- Faculty of Architecture and Urbanism, University of São Paulo, São Paulo, Brazil
During the COVID-19 pandemic, social distancing protocols imposed the suspension of many activities in mental healthcare facilities, limiting the use of the facility to people in comprehensive care. With the advancement of vaccination, these buildings are gradually reopening for community use. However, managers and workers now face challenges in accommodating new design demands related to reducing the risk of contamination by COVID-19 within the building. This research adopted a multi-method approach in two phases, combining a post-occupancy evaluation with a cocreation activity to help mental healthcare workers and patients to suggest design changes in their environment. Three Psychosocial Care Centers (CAPS) in São Paulo were selected as case-study buildings. The first phase was the Post-Occupancy Evaluation (POE), in which the lead researcher conducted a walkthrough with the facility administrator, applied questionnaires to 100 employees, and conducted a walking interview with 12 patients. During Phase 02, a codesign activity entitled “Dream CAPS” was conducted with 25 healthcare workers and 12 patients. In this activity, participants were asked to customize a physical model of a mental healthcare facility, choosing the wall and floor finishings, the types of openings (windows, doors), furniture, and ornaments. Afterward, they participated in an interview with illustrated cards. All activities were audio-recorded and textual analysis qualified and categorized the content. Objective and subjective data analysis identified five characteristics of the built environment that prevented or increased risk of COVID-19 spread: Places that support risk mitigation procedures, access and circulation control, extended use of outdoor spaces, natural and artificial air renovation systems, and materials resistant to terminal cleaning. Patients participated in the activities but did not express opinions on the impact of architecture on airborne disease prevention. Healthcare workers claimed that environments that improve mental health must be attractive and prone to social interaction and relaxation without compromising biological safety. The combination of post-occupancy evaluation and codesign proved an excellent tool to identify the demands of mental healthcare buildings and discuss the solutions that must be implemented to deal with contemporary and future crises in a pandemic context.
1 Introduction
Since the end of the 20th century, many countries have adopted the community mental health service model, in which people who suffer from mental illnesses are treated in a domiciliary setting with the support of mental health centers, instead of being institutionalized in a psychiatric hospital. In Brazil, such centers are denominated Psychosocial Care Centers (CAPS). These are places where the mentally distressed can seek psychiatric care through tailored programs, including sporadic appointments with psychologists and doctors, group therapy, and comprehensive care for those in extreme vulnerability. The CAPS operates under an open-door policy, meaning that patients and family members may circulate throughout the facility. It represents the institution’s commitment to offering psychiatric services without compromising the freedom and autonomy of its patients. However, during the COVID-19 pandemic, social distancing protocols imposed the suspension of “open-door” practices. As a result, community activities were cancelled, and the use of the facility was limited to people in comprehensive care who stayed in the inpatient rooms for psychiatric follow-up. With the advancement of vaccination, CAPS were gradually reopening for community use. Notwithstanding, managers and workers now face challenges related to new design demands generated by this new context. Such demands include, for example, improved ventilation, better organization of circulation routes, rooms adapted to the accommodation COVID-19 patients, and larger open areas.
This situation finds parallelism with other Mental healthcare facilities worldwide, which despite their heterogeneity, made responsive adaptations in their architecture and healthcare protocols (Pinals et al., 2020). Above all, studies indicate that the COVID-19 pandemic, and the social and economic impacts that follow, are etiologically related to losses in Mental Health (Maulik et al., 2020; Moreno et al., 2020; Holland et al., 2021; Sung et al., 2021). Some populations are more vulnerable than others, being at a higher risk of exposure to SARS-CoV-2 infection and experiencing increased physical burden related to the pandemic. That is the case for ethnic minorities, people living in poverty, people with pre-existing mental health disorders, and healthcare providers (Ferreira et al., 2020; Moreno et al., 2020; Brunoni et al., 2021; Sung et al., 2021). Further, there is an indication that visit rates for mental health conditions, including suicide attempts and drug overdoses, increased during the COVID-19 pandemic (Moreno et al., 2020). Estimations claim that this situation will outlast the short-term emergency period and intensify in future epidemics (Holland et al., 2021; Maluik et al., 2020; Moreno et al., 2020). This situation pressures stakeholders, healthcare providers, and users to revisit mental healthcare and psychosocial care practices, investing in strategies to develop renovation projects that accommodate new demands so that the project can keep up with their evolving needs.
A conspicuous way to develop functional and technical adaptation design projects in healthcare facilities is by foremost implementing a Post-Occupancy Evaluation (POE). POE employs a multi-method approach to evaluate the performance of built environments, combining an extensive survey of the building condition and data on the user’s experience. It helps to establish adequate use and maintenance of the building and offers the necessary feedback to improve the design of future mental healthcare facilities (Ornstein et al., 2009). However, POE in the context of mental health buildings presents, as an extra challenge, the difficulty of incorporating user input into the design process. Whereas service users may have difficulties expressing their perceptions, mental health workers are often submitted to an uninterrupted routine and they often experience emotional exhaustion (O’Connor et al., 2018), which compromises their ability to participate in POE. Codesigning tools might mitigate these difficulties, given that they accommodate different participant profiles, with forthright activities that facilitate end-user cooperation.
This article is part of a larger study entitled “Environmental Quality in Psychosocial Treatment Units,” which aims to determine the objective and subjective aspects of the ambiance in mental healthcare facilities that can contribute to its positive evaluation by users. An ambiance is the juxtaposition of three dimensions of space: Physical (a place that promotes environmental comfort), social (a place that promotes the exchange of experiences), and institutional (a place that promotes healthcare) (Brasil 2004). The field of Environmental Psychology delves into the concept of ambiance, studying the built space according to its capacity to frame life experiences and emotional bonds (Elali 2009). In a more comprehensive approach, ambiance can be understood as part of the aspects that constitute the quality of buildings. According to Van der Voordt and Van Wegen (2005), environmental quality in its broadest sense integrates formal aspects (aesthetic beauty, perceptional qualities, cultural values, and symbolic meanings), functional aspects (utility of space, subdivisions, and spatial relationships), construction aspects (technical quality of materials, structure, and services), and cost-effectiveness. In an attempt to approach the idea of ambiance, this research converges its observations on the formal and functional aspects of environmental quality.
A combination of POE and Codesign activities were implemented in three Psychosocial Care Centers (CAPS) in São Paulo. The POE surveyed the technical-physical, functional, and environmental performances of each building. This first phase occurred during a critical period of the COVID pandemic in Brazil, from August to November 2020. As vaccines became widely available a year later, healthcare workers and inpatients participated in the Codesign activities.
This manuscript presents partial results of this research project, focusing primarily on considerations regarding design changes caused by the COVID-19 pandemic. Healthcare workers provided several suggestions for renovating the existing space and incorporating new design features during the codesigning activities. Thus, the discussion revolves around the utility of combining POE methods with a codesign instrument to conceive better solutions for designing a Mental Healthcare building that is efficient and fit for the user’s needs.
2 Materials and methods
Considering the scope of this project, we decided to adopt a multi-method approach with two data collection phases to study the characteristics of mental healthcare architecture from the occupant’s perspective. The first phase was the Post-Occupancy Evaluation (POE), in which the lead researcher conducted a walkthrough to assess the environmental quality of the units from the technical perspective and conducted questionnaires and walking interviews to assess the occupants’ perceptions. The second phase consisted of the codesign activity, which followed the design of the “Participatory Prototyping Cycle” (PPC) co-creation framework. It unfolds an interactive loop of making, telling, and enacting to accommodate participants with different abilities (Sanders, 2013). The PPC was entitled “Dream CAPS,” and consisted of two tools: The customizable physical model and illustrated cards. This article focuses on the presentation and analysis of extracts of the collected data that allow for an in-depth discussion on design aspects related to preventing COVID-19 spread.
2.1 Case study areas
This research evaluates three Psychosocial Care Centers for Alcohol and Drug Addicts (CAPS-AD III, in its Portuguese acronym). These units were selected because they have the highest level of complexity within the Brazilian public mental healthcare service, offering 24-h accommodation for people in need and a general practitioner clinic, besides essential healthcare services, psychosocial support, and daily mental health activities program. Every CAPS AD III unit in São Paulo was contacted, and four expressed interest in participating. Of these, we selected as case studies those three that had been operating for at least 1 year and met the minimum requirements regarding service staff and infrastructure. The units are located in the peripheric neighborhoods of São Paulo City, Brazil. They serve people in the middle and lower socioeconomic status, including people in extreme vulnerability, such as those without housing.
