
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Built Environ. , 13 February 2025
Sec. Indoor Environment
Volume 11 - 2025 | https://doi.org/10.3389/fbuil.2025.1510965
Introduction: Indoor air quality in dwellings has particular importance regarding occupants’ health. Ventilation is an important means to improve indoor air quality and guarantee occupants’ health.
Methods: We utilized CO2 produced by occupants to measure air exchange rate (i.e., the volumetric out-to-indoor airflow rate divided by building volume, h−1) in Chinese homes, which were then linked to health outcomes like asthma and sick building syndrome symptom. Finally, we proposed a “health-demand” ventilation control strategy according to the relationship between air exchange rate and health outcomes.
Results and Discussion: Each 0.1 h−1 increase in air exchange rate at night was associated with adjusted odds ratios of 0.97 (Confidence Interval (CI): 0.94–1.00) for rhinitis among children and 0.95 (95% CI: 0.91–0.98) for mucosal sick building symptom among adults. Finally, we proposed a “health-demand” ventilation control strategy according to the relationship between air exchange rate and health outcomes. Air exchange rate of 2.5 h−1 and 6.5 h−1 was suggested to deal with sick building syndrome symptoms among adults and rhinitis symptoms among children, respectively.
People spend most of their time indoors, and especially in homes (Tudor-Locke et al., 2009). Indoor environment plays an important role on occupants’ comfort and health. With China’s rapid modernization and urbanization in just a few decades, hundreds of millions of Chinese have experienced rapid and dramatic changes in indoor air environment. Dwellings in Chinese cities have changed from Pingfang (i.e., one-story single family house) to high-rise buildings (China Statistical Yearbook, 2018). A variety of new synthetic building materials, furniture, personal care and indoor cleaning products have been widely used in homes. Pollutants, including formaldehyde, volatile organic compounds (VOCs), semi-VOCs, and bioeffluent have been found indoors, indicating a common indoor air quality (IAQ) issue in Chinese residences (Huang et al., 2017; Zhang et al., 2020). Some indoor pollutants produce odors or are related to irritation, while some pose chronic and/or acute health effects on occupants via inhalation, dermal or other pathways (Ostro et al., 2015; Sundell, 2017; Zhu et al., 2022; Wan et al., 2024; Zhao et al., 2024).
Ventilation is one of the most important means to remove or dilute indoor pollutants and maintain a habitable space for human beings (Sundell et al., 2011; Wargocki et al., 2002; Chenari et al., 2016). Bornehag (Bornehag et al., 2005) studied the association of ventilation with asthma and allergy among Swedish children. They found that children with no signs of any allergies were living in homes with higher ventilation rates, compared to those in homes of allergic children (0.37 h−1 v. s. 0.32 h−1). Smedje (Smedje et al., 2017) investigated indoor environments in 1,160 adults’ homes in Sweden and found that both mucous and dermal symptoms were less prevalent among occupants living in bedrooms with higher ventilation rates. Few study on health effects of ventilation has been performed in Chinese homes. Sun et al. reported significant higher prevalence of wheezing and sick building syndrome (SBS) symptoms among college students in dorm rooms with air exchange rate less than 0.7 h−1 (Sun et al., 2011; Sun et al., 2013).
The establishment of ventilation requirements for occupied spaces has a long history. The minimum ventilation rate nowadays is recommended mainly on perception of air quality, rather than directly addressing occupants’ health (Janssen, 1999; Sundell et al., 2011; Klauss et al., 2011). For example, the ASHRAE Standard 62 (ASHRAE, 2016) sets outdoor airflow rate of 21–35 L/s as the required ventilation in homes for a 47–93 m2 floor area, which is equivalent to air exchange rate of 0.5–0.6 h−1. This was basically the lowest permissible ventilation rate to dilute occupant odors to a concentration acceptable to 80% of occupants. Carbon dioxide was used as a surrogate for occupant odor, but not a health risk, with ceiling concentration of 1,000 ppm (0.1%). A ventilation standard based on health effects rather than air quality perception is more important.
