- 1Laboratory of Stem Cells for Tissue Engineering, IRCCS Policlinico San Donato, San Donato Milanese, Italy
- 2Institute for Molecular and Translational Cardiology (IMTC), San Donato Milanese, Italy
- 3Department of Surgery, Indiana University School of Medicine, Indianapolis, IN, United States
- 4Indiana University Melvin and Bren Simon Comprehensive Cancer Center, Indianapolis, IN, United States
- 5Indiana Center of Musculoskeletal Health, Indianapolis, IN, United States
- 6Richard L. Roudebush Veterans Administration Medical Center, Indianapolis, IN, United States
- 7IRCCS Istituto Ortopedico Galeazzi, Milan, Italy
- 8Department of Biomedical Sciences for Health, University of Milan, Milan, Italy
Editorial on the Research Topic
Metabolic Adaptation of Muscle Tissue in Diseases Associated With Cachexia
This Research Topic on skeletal muscle metabolism alterations in diseases associated with cachexia attempts to further elucidate how newly discovered molecular targets can influence muscle tissue structure and function. The skeletal apparatus, which accounts for approximately 30%–40% of total body weight (Kim et al., 2002), plays a critical physiological role in maintaining posture, controlling movement, altering thoracic volume for respiration, regulating temperature homeostasis, and cellular metabolism (Baskin et al., 2015; Frontera and Ochala, 2015; Rowland et al., 2015). Accelerated and excessive loss of skeletal muscle mass is a condition that occurs in several diseases, including cancer cachexia, which is closely correlated with a marked reduction in quality of life and shortened survival (Evans, 2010). In this context, cachexia has been recognized as a complex multifactorial metabolic syndrome characterized by glucose, lipid, and protein metabolism alterations, that contribute to the poor prognosis in affected patients (Rohm et al., 2019) (Figure 1). In recent years, the understanding of the molecular bases of these metabolic alterations has revealed novel targets for treating the syndrome. This generated an increasing number of new studies to further elucidate the molecular biomarkers of cachexia and to develop new therapeutic approaches that could counteract and reduce muscle wasting.
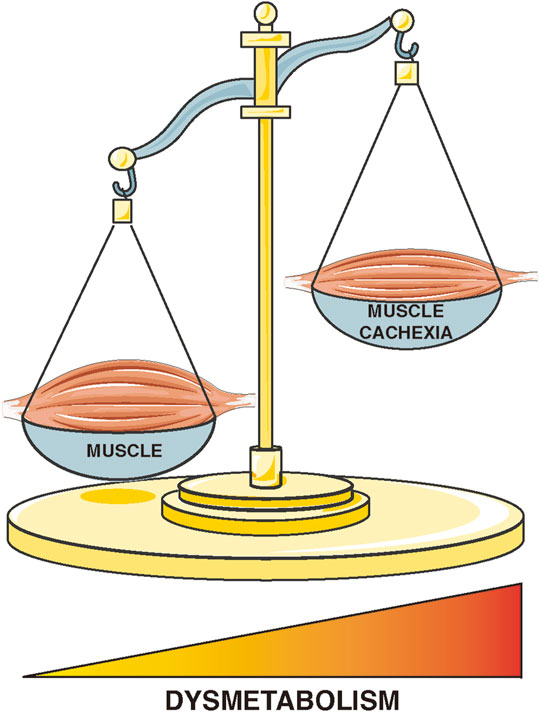
FIGURE 1. Schematic representation of changes in skeletal muscle metabolism in diseases associated with cachexia.
In this Research Topic, we collected four papers, three of which focus on cancer-derived cachexia and examine the role of several mitochondrial targets in influencing the metabolic profile during cancer progression.
In an elegant original article originating from patient samples and functionally interrogated in cultured murine myotubes, Mao et al. demonstrated that cachectic cancer patients exhibit reduced myofiber area, enlarged mitochondria with aberrant morphology and evidence of altered mitochondrial dynamics. Specifically, they observed upregulation of phosphorylated dynamin-related protein 1 (DRP1) at the Ser616 site, associated with markers of increased mitochondrial fission and consequent active fragmentation. The authors examined the relationship between DRP1, muscle degradation, and mitochondria using an in vitro model of cancer cachexia obtained by treating C2C12 myotubes with a conditioned C26 cell medium. They observed that inhibition of mitochondrial fission with Mdivi-1, a specific DRP1 inhibitor, counteracts muscle wasting by reducing protein degradation and improving mitochondrial function. While DRP1 regulates mitochondrial fission under normal physiological conditions, its overexpression in cancer patients with cachexia leads to promote myocellular mitochondrial dysfunction and myotube wasting.
