- 1Affiliated Hospital of Jining Medical University, Jining Medical University, Jining, China
- 2Medical Laboratory of Jining Medical University, Jining Medical University, Jining, China
Tuberculous infection in a skin wound is a rare but well-known condition. This study describes a child infected with tuberculosis after being wounded. Because of swelling and pain in his wrist tissue, he was admitted to the Affiliated Hospital of Jining Medical University of Shandong Province on 16 October 2021. His medical history only included a wound. He was discharged after debridement. The laboratory data were normal. Two months after surgery, his wound was still swollen and painful. Secretions from the wound were sent for metagenomic next-generation sequencing (mNGS), which revealed three reads related to the Mycobacterium tuberculosis complex group (MTBC). A diagnosis of cutaneous tuberculosis (TB) was made. The wound disappeared after anti-TB drugs were administered. This case demonstrates that, while TB presenting as a severe cutaneous wound is rare, it should be considered in the clinical diagnosis. Clinicians should also pay attention to extrapulmonary infection with MTBC in patients, particularly in some long-suffering patients, and identify the specific pathogen as soon as possible. mNGS could help to identify pathogens and facilitate early treatment, thereby improving the prognosis.
Introduction
Multiple epidemic diseases are affecting human health in China, including tuberculosis (TB). TB must be monitored and treated because of its extremely high death rate (Etter et al., 2006; Cardona, 2018). Among all types of TB, cutaneous TB is a rare form of extrapulmonary TB responsible for 1%–2% of all cases (Bravo and Gotuzzo, 2007; Ketata et al., 2015). Mycobacterium tuberculosis complex group (MTBC) usually enters the body through hangnail wounds, small wounds, impetigo, or furuncles (Hill and Sanders, 2017; Bespiatykh et al., 2021; Kanabalan et al., 2021). Its pathogenesis is similar to that of some other epidemic diseases (Issa et al., 2012). Over 2–4 weeks, Mycobacterium enters the body and slowly develops into a tuberculous chancre. The infection could progress to impetiginous or ichthyotic forms. Lymphatic extension occurs, and lymphadenopathy occurs 1–2 months after skin infection (Hill and Sanders, 2017; Tang et al., 2021).
Cutaneous TB is caused by members of MTBC (Sethuraman and Ramesh, 2013). Phylogenetically, MTBC is contained within the phylum Actinobacteria (Mostowy and Behr, 2005). Whole-genome sequencing has identified more than 20,000 strains of Mycobacterium, including 13,974 strains of M. tuberculosis complex, 13,896 strains of M. tuberculosis (Banuls et al., 2015), 69 strains of M. canettii (Supply and Brosch, 2017), 2 strains of M. mungi (Alexander et al., 2016), and 5 strains of M. orygis (Marcos et al., 2017). To date, the diagnostic method of TB has been traditional culture methods and multiple molecular approaches (Chen et al., 2020). Owing to the inherently slow growth rate of MTBC, conventional microbial culture results have an extremely low positivity rate. This increases the difficulty of clinical diagnosis and treatment. Therefore, rapid clarification of the etiology is necessary (Ma et al., 2022). Clinically, treatment is administered according to the doctor’s experience in most cases, leading to a higher possibility of the development of drug-resistant bacteria and the possible occurrence of secondary infections (Rimola et al., 2000; Grek and Arasi, 2016; Nanchal and Ahmad, 2016).
In recent decades, metagenomic next-generation sequencing (mNGS) has emerged as a rapidly developing new technology for etiological diagnosis (Jacob et al., 2019; Guo et al., 2021). In some infectious diseases (e.g., blood infection, central nervous system infection, lung infection, or focal infection), mNGS plays an important role in etiological diagnosis, especially in the identification of MTBC and rare pathogens, such as mycoplasma, Chlamydia, parasite, and viruses (Bezerra et al., 2020; Chen et al., 2020; Haston et al., 2020; Yu et al., 2020; Chen et al., 2021; Jing et al., 2021).
mNGS has the advantages of conventional culture and many other excellent properties (e.g., short turnaround times, high sensitivity and specificity) (Haslam, 2021). Furthermore, unrecorded pathogens can be initially detected by mNGS, along with the identification of non-culturable pathogens (Ren et al., 2021; Tang et al., 2021; Bohl et al., 2022). In the future, mNGS technology could become the primary method of identifying, predicting, and preventing infectious diseases (Han et al., 2019; Garnica et al., 2021; Yu et al., 2021).
