
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cell. Infect. Microbiol., 03 May 2023
Sec. Antibiotic Resistance and New Antimicrobial drugs
Volume 13 - 2023 | https://doi.org/10.3389/fcimb.2023.1093842
This article is part of the Research TopicEnterobacteriaceae Antimicrobial Agents and Resistance: Relationship with the Therapeutic Approach, Volume IIView all 11 articles
 Wei Zhang1†
Wei Zhang1† Chun-Yu Yan2†
Chun-Yu Yan2† Shu-Rui Li3†
Shu-Rui Li3† Ting-Ting Fan1†
Ting-Ting Fan1† Shan-Shan Cao1
Shan-Shan Cao1 Bin Cui4
Bin Cui4 Meng-Ying Li5
Meng-Ying Li5 Bo-Yuan Fan6
Bo-Yuan Fan6 Bo Ji7
Bo Ji7 Li Wang7
Li Wang7 Fei Cui8
Fei Cui8 Jia Cui1
Jia Cui1 Lei Wang1
Lei Wang1 Yue Guan1*
Yue Guan1* Jing-Wen Wang1*
Jing-Wen Wang1*Introduction: Extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae pose a huge threat to human health, especially in the context of complicated urinary tract infections (cUTIs). Carbapenems and piperacillin–tazobactam (PTZ) are two antimicrobial agents commonly used to treat cUTIs.
Methods: A monocentric retrospective cohort study focused on the treatment of cUTIs in adults was conducted from January 2019 to November 2021. Patients with a positive urine culture strain yielding ≥ 103 colony-forming units per milliliter (CFU/mL), and sensitive to PTZ and carbapenems, were included. The primary endpoint was clinical success after antibiotic therapy. The secondary endpoint included rehospitalization and 90-day recurrence of cUTIs caused by ESBL-producing Enterobacteriaceae.
Results: Of the 195 patients included in this study, 110 were treated with PTZ while 85 were administered meropenem. The rate of clinical cure was similar between the PTZ and meropenem groups (80% vs. 78.8%, p = 0.84). However, the PTZ group had a lower duration of total antibiotic use (6 vs. 9; p < 0.01), lower duration of effective antibiotic therapy (6 vs. 8; p < 0.01), and lower duration of hospitalization (16 vs. 22; p < 0.01).
Discussion: In terms of adverse events, the safety of PTZ was higher than that of meropenem in the treatment of cUTIs.
Complicated urinary tract infections (cUTIs) are defined by the presence of systemic symptoms or by the susceptibility of the host to a complicated disease course (Geerlings et al., 2013). Systemic symptoms include fever, febrile UTI, and other symptoms indicative of tissue infections like pyelonephritis, prostatitis, or urosepsis syndrome (Geerlings et al., 2013). cUTIs occur in patients having a structural or functional abnormality in their genitourinary tract or through infection of urinary catheters (Melekos and Naber, 2000; Kongnakorn et al., 2019). Most of the challenging cUTIs are caused by Gram-negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, that can resist multiple antimicrobial agents by producing extended-spectrum β-lactamase (ESBL) enzymes, such as CTX-M enzymes, AmpC β-lactamases, and carbapenemases (Chatterjee et al., 2021; Syed, 2021; Jean et al., 2022; López Montesinos et al., 2022; Wald-Dickler et al., 2022; Zilberberg et al., 2022). By prolonging hospitalization, cUTIs have imposed a serious burden on healthcare systems (Food and Drug Administration, 2018; Vallejo-Torres et al., 2018; Zilberberg et al., 2021).
The treatment options for cUTIs are distinct from those for uncomplicated UTIs. For decades, carbapenems—members of the broad-spectrum β-lactam family—have been identified as the gold standard antibiotic therapy for cUTIs caused by ESBL-producing Enterobacteriaceae. They potently inhibit cell wall biosynthesis by preventing transpeptidation in many Gram-positive, Gram-negative, and anaerobic bacteria (Zhanel et al., 2007; Bush and Bradford, 2016; Armstrong et al., 2021). Meropenem is an antibacterial agent from the carbapenem family that is commonly used in empirical therapy for serious infections before the causative organism has been identified (Wiseman et al., 1995; Baldwin et al., 2008).
Piperacillin is a β-lactam antibiotic that is commonly used to boost the antibacterial activity of tazobactam (Drawz and Bonomo, 2010). ESBL-producing Enterobacteriaceae are susceptible to β-lactam/β-lactamase inhibitor combinations, such as piperacillin–tazobactam (PTZ), which can inhibit ESBL enzymes that confer antibiotic resistance.
Meropenem and PTZ constitute a considerable part of the therapeutic regimens employed in clinical practice at Xijing Hospital. The real-world setting for the treatment of cUTIs involves complex medical complications and variable physical conditions, which make the choice of the optimum antibiotic regimen a challenging one. Retrospective studies with real-world data can help clinical practitioners deliver precise prescriptions in the future.
This study aimed to utilize real-world data assessing the efficacy and safety of β-lactam antibiotics (PTZ) versus carbapenems (meropenem) for the effective treatment of cUTIs caused by ESBL-producing Enterobacteriaceae.
A monocentric and retrospective cohort study was conducted involving patients treated for cUTIs between January 2019 and November 2021. The objective of this study was to compare the efficacy and safety of PTZ and meropenem for treating cUTIs caused by ESBL-producing Enterobacteriaceae.
Adult patients were eligible if they were diagnosed with cUTIs caused by ESBL-producing Enterobacteriaceae that were non-susceptible to ceftriaxone or cefotaxime, but susceptible to PTZ and meropenem. Some patients may suffer from acute cystitis and acute pyelonephritis due to the administered interventions. Patients were treated with PTZ or meropenem for more than 72 h. General practitioners adapted the antibiotic dosage, administration route, and treatment duration for each individual based on their renal function as measured by their creatinine clearance rate.
The local research team screened patients manually using inclusion and exclusion criteria, and data were selected from patient medical charts using standardized case report forms.
Patients who met all the following criteria were included in this study:
● Age ≥ 18 years
● Documented cUTIs, with a positive urine culture strain ≥ 103 colony-forming units per milliliter (CFU/ml) that is sensitive to PTZ and carbapenems. The cUTIs must be accompanied by at least two of the following signs and symptoms (Food and Drug Administration, 2018):
● chills or fever (temperature > 38°C)
● nausea or vomiting
● flank or pelvic pain
● dysuria, urinary frequency, or urgency
● costovertebral angle tenderness on physical examination (Delory et al., 2021)
Patients who met any of the following criteria were excluded from this study:
● Antibiotic treatment for less than 72 h
● Urine culture positive for Gram-positive bacteria at a colony count ≥ 105 CFU/ml
● Urine culture positive for fungi at a colony count > 103 CFU/ml
● Repeated exposure to the drugs used in this study
The experimental procedures included baseline urine collection for quantitative culture. The signs and symptoms of cUTIs and adverse events were routinely monitored. Prespecified laboratory data, including chemistry panels and urine cultures, were collected.