Previous studies have not fully established a quantitative relationship between ventilation rate and health outcomes of occupants. Therefore, the aims of this paper are: 1) to provide knowledge on the relationship between ventilation in residences and occupants’ health; 2) to propose a health-demand ventilation control strategy in residential buildings.
We measured ventilation rate (expressed as air exchange rate, h−1) in northern Chinese homes by using occupants-generated CO2 as tracer gas (Hou et al., 2018). This method (“CO2 method”) is based on the mass balance of CO2 in investigated space (Equation 1).
where
The emission rate of CO2 can be calculated as in Equation 2 (Persily, 1996):
where
By solving Equation 1, indoor CO2 concentration can be expressed as in Equation 3:
where
We measure CO2 concentrations in the investigated space continuously by CO2 monitors (AZ 7798, China, see Figure 1) at an interval of 1 min for at least 24 h and ask the height and weight of each occupant. Outdoor CO2 concentrations are assumed as 400 ppm. CO2 concentration measured during sleeping time is used to estimate air exchange rate. A presumed air exchange rate, as well as initial value of measured CO2 concentration, outdoor CO2 concentration, emission rate of CO2, volume of space are inputted into Equation 3 to estimate value of CO2 concentrations at each
where
This “CO2” method does not require apparatus to inject tracer gas, with no intervention on occupants’ behaver, therefore can measure long-term ventilation rate in real living conditions.
From 2013 to 2016, we performed a study on children’s asthma and allergy and home environment in Tianjin, China as part of the CCHH (China, Children, Homes, Health) study. In the Tianjin CCHH study, we surveyed the prevalence rate of asthma and allergy among 7366 children who were 0–8 years old (Sun et al., 2019b). Questionnaires were sent to daycare centers and elementary schools. Parents responded to the questionnaire, giving us information on their children. Based on this cross-sectional data, 200 case children (with at least two symptoms of asthma, rhinitis and eczema) and 200 controls (without any asthma and allergy symptoms) were invited into home inspections, during which we measured ventilation rate (expressed as air exchange rate) in their home based on “CO2 method,” as well as a serial of physical (air temperature, relative humidity and CO2 concentrations), chemical (such as phthalates) and biological (house dust mite allergen and endotoxin) parameters (Sun et al., 2024).
From Mar. 2018 to Feb. 2019, we conducted a “Indoor Air Quality (IAQ) and Ventilation in Homes” study in Tianjin, China, during which we repeatedly inspected 32 Chinese homes, once during each season. During each home inspection, occupants responded to questionnaires that surveyed their SBS symptoms. The home inspection process included measurements of environmental parameters such as indoor air temperature (T), relative humidity (RH), CO2, air exchange rate, volatile organic compounds (VOCs), formaldehyde, particulate matters and ozone (Sun et al., 2019a).
Logistic regression analyses were used to evaluate the association of occupants’ health with air exchange rate. Potential confounders were determined a priori from literature review (Weinmayr et al., 2013). The confounders were gender, age, family allergic history, dampness, environmental tobacco smoke exposure, outdoor PM10 and measurement seasons for the asthma and allergy analysis. Gender, age and household income were adjusted for SBS symptoms analysis. These variables have been found to be related to either ventilation or health outcomes. Therefore, they were adjusted for the association of ventilation with asthma and allergy, and SBS symptoms.
Northern China is cold and dry in winter, and warm and moist in summer. Almost all homes in China have natural ventilation system, which rely on opening windows and infiltration for outdoor air supply. In northern China, people prefer to close windows on most days, especially in cold winter to keep indoor thermal comfort. Previous study has reported that more than 70% of the time during winter months had window closed at home (Hou et al., 2018).
