
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Cell. Infect. Microbiol. , 08 February 2023
Sec. Antibiotic Resistance and New Antimicrobial drugs
Volume 13 - 2023 | https://doi.org/10.3389/fcimb.2023.1075255
This article is part of the Research Topic Antimicrobial Resistance and One Health: From Culture to Genomics View all 8 articles
The occurrence and transmission of carbapenemase-producing-Enterobacterales (CPE) on a global scale has become a major issue. Clinical reports are rarely providing information on the genomic and plasmid features of carbapenem-resistant Serratia marcescens. Our objective was to investigate the resistance and transmission dynamics of two carbapenem-resistant S. marcescens that are resistant to carbapenem and have caused bacteremia in China. Blood specimens were taken from two individuals with bacteremia. Multiplex PCR was employed to identify genes that code for carbapenemase. Antimicrobial susceptibility tests and plasmid analysis were conducted on S. marcescens isolates SM768 and SM4145. The genome of SM768 and SM4145 were completely sequenced using NovaSeq 6000-PE150 and PacBio RS II platforms. Antimicrobial resistance genes (ARGs) were predicted using the ResFinder tool. S1 nuclease pulsed-field gel electrophoresis (S1-PFGE) and southern blotting were employed to analyze plasmids. Two S. marcescens that produced KPC-2 were identified from bloodstream infections. The antimicrobial susceptibility testing demonstrated that both of the isolates had a resistance to various antibiotics. The whole-genome sequence (WGS) and plasmid analysis revealed the presence of blaKPC-2-bearing IncR plasmids and multiple plasmid-borne antimicrobial resistance genes in the isolates. Our comparative plasmid analysis suggested that the two IncR plasmids identified in this study could be derived from a common ancestor. Our findings revealed the emergence of blaKPC-2-bearing IncR plasmid in China, which could be a hindrance to the transmission of KPC-2-producing S. marcescens in clinical settings.
Serratia marcescens is a type of Gram-negative bacteria belonging to the order Enterobacterales, family Enterobacteriaceae (Park et al., 2007). S. marcescens is frequently encountered in a range of habitats, such as moist areas, prosthetic material, and within the respiratory tract and gastrointestinal flora (Casolari et al., 2013; Rosenthal et al., 2020). Its capacity to cause opportunistic infections in medical facilities is enhanced by these factors. This opportunistic pathogen frequently responsible for hospital-acquired infections, including urinary tract infections (UTIs), respiratory tract infections, conjunctivitis, tear duct infections, and keratitis (Elsherbiny et al., 2018; Konecka et al., 2019; Millan-Lou et al., 2022; Prado et al., 2022; Anderson et al., 2022). S. marcescens is a significant hospital-acquired pathogen, and its invasive infections have resulted in high mortality rates (Yeo et al., 2020; do Prado et al., 2021; Bes et al., 2021).
The emergence of acquired antimicrobial resistance (AMR) in S. marcescens has become a major health risk to the general public (Prado et al., 2022). There are now several reports of multi-drug resistant (MDR) S. marcescens outbreaks carrying either extended-spectrum β-lactamases (ESBLs) or carbapenemases, which confer extended spectrum cephalosporin and carbapenem resistance, respectively (Elsherbiny et al., 2018; Phan et al., 2018; Firmo et al., 2020; Bes et al., 2021; Tamma et al., 2021; Loqman et al., 2021).
In hospital-acquired infections, the prevalence rate of carbapenem-resistant S. marcescens has increased recently (Prado et al., 2022). The production of carbapenemase is the primary cause for the rapid and widespread proliferation of S. marcescens drug resistance (Firmo et al., 2020; Jimenez et al., 2020). Despite its clinical relevance and the increasing concerns about AMR, little is known about the epidemiology and genetic diversity of carbapenem-resistant S. marcescens within healthcare institutions.
Here, we present two cases of bloodstream infections caused by S. marcescens isolates that produce KPC-2. We further sequenced two isolates to characterize their genetic diversity, assess for evidence of nosocomial transmission, and determine the genetic context of acquired AMR determinants. These results help the timely implementation of infection control measures.
Identification of the bacterial species was performed by MALDI-TOF MS and 16S rRNA sequence analysis, as described previously (Wang et al., 2019). The isolates were further subjected to PCR to detect the carbapenemase gene as previously described (Zheng et al., 2015).
Minimum inhibitory concentrations (MICs) of ten antimicrobial agents (imipenem, meropenem, piperacillin-tazobactam, cefotaxime, ceftazidime, aztreonam, ciprofloxacin, gentamicin, amikacin, tobramycin) were determined by agar dilution method, except for colistin and tigecycline, which were determined by the broth microdilution method. Susceptibility was interpreted according to CLSI (2022) and European Committee on Antimicrobial Susceptibility Testing (EUCAST 2022) guidelines (https://www.eucast.org/). Escherichia coli ATCC25922 was used as quality control (Wang et al., 2019).
