ESCC, while that of other genera increased. Finally, through various combination tests, it was found that the combination of Streptococcus and Neisseria could be used as a microbial prediction model for ESCC and its precancerous lesions. Yang et al. (2021) also showed that the microbial composition in tumor tissues of ESCC patients was significantly different from that in normal esophageal tissues. Specifically, in ESCC patients, the observed decreased microbial diversity and decreased abundance of Bacteroidetes, Spirochaetes and Fusobacterium. Taking these microbial groups as the imbalance index, it can be found that the imbalance flora can well distinguish ESCC from normal esophagus. In addition, Li et al. (2021b) and Yamamura et al. (2016) focused specifically on Fusobacterium nucleatum in ESCC tumor tissues, and found that the relative abundance of F. nucleatum in tumor tissues was significantly higher than that in paired normal tissues, and a higher positive rate of F. nucleatum could be observed in tumors with metastasis compared to tumors without metastasis. Moreover, the cancer specific survival was shortened and the cancer specific mortality was significantly increased in patients with F. nucleatum positive, indicating a close relationship between F. nucleatum, ESCC pT stage, and clinical stage. The researchers suggested that the abundance of F. nucleatum may be used in combination with other indicators to predict ESCC metastasis and prognosis (Table 4).
Conclusions
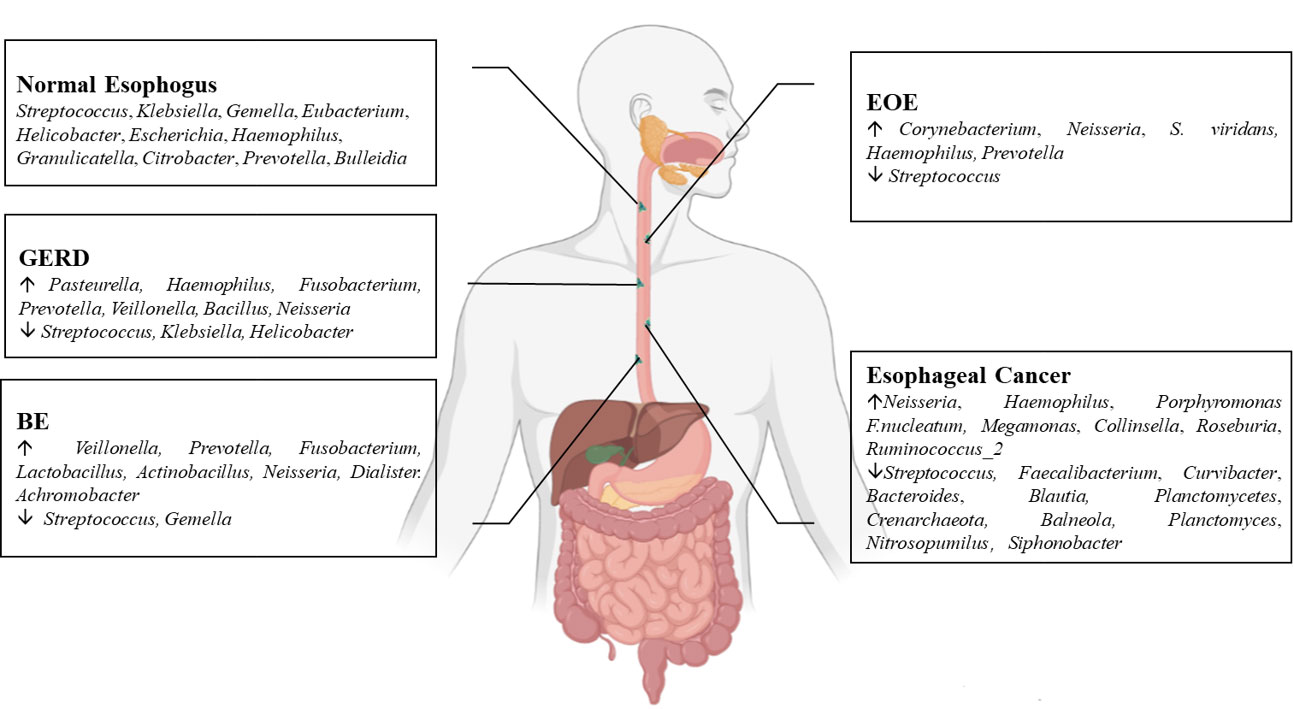
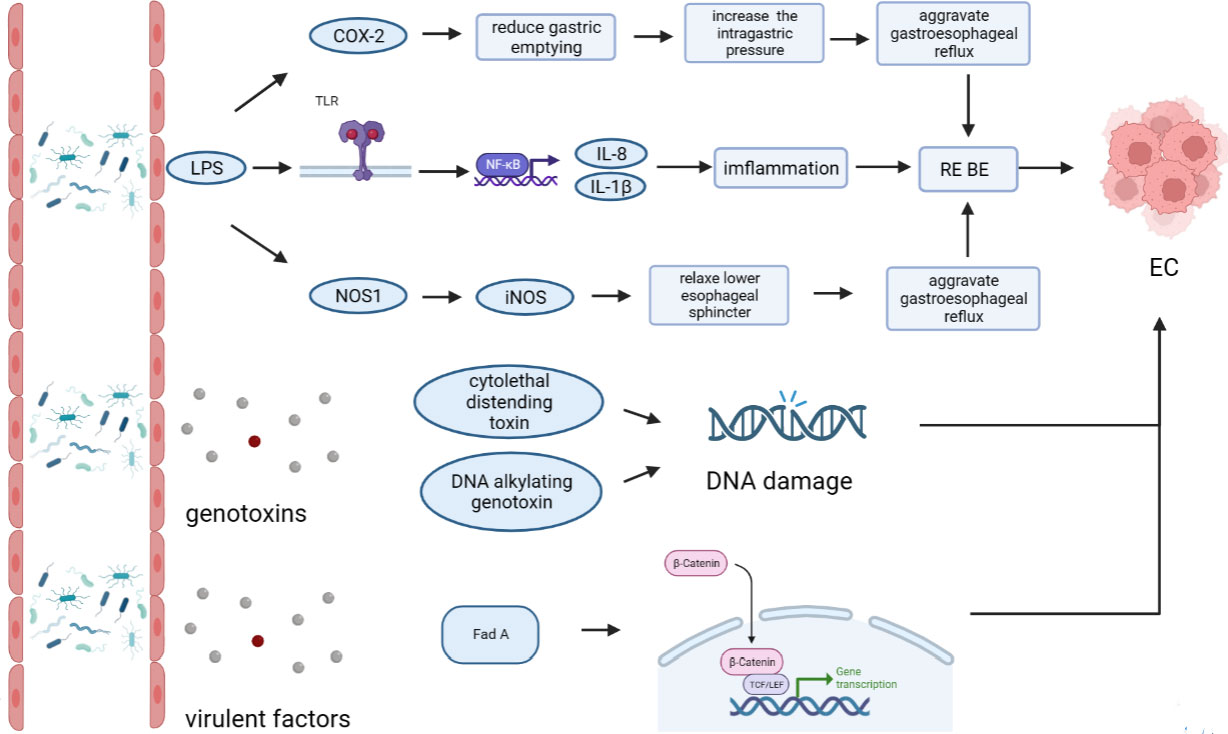
The esophageal microflora is gradually attracting attention in recent years, with a growing number of studies conducted on this topic. Current studies indicate that there is resident microflora in both the normal esophagus and the esophagus suffering from esophageal diseases, and the composition of the esophageal microflora varies among different diseases (Figure 1). As we known, the esophageal microflora is not completely consistent with that of any other part of human body, means that the esophageal microflora has its own uniqueness. But it has been observed that the taxon and composition of bacteria in the esophagus were similar to those in the oral cavity, suggesting that some esophageal bacteria come from the oral cavity, which may be related to the fact that bacteria in the oral cavity can migrate to the esophagus through swallowing and saliva (Mannell et al., 1983; Dewhirst et al., 2010; Yang et al., 2021). Additionally, the esophageal microflora is also influenced by refluxed gastric bacteria. In the normal esophagus, gram-positive bacteria dominate, including six phyla (Firmicutes, Bacteroidetes, Proteobacteria, Fusobacteria, Actinobacteria, Saccharibacteria). Among them, Firmicutes is the most dominant