
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Clin. Diabetes Healthc., 24 February 2023
Sec. Diabetes and Pregnancy
Volume 4 - 2023 | https://doi.org/10.3389/fcdhc.2023.1086186
This article is part of the Research TopicDiabetes Care Reform: Improve Health and Health EquityView all 4 articles
 Amelia J. Lake1,2*
Amelia J. Lake1,2* Amelia Williams1,2
Amelia Williams1,2 Adriana C. H. Neven3
Adriana C. H. Neven3 Jacqueline A. Boyle3,4
Jacqueline A. Boyle3,4 James A. Dunbar5
James A. Dunbar5 Christel Hendrieckx1,2
Christel Hendrieckx1,2 Melinda Morrison6
Melinda Morrison6 Sharleen L. O’Reilly7,8
Sharleen L. O’Reilly7,8 Helena Teede3
Helena Teede3 Jane Speight1,2 on behalf of the ME-MaGDA study group
Jane Speight1,2 on behalf of the ME-MaGDA study groupIntroduction: Women with previous gestational diabetes mellitus (GDM) are at increased risk of type 2 diabetes (T2D). Guidelines recommend postnatal diabetes screening (oral glucose tolerance test or HbA1c) typically 6-12 weeks after birth, with screening maintained at regular intervals thereafter. Despite this, around half of women are not screened, representing a critical missed opportunity for early identification of prediabetes or type 2 diabetes. While policy and practice-level recommendations are comprehensive, those at the personal-level primarily focus on increasing screening knowledge and risk perception, potentially missing other influential behavioral determinants. We aimed to identify modifiable, personal-level factors impacting postpartum type 2 diabetes screening among Australian women with prior gestational diabetes and recommend intervention functions and behavior change techniques to underpin intervention content.
Research design and methods: Semi-structured interviews with participants recruited via Australia’s National Gestational Diabetes Register, using a guide based on the Theoretical Domains Framework (TDF). Using an inductive-deductive approach, we coded data to TDF domains. We used established criteria to identify ‘important’ domains which we then mapped to the Capability, Opportunity, Motivation–Behavior (COM-B) model.
Results: Nineteen women participated: 34 ± 4 years, 19 ± 4 months postpartum, 63% Australian-born, 90% metropolitan, 58% screened for T2D according to guidelines. Eight TDF domains were identified: ‘knowledge’, ‘memory, attention, and decision-making processes’, ‘environmental context and resources’, ‘social influences’, ‘emotion’, ‘beliefs about consequences’, ‘social role and identity’, and ‘beliefs about capabilities’. Study strengths include a methodologically rigorous design; limitations include low recruitment and homogenous sample.
Conclusions: This study identified numerous modifiable barriers and enablers to postpartum T2D screening for women with prior GDM. By mapping to the COM-B, we identified intervention functions and behavior change techniques to underpin intervention content. These findings provide a valuable evidence base for developing messaging and interventions that target the behavioral determinants most likely to optimize T2D screening uptake among women with prior GDM.
Gestational diabetes mellitus (GDM) affects approximately 13% of births worldwide, and is acknowledged as “the fastest growing type of diabetes in Australia” (1, 2). Women with prior GDM have an eight-fold increased lifetime risk of type 2 diabetes (T2D) compared to women with normoglycemic pregnancies (3). Early and regular postpartum T2D screening is essential as undiagnosed and persistent elevated blood glucose levels (hyperglycaemia) increases risk for adverse health outcomes (4). Australian guidelines recommend T2D screening (currently via an Oral Glucose Tolerance Test or OGTT), 6-12 weeks postpartum and, every 1-3 years thereafter (5). Despite the benefits, only 43-58% of women in Australia complete the OGTT (6), reflecting screening rates worldwide (7, 8).
National and international studies have highlighted that policy, practice, and personal-level factors contribute to low screening uptake. Common policy-level factors include limitations related to public healthcare and lack of consensus on screening guidelines (9). Practice-level factors include healthcare silos, lack of focus on ongoing risk in consultations, and lack of reminder systems (9–11). Systematic reviews of qualitative studies have identified common personal-level screening barriers, including competing demands, lack of practical social support, challenges related to the screening procedure, lack of knowledge and absence of advice from health professionals (12–14). Similar findings are reflected in an Australian context (15–21).
Recommendations to increase screening uptake have primarily focused on initiatives at policy and practice-levels including information provision and reminders (12–14). The limitations of such approaches have been acknowledged (6, 22–24). A key element of best practice personal-level intervention development is explicit use of theoretical approaches to both identify behavioral determinants and targeting them via intervention content underpinned by behavior change techniques (25, 26). To date, there has been a paucity of such research. Thus, in-depth exploration of personal-level behavioral factors influencing women’s screening is warranted, to develop recommendations for persuasive messaging grounded in health behavior change theory.
The Theoretical Domains Framework (TDF) is an example of a theoretical approach to identifying determinants of a defined behaviour. The TDF comprises 14 behavior change domains derived from 33 behavior change theories (27). The TDF has been used to identify determinants of health behaviors, including among women with GDM (28).
The TDF maps to the multi-layered Behavior Change Wheel (BCW, Figure 1) (29). The BCW is an eight-step intervention development framework grounded in behavioural science. The framework has been used widely, including to address barriers to diabetes self-management (30). Adjacent to the TDF layer, and at the core of the BCW, is the Capability, Opportunity, Motivation-Behavior (COM-B) model which posits that behavior is an interaction between Capability (physical and psychological), Opportunity (physical and social) and Motivation (reflective and automatic processes). The COM-B and TDF are encircled by nine intervention functions: persuasion, incentivization, environmental restructuring, education, coercion, enablement, modelling, training, and restrictions. The nine functions and 14 TDF domains are linked to established behavior change techniques, defined as “active components of an intervention designed to change behavior” (29, 31).