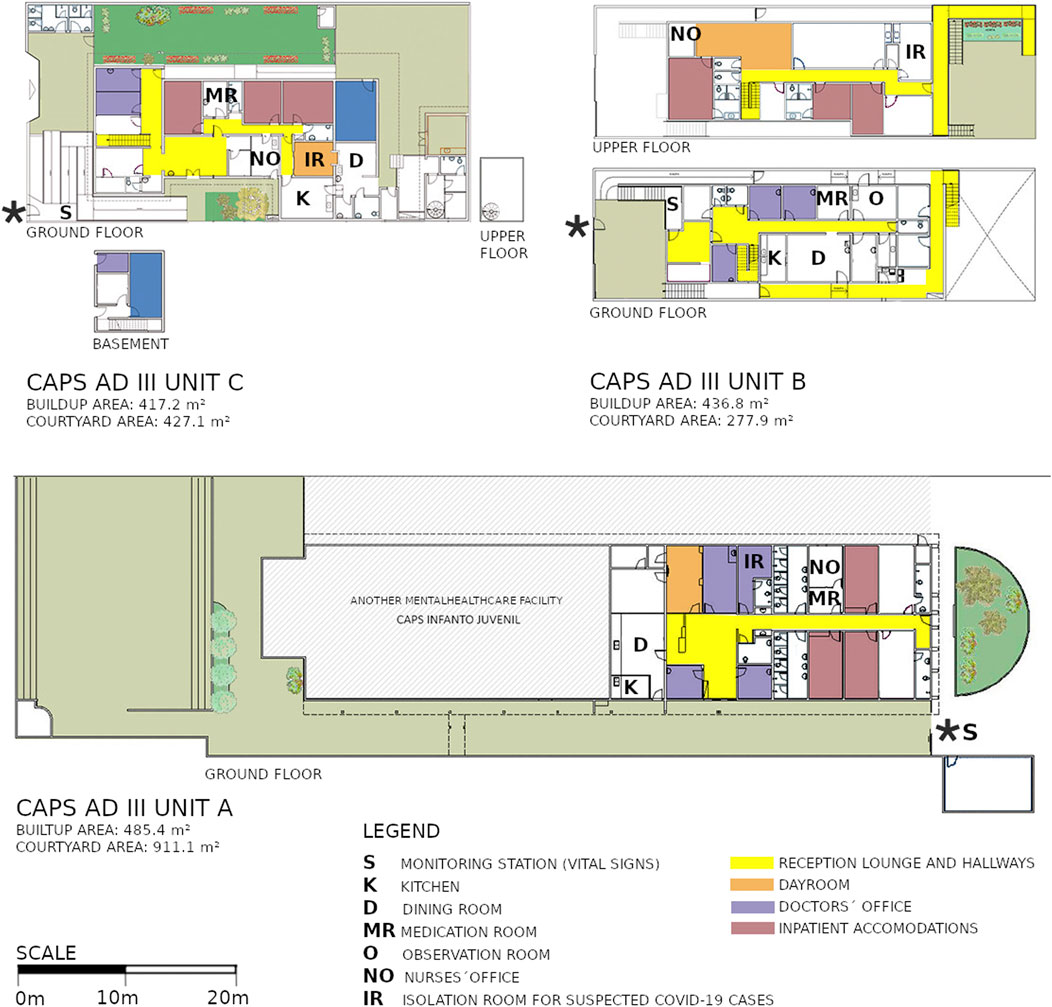
The chosen units differ in the following aspects:
• Unit A: The initial design of the building was developed to be a motel. Later, it was renovated to serve as a psychiatric inpatient unit. In 2014, the 7,000 m2 compound was revitalized and transformed into a healthcare facility complex, with several basic public health units including a CAPS AD III. It has a total staff of 38 employees.
• Unit B: The building was designed as a residential unit and housed an orphanage before being rented and renovated to house the CAPS AD III unit. It has a total staff of 51 employees.
• Unit C: This CAPS ADIII building was originally an 800 m2 high-end family home surrounded by nature, an environmental reserve a few meters from a lake. Few renovations were done to adapt this space to become a CAPS AD III unit. It has a total staff of 59 employees.
2.2 Phase 01—Post-occupancy evaluation
The Post-Occupancy Evaluation occured between 1 August 2020 and 25 November 2020. This phase was carried out when vaccination against COVID-19 was available to healthcare workers and older people, but not to the general public. Therefore, the CAPS AD III units had to restrict their activities to individual care for the most vulnerable patients.
2.2.1 Participants
Healthcare workers and administrative staff were introduced to the research in a meeting, which clarified all inquiries. Then, a representative sample of employees was gathered by random selection, with a 95% confidence interval and a 5% margin of error. One hundred participants agreed to respond to the questionnaire and signed a consent form (26 in unit A, 36 in unit B, and 38 in unit C). For the walking interviews, patients staying in for 24-h comprehensive care were selected by convenience, according to their willingness to participate. 12 patients agreed to participate, four in unit A, three in unit B, and five in unit C.
2.2.2 Tools and techniques
• Walkthrough: The product of a walkthrough visit includes notes and sketches based on the architect’s exploratory observations and the filling of a checklist. For this study, a semi-structured approach was adopted. Each room was visited twice to fill in the checklist and gather information about the functional, technical-physical and environmental aspects of the building. During one of the visits, the lead researcher was accompanied by a healthcare professional, who indicated the measures due to SARS-CoV-2 contingencies. This information was compiled in a checklist developed for this study based on the information collected in the relevant literature on the topic (D’Agostino et al., 2020; Mukhtar and Rana, 2020; Burridge, et al., 2021; Fadaei, 2021). The checklist consists of five aspects of the building’s configuration that prevent or increases risk of COVID-19 spread: 1) Nurses’ station and medication room, 2) Reception and circulation control, 3) Isolation/quarantine accommodations, 4) Outdoor open spaces, 5) Ventilation.
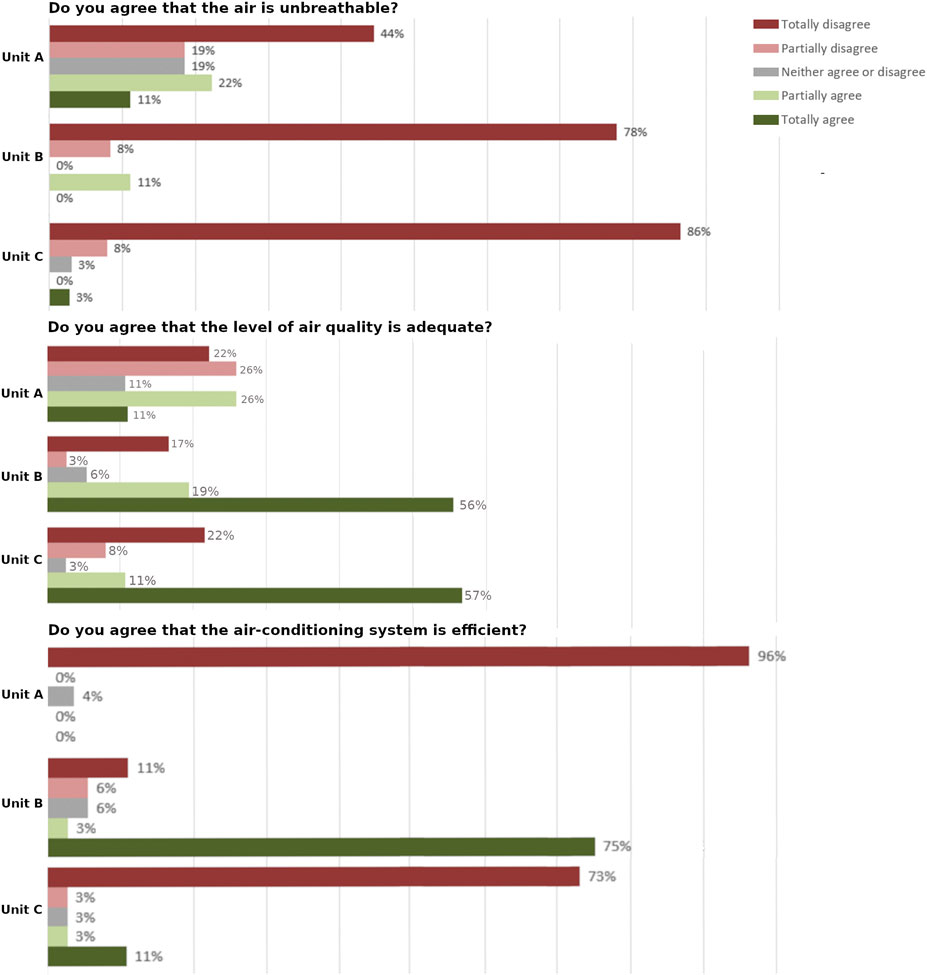
• Questionnaire: The “Perceived Hospital Environment Quality Indicators” Questionnaire (Andrade et al., 2012; Morais et al., 2015) was administered to workers. This instrument had 36 questions organized in 9 dimensions that evaluate aspects of healthcare facilities: 1) spatial-physical comfort, 2) temperature and air quality, 3) orientation, 4) views and lighting, 5) quietness, 6) privacy, 7) care of social and organizational relationships, 8) upkeep and care of external areas, and 9) green areas. The second dimension had three questions that we consider relevant to this analysis: “Do you agree that the level of air quality is adequate?,” “Do you agree that the air conditioning system is efficient?” and “Do you agree that the air is unbreathable?”