In the “China, Children, Homes, Health” study, we surveyed the prevalence of wheeze, rhinitis and eczema symptoms in the last 12 months among 7,366 children (aged 0–8 years old) in Tianjin region (see Table 1). We obtained the air exchange rates in 374 children’s bedroom (see Table 2) and investigated its association with children’s asthma and allergy (see Table 3). It shows that the median value of air exchange rate was 0.4 h−1. Air exchange rate in child’s bedroom revealed a clear dose-response relationship with child’s rhinitis symptom in the last 12 months. Previous study discovered that with the increment of air exchange rate (Δ = 1 h−1), house dust mite allergen concentration decreased by 32%–57% (Sun et al., 2022). Epidemiologic studies have shown that exposure to house dust mite increased the prevalence rate of asthma and allergy (Celedón et al., 2007; Wan et al., 2024). Therefore, the impact of insufficient ventilation on child’s asthma and allergy might be explained through the “chain” of house dust mite exposure in tightly constructed buildings.
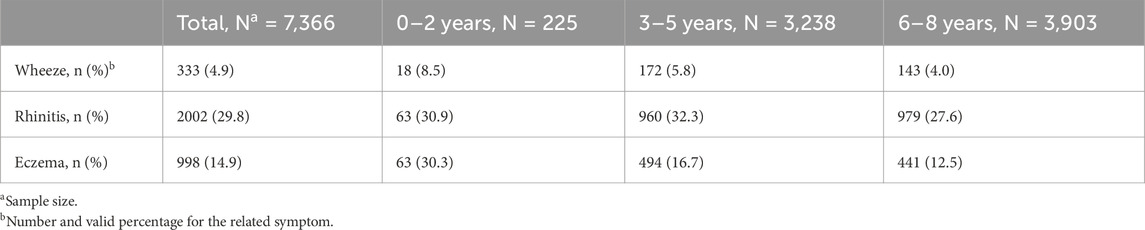
Table 1. Prevalence of wheeze, rhinitis and eczema in the last 12 months among children 0–8 years old in Tianjin, China, 2013.
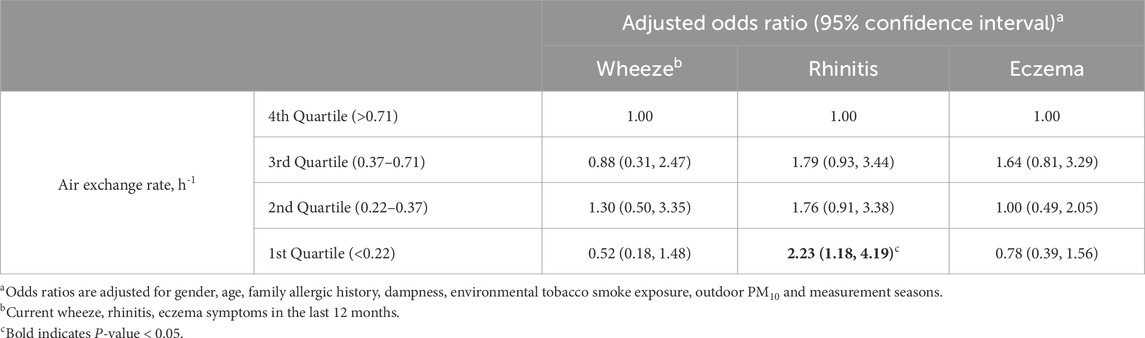
Table 3. Dose-response relationship between air exchange rate in child’s bedroom and allergic symptoms among children, Tianjin, China.
In this study the adjusted odds ratio (AOR) of stepwise increment of air exchange rate (Δ = 0.1 h−1) was 0.97 (95% Confidence Interval (CI): 0.94–1.00) for rhinitis symptom. Based on the background level of 29.8% for rhinitis (see Table 1) and the median value of 0.4 h−1 for air exchange rate in children’s bedrooms (see Table 2), the prevalence of rhinitis could be regressed as a function of air exchange rate, as shown in Equation 5. Assuming this relationship to be causal, we may predict the rhinitis prevalence with various ventilation rates.