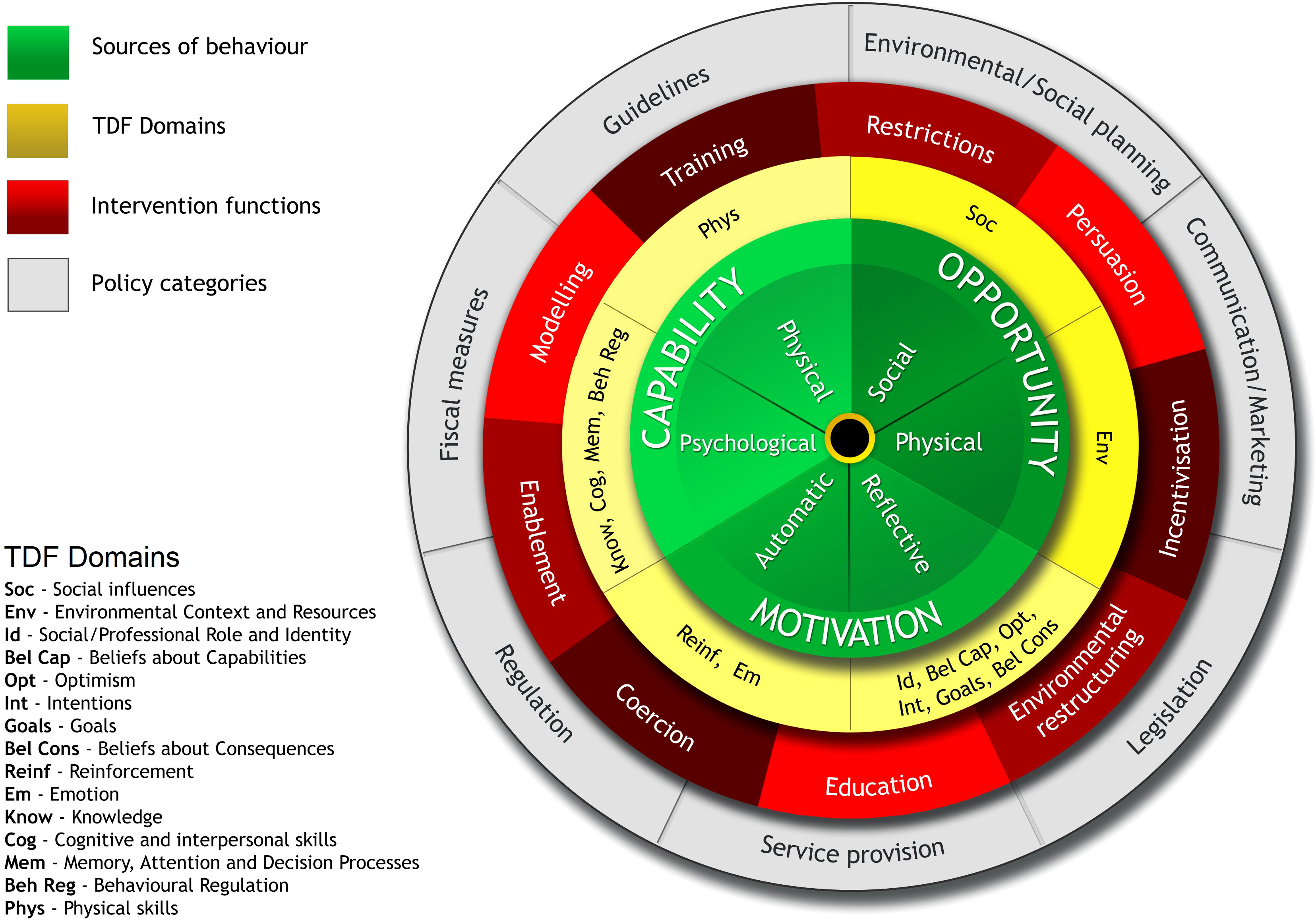
Figure 1 Behavior Change Wheel (reproduced with permission) (29).
While the BCW and COM-B/TDF components have demonstrated utility in identifying factors impacting health lifestyle behaviors (32, 33), to date, no studies have utilised it specifically to explore, in-depth, determinants of uptake of T2D screening among women with previous GDM. The aims of this study were to i) apply the BCW theoretical approach to identify modifiable barriers to, and enablers of, T2D screening among Australian women with prior GDM and ii) recommend intervention functions and behavior change techniques to underpin personal-level intervention messaging to optimise postpartum T2D screening uptake.
We conducted in-depth, semi-structured interviews. Ethics approval was provided by Deakin University Human Research Ethics Committee (HEAG-H 09_2020). This study is reported according to COnsolidated criteria for REporting Qualitative research (COREQ) and Standards for Reporting Qualitative Research (SRQR, Supplemental Materials S1-S2) (34, 35).
Two female researchers, both experienced in (health) psychology and qualitative research, engaged with study participants: AL is a postdoctoral research fellow, and AW is a postgraduate research assistant. They had no relationship with participants outside the study and no involvement in their clinical care. To enhance reflexivity, the interviewer (AL) completed a reflective journal with each interview, exploring perceptions, assumptions, and subjectivities.
All participants were registered on the National Diabetes Services Scheme (NDSS) National Gestational Diabetes Register (NGDR). The NDSS is an initiative of the Australian Government administered by Diabetes Australia. The NDSS coordinated invitations to 953 NGDR registrants via email (July 2020; reminder September). Eligibility criteria included: age 18-50 years, consent to being contacted for research purposes, 12-24 months postpartum, and English speaking. Participants registered interest via email and were telephoned by the researchers to discuss the study and schedule an interview.
We developed a semi-structured interview guide based on the TDF domains (Supplemental Materials S3). The guide was pilot tested with a volunteer who had prior GDM, and minor modifications were made. In response to the COVID-19 pandemic, a question was added to invite opinions on home-based alternatives to the 6–12-week OGTT.
All participants received a cover letter, plain language statement and a consent form, which they completed prior to interview (Supplemental Materials S4). Interviews were conducted by AL, via Zoom or telephone, from July to October 2020. Following recommendations for theory-based qualitative research, we set an a priori minimum sample target of N=10. At 15 interviews, we considered no new information was forthcoming (36), and conducted four additional interviews as confirmation. Each participant received an AUD$30 e-voucher and was invited to review the transcript of their interview.
All interviews were audio-recorded, de-identified and transcribed professionally. Transcripts and participant details were stored digitally in password-protected files. We analysed data using NVivo (released in March 2020) (37).
