- 1Laboratory of Bacterial Pathogenesis and Immunology, Rockefeller University, New York, NY, United States
- 2Executive Office, MMF Systems, Inc., New York, NY, United States
- 3Data Science and Engineering, MyMedicalFiles (MMF) Systems, Inc., New York, NY, United States
- 4Nutrition Innovation Centre for Food and Health (NICHE), School of Biomedical Sciences, Ulster University, Coleraine, United Kingdom
- 5Central European Institute of Technology (CEITEC), Masaryk University, Brno, Czechia
- 6Department of Biology, Faculty of Medicine, Masaryk University, Brno, Czechia
The discovery of T-cell responses to SARS-CoV-2 in non-infected individuals indicates cross-reactive immune memory from prior exposure to human coronaviruses (HCoV) that cause the common cold. This raises the possibility that “immunity” could exist within populations at rates that may be higher than serology studies estimate. Besides specialized research labs, however, there is limited ability to measure HCoV CD4+ and CD8+ T-cell responses to SARS-CoV-2 infection, which currently impedes interpretation of any potential correlation between COVID-19 disease pathogenesis and the calibration of pandemic control measures. Given this limited testing ability, an alternative approach would be to exploit the large cohort of currently available data from which statistically significant associations may be generated. This would necessitate the merging of several public databases including patient and contact tracing, which could be created by relevant public health organizations. Including data from both symptomatic and asymptomatic patients in SARS-CoV-2 databases and surveillance systems could provide the necessary information to allow for more informed decisions.
Introduction—Asymptomatic Infection in Dense Populations
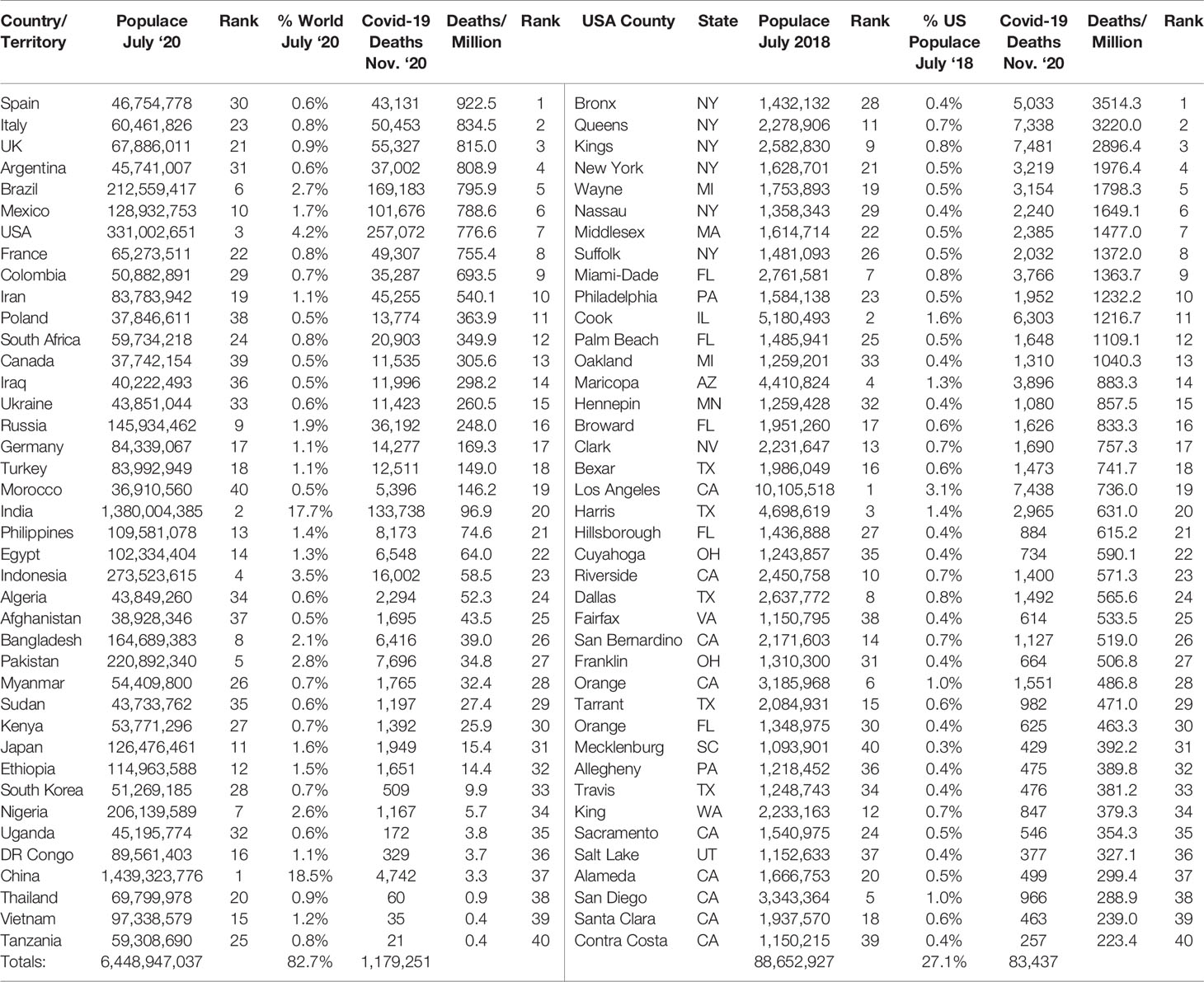
