
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Clin. Diabetes Healthc. , 24 December 2021
Sec. Diabetes Self-Management
Volume 2 - 2021 | https://doi.org/10.3389/fcdhc.2021.769528
This article is part of the Research Topic Psychosocial Repercussions of the Covid-19 Pandemic for People Living with or Supporting Others with Diabetes View all 10 articles
The aim of this study was to take ‘snapshots’ of how people with diabetes are feeling emotionally during the coronavirus disease 2019 (COVID-19) pandemic. Three ‘snapshot’ surveys were conducted during May 2020, August 2020 and April 2021, each over a two-week period. Adults (≥18 years) with diabetes calling the Australian Government’s National Diabetes Services Scheme Helpline (NDSS) were invited to participate. Those who accepted were asked three questions sourced/adapted from the Problem Areas in Diabetes scale. Responses were recorded on a 5-point scale (0=’not a problem’, 4=’serious problem’). Of interest were scores ≥2, indicating this was at least a ‘moderate problem’. The survey was administered by NDSS Helpline staff via telephone. Basic demographic and clinical data were collected. In total, 1,278 surveys were completed over the three ‘snapshots’ (1st N=449; 2nd N=414; 3rd N=415). Participants were aged (median[IQR]) 62[47,72] years, 56% were women, and 57% had type 2 diabetes. At the 3rd ‘snapshot’, 21% had received a COVID-19 vaccine. Our findings show that feeling at least moderately ‘burned out’ by the constant effort needed to manage diabetes is salient, and consistently experienced by adults with diabetes calling the NDSS Helpline at three timepoints during the coronavirus pandemic. Those who participated in the 3rd ‘snapshot’ survey were less likely to report that feeling ‘alone with their diabetes’ or ‘worrying about their diabetes because of the COVID-19 pandemic’ were moderate or serious problems for them. Except for younger adults, findings indicate that the easing of restrictions may mitigate some of the effects of the pandemic on diabetes-specific emotional problems, including feeling ‘burned out’, ‘alone’ with diabetes, and/or worried about diabetes due to COVID-19. Prospective data are needed to improve our understanding of the emotional impact of COVID-19 on people with diabetes and to inform when and how to target support for those who need it most.
The novel coronavirus disease (COVID-19) is associated with serious physical consequences (1). Mounting evidence highlights that the pandemic (and associated restrictions to personal freedoms) is having a detrimental impact on mental health in the general population (2). For people with diabetes, COVID-19 infection is associated with increased risk of serious complications and/or death (3, 4), while the pandemic and associated restrictions contribute to increased distress, stigmatisation and social isolation (5). Changes in the number of active cases in the community, levels of restrictions, and vaccination rates, may impact how people are coping with, and adapting to, the challenges of this novel virus at any given point in time.
Our aim was to obtain brief snapshots of how adults are feeling about their diabetes at three timepoints during the COVID-19 pandemic. Prior to the first ‘snapshot’ survey period (26 May to 9 June 2020), pandemic restrictions had been in place but were about to be eased nationally. During the second ‘snapshot’ (20 August to 3 September 2020), Melbourne had widespread community transmission, and a second lockdown, while all other states reported zero or few cases and minimal restrictions. During the third ‘snapshot’ (27 April to 13 May 2021), most states had no community transmission and minimal restrictions. Furthermore, the Australian Government’s COVID-19 vaccination program had commenced, though only 2.9 million doses (11 per 100 people) had been administered at that time (6).
We conducted three cross-sectional ‘snapshot’ surveys of diabetes-specific distress, associated with feeling ‘burned out’, alone and worried because of the COVID-19 pandemic, among inbound callers to the National Diabetes Services Scheme (NDSS) Helpline. The NDSS Helpline service provides practical support for people with diabetes, including advice on diabetes self-management and information about NDSS services and products. Each ‘snapshot’ survey was conducted over two-week periods commencing May and August 2020 and April 2021. Adults (≥18 years) with diabetes calling the NDSS Helpline (for any reason) were invited to take part in the brief telephone surveys.