This study explored the utility of mNGS for identifying pathogens in infected patients. Additionally, we explored the application of second-generation sequencing technology in wound infection.
Case description
The case involved a 15-year-old Asian boy. Because of wrist swelling and painful discomfort after a bruise of the right wrist (on 30 September 2021), he was admitted to the Affiliated Hospital of Jining Medical University of Shandong Province, in China, on 16 October 2021.
The patient underwent fascial excision debridement to treat swelling and pain in the wrist tissue on 18 October 2021. Because the wound infection was alleviated and no exudation was noted, the patient was discharged on 31 October 2021. After discharge, the patient was reminded to regularly change the dressing and exercise.
However, the wound healed poorly, and there was still exudate 2 months later. The patient was again admitted on 9 December 2021 and underwent a second fascial excision debridement 2 days later. Samples of wound tissue were sent for microbial culture and mNGS (11 December 2021). The culture and mNGS failed to identify a pathogen. Infection-related indices, such as white blood cell count, C-reactive protein level, and neutrophilic granulocyte percentage, were normal although this was not true for procalcitonin. Thus, clinicians administered cefoperazone sodium as anti-infection therapy. One week later, most of the wounds on the right wrist had healed, except for a 3-mm wound in the middle of the wrist. Some exudate from the wound was present on the back of the right wrist (21 December 2021). Secretions from the wound were sent for mNGS, which revealed three reads for MTBC. Therefore, a diagnosis of cutaneous TB was considered. Accordingly, cefoperazone sodium administration was discontinued. Isoniazid (0.3 g/day), rifampicin (0.45 g/day), and pyrazinamide (1.5 g/day) were provided as anti-TB therapy for 3 months, and ethambutol (0.75 g) was provided as anti-TB therapy for one time. Re-examination of the wound on 29 January 2022 revealed that it had healed well. The clinicians recommended that the patient complete the course of anti-TB therapy.
The patient was in good condition during 3 months of follow-up. No significant abnormalities were found in the white blood cell count and C-reactive protein, procalcitonin, and uric acid levels in the serum.
Materials and methods
Specimen collection and processing
A 2.0- to 4.0-ml wound fluid sample (rinse solution) was collected from a debridement according to sample pretreatment instructions and inactivated in a water bath at 65°C for 30 min. A 1.5-ml microcentrifuge tube containing 480 μl of the sample and 72 U of lysozyme (Labnet VX-200, Xibao Biotechnology Co., Ltd., Shanghai, China) was placed in a metal bath at 30°C for 10 min. A screw tube containing the aforementioned sample and 250 μl of 0.5-mm glass beads was placed in a Labnet VX-200 oscillator set to the maximum oscillation for 20 min. Then, the sample was centrifuged at 8,000 rpm for 30 s, 300 μl of the supernatant was separated into a new 1.5-ml microcentrifuge tube, and DNA was extracted using a DNA Purification Kit (Huada Biotechnology Co., Ltd., Wuhan, China) according to the manufacturer’s instructions. A dsDNA HS Assay Kit 4.0 fluorometer was used to measure the DNA concentration, and DNA fragmentation was performed using a DNA enzyme digestion reaction kit (Huada Biotechnology Co., Ltd.) (Long et al., 2016).
Preparation of DNA libraries and sequencing
DNA libraries were prepared using a PMseq™ High-throughput DNA Detection Kit (Huada Biotechnology Co., Ltd.). Processes, such as DNA fragmentation, repair, adapter ligation, and unbiased polymerase chain reaction (PCR) amplification, were performed strictly in accordance with the instructions. A Qubit dsDNA HS Assay Kit 4.0 fluorometer was used to measure the DNA concentration in each sample. The quality-qualified libraries were pooled in a 0.2-ml PCR tube. A MiSeq™ Dx Reagent Kit (Huada Biotechnology Co., Ltd.) was used to prepare the DNA nanoball. Finally, the samples were sequenced using the Huada mNGS platform (Jeon et al., 2014).