We developed a coding framework using an inductive-deductive model to avoid ‘rigid operationalisation’ of the TDF (38). Using an inductive approach, two researchers (AL, AW) generated theme labels for similar clusters of data. We developed theme definitions in consultation with co-authors. For the deductive element, we categorised themes into domains using a TDF-based coding manual, which contained clear statements about how the inductively generated themes would be categorised within the TDF (Supplemental Materials S5). We updated the coding framework and manual iteratively during data collection, practising reflexivity throughout (39).
After data familiarisation, two researchers (AL, AW) jointly coded one transcript. Using the manual, we coded all text relevant to the target behavior into its corresponding TDF domain, and again as a barrier or enabler. Following this, both researchers coded two (10%) transcripts independently. Inter-rater reliability was calculated using the NVivo coding comparison function (Kappa coefficient=0.73, 99% agreement). Coding differences were discussed and considered within the broader contextual meaning. Following this, one researcher (AW) coded remaining transcripts with queries addressed in consultation with co-authors. Participant responses about preferences for resource and reminders formats, and home-based alternatives to the postpartum OGTT were excluded from the main analysis but are available in Supplemental Materials (S6).
We used three established criteria to identify TDF domains of ‘high importance’: frequency (total number of codes to a TDF domain), presence of conflicting beliefs/themes, and evidence of themes likely to influence behavior (39). Responses to ‘important’ TDF domains are reported below, responses to remaining TDF domains are reported in Supplemental Materials (S7).
Using the BCW (Figure 1), we developed a conceptual model linking qualitative data (synthesised into the TDF domains of ‘high importance’ and mapped to COM-B elements) to intervention functions (29). We then used established procedure and taxonomies to make recommendations on behavior change techniques to underpin intervention content (29, 31).
Twenty-one women (2%) registered interest; 19 were interviewed, two were uncontactable. Participants were (mean+SD): 34 ± 4 years, 19 ± 4 months post-partum. Most had completed OGTT within guidelines (58%), were Australian born (63%) and resided in metropolitan areas (90%), Table 1. Average interview duration was 41 minutes (range: 26-59). All participants reviewed and approved their transcripts; no changes were requested.
Themes were coded to 13 of the 14 TDF domains. Eight domains were represented in at least two of the three importance criteria and assessed as ‘high’ importance (Table 2). The eight important TDF domains are described below and in Table 3.
All participants were aware of the association between GDM and T2D and understood that the purpose of postpartum screening was “…to make sure it [GDM] disappeared” (ID11). Women who understood that GDM increases the risk of developing T2D generally assigned greater importance to screening: “I’m higher risk … I have gone and done the follow-up testing” (ID10). Some noted that knowledge of the OGTT procedure and requirements acquired at GDM diagnosis was helpful as “…you know what to expect” (ID05).
Women’s knowledge of ongoing screening requirements was low: “It hadn’t registered that it was a yearly thing” (ID04) and “It’s just one blood test you have to take, is it?” (ID12). Relatedly, lack of knowledge of immediate and ongoing T2D risk translated into confusion about the rationale for regular follow-up: “I thought once I had the – the six week one, I’d be in the all-clear” (ID14).
Women described the impact of cognitive overload associated with the demands of managing life with a baby: “I don’t think I actively decided against it [OGTT], it was just … a bit too hard” (ID01). Women also had difficulty maintaining attention to ongoing risk and screening requirements: “I put it out of my mind for a little bit … and then I forgot” (ID11). Relatedly, the asymptomatic nature of T2D meant that it was “easy to … forget when you have no symptoms” (ID01). Conversely, screening reminders were unanimously valued “my trigger to get it done” (ID03) and prompted attention to ongoing risk: “this is something you should still check-up on” (ID13).
Competing demands. Women often described how personal circumstances reduced opportunity to schedule “A time around their [newborn] chaotic routine” (ID08). This was just one of multiple competing demands the women faced: “I don’t feel like I’ve got any time ever to do things that I need to do” (ID13).
Screening requirements and environment. Women expressed that the requirements, timing, and duration of screening were impractical: “…you have to sit around for at least two hours, and it was just not very possible with the newborn” (ID01). For some, seeking alternate care for their newborn was undesirable: “… it’s not very practical … for a mum to leave the baby for that long” (ID03). Lack of child and nursing-friendly facilities and extended waiting times exacerbated these challenges: “…there’s just nowhere nice to sit and breastfeed and it was dusty” (ID08). Unique to the context of the COVID-19 pandemic were concerns about physical safety during the screening visit: “I don’t want to sit in a hospital around sick people for three hours … and especially now with all this Coronavirus, I definitely wouldn’t do it” (ID02).
Education and resources. Antenatal education was a key enabler to understanding T2D risk and importance of postpartum screening: “…in the first education session, they drilled it into us just to make sure you go” (ID04). For some, print-based resources reinforced learnings. Conversely, some noted reduction of “information after having the baby” (ID10), while others perceived that screening information was buried within an excess of “…piles of paperwork” (ID15).
Social support. Availability of practical support for the logistics of screening reduced the strain of competing demands: “I have a very supportive husband … he made sure that he was helpful with the other kids so that I could get to the appointment” (ID10). Family and friends were a powerful influence on women’s screening decisions: “… if they’re concerned about me or are trying to support me in trying to do something for my own health then I certainly respect that and listen to them” (ID16).
Communication with health professionals. Health professionals were regarded as a trusted and valuable source of information: “…they know your health status … if your GP calls you and tells you to do something, you generally do it” (ID14). Continuity of care reinforced the value placed on advice: “I already had that trusting relationship with them, and they knew my history … I was comfortable in her expertise in the condition” (ID14). While most women were informed about their T2D risk, few were advised about ongoing screening requirements: “She [GP] didn’t tell me” (ID02).
Social comparison. Knowing that other women attended screening was an enabler. For example, one participant identified closely with an online blogger who had been diagnosed with T2D after GDM, and whose narrative reinforced the importance of screening: “I had it in the back of my mind that she had developed it … I’m sure that probably had a subconscious role to play” (ID03).