phylum, and Streptococcus was the most prevalent genus. However, in patients with esophagitis, including reflux esophagitis, Barrett’s esophagitis and eosinophilic esophagitis, gram-negative bacteria dominate, and the abundance of Streptococcus decreases. Lipopolysaccharide (LPS) present in gram-negative bacteria can activate Toll-like receptors (TLR), which further activate the NF-κB pathway, promoting the secretion of pro-inflammatory cytokine IL-8, IL-1β. This activation is a key step in the transformation of normal esophagus to BE or esophageal cancer (Pikarsky et al., 2004; Tsukamoto et al., 2018). LPS can also activate inducible nitric oxide synthase one (NOS1) and up-regulate iNOS, leading to the relaxation of the lower esophageal sphincter (Yang et al., 2012). Furthermore, LPS can delay gastric emptying by inducing COX-2 expression (Calatayud et al., 2002), leading to increased gastric pressure. The relaxation of the lower esophageal sphincter and increased gastric pressure can both aggravate gastroesophageal reflux, and long-term gastroesophageal reflux increases the risk of BE and esophageal cancer. Additionally, certain toxins produced by bacteria can cause DNA damage and promote the occurrence of tumors. For instance, several gram-negative bacteria, including Escherichia coli, Actinobacillus actinomycetemcomitans and Campylobacter, can produce cytotoxic swelling toxin (CDT), which can cause DNA damage, promoting the occurrence of cancer (Nesic et al., 2004; He et al., 2019). F. nucleatum can produce virulence factor Fad A, which promotes tumor development by interacting with E-cadherin to activate β-catenin signal (Rubinstein et al., 2013). Despite the increase of gram-negative bacteria, the diversity of the esophageal microflora in esophageal cancer tends to decline. Studies have found that different tumor types, and the presence or absence of lymph node metastasis can lead to significant changes in esophageal microflora, although there are different opinions on whether there are significant differences in esophageal microflora of different tumor stages. However, most studies believe that the esophageal microflora of esophageal tumors at different clinical stages varies. The load of gram-positive bacteria can be utilized as a prognostic indicator for esophageal cancer. F. nucleatum was significantly higher in tumor tissues compared to paired normal tissues, with a higher positive rate observed in tumors with metastasis compared to tumors without metastasis. This finding is consistent with the aforementioned virulence factor Fad A of F. nucleatum, which promotes tumor development by activating β-catenin signaling. While several mechanisms linking the esophageal microflora to esophageal diseases have been proposed (Figure 2), more research is needed to fully