• Walking interview: Patients participated in this activity by showing to the researcher their favorite environments and their impressions and feelings about each location. Each interview had a semi-structured format and lasted 10 min. The patients were asked to show their dorms and favorite places to relax, play and interact with others. They were encouraged to express themselves about the architecture and design aspects of the building and reflect on their likes and dislikes.
2.2.3 Procedures
During the Post-Occupancy Evaluation, the lead researcher, an expert in environmental psychology and healthcare architecture, conducted six technical visits to each building to evaluate its environmental quality and the user’s perception. The first technical visit was a walkthrough with the facility administrator, in which every room was inspected. The CAPS administrators were experts in medical and psychiatric services, and due to the COVID-19 pandemic, they have received successive guidelines and training to help containing SARV-CoV-2 spread within the unit. During this activity, the researcher took notes on functional aspects of each room (effective use of space, suitability for the activities performed in it, furniture quality, circulation, and spatial organization). The facility administrator was then inquired about changes to the configuration of the building that prevented or increases risk of COVID-19 spread. The second visit was also a walkthrough, in which the researcher revisited each room, this time to make sketches and take notes on technical-physical aspects (the quality of structural elements, windows, doors, flooring, wall finishings, and building installations) and environmental aspects (thermal, lighting and acoustic comfort; indoor air quality; visual comfort; and ergonomics). The visits yielded a series of documental data such as notes, sketches, and photographs. The last visits focused on user perception. The researcher went to each unit on three different weekdays to administer the questionnaires to the employees, using the face-to-face method. At last, walking interviews were conducted with patients.
2.2.4 Analysis
The data collected during de POE was synthesized into a diagnostic report that describes the situation of each CAPS unit. The report features information on the facility territory, users, therapeutic activities, building infrastructure, space usability, functionality, humanization, and workers’ perception of the environment. Data from the questionnaires were computed on a scale ranging from −2 (totally disagree) to +2 (totally agree). Walking interviews were audio-recorded and transcribed. Complementary material consisted of a diagnostic map identifying problems found in each analyzed room. The reports allow for the visualization of data concerning the technical-physical, functional and environmental quality of the unit and illustrate how these space aspects can impact user perception.
For this study, the lead researcher examined the reports to identify characteristics of the built environment that prevents or increases risk of COVID-19 spread, according to the relevant literature on this subject (D’Agostino et al., 2020; Mukhtar and Rana, 2020; Burridge, et al., 2021; Fadaei, 2021).
2.3 Phase 02—Participatory prototyping cycle
The Participatory Prototyping Cycle occurred between 15 February 2022, and 21 April 2022. The Codesign activity was carried out when the units began operating without restrictions other than the imposition of personal protective equipment use. When arriving at the unit, visitors and employees were requested to measure their temperature and state if they had any respiratory symptoms, sanitize their hands with alcohol gel, wear face masks, and wash their hands constantly.
2.3.1 Participants
The participant selection was according to convenience. Interested employees and patients volunteered and during 4 days the researcher was available to apply the Participatory Prototyping Cycle. Every effort was made all interested parties to participate. In total, 25 employees participated in the PCC. 10 in unit C (4 nurses, one Physical Education professional, two psychologists, two social workers, one artist), seven in unit A (two nurses, two psychologists, two occupational therapists, one administrative staff member) and eight in unit B (one social worker, one occupational therapist, two pharmacists, three nurses, one administrative staff member). 12 patients participated in the PCC, four in each unit.
2.3.2 Tools and techniques
• Physical model of a Mental Healthcare Facility: This tool was developed to conduct Codesign activities in Mental Healthcare Facilities. It consists of a 1:20-scale model that is entirely customizable, with three indoor spaces (bedroom, dayroom, and nursing station) and a courtyard. The size of the rooms corresponded to the minimum space required by Brazilian regulations for healthcare units. However, the walls could be modified to resize the area or create new spaces. Further, the participants could decide the wall and floor finishings, as well as the type of opening, furniture, and ornaments. This activity required participants to use “making” and “enacting” abilities.
• Illustrated cards: Based on Sanoff’s “Space Rating Scale” (Sanoff, 2001, 37–38), this item consisted of 15 cards with images of mental healthcare facilities. The images featured projects in different degrees of humanization; hospital environments; residential-style settings; and vibrant, dynamic spaces. The interviewees should express their impressions of the environment while holding a paper with suggestions of spatial characteristics, such as interesting, dynamic, repelling, novel, unpleasant, friendly, and others (Figure 1). Then, each interviewee should say if the displayed image would function as a mental healthcare environment. This activity requires participants to use “telling” abilities.

FIGURE 1. Example of four illustrated cards representing reception rooms in mental healthcare facilities. On the right, is the card with suggestions of spatial characteristics.
2.3.3 Procedures
In the second phase, the results of the POE were presented to administrators and healthcare employees. Then, the researcher proposed enacting the Codesign activity “Dream CAPS” to bring about in-depth discussions about architectural aspects of mental healthcare facilities that positively impact service quality. On this occasion, healthcare employees volunteered for the codesign activity. With the help of the unit administrator, we recruited 12 end-users (patients in 24-h accommodations) willing to participate in the PPC.
The “Dream CAPS” codesign activity was carried out by the lead researcher in 14 sessions with one to two participants. Workers would do this activity in pairs while end-users participated individually. Each session lasted about 40 min and was composed of two tools: the interactive physical model and the illustrated cards. First, the participants received the necessary instructions and signed an informed consent form, confirming their decision to contribute to the research. The presentation of this document was demanded by the Research Ethics Committee since it is an essential component in the ethical conduct of research with human subjects. In sequence, they would customize the 1:20-scale physical model to create an idealized interpretation of the inpatient’s bedroom, the dayroom, the courtyard, the service rooms, and the nursing station.
During this activity, the researcher would start with open questions and then call the pros and cons of each material and furniture, suggesting several design solutions for them and being careful enough not to interfere with the participant’s point of view. This intervention, however, would occur at the participant’s request. For example, while creating a bedroom, the participant could ask what materials had better cost-benefit, what pieces of furniture were most resistant, what the better solutions for ventilation were, and so on. In this manner, aware of every possible design solution, the participant could create the “Dream CAPS” that meet their demands.
After the assembly of the physical model, the participants attended interview with illustrated cards in which they expressed their feelings and preferences regarding images of different styles of dayrooms, resident bedrooms, and reception rooms. The entire activity was audio-recorded, and the finished physical model was photographed.
2.3.4 Analysis
All activities of the PPC were audio-recorded, and textual analyses categorized and qualified the content, signaling important information regarding necessities for post-COVID functional and technical adaptations. Starting with the careful examination of all content discussed during the PCC, researchers conducted a reflexive analysis to identify textual extracts of ideas, perceptions, and suggestions related to design solutions in a post-pandemic reality. Every mention of the COVID-19 pandemic was marked and contextualized according to the participants’ proposed solutions. Following the categorization, the extracts were qualified according to the participant’s assessment on the matter. The analysis identified which participants were favorable to changes, their reasons, and their motivations. Also, we pointed out user preferences towards a homelike or hospital environment.
3 Results
This section presents every mental health facility design and architecture element in a post-pandemic context that emerged during the Post-Occupancy Evaluation and the Participatory Prototyping Cycle. The objective is to identify elements that support the management of the CAPS environment, considering the possibility of a future with continuous contamination of COVID-19 and other diseases. According to the analysis, only three of the applied methods resulted in relevant information for functional and technical adaptations in post-COVID-19 reality (Figure 2). The walkthrough offered data on which room underwent adaptations to accommodate new demands imposed by the pandemic and aspects of the building’s configuration that either prevent or increases risk of COVID-19 spread. The questionnaire had three questions on the employees’ perceptions of air quality and efficacy of the air conditioning system, which helped us access the state of air renewal systems. The customization of the Physical Model created opportunities to discuss issues related to the formal and functional aspects of the CAPS units that must undergo adaptations to resolve issues related to the pandemic. However, only employees showed interest in this topic and brought in design ideas to adjust the CAPS environment to caring for patients without exposing them to risks associated with respiratory diseases. Patients were more interested in telling stories and personal experiences that occurred within the unit, creating “Dream Caps” that could reduce the chance of personal and interpersonal conflicts they had in a time prior to the pandemic. When asked about adaptations that could minimize the risk of contracting COVID-19, they claimed they did not have the necessary knowledge to contribute.