Where
In the “IAQ and Ventilation in Homes” study, we surveyed and measured 32 homes repeatedly in each season. Among the 120 valid samples for self-reported SBS symptoms, the complaining frequency for general symptoms was 73%, followed by 67% for mucous and 40% for dermal symptoms (see Table 4). The distribution of 123 measurements of air exchange rate in adults’ bedrooms at night and its association with SBS symptoms are shown in Tables 5, 6 respectively. Dose-response relationship was observed between air exchange rate and SBS symptoms, especially for mucosal symptoms which indicated that a low air exchange rate at night increased the risk of mucosal complaints. Our result is consistent with previous studies. The Swedish Office Illness study indicated that increased air exchange rate decreased the risk of SBS (Sundell et al., 1994). Sun et al. (2013) found that prevalence of general and skin symptoms among students living in dorms increased with air exchange rate below 0.7 h−1. In another paper, we observed that low air exchange rate in rooms led to higher concentrations of formaldehyde and volatile organic compounds (Sun et al., 2019a). Studies in Australia, Japan and Sweden have shown that high formaldehyde concentration was associated with increased risk of SBS symptoms as well as of asthma, allergies, and airway diseases (Zuraimi et al., 2007; Norback et al., 1995; Garrett et al., 1999; Wieslander et al., 1997). Exposure to higher concentration of VOCs due to low ventilation might be the mechanism “chain” for the association between air exchange rate and SBS symptom complaints.
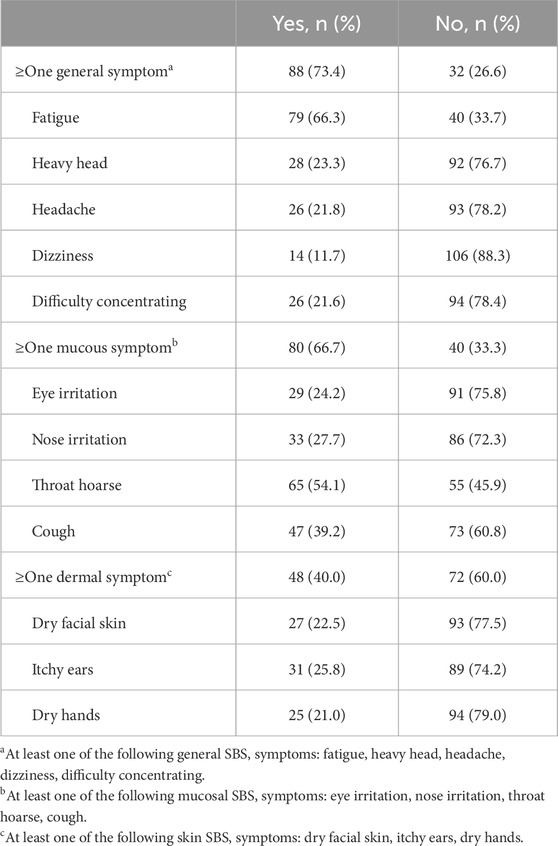
Table 4. Prevalence of sick building syndrome symptoms among adults in the investigate homes in Tianjin, China, 2018.

Table 6. Dose-response relationship between air exchange rate in adults’ bedroom and sick building syndrome symptoms, Tianjin, China.
We found the adjusted odds ratio (AOR) of stepwise increment of air exchange rate (Δ = 0.1 h−1) was 0.95 (95% CI: 0.91–0.98) for mucous symptom. Based on the background level of 66% for mucous symptoms among adults (see Table 4) and the median value of 0.4 h−1 for air exchange rate in Tianjin homes (see Table 5), the prevalence of mucous SBS symptom complaint can be expressed as a function of air exchange rate, see Equation 6.