Fear/anxiety. Some participants fear of T2D diagnosis impacted screening behavior: “I was worried that I would have it” (ID04). Often, this arose from perceiving T2D management as analogous to the “…regimented living style” (ID06) experienced during GDM. While fear was a clear barrier, a sense of relief and “peace of mind” (ID01) encouraged women “to keep getting the checks done” (ID21). Conversely, for a minority, an appropriate level of concern motivated screening attendance: “I was nervous that I might still have it … I wanted to get it done” (ID16). Some participants feared “needles” (ID12) or had misconceptions about potential harm: “…I felt the sugar flushed in my blood … you always worry about whether your body will react properly” (ID09).
Postpartum abandonment. Participants described disappointment about the rapid reduction of support after birth which greatly contrasted with experiences during pregnancy: “…the support that we received was fantastic … the minute the baby was born it, sort of, stopped” (ID16). Some described postpartum care as highly infant-focused: “I did leave that session thinking, ‘Great. My baby’s happy and healthy.’ But, for me it was, like, two questions and done” (ID04). Participants noted the need for ongoing support to prioritise their health: “reinforcing you are as important as your baby” (ID12).
Perceived necessity. Believing that T2D screening is important for future health was a powerful enabler: “for my own body’s sake, it was the right thing to do” (ID04). Conversely, lack of symptoms and “feeling okay” (ID06) reduced perceived necessity: “I don’t feel any different from before I was pregnant, so it’s not of real urgency for me” (ID02). Perceiving GDM as transient meant screening was “less of a priority” (ID01) for some. Annual screening was sometimes perceived as unnecessary if the women had received a negative OGTT result “…it’ll be fine” (ID08) or were planning another pregnancy: “… they’ll screen me when I get pregnant again” (ID13).
Consequences of screening. Screening benefits typically outweighed costs. Knowing one’s health status was an enabler for some: “It’s important for women to be aware of what’s going on in their bodies, so the screening is really helpful” (ID10), but not all: “I’m not prepared to know” (ID06). For some, the appointment provided opportunity for personal time in the early postpartum period: “being able to just sit and have some time out to read a book was actually pleasant” (ID21). Most described minimal negative consequences: “It wasn’t really anything too onerous, except for a couple of hours to sit around and wait, which didn’t bother me” (ID04).
Anticipated outcome. For some, the possibility of undiagnosed diabetes was a motivator: “…it could be worse if I wasn’t tested regularly” (ID05). For others, anticipating that they may already have T2D was a barrier: “…it could be too late” (ID06). Expectation of a negative OGTT result was an enabler: “I knew it was going to be a normal test, so I wasn’t anxious” (ID01).
Social identity and motherhood role expectations were both barriers and enablers. Some women described that they “prioritise [their child’s] health over [their] own health” (ID12). For others, being a mother motivated them to screen: “…to be a good mum … you need to make sure that you’re also looking after yourself” (ID21).
Perceived competence. For some, compensatory strategies such as continuing to self-monitor blood glucose or engaging in healthy habits reduced the perceived necessity of screening: “…I haven’t had a test yet, but I’ve pricked myself a few times and it’s always been normal” (ID02). A minority believed that they would recognize symptoms of T2D: “I can read my body pretty well … if everything felt fine I probably wouldn’t [screen]” (ID13).
Perceived ability to manage T2D risk. Believing that T2D can be prevented, delayed, or managed influenced willingness to screen. High self-efficacy (i.e., belief in capability to manage risk or T2D) appeared to foster a sense of agency and reduce apprehension related to screening: “I feel like it’s within my control to a certain extent” (ID05). Conversely, one participant reported that low confidence in making diet and lifestyle change led to avoidance of screening: “I haven’t learned a different way of how to deal with stress aside from eating” (ID06).
We identified five intervention functions (education, environmental restructuring, enablement, persuasion, modelling) and 12 behavior change techniques to address the eight ‘important’ TDF domains (29). We illustrate the linkages from evidence (synthesised into TDF domains) to intervention components (functions and behavior change techniques) in Figure 2.
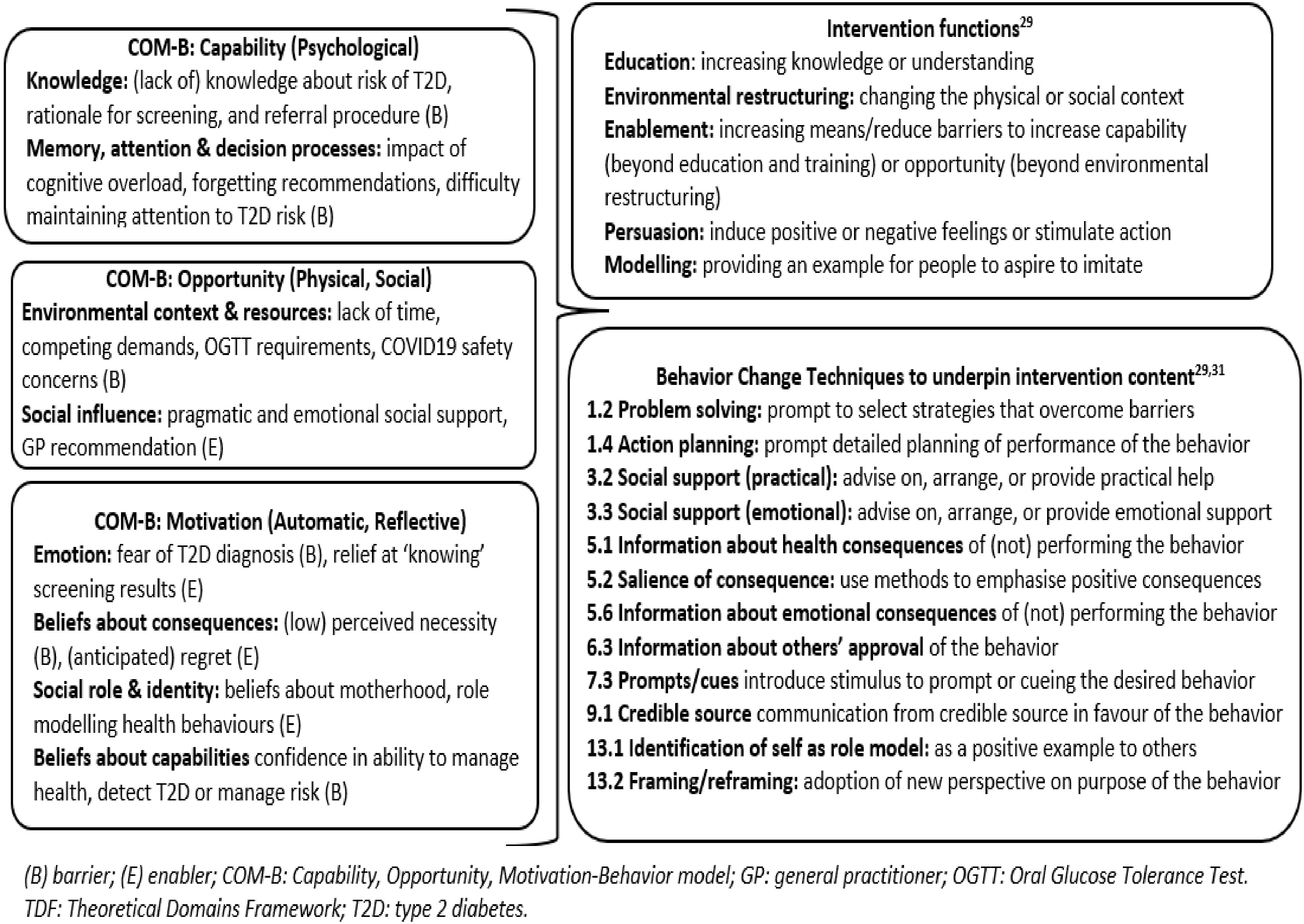
Figure 2 TDF domains/COM-B components linked to intervention functions and behavior change techniques.