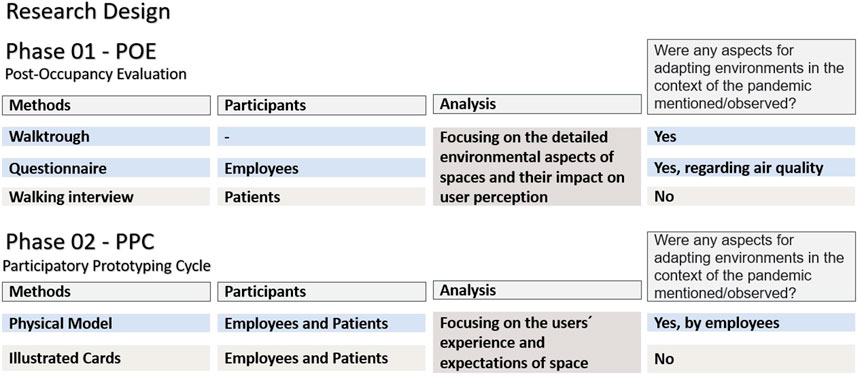
FIGURE 2. Diagram of the research design, illustrating which of the applied methods resulted in relevant information for functional and technical adaptations in post COVID-19 reality.
3.1 Phase 01—Post-occupancy evaluation
The buildings selected for this study were not initially designed as community mental healthcare service facilities. They are rented properties that underwent extensive renovations to suit the programming of a CAPS unit. Renting and adapting buildings to a specific purpose, such as the case-study buildings, are currently the prevalent practice in Brazil’s Unified Healthcare System. On this account, units B and C, which are adapted residential buildings, had undersized corridors and fragmented circulation (Figure 3). Particularly in unit C, inpatients must cross the kitchen and dining room to reach the courtyard. No case-study buildings featured an overnight stay bedroom for staff. Units B and C had different accommodations for the Medication Room and the Nurses’ Station, which means that testing procedures for COVID-19 can take place in a controlled and restricted environment. Additionally, in the case of Unit B, the Nurses’ Station was attached to the Medication Room so that ill patients could rest undisturbed in a different environment.
Most employees in units B and C agree that the air quality is adequate (Figure 4). Except for one person, participants in unit C do not consider the air in their workplaces to be unbreathable. In unit B, four participants (11% of the sample) partially agreed that the air was unbreathable up from the basement dayroom and that group room did not have any cross-ventilation. In unit A, a considerable number of people feel that the air quality is inadequate (13 participants, 46% of the sample). Unit A had rooms with no natural or mechanical ventilation, such as the dining room and bathrooms. Therefore, some participants completely (three participants, 11% of the sample) or partially (6 participants, 22% of the sample) agreed that the air in the unit is unbreathable. Of the three units, only unit B had an air-conditioning system, and most of its employees fully agreed (27 participants, 75% of the sample) that it is efficient.
Unit C adopted an interior design style that resembles a homelike environment, featuring colored walls, comfortable furniture, works of art, indoor plants, among other things. In addition, this facility had the most compelling courtyard, with four ambiances: one therapeutic garden, one patio for physical activities, a reception garden, and a front patio. Regarding humanization, Unit B had also made efforts to adapt its environment accordingly. However, the small size of the dayroom and reception lounge are obstacles to a comfortable, homelike atmosphere. Although having the largest area, Unit A still needs to invest in humanization elements. Its courtyard had few places to sit, few decorative elements, plain white walls, and hidden corners, far from the nurses’ supervision (Figure 5).

FIGURE 5. Compilation of photographs of the internal and external environments of the investigated units.
The technical visits also surveyed the environmental aspects that might contain the spread of the SARS-CoV-2 virus within the building. These consist of pre-existing building characteristics (size of the rooms, building configuration, air renovation systems) and adaptations made by workers to use and occupy the space (adaptations in inpatient accommodations, circulation control, installation of monitoring stations). Table 1 features these design aspects.
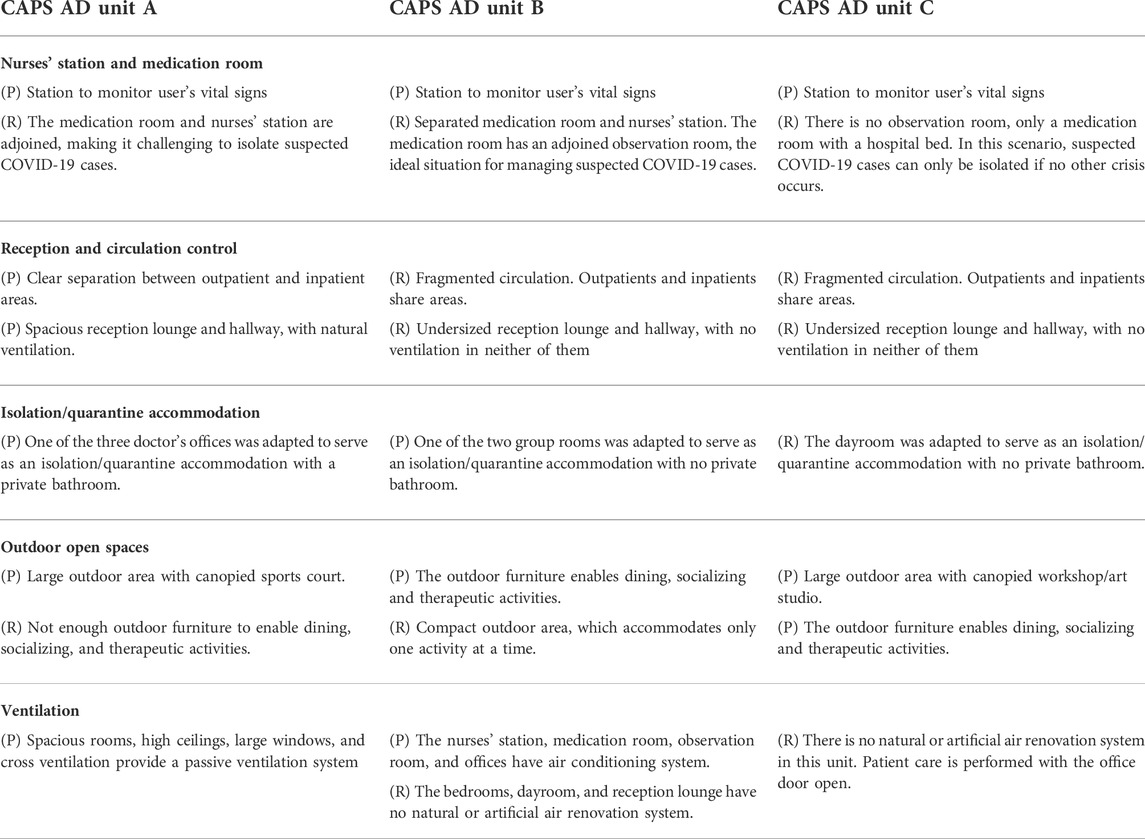
TABLE 1. Aspects of the building’s configuration that prevents (P) or increases risk (R) of COVID-19 spread.
3.2 Phase 02—“Dream CAPS” participatory prototyping circle
During the “Dream CAPS” interactive 3D model, all 25 participants suggested adjustments in the building designs to meet several technical and functional needs. However, only 14 participants expressed the need to adapt their buildings to meet criteria related explicitly to managing patients with COVID-19 or suspected COVID-19 cases. Of these participants, five are from unit A (two nurses, one psychologist, one occupational therapist, and one social worker), six from unit B (two pharmacists, two occupational therapists, one social worker and one nurse), and three from unit C (one psychologist, one occupational therapist and one nurse). These participants’ suggestions are the key content analyzed in this manuscript. They mentioned several design strategies that may help weaken the spread of COVID-19 throughout the facility (Table 2). These strategies included increased ventilation (two participants), rooms adapted for the accommodation of patients with COVID-19 or its suspected cases (two participants), building stations to monitor user’s vital signs (three participants), larger open areas that support dining, socializing, and therapeutic activities (three participants), and materials and finishings that are resistant to terminal cleaning1 (four participants).