It is most curious that the majority of poor, highly populated countries have seen fewer deaths per million during the current pandemic than most advanced Western nations. In contrast, during the 1918 influenza pandemic, which had a global death rate approaching 3%, less-developed countries saw noticeably higher rates (Spreeuwenberg et al., 2018). The large variation in SARS-CoV-2 deaths per million people between countries, and even states and counties within the U.S., are on the surface confusing and difficult to explain. It seems counterintuitive that countries with both limited health resources and sick, aging populations have reported far fewer mortalities due to SARS-CoV-2 than countries with advanced healthcare resources, relatively healthy populations and greater lock-down measures (Worldometer; Contributors W; Engineering JHUCfSSa, 2020) (Table 1).
While a number of factors may explain this anomaly, including differences in age, co-morbidities, socio-economic status, and testing capacity, it should not be overlooked that individuals in these poorer countries, who often reside in crowded multi-generational family groups with shared facilities, may have experienced increased and possibly sustained, exposure to human coronaviruses (HCoVs) that cause the “common cold”. This elevated exposure, which may lead to greater levels of cross-immunity to SARS-CoV-2, may help explain why:
● A serology study of slums in three wards of Mumbai showed that residents there had 3·5 times the SARS-CoV-2 infection rate of those in housing societies (57% versus 16%), but lower fatality rates (0·05%–0·10%) (Malani et al., 2020). None of the people included in the study had been tested for active SARS-CoV-2 infection using an RT-qPCR assay, suggesting either asymptomatic infection or very mild symptoms.
● A study of the United States state prison systems in Arkansas, North Carolina, Ohio, and Virginia revealed a 70% infection rate amongst the 4,693 inmates tested, of whom 96% were asymptomatic. A significant number of these prisoners were older and, therefore, presumed to be more prone to complications, but this was not the case (So and Smith, 2020).
● Approximately 90% of 147 homeless shelter residents in Boston who were infected with SARS-CoV-2 exhibited no symptoms, even though the shelter’s living space was shared by all residents. Similarly, 95% of the 481 infected workers at a Tyson Foods poultry plant in Springdale, Arkansas were asymptomatic (Cha, 2020).