Using a methodology grounded in behavior change theory, we identified multiple modifiable determinants of T2D screening uptake among Australian women with prior GDM. Eight ‘high’ importance TDF domains, mapped onto the COM-B model, provide an evidence base for future messaging development and intervention targets.
Participants had high awareness of T2D risk and the rationale for screening, consistent with prior Australian studies (16, 18, 19, 21). Linkages between TDF domains provide context for this finding. Knowledge was acquired via health professional advice (‘social influences’) and education/resources (‘environmental context & resources’). Despite this knowledge, some participants reported a missed or delayed OGTT, emphasising the need for messaging that targets additional psychosocial factors.
Knowledge related to ongoing T2D screening and risk appears to be lacking, as evidenced by confusion about frequency, test type and rationale for periodic screening. This was likely influenced by the temporary suspension of NGDR annual reminders in response to changes to guidelines (40) for postpartum testing during the COVID-19 pandemic. However, uptake in Australia is typically low (6). Our findings suggest that this reflects cognitive overload due to fatigue and parenting demands, and a disproportionate emphasis on the onerous 6-12-week OGTT, whereas future follow-up is the simpler fasting glucose or HbA1c (4, 12–14). Two distinguishing screening enablers were maternal identity and social-emotional support. These novel findings suggest that addressing stereotypical norms and beliefs about maternal role and providing emotional support may be effective in motivating screening uptake.
Previous research has recommended the use of system-based or local reminders, as forgetting is a common barrier to screening (12). This was not identified in the present study. While our findings contrast with prior Australian qualitative research (15, 18), they may reflect system-based improvements in the NGDR and high registration rate (6). Prior research has indicated that NGDR reminders are not effective in promoting screening uptake (6, 22). Our research confirms that women value reminders and there is scope to incorporate messages targeting the psychosocial barriers and enablers identified in this study.
Competing demands and screening-related challenges were key personal-level barriers in this and other studies (14). Prior recommendations suggest altering the physical environment to be more ‘baby friendly’ (12). Women’s expressed concerns regarding physical safety in the context of the COVID-19 pandemic challenge this recommendation; supported by findings from a recent Danish study (41). Instead, clinician support and encouraging women to seek practical social support (a key enabler in overcoming situational and contextual barriers) may be more pragmatic (26).
Concordant with prior research, women often prioritised their child’s needs over their own health (14). Reduced healthcare information and support postpartum (‘postpartum abandonment’) was disempowering and served to confirm women’s perceptions of their own health being less important, an issue identified in a recent scoping review (26).
Fear of T2D diagnosis was the most frequently reported motivational barrier, and often related to extrapolation of prior experience of GDM management to future diabetes management. Fear is a widely identified emotion in health behavior change research, including for postpartum diabetes screening (14). While appropriate concern is a necessary component of risk perception, fear is unlikely to promote behavior change, particularly in the absence of self-efficacy and response efficacy (i.e., a person’s belief that changing their behavior will reduce risk) (42). The present findings align with this behavioral pathway. For example, key enablers were understanding personal risk and perceiving screening as an important health behavior that may mitigate potential adverse health consequences (high response efficacy). Conversely, barriers included low, or distal representations of personal risk and lack of perceived benefit, or necessity, of screening (low response efficacy). Similar findings, reported elsewhere, suggest that addressing beliefs and perceived personal risk is essential in increasing T2D screening uptake (12–14).
Relatedly, a major screening barrier for some women was perceived competence in managing their own health, mostly among those who had delayed or not attended screening. Misplaced beliefs in their own capability to recognize T2D symptoms reduced the priority women assigned to formal screening (14). Previous research noted use of compensatory strategies (e.g. self-testing) in-lieu of formal screening (14). Finally, while home-based alternatives to formal OGTT may be attractive and viable options in future (43), further research is needed to establish their feasibility and effectiveness, given the concerns raised by the women in this study. Collectively, these findings indicate the need for education to address misconceptions about the ability to recognize T2D symptoms, and the rationale for timely, formal screening and ongoing surveillance.
These findings suggest the potentially important role of self-efficacy in screening uptake. Low self-efficacy, regarding personal capability to prevent or manage T2D, negatively impacted willingness to screen, which has been noted in only two other Australian studies (15, 21). Uniquely, our study also shows the positive influence of self-efficacy, which has not been previously reported. This novel finding aligns with research proposing the mediating relationship between fear and self-efficacy and suggests the potential value of increasing self-efficacy through empowerment-based messaging to increase screening uptake (42).