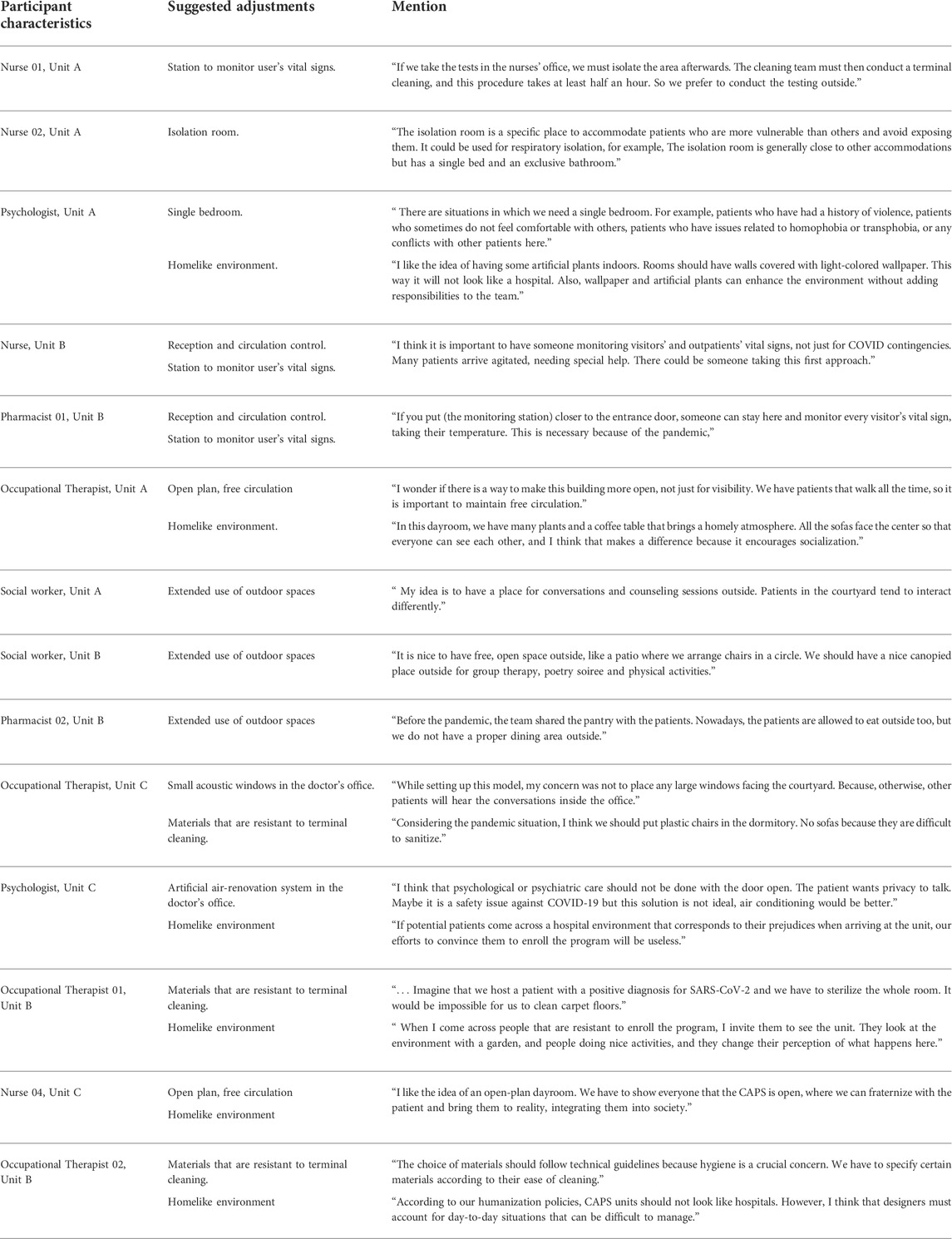
TABLE 2. Participants’ opinions on the impact that the COVID-19 pandemic had on the CAPS unit’s environmental quality.
Participants showed concern that some of these design strategies might hinder their efforts to humanize the mental healthcare service. For example, easy-to-clean material was deemed an institutional style compared to homelike furniture and finishings (six participants). Also, some workers understood that excessive surveillance and controlled environments were against the CAPS’ open-door policy (two participants). However, during the assembly of the models, no one completely rejected the idea of using elements made of wood, fabric, or wallpapers. Also, few models did not show the use of any metallic hospital furniture, which is resistant and easier to clean and resistant. All models sought to balance the use of residential and hospital furniture (Figures 6, 7).
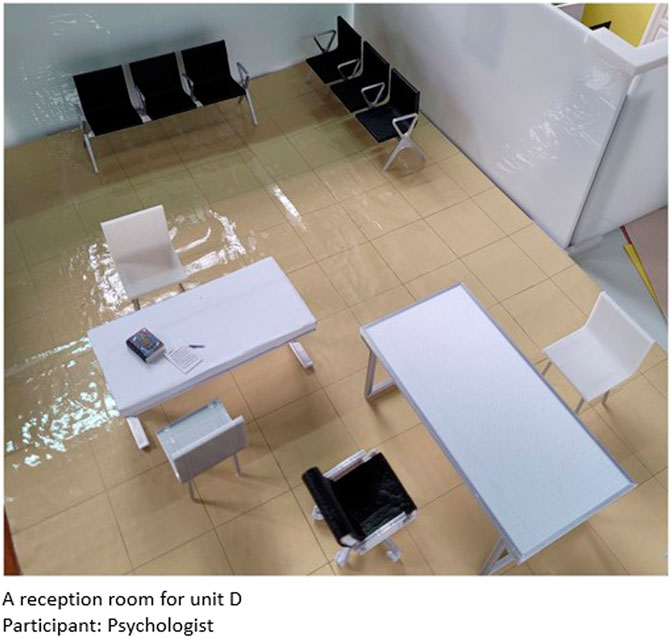
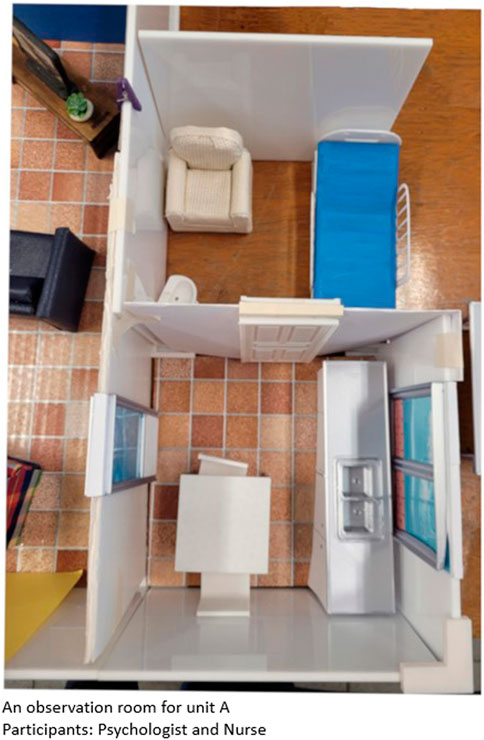
Eleven physical models customized by the mental healthcare workers had an open-plan dayroom (Figure 8). Participants claimed that this configuration could enhance natural ventilation, patient interaction, and surveillance. Two models (four participants) opted to have a medication room opening towards the nurses’ office (Figure 9). One participant designed an isolation and quarantine room exclusively for COVID-19 cases (Figure 10). One participant designed a reception room with a trial station in a separate anteroom (Figure 11).
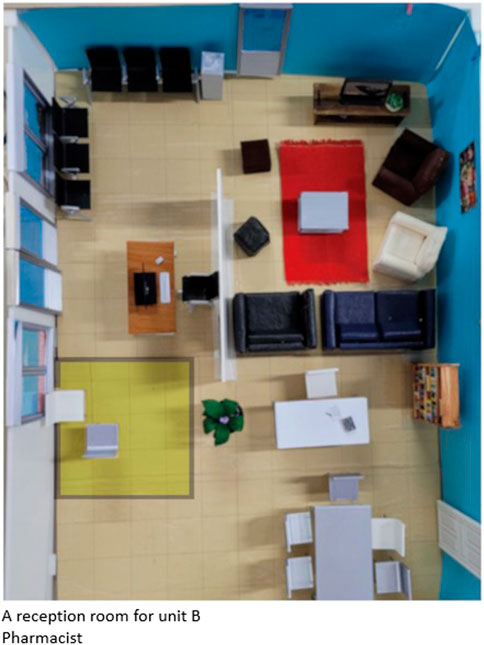
FIGURE 11. Connected Reception Room and Dayroom with a trial station in a separate anteroom—marked in yellow.
4 Discussion
Brazilian CAPS are mental healthcare services that follow the community-based model of care, offering comprehensive treatment delivered by a multidisciplinary team of counselors, occupational therapists, psychologists, psychiatrists, pharmacists, among others. Its service network provides a full range of psychiatric care for both inpatients and outpatients. During the first months of the COVID-19 pandemic, the CAPS AD III units had to discontinue their daily outpatient services and group activities, restricting general psychiatric services to urgent cases and people in extreme vulnerability. This protocol is similar to the Italian experience (D’Agostino et al., 2020) and it was implemented in all Brazilian CAPS units.
However, the pandemic has proved to be an additional stressor for the mentally ill, limiting their social networking and support systems, as well as worsening their prognosis (Mukhtar and Rana, 2020). In order to resume their services, the CAPS AD III workers had to make a series of adjustments to their environment to reduce the risks of COVID-19 infection without depreciating the quality of the community-based service. This study verified that a POE allied to codesigning activities created an environment conducive to dialogue. The participants availed themselves of this opportunity to express their recent experiences, suggest new alternatives for the use of space, and discuss its feasibility with an architect.
