
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Cell. Infect. Microbiol. , 29 December 2022
Sec. Fungal Pathogenesis
Volume 12 - 2022 | https://doi.org/10.3389/fcimb.2022.1104519
This article is part of the Research Topic Tropical Fungal Diseases View all 10 articles
Editorial on the Research Topic
Tropical fungal diseases
The tropical region of Earth occurs between the latitude lines of the Tropic of Cancer and the Tropic of Capricorn. The tropics include parts of North America, South America, Africa, Asia, and Australia (Figure 1). The climate in the tropics is characterized by a more direct sunlight than the rest of Earth, meaning that the tropics are generally hotter and wetter and less affected by the solar seasons.
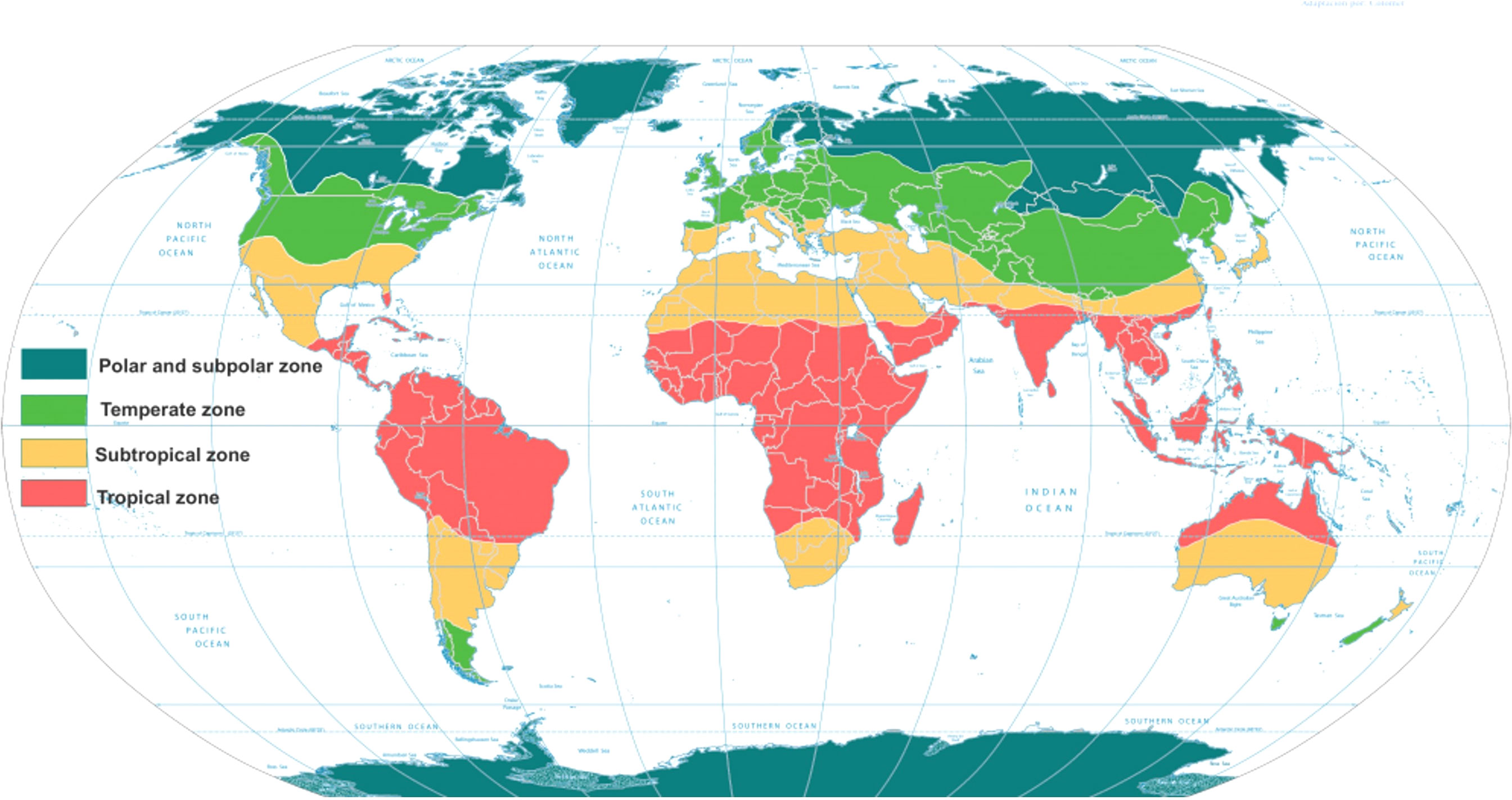
Figure 1 World map with the intertropical zone highlighted in red. (https://content.meteoblue.com/pt/research-education/educational-resources/meteoscool/zonas-climaticas-em-geral).