Prior recommendations to increase screening uptake typically targeted knowledge (12, 13). While an important prerequisite, our findings suggest that ‘Knowledge’ is already broadly addressed by existing educational policies in an Australian context. However, screening prompts and reminders provided by Australia’s National Gestational Diabetes Register could be improved by review to ensure that the messaging both addresses the determinants identified in this study and is underpinned by the recommended behaviour change techniques. Most of the modifiable determinants of T2D screening uptake relate to the Opportunity and Motivation elements of the COM-B model. Therefore, screening uptake is most likely to be improved by timely (44), person-centred messaging that addresses opportunistic barriers (e.g., competing demands and elements of the screening procedure), motivational factors (e.g., emotions, beliefs, self-efficacy, maternal identity).
A further consideration for policymakers is the current reliance on the 6–12-week OGTT, which is a barrier to screening and could be replaced with a simpler fasting glucose, HbA1c or home-based alternatives. This would require further research to establish their feasibility and effectiveness. Finally, the women’s concerns about postpartum abandonment suggest that greater consideration needs to be given to ensuring appropriate handovers from tertiary to primary care, and continued support during this time.
We have identified behavior change techniques to underpin psychoeducational messaging (Figure 2). These techniques can be extrapolated for use in the clinical context. For example, clinicians could promote screening uptake through providing accurate and timely information about T2D risk, the rationale and positive health consequences of screening. It is important that clinicians use a gain-framed approach to emphasize the potential positive outcomes of screening such as reassurance if screening is negative and the ability to access timely and effective treatments if screening is positive. Clinicians are well placed to arrange or address practical or emotional support to overcome the unique barriers that the woman may be experiencing. Further, clinicians can frame screening as an important role modelling behavior which is of direct benefit to the health and wellbeing of the family (44). Specific communication points for clinicians are reported in a recent systematic review published by our research team (14).
This study was limited by the homogenous sample: most participants reported having attended the postpartum OGTT (some overdue). Participation rate was low, and recruitment coincided with the onset of the COVID-19 pandemic, suggesting that those who participated were highly engaged. All participants were fluent English speakers, and most lived in metropolitan areas and had strong social networks. Further, the generalizability to Indigenous women and culturally and linguistically diverse populations is limited by the predominantly Anglo-Australian participants. Recognising the inherent limitations of representativeness (45), our findings provide valuable insight into enabling factors and strategies to overcome screening barriers.
A key strength is the study design, underscored by explicit use of theoretical approach and intervention development frameworks (25). Data collection was optimised by piloting the interview schedule and including follow-up prompts to promote in-depth exploration (39). Several strategies were implemented to enhance the trustworthiness of the data, including participant checking, reflective journals, audit trails and involvement of multiple researchers at each stage of the analysis (34, 35).
Next steps involve developing discrete, person-centered psycho-educational messages for implementation within the national register and other delivery approaches. We have proposed behavior change techniques to underpin the messaging (Figure 2) although others shown to be associated with significant improvements in diabetes self-management (e.g., goal setting) (46) should also be considered.
Finally, further research is needed to establish the unique behavioral determinants of screening among women from culturally diverse and minority backgrounds. Indigenous, Chinese, and non-English speaking women are at greater risk of T2D than women of White European ethnicity. Given that the former experience unique barriers to T2D prevention and screening (3, 47, 48) this needs to be a priority area for future research (48).
This study identified numerous modifiable barriers and enablers to postpartum T2D screening for women with prior GDM. By mapping to the BCW, we identified intervention functions and behavior change techniques to underpin intervention content. These findings provide a valuable evidence base for developing messaging and interventions that target the behavioral determinants most likely to optimise T2D screening uptake among women with prior GDM.
NVivo (RRID : SCR_014802).
Additional detail about the datasets analyzed for this study can be found in supplemental materials. The data generated and analyzed during the current study are not publicly available due to restrictions on sharing qualitative data. Requests to access the datasets should be directed to Dr Amelia J Lake (E:YWxha2VAYWNicmQub3JnLmF1).
The studies involving human participants were reviewed and approved by Deakin University Human Research Ethics Committee (HEAG-H 09_2020). The participants provided their written informed consent to take part in this study.
AL designed the interview guide and TDF-based coding manual in consultation from co-authors. AL conducted all interviews. AL and AW coded, analysed and interpreted data and prepared the manuscript with input, review, and approval from all co-authors. All authors contributed to the article and approved the submitted version.
This project was funded by the Australian Government Department of Health (Health/18/1904983). CH and JS are supported by the core funding to the Australian Centre for Behavioral Research in Diabetes provided by the collaboration between Diabetes Victoria and Deakin University. HT is supported by an NHMRC fellowship.
The authors would like to thank the women who participated in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The views expressed in the submitted article are our own and not an official position of the institutions or funding body.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcdhc.2023.1086186/full#supplementary-material
BCW, Behavior Change Wheel; COM-B, Capability, Opportunity, Motivation-Behavior model; GDM, Gestational Diabetes Mellitus; NDSS, National Diabetes Services Scheme; NGDR, National Gestational Diabetes Register; OGTT, Oral Glucose Tolerance Test; TDF, Theoretical Domains Framework; T2D, Type 2 diabetes.
1. International Diabetes Federation IDF diabetes atlas (10th edition) 2021 . Available at: http://www.diabetesatlas.org/.
2. Diabetes Australia Position statement: Gestational diabetes in Australia 2020 . Available at: https://www.diabetesaustralia.com.au/wp-content/uploads/Gestational-Diabetes-in-Australia-Position-Statement-2020.pdf.
3. Dennison RA, Chen ES, Green ME, Legard C, Kotecha D, Farmer G, et al. The absolute and relative risk of type 2 diabetes after gestational diabetes: A systematic review and meta-analysis of 129 studies. Diabetes Res. Clin. Practice. (2021) 171. doi: 10.1016/j.diabres.2020.108625
4. Zhang M, Zhou Y, Zhong J, Wang K, Ding Y, Li L. Current guidelines on the management of gestational diabetes mellitus: a content analysis and appraisal. BMC Pregnancy Childbirth (2019) 19(1):200. doi: 10.1186/s12884-019-2343-2
5. Nankervis A, McIntyre HD, Moses R, Ross GP, Callaway L, Porter C, et al. ADIPS consensus guidelines for the testing and diagnosis of hyperglycaemia in pregnancy in Australia and new Zealand 2014 . Available at: https://www.adips.org/downloads/2014ADIPSGDMGuidelinesV18.11.2014_000.pdf.