There is a growing interest in involving health professionals (and patients) in participative procedures to improve service care using surveys, interviews, focus groups, and observations (Robert et al., 2015). Nevertheless, only a handful of studies use these user-centered techniques to improve the design of mental healthcare facilities (Tyson et al., 2002; Cleary et al., 2009; Daykin et al., 2010; Novotná et al., 2011; Van Der Schaaf et al., 2013; Shepley et al., 2016; Liddicoat, 2019). Both POE and codesign are considered user-centered design methodologies, but the latter is defined as having greater user participation (Sanders and Stappers, 2008). POE is an excellent technique for gaining feedback on how the building supports the occupying organization and individual end-users, but multi-method approaches are necessary to access contingent cases (Jensen et al., 2011). In this study, applying the POE during the first phase of data collection was essential to understand how the building configuration affected mental healthcare services during the COVID-19 pandemic and what design features were preventing or facilitating COVID-19 spread. The “Dream CAPS” codesigning activity made the participants 1) reflect on general questions about the importance of the physical environment for mental healthcare and 2) highlight relevant aspects of a more urgent problem, more specifically the adaptation of units to prevent the spread of the COVID-19 virus. These in-depth discussions were fundamental for accessing the healthcare workers’ experience since they facilitated a focused and responsive conversation on the issues raised during the POE.
The design of mental healthcare facilities must satisfy the user’s needs and correspond to the current health protocols. Nonetheless, mental healthcare services continually incorporate new technologies and treatment methods, and these changes pressure the facility infrastructure, creating demands for functional and technical adaptations. The changes caused by the COVID-19 pandemic were abrupt and urgent, and this situation evinced the need for a specific toolkit to incorporate occupant experience into design adjustments, and make adaptations more efficient.
4.1 Places that support risk mitigation procedures
Since the pandemic began, the administration of CAPS AD III units has implemented several contingency protocols, including procedures for identifying, containing, and treating suspected COVID-19 cases. This demand requires several design changes, because mental healthcare facilities typically do not have the same infection-precaution elements of hospital environments (Van der Voordt, 2021). Ideally, the CAPS AD III units would have separate rooms for the nurses to carry out administrative tasks, manage medications and observe patients in acute care. In the case of CAPS AD III unit A, all these tasks happen in the same space, whereas unit C had one single room for administering medication and observing patients. Participants describe the experience of working in a unit where there is no separation between spaces for daily patient care and spaces for testing and managing suspected COVID-19 cases as inconvenient and unproductive (Nurse 01, unit A, Table 2).
Participants also brought up considerations about the accommodations for comprehensive-care patients (Table 2). A community mental healthcare unit like CAPS AD III provides care for people with psychological distress where they live. However, some patients might need comprehensive care for numerous reasons. It is possible to mention, for instance, people with substance use disorder in need of rehabilitation, people suffering from violence or deprivation within their home, and people without adequate housing. To continually provide this type of service during the COVID-19 pandemic, mental healthcare facilities must isolate patients who are positive for SARS-CoV-2 (D’Agostino et al., 2020; Moreno et al., 2020). During the PPC, two participants highlighted the need for individual accommodations for patients with airborne diseases and other vulnerabilities (Nurse 02, psychologist, unit A, Table 2).
The proposed “isolation room” should not be understood or used as a seclusion room, i.e., a place for the involuntary confinement of a distressed or agitated person (IHFG, 2010). Unlike the seclusion room, the isolation room has a private bathroom and can feature decorative elements, counters, and cabinets, as long as they are resistant to terminal cleaning. A participant commented on further advantages of having a single bedroom in CAPS AD III units, like its usefulness in accommodating vulnerable patients or interpersonal conflict situations. (Psychologist, unit A, Table 2).
According to healthcare design specialists, single bedrooms threaten patient and staff safety because they are difficult to supervise (Tyson et al., 2002; Shepley et al., 2016). Nonetheless, private spaces increase patients’ autonomy and well-being, reduce noise, and, in some cases, increase participation in the treatment (Karlin and Zeiss, 2006; Van Der Schaaf et al., 2013; Ulrich et al., 2018). Private rooms might be more common in the future, considering their infection-control benefits (Van der Voordt, 2021).
Suggestions put forward during the PPC include building an enclosed space for testing and observing short-time inpatients under suspicion of COVID-19 infection. First, newcomers should undergo a clinical examination and rapid antigen test in the observation room. Then, if positive for SARS-CoV-2, the patient would be directed to the individual accommodation suite, where they would be kept in respiratory isolation for the necessary period of time.
4.2 Access and circulation control
The lack of adequate infrastructure led the staff of all three case studies to set temporary tents at the facility’s main entrance to check outpatients’ vital signs, store and dispose of personal protective equipment (PPE), and clean hands. Despite being temporary, implementing this “trialing tent” brought advantages in controlling people’s access to the unit. As mentioned by one participant (Nurse, Unit B, Table 2), the person in charge of the trials further assists the staff by welcoming new patients, giving general information about the service, and supporting people in distress. Thus, the trial station should become permanent, given its potential to strengthen humanized reception practices.
An alternative solution presented in one of the “Dream CAPS” models featured a trial station inside the unit, at a distance from the reception desk, in a separate anteroom or front porch (Pharmacist, Unit B, Figure 8). This proposal compensates for the inconvenience that small tents cause since they do not offer adequate protection against bad weather and accommodate only two people at a time.
The models created during the codesign activity had different configurations, but they all sought to follow the guidelines of an open-door care policy. “Open door” refers to the deinstitutionalization of patients and the development of actions promoting patient autonomy and community insertion (Sampaio and Bispo Júnior, 2021). In architecture, “open door” refers to large openings, free-flowing circulation, open-plan dayrooms, and many outdoor and indoor communal and living spaces. While customizing their models, some participants explained how these design choices made the space proper for developing patients’ abilities, such as autonomy, socialization, sense of freedom, and co-presence (Occupational therapist, unit A, nurse, unit C, Table 2).
Unfortunately, some design strategies that prevent airborne disease contamination can make the CAPS environment seem contained, limiting, and controlling. Social distancing is one of the most effective COVID-19 control strategies (Fadaei, 2021), implemented in many mental health services for infection-control measures (Moreno et al., 2020). However, reducing patients’ access to communal rooms and living spaces neutralizes the “open-door” concept. Architects should emphasize other solutions to compensate for the fact that circulation control is not appropriate for a community mental healthcare unit.
4.3 Extended use of outdoor spaces
A comprehensive mental healthcare program offers several health-promotion activities in designated spaces, such as educational kitchens, communal dining areas, group activity rooms, coffee lounges, fitness facilities, libraries, and dayrooms (Davis et al., 1979; Gross et al., 1998; Karlin and Zeiss, 2006; Van der Voordt, 2021). However, crowding people indoors hampers social distancing and increases the risk of virus spreading (Burridge et al., 2021). Therefore, it is convenient to have a large, multi-use outdoor area to which most group activities can be transferred, as suggested by some participants (Social Worker, unit A, Pharmacist 2, unit B, Social Worker, unit C, Table 2).
Outdoor weather-protected private spaces are ideal for group meetings, family visits, and counseling. Also, increasing the area of outdoor spaces allows for a greater variety of nature-related therapeutic activities (planting, caring for plants and harvesting), physical activities, and quietness and relaxation experience (Whitehead et al., 1976; Gross et al., 1998; Marcheschi et al., 2016; Shepley et al., 2016; Ulrich et al., 2018).
People with psychological distress living in mental healthcare institutions wish for more freedom of movement and less control over their actions (Smith et al., 1996; Cleary et al., 2009; Novotná et al., 2011). The offering of a wide range of outdoor activities may naturally attract inpatients to environments that are therapeutic and offer lower contamination risk.
4.4 Natural and artificial air renovation systems
Temperature and humidity control influences SARS-CoV-2 survival time in the air and on surfaces, and the supply of clean outdoor air dilutes any virus particles and pollutants indoors. Ideally, healthcare settings and public buildings should have a high-efficiency particulate air-filtering system that combines particle filtration and air renewal. If not installed properly, conventional artificial air renovation systems may cause further dissemination of respiratory droplets containing pathogens within the facility (Burridge et al., 2021; Fadaei, 2021).
Data collected during the POE shows that none of the case-study buildings had an adequate air renovation system. Unit B had a split HVAC system installed in the healthcare team’s working rooms. However, dayrooms, bedrooms, and other indoor spaces where patients stayed had ceiling fans. In unit C, rooms had no natural or artificial ventilation solutions other than simple ceiling fans. Ceiling fans only increase air mixing within a room and must be installed close to oversized windows to enhance the bulk supply of outdoor air (Burridge et al., 2021). Unit A performed best in general, combining several design elements that favor passive ventilation (cross ventilation, high ceilings, large windows, and spacious rooms). However, the bathrooms and the dining room were built without any type of mechanical or natural ventilation, which is why some participants deemed the air as “unbreathable.” It is of utmost importance to install air renewal systems in these spaces to purify the environment of viruses such as SARS-CoV-2 and mainly to reduce the risk of mold and other microorganisms.