Asymptomatic Infection in School Children
Schools are densely populated environments, so their reopening has left many people anxious about the role they may play in spreading SARS-CoV-2 within homes and the wider community. Data has consistently shown that children who become infected with SARS-CoV-2 typically experience mild or no symptoms. There may be multiple reasons for this clinical outcome, including the lack of comorbidities and/or age-related immune system characteristics. However, an intriguing possibility is that cross-reactive T-cells generated in response to HCoV-related colds may be present at a higher prevalence within the younger population due to exposure in school environments (Arroll, 2011; Steinman et al., 2020). It may be possible that these “circulating” cross-reactive T-cells could suppress the development of clinical symptoms, despite a recent study demonstrating that viral nucleic acid loads in 5- to 17-year-olds match or exceed (for those less than 5 years old) those found in adults (Heald-Sargent et al., 2020). It is also unclear to what extent infected children shed SARS-CoV-2 or are vectors for its spread, especially those who are symptom-free. Studies to date have suggested that children, especially those in primary or elementary schools, are at low risk of contracting the disease, may be the initial source of infection in only a very small number of cases, and are unlikely to pass it on via child-to-child or child-to-adult transmission (Armann et al., 2020, Davies et al., 2020; Munro and Faust, 2020; Posfay-Barbe et al., 2020).
T-Cell Responses to SARS-CoV-2 in Non-Infected and Asymptomatic Individuals
While T-cell responses to SARS-CoV-2 in infected individuals have now been reported, the emerging descriptions of pre-existing SARS-CoV-2 cross-reactive CD4+ and CD8+ T-cells amongst individuals who have not been infected are of particular interest (Corman et al., 2018; Braun et al., 2020; Grifoni et al., 2020; Sette and Crotty, 2020). The presence of these cross-reactive T-cells appears to be explained by prior exposure to HCoVs, such as HCoV-HKU1, HCoV-OC43H, CoV-NL63, and HCoV-229E, that generate T-cells capable of recognizing SARS-CoV-2 antigens (Mateus et al., 2020). Though involving different viruses, a similar situation is reminiscent in the historical findings of physician Edward Jenner, who discovered that milkmaids rarely succumbed to smallpox and correctly deduced that exposure to cowpox, a related virus causing a much milder illness, protected them. Similarly, during the 2009 swine flu pandemic caused by H1N1/09, the majority of people over the age of 60 displayed levels of pre-existing immunity resulting from exposure to similar flu viruses earlier in life, while young individuals had very little immunity and were, in contrast to the current situation, at greater risk (Xu et al., 2010).
Immunocompetent children and adults with respiratory infections (the common cold) often present as asymptomatic, or develop mild respiratory tract illnesses. More than 200 viral strains have been implicated as causal factors of the common cold. Rhinoviruses are responsible for ~35% of upper respiratory infections; HCoVs, often asymptomatic, cause 15-25% of cases, while influenza, adenoviruses, and other viral types account for the rest. Adults average two to three common colds each year, while children get six to eight, of which one or two are caused by HCoVs (Simasek and Blandino, 2007). Accordingly, it was found in a study of 100 subjects that most individuals had evidence of serum antibodies to all four HCoV strains (Gorse et al., 2010). We envisage one potential study resulting from a synthesis of these observations could be to investigate whether levels of longer-lasting “immunity” to SARS-CoV-2 could be higher than serology tests indicate. A positive result would be welcome news from a public health perspective.
Our ability to measure HCoV CD4+ and CD8+ T-cell responses to SARS-CoV-2 infection is limited due to the specialized nature of the tests. This major knowledge gap makes the interpretation of COVID-19 disease pathogenesis more difficult and clouds our ability to quantify the usefulness of pandemic control measures, such as social distancing.