Baseline urine cultures at a colony count ≥ 105 CFU/ml were sent to the central laboratory (Department of Laboratory Medicine, Institute of Clinical Laboratory Medicine of PLA, Xijing Hospital, Air Force Military Medical University) for identification, quantification, susceptibility testing, and further characterization of the organism(s). The minimum inhibitory concentrations (MICs) of PTZ and meropenem were determined using the agar dilution reference method, following the laboratory procedures and MIC breakpoints provided by CLSI (2021).
The primary efficacy endpoint of this study was the clinical and microbiological response in patients with cUTIs at the end of the initial antibiotic regimens. The clinical response was defined by the Food and Drug Administration (FDA) as follows:
● Resolution of all core cUTI symptoms, including fever (temperature > 38°C), dysuria, urinary frequency, urinary urgency, suprapubic pain, and flank pain
● No appearance of new cUTI symptoms
● No further use of antibiotics with microbiological cure (urine culture at a colony count < 103 CFU/ml, negative blood culture)
According to the FDA guidelines, the microbiological response was defined as a colony count of the bacterial pathogen, identified at trail entry, falling below 103 CFU/ml in the urine (Food and Drug Administration, 2018).
Clinical failure was defined as the non-resolution of fever (temperature > 38°C) and cUTI symptoms, the development of new symptoms, or all-cause mortality of the patient. Microbiological failure was defined as the pathogen at a colony count exceeding or equalling 103 CFU/ml during or after the treatment. Clinical uncertainty was defined as the loss of urine samples after baseline therapy.
The secondary efficacy endpoint pertained to the determination of sustained microbiological success and all clinical cures. It was measured in terms of the rates of rehospitalization and recurrent cUTIs due to the same ESBL-producing Enterobacteriaceae within 3 months of the initial antibiotic treatment.
The safety endpoints included the incidence of Clostridium difficile infections, rehospitalization, the loss of intervention and follow-up, and all-cause mortality within 3 months of the first day of effective treatment.
The International Business Machines Corporation SPSS Statistics for Windows Version 22.0 and Microsoft Excel (MS Office 2019) were used for data analysis. The analysis population, which included any patients receiving the correct antibiotics, was used to compare the efficacy and safety of the treatment group (PTZ) with that of the control group (meropenem), in terms of the primary and secondary outcomes. The study outcomes were presented using descriptive statistics, such as frequencies and percentages, medians, and interquartile ranges. Medians and interquartile ranges were reported instead of means and standard deviations because the continuous variables were not normally distributed. Nonparametric tests were used in this data analysis. The primary analysis included a chi-squared test to compare the proportion of patients with cUTIs that showed clinical success in the PTZ and meropenem groups. The continuous variables were compared using chi-squared or Fisher’s exact test. For all tests and results, a p-value less than 0.05 was considered to denote a statistically significant difference. The strength of association with primary and secondary endpoints was computed using conditional logistic regression adjusted on the study arm. Associations were reported as odds ratios with 95% confidence intervals. Data curation and statistical analyses were performed using Review Manager 5.3.
From a total of 323 patients with cUTIs, 128 were excluded: 16 received antibiotics for less than 72 h, 59 carried Gram-positive organisms in their urine, 18 tested positive for fungi, and 35 had been repeatedly exposed to the studied antibiotics (Figure 1). Of the 195 patients eligible for this study, 110 constituted the PTZ group and 85 formed the meropenem group (Table 1). Between these two groups, 48 patients (25%) suffered from chronic liver diseases, and 32 (16%) took at least 20 mg of oral corticosteroids daily.
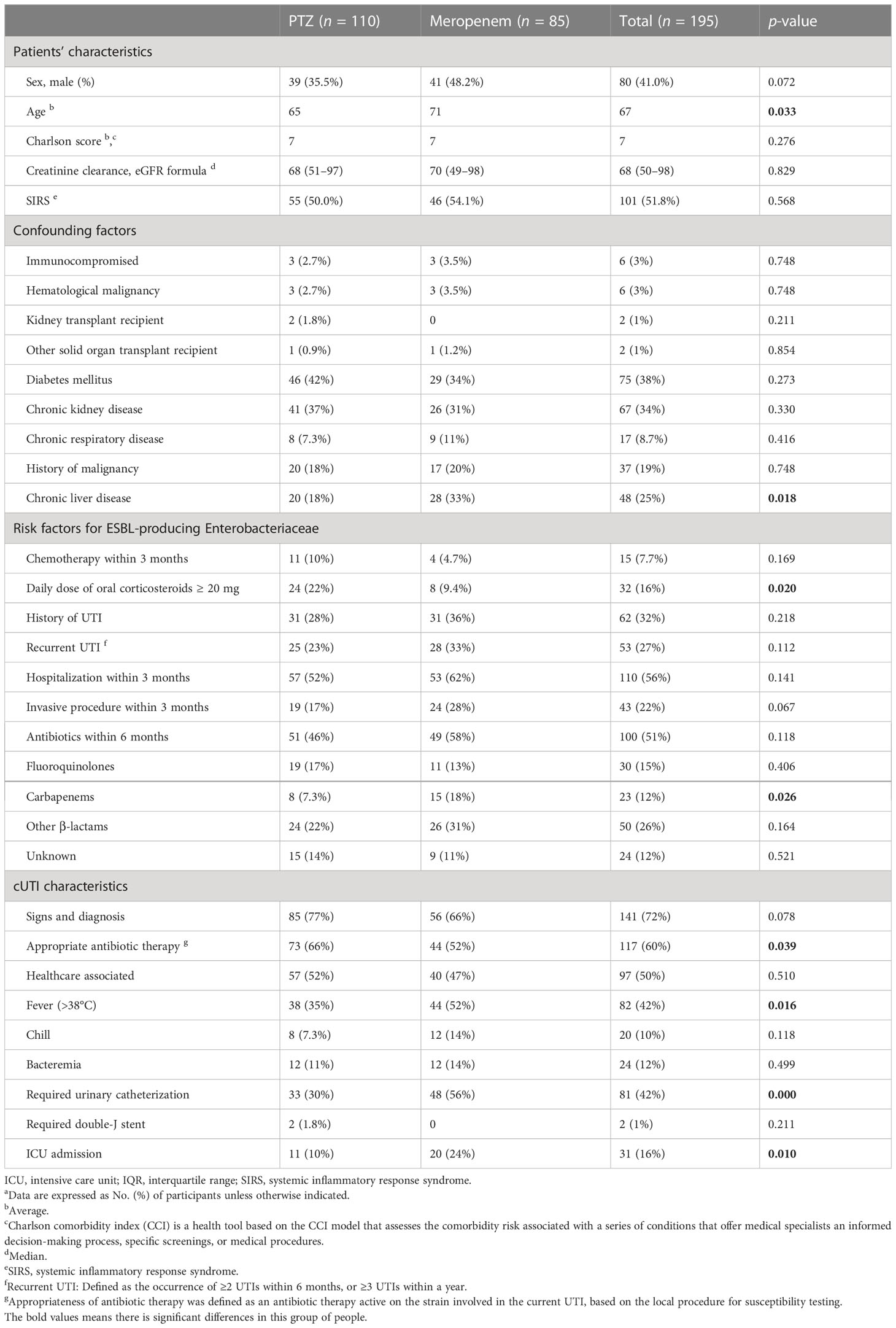
Table 1 Patients’ and cUTI characteristics at baseline a.