understand how these microorganisms interact with each other and with the host’s immune system in order to cause or exacerbate esophageal diseases. Moreover, there is ongoing debate about whether changes in the microbiota lead to the development of esophageal diseases, or if esophageal diseases drive the transformation of the microbiota. Esophageal diseases such as esophagitis, GERD, or esophageal cancer can cause changes in the esophageal mucosa and local environment, resulting in alterations in the esophageal microbiota. Studies have shown a dose-dependent association between penicillin exposure and an increased risk of cancer, including esophageal cancer (Boursi et al., 2015), providing support for the idea that changes in the microflora precede inflammation and disease. Other studies have shown that the imbalance of microflora is a potential side effect of acidic environment caused by GERD (Amir et al., 2014), P.gingivalis can selectively infect the ESCC subjects’ tumor and adjacent mucosa, but cannot infect the healthy mucosa of the control group (Gao et al., 2016), indicating that esophageal disease can lead to the changes of esophageal microflora. These researches suggest a reciprocal causal relationship between esophageal disease and changes in esophageal microflora, whereby the mucosal microenvironment can be remodeled by pathogenic microflora, and changes in the mucosal microenvironment can further promote alterations in the microflora. However, despite the increasing number of studies on esophageal microflora, achieving complete uniformity of results is challenging due to differences in inclusion and exclusion criteria, sampling methods, sampling sites, culture and determination methods, among others. Various limitations exist in current methods of studying esophageal microflora, including the invasiveness of mucosal biopsy, inability to successfully sample certain bacteria attached to the mucosa with esophageal aspirate, bias in traditional bacterial culture, and inability of gene amplification technology to assess bacterial viability or potential amplification bias after treatment steps in 16S rRNA gene sequencing. With the development of genomics, we can make use of the prospect of multi-omics, that is, meta-proteinomics, metatranscriptomics to know the expression of each gene and metabolomics to see the potential impact of metabolites of flora on the disease. In the near future, utilizing these advanced techniques may enable us to better understand the role of esophageal microbiome in esophageal diseases, identify effective molecular markers for predicting conditions such as BE, esophageal cancer, and other esophageal diseases, and develop more accurate screening and diagnostic plans to contribute to the prevention and treatment of esophageal diseases.