Current Databases Do Not Capture Severity of Symptoms and Cohabitation Data
Searches of relevant publicly available databases, including the Johns Hopkins Coronavirus Resource Centre, National Institutes of Health Open-Access Data and Computational Resources to Address COVID-19, CDC World Dataset, The Covid-19 Tracking Project, Florida Department of Health, New York City Department of Health and Mental Hygiene, 1Point3Acres, and others, revealed a lack of information relating to the severity of symptoms (symptomatic vs. asymptomatic), possibly related to lower testing rates in highly populated or developing countries for individuals who are asymptomatic. More importantly, information pertaining to cohabitation and contact tracing was not included. A retrospective analysis that combines information from SARS-CoV-2 patient and contact tracing databases might be useful in determining whether individuals infected with SARS-CoV-2 who reside with school-age children are more likely to be asymptomatic. Such an analysis could be used to test the hypothesis that exposure to HCoV in densely populated environments leads to greater levels of cross-immunity to SARS-CoV-2.
The Need to Include Asymptomatic Individuals in Surveillance Studies
Surveillance studies of respiratory virus circulation in the United States (and globally) are typically limited to data collected by clinical labs from symptomatic individuals. This approach does not capture the impact of respiratory infections that are asymptomatic or associated with mild respiratory tract illness in immunocompetent children and adults. The largest such surveillance study of symptomatic HCoV patients, which was conducted in the U.S. from 1st July, 2014 through 30th June, 2017, contained the results of 854,575 HCoV rRT-PCR tests performed by 117 laboratories in 42 states. Overall, 2·2% were positive for HCoV-OC43, 1·0% for HCoV-NL63, 0·8% for HCoV-229E, and 0·6% for HCoV-HKU1 (Killerby et al., 2018). These data suggest that less than about 5% of symptomatic HCoV infections (colds) are likely to help build cross-immunity to SARS-CoV-2.
For a different perspective we turn to a unique, cross-sectional longitudinal study of individuals, both symptomatic and asymptomatic, that sought to identify changes in respiratory virus colonization before and after the 2013 Hajj, a 5- to 6-day religious pilgrimage to Mecca, Saudi Arabia (attended by more than 2 million people) (Memish et al., 2015). Pre- and post-Hajj nasal specimens were prospectively obtained from a paired cohort (692 pilgrims) and from nonpaired cohorts (514 arriving and 470 departing pilgrims) from 13 countries including the United States (8·4%) and countries in Africa (44·2%), Asia (40·2%), and Europe (7·2%). Nasal specimens were tested for 34 respiratory pathogens using RT-PCR. The prevalence of viruses increased from 7·4% before the Hajj to 45·4% after the Hajj, due to the acquisition of rhinoviruses, coronaviruses (229E, HKU1, OC43), and influenza A H1N1. Among the paired cohort, HCoV 229E infections increased from six to 101 (0·9%–14·6%; p < 0·001). Among the non-paired cohort, HCoV 229E infections increased from five to 48 (1·0%–10·2%; p < 0·001). These data, taken from both symptomatic and asymptomatic adults, show that HCoV 229E can, given the right conditions, spread extremely quickly in a short period of time. This supports the hypothesis that children, and potentially the adults with whom they live, are likely to have been exposed to HCoV strains that can elicit T-cells cross-reactive to SARS-CoV-2, perhaps leading to a clinically relevant easing of symptoms. However, acquiring the information needed to truly test the hypothesis, and make more informed decisions, necessitates the inclusion of data from both asymptomatic and symptomatic patients, SARS-CoV-2 databases, and surveillance systems.
Conclusion
It may be the case that seasonal HCoV colds have actually been, and will continue to be, one of our greatest allies in the fight against the current SARS-CoV-2 pandemic and possibly SARS-CoV-1 which surfaced in November 2002 (Feng et al., 2009).