Overall, the baseline characteristics of the two groups were similar (Table 1), although the average age and the proportion of patients with chronic liver diseases were both higher in the meropenem group (71 years vs. 65 years, 33% vs. 18%, respectively). In addition, the proportion of patients who received ≥ 20 mg of oral corticosteroids was 22% and 9.4% in the PTZ and meropenem groups, respectively. Before hospitalization and treatment, a larger proportion of patients in the PTZ group were receiving appropriate antibiotic treatments (66% vs. 52%). Moreover, 18% of patients took carbapenem antibiotics in the meropenem group, compared with 7.3% in the PTZ group. More patients from the meropenem group suffered from fever, urethral catheterization, and intensive care unit treatment (52% vs. 35%, 56% vs. 30%, and 24% vs. 10%, respectively). The etiological agents causing cUTIs were similarly distributed between the two groups (Table 2): a total of 82 patients (42%) were infected with E. coli, 35 (18%) with K. pneumoniae, and 11 with Pseudomonas aeruginosa (5.6%).
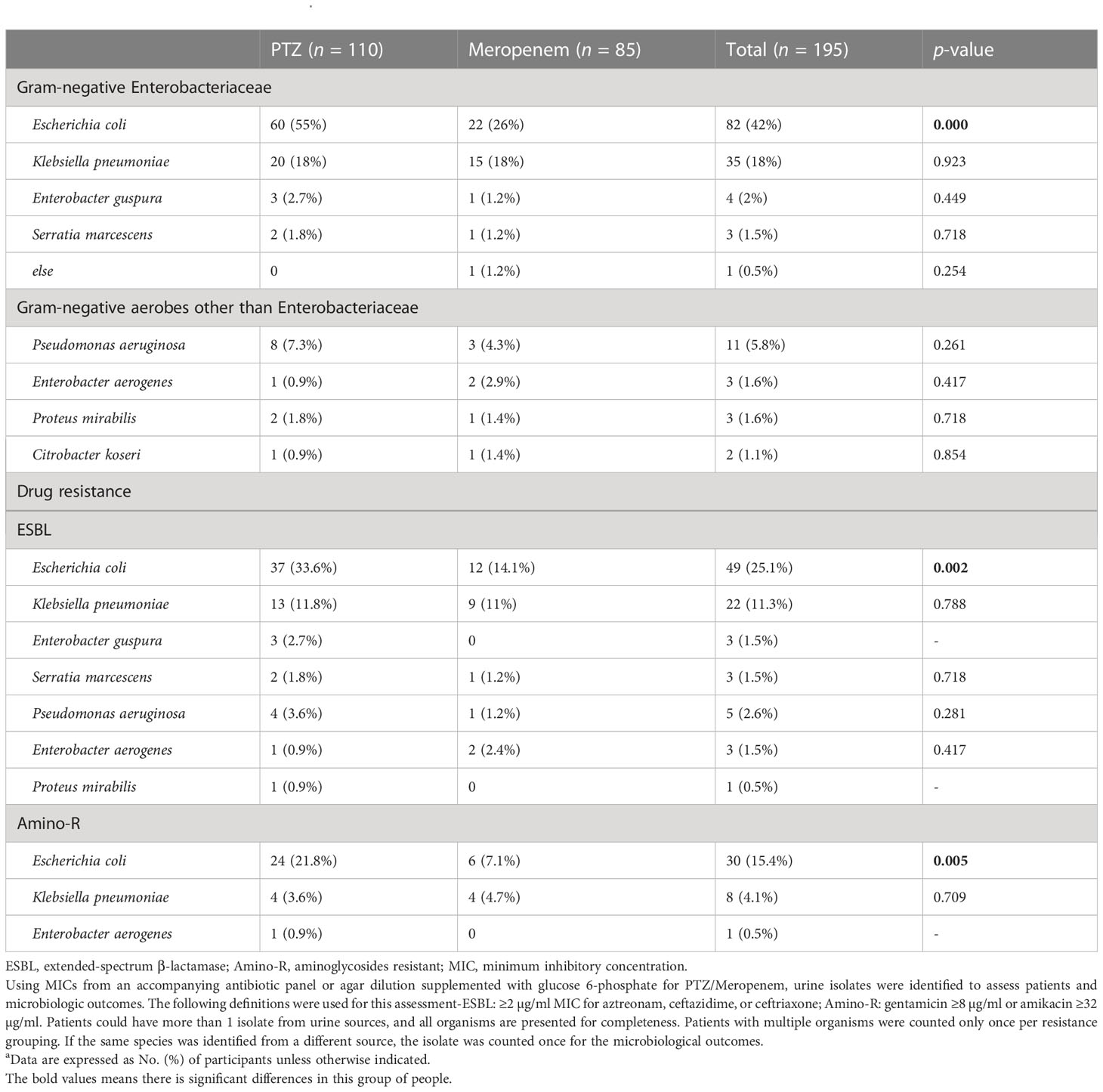
Table 2 Microbiological characteristics a.
E. coli and K. pneumoniae were considered the most common infection-causing pathogens in this study cohort. For the treatment of E. coli infections, 55% (60/110) of the patients received PTZ while 26% (22/85) chose meropenem. In contrast, 18% of the patients from both the groups (20/110, 15/85) chose the respective drugs to treat K. pneumoniae infections. ESBL-producing and aminoglycosides-resistant (amino-R) E. coli were identified as the most resistant pathogens. To combat the former, 33.6% (37/110) and 14.1% (12/85) of the patients used PTZ and meropenem, respectively. For the latter, 21.8% (24/110) and 7.1% (6/110) of the patients chose PTZ and meropenem, respectively. Overall, a higher proportion of patients in the PTZ group tested positive for three different types of Enterobacteriaceae in their urine: E. coli, ESBL-producing E. coli, and amino-R E. coli (p = 0.000, 0.002, and 0.005, respectively) (Table 2).
The overall duration of antibiotic therapy (9 vs. 6), the effective duration of antibiotic therapy (8 vs. 6), the length of hospital stay (22 vs. 16), and all-cause mortality (18.8% vs. 7.3%) were all higher in the meropenem group than in the PTZ group (Table 3). However, no significant difference was observed between the two groups in the relapse of cUTIs, rehospitalization, and loss to follow-up.