Three brief questions were sourced or adapted from the Problem Areas in Diabetes (PAID) scale (7). Respondents were asked, “Which of the following are currently a problem for you?”: a) Feeling ‘burned out’ by the constant effort needed to manage diabetes? b) Feeling alone with your diabetes? c) Worrying about your diabetes because of the COVID-19 pandemic? Participants rated each item (from 0=not a problem, to 4=serious problem). The three items demonstrated acceptable internal consistency (Cronbach's α=0.733). These items were selected given the salience of these issues for people with type 1 diabetes (T1D) and type 2 diabetes (T2D) (7, 8), particularly during the COVID-19 pandemic (9, 10); and also because NDSS factsheets offering support for these issues were readily available for those experiencing problems in these areas (11). Thus, if the caller’s responses indicated that any item was a moderate or serious problem (score ≥2), NDSS Helpline call operators recommended relevant NDSS emotional health factsheets (8): ‘Diabetes distress’ (item 1), ‘Peer support’ (item 2), and ‘Managing worry about COVID-19 and diabetes” (item 3). The factsheets were recommended in addition to usual referrals and support suggested by Helpline staff, including the offer of referral to an ‘on-call health professional’.
In addition to the three survey items, for each participant, the following data were recorded: NDSS registration number, age, gender, postcode, diabetes type and, for those with T2D: treatment type (typically, insulin versus non-insulin). Participants who completed the 2nd and 3rd ‘snapshots’ were asked if they had taken part in the 1st or 2nd surveys. Unique to the 3rd ‘snapshot’ survey, participants were also asked if they had received a COVID-19 vaccine.
We examined the proportion of participants, by diabetes type, who reported scores of ≥2, indicating the item was at least a moderate problem, at each time point. We examined scores ≥2 given that moderate levels of diabetes distress are regarded to be clinically significant in the scoring of diabetes distress measures and can have a significant impact on how a person manages their diabetes (3, 4, 7, 8). Differences between timepoints were analysed using Pearson Chi-square tests or Fisher’s exact tests. Between the three timepoints, item scores (0-4) were also compared using Kruskal-Wallis tests. Post-hoc pairwise tests with Bonferroni correction were performed on categories with significant (P<0.05) Kruskal-Wallis results.