According to the literature, there are many fungal infections that occur more frequently in tropical zones or are restricted to certain regions within the tropics. The interference in ecosystems mainly by deforestation of tropical areas and re-adaptation of wild animals into the cities has modified the spectrum of the mycoses. Many of these fungal infections, although with important impacts on public health, are still considered neglected and low visibility diseases. The number of reports of immunosuppressed patients with opportunistic fungal diseases has increased significantly across the world. In this special issue, we will explore some of the main or even rare fungal infections that affect tropical areas of the planet. Included among these diseases are cutaneous (dermatophytes or non-dermatophytes), subcutaneous (chromoblastomycosis and sporotrichosis), systemic (cryptococcosis), and endemic (histoplasmosis) mycoses.
Cutaneous mycoses are a group of fungal infections affecting the skin, hair, and nails; however, in patients with autosomal recessive CARF9 deficiency or immunodeficiencies, dermatophytes can cause systemic mycosis (de Oliveira Pereira et al., 2021). The use of tools such as multilocus phylogenetic analysis has distinguished seven main clades: the genera Arthroderma, Lophophyton, Microsporum, Paraphyton, Nannizzia, Epidermophyton, and Trichophyton (reviewed by de Oliveira Pereira et al., 2021). Treatment of dermatophytosis is very complex and depends on several factors arising from both the host and the fungus. Drug resistance is a major problem, especially in the treatment of dermatophytosis. Terbinafine is a highly recommended drug to treat dermatophytosis. The determination of the antifungal susceptibility and punctual mutations in isolates of dermatophytes resistant to terbinafine is essential to assist physicians in the management of patients (Pashootan et al.).
Dematiaceous or melanized fungi include a large and heterogeneous group of fungi that cause several diseases including chromoblastomycosis, phaeohyphomycosis, and eumycetoma (reviewed by Arcobello and Revankar, 2020). Phaeohyphomycosis refers to a group of mycoses caused by pigmented fungi characterized by yeast-like cells, hyphae, or a combination of both morphotypes in tissues and should be distinguished from primary implantation mycoses. In the last two decades, the frequency of reports and the diversity of the etiological agents involved in this type of mycosis have increased, especially in immunosuppressed individuals (He et al.). Chromoblastomycosis is one of the most prevalent implantations or subcutaneous fungal infections characterized by traumatic inoculation from an environmental source with clinically polymorphic lesions (Queiroz-Telles et al., 2017). The main agents of Chromoblastomycosis include Fonsecaea spp., Phialophora verrucosa, Cladophialophora carrionii, Exophiala dermatitidis, and Rinocladiella aquaspersa (Queiroz-Telles et al., 2017). Uncommon agents such as Chrysosporium keratinophilum, a saprophytic filamentous fungus commonly found in soil, dung, and animal fur, and rarely involved in infections in humans, was reported in a patient with severe chromoblastomycosis-like lesions (Mijiti et al.).
Genomic studies involving Fonsecaea and Cladophialophora genera from adverse microhabitats and mammal tissue are extremely important to understand virulence factors. The results of a study suggested a higher level of extremotolerance of environmental species (Vicente et al.). Another study focused on the degree with which Fonsecaea agents are involved in pathogenicity. The authors aimed to evaluate a model of trans-kingdom infection. The plant infection models employed suggested that all Fonsecaea were saprobic. The authors observed, for the first time, structures similar to muriform cells, in a larvae model, that were produced during infection of human tissue, confirming the role of muriform cells as a pathogenic adaptation in animal tissues (Fornari et al.).
Sporotrichosis, caused by Sporothrix brasiliensis, a cat-transmitted fungal infection, is an endemic and neglected mycosis found mainly in Brazil (Gremião et al., 2021). The geographic expansion of this zoonosis has been reported in different regions of Brazil, and more recently, cases were reported in other countries in South America (Gremião et al, 2021). Environmental and epidemiological studies are essential to control the spread of this mycosis. A study conducted in Rio de Janeiro (Brazil), an area highly endemic for feline and human diseases, showed that S. brasiliensis can maintain itself persistently in its environment for years. In addition, antifungal susceptibility tests indicated that minimal inhibitory concentration of itraconazole from the environmental isolates was lower with cat isolates; however, with amphotericin B and terbinafine it was similar (Rabello et al.).