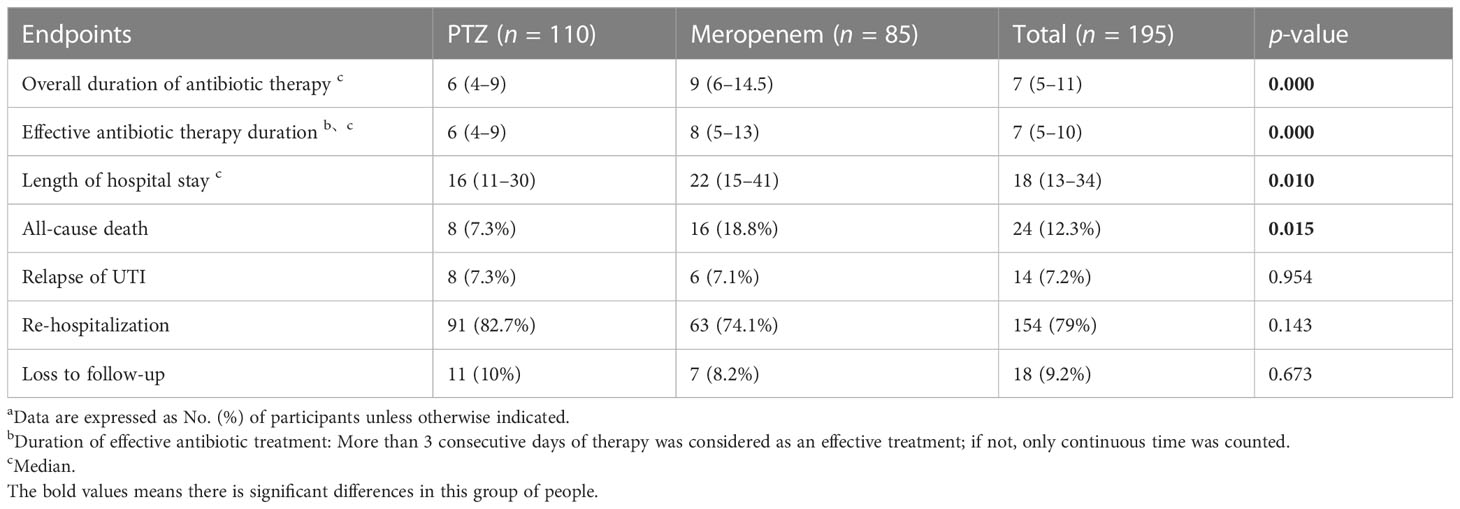
Table 3 Several occurrences of safety endpoints a.
In terms of clinical cure and microbial eradication, the clinical success of both the groups was comparable. The overall success in the two groups was 80% and 78.8% (treatment difference, 1.2%; 95% confidence interval, 10.3–12.6) (Table 4, Figure 2).
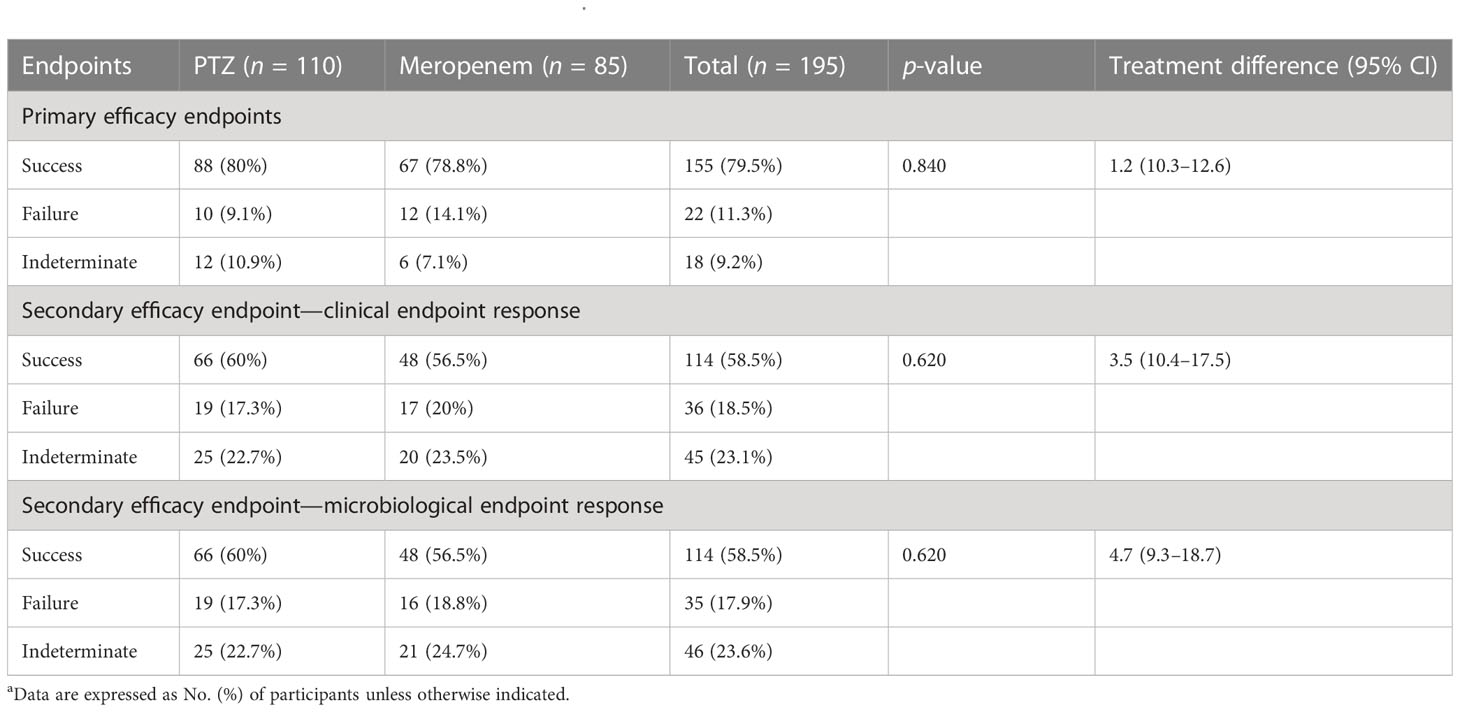
Table 4 Occurrence of primary and secondary endpoints a.
Subgroup analyses focused on ESBL-producing and amino-R E. coli were conducted. Although clinical cure rates were high and did not differ significantly between the two groups, clinical and microbiological endpoint success was more significant in the PTZ group than in the meropenem group (Tables 5–7).