All tests were 2-sided, with p<0.05 considered statistically significant. Analyses were performed using SPSS v26.
During the 2-week survey periods, the NDSS Helpline received N=5,932 inbound calls from people with diabetes: n=2,168 (1st), n=2,119 (2nd) and n=1,645 (3rd). Of these callers, 479 (22%), 454 (21%) and 451 (27%) were invited to participate, respectively in the 1st, 2nd and 3rd ‘snapshot’ surveys. In total, N=1,278 surveys were completed over the three ‘snapshots’ (1st N=449; 2nd N=414; 3rd N=415) by 1,248 eligible adults (n=30 completed a survey at 2 timepoints), representing a 94%, 92% and 93% acceptance rate among those invited. Demographic and clinical characteristics were similar across timepoints (Table 1). At the 3rd ‘snapshot’, 21% (n=88) had received a COVID-19 vaccine dose. There were no differences (by gender, state or diabetes type) between those who had and had not received the vaccine. Of those who received a vaccine dose, 50% were >70 years old and 39% were 50-69 years old.
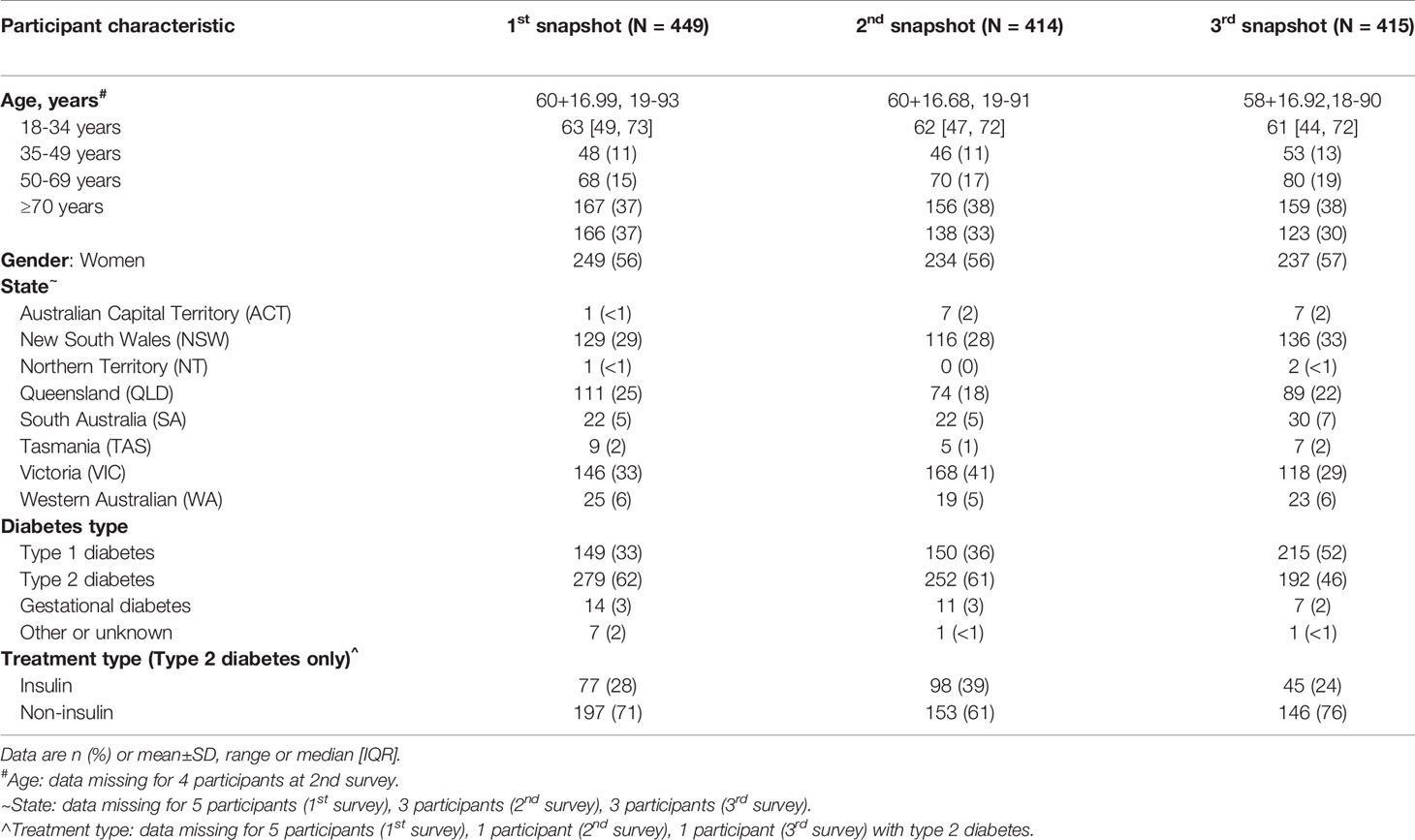
Table 1 Participants’ demographic and clinical characteristics in the 1st (May 2020), 2nd (August 2020) and 3rd (April 2021) ‘snapshot’ surveys.
During the 1st, 2nd and 3rd ‘snapshots’, 42% (n=530) of respondents reported diabetes-specific distress related to at least one problem (i.e. score ≥2 on at least one survey item). This differed between timepoints: 48% in the 2nd survey, compared to 40% in the 1st and 37% in the 3rd ‘snapshot’ (p=0.004). More participants in the 2nd ‘snapshot’ reported that all three survey items were at least a moderate problem (11%) compared to participants in the 1st (8%) and 3rd (6%) ‘snapshots’ (p=0.029).
During the 1st, 2nd and 3rd ‘snapshots’, 30%, 41% and 38% of adults with T1D and 24%, 29% and 23% of adults with T2D, respectively reported feeling at least moderately ‘burned out’ by the constant effort needed to manage their diabetes (Table 2). Item scores were not significantly different between timepoints (Kruskal–Wallis test: T1D, p=0.476, T2D, p=0.316).