Author contributions
QZ: data curation, formal analysis, writing-original draft. LF, XC and YQ: review, revision and editing. LX: resources, supervision, project administration and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by National Natural Science Foundation of Shenzhen (JCYJ20190808111610984).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abnet, C. C., Arnold, M., Wei, W. Q. (2018). Epidemiology of esophageal squamous cell carcinoma. Gastroenterology 154 (2), 360–373. doi: 10.1053/j.gastro.2017.08.023
Amir, I., Konikoff, F. M., Oppenheim, M., Gophna, U., Half, E. E. (2014). Gastric microbiota is altered in oesophagitis and barrett’s oesophagus and further modified by proton pump inhibitors. Environ. Microbiol. 16 (9), 2905–2914. doi: 10.1111/1462-2920.12285
Benitez, A. J., Hoffmann, C., Muir, A. B., Dods, K. K., Spergel, J. M., Bushman, F. D., et al. (2015). Inflammation-associated microbiota in pediatric eosinophilic esophagitis. Microbiome 3, 23. doi: 10.1186/s40168-015-0085-6
Boursi, B., Mamtani, R., Haynes, K., Yang, Y. X. (2015). Recurrent antibiotic exposure may promote cancer formation–another step in understanding the role of the human microbiota? Eur. J. Cancer 51 (17), 2655–2664. doi: 10.1016/j.ejca.2015.08.015
Calatayud, S., Garcia-Zaragoza, E., Hernandez, C., Quintana, E., Felipo, V., Esplugues, J. V., et al. (2002). Downregulation of nNOS and synthesis of PGs associated with endotoxin-induced delay in gastric emptying. Am. J. Physiol. Gastrointest Liver Physiol. 283 (6), G1360–G1367. doi: 10.1152/ajpgi.00168.2002
Cook, M. B., Chow, W. H., Devesa, S. S. (2009). Oesophageal cancer incidence in the united states by race, sex, and histologic type, 1977-2005. Br. J. Cancer 101 (5), 855–859. doi: 10.1038/sj.bjc.6605246
Cox, M. J., Cookson, W. O., Moffatt, M. F. (2013). Sequencing the human microbiome in health and disease. Hum. Mol. Genet. 22 (R1), R88–R94. doi: 10.1093/hmg/ddt398
Dewhirst, F. E., Chen, T., Izard, J., Paster, B. J., Tanner, A. C. R., Yu, W.-H., et al. (2010). The human oral microbiome. J. Bacteriol 192 (19), 5002–5017. doi: 10.1128/JB.00542-10
Finlay, I. G., Wright, P. A., Menzies, T., McArdle, C. S. (1982). Microbial flora in carcinoma of oesophagus. Thorax 37 (3), 181–184. doi: 10.1136/thx.37.3.181
Gagliardi, D., Makihara, S., Corsi, P. R., Viana Ade, T., Wiczer, M. V., Nakakubo, S., et al. (1998). Microbial flora of the normal esophagus. Dis. Esophagus 11 (4), 248–250. doi: 10.1093/dote/11.4.248
Gao, S., Li, S., Ma, Z., Liang, S., Shan, T., Zhang, M., et al. (2016). Presence of porphyromonas gingivalis in esophagus and its association with the clinicopathological characteristics and survival in patients with esophageal cancer. Infect. Agent Cancer 11, 3. doi: 10.1186/s13027-016-0049-x
Harris, J. K., Fang, R., Wagner, B. D., Choe, H. N., Kelly, C. J., Schroeder, S., et al. (2015). Esophageal microbiome in eosinophilic esophagitis. PloS One 10 (5), e0128346. doi: 10.1371/journal.pone.0128346
He, Z., Gharaibeh, R. Z., Newsome, R. C., Pope, J. L., Dougherty, M. W., Tomkovich, S., et al. (2019). Campylobacter jejuni promotes colorectal tumorigenesis through the action of cytolethal distending toxin. Gut 68 (2), 289–300. doi: 10.1136/gutjnl-2018-317200
Helmink, B. A., Khan, M. A. W., Hermann, A., Gopalakrishnan, V., Wargo, J. A. (2019). The microbiome, cancer, and cancer therapy. Nat. Med. 25 (3), 377–388. doi: 10.1038/s41591-019-0377-7