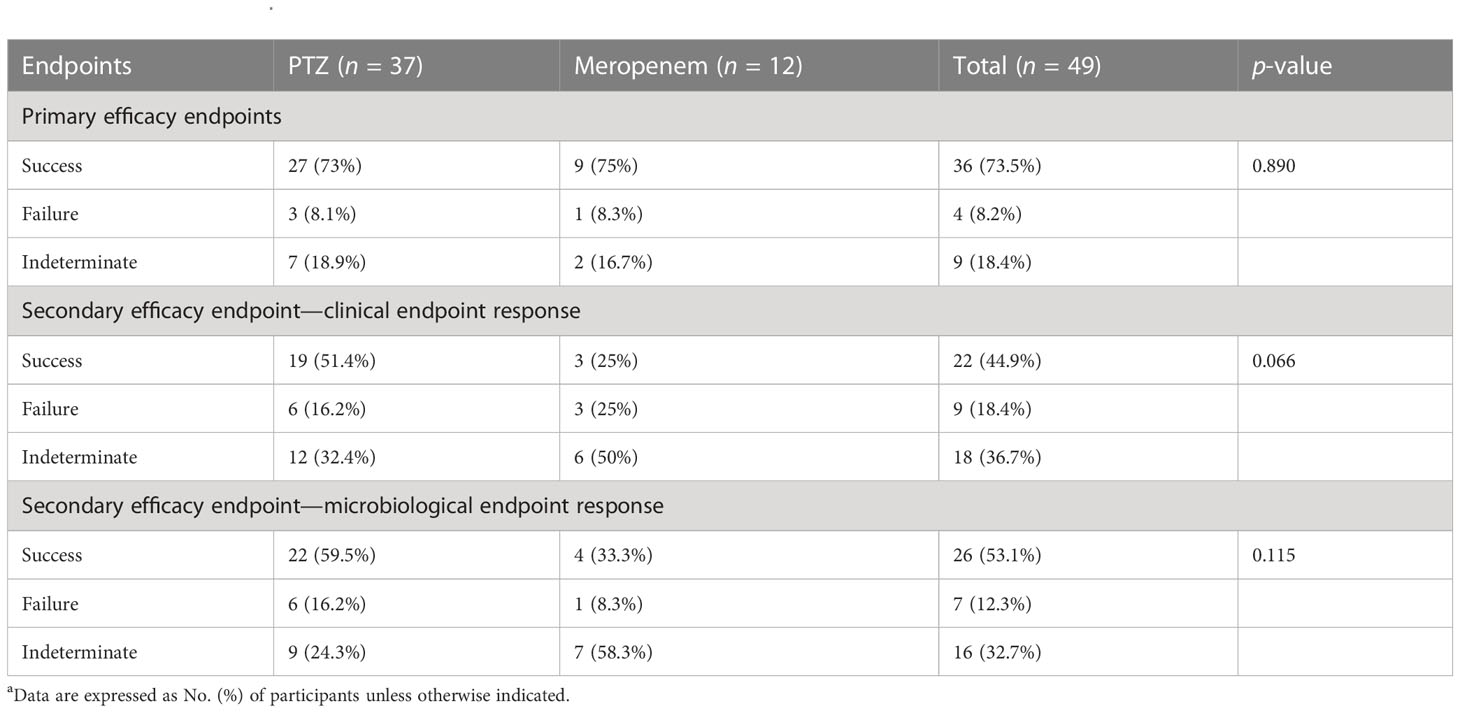
Table 5 Clinical and microbiologic outcomes among patients with baseline ESBL-producing Escherichia coli characteristics (occurrence of primary and secondary endpoints) a.
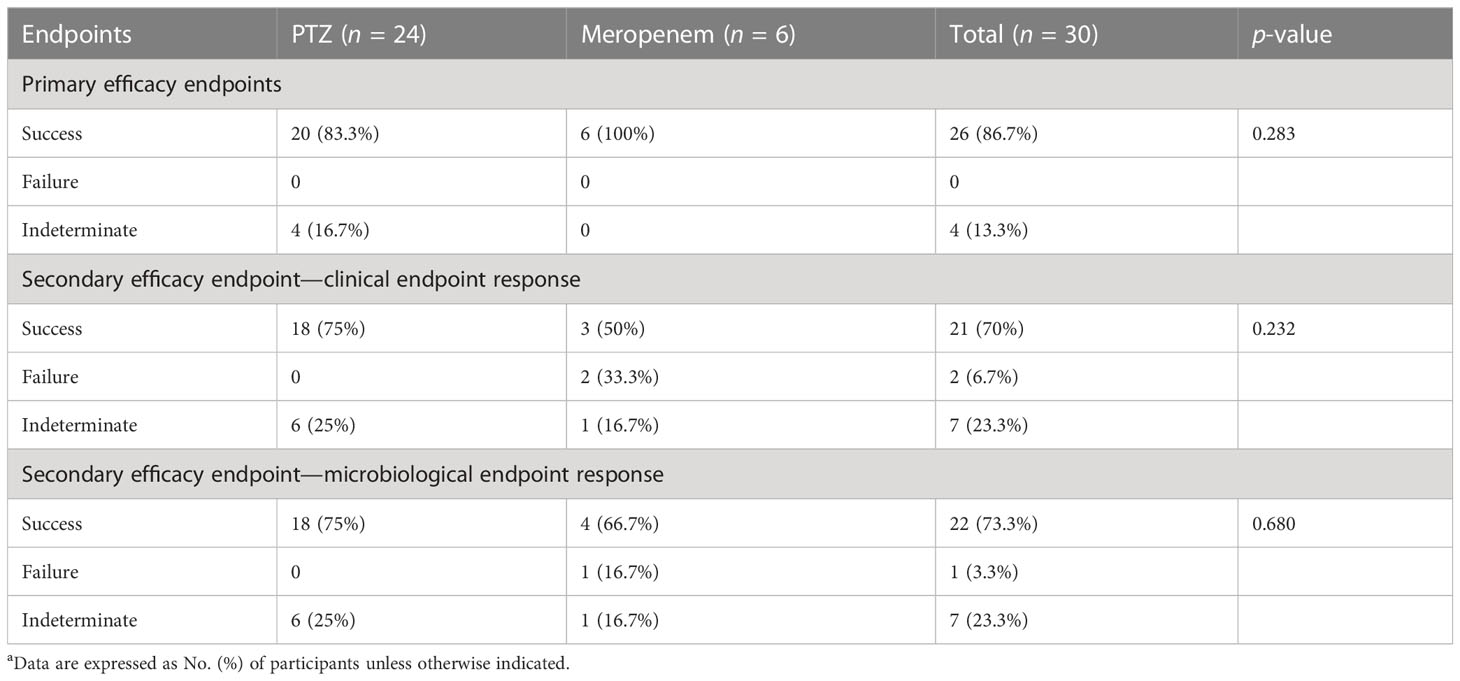
Table 6 Clinical and microbiologic outcomes among patients with baseline amino-R Escherichia coli characteristics (occurrence of primary and secondary endpoints)a.