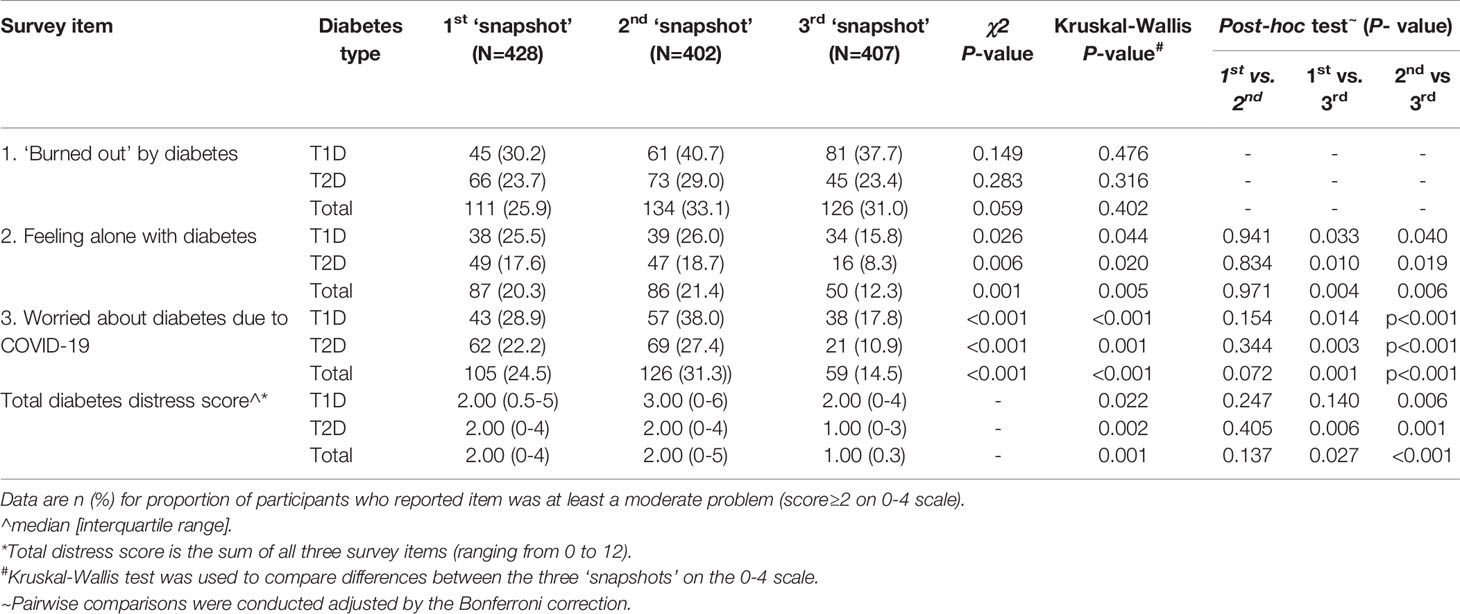
Table 2 Proportion of participants with type 1 diabetes and type 2 diabetes who reported each issue as ‘a moderate-to-serious’ problem during the 1st (May 2020), 2nd (August 2020) and 3rd (April 2021) ‘snapshot’ surveys.
During the 1st, 2nd and 3rd ‘snapshots’, 26%, 26% and 16% of participants with T1D, and 17%, 18% and 8% of adults with T2D, respectively, reported feeling ‘alone’ with diabetes was at least a moderate problem for them (Kruskal–Wallis test: T1D, p=0.044, T2D, p=0.020). Post-hoc comparisons, adjusted by the Bonferroni correction comparing differences in item scores between timepoints (Table 2) found that feeling ‘alone with your diabetes’ was less problematic at the 3rd ‘snapshot’ compared to the 1st (T1D, p=0.033; T2D, p=0.010) and 2nd (T1D, p=0.040; T2D, p=0.019).
During the 1st, 2nd and 3rd ‘snapshots’, 29%, 38% and 18% of participants with T1D, and 22%, 27% and 11% of adults with T2D, respectively, reported feeling at least moderately ‘worried about their diabetes because of COVID-19’ (Kruskal–Wallis test: T1D, p<0.001, T2D, p=0.001). Post-hoc comparisons, adjusted by the Bonferroni correction comparing differences in item scores between timepoints found that ‘worrying about diabetes because of COVID-19’ was less problematic at the 3rd ‘snapshot’ compared to the 1st (T1D, p=0.014; T2D, p=0.003) and 2nd (T1D, p<0.001; T2D, p<0.001) (Table 2).
Younger participants (18-34 years) were more likely to report feeling at least moderately ‘burned out’ during the 3rd ‘snapshot’ (47%), compared to 17% and 30% during the 1st and 2nd surveys, respectively (p=0.004; Table 3).