During the COVID-19 pandemic, the administration of the analyzed CAPS AD units advised workers to leave windows and doors wide open while examining or hearing the patient. This strategy aimed to increase the supply of outside air. Nevertheless, two participants pointed out that this caused several privacy-related issues (Psychologist, occupational therapist, unit C, Table 2).
A patient’s fundamental right to privacy should never be impaired, as highlighted in the guidelines of the Brazilian Program for Mental Healthcare Humanization (Brasil, 2004). On this account, doors and windows must be kept closed during private sessions. Proper investment should be made in air conditioning systems to guarantee adequate air quality inside the CAPS AD enclosed spaces. A proper ventilation system combines technologies to control the temperature and humidity and purify the air in order to decrease the survival of the SARS-CoV-2 virus, including key features such as HEPA filters, UV cleaners, or photocatalytic oxidation (Burridge et al., 2021; Fadaei, 2021).
4.5 Terminal cleaning-proof materials and finishings
Research indicates that SARS-CoV-2 has different survival periods on distinct surfaces, varying from 3 h (on paper and tissues) to up to 72 h (on hard and smooth surfaces, such as plastic and stainless steel) (Burridge et al., 2021). These facts led to the recommendation of regularly cleaning often-handed objects and surfaces in public spaces. Participants of this study reported that thorough cleaning (denominated “terminal cleaning”) became more recurrent because of the COVID-19 pandemic. The usual protocol includes daily terminal cleaning in bedrooms, nurse stations, and bathrooms, and weekly cleaning of dining rooms, dayrooms, and offices. The medication room and the observation room were cleaned after each use. Therefore, furniture and surfaces need to be made with materials resistant to heavy cleaning products to ensure durability.
Choosing the correct furniture set was one of the participants’ major concerns. Most psychotherapists in this study mentioned that materials resistant to deep cleaning procedures (white ceramics, smooth walls, metal furniture) do not correspond to the residential-style architecture, an essential aspect in community mental healthcare settings. The residential-style design consists of the aesthetic choices that create homelike environments. This design strategy is preferred by patients, especially women, and aims to create a welcoming, familiar and comfortable environment for all (Vaaler et al., 2005). According to the participants, residential-style architecture can dissociate the CAPS unit from the image of the psychiatric asylum, facilitating patient engagement in the program (Psychologist, unit C, occupational therapist 01, unit B, Table 2).
The results of the codesign activities show that mental healthcare facilities should not give up every decorative or residential element for the sake of sanitization. Elements that correspond to residential aesthetics are textured walls, colored ceramic tiles, low ceilings, window curtains, wooden cabinets, upholstered chairs and sofas, floral arrangements, potted plants, and personal items in the patients’ rooms. (Davis et al., 1979; Devlin, 1992; Gross et al., 1998; Vaaler et al., 2005). Now that airborne diseases are preeminent, some residential elements that accumulate dirt, bacteria, and viruses, such as carpets and rugs, no longer make sense in a public healthcare building (Occupational Therapist 01, unit B, Table 2). On the other hand, decorations like plants, wallpapers, or paintings must be kept in favor of a more welcoming environment (Psychologist, Occupational Therapist, unit A, Table 2).
The built environment is crucial in portraying the type of care delivered and profoundly affects the relationship between therapists and their patients (Anthony and McCaffrey, 2018). During the PPC, the architect and mental healthcare workers came up with two solutions to maintain the residential atmosphere without overburdening the cleaning staff. First, by using synthetic versions of natural materials, such as faux leather upholstery, wood-look porcelain tiles, and other faux wood floorings. Notably, these choices would increase building costs significantly. Another proposed solution was furnishing just the isolation and medication rooms with materials and finishings suitable to withstand terminal cleaning. Patients with COVID-19 or waiting for viral test results could use this accommodation, while other rooms would feature common residential-style materials and furniture.
4.6 Methodological lessons
The study presented here shows how implementing a Post-Occupancy Evaluation, combined with codesign methods, leads to an outright comprehension of a building architecture. During the first phase of data collection, POE focused on detailed environmental aspects of spaces and their impact on user perception. This information provided a good understanding of how the unit works and on aspects related to its ambiance. Also, we could seize which new demands have been incorporated into the program since the construction of these buildings. The codesign activity was then developed to discuss these issues with the participants and seek solutions to problems identified during the POE, focusing on the users’ experience and expectations of space.
From a methodological point of view, four valuable lessons were learned from conducting the chosen methods and techniques. Firstly, carrying out successive walkthroughs during phase 01 was fundamental to thoroughly document the functional, technical-physical and environmental aspects of the building. This way, it was possible to anticipate issues to discuss over the walkthrough with the expert and make the most of this opportunity. The fact that the administrative staff of each unit had know-how in both COVID-19 contingency plan strategies and psychiatric services was very fortunate. Future applications of this method in other contexts may require the researcher to run more than one walkthrough with the experts. The second lesson relates to the decision to run a preliminary analysis of the POE before implementing the PPC, optimizing the assembling of the “Dream CAPS” codesigning tool. Observations during the first phase brought out the need to discuss issues related to ventilation, circulation routes, occupation of outdoor spaces, and terminal cleaning-proof materials. Regarding the time gap between the two phases, it was possible to incorporate the model objects that would trigger conversations about these relevant aspects.
Another methodological lesson relates to conducting the illustrated cards immediately after the customization of the 3D model. This tool was useful to access participants’ first impressions of mental healthcare environments and to reinforce some themes that emerged during the previous activity. However, the images showed spaces designed in a pre-pandemic context in a way that did not inspire participants to discuss functional and technical adaptations in post COVID-19 reality. On further reflection, it would be interesting to design a third data collection phase to test the proposed redesign’s results. In this case, photo-realistic images of the adaptations proposed during the PPC could be incorporated into the illustrated cards collection.
Finally, we have observed that patients’ contributions focused mainly on formal aspects of the buildings, such as aesthetics, cultural values, and symbolic meanings. Despite being motivated and willing to participate, patients showed some insecurity in addressing functional aspects, construction aspects, and cost-effectiveness. Previous research reports have drawn attention to the insecurity and self-consciousness of mental health patients during codesign activities, which lessens when the environment in which participatory design unfolds is transparent, flexible, secure, and informal (Springham and Robert 2015; Terp et al., 2016).
A dilemma arose after comparing the results of the two data collection phases. Namely, design strategies that prevent or increases risk of COVID-19 spread conflict with mental healthcare humanization policies. For instance:
a. The programme of requirements in a CAPS AD III includes collective dormitories, dayrooms, and activity spaces, so that the participants may develop their social skills and interact with peers. However, collective spaces may get crowded, compromising social distancing strategies.
b. The need to control patients’ access and circulation through the facility conflicts with the CAPS “open-door” policy.
c. The recommendation to leave windows open to reduce the incidence of SARS-CoV-2 aerosol exposure compromises privacy, an essential element in patient-to-carer interactions.
d. Terminal cleaning-proof materials and finishings like plastic walls and stainless-steel surfaces are seen as too bleak and, because of that, prone to impair the efforts to design a welcoming atmosphere.
During the application of the codesigning activities, these issues could be discussed extensively, and the participants came up with reasonable solutions that could be easily implemented:
a. An isolation bedroom must be built to settle patients with respiratory symptoms or needing specialized care. This way, collective spaces would be available for use by those patients who have already been tested for COVID-19. Co-created solutions also include environmental enrichment of outdoor areas so that more activities can be transferred to these places.
b. Quick testing and trials at the entrance of the building can ensure that every person circulating throughout the facility is free of COVID. So, wandering patients would be free to explore the facility, experiencing greater autonomy and perceived control.
c. Ideally, every room should have air-conditioning with HEPA filtering. Nevertheless, considering budget limitations or the impracticality of a major renovation, rooms used for interactions between patient and healthcare worker should be prioritized.
d. The medication and isolation rooms must be furnished with materials that withstand terminal cleaning. In other spaces, the interior design project should prioritize the use of synthetic versions of natural materials, which have greater durability and resistance to heavy cleaning products.
Finally, with the proposed method, it was possible to investigate the reality of CAPS AD III units in the post-pandemic context and use the knowledge and experience of their workers to propose new design solutions and overcome problems. The results of this study can be implemented in other mental healthcare buildings, especially those that operate according to the community mental healthcare model. Broadly, every public facility that offers daily social assistance can benefit from the design solutions proposed here: Adult daycares, women’s shelters, homeless people’s shelters, youth centers, and others. Psychiatric wards in hospitals, where patients are cared for on inpatient basis, can benefit from applying the combination of POE and codesign methods, as proposed in this study, to find tailored solutions for their stricter safety protocols.