Genomic DNA was extracted using QIAamp DNA Mini Kit (Qiagen, Hilden, Germany) and sequenced using NovaSeq 6000-PE150 (Illumina, San Diego, CA, USA) and PacBio RS II platform (Pacific Biosciences, California, USA). De novo assembly was generated by using SPAdes 3.11.0 (Hu et al., 2011). Plasmid replicons and antimicrobial resistance genes were predicted through the PlasmidFinder (https://bitbucket.org/genomicepidemiology/plasmidfinder/src/master/) and ResFinder website (https://cge.cbs.dtu.dk/services/ResFinder/), respectively. The genetic environment surrounding blaKPC-2 was annotated using RAST3 and Easyfig 2.2.3 (Chi et al., 2019). The complete genome sequences of S. marcescens SM768 and SM4145 were uploaded to NCBI with the following project number: PRJNA841282.
SM768 and SM4145 were tested by S1 nuclease pulsed-field gel electrophoresis (S1-PFGE) and southern blotting to validate the location of blaKPC-2. Whole-cell DNA of two isolates was extracted and embedded in gold agarose gel plugs (SeaKem® Gold Agarose, Lonza, Atlanta, GA, USA). The plugs were digested with S1 nuclease (TaKaRa, Dalian, China) and separated by PFGE. Plasmids obtained by PFGE were transferred horizontally to a nylon membrane (Millipore, USA) and hybridized with digoxin-labelled blaKPC-2-specific probes obtained and the Dig High Prime DNA Labeling and Detection Starter Kit (Roche Diagnostics) (Zheng et al., 2019). The Salmonella enterica serotype Braenderup strain H9812 was used as the DNA marker.
Transfer of blaKPC-2 was investigated using conjugation for isolates SM768 and SM4145. The recipient strains for this experiment were E. coli J53 (azide-resistant) and E. coli EC600 (rifampicin-resistant), while SM768 and SM4145 were selected as donor strains (Wang et al., 2019).
Samples of blood from a 36-year-old female and a 49-year-old male yielded two isolates of S. marcescens, SM768 and SM4145, both of which were found to be resistant to carbapenems. PCR test for carbapenemase-encoding genes confirmed that both isolates carried the blaKPC-2 gene.
Isolates SM768 and SM4145 showed resistance to imipenem, piperacillin-tazobactam, cefotaxime, ceftazidime, and aztreonam (Table S1). In addition, two isolates were susceptible to amikacin and tobramycin. It is expected that SM768 and SM4145 both exhibited high-level resistance to colistin, as Serratia has an intrinsic resistance to this antibiotic. Whole-genome sequencing showed that SM4145 carried multiple antimicrobial resistance genes (ARGs). These include ESBLs resistance gene blaCTX-M-14, the plasmid-encoded quinolone resistance gene qnrS1, and the aminoglycoside resistance gene aac6’-Ic.