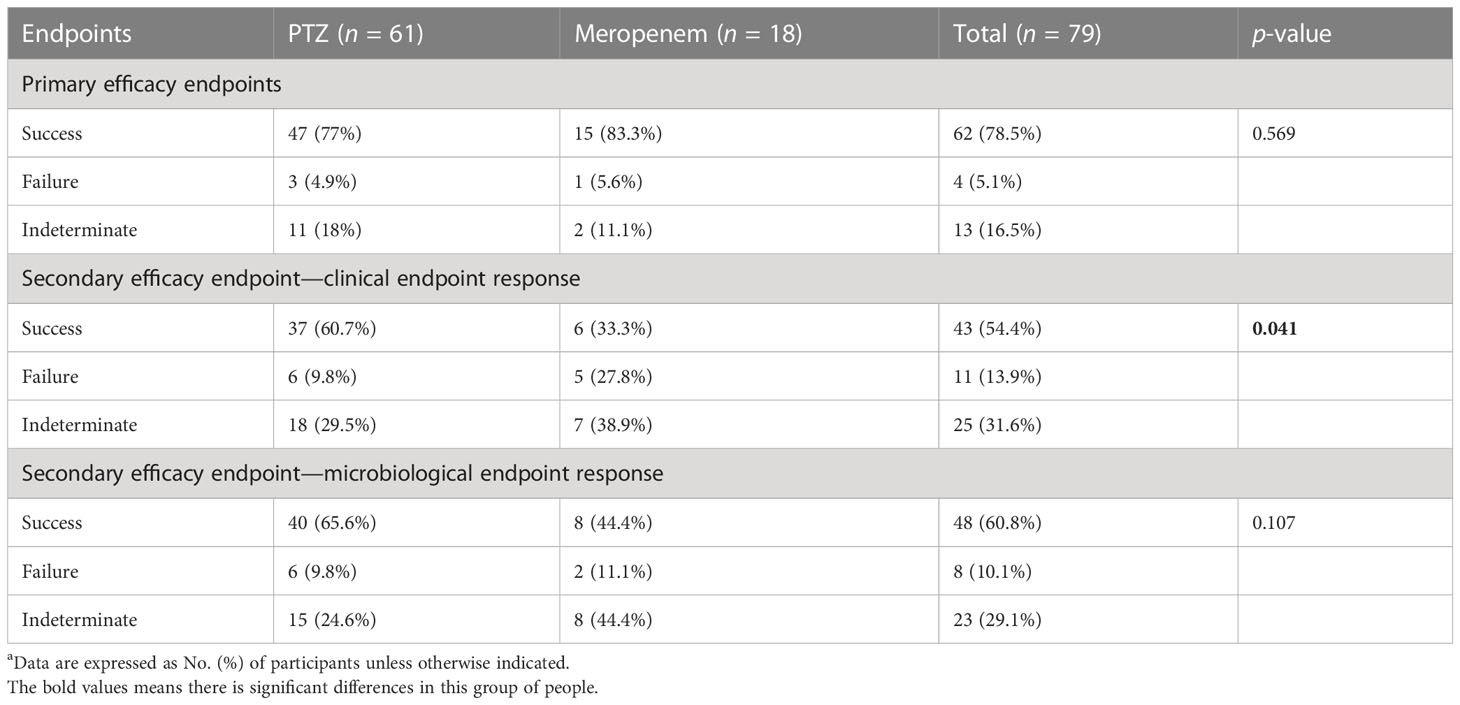
Table 7 Clinical and microbiologic outcomes among patients with baseline ESBL-producing and amino-R Escherichia coli characteristics (occurrence of primary and secondary endpoints)a.
The incidence of adverse events was significantly lower in the PTZ group (4.5% vs. 15.3%, p = 0.01). In the meropenem group, the most common adverse event was abnormal liver function, afflicting 5.9% of the patients. In the PTZ group, the most common adverse event was anaphylaxis, affecting 2.7% of the patients (Table 8).
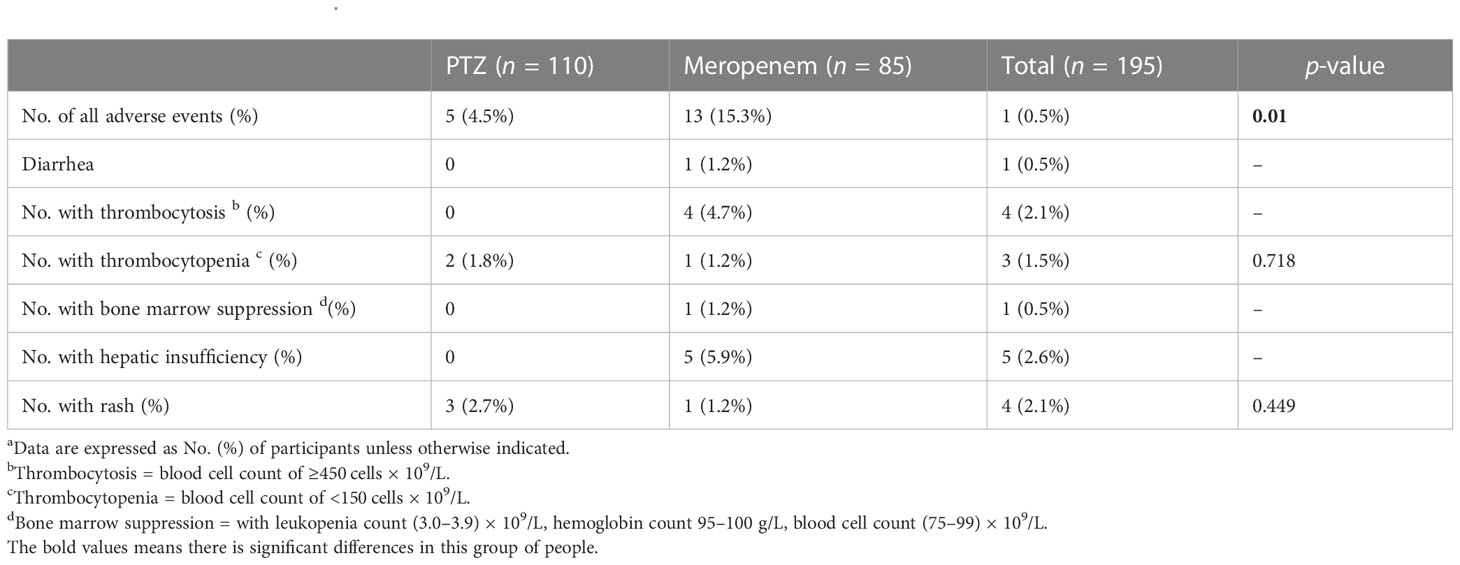
Table 8 Adverse patient events a.
According to the FDA (US Food & Drug Administration, 2018) and the Association of the British Pharmaceutical Industry, real-world evidence is defined as the analysis of real-world clinical data to evaluate what is happening in normal clinical practice. Following appeals from many agencies, studies focusing on real-world evidence have received much attention. Different from randomized clinical trials, clinical studies in the real-world setting deal with larger populations with complex situations, physical functions, and variable treatment combinations. Such studies represent the general population, provide deeper insights into clinical practice, and help discover real-life problems (Kim et al., 2018).