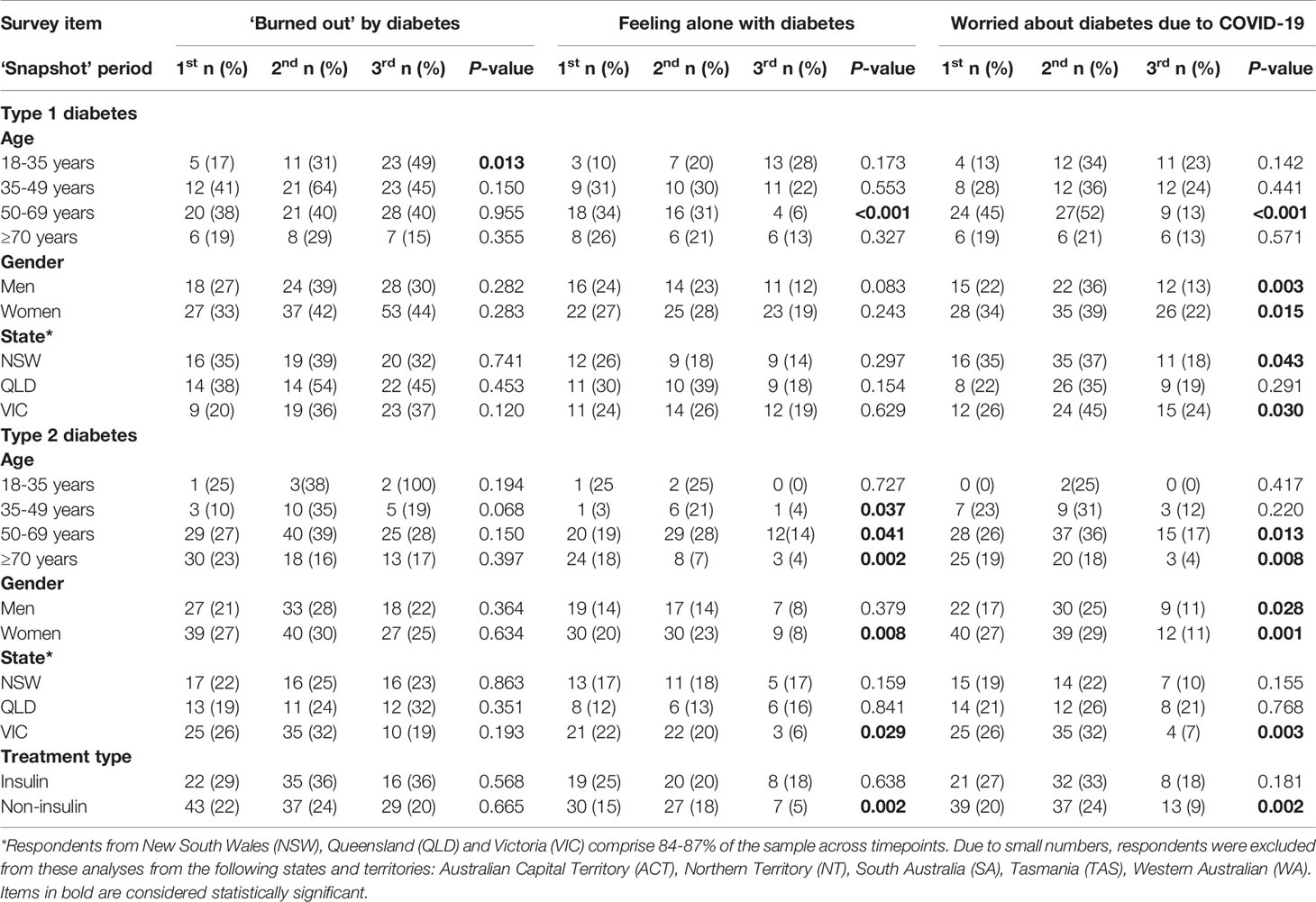
Table 3 Proportion of participants with T1D and T2D during the 1st (May 2020), 2nd (August 2020) and 3rd (April 2021) ‘snapshot’ surveys who reported each item as ‘a moderate-to-serious’ problem (score ≥2), by type of diabetes and demographic characteristics.
Overall, men and women with T1D and T2D reported feeling less worried about their diabetes due to COVID-19 during the 3rd ‘snapshot’ compared with earlier surveys (Table 3). However, during the 1st ‘snapshot’, women with T2D were more likely to report feeling worried about their diabetes due to COVID-19 compared with men (p=0.043).
During the 3rd survey, there was a trend towards a higher proportion of women with T1D feeling at least moderately ‘burned out ‘compared with men (p=0.047).
Within state comparisons over time showed that feeling at least moderately worried about diabetes due to COVID-19 was more likely at the 2nd than the 3rd ‘snapshot’ among participants residing in New South Wales (2nd: 28% vs 3rd: 13%; p=0.008) and Victoria (2nd: 35% vs 3rd: 16%; p=0.001). No significant differences were found between the states on any of the three survey items.
At the 3rd ‘snapshot’, no significant differences were found on any of the survey items by vaccination status among adults with T1D and T2D (Table 4).