Sequencing analysis and determination of pathogens
Some data, such as those for adapter contamination and low-quality and low-complexity reads, were quality-filtered. Next, Burrows-Wheeler Alignment (Version 0.7.10) was used to map the filtered sequences to a human reference database (Li and Durbin, 2009). The rest of the data were assembled using PMSEQ bioinformatics analysis software and classified via simultaneous alignment to the pathogen metagenomics database (PMDB) containing 17,500 pathogens. To date, the PMDB contains 10,989 bacterial genomes or scaffolds (196 Mycobacterium and 159 Mycoplasma, Chlamydia, and Rickettsia), 1,179 fungi related to human diseases, 5,050 whole-genome sequences of viral taxa, and 282 parasites associated with human infection (Chen et al., 2021; Yu et al., 2021; Ma et al., 2022).
The read counts and genomic coverage were classified and recorded. After receiving the results of taxonomic assignments, we aligned reads mapped to MTBC by MegaBLAST to the PMDB pathogen metagenomics database with default parameters for further confirmation. For example, the mNGS result was positive when the number of bacterial or viral reads was 10-fold greater than that of any other microbes and when the number of fungi (species level) was 5-fold greater than that of other fungi. A positive result for mNGS was given as long as the number of MTBC reads at the genus level was only 1 (Ma et al., 2022). The stringent mapped reads number (SMRN) and genomic coverage (GC) were also used as references. SMRN refers to the number of reads that are strictly mapped to the genus of the pathogen, and it can reflect the sequencing depth of the detected pathogens to some extent. Multiple factors (e.g., content of pathogen in the sample, the size of the pathogen genome, the amount of DNA extracted from the sample) affect SMRN. A higher SMRN indicates a greater likelihood that the detected microbe is pathogenic. GC refers to the percentage of the DNA sequence length of the detected pathogen that matches the known genomic sequence of the pathogen. Generally speaking, a higher GC indicates greater credibility regarding the detected pathogen. However, GC is also influenced by the type and content of the pathogen (Tang et al., 2021).
Results and discussion
TB is a pandemic disease that typically presents with clinical symptoms including fever, cough of any duration, night sweats, and weight loss (Burke et al., 2022). Currently, pathogen detection methods and techniques (e.g., traditional culture methods and multiple molecular approaches) are the predominant options for diagnosing TB (Austin, 2017).