6. Boyle DIR, Versace VL, Dunbar JA, Scheil W, Janus E, Oats JJN, et al. Results of the first recorded evaluation of a national gestational diabetes mellitus register: Challenges in screening, registration, and follow-up for diabetes risk. PloS One (2018) 13(8):e0200832. doi: 10.1371/journal.pone.0200832
7. Linnenkamp U, Greiner GG, Haastert B, Adamczewski H, Kaltheuner M, Weber D, et al. Postpartum screening of women with GDM in specialised practices: Data from 12,991 women in the GestDiab register. Diabetic Med. (2022) 39(7):e14861. doi: 10.1111/dme.14861
8. Tovar A, Chasan-Taber L, Eggleston E, Oken E. Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev. Chronic Dis. (2011) 8(6):A124.
9. Nielsen KK, Kapur A, Damm P, de Courten M, Bygbjerg IC. From screening to postpartum follow-up - the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth. (2014) 14:41. doi: 10.1186/1471-2393-14-41
10. Lithgow GE, Rossi J, Griffin SJ, Usher-Smith JA, Dennison RA. Barriers to postpartum diabetes screening: a qualitative synthesis of clinicians' views. Br. J. Gen. Pract. (2021) 71(707):e473–e82. doi: 10.3399/bjgp.2020.0928
11. Nielsen JH, Melendez-Torres GJ, Rotevatn TA, Peven K, Fonager K, Overgaard C. How do reminder systems in follow-up screening for women with previous gestational diabetes work? - a realist review. BMC Health Serv. Res. (2021) 21(1):535. doi: 10.1186/s12913-021-06569-z
12. Dennison RA, Fox RA, Ward RJ, Griffin SJ, Usher-Smith JA. Women's views on screening for type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for increasing uptake. Diabetes Med. (2020) 37(1):29–43. doi: 10.1111/dme.14081
13. Sanderson H, Loveman E, Colquitt J, Royle P, Waugh N, Tan BK. Improving uptake of postnatal checking of blood glucose in women who had gestational diabetes mellitus in universal healthcare settings: A systematic review. J. Clin. Med. (2019) 8(1). doi: 10.3390/jcm8010004
14. Lake AJ, Neven ACH, Williams A, O'Reilly SL, Hendrieckx C, Morrison M, et al. Barriers to and enablers of type 2 diabetes screening among women with prior gestational diabetes: a systematic review update and qualitative synthesis applying the theoretical domains framework. Diabetic Med. J. Br. Diabetic Assoc. (2021) 39(4):e14772. doi: 10.1111/dme.14772
15. Campbell S, Roux N, Preece C, Rafter E, Davis B, Mein J, et al. Paths to improving care of Australian aboriginal and Torres strait islander women following gestational diabetes. Prim Health Care Res. Dev. (2017) 18(6):549–62. doi: 10.1017/s1463423617000305
16. Kilgour C, Bogossian FE, Callaway L, Gallois C. Postnatal gestational diabetes mellitus follow-up: Australian women's experiences. Women Birth. (2015) 28(4):285–92. doi: 10.1016/j.wombi.2015.06.004
17. Morrison MK, Lowe JM, Collins CE. Australian Women's experiences of living with gestational diabetes. Women Birth. (2014) 27(1):52–7. doi: 10.1016/j.wombi.2013.10.001
18. Zulfiqar T, Lithander FE, Banwell C, Young R, Boisseau L, Ingle M, et al. Barriers to a healthy lifestyle post gestational-diabetes: An Australian qualitative study. Women Birth. (2017) 30(4):319–24. doi: 10.1016/j.wombi.2016.12.003
19. Pennington AVR, O'Reilly SL, Young D, Dunbar JA. Improving follow-up care for women with a history of gestational diabetes: perspectives of GPs and patients. Aust. J. Prim Health (2017) 23(1):66–74. doi: 10.1071/py15177
20. Sterne V, Logan T, Palmer M. Factors affecting attendance at postpartum diabetes screening in women with gestational diabetes mellitus. Pract. Diabetes Int. (2011) 28(2):64–8. doi: 10.1002/pdi.1559
21. Bandyopadhyay M. Attendance for postpartum glucose tolerance testing following gestational diabetes among south Asian women in Australia: A qualitative study. J. Women’s Health Issues Care (2015) 4(1). doi: 10.4172/2325-9795.1000178
22. O'Reilly SL, Versace VL, Skinner TC, Dunbar JA, Group tMS. Women's engagement with diabetes prevention activities and the influence of contact by the Australian national gestational diabetes register. Pract. Diabetes. (2021) 38(3):14–9b. doi: 10.1002/pdi.2336
23. Brown SD, Hedderson MM, Zhu YY, Tsai AL, Feng JR, Quesenberry CP, et al. Uptake of guideline-recommended postpartum diabetes screening among diverse women with gestational diabetes: associations with patient factors in an integrated health system in USA. BMJ Open Diabetes Res. Care (2022) 10(3). doi: 10.1136/bmjdrc-2021-002726
24. Hewage SS, Aw S, Chi C, Yoong J. Factors associated with intended postpartum OGTT uptake and willingness to receive preventive behavior support to reduce type 2 diabetes risk among women with gestational diabetes in Singapore: An exploratory study. Nutr. Metab. Insights (2021) 14:11786388211016827. doi: 10.1177/11786388211016827
25. O'Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open (2019) 9(8):e029954. doi: 10.1136/bmjopen-2019-029954
26. Pham S, Churruca K, Ellis LA, Braithwaite J. A scoping review of gestational diabetes mellitus healthcare: experiences of care reported by pregnant women internationally. BMC Pregnancy Childbirth. (2022) 22(1). doi: 10.1186/s12884-022-04931-5
27. Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science. (2012) 7(1):37. doi: 10.1186/1748-5908-7-37
28. Martis R, Brown J, McAra-Couper J, Crowther CA. Enablers and barriers for women with gestational diabetes mellitus to achieve optimal glycaemic control - a qualitative study using the theoretical domains framework. BMC Pregnancy Childbirth. (2018) 18(1):91. doi: 10.1186/s12884-018-1710-8
29. Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. United Kingdom: Silverback Publishing (2014).