S1-PFGE and Southern blot revealed that SM768 isolate carried a ~105 kb plasmid harbouring blaKPC-2 gene. In contrast, SM4145 isolate harbouring a ~70 kb plasmid encoding blaKPC-2 gene (Figure 1). Furthermore, the blaKPC-2 genes could be transferred from SM768 into the recipient E. coli strains via conjugation, confirmed by PCR. In contrast, SM4145 was negative for the transferability test (data not shown).
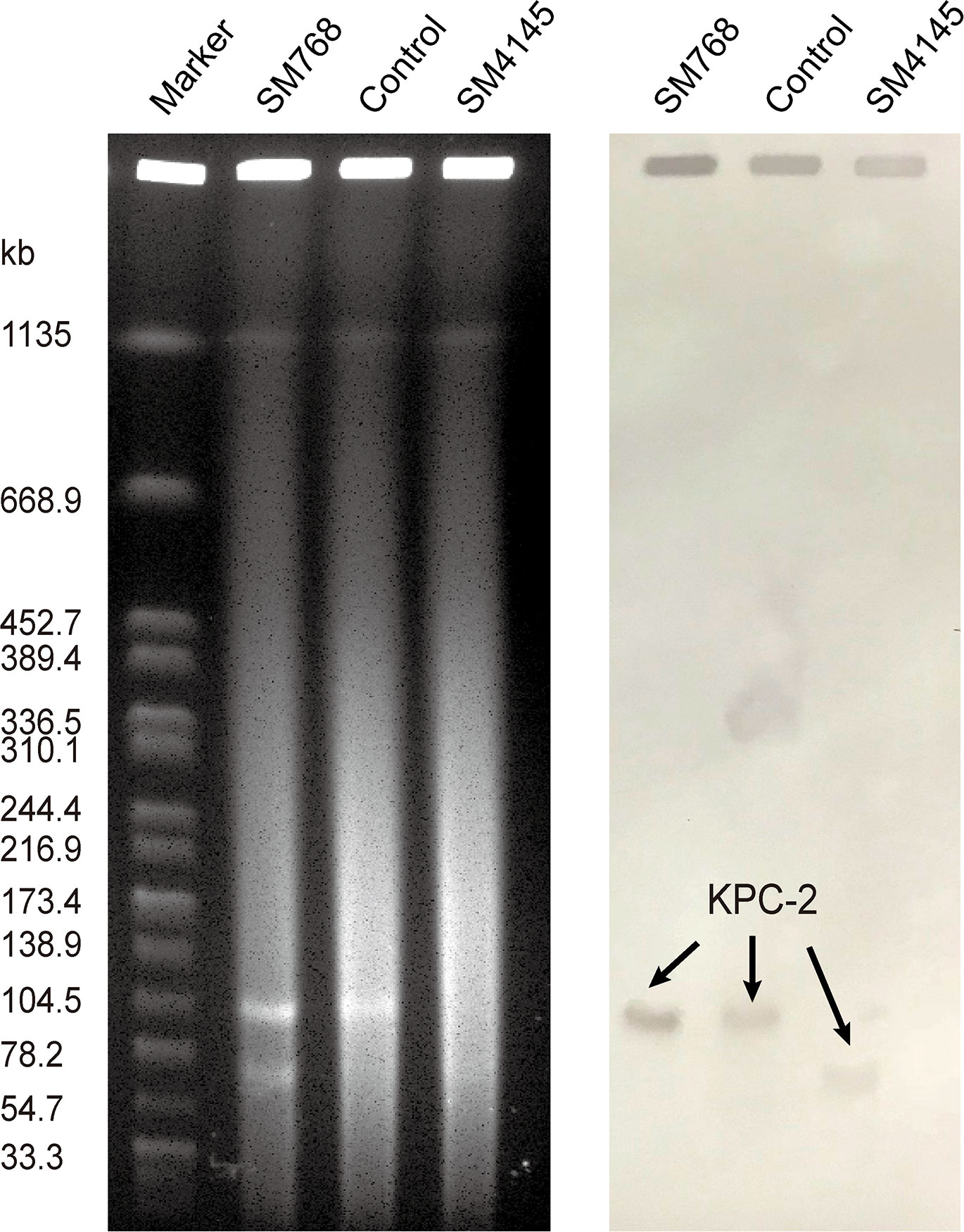
Figure 1 S1-PFGE analysis of KPC-2-producing S. marcescens isolates and southern hybridization using a blaKPC-2 probe. Lane M, molecular weight marker Salmonella Braenderup H9812; Lane SM768, isolate S. marcescens SM768; Lane control, KPC-2-producing Klebsiella pneumoniae isolate 1095 served as the control; Lane SM4145, isolate S. marcescens SM4145.
The WGS results demonstrated that two blaKPC-2-encoding plasmids, pSM768-KPC-2, were IncR-type plasmids with 107,813 bp, and pSM4145-KPC-2 was also an IncR-type plasmid with the size of 69,528 bp, respectively (Figure 2). Plasmid pSM768-KPC-2 contained a collection of genes involved in segregation, fertility inhibition, stability, and conjugal transfer of the plasmid (parA, parM, finO, umuCD, and tra regulon), which together constructed the essential backbone of pSM768-KPC-2. In contrast, the tra regulon was absent in plasmid pSM4145-KPC-2.
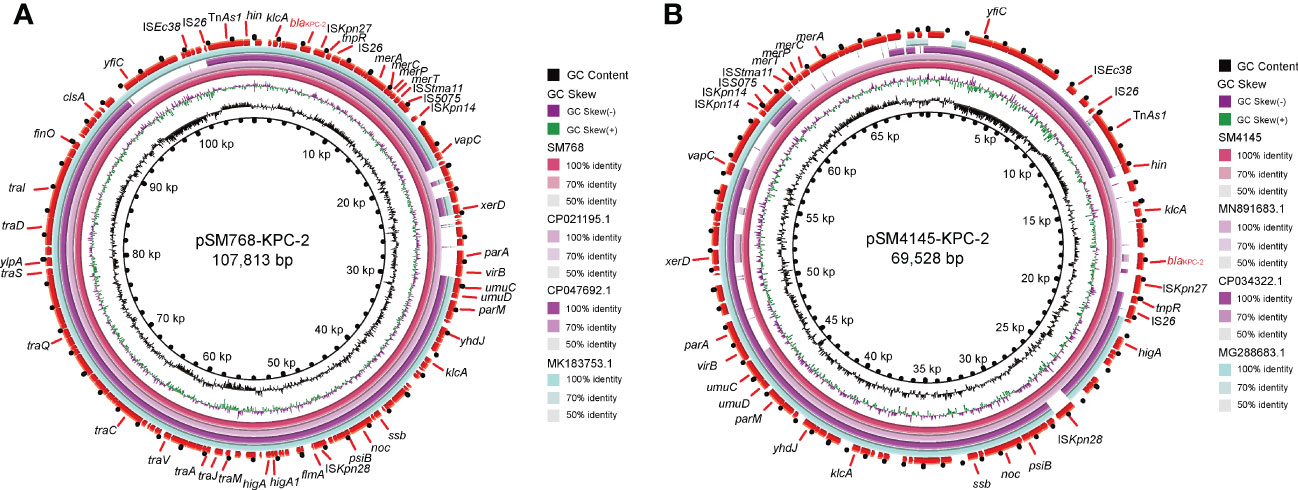
Figure 2 Complete sequences of two blaKPC-2-harbouring IncR plasmids were recovered in this work. (A) Alignment of plasmid sequence of pSM768-KPC-2 with other blaKPC-2-bearing plasmids pH17-2 (CP021195), pC110-KPC (CP047692), and p17-15-KPC (MK183753). (B) Comparison of pSM4145-KPC-2 with plasmids pK033_1 (CP034322), p314013-KPC (MN891683), and pE20-NR (MG288683). Circles inside to outside denote the GC content, GC screw, and the ORFs in both DNA strands. Block arrows represent coding sequences and indicate the direction of transcription. blaKPC-2 gene is highlighted in red. Arrow size is proportional to gene length. The circular image of multiple plasmids comparisons was generated with the BLAST Ring Image Generator.