Among TB types, cutaneous TB is frequently found, especially in developing and tropical countries (Padmavathy et al., 2007). Wound infection is one of the most serious complications of trauma. Most patients have open wounds caused by accidents. Long-term exposure to the air makes them vulnerable to contamination by pathogenic bacteria in the environment, resulting in wound infection. Cutaneous TB is a rare infectious disease. It can present with some common clinical manifestations (e.g., lupus vulgaris, scrofuloderma, TB verrucosa cutis, orificial TB, tuberculous gumma, tuberculous chancre, and acute cutaneous miliary TB) (Santos et al., 2014). However, some studies reported that the clinical manifestations are not specific in most cases of TB. To date, culture and acid-fast bacilli tests are the gold standards for TB diagnosis. TB bacilli should be easily detected in specimens; however, few or no TB bacilli can be detected because of the difficulty of culture (Vashisht et al., 2007).
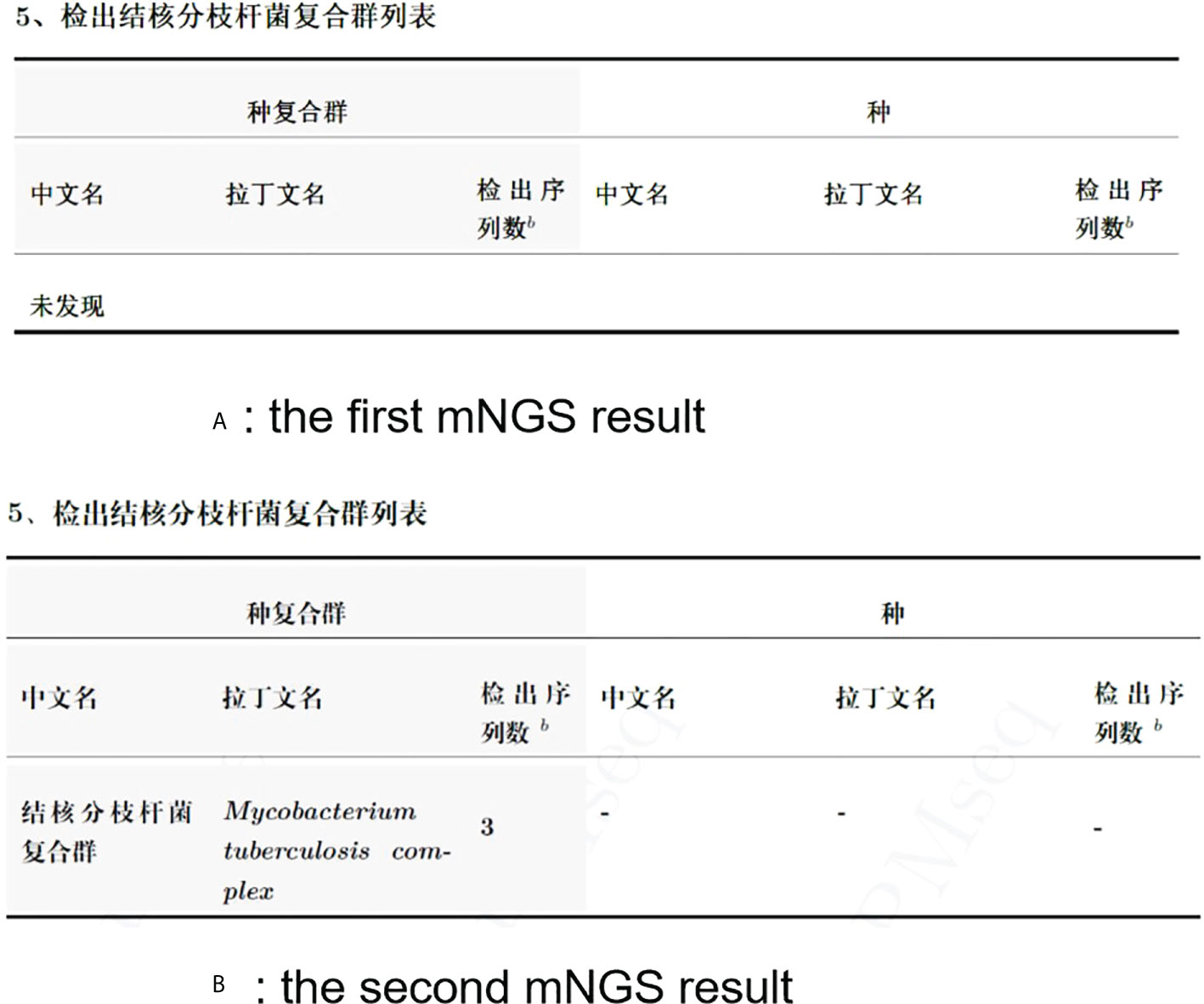
In this study, the patient underwent debridement surgery. The laboratory findings from the patient (white blood cells, 4.92; C-reactive protein, 0.25; procalcitonin, 0.055; erythrocyte sedimentation rate, 1.00) were almost normal. No pathogen was detected in the culture and smear. However, the postoperative healing was poor. In addition, targeted medication could not be used without an etiological basis. Two months later, the patient underwent another debridement surgery. The wound secretion of the patient was again negative in culture, and his laboratory findings were normal. However, MTBC was detected by mNGS (SMRN, 3; GC, 54/4,318, 603). The two results obtained by mNGS are presented in Figure 1. The patient improved after treatment with anti-TB drugs (rifampicin, pyrazinamide, isoniazid, and ethambutol) for 3 months. On 3 May 2022, anti-TB therapy has since been discontinued.
The difficulty of detecting the pathogenic cause of cutaneous TB is difficult for several reasons. First, tuberculous bacilli have a long growth cycle, and they are difficult to culture. Second, the patient was already on medication before pathogen identification, thereby increasing the chances of a negative culture. Finally, mNGS has significantly better sensitivity and specificity for detecting pathogenic bacteria than culture.
In June 2020, Chinese experts published an expert consensus for the application of China’s mNGS technology in pathogen detection in moderate and severe clinical infections (Consensus Group of Experts on Application of Metagenomic Next Generation Sequencing in the Pathogen Diagnosis in Clinical, Moderate, Severe, Infections, Professional Committee Of, Sepsis, Shock Chinese Research Hospital, Association, Professional Committee of Microbial Toxins Chinese Society For, Microbiology, and Professional Committee of Critical Care Medicine Shenzhen Medical, Association, 2020). This statement described the expert consensus regarding etiological diagnosis based on mNGS in the scope of detection, rules, and applications in moderate and severe clinical infections and highlighted the future improvement of its clinical application.