However, clinical retrospective studies in the real world suffer from some unavoidable drawbacks. The healthcare practitioners directly decide the drugs to be administered after analyzing multi-indicators. Changing the medicines for finishing the clinical study without considering clinical ethics is illegal.
This study aimed to compare the efficacy and safety of PTZ and meropenem in treating cUTIs in the real world. In this monocentric and case–control study, patients diagnosed with cUTIs received antibiotic therapy, and the clinical cure rate was high (79.5%) at the end of the treatment. The clinical characteristics of patients who took PTZ and meropenem were similar, and their clinical response rates were 80% and 78.8%, respectively. Furthermore, the clinical response did not differ significantly among patients with several health conditions, including immunocompromised patients and those with hematological malignancies, kidney and other solid organ transplantations, diabetes, chronic kidney disease, chronic respiratory disease, and other malignancies.
The higher clinical response of PTZ (80%) was not related to the microbiological or clinical characteristics of the patients. PTZ was used at a standard dosage of 4.5 g q8h, or adjusted according to creatinine clearance for pathogenic infections with a minimum inhibitory concentration ≤ 8 mg/L. In this study, the most common pathogens were E. coli (42%) and K. pneumoniae (18%), and one-third of the patients were diagnosed with diabetes mellitus or chronic kidney diseases.
The clinical efficacy and safety of PTZ and meropenem were similar in treating cUTIs. However, the increased use of carbapenems may lead to the selection of carbapenem resistance in Gram-negative bacilli and the spread of carbapenemase-encoding antibiotic resistance genes (Mendes et al., 2018). To avoid serious outcomes and achieve appropriate prescriptions, many studies have compared carbapenems with other antibacterials (Chen et al., 2018; Sternbach et al., 2018; Zhong et al., 2018; Ezure et al., 2022). In these meta-analyses, carbapenems present similar clinical efficacies and possibly better microbiological responses than other antibacterial agents. When using antibiotics, the possibility and consequences of resistance and related health economics must be considered.
The efficacy of drugs varies with the patients’ physical conditions, complications, and history of taking other drugs. We, as clinical practitioners, found that there is a lack of therapeutic advice on drugs that share similar indications or targeting the same pathogens, to help physicians deliver more effective, precise, and cost-effective treatments to different patients. More clinical real-world data need to be collected and analyzed to construct detailed guidelines for drug administration. These studies should be designed based on the standard format of medical records between multiple centers and should overcome limitations as much as possible.
This study had several limitations. Firstly, this monocenter and retrospective study was limited by an insufficient sample size and a small number of case events, which led to restricted statistical power to manage confounding factors. Secondly, the extensive use of PTZ in the first line resulted in a population selection and biased measurement of point estimates. Only randomization can prevent such biases. Lastly, other antibiotics in clinical practice may influence the clinical efficacy and incidence of adverse effects.
PTZ is an effective, safe, and definite treatment option for cUTIs due to the presence of ESBL-producing and amino-R Enterobacteriaceae. Its efficacy is consistent with that of immunocompromised patients, including those with hematological malignancies, kidney and other solid organ transplant recipients, diabetes mellitus, chronic kidney disease, chronic respiratory disease, and a history of malignancies. However, the risk of emerging resistance stresses the need for close monitoring. A randomized comparison with carbapenems is warranted.
The data analyzed in this study is subject to the following licenses/restrictions: Hospital Personal Information. Requests to access these datasets should be directed to 1358359@qq.com.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of the First Affiliated Hospital of the Air Force Medical University. The patients/participants provided written informed consent to participate in the study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
J-WW designed the study and approved the final version of the manuscript. WZ, C-YY, T-TF, YG, and S-RL performed the study. WZ and C-YY analyzed the data and wrote the manuscript. S-SC, BC, M-YL, B-YF, BJ, LiW, FC, JC, and LeW were involved in conceptualization, methodology, and analysis of the study. BC and T-TF provided statistical analysis assistance and helped to revise the manuscript. All authors have read and approved the final manuscript.
This work was supported by the National Natural Science Foundation of China (No. 72074218).
We are grateful to Li-Hui Duo, Yu Zong, Mei-Xiang You, and Zhen-Hua Lei for technical assistance.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ESBL, extended-spectrum β-lactamase; cUTIs, complicated urinary tract infections; BLBLIs, β-lactam/β-lactamase inhibitors; AEs, adverse events; IQR, interquartile range; OR, odds ratio; CI, confidence intervals; ICU, intensive care unit; SIRS, systemic inflammatory response syndrome; CCI, Charlson comorbidity index; Amino-R, aminoglycosides resistant; MIC, minimum inhibitory concentration; RCTs, randomized clinical trials.
Armstrong, T., Fenn, S. J., Hardie, K. R. (2021). JMM profile: Carbapenems: a broad-spectrum antibiotic. J. Med. Microbiol. 70 (12). doi: 10.1099/jmm.0.001462
US Food & Drug Administration (2018). Framework for FDA’s real-world evidence program Available at: https://www.fda.gov/media/120060/download.
Baldwin, C. M., Lyseng-Williamson, K. A., Keam, S. J. (2008). Meropenem: a review of its use in the treatment of serious bacterial infections. Drugs 68 (6), 803–838. doi: 10.2165/00003495-200868060-00006
Bush, K., Bradford, P. A. (2016). β-lactams and β-lactamase inhibitors: An overview. Cold Spring Harb. Perspect. Med. 6 (8). doi: 10.1101/cshperspect.a025247
Chatterjee, S., Chakraborty, D. S., Choudhury, S., Lahiry, S. (2021). Cefiderocol- a new antimicrobial for complicated urinary tract infection (CUTI) caused by carbapenem resistant enterobacteriaceae (CRE). Curr. Drug Res. Rev. 14 (1), 20–23. doi: 10.2174/2589977513666211206100749
Chen, M., Zhang, M., Huang, P., Lin, Q., Sun, C., Zeng, H., et al. (2018). Novel β-lactam/β-lactamase inhibitors versus alternative antibiotics for the treatment of complicated intra-abdominal infection and complicated urinary tract infection: A meta-analysis of randomized controlled trials. Expert Rev. Anti Infect. Ther. 16 (2), 111–120. doi: 10.1080/14787210.2018.1429912
CLSI (2021). Performance standards for antimicrobial susceptibility testing, M100. 31st ed (Wayne, PA: Clin Lab Stand Institute).
Delory, T., Gravier, S., Le Pluart, D., Gaube, G., Simeon, S., Davido, B., et al. (2021). Temocillin versus carbapenems for urinary tract infection due to ESBL-producing enterobacteriaceae: A multicenter matched case-control study. Int. J. Antimicrob. Agents. 58 (1), 106361. doi: 10.1016/j.ijantimicag.2021.106361
Drawz, S. M., Bonomo, R. A. (2010). Three decades of beta-lactamase inhibitors. Clin. Microbiol. Rev. 23 (1), 160–201. doi: 10.1128/CMR.00037-09
Ezure, Y., Rico, V., Paterson, D. L., Hall, L., Harris, P. N. A., Soriano, A., et al. (2022). Efficacy and safety of carbapenems vs new antibiotics for treatment of adult patients with complicated urinary tract infections: A systematic review and meta-analysis. Open Forum Infect. Dis. 9 (5), ofaa480. doi: 10.1093/ofid/ofaa480
Food and Drug Administration. (2018). Complicated urinary tract infections: Developing drugs for treatment guidance for industry.