Where
The dose-response relationship between air exchange rate and health outcomes (i.e., Equations 5, 6) provides basic data and guidance on ventilation to guarantee occupants’ health in dwellings, based on which we propose a health-demand ventilation control strategy to meet the health needs of occupants and to minimize energy consumption as well. For occupancy scenario, ventilation shall be maintained to protect child from rhinitis and adult from mucosal SBS symptom. Otherwise minimum ventilation rate recommended in the existing domestic/international standards for indoor air quality shall be met.
The health-demand ventilation control strategy is described as follows in details:
• When the space is not occupied, ventilation is maintained at base rate as recommended in the existing ventilation standards (e.g., 0.5 h−1 as in ASHRAE Standard 62, 2016);
• When the space is occupied, required ventilation is determined directly to deal with health effects.
◆ The cause of SBS symptoms might be within host factors as well, besides by environmental factors. We are dealing with a window of complaint rate above 20% (Wolkoff, 2018). When the SBS symptoms among adults are supposed to be at 20%, the demand ventilation is 2.5 h−1 (see Equation 6);
◆ The population attributable fraction of genetic factor to rhinitis among child was 12% (Sun et al., 2019b). Therefore, we are dealing with a lower limit of 4% [i.e., prevalence of rhinitis 29.8% (see Table 1)*12% = 4%] regarding the rhinitis symptom among child. The corresponding demand ventilation is 6.5 h−1 (see Equation 5).
We additionally calculated required ventilation rate for controlling formaldehyde and house dust mite concentrations in typical northern Chinese homes, as shown in Supplementary Material. The minimum ventilation rate for indoor air quality demand regarding formaldehyde or house dust mite concentration was supposed to be 0.57 h−1 and 0.46 h−1, respectively. This is lower than the required ventilation rate for health demand, which indicates the complex health effects of indoor pollutants’ mixture. Source control strategy can be effective in reducing concentration of indoor pollutants, such as using indoor decoration materials with low emission rate of volatile organic compounds and/or decreasing occupancy level to reduce indoor moisture contents. When it is not possible to remove or control the source of indoor air pollution, and air filtration is ineffective, the pollution concentration can only be lowered by ventilation with fresh air, i.e., by diluting the indoor pollutants with outdoor fresh air. Sufficient ventilation rate to guarantee occupants’ health should be regulated.
The health-demand ventilation control strategy can be implemented through a smart ventilation control system, which consists of data detection unit, central processing unit (CPU) and terminal display unit (as shown in Figure 3). The data detection unit includes CO2 sensor and occupancy sensor. The CPU processes CO2 concentration and occupancy level to estimate real-time air exchange rate by using CO2 method, meanwhile the corresponding prevalence rate of rhinitis and mucosal SBS symptom can be predicted using Equations 5, 6 respectively. Terminal display unit demonstrates the real-time air exchange rate and the predicted prevalence of health outcomes. In addition, the CPU compare the real-time air exchange rate and the desired values in different scenarios, based on which to control and adjust ventilator.

Figure 3. Implement process of health-demand ventilation control system. aEmpty scenario: ACR = 0.5 h−1 is set as recommended in ASHRAE Standard 62; bOccupancy with adult scenario: ACR = 2.5 h−1 is set to guarantee mucosal sick building symptom among adults as low as 20%; cOccupancy with child scenario: ACR = 6.5 h−1 is set to guarantee rhinitis symptom among children as low as 4%.
This smart control system can work for hybrid ventilation, which is a combination of mechanical and natural ventilation. When wind pressure or temperature gradients are not sufficient to drive the flow by natural means, the desired ventilation rates can still be maintained by the mechanical systems. We believe the control system simultaneously guarantees occupants’ health and lowers energy consumption.
The clear dose-response relationship between ventilation and health outcomes were obtained through systematic measurements and multivariable analysis in large scale Chinese home studies.