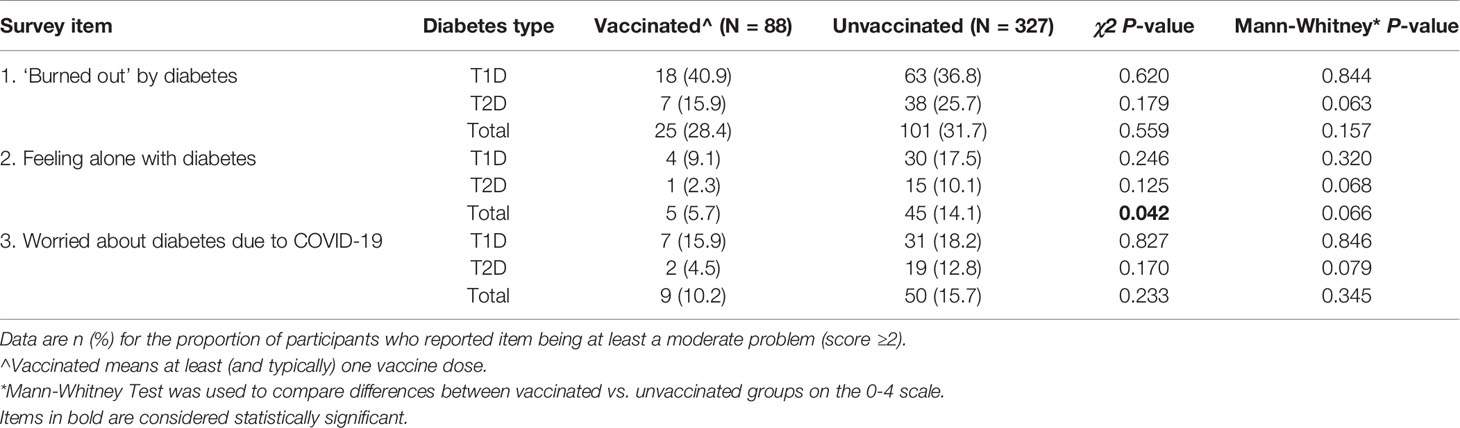
Table 4 Proportion of participants who reported each issue as ‘a moderate-to-serious’ problem during the 3rd ‘snapshot’ survey (April 2021), by diabetes type and vaccination status.
Table 5 summarises the rate of acceptance of relevant NDSS factsheets and uptake of a referral to an ‘on-call’ diabetes health professional (where item scores indicated at least a moderate problem). The rates of uptake when participants were offered a relevant NDSS factsheet were lower during the 3rd survey compared to the previous two surveys (p=0.022). Rates of uptake when participants were offered a referral to an ‘on-call’ health professional were comparable across surveys (p=0.064).
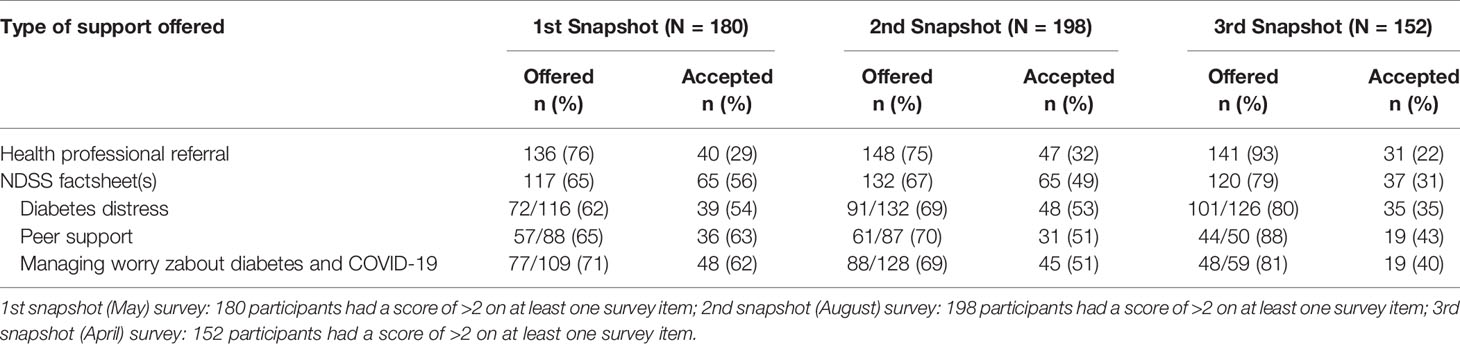
Table 5 Referral type and uptake by participants who reported ‘moderate-to-severe diabetes distress’ in the 1st, 2nd and 3rd ‘snapshot’ surveys.