Hu, M., Bai, W., Zhao, C., Wang, J. (2020). Distribution of esophagus flora in esophageal squamous cell carcinoma and its correlation with clinicopathological characteristics. Transl. Cancer Res. 9 (6), 3973–3985. doi: 10.21037/tcr-20-1954
Jensen, E. T., Dellon, E. S. (2018). Environmental factors and eosinophilic esophagitis. J. Allergy Clin. Immunol. 142 (1), 32–40. doi: 10.1016/j.jaci.2018.04.015
Jensen, E. T., Kuhl, J. T., Martin, L. J., Langefeld, C. D., Dellon, E. S., Rothenberg, M. E. (2018). Early-life environmental exposures interact with genetic susceptibility variants in pediatric patients with eosinophilic esophagitis. J. Allergy Clin. Immunol. 141 (2), 632–637.e635. doi: 10.1016/j.jaci.2017.07.010
Jiang, Z., Wang, J., Shen, Z., Zhang, Z., Wang, S. (2021). Characterization of esophageal microbiota in patients with esophagitis and esophageal squamous cell carcinoma. Front. Cell Infect. Microbiol. 11, 774330. doi: 10.3389/fcimb.2021.774330
Johnson, J., Dellon, E. S., McCoy, A. N., Sun, S., Jensen, E. T., Fodor, A. A., et al. (2021). Lack of association of the esophageal microbiome in adults with eosinophilic esophagitis compared with non-EoE controls. J. Gastroint Liver Dis. 30 (1), 17–24. doi: 10.15403/jgld-3049
Kovaleva, O., Podlesnaya, P., Rashidova, M., Samoilova, D., Petrenko, A., Mochalnikova, V., et al. (2021). Prognostic significance of the microbiome and stromal cells phenotype in esophagus squamous cell carcinoma. Biomedicines 9 (7), 743. doi: 10.3390/biomedicines9070743
Laserna-Mendieta, E. J., FitzGerald, J. A., Arias-Gonzalez, L., Ollala, J. M., Bernardo, D., Claesson, M. J., et al. (2021). Esophageal microbiome in active eosinophilic esophagitis and changes induced by different therapies. Sci. Rep. 11 (1), 7113. doi: 10.1038/s41598-021-86464-z
Lau, W. F., Wong, J., Lam, K. H., Ong, G. B. (1981). Oesophageal microbial flora in carcinoma of the oesophagus. Aust. N Z J. Surg. 51 (1), 52–55. doi: 10.1111/j.1445-2197.1981.tb05905.x
Li, Z., Dou, L., Zhang, Y., He, S., Zhao, D., Hao, C., et al. (2021a). Characterization of the oral and esophageal microbiota in esophageal precancerous lesions and squamous cell carcinoma. Front. Cell Infect. Microbiol. 11, 714162. doi: 10.3389/fcimb.2021.714162
Li, M., Shao, D., Zhou, J., Gu, J., Qin, J., Chen, W., et al. (2020). Signatures within esophageal microbiota with progression of esophageal squamous cell carcinoma. Chin. J. Cancer Res. 32 (6), 755–767. doi: 10.21147/j.issn.1000-9604.2020.06.09
Li, Z., Shi, C., Zheng, J., Guo, Y., Fan, T., Zhao, H., et al. (2021b). Fusobacterium nucleatum predicts a high risk of metastasis for esophageal squamous cell carcinoma. BMC Microbiol. 21 (1), 301. doi: 10.1186/s12866-021-02352-6
Lin, Z., Rao, W., Xiang, Z., Zeng, Q., Liu, S., Yu, K., et al. (2022). Characteristics and interplay of esophageal microbiota in esophageal squamous cell carcinoma. BMC Cancer 22 (1), 696. doi: 10.1186/s12885-022-09771-2
Liu, N., Ando, T., Ishiguro, K., Maeda, O., Watanabe, O., Funasaka, K., et al. (2013). Characterization of bacterial biota in the distal esophagus of Japanese patients with reflux esophagitis and barrett’s esophagus. BMC Infect. Dis. 13, 130. doi: 10.1186/1471-2334-13-130
Mannell, A., Plant, M., Frolich, J. (1983). The microflora of the oesophagus. Ann. R Coll. Surg. Engl. 65 (3), 152–154.