Several studies have reported the ability of mNGS to detect pathogens (Xia et al., 2019; Liu et al., 2021; Zhao et al., 2021). For example, clinicians suspected bacterial infection even though conventional microbiological tests were negative. Meanwhile, a positive result was obtained via mNGS, illustrating its greater utility for detecting pathogens (e.g., herpesvirus type 6, Pneumocystis jirovecii, or Stenotrophomonas maltophilia) in some cases. In addition, mNGS can be used to exclude fever as a sign of infection and reduce the abuse of antibiotics in infected patients (Zinner, 2007; Tang et al., 2021).
However, mNGS has limitations (Filkins et al., 2020). First, there is no uniform standard experimental procedure, and it is difficult to distinguish between pathogens and colonizing bacteria (Filkins et al., 2020). Second, the use of antibiotics can affect the diagnostic results of mNGS. Third, RNA is generally not sequenced in patient samples because of its high cost; therefore, infections caused by RNA viruses (e.g., human immunodeficiency virus or influenza A virus) may be partially undetected (Chiu and Miller, 2019). Fourth, it is especially difficult to differentiate contaminants, colonizers, and pathogens using mGNS in the case of severe infections. Finally, the cost of mNGS can be prohibitive to patients. It is not conducive to the development of clinical work and cannot help in learning how mNGS can be implemented in real-world clinical settings.
In conclusion, the findings suggest that mNGS is superior to traditional laboratory testing methods, and this method can be performed more rapidly. We believe that mNGS will soon become a candidate method for clinical diagnosis in patients infected with TB. mNGS will likely be used for the rapid detection of pathogens in the future, particularly in the context of opportunistic pathogens and mixed infections or in patients with negative conventional microbiological test results. Therefore, to better serve the clinic, we must clarify how to identify pollutants, colonizers, and pathogens in the future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MK and AH performed the experiments and analyzed the genomics data. WL analyzed and interpreted patient data. MK, QK, HD, and LJ wrote the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Medical Laboratory of Jining Medical University, Jining Medical University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MTBC, Mycobacterium tuberculosis complex; TB, tuberculosis; mNGS, metagenomic next-generation sequencing.
References
Alexander, K. A., Sanderson, C. E., Larsen, M. H., Robbe-Austerman, S., Williams, M. C., Palmer, M. V. (2016). Emerging tuberculosis pathogen hijacks social communication behavior in the group-living banded mongoose (Mungos mungo). mBio 7 (3), e00281-16. doi: 10.1128/mBio.00281-16
Austin, B. (2017). The value of cultures to modern microbiology. Antonie Van Leeuwenhoek. 110 (10), 1247–1256. doi: 10.1007/s10482-017-0840-8
Banuls, A. L., Sanou, A., Van Anh, N. T., Godreuil, S. (2015). Mycobacterium tuberculosis: Ecology and evolution of a human bacterium. J. Med. Microbiol. 64 (11), 1261–1269. doi: 10.1099/jmm.0.000171
Bespiatykh, D., Bespyatykh, J., Mokrousov, I., Shitikov, E. (2021). A comprehensive map of mycobacterium tuberculosis complex regions of difference. mSphere. 6 (4), e0053521. doi: 10.1128/mSphere.00535-21
Bezerra, R. D. S., Diefenbach, C. F., Pereira, D. V., Kashima, S., Slavov, S. N. (2020). Viral metagenomics performed in patients with acute febrile syndrome during toxoplasma gondii outbreak in south Brazil. Braz. J. Infect. Dis. 24 (3), 250–255. doi: 10.1016/j.bjid.2020.04.011