Our findings demonstrate that adults calling the NDSS Helpline at three time-points during the COVID-19 pandemic were at least moderately distressed about their diabetes. On average, 42% (n=530) of respondents reported that at least one of the three issues explored was a moderate-to-severe problem for them. Participants were more likely to report feeling ‘burned out’, alone and worried about their diabetes because of COVID-19 during the 2nd ‘snapshot’ compared to other timepoints. During the 2nd ‘snapshot’, 6 months into the pandemic, a second lockdown was imposed in Melbourne (with some restrictions at a state level in Victoria). The state was also experiencing a peak number of daily new infections compared to the other timepoints.
Our findings suggest that, during the first year of the COVID-19 pandemic, adults with diabetes are more likely to report feeling ‘burned out’ and ‘alone with their diabetes’, compared with pre-COVID-19 levels (8, 12–14). There is a paucity of data reporting on the longitudinal impact of the COVID-19 pandemic on diabetes distress. A longitudinal study of adults with diabetes in Denmark, found that diabetes distress and general loneliness reduced three months into the COVID-19 pandemic. Similarly, compared to 6 and 12 months prior, participants completing the 3rd ‘snapshot’ were feeling less concerned about their diabetes due to COVID-19. They were also feeling less alone with their diabetes. Our findings likely reflect a reduction in the number of COVID-19 cases in the community at this timepoint, the easing of restrictions and people re-engaging socially.
Younger adults (18-34 years) appear especially impacted emotionally and feeling ‘burned out’ was most common at the 3rd ‘snapshot’. This is consistent with Australian findings among younger adults with type 2 diabetes (11).
The strengths of this study are that these novel ‘snapshot’ data have enabled examination of how people with diabetes are feeling during three timepoints during the COVID-19 pandemic. Participants were receptive to being asked by NDSS Helpline staff about their emotions related to diabetes, and referral options (i.e. factsheets and ‘on-call health professionals’) were in place for those experiencing distress. This is encouraging given that most callers were phoning the NDSS Helpline for practical support with the management of their diabetes.
Limitations include the cross-sectional study design, which precludes inferences about the impact of the pandemic on distress within participants over time. Around 20% of NDSS Helpline callers were invited to participate and most accepted. However, it is unclear whether their experience of diabetes concerns related to feeling ‘burned out’, ‘alone’, and ‘worried due to COVID-19’ can be generalised to those who were not invited to participate, nor to the general adult population living with diabetes. This is particularly pertinent given the higher number of adults with T1D who participated in our surveys and the under-representation of adults with T2D. Another limitation is the selection of only three PAID items, which limits insights into diabetes distress typically captured by a 20-item measure. It is possible that participants may have been experiencing general or diabetes distress or mental health problems not captured by these survey items.
In conclusion, the three ‘snapshots’ suggest that diabetes distress, specifically associated with feeling ‘burned out’, ‘alone’, and ‘worried due to COVID-19’, are significant issues for adults with diabetes in Australia during COVID-19. Prospective data are needed to improve understanding of the trajectory of the emotional impact of COVID-19 on people with diabetes and to inform when and how to target support for those who need it most.
Data was collected by the Australian National Diabetes Services Scheme (NDSS). De-identified raw data was provided to the co-authors. Requests to access the data would need to be approved by the NDSS. Requests to access the datasets should be directed toZWhvbGxvd2F5QGFjYnJkLm9yZy5hdQ==.
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JS and CH conceived of the project with input from TS, EH, and GC. EH and GC coordinated the surveys. EH conducted the data analysis. EH prepared the first and subsequent drafts of this manuscript, following co-author review. All authors reviewed and approved submission of the final manuscript.
The ‘snapshot’ surveys were conducted in 2020-21 as part of the NDSS Mental Health and Diabetes National Priority Area, and funded by the NDSS. The NDSS is an initiative of the Australian Government administered by Diabetes Australia. CH and JS are supported by core funding to the Australian Centre for Behavioural Research in Diabetes provided by the collaboration between Diabetes Victoria and Deakin University.
GC is the manager of the NDSS Helpline, and JS is the Leader of the NDSS Mental Health and Diabetes National Priority Area.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer AS declared a past co-authorship with the authors to the handling editor.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the people with diabetes who shared their time and experiences during the surveys, as well as the NDSS Helpline staff for their support and involvement in administering the surveys.