Given other HCoVs are likely to provide levels of protection against SARS-CoV-2 via cross-reactive immune memory, it is important to maintain levels of immunity to the broader spectrum of HCoVs in the current environment. If the spread of other mild respiratory and HCoV-related infections in school is reduced from normal levels, what impact will this have on the normal transmission of the “common cold” between children and those with whom they reside, as well as the wider community? Could this lead to a reduction in the temporary buildup of cross-reactive T-cell responses to SARS-CoV-2 that could provide some vital protection in an older, higher risk population, particularly given the reduced level of T-cell diversity and loss of immunity to previous HCoV infections as individuals age? While speculative at this stage, it is possible that differential spread of respiratory viruses other than SARS-CoV-2 within the younger population could be beneficial for their older relatives.
Besides specialized research labs there is a limited ability to measure HCoV CD4+ and CD8+ T-cell responses to SARS-CoV-2 infection. This major knowledge gap currently impedes interpretation of COVID-19 disease pathogenesis, and the calibration of pandemic control measures including social distancing. Unfortunately, the data needed to demonstrate this is not available because current SARS-CoV-2 databases and surveillance systems do not include information about the people who might be benefitting from cross-reactive immune memory ie., those who are asymptomatic. Inclusion of this data could help paint a more accurate picture of the clinical course of the SARS-CoV-2 pandemic and enable better decision making.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author Contributions
MC conceived the idea for the manuscript and wrote the first draft. MC, FA, AM, and OS participated in rewriting, editing, and conducting literature search. All authors contributed to the article and approved the submitted version.
Conflict of Interest
Authors MC and FA were employed by the company MMF Systems, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Dr. Vincent A. Fischetti and John C. Baird for their insight and support.
References
Armann J. P., Unrath M., Kirsten C., Lueck C., Dalpke A., Berner R. (2020). Anti-SARS-CoV-2 IgG antibodies in adolescent students and their teachers in Saxony, Germany (SchoolCoviDD19): very low seropraevalence and transmission rates. doi: 10.1101/2020.07.16.20155143
Braun J., Loyal L., Frentsch M., Wendisch D., Georg P., Kurth F., et al. (2020). SARS-CoV-2-reactive T cells in healthy donors and patients with COVID-19. Nature. doi: 10.1038/s41586-020-2598-9
Cha A. E. (2020). Forty percent of people with coronavirus infections have no symptoms. Might they be the key to ending the pandemic? Washington Post 2020.
Contributors W. List of the most populous counties in the United States. Wikipedia, The Free Encyclopedia. Available at: https://en.wikipedia.org/w/index.php?title=List_of_the_most_populous_counties_in_the_United_States&oldid=967385264 (Accessed 28 July 2020).
Corman V. M., Muth D., Niemeyer D., Drosten C. (2018). Hosts and Sources of Endemic Human Coronaviruses. Adv. Virus Res. 100, 163–188. doi: 10.1016/bs.aivir.2018.01.001
Davies N. G., Klepac P., Liu Y., Prem K., Jit M., Group C. C.-W., et al. (2020). Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 26, 1205–1211. doi: 10.1101/2020.03.24.20043018
Engineering JHUCfSSa. (2020). Coronavirus Resource Center (Johns Hopkins University). Available at: https://coronavirus.jhu.edu/ (Accessed July 27, 2020)
Feng D., de Vlas S. J., Fang L. Q., Han X. N., Zhao W. J., Sheng S., et al. (2009). The SARS epidemic in mainland China: bringing together all epidemiological data. Trop. Med. Int. Health 14 (Suppl 1), 4–13. doi: 10.1111/j.1365-3156.2008.02145.x
Gorse G. J., Patel G. B., Vitale J. N., O’Connor T. Z. (2010). Prevalence of antibodies to four human coronaviruses is lower in nasal secretions than in serum. Clin. Vaccine Immunol. 17 (12), 1875–1880. doi: 10.1128/CVI.00278-10
Grifoni A., Weiskopf D., Ramirez S. I., Mateus J., Dan J. M., Moderbacher C. R., et al. (2020). Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181 (7), 1489–1501.e1415.