In general, invasive fungal diseases are rare in immunocompetent individuals; however, an increasing population of immunocompromised patients and ongoing climate change could significantly increase the prevalence of fungal diseases (Casadevall, 2022). Histoplasma spp., the causal agent of histoplasmosis, is an environmental dimorphic fungus with a worldwide distribution. In immunocompetent patients, histoplasmosis usually occurs in a less aggressive form, whereas immunocompromised patients present with a more aggressive clinical form. Hemophagocytic lymphohistiocytosis (HLH) is a rare disorder and is characterized by persistent immune activation of natural killer (NK) and cytotoxic T cells. In this special issue, Chen et al. reviewed cases of HLH secondary to disseminated histoplasmosis in HIV seronegative patients and highlighted that this condition has become increasingly common in emerging endemic areas, carrying a high mortality rate. However, timely diagnosis and early use of antifungals can lead to a favorable prognosis.
Similarly, cryptococcosis is a fungal infection found in immunosuppressed patients, well described in HIV-infected patients, and more rarely occurring in immunocompetent individuals. Goupil de Bouillé et al. described the clinical, mycological, immunological, and genetic characteristics of six HIV-negative patients from French Guiana presenting with invasive cryptococcosis. Despite the available antifungal drugs for cryptococcosis treatment, morbidity and mortality rates remain high. A vaccine would be an important strategy against cryptococcosis infection. Normile and Del Poeta showed in previous studies that a live, attenuated, Cryptococcus neoformans Δsgl1 mutant accumulating steryl glucosides was found to be avirulent and protected mice from an otherwise lethal infection. In this study, the validation of three different models of successful vaccination strategies against cryptococcosis are shown, which used heat-killed C. neoformans Δsgl1 in a CD4+ T cell deficiency setting.
The contributions described above in this research topic illustrate the changes in behavior and the increase of fungal infections in the tropics, such as the increase in the spread of feline sporotrichosis, the increase in the resistance to antifungals of dermatophytes, and the invasive infection of immunocompetent hosts by “opportunistic” fungi such as Cryptococcus, as well as successful advances in experimental vaccines against cryptococcosis. Nonetheless, fungal diseases in tropical and subtropical areas continue to be a public health problem. Most of these fungal diseases are neglected and have low visibility, thereby affecting immunocompromised patients (such as persons living with HIV), people in low-income countries, and particularly agricultural workers in rural areas.
AG, CT, and JM edited the topic and wrote the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Arcobello, J. T., Revankar, S. G. (2020). Phaeohyphomycosis. Semin. Respir. Crit. Care Med. 41 (1), 131–140. doi: 10.1055/s-0039-3400957
Casadevall, A. (2022). Immunity to invasive fungal dieseases. Annu. Rev. Immunol. 40, 121–141. doi: 10.1146/annurev-immunol-101220-034306
de Oliveira Pereira, F., Gomes, S. M., Lima da Silva, S., Paula de Castro Teixeira, A., Lima, I. O. (2021). The prevalence of dermatophytoses in Brazil: A systematic review. J. Med. Microbiol. 70 (3). doi: 10.1099/jmm.0.001321
Gremião, I. D. F., Martins, da S., da Rocha, E., Montenegro, H., Carneiro, A. J. B., Xavier, M. O., et al. (2021). Guideline for the management of feline sporotrichosis caused by sporothrix brasiliensis and literature revision. Braz. J. Microbiol. 52 (1), 107–124. doi: 10.1007/s42770-020-00365-3
Keywords: tropical diseases, laboratory diagnostic, antifungal treatment, molecular biology, proteomics
Citation: Taborda CP, Muñoz JE and Gonzalez A (2022) Editorial: Tropical fungal diseases. Front. Cell. Infect. Microbiol. 12:1104519. doi: 10.3389/fcimb.2022.1104519
Received: 21 November 2022; Accepted: 29 November 2022;
Published: 29 December 2022.
Edited and Reviewed by:
Anuradha Chowdhary, University of Delhi, IndiaCopyright © 2022 Taborda, Muñoz and Gonzalez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlos P. Taborda, VGFib3JkYUB1c3AuYnI=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.