1. Rothan HA, Byrareddy SN. The Epidemiology and Pathogenesis of Coronavirus Disease (COVID-19) Outbreak. J. Autoimmun (2020) 109:102433. doi: 10.1016/j.jaut.2020.102433
2. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary Research Priorities for the COVID-19 Pandemic: A Call for Action for Mental Health Science. Lancet Psychiatry (2020) 7(6):547–60. doi: 10.1016/S2215-0366(20)30168-1
3. Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL, et al. Practical Recommendations for the Management of Diabetes in Patients With COVID-19. Lancet Diabetes Endocrinol (2020) 8(6):546–50. doi: 10.1016/S2213-8587(20)30152-2
4. Barron E, Bakhai C, Kar P, Weaver A, Bradley D, Ismail H, et al. Associations of Type 1 and Type 2 Diabetes With COVID-19-Related Mortality in England: A Whole-Population Study. Lancet Diabetes Endocrinol (2020) 8(10):813–22. doi: 10.1016/S2213-8587(20)30272-2
5. Skinner T, Speight J. Supporting People With Diabetes During a Pandemic. Diabetes Med (2020) 37(7):1155–6. doi: 10.1111/dme.14320
6. Our World in Data. Statistics and Research. Coronavirus (COVID-19) Vaccinations: Australia 2021. Available at: https://ourworldindata.org/covid-vaccinations?country=~AUS.
7. Sturt J, Dennick K, Due-Christensen M, McCarthy K. The Detection and Management of Diabetes Distress in People With Type 1 Diabetes. Curr Diabetes Rep (2015) 15(11):1–14. doi: 10.1007/s11892-015-0660-z
8. Ventura A, Browne J, Holmes-Truscott E, Hendrieckx C, Pouwer F, Speight J. Diabetes MILES-2: 2016 Survey Report. In: Australian Centre for Behavioural Research in Diabetes. Melbourne, Victoria: Australian Centre for Behavioural Research in Diabetes (2016).
9. Madsen KP, Willaing I, Rod NH, Varga TV, Joensen LE. Psychosocial Health in People With Diabetes During the First Three Months of the COVID-19 Pandemic in Denmark. J Diabetes Complications (2021) 35(4):107858. doi: 10.1016/j.jdiacomp.2021.107858
10. Singhai K, Swami MK, Nebhinani N, Rastogi A, Jude E. Psychological Adaptive Difficulties and Their Management During COVID-19 Pandemic in People With Diabetes Mellitus. Diabetes Metab. Syndrome: Clin Res Rev (2020) 14(6):1603–5. doi: 10.1016/j.dsx.2020.08.025
11. National Diabetes Services Scheme. Mental Health Fact Sheets. Available at: https://www.ndss.com.au/living-with-diabetes/health-management/mental-health/.
12. Speight J, Holmes-Truscott E, Harvey DM, Hendrieckx C, Hagger VL, Harris SE, et al. Structured Type 1 Diabetes Education Delivered in Routine Care in Australia Reduces Diabetes-Related Emergencies and Severe Diabetes-Related Distress: The OzDAFNE Program. Diabetes Res Clin Pract (2016) 112:65–72. doi: 10.1016/j.diabres.2015.11.002
13. Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-Related Emotional Distress in Dutch and US Diabetic Patients: Cross-Cultural Validity of the Problem Areas in Diabetes Scale. Diabetes Care (2000) 23(9):1305–9. doi: 10.2337/diacare.23.9.1305
Keywords: diabetes, diabetes distress, emotional wellbeing, COVID-19, mental health, survey
Citation: Holloway EE, Hendrieckx C, Company G, Skinner TC and Speight J (2021) Diabetes Distress During COVID-19: Three Brief ‘Snapshot’ Surveys of Adults With Diabetes Calling the Australian National Diabetes Services Scheme Helpline. Front. Clin. Diabetes Healthc. 2:769528. doi: 10.3389/fcdhc.2021.769528
Received: 02 September 2021; Accepted: 16 November 2021;
Published: 24 December 2021.
Edited by:
Emma Berry, Queen's University Belfast, United KingdomReviewed by:
Andrea Lukács, University of Miskolc, HungaryCopyright © 2021 Holloway, Hendrieckx, Company, Skinner and Speight. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Edith E. Holloway, ZWhvbGxvd2F5QGFjYnJkLm9yZy5hdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.