The blaKPC-2 gene surrounding pSM768-KPC-2 and pSM4145-KPC-2 showed the same genetic background. The blaKPC-2 gene was flanked by an ISKpn27, tnpR, and IS26 elements downstream and a klcA gene upstream (Figure 3). Comparative plasmid analysis revealed that pSM768-KPC-2 shares a high identity with pSM4145-KPC-2, except a ~38 kb sequence was inserted in pSM768-KPC-2 plasmid. This indicated that pSM768-KPC-2 and pSM4145-KPC-2 might be derived from a common ancestor. In addition, in silico analysis also found that pSM768-KPC-2 exhibits high relatedness with a ~107 kb KPC-2-carrying IncR plasmid pH17-2 (CP021195) from Escherichia coli and a ~150 kb plasmid pK033_1 (CP034322) from K. pneunomiae.
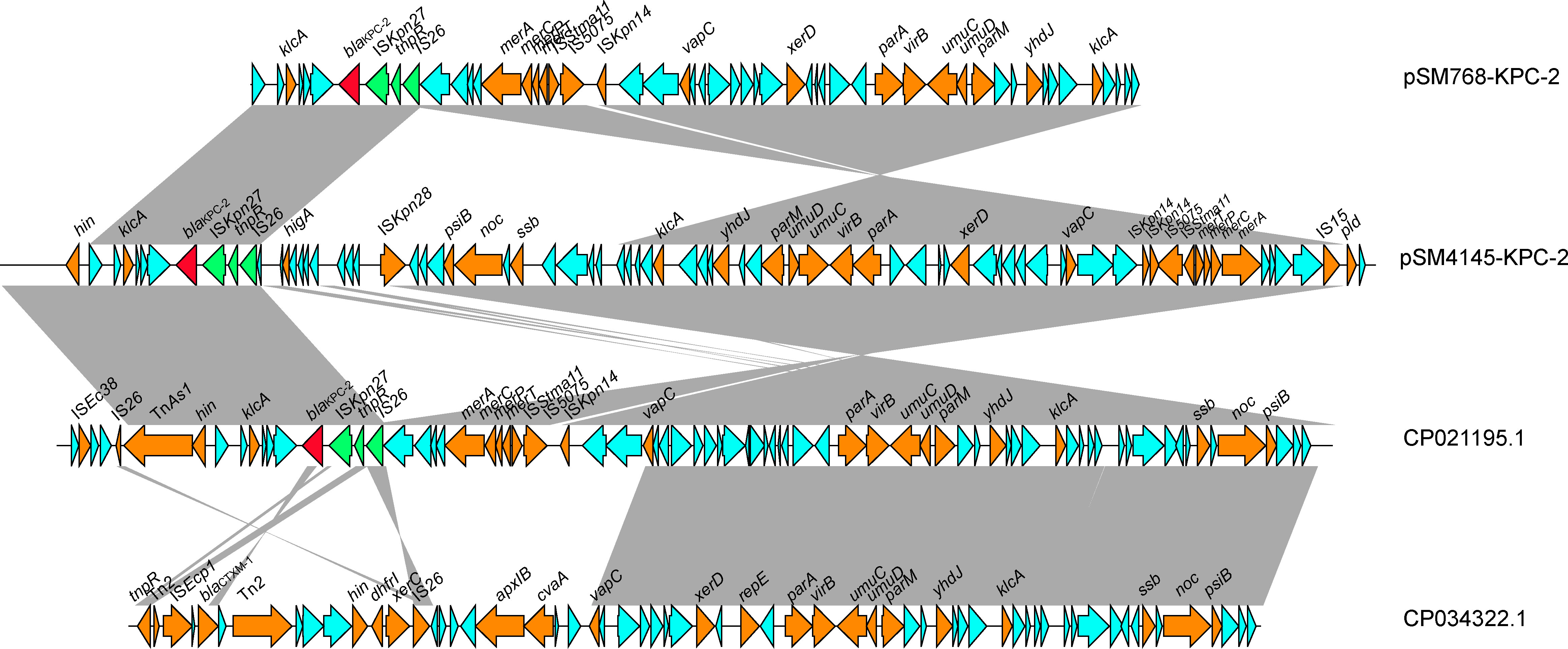
Figure 3 Colinear genome alignment of pSM768-KPC-2, pSM4145-KPC-2, pH17-2, and pK033_1. Arrows represent the direction of transcription. Red open reading frames (ORFs) indicate KPC-2.
Serratia marcescens is a well-known opportunistic pathogen that is often seen to be responsible for infections in intensive care, surgical and dialysis facilities (Ferreira et al., 2020). Antimicrobial resistance of S. marcescens has not been widely explored in China (Lin et al., 2016; Su et al., 2017; Huang et al., 2021; Zhong et al., 2022; Hou et al., 2022). Herein, we found two carbapenem-resistant S. marcescens from patients with bloodstream infections in China, and the blaKPC-2 gene, which is native to the area, is likely to be disseminated through the transmission of IncR plasmids.