Matson, V., Chervin, C. S., Gajewski, T. F. (2021). Cancer and the microbiome-influence of the commensal microbiota on cancer, immune responses, and immunotherapy. Gastroenterology 160 (2), 600–613. doi: 10.1053/j.gastro.2020.11.041
Metzker, M. L. (2010). Sequencing technologies - the next generation. Nat. Rev. Genet. 11 (1), 31–46. doi: 10.1038/nrg2626
Nardone, G., Compare, D., Rocco, A. (2017). A microbiota-centric view of diseases of the upper gastrointestinal tract. Lancet Gastroenterol. Hepatol. 2 (4), 298–312. doi: 10.1016/S2468-1253(16)30108-X
Nesic, D., Hsu, Y., Stebbins, C. E. (2004). Assembly and function of a bacterial genotoxin. Nature 429 (6990), 429–433. doi: 10.1038/nature02532
Norder Grusell, E., Dahlen, G., Ruth, M., Bergquist, H., Bove, M. (2018). The cultivable bacterial flora of the esophagus in subjects with esophagitis. Scand. J. Gastroenterol. 53 (6), 650–656. doi: 10.1080/00365521.2018.1457712
Okereke, I. C., Miller, A. L., Jupiter, D. C., Hamilton, C. F., Reep, G. L., Krill, T., et al. (2021). Microbiota detection patterns correlate with presence and severity of barrett’s esophagus. Front. Cell Infect. Microbiol. 11, 555072. doi: 10.3389/fcimb.2021.555072
Park, C. H., Seo, S. I., Kim, J. S., Kang, S. H., Kim, B. J., Choi, Y. J., et al. (2020). Treatment of non-erosive reflux disease and dynamics of the esophageal microbiome: a prospective multicenter study. Sci. Rep. 10 (1), 15154. doi: 10.1038/s41598-020-72082-8
Paull, G., Yardley, J. H. (1988). Gastric and esophageal Campylobacter pylori in patients with barrett’s esophagus. Gastroenterology 95 (1), 216–218. doi: 10.1016/0016-5085(88)90316-2
Pei, Z., Bini, E. J., Yang, L., Zhou, M., Francois, F., Blaser, M. J. (2004). Bacterial biota in the human distal esophagus. Proc. Natl. Acad. Sci. U.S.A. 101 (12), 4250–4255. doi: 10.1073/pnas.0306398101
Peter, S., Pendergraft, A., VanDerPol, W., Wilcox, C. M., Kyanam Kabir Baig, K. R., Morrow, C., et al. (2020). Mucosa-associated microbiota in barrett’s esophagus, dysplasia, and esophageal adenocarcinoma differ similarly compared with healthy controls. Clin. Transl. Gastroenterol. 11 (8), e00199. doi: 10.14309/ctg.0000000000000199
Pikarsky, E., Porat, R. M., Stein, I., Abramovitch, R., Amit, S., Kasem, S., et al. (2004). NF-kappaB functions as a tumour promoter in inflammation-associated cancer. Nature 431 (7007), 461–466. doi: 10.1038/nature02924
Polyzos, S. A., Zeglinas, C., Artemaki, F., Doulberis, M., Kazakos, E., Katsinelos, P., et al. (2018). Helicobacter pylori infection and esophageal adenocarcinoma: a review and a personal view. Ann. Gastroenterol. 31 (1), 8–13. doi: 10.20524/aog.2017.0213
Rajagopala, S. V., Vashee, S., Oldfield, L. M., Suzuki, Y., Venter, J. C., Telenti, A., et al. (2017). The human microbiome and cancer. Cancer Prev. Res. (Phila) 10 (4), 226–234. doi: 10.1158/1940-6207.CAPR-16-0249
Rubinstein, M. R., Wang, X., Liu, W., Hao, Y., Cai, G., Han, Y. W. (2013). Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating e-cadherin/beta-catenin signaling via its FadA adhesin. Cell Host Microbe 14 (2), 195–206. doi: 10.1016/j.chom.2013.07.012
Sepich-Poore, G. D., Zitvogel, L., Straussman, R., Hasty, J., Wargo, J. A., Knight, R. (2021). The microbiome and human cancer. Science 371 (6536), eabc4552. doi: 10.1126/science.abc4552