Heald-Sargent T., Muller W. J., Zheng X., Rippe J., Patel A. B., Kociolek L. K. (2020). Age-Related Differences in Nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Levels in Patients With Mild to Moderate Coronavirus Disease 2019 (COVID-19). JAMA Pediatr. 174, 902–903. doi: 10.1001/jamapediatrics.2020.3651
Killerby M. E., Biggs H. M., Haynes A., Dahl R. M., Mustaquim D., Gerber S. I., et al. (2018). Human coronavirus circulation in the United States 2014-2017. J. Clin. Virol. 101, 52–56. doi: 10.1016/j.jcv.2018.01.019
Malani A., Shah D., Kang G., Lobo G. N., Shastri J., Mohanan M., et al. (2020). Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India. Lancet Glob. Health.
Mateus J., Grifoni A., Tarke A., Sidney J., Ramirez S. I., Dan J. M., et al. (2020). Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science 370, 89–94. doi: 10.1126/science.abd3871
Memish Z. A., Assiri A., Turkestani A., Yezli S., Al Masri M., Charrel R., et al. (2015). Mass gathering and globalization of respiratory pathogens during the 2013 Hajj. Clin. Microbiol. Infect. 21 (6), 571.e571–578. doi: 10.1016/j.cmi.2015.02.008
Munro A. P. S., Faust S. N. (2020). Children are not COVID-19 super spreaders: time to go back to school. Arch. Dis. Child. 105 (7), 618–619. doi: 10.1136/archdischild-2020-319474
Posfay-Barbe K. M., Wagner N., Gauthey M., Moussaoui D., Loevy N., Diana A., et al. (2020). COVID-19 in Children and the Dynamics of Infection in Families. Pediatrics 146, e20201576. doi: 10.1542/peds.2020-1576
Sette A., Crotty S. (2020). Pre-existing immunity to SARS-CoV-2: the knowns and unknowns. Nat. Rev. Immunol. 20, 457–458.
Simasek M., Blandino D. A. (2007). Treatment of the common cold. Am. Fam. Physician 75 (4), 515–520.
So L., Smith G. (2020). In four U.S. state prisons, nearly 3,300 inmates test positive for coronavirus – 96% without symptoms. Reuters 2020.
Spreeuwenberg P., Kroneman M., Paget J. (2018). Reassessing the Global Mortality Burden of the 1918 Influenza Pandemic. Am. J. Epidemiol. 187 (12), 2561–2567.
Steinman J. B., Lum F. M., Ho P. P., Kaminski N., Steinman L. (2020). Reduced development of COVID-19 in children reveals molecular checkpoints gating pathogenesis illuminating potential therapeutics. Proc. Natl. Acad. Sci. U. S. A. 117, 24620–24626.
Worldometer. Countries in the world by population. Available at: https://www.worldometers.info/world-population/population-by-country/ (Accessed July 27, 2020).
Keywords: SARS-CoV-2, COVID-19, T-cell, human coronaviruses, immunity, contact tracing, children
Citation: Capoor MN, Ahmed FS, McDowell A and Slaby O (2020) Is the “Common Cold” Our Greatest Ally in the Battle Against SARS-CoV-2? Front. Cell. Infect. Microbiol. 10:605334. doi: 10.3389/fcimb.2020.605334
Received: 11 September 2020; Accepted: 18 November 2020;
Published: 18 December 2020.
Edited by:
Binod Kumar, Loyola University Chicago, United StatesReviewed by:
Subodh Samrat, Wadsworth Center, United StatesSuganya Sivagurunathan, Northwestern University, United States
Copyright © 2020 Capoor, Ahmed, McDowell and Slaby. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Manu N. Capoor, bWNhcG9vckBtYWlsLnJvY2tlZmVsbGVyLmVkdQ==
 Manu N. Capoor
Manu N. Capoor Fahad S. Ahmed
Fahad S. Ahmed Andrew McDowell
Andrew McDowell Ondrej Slaby
Ondrej Slaby