Bohl, J. A., Lay, S., Chea, S., Ahyong, V., Parker, D. M., Gallagher, S., et al. (2022). Discovering disease-causing pathogens in resource-scarce southeast Asia using a global metagenomic pathogen monitoring system. Proc. Natl. Acad. Sci. U.S.A. 119 (11), e2115285119. doi: 10.1073/pnas.2115285119
Bravo, F. G., Gotuzzo, E. (2007). Cutaneous tuberculosis. Clin. Dermatol. 25 (2), 173–180. doi: 10.1016/j.clindermatol.2006.05.005
Burke, R. M., Rickman, H. M., Singh, V., Kalua, T., Labhardt, N. D., Hosseinipour, M., et al. (2022). Same-day antiretroviral therapy initiation for people living with hiv who have tuberculosis symptoms: A systematic review. HIV Med. 23 (1), 4–15. doi: 10.1111/hiv.13169
Cardona, P. J. (2018). Pathogenesis of tuberculosis and other mycobacteriosis. Enferm Infecc Microbiol. Clin. (Engl Ed) 36 (1), 38–46. doi: 10.1016/j.eimc.2017.10.015
Chen, X., Cao, K., Wei, Y., Qian, Y., Liang, J., Dong, D., et al. (2020). Metagenomic next-generation sequencing in the diagnosis of severe pneumonias caused by chlamydia psittaci. Infection. 48 (4), 535–542. doi: 10.1007/s15010-020-01429-0
Chen, M., Lu, W., Wu, S., Wang, S., Lu, T., Peng, C. (2021). Metagenomic next-generation sequencing in the diagnosis of leptospirosis presenting as severe diffuse alveolar hemorrhage: A case report and literature review. BMC Infect. Dis. 21 (1), 1230. doi: 10.1186/s12879-021-06923-w
Chen, P., Sun, W., He, Y. (2020). Comparison of metagenomic next-generation sequencing technology, culture and genexpert Mtb/Rif assay in the diagnosis of tuberculosis. J. Thorac. Dis. 12 (8), 4014–4024. doi: 10.21037/jtd-20-1232
Chiu, C. Y., Miller, S. A. (2019). Clinical metagenomics. Nat. Rev. Genet. 20 (6), 341–355. doi: 10.1038/s41576-019-0113-7
Consensus Group of Experts on Application of Metagenomic Next Generation Sequencing in the Pathogen Diagnosis in Clinical, Moderate, Severe, Infections, Professional Committee Of, Sepsis, Shock Chinese Research Hospital, Association, Professional Committee of Microbial Toxins Chinese Society For, Microbiology, and Professional Committee of Critical Care Medicine Shenzhen Medical, Association (2020). Expert consensus for the application of metagenomic next generation sequencing in the pathogen diagnosis in clinical moderate and severe infections (First edition). Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 32 (5), 531–536. doi: 10.3760/cma.j.cn121430-20200228-00095
Etter, E., Donado, P., Jori, F., Caron, A., Goutard, F., Roger, F. (2006). Risk analysis and bovine tuberculosis, a re-emerging zoonosis. Ann. N Y Acad. Sci. 1081, 61–73. doi: 10.1196/annals.1373.006
Filkins, L. M., Bryson, A. L., Miller, S. A., Mitchell, S. L. (2020). Navigating clinical utilization of direct-from-Specimen metagenomic pathogen detection: Clinical applications, limitations, and testing recommendations. Clin. Chem. 66 (11), 1381–1395. doi: 10.1093/clinchem/hvaa183
Garnica, M., Pierrotti, L. C., Oliveira, P. V., Mazzi, M., Chebabo, A. (2021). Metagenomic next-generation sequencing (Mngs) for diagnostically challenging infectious diseases in patients with acute leukemia. Braz. J. Infect. Dis. 25 (2), 101548. doi: 10.1016/j.bjid.2021.101548
Grek, A., Arasi, L. (2016). Acute liver failure. AACN Adv. Crit. Care. 27 (4), 420–429. doi: 10.4037/aacnacc2016324
Guo, Y., Li, H., Chen, H., Li, Z., Ding, W., Wang, J., et al. (2021). Metagenomic next-generation sequencing to identify pathogens and cancer in lung biopsy tissue. EBioMedicine. 73, 103639. doi: 10.1016/j.ebiom.2021.103639
Han, D., Li, Z., Li, R., Tan, P., Zhang, R., Li, J. (2019). Mngs in clinical microbiology laboratories: On the road to maturity. Crit. Rev. Microbiol. 45 (5-6), 668–685. doi: 10.1080/1040841X.2019.1681933