The global spread of the resistance of Enterobacterales to many antibiotics, seriously affecting the treatment of infections, has become a major public issue (Hu et al., 2018; Dong et al., 2018; Dong et al., 2018; Zheng et al., 2020). The major plasmid types carrying blaKPC-2 published included IncFII, IncF, IncP-6, IncN, ColRNAI, and IncI2 (Xu et al., 2018; Hu et al., 2019; Xiaoliang et al., 2019; Abril et al., 2021; Peng et al., 2022). To the best of our knowledge, this is the first time that blaKPC-2 genes have been found to be carried by IncR plasmid in S. marcescens isolates from bacteremia.
It is now acknowledged that S. marcescens has the potential to cause disease in vulnerable individuals. Although S. marcescens displayed relatively low virulence, the emergence of carbapenem-resistant S. marcescens has become a real threat to patients (Zhang et al., 2007). In China, the identification of KPC-2-producing S. marcescens was first described in 2007 (Zhang et al., 2007). Since then, related reports mainly originated from eastern China (Miao et al., 2018; Li et al., 2018; Xie et al., 2020; Xu et al., 2020), which indicates that regional dissemination of such pathogens might be due to the blaKPC-2-harbouring plasmids.
The global distribution of CTX-M variants showed that the CTX-M-1 group (especially CTX-M-15) was the dominant genotype in most regions, while the CTX-M-9 group (especially CTX-M-14) has been reported to be the most common genotypes in China in recent years (Zhang et al., 2016; Shen et al., 2017; Huang et al., 2018; Feng et al., 2019; Yuan et al., 2019; Zheng et al., 2021). A previous study found that CTX-M-14 was the most common gene type in S. marcescens isolates in China (Yang et al., 2012). Our data is consistent with these findings.
Previous studies have indicated that S. marcescens often presents carbapenem resistance caused by plasmids with differing replicon types that contain the blaKPC gene (Xu et al., 2020). In this work, we identified and characterized two IncR plasmids from S. marcescens. We further employed NovaSeq and PacBio RS II platforms to clarify the genetic context of IncR plasmids, which are acutely lacking for blaKPC-bearing IncR plasmids. However, the small size of blaKPC-harbouring IncR plasmids identified in this study is the limitation merit mentioning. A further comprehensive investigation is warranted on the spread of blaKPC-harbouring IncR plasmid in other Enterobacterales.
To summarize, we characterized KPC-2-producing S. marcescens isolates from bloodstream infections in terms of their antimicrobial susceptibility, antimicrobial resistance genes, and plasmid transfer mechanism. Both blaKPC genes were located on the IncR plasmid, which presents a potential challenge for interrupting the transmission of KPC-2-producing S. marcescens in clinical settings. Our insights may have implications in the clinical care and monitoring of KPC-2-producing bacteria.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
AX and JJ designed and executed the study, performed the results analyses, and drafted the manuscript. JJ, LH, LZ, and YS handled the molecular experiments. WC and HX established and performed the whole genome sequencing. All authors contributed to the article and approved the submitted version.
This work was supported by the Major Medical Science and Technology Projects in Henan Province (SBGJ202001006).
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2023.1075255/full#supplementary-material
Abril, D., Vergara, E., Palacios, D., Leal, A. L., Marquez-Ortiz, R. A., Madronero, J., et al. (2021). Within patient genetic diversity of blaKPC harboring klebsiella pneumoniae in a Colombian hospital and identification of a new NTEKPC platform. Sci. Rep. 11 (1), 21409. doi: 10.1038/s41598-021-00887-2
Anderson, M. T., Himpsl, S. D., Mitchell, L. A., Kingsley, L. G., Snider, E. P., Mobley, H. L. T. (2022). Identification of distinct capsule types associated with serratia marcescens infection isolates. PloS Pathog. 18 (3), e1010423. doi: 10.1371/journal.ppat.1010423
Bes, T., Nagano, D., Martins, R., Marchi, A. P., Perdigao-Neto, L., Higashino, H., et al. (2021). Bloodstream infections caused by klebsiella pneumoniae and serratia marcescens isolates co-harboring NDM-1 and KPC-2. Ann. Clin. Microbiol. Antimicrob. 20 (1), 57. doi: 10.1186/s12941-021-00464-5
Casolari, C., Pecorari, M., Della Casa, E., Cattani, S., Venturelli, C., Fabio, G., et al. (2013). Serratia marcescens in a neonatal intensive care unit: Two long-term multiclone outbreaks in a 10-year observational study. New Microbiol. 36 (4), 373–383.
Chi, X., Berglund, B., Zou, H., Zheng, B., Borjesson, S., Ji, X., et al. (2019). Characterization of clinically relevant strains of extended-spectrum beta-Lactamase-Producing klebsiella pneumoniae occurring in environmental sources in a rural area of China by using whole-genome sequencing. Front. Microbiol. 10, 211. doi: 10.3389/fmicb.2019.00211
CLSI. (2022). M100–performance standards for antimicrobial susceptibility testing, 32nd edition. Ed. Wayne, P. A. (Malvern, PA: Clinical and Laboratory Standards Institute).