30. McGuigan K, Hill A, McCay D, O’Kane M, Coates V. Overcoming barriers to injectable therapies: Development of the ORBIT intervention within a behavioural change framework. Front. Clin. Diabetes Healthcare. (2021) 2:792634. doi: 10.3389/fcdhc.2021.792634
32. Boyd J, McMillan B, Easton K, Delaney B, Mitchell C. Utility of the COM-b model in identifying facilitators and barriers to maintaining a healthy postnatal lifestyle following a diagnosis of gestational diabetes: a qualitative study. BMJ Open (2020) 10(8):e037318. doi: 10.1136/bmjopen-2020-037318
33. Muhwava LS, Murphy K, Zarowsky C, Levitt N. Experiences of lifestyle change among women with gestational diabetes mellitus (GDM): A behavioural diagnosis using the COM-b model in a low-income setting. PloS One (2019) 14(11):e0225431. doi: 10.1371/journal.pone.0225431
34. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care (2007) 19(6):349–57. doi: 10.1093/intqhc/mzm042
35. O'Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad. Med. (2014) 89(9):1245–51. doi: 10.1097/acm.0000000000000388
36. Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. What is an adequate sample size? operationalising data saturation for theory-based interview studies. Psychol. Health (2010) 25(10):1229–45. doi: 10.1080/08870440903194015
37. NVivo . Available at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home.
38. McGowan LJ, Powell R, French DP. How can use of the theoretical domains framework be optimized in qualitative research? a rapid systematic review. Br. J. Health Psychol. (2020) 25(3):677–94. doi: 10.1111/bjhp.12437
39. Atkins L, Francis J, Islam R, O'Connor D, Patey A, Ivers N, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implementation Science. (2017) 12:1–18. doi: 10.1186/s13012-017-0605-9
40. Australasian Diabetes in Pregnancy Society (ADIPS), Australian Diabetes Society (ADS), Australian Diabetes Educators Association (ADEA), Diabetes Australia (DA). Diagnostic testing for gestational diabetes mellitus (GDM) during the COVID-19 pandemic: Antenatal and postnatal testing advice. (2020).
41. Jensen NH, Nielsen KK, Dahl-Petersen IK, Maindal HT. The experience of women with recent gestational diabetes during the COVID-19 lockdown: a qualitative study from Denmark. BMC Pregnancy Childbirth. (2022) 22(1). doi: 10.1186/s12884-022-04424-5
42. French DP, Cameron E, Benton JS, Deaton C, Harvie M. Can communicating personalised disease risk promote healthy behaviour change? a systematic review of systematic reviews. Ann. Behav. Med. (2017) 51(5):718–29. doi: 10.1007/s12160-017-9895-z
43. Dunseath GJ, Bright D, Jones C, Dowrick S, Cheung WY, Luzio SD. Performance evaluation of a self-administered home oral glucose tolerance test kit in a controlled clinical research setting. Diabetic Med. J. Br. Diabetic Assoc. (2019) 36(7):862–7. doi: 10.1111/dme.13961
44. Brown JA, Leonard M, Clinton T, Bower JK, Gillespie SL, Fareed N, et al. Mothers' perspectives on a Mother/Infant dyad postpartum primary care program following gestational diabetes mellitus: A qualitative pilot study. Sci. Diabetes Self Manag Care (2022) 48(4):247–57. doi: 10.1177/26350106221100539
45. Yardley L. Dilemmas in qualitative health research. Psychology & Health (2007) 15(2):215–228. doi: 10.1080/08870440008400302
46. Upsher R, Onabajo D, Stahl D, Ismail K, Winkley K. The effectiveness of behavior change techniques underpinning psychological interventions to improve glycemic levels for adults with type 2 diabetes: A meta-analysis. Front. Clin. Diabetes Healthcare. (2021) 2:699038. doi: 10.3389/fcdhc.2021.699038
47. Chamberlain CR, Oldenburg B, Wilson AN, Eades SJ, O'Dea K, Oats JJ, et al. Type 2 diabetes after gestational diabetes: greater than fourfold risk among indigenous compared with non-indigenous Australian women. Diabetes Metab. Res. Rev. (2016) 32(2):217–27. doi: 10.1002/dmrr.2715
48. Neven ACH, Lake AJ, Williams A, O'Reilly SL, Hendrieckx C, Morrison M, et al. Barriers to and enablers of postpartum health behaviours among women from diverse cultural backgrounds with prior gestational diabetes: A systematic review and qualitative synthesis applying the theoretical domains framework. Diabetic Med. J. Br. Diabetic Assoc. (2022) 39(11):e14945. doi: 10.1111/dme.14945
Keywords: gestational diabetes, type 2 diabetes mellitus, glucose tolerance test, postpartum period, female, behavior therapy, persuasive communication, qualitative
Citation: Lake AJ, Williams A, Neven AHC, Boyle JA, Dunbar JA, Hendrieckx C, Morrison M, O’Reilly SL, Teede H and Speight J (2023) Barriers to and enablers of type 2 diabetes screening among women with prior gestational diabetes: A qualitative study applying the Theoretical Domains Framework. Front. Clin. Diabetes Healthc. 4:1086186. doi: 10.3389/fcdhc.2023.1086186
Received: 01 November 2022; Accepted: 12 January 2023;
Published: 24 February 2023.
Edited by:
Joseph M. Pappachan, Lancashire Teaching Hospitals NHS Foundation Trust, United KingdomReviewed by:
Chitra Selvan, M.S. Ramaiah Medical College, IndiaCopyright © 2023 Lake, Williams, Neven, Boyle, Dunbar, Hendrieckx, Morrison, O’Reilly, Teede and Speight. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amelia J. Lake, YWxha2VAYWNicmQub3JnLmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.