Shen, W., Tang, D., Wan, P., Peng, Z., Sun, M., Guo, X., et al. (2022). Identification of tissue-specific microbial profile of esophageal squamous cell carcinoma by full-length 16S rDNA sequencing. Appl. Microbiol. Biotechnol. 106 (8), 3215–3229. doi: 10.1007/s00253-022-11921-2
Team NIHHMPA (2019). A review of 10 years of human microbiome research activities at the US national institutes of health, fiscal years 2007-2016. Microbiome 7 (1), 31. doi: 10.1186/s40168-019-0620-y
Tian, Z., Yang, Z., Gao, J., Zhu, L., Jiang, R., Jiang, Y. (2015). Lower esophageal microbiota species are affected by the eradication of helicobacter pylori infection using antibiotics. Exp. Ther. Med. 9 (3), 685–692. doi: 10.3892/etm.2015.2169
Tsukamoto, H., Takeuchi, S., Kubota, K., Kobayashi, Y., Kozakai, S., Ukai, I., et al. (2018). Lipopolysaccharide (LPS)-binding protein stimulates CD14-dependent toll-like receptor 4 internalization and LPS-induced TBK1-IKKϵ-IRF3 axis activation. J. Biol. Chem. 293 (26), 10186–10201. doi: 10.1074/jbc.M117.796631
Yamamura, K., Baba, Y., Nakagawa, S., Mima, K., Miyake, K., Nakamura, K., et al. (2016). Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clin. Cancer Res. 22 (22), 5574–5581. doi: 10.1158/1078-0432.CCR-16-1786
Yang, W., Chen, C. H., Jia, M., Xing, X., Gao, L., Tsai, H. T., et al. (2021). Tumor-associated microbiota in esophageal squamous cell carcinoma. Front. Cell Dev. Biol. 9, 641270. doi: 10.3389/fcell.2021.641270
Yang, L., Francois, F., Pei, Z. (2012). Molecular pathways: pathogenesis and clinical implications of microbiome alteration in esophagitis and Barrett esophagus. Clin. Cancer Res. 18 (8), 2138–2144. doi: 10.1158/1078-0432.CCR-11-0934
Yang, L., Lu, X., Nossa, C. W., Francois, F., Peek, R. M., Pei, Z. (2009). Inflammation and intestinal metaplasia of the distal esophagus are associated with alterations in the microbiome. Gastroenterology 137 (2), 588–597. doi: 10.1053/j.gastro.2009.04.046
Yu, Y., Gao, F., Chen, X., Zheng, S., Zhang, J. (2019). Changes in the distal esophageal microbiota in Chinese patients with reflux esophagitis. J. Dig Dis. 20 (1), 18–24. doi: 10.1111/1751-2980.12692
Zhang, B., Xiao, Q., Chen, H., Zhou, T., Yin, Y. (2022). Comparison of tumor-associated and nontumor-associated esophageal mucosa microbiota in patients with esophageal squamous cell carcinoma. Med. (Baltimore) 101 (37), e30483. doi: 10.1097/MD.0000000000030483
Zhou, J., Shrestha, P., Qiu, Z., Harman, D. G., Teoh, W. C., Al-Sohaily, S., et al. (2020). Distinct microbiota dysbiosis in patients with non-erosive reflux disease and esophageal adenocarcinoma. J. Clin. Med. 9 (7), 2162. doi: 10.3390/jcm9072162
Keywords: esophageal diseases, microbiota, gastroesophageal reflux, Barrett’s esophagus, eosinophilic esophagitis, esophageal cancer
Citation: Zou Q, Feng L, Cai X, Qian Y and Xu L (2023) Esophageal microflora in esophageal diseases. Front. Cell. Infect. Microbiol. 13:1145791. doi: 10.3389/fcimb.2023.1145791
Received: 16 January 2023; Accepted: 09 May 2023;
Published: 19 May 2023.
Edited by:
Gang Sun, The First Affiliated Hospital of People’s Liberation Army General Hospital, ChinaReviewed by:
Toshimi Chiba, Iwate Medical University, JapanYoulian Zhou, Guangzhou First People’s Hospital, China
Copyright © 2023 Zou, Feng, Cai, Qian and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Long Xu, bG9uZ3h1MTAxMkBzenUuZWR1LmNu
 Qian Zou
Qian Zou Lijuan Feng
Lijuan Feng Xunchao Cai
Xunchao Cai Yun Qian
Yun Qian