Dong, N., Lin, D., Zhang, R., Chan, E. W., Chen, S. (2018). Carriage of blaKPC-2 by a virulence plasmid in hypervirulent klebsiella pneumoniae. J. Antimicrob. Chemother. 73 (12), 3317–3321. doi: 10.1093/jac/dky358
Dong, N., Yang, X., Zhang, R., Chan, E. W., Chen, S. (2018). Tracking microevolution events among ST11 carbapenemase-producing hypervirulent klebsiella pneumoniae outbreak strains. Emerg. Microbes Infect. 7 (1), 146. doi: 10.1038/s41426-018-0146-6
do Prado, G. V. B., Mendes, E. T., Martins, R. C. R., Perdigao-Neto, L. V., Freire, M. P., Spadao, F., et al. (2021). Carbapenem-resistant serratia marcescens bloodstream infection in hematopoietic stem cell transplantation patients: Will it be the next challenge? Transpl Infect. Dis. 23 (4), e13630 doi: 10.1111/tid.13630.
Elsherbiny, N. M., Ali, I. M., Hassanein, K. M., Ahmed, M. T. (2018). Extended-spectrum beta-lactamase (ESBL)-producing serratia marcescens causing healthcare-associated infections in assiut university hospitals, Egypt. J. Glob Antimicrob. Resist. 13, 96–97. doi: 10.1016/j.jgar.2018.03.011
Feng, C., Wen, P., Xu, H., Chi, X., Li, S., Yu, X., et al. (2019). Emergence and comparative genomics analysis of extended-Spectrum-beta-Lactamase-Producing escherichia coli carrying mcr-1 in fennec fox imported from Sudan to China. mSphere 4 (6), e00732-19. doi: 10.1128/mSphere.00732-19
Ferreira, R. L., Rezende, G. S., Damas, M. S. F., Oliveira-Silva, M., Pitondo-Silva, A., Brito, M. C. A., et al. (2020). Characterization of KPC-producing serratia marcescens in an intensive care unit of a Brazilian tertiary hospital. Front. Microbiol. 11, 956. doi: 10.3389/fmicb.2020.00956
Firmo, E. F., Beltrao, E. M. B., Silva, F., Alves, L. C., Brayner, F. A., Veras, D. L., et al. (2020). Association of blaNDM-1 with blaKPC-2 and aminoglycoside-modifying enzyme genes among klebsiella pneumoniae, Proteus mirabilis and serratia marcescens clinical isolates in Brazil. J. Glob Antimicrob. Resist. 21, 255–261. doi: 10.1016/j.jgar.2019.08.026
Hou, J., Mao, D., Zhang, Y., Huang, R., Li, L., Wang, X., et al. (2022). Long-term spatiotemporal variation of antimicrobial resistance genes within the serratia marcescens population and transmission of s. marcescens revealed by public whole-genome datasets. J. Hazard Mater 423 (Pt B), 127220. doi: 10.1016/j.jhazmat.2021.127220
Huang, X., Shen, S., Shi, Q., Ding, L., Wu, S., Han, R., et al. (2021). First report of bla (IMP-4) and bla (SRT-2) coproducing serratia marcescens clinical isolate in China. Front. Microbiol. 12, 743312. doi: 10.3389/fmicb.2021.743312
Huang, C., Zheng, B., Yu, W., Niu, T., Xiao, T., Zhang, J., et al. (2018). Antibacterial effect evaluation of moxalactam against extended-spectrum beta-lactamase-producing escherichia coli and klebsiella pneumoniae with in vitro pharmacokinetics/pharmacodynamics simulation. Infect. Drug Resist. 11, 103–112. doi: 10.2147/IDR.S150431
Hu, X., Xu, H., Shang, Y., Guo, L., Song, L., Zhang, H., et al. (2018). First genome sequence of a blaKPC-2-carrying citrobacter koseri isolate collected from a patient with diarrhoea. J. Glob Antimicrob. Resist. 15, 166–168. doi: 10.1016/j.jgar.2018.09.016
Hu, X., Yu, X., Shang, Y., Xu, H., Guo, L., Liang, Y., et al. (2019). Emergence and characterization of a novel IncP-6 plasmid harboring bla KPC-2 and qnrS2 genes in aeromonas taiwanensis isolates. Front. Microbiol. 10, 2132. doi: 10.3389/fmicb.2019.02132
Hu, Y., Zhang, W., Liang, H., Liu, L., Peng, G., Pan, Y., et al. (2011). Whole-genome sequence of a multidrug-resistant clinical isolate of acinetobacter lwoffii. J. Bacteriol. 193 (19), 5549–5550. doi: 10.1128/JB.05617-11
Jimenez, A., Abbo, L. M., Martinez, O., Shukla, B., Sposato, K., Iovleva, A., et al. (2020). KPC-3-Producing serratia marcescens outbreak between acute and long-term care facilities, Florida, USA. Emerg. Infect. Dis. 26 (11), 2746–2750. doi: 10.3201/eid2611.202203