There are several limitations. Firstly, we only considered the health effects of ventilation on asthma, allergy, and SBS symptoms. Other health outcomes should be considered in further studies. Secondly, the health effects investigated in this study were specific to residential building, and the applicability may vary in other types of building. Thirdly, air exchange rate was estimated during night with ignoring diurnal dynamic variations. However, the significant associations between air exchange rate and health outcomes cannot be explained by this limitation.
Dose-response relationships between ventilation and asthma and allergy among children {prevalence of current rhinitis = 0.341*e^ [−0.336*(air exchange rate)]} and SBS symptoms among adults {prevalence of mucous symptoms = 0.832*e^ [−0.555*(air exchange rate)]} are established. Further studies on dose-response relationship between ventilation and other health outcomes are needed in the future. Based on the health effects of ventilation, a health-demand ventilation control strategy is proposed, with required air exchange rate of 0.5 h−1 and 2.5∼6.5 h−1 for empty and occupancy scenario, respectively. This indicates that in order to guarantee occupants’ health in urban area as Tianjin, ventilation rate in dwellings needs to be improved greatly.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Tianjin University Research Office. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
ZW: Conceptualization, Investigation, Writing–original draft, Writing–review and editing. JH: Data curation, Methodology, Writing–original draft, Writing–review and editing. JF: Formal Analysis, Visualization, Writing–original draft, Writing–review and editing. ZT: Conceptualization, Supervision, Writing–original draft, Writing–review and editing. SF: Data curation, Writing–original draft, Writing–review and editing. RK: Conceptualization, Writing–original draft, Writing–review and editing. YS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Supervision, Methodology, Writing–original draft, Writing–review and editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the (China-Finland Intergovermental Joint Project) under Grant (2024YFE0106800) (National Key Research and Development Program of China) under Grant (2023YFC3708400); and (National Natural Science Foundation of China) under Grant (21207097).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbuil.2025.1510965/full#supplementary-material
ASHRAE (2016). “Ventilation for acceptable indoor air quality in residential buildings,” in ASHRAE. ANSI/ASHRAE standard 62.2-2016 (Atlanta, GA, USA: ASHRAE).
Bornehag, C. G., Sundell, J., Hägerhed-Engman, L., and Sigsgaard, T. (2005). Association between ventilation rates in 390 Swedish homes and allergic symptoms in children. Indoor Air 15 (4), 275–280. doi:10.1111/j.1600-0668.2005.00372.x
Celedón, J. C., Milton, D. K., Ramsey, C. D., Litonjua, A. A., Ryan, L., Platts-Mills, T. A. E., et al. (2007). Exposure to dust mite allergen and endotoxin in early life and asthma and atopy in childhood. J. Allergy Clin. Immunol. 120 (1), 144–149. doi:10.1016/j.jaci.2007.03.037
Chenari, B., Carrilho, J. D., and da Silva, M. G. (2016). Towards sustainable, energy-efficient and healthy ventilation strategies in buildings: a review. Renew. Sustain. Energy Rev. 59, 1426–1447. doi:10.1016/j.rser.2016.01.074
China Statistical Yearbook (2018). China statistical yearbook, 4-5. Beijing: National Bureau of Statistics of China.
Garrett, M. H., Hooper, M. A., Hooper, B. M., Rayment, P. R., and Abramson, M. J. (1999). Increased risk of allergy in children due to formaldehyde exposure in homes. Allergy 54 (4), 330–337. doi:10.1034/j.1398-9995.1999.00763.x
Hou, J., Zhang, Y. F., Sun, Y. X., Wang, P., Zhang, Q. N., Kong, X. R., et al. (2018). Air change rates at night in northeast Chinese homes. Build. Environ. 132, 273–281. doi:10.1016/j.buildenv.2018.01.030
Huang, S. D., Wei, W. J., Weschler, L. B., Salthammer, T., Kan, H. D., Bu, Z. M., et al. (2017). Indoor formaldehyde concentrations in urban China: preliminary study of some important influencing factors. Sci. Total Environ. 590, 394–405. doi:10.1016/j.scitotenv.2017.02.187
Janssen, J. E. (1999). The history of ventilation and temperature control. ASHRAE J. 41 (10), 62–71.