Haslam, D. B. (2021). Future applications of metagenomic next-generation sequencing for infectious diseases diagnostics. J. Pediatr. Infect. Dis. Soc. 10 (Supplement_4), S112–S117. doi: 10.1093/jpids/piab107
Haston, J. C., Rostad, C. A., Jerris, R. C., Milla, S. S., Mccracken, C., Pratt, C., et al. (2020). Prospective cohort study of next-generation sequencing as a diagnostic modality for unexplained encephalitis in children. J. Pediatr. Infect. Dis. Soc. 9 (3), 326–333. doi: 10.1093/jpids/piz032
Hill, M. K., Sanders, C. V. (2017). Cutaneous tuberculos. Microbiol. Spectr. 5 (1), 28233513. doi: 10.1128/microbiolspec.TNMI7-0010-2016
Issa, R., Mohd Hassan, N. A., Abdul, H., Hashim, S. H., Seradja, V. H., Abdul Sani, A. (2012). Detection and discrimination of mycobacterium tuberculosis complex. Diagn. Microbiol. Infect. Dis. 72 (1), 62–67. doi: 10.1016/j.diagmicrobio.2011.09.021
Jacob, J. J., Veeraraghavan, B., Vasudevan, K. (2019). Metagenomic next-generation sequencing in clinical microbiology. Indian J. Med. Microbiol. 37 (2), 133–140. doi: 10.4103/ijmm.IJMM_19_401
Jeon, Y. J., Zhou, Y., Li, Y., Guo, Q., Chen, J., Quan, S., et al. (2014). The feasibility study of non-invasive fetal trisomy 18 and 21 detection with semiconductor sequencing platform. PloS One. 9 (10), e110240. doi: 10.1371/journal.pone.0110240
Jing, C., Chen, H., Liang, Y., Zhong, Y., Wang, Q., Li, L., et al. (2021). Clinical evaluation of an improved metagenomic next-generation sequencing test for the diagnosis of bloodstream infections. Clin. Chem. 67 (8), 1133–1143. doi: 10.1093/clinchem/hvab061
Kanabalan, R. D., Lee, L. J., Lee, T. Y., Chong, P. P., Hassan, L., Ismail, R., et al. (2021). Human tuberculosis and mycobacterium tuberculosis complex: A review on genetic diversity, pathogenesis and omics approaches in host biomarkers discovery. Microbiol. Res. 246, 126674. doi: 10.1016/j.micres.2020.126674
Ketata, W., Rekik, W. K., Ayadi, H., Kammoun, S. (2015). Extrapulmonary tuberculosis. Rev. Pneumol Clin. 71 (2-3), 83–92. doi: 10.1016/j.pneumo.2014.04.001
Li, H., Durbin, R. (2009). Fast and accurate short read alignment with burrows-wheeler transform. Bioinformatics. 25 (14), 1754–1760. doi: 10.1093/bioinformatics/btp324
Liu, L., Yuan, M., Shi, Y., Su, X. (2021). Clinical performance of bal metagenomic next-generation sequence and serum (1,3)-Beta-D-Glucan for differential diagnosis of pneumocystis jirovecii pneumonia and pneumocystis jirovecii colonisation. Front. Cell Infect. Microbiol. 11, 784236. doi: 10.3389/fcimb.2021.784236
Long, Y., Zhang, Y., Gong, Y., Sun, R., Su, L., Lin, X., et al. (2016). Diagnosis of sepsis with cell-free DNA by next-generation sequencing technology in icu patients. Arch. Med. Res. 47 (5), 365–371. doi: 10.1016/j.arcmed.2016.08.004
Ma, N., Chen, M., Ding, J., Wang, F., Jin, J., Fan, S., et al. (2022). Recurrent pneumonia with tuberculosis and candida Co-infection diagnosed by metagenomic next-generation sequencing: A case report and literature review. Front. Med. (Lausanne). 9, 755308. doi: 10.3389/fmed.2022.755308
Marcos, L. A., Spitzer, E. D., Mahapatra, R., Ma, Y., Halse, T. A., Shea, J., et al. (2017). Mycobacterium orygis lymphadenitis in new York, USA. Emerg. Infect. Dis. 23 (10), 1749–1751. doi: 10.3201/eid2310.170490
Mostowy, S., Behr, M. A. (2005). The origin and evolution of mycobacterium tuberculosis. Clin. Chest Med. 26 (2), 207–16, v-vi. doi: 10.1016/j.ccm.2005.02.004
Nanchal, R. S., Ahmad, S. (2016). Infections in liver disease. Crit. Care Clin. 32 (3), 411–424. doi: 10.1016/j.ccc.2016.03.006
Padmavathy, L., Rao, L. L., Ethirajan, N., Krishnaswami, B. (2007). Ulcerative lupus vulgaris of face: An uncommon presentation in India. Indian J. Tuberc. 54 (1), 52–54.