Konecka, E., Mokracka, J., Krzyminska, S., Kaznowski, A. (2019). Evaluation of the pathogenic potential of insecticidal serratia marcescens strains to humans. Pol. J. Microbiol. 68 (2), 185–191. doi: 10.33073/pjm-2019-018
Li, B., Feng, J., Zhan, Z., Yin, Z., Jiang, Q., Wei, P., et al. (2018). Dissemination of KPC-2-Encoding IncX6 plasmids among multiple enterobacteriaceae species in a single Chinese hospital. Front. Microbiol. 9, 478. doi: 10.3389/fmicb.2018.00478
Lin, X., Hu, Q., Zhang, R., Hu, Y., Xu, X., Lv, H. (2016). Emergence of serratia marcescens isolates possessing carbapenem-hydrolysing beta-lactamase KPC-2 from China. J. Hosp Infect. 94 (1), 65–67. doi: 10.1016/j.jhin.2016.04.006
Loqman, S., Soraa, N., Diene, S. M., Rolain, J. M. (2021). Dissemination of carbapenemases (OXA-48, NDM and VIM) producing enterobacteriaceae isolated from the Mohamed VI university hospital in marrakech, Morocco. Antibiotics (Basel) 10 (5), 492. doi: 10.3390/antibiotics10050492
Miao, M., Wen, H., Xu, P., Niu, S., Lv, J., Xie, X., et al. (2018). Genetic diversity of carbapenem-resistant enterobacteriaceae (CRE) clinical isolates from a tertiary hospital in Eastern China. Front. Microbiol. 9, 3341. doi: 10.3389/fmicb.2018.03341
Millan-Lou, M. I., Lopez, C., Bueno, J., Perez-Laguna, V., Lapresta, C., Fuertes, M. E., et al. (2022). Successful control of serratia marcescens outbreak in a neonatal unit of a tertiary-care hospital in Spain. Enferm Infecc Microbiol. Clin. 40 (5), 248–254. doi: 10.1016/j.eimc.2021.05.003
Park, Y. J., Yu, J. K., Lee, S., Oh, E. J., Woo, G. J. (2007). Prevalence and diversity of qnr alleles in AmpC-producing enterobacter cloacae, enterobacter aerogenes, citrobacter freundii and serratia marcescens: A multicentre study from Korea. J. Antimicrob. Chemother. 60 (4), 868–871. doi: 10.1093/jac/dkm266
Peng, C., Feng, D. H., Zhan, Y., Wang, Q., Chen, D. Q., Xu, Z., et al. (2022). Molecular epidemiology, microbial virulence, and resistance of carbapenem-resistant enterobacterales isolates in a teaching hospital in guangzhou, China. Microb. Drug Resist 28(6), 698-709. doi: 10.1089/mdr.2021.0156
Phan, H. T. T., Stoesser, N., Maciuca, I. E., Toma, F., Szekely, E., Flonta, M., et al. (2018). Illumina short-read and MinION long-read WGS to characterize the molecular epidemiology of an NDM-1 serratia marcescens outbreak in Romania. J. Antimicrob. Chemother. 73 (3), 672–679. doi: 10.1093/jac/dkx456
Prado, G., Mendes, E. T., Martins, R. C. R., Perdigao-Neto, L. V., Freire, M. P., Marchi, A. P., et al. (2022). Phenotypic and genotypic characteristics of a carbapenem-resistant serratia marcescens cohort and outbreak: Describing an opportunistic pathogen. Int. J. Antimicrob. Agents 59 (1), 106463. doi: 10.1016/j.ijantimicag.2021.106463
Rosenthal, V. D., Belkebir, S., Zand, F., Afeef, M., Tanzi, V. L., Al-Abdely, H. M., et al. (2020). Six-year multicenter study on short-term peripheral venous catheters-related bloodstream infection rates in 246 intensive units of 83 hospitals in 52 cities of 14 countries of middle East: Bahrain, Egypt, Iran, Jordan, kingdom of Saudi Arabia, Kuwait, Lebanon, Morocco, Pakistan, Palestine, Sudan, Tunisia, Turkey, and united Arab Emirates-international nosocomial infection control consortium (INICC) findings. J. Infect. Public Health 13 (8), 1134–1141. doi: 10.1016/j.jiph.2020.03.012
Shen, P., Fan, J., Guo, L., Li, J., Li, A., Zhang, J., et al. (2017). Genome sequence of shigella flexneri strain SP1, a diarrheal isolate that encodes an extended-spectrum beta-lactamase (ESBL). Ann. Clin. Microbiol. Antimicrob. 16 (1), 37. doi: 10.1186/s12941-017-0212-2
Su, W. Q., Zhu, Y. Q., Deng, N. M., Li, L. (2017). Imipenem-resistance in serratia marcescens is mediated by plasmid expression of KPC-2. Eur. Rev. Med. Pharmacol. Sci. 21 (7), 1690–1694.