Klauss, A. K., Tull, R. H., Roots, L. M., and Pfafflin, J. R. (2011). History of the changing concepts in ventilation requirements. ASHRAE J. 53 (2), 34–43.
Norback, D., Bjornsson, E., Janson, C., Widstrom, J., and Boman, G. (1995). Asthmatic symptoms and volatile organic compounds, formaldehyde, and carbon dioxide in dwellings. Occup. Environ. Med. 52 (6), 388–395. doi:10.1136/oem.52.6.388
Ostro, B., Hu, J. L., Goldberg, D., Reynolds, P., Hertz, A., Bernstein, L., et al. (2015). Associations of mortality with long-term exposures to fine and ultrafine particles, species and sources: results from the California teachers study cohort. Environ. Health Perspect. 123 (6), 549–556. doi:10.1289/ehp.1408565
Persily, A. (1996). Evaluating building IAQ and ventilation with indoor carbon dioxide. ASHRAE Trans. 103.
Smedje, G., Wang, J., Norbäck, D., Nilsson, H., and Engvall, K. (2017). SBS symptoms in relation to dampness and ventilation in inspected single-family houses in Sweden. Int. Archives Occup. Environ. Health 90 (7), 703–711. doi:10.1007/s00420-017-1233-z
Sun, Y. X., Cui, L. W., Hou, J., Luo, S. G., Norbäck, D., and Sundell, J. (2022). Role of ventilation and cleaning for controlling house dust mite allergen infestation: a study on associations of house dust mite allergen concentrations with home environment and life styles in Tianjin area, China. Indoor Air 32 (8), e13084. doi:10.1111/ina.13084
Sun, Y. X., Hou, J., Cheng, R. S., Sheng, Y., Zhang, X. Y., and Sundell, J. (2019a). Indoor air quality, ventilation and their associations with sick building syndrome in Chinese homes. Energy Build. 197, 112–119. doi:10.1016/j.enbuild.2019.05.046
Sun, Y. X., Hou, J., Sheng, Y., Kong, X. R., Weschler, L. B., and Sundell, J. (2019b). Modern life makes children allergic. A cross-sectional study: associations of home environment and lifestyles with asthma and allergy among children in Tianjin region, China. Int. Archives Occup. Environ. Health 92 (4), 587–598. doi:10.1007/s00420-018-1395-3
Sun, Y. X., Marasinghe, S. A., Hou, J., Wang, P., Zhang, Q. N., and Sundell, J. (2024). Household indoor air quality in northeast China: on-site inspection and measurement in 399 Tianjin area residences. Environ. Int. 190, 108825. doi:10.1016/j.envint.2024.108825
Sun, Y. X., Zhang, Y. F., Bao, L. J., Fan, Z. G., and Sundell, J. (2011). Ventilation and dampness in dorms and their associations with allergy among college students in China: a case-control study. Indoor Air 21 (4), 277–283. doi:10.1111/j.1600-0668.2010.00699.x
Sun, Y. X., Zhang, Y. F., Bao, L. J., Fan, Z. G., Wang, D. S., and Sundell, J. (2013). Effects of gender and dormitory environment on sick building syndrome symptoms among college students in Tianjin, China. Build. Environ. 68, 134–139. doi:10.1016/j.buildenv.2013.06.010
Sundell, J. (2017). Reflections on the history of indoor air science, focusing on the last 50 years. Indoor Air 27 (4), 708–724. doi:10.1111/ina.12368
Sundell, J., Levin, H., Nazaroff, W. W., Cain, W. S., Fisk, W. J., Grimsrud, D. T., et al. (2011). Ventilation rates and health: multidisciplinary review of the scientific literature. Indoor Air 21 (3), 191–204. doi:10.1111/j.1600-0668.2010.00703.x