Ren, D., Ren, C., Yao, R., Zhang, L., Liang, X., Li, G., et al. (2021). The microbiological diagnostic performance of metagenomic next-generation sequencing in patients with sepsis. BMC Infect. Dis. 21 (1), 1257. doi: 10.1186/s12879-021-06934-7
Rimola, A., García-Tsao, G., Navasa, M., Piddock, L. J., Planas, R., Bernard, B., et al. (2000). Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis a consensus document. international ascites Club.Pdf. J. Hepatol. 32 (1), 142–153. doi: 10.1016/S0168-8278(00)80201-9
Santos, J. B., Figueiredo, A. R., Ferraz, C. E., Oliveira, M. H., Silva, P. G., Medeiros, V. L. (2014). Cutaneous tuberculosis: Epidemiologic, etiopathogenic and clinical aspects - part I. Bras. Dermatol. 89 (2), 219–228. doi: 10.1590/abd1806-4841.20142334
Sethuraman, G., Ramesh, V. (2013). Cutaneous tuberculosis in children. Pediatr. Dermatol. 30 (1), 7–16. doi: 10.1111/j.1525-1470.2012.01794.x
Supply, P., Brosch, R. (2017). The biology and epidemiology of mycobacterium canettii. Adv. Exp. Med. Biol. 1019, 27–41. doi: 10.1007/978-3-319-64371-7_2
Tang, W., Zhang, Y., Luo, C., Zhou, L., Zhang, Z., Tang, X., et al. (2021). Clinical application of metagenomic next-generation sequencing for suspected infections in patients with primary immunodeficiency disease. Front. Immunol. 12, 696403. doi: 10.3389/fimmu.2021.696403
Vashisht, P., Sahoo, B., Khurana, N., Reddy, B. S. (2007). Cutaneous tuberculosis in children and adolescents: A clinicohistological study. J. Eur. Acad. Dermatol. Venereol. 21 (1), 40–47. doi: 10.1111/j.1468-3083.2006.01858.x
Xia, H., Guan, Y., Zaongo, S. D., Xia, H., Wang, Z., Yan, Z., et al. (2019). Progressive multifocal leukoencephalopathy diagnosed by metagenomic next-generation sequencing of cerebrospinal fluid in an hiv patient. Front. Neurol. 10, 1202. doi: 10.3389/fneur.2019.01202
Yu, G., Wang, X., Zhu, P., Shen, Y., Zhao, W., Zhou, L. (2021). Comparison of the efficacy of metagenomic next-generation sequencing and xpert Mtb/Rif in the diagnosis of tuberculous meningitis. J. Microbiol. Methods. 180, 106124. doi: 10.1016/j.mimet.2020.106124
Yu, G., Zhao, W., Shen, Y., Zhu, P., Zheng, H. (2020). Metagenomic next generation sequencing for the diagnosis of tuberculosis meningitis: A systematic review and meta-analysis. PLoS One. 15 (12), e0243161. doi: 10.1371/journal.pone.0243161
Zhao, Z., Song, J., Yang, C., Yang, L., Chen, J., Li, X., et al. (2021). Prevalence of fungal and bacterial Co-infection in pulmonary fungal infections: A metagenomic next generation sequencing-based study. Front. Cell Infect. Microbiol. 11, 749905. doi: 10.3389/fcimb.2021.749905
Keywords: tuberculosis, cutaneous tuberculosis, mycobacterium tuberculosis complex, metagenomic next-generation sequencing, pathogen
Citation: Kong M, Li W, Kong Q, Dong H, Han A and Jiang L (2022) Application of metagenomic next-generation sequencing in cutaneous tuberculosis. Front. Cell. Infect. Microbiol. 12:942073. doi: 10.3389/fcimb.2022.942073
Received: 12 May 2022; Accepted: 12 September 2022;
Published: 23 September 2022.
Edited by:
Saurabh Pandey, Jamia Hamdard University, IndiaReviewed by:
Md Irshad Ahmad, All India Institute of Medical Sciences, IndiaMd. Aejazur Rahman, Africa Health Research Institute (AHRI), South Africa
Copyright © 2022 Kong, Li, Kong, Dong, Han and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liqing Jiang, anlqaWFuZ2xpcWluZ0AxNjMuY29t
 Min Kong
Min Kong Wei Li1
Wei Li1 Liqing Jiang
Liqing Jiang