Tamma, P. D., Smith, T. T., Adebayo, A., Karaba, S. M., Jacobs, E., Wakefield, T., et al. (2021). Prevalence of bla CTX-m genes in gram-negative bloodstream isolates across 66 hospitals in the united states. J. Clin. Microbiol. 59 (6), e00127-21. doi: 10.1128/JCM.00127-21
Wang, S., Xu, L., Chi, X., Li, Y., Kou, Z., Hou, P., et al. (2019). Emergence of NDM-1- and CTX-M-3-Producing raoultella ornithinolytica in human gut microbiota. Front. Microbiol. 10, 2678. doi: 10.3389/fmicb.2019.02678
Xiaoliang, W., Huiming, H., Chunlei, C., Beiwen, Z. (2019). Genomic characterisation of a colistin-resistant klebsiella pneumoniae ST11 strain co-producing KPC-2, FloR, CTX-M-55, SHV-12, FosA and RmtB causing a lethal infection. J. Glob Antimicrob. Resist. 19, 78–80. doi: 10.1016/j.jgar.2019.08.023
Xie, S., Fu, S., Li, M., Guo, Z., Zhu, X., Ren, J., et al. (2020). Microbiological characteristics of carbapenem-resistant enterobacteriaceae clinical isolates collected from county hospitals. Infect. Drug Resist. 13, 1163–1169. doi: 10.2147/IDR.S248147
Xu, Q., Fu, Y., Zhao, F., Jiang, Y., Yu, Y. (2020). Molecular characterization of carbapenem-resistant serratia marcescens clinical isolates in a tertiary hospital in hangzhou, China. Infect. Drug Resist. 13, 999–1008. doi: 10.2147/IDR.S243197
Xu, H., Wang, X., Yu, X., Zhang, J., Guo, L., Huang, C., et al. (2018). First detection and genomics analysis of KPC-2-producing citrobacter isolates from river sediments. Environ. pollut. 235, 931–937. doi: 10.1016/j.envpol.2017.12.084
Yang, H. F., Cheng, J., Hu, L. F., Ye, Y., Li, J. B. (2012). Plasmid-mediated quinolone resistance in extended-spectrum-beta-lactamase- and AmpC beta-lactamase-producing serratia marcescens in China. Antimicrob. Agents Chemother. 56 (8), 4529–4531. doi: 10.1128/AAC.00493-12
Yeo, K. T., Octavia, S., Lim, K., Lin, C., Lin, R., Thoon, K. C., et al. (2020). Serratia marcescens in the neonatal intensive care unit: A cluster investigation using molecular methods. J. Infect. Public Health 13 (7), 1006–1011. doi: 10.1016/j.jiph.2019.12.003
Yuan, S., Wu, G., Zheng, B. (2019). Complete genome sequence of an IMP-8, CTX-M-14, CTX-M-3 and QnrS1 co-producing enterobacter asburiae isolate from a patient with wound infection. J. Glob Antimicrob. Resist. 18, 52–54. doi: 10.1016/j.jgar.2019.05.029
Zhang, R., Zhou, H. W., Cai, J. C., Chen, G. X. (2007). Plasmid-mediated carbapenem-hydrolysing beta-lactamase KPC-2 in carbapenem-resistant serratia marcescens isolates from hangzhou, China. J. Antimicrob. Chemother. 59 (3), 574–576. doi: 10.1093/jac/dkl541
Zhang, J., Zhou, K., Zheng, B., Zhao, L., Shen, P., Ji, J., et al. (2016). High prevalence of ESBL-producing klebsiella pneumoniae causing community-onset infections in China. Front. Microbiol. 7, 1830. doi: 10.3389/fmicb.2016.01830
Zheng, B., Feng, C., Xu, H., Yu, X., Guo, L., Jiang, X., et al. (2019). Detection and characterization of ESBL-producing escherichia coli expressing mcr-1 from dairy cows in China. J. Antimicrob. Chemother. 74 (2), 321–325. doi: 10.1093/jac/dky446
Zheng, B., Xu, H., Lv, T., Guo, L., Xiao, Y., Huang, C., et al. (2020). Stool samples of acute diarrhea inpatients as a reservoir of ST11 hypervirulent KPC-2-Producing klebsiella pneumoniae. mSystems 5 (3), e00498-20. doi: 10.1128/mSystems.00498-20
Zheng, W., Yue, M., Zhang, J., Ruan, Z. (2021). Coexistence of two bla(CTX-M-14) genes in a bla(NDM-5)-carrying multidrug-resistant escherichia coli strain recovered from a bloodstream infection in China. J. Glob Antimicrob. Resist. 26, 11–14. doi: 10.1016/j.jgar.2021.05.002
Zheng, B., Zhang, J., Ji, J., Fang, Y., Shen, P., Ying, C., et al. (2015). Emergence of raoultella ornithinolytica coproducing IMP-4 and KPC-2 carbapenemases in China. Antimicrob Agents Chemother 59 (11), 7086–7089. doi: 10.1128/AAC.01363-15
Keywords: carbapenem-resistant S. marcescens, KPC-2, bacteremia, CTX-M-14, IncR
Citation: Jia J, Huang L, Zhang L, Sheng Y, Chu W, Xu H and Xu A (2023) Genomic characterization of two carbapenem-resistant Serratia marcescens isolates causing bacteremia: Emergence of KPC-2-encoding IncR plasmids. Front. Cell. Infect. Microbiol. 13:1075255. doi: 10.3389/fcimb.2023.1075255
Received: 20 October 2022; Accepted: 10 January 2023;
Published: 08 February 2023.
Edited by:
Afsatou Ndama (Safi) Traore, University of Venda, South AfricaReviewed by:
Nayeem Ahmad, Arabian Gulf University, BahrainCopyright © 2023 Jia, Huang, Zhang, Sheng, Chu, Xu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aiguo Xu, YWlndW94dUB6enUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.