Geerlings, S. E., Van Nieuwkoop, C., Van Haarst, E., van Buren, M., Knotterus, B. J., Stobberingh, E. E., et al. (2013). SWAB guidelines for antimicrobial therapy of complicated urinary tract infections in adults (The Netherlands Institute for Health Services Research: SWAB Guidel).
Jean, S.-S., Lu, M.-C., Ho, M.-W., Ko, W.-C., Hsueh, P.-R. (2022). Non-susceptibilities to antibiotics against important gram-negative bacteria, and imipenem-relebactam, meropenem-vaborbactam against carbapenem non-susceptible enterobacterales and pseudomonas aeruginosa isolates implicated in complicated intra-abdominal. Int. J. Antimicrob. Agents, 106521. doi: 10.1016/j.ijantimicag.2022.106521
Kim, H.-S., Lee, S., Kim, J. H. (2018). Real-world evidence versus randomized controlled trial: Clinical research based on electronic medical records. J. Korean Med. Sci. 33 (34), e213. doi: 10.3346/jkms.2018.33.e213
Kongnakorn, T., Wagenlehner, F., Falcone, M., Tichy, E., Di Virgilio, R., Baillon-Plot, N., et al. (2019). Cost-effectiveness analysis of ceftazidime/avibactam compared to imipenem as empirical treatment for complicated urinary tract infections. Int. J. Antimicrob. Agents. 54 (5), 633–641. doi: 10.1016/j.ijantimicag.2019.06.008
López Montesinos, I., Gómez-Zorrilla, S., Palacios-Baena, Z. R., Prim, N., Echeverria-Esnal, D., Gracia, M. P., et al. (2022). Aminoglycoside or polymyxin monotherapy for treating complicated urinary tract infections caused by extensively drug-resistant pseudomonas aeruginosa: A propensity score-adjusted and matched cohort study. Infect. Dis. Ther. 11 (1), 335–350. doi: 10.1007/s40121-021-00570-z
Melekos, M. D., Naber, K. G. (2000). Complicated urinary tract infections. Int. J. Antimicrob. Agents. 15 (4), 247–256. doi: 10.1016/S0924-8579(00)00168-0
Mendes, R. E., Castanheira, M., Woosley, L. N., Stone, G. G., Bradford, P. A., Flamm, R. K. (2018). Molecular β-lactamase characterization of gram-negative pathogens recovered from patients enrolled in the ceftazidime-avibactam phase 3 trials (RECAPTURE 1 and 2) for complicated urinary tract infections: Efficacies analysed against susceptible and resis. Int. J. Antimicrob. Agents. 52 (2), 287–292. doi: 10.1016/j.ijantimicag.2018.04.001
Sternbach, N., Leibovici Weissman, Y., Avni, T., Yahav, D. (2018). Efficacy and safety of ceftazidime/avibactam: a systematic review and meta-analysis. J. Antimicrob. Chemother. 73 (8), 2021–2029. doi: 10.1093/jac/dky124
Syed, Y. Y. (2021). Cefiderocol: A review in serious gram-negative bacterial infections. Drugs. 81 (13), 1559–1571. doi: 10.1007/s40265-021-01580-4
Vallejo-Torres, L., Pujol, M., Shaw, E., Wiegand, I., Vigo, J. M., Stoddart, M., et al. (2018). Cost of hospitalised patients due to complicated urinary tract infections: A retrospective observational study in countries with high prevalence of multidrug-resistant gram-negative bacteria: The COMBACTE-MAGNET, RESCUING study. BMJ Open 8 (4), e020251. doi: 10.1136/bmjopen-2017-020251
US Food & Drug Administration. (2018). Framework for FDA’s real-world evidence program. Available at: https://www.fda.gov/media/120060/download.
Wald-Dickler, N., Lee, T. C., Tangpraphaphorn, S., Butler-Wu, S. M., Wang, N., Degener, T., et al. (2022). Fosfomycin vs ertapenem for outpatient treatment of complicated urinary tract infections: A multicenter, retrospective cohort study. Open Forum Infect. Dis. 9 (1), ofab620. doi: 10.1093/ofid/ofab620
Wiseman, L. R., Wagstaff, A. J., Brogden, R. N., Bryson, H. M. (1995). Meropenem. a review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs. 50 (1), 73–101. doi: 10.2165/00003495-199550010-00007
Zhanel, G. G., Wiebe, R., Dilay, L., Thomson, K., Rubinstein, E., Hoban, D. J., et al. (2007). Comparative review of the carbapenems. Drugs. 67 (7), 1027–1052. doi: 10.2165/00003495-200767070-00006
Zhong, H., Zhao, X. Y., Zhang, Z. L., Gu, Z. C., Zhang, C., Gao, Y., et al. (2018). Evaluation of the efficacy and safety of ceftazidime/avibactam in the treatment of gram-negative bacterial infections: A systematic review and meta-analysis. Int. J. Antimicrob. Agents. 52 (4), 443–450. doi: 10.1016/j.ijantimicag.2018.07.004
Zilberberg, M. D., Nathanson, B. H., Sulham, K., Shorr, A. F. (2021). Multiple antimicrobial resistance and outcomes among hospitalized patients with complicated urinary tract infections in the US, 2013-2018: A retrospective cohort study. BMC Infect. Dis. 21 (1), 159. doi: 10.1186/s12879-021-05842-0
Keywords: complicated urinary tract infections, piperacillin-tazobactam, ESBL, antibiotic treatment, meropenem
Citation: Zhang W, Yan C-Y, Li S-R, Fan T-T, Cao S-S, Cui B, Li M-Y, Fan B-Y, Ji B, Wang L, Cui F, Cui J, Wang L, Guan Y and Wang J-W (2023) Efficacy and safety of piperacillin–tazobactam compared with meropenem in treating complicated urinary tract infections including acute pyelonephritis due to extended-spectrum β-lactamase-producing Enterobacteriaceae. Front. Cell. Infect. Microbiol. 13:1093842. doi: 10.3389/fcimb.2023.1093842
Received: 18 November 2022; Accepted: 14 March 2023;
Published: 03 May 2023.
Edited by:
Ying Zhang, Zhejiang University, ChinaReviewed by:
Timothy Kudinha, Charles Sturt University, AustraliaCopyright © 2023 Zhang, Yan, Li, Fan, Cao, Cui, Li, Fan, Ji, Wang, Cui, Cui, Wang, Guan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Guan, MjMzOTU2OTFAcXEuY29t; Jing-Wen Wang, d2FuZ2ppbmd3ZW44MDIxQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.