Mitochondrial alterations, as a target for cachexia therapy, are also the main object of original article by Pin et al. The authors examined the effects of Mitoquinone Q (MitoQ), one of the most widely used antioxidants for mitochondria, on skeletal muscle wasting and metabolism in vitro and in vivo. Specifically, they found that MitoQ protects myotubes from atrophy in vitro by preventing increases in Atrogin-1 and Murf1 gene expression. In addition, they described MitoQ as a tool to prevent mitochondrial changes and improve the cachectic phenotype in C26 tumor-bearing mice. Specifically, MitoQ administration partially corrected skeletal muscle atrophy in male CD2F1 mice inoculated with C26 tumor cells. The authors demonstrated that MitoQ is an effective approach to improve mitochondrial function and metabolism by promoting a shift in fiber composition from glycolytic to oxidative, confirming the anticachectic properties of MitoQ in vivo. The authors suggest MitoQ could be administered concomitantly with chemotherapeutic agents routinely used in the clinic to counteract cancer-induced skeletal muscle atrophy. Whether MitoQ would be protective against chemotherapy-induced cachexia in the context of cancer or affect tumor response to chemotherapy remains to be determined in pre-clinical models.
The discovery of novel metabolic biomarkers involved in the onset and progression of cachexia is necessary to develop new therapies to treat patients and improve disease outcomes. In this context, O’Connell et al. have developed an original article in an experimental model, focused on identifying molecular targets of cancer cachexia in the early stages with the goal of preventing refractory phase, which is characterized by patients becoming unresponsive to therapies and exhibiting uncontrolled weight loss. The unique feature of this study is the multiplatform strategy used (NMR, MS, and NMR-based lipoprotein platforms) to profile progressive changes in the metabolome across the time course in C26 tumor-bearing mice. The authors found that the tumor progression induces significant differences in circulating amino acids, acylcarnitines, and lipoproteins prior to evident weight loss. These findings suggest that for patients, specific plasma metabolite biomarkers could serve as diagnostic predictors of cancer cachexia development or progression. Such a validated biomarker panel in patients would greatly facilitate drug development by identifying patients at risk of developing cachexia and monitoring response to therapy.
The original article by Wen et al. addresses potential mechanisms driving the loss of skeletal muscle tissue in patients exposed to long-term controlled mechanical ventilation (CMV) in Intensive Care Units (ICUs). Specifically, CMV results in severe cachectic phenotype with impaired strength and movement, as well as alterations in other important skeletal muscle functions such as secretion of hormones, formation of metabolites, and reserve of amino acids. The authors conducted an in vivo study using Sprague-Dawley rats exposed to CMV for 5 days and then performed a metabolomic analysis of two respiratory muscles (diaphragm and intercostal muscle) and lung tissue. The authors showed a dramatic change in the metabolomic profile of lipids (Acyl Carnitine) and amino acids (Leucine, Isoleucine and Valine) with a specific signature for each tissue associated with increased protein breakdown in the two respiratory muscles, active inflammation in all tissues, attenuated energy production in the muscles, and enhance energy production in the lungs. This provides a pre-clinical basis for future studies in patients and for the ultimate discovery of biomarkers for early diagnosis to prevent the risk of secondary pulmonary complications and mortality.
In conclusion, the articles published in this Research Topic illustrate novel insights and highlight the role of skeletal muscle metabolism as a potential candidate for exploring innovative therapeutic approaches for the treatment of diseases associated with cachexia.
Author Contributions
FC wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Baskin, K. K., Winders, B. R., and Olson, E. N. (2015). Muscle as a "mediator" of Systemic Metabolism. Cell. Metab. 21 (2), 237–248. doi:10.1016/j.cmet.2014.12.021
Evans, W. J. (2010). Skeletal Muscle Loss: Cachexia, Sarcopenia, and Inactivity. Am. J. Clin. Nutr. 91 (4), 1123S–1127S. doi:10.3945/ajcn.2010.28608A
Frontera, W. R., and Ochala, J. (2015). Skeletal Muscle: a Brief Review of Structure and Function. Calcif. Tissue Int. 96 (3), 183–195. doi:10.1007/s00223-014-9915-y
Kim, J., Wang, Z., Heymsfield, S. B., Baumgartner, R. N., and Gallagher, D. (2002). Total-body Skeletal Muscle Mass: Estimation by a New Dual-Energy X-Ray Absorptiometry Method. Am. J. Clin. Nutr. 76 (2), 378–383. doi:10.1093/ajcn/76.2.378
Rohm, M., Zeigerer, A., Machado, J., and Herzig, S. (2019). Energy Metabolism in Cachexia. EMBO Rep. 20 (4), e47258. doi:10.15252/embr.201847258
Keywords: cachexia, skeletal muscle wasting, biomarker, metabolism, mitochondria
Citation: Cirillo F, Zimmers TA and Mangiavini L (2022) Editorial: Metabolic Adaptation of Muscle Tissue in Diseases Associated With Cachexia. Front. Cell Dev. Biol. 10:947902. doi: 10.3389/fcell.2022.947902
Received: 19 May 2022; Accepted: 23 May 2022;
Published: 03 June 2022.
Edited and reviewed by:
Cecilia Giulivi, University of California, Davis, United StatesCopyright © 2022 Cirillo, Zimmers and Mangiavini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Federica Cirillo, ZmVkZXJpY2EuY2lyaWxsb0BncnVwcG9zYW5kb25hdG8uaXQ=
 Federica Cirillo
Federica Cirillo Teresa A. Zimmers
Teresa A. Zimmers Laura Mangiavini
Laura Mangiavini