Sundell, J., Lindvall, T., and Stenberg, B. (1994). Associations between type of ventilation and air flow rates in office buildings and the risk of SBS-symptoms among occupants. Environ. Int. 20 (2), 239–251. doi:10.1016/0160-4120(94)90141-4
Tudor-Locke, C., Washington, T. L., Ainsworth, B. E., and Troiano, R. P. (2009). Linking the American time use survey (ATUS) and the compendium of physical activities: methods and rationale. J. Phys. Activity & Health 6 (3), 347–353. doi:10.1123/jpah.6.3.347
Wan, M. F., Sun, Y. X., Luo, S. G., Hou, J., and Norback, D. (2024). Associations between house dust mite concentrations in bedroom dust in Northern China and childhood asthma, rhinitis and eczema. Build. Environ. 247, 110952. doi:10.1016/j.buildenv.2023.110952
Wargocki, P., Sundell, J., Bischof, W., Brundrett, G., Fanger, P. O., Gyntelberg, F., et al. (2002). Ventilation and health in non-industrial indoor environments: report from a European multidisciplinary scientific consensus meeting (EUROVEN). Indoor Air 12 (2), 113–128. doi:10.1034/j.1600-0668.2002.01145.x
Weinmayr, G., Gehring, U., Genuneit, J., Büchele, G., Kleiner, A., Siebers, R., et al. (2013). Dampness and moulds in relation to respiratory and allergic symptoms in children: results from phase two of the international study of asthma and allergies in childhood (ISAAC phase two). Clin. Exp. Allergy 43 (7), 762–774. doi:10.1111/cea.12107
Wieslander, G., Norback, D., Bjornsson, E., Janson, C., and Boman, G. (1997). Asthma and the indoor environment: the significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int. Archives Occup. Environ. Health 69 (2), 115–124. doi:10.1007/s004200050125
Wolkoff, P. (2018). The mystery of dry indoor air-An overview. Environ. Int. 121, 1058–1065. doi:10.1016/j.envint.2018.10.053
Zhang, Q. H., Sun, Y. X., Zhang, Q. N., Hou, J., Wang, P., Kong, X. R., et al. (2020). Phthalate exposure in Chinese homes and its association with household consumer products. Sci. Total Environ. 719, 136965. doi:10.1016/j.scitotenv.2020.136965
Zhao, Y. X., Liu, Y. X., Cui, L. W., Hou, J., Gao, F., Norback, D., et al. (2024). Endotoxins in household dust in Northern China: associations with home environment factors and childhood asthma and allergies. Atmosphere 15, 759. doi:10.3390/atmos15070759
Zhu, C. Q., Sun, Y. X., Zhao, Y. X., Hou, J., Zhang, Q. N., and Wang, P. (2022). Associations between children’s asthma and allergic symptoms and phthalates in dust in metropolitan Tianjin, China. Chemosphere 302, 134786. doi:10.1016/j.chemosphere.2022.134786
Keywords: air exchange rate, carbon dioxide, sick building syndrome, asthma and allergy, dose-response relationship
Citation: Wang Z, Hou J, Fu J, Tian Z, Feng S, Kosonen R and Sun Y (2025) Health-demand ventilation control strategy in northern Chinese homes: how much ventilation do we need to protect occupants’ health. Front. Built Environ. 11:1510965. doi: 10.3389/fbuil.2025.1510965
Received: 14 October 2024; Accepted: 23 January 2025;
Published: 13 February 2025.
Edited by:
Hasim Altan, Prince Mohammad bin Fahd University, Saudi ArabiaReviewed by:
Roberto Alonso González-Lezcano, CEU San Pablo University, SpainCopyright © 2025 Wang, Hou, Fu, Tian, Feng, Kosonen and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuexia Sun, eXVleGlhc3VuQHRqdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.