5 Conclusion
Healthcare establishments are constantly demanding functional and technical adaptations to accommodate new necessities. New demands could derive from changes in therapeutic procedures, equipment upgrades, or, in the case of this study, the emergence of new health threats. As shown, the combination of a Post-Occupancy Evaluation and a codesign activity was an excellent strategy to survey mental healthcare workers’ challenges and opinions on their environment and help them find solutions for the dificulties they have faced during the pandemic. This methodology assisted users in expressing their experiences and knowledge about the CAPS environment, providing relevant data and insights on how the space should be designed.
One of this study limitations was the time taken to prototype and build the “Dream CAPS” model. This 3D model was handmade, specifically for this study, using mixed methods with fabric and wooden pieces combined with 3D-printed plastic models. Another relevant limitation is the lack of testing the results of the proposed redesign in a realistic context. Virtual reality tools are promising, less time-consuming alternative that can solve both problems mentioned above (Liddicoat, 2019). Further studies could investigate the usefulness of computer-aided codesign tools in this context.
Codesign methods have the potential to make patient-centered services a reality (Robert et al., 2015). This research contributes to the environmental quality of mental healthcare facilities by presenting a proper toolbox for participatory design in this context. Through this method, designers can develop adaptation projects that can accommodate new demands without negatively influencing caregivers’ work quality and patients’ freedom and autonomy (Sanoff, 2001).
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Comitê de Ética em Pesquisa da Escola de Artes, Ciências e Humanidades da Universidade de São Paulo (CEP EACH USP). The patients/participants provided their written informed consent to participate in this study.
Author contributions
FG and RO contributed to the conception and design of the study. FG collected data and organized the database. FG wrote the first draft of the manuscript. RO contributed to manuscript revision and read.
Funding
This research was funded by the São Paulo Research Foundation—FAPESP and the Brazilian National Council for Scientific and Technological Development—CNPq. A Ph.D. scholarship was made available to Fernanda Goulart (FAPESP—process no 2018/25152-1), and a level two productivity scholarship was made available to Rosaria Ono (CNPq—process no 08638/20204).
Acknowledgments
This work would not have been possible without the support of the managers and workers of the investigated CAPS AD III unit, who provided their time to contribute to the data collection. Special thanks to the Municipal Health Department of São Paulo, our co-participant, for facilitating the contact with the building’s managers.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1Terminal cleaning is the standard protocol for the disinfection of healthcare spaces, required in circumstances of disease outbreak or increased infection risk. It consists of the thorough cleaning and disinfection of all surfaces, including floors and furniture within a specific room.
References
Andrade, C., Lima, M. L., Fornara, F., and Bonaiuto, M. (2012). Users’ views of hospital environmental quality: Validation of the perceived hospital environment quality Indicators (PHEQIs). J. Environ. Psychol. 32, 97–111. doi:10.1016/j.jenvp.2011.12.001
Anthony, K. H., and McCaffrey, K. (2018). Designing mental and behavioral health facilities: Psychological, social, and cultural issues. Elsevier. doi:10.1016/B978-0-12-811481-0.00013-5
Brasil (2004). HumanizaSUS Política Nacional de Humanização: A Humanização como Eixo Norteador das Práticas de Atenção e Gestão em Todas as instâncias do SUS. Série B. Textos Básicos de Saúde. 1st ed. Brasília, DF.
Brunoni, A. R., Suen, P. J. C., Bacch, P. S., Razza, L. B., Klein, I., dos Santos, L. A., et al. (2021). Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: Findings from the elsa-brasil covid-19 mental health cohort. Psychol. Med., 1–12. doi:10.1017/S0033291721001719
Burridge, H. C., Bhagat, R. K., Stettler, M. E. J., Kumar, P., De Mel, I., Demis, P., et al. (2021). The ventilation of buildings and other mitigating measures for COVID-19: A focus on wintertime. Proc. R. Soc. A A477, 20200855. doi:10.1098/rspa.2020.0855
Cleary, M., Hunt, G., and Walter, G. (2009). A comparison of patient and staff satisfaction with services after relocating to a new purpose-built mental health facility. Australas. Psychiatry 17, 212–217. doi:10.1080/10398560802691693
D’Agostino, A., Demartini, B., Cavallotti, S., and Gambini, O. (2020). Mental health services in Italy during the COVID-19 outbreak. Lancet Psychiatry 7, 385–387. doi:10.1016/S2215-0366(20)30133-4
Davis, C., Glick, I. D., and Rosow, I. (1979). The architectural design of a psychotherapeutic milieu. Psychiatr. Serv. 30, 453–460. doi:10.1176/ps.30.7.453
Daykin, N., Byrne, E., Soteriou, T., and O’Connor, S. (2010). Using arts to enhance mental healthcare environments: Findings from qualitative research. Arts Health 2, 33–46. doi:10.1080/17533010903031408
Devlin, A. S. (1992). Psychiatric ward renovation: Staff perception and patient behavior. Environ. Behav. 24 (1), 66–84. doi:10.1177/07399863870092005
Elali, G. A. (2009). “Relações Entre Comportamento Humano e Ambiência: Uma Reflexão Com Base Na Psicologia Ambiental,” in International Colloquium Ambiences Em Partage: Culture, Corps et Language, 1–17.
Fadaei, A. (2021). Ventilation systems and COVID-19 spread: Evidence from a systematic review study. Eur. J. Sustain. Dev. Res. 5, em0157. doi:10.21601/ejosdr/10845
Ferreira, D. C. S., Oliveira, W. L., Delabrida, Z. L. C., Faro, A., and Cerqueira-santos, E. (2020). Intolerance of uncertainty and mental health in Brazil during the covid-19 pandemic. SUMA Psicológica 27 (1), 62–69. doi:10.14349/sumapsi.2020.v27.n1.8
Gross, R., Sasson, Y., Zarhy, M., and Zohar, J. (1998). Healing environment in psychiatric hospital design. Gen. Hosp. Psychiatry 20, 108–114. doi:10.1016/S0163-8343(98)00007-3
Holland, K. M., Jones, C., Vivolo-Kantor, A. M., Idaikkadar, N., Hoots, M. Z. B., Yard, E., et al. (2021). Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 78 (4), 372–379. doi:10.1001/jamapsychiatry.2020.4402
International Health Facility Guidelines (2010). Seclusion room data sheet. Stand. Components. Available at: https://www.healthfacilityguidelines.com/StandardComponents/ItemDetails/Seclusion-Room.
Jensen, P. A., Alexander, K., and Fronczek-munter, A. (2011). “Towards an agenda for user oriented research,” in Construction, 25–42.
Karlin, B. E., and Zeiss, R. A. (2006). Best practices: Environmental and therapeutic issues in psychiatric hospital design: Toward best practices. Psychiatr. Serv. 57, 1376–1378. doi:10.1176/ps.2006.57.10.1376
Liddicoat, S. (2019). Mental health facility codesign: A new research method for integrating the service user voice in design processes using virtual reality. Gen. Psychiatr. 32, e100061–e100066. doi:10.1136/gpsych-2019-100061
Marcheschi, E., Johansson, M., Laike, T., and Brunt, D. (2016). Housing design and people with severe mental illness: An observational approach to the investigation of supported housing facilities. Scand. J. Psychol. 57, 12–21. doi:10.1111/sjop.12259
Maulik, P. K., Thornicroft, G., and Saxena, S. (2020). Roadmap to strengthen global mental health systems to tackle the impact of the COVID-19 pandemic. Int. J. Ment. Health Syst. 14 (1), 57–13. doi:10.1186/s13033-020-00393-4
Morais, R., Andrade, C., Bernardes, S., and Pereira, C. R. (2015). Escalas de Medida da percepção da qualidade do ambiente hospitalar - um estudo em unidades de Dor. Psic, Teor. Pesq. 31 (3), 381–388. doi:10.1590/0102-37722015031906381388
Moreno, C., Wykes, T., Galderisi, S., Nordentoft, M., Crossley, N., Jones, N., et al. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 7, 813–824. doi:10.1016/S2215-0366(20)30307-2
Mukhtar, S., and Rana, W. (2020). COVID-19 and individuals with mental illness in psychiatric facilities. Psychiatry Res. 289, 113075. doi:10.1016/j.psychres.2020.113075
Novotná, G., Urbanoski, K. A., and Rush, B. R. (2011). Client-centered design of residential addiction and mental health care facilities: Staff perceptions of their work environment. Qual. Health Res. 21, 1527–1538. doi:10.1177/1049732311413782
O’Connor, K., Muller Neff, D., and Pitman, S. (2018). Burnout in mental health professionals: A systematic review and meta-analysis of prevalence and determinants. Eur. Psychiatr. 53, 74–99. doi:10.1016/j.eurpsy.2018.06.003
Ornstein, S. W., Ono, R., Lopes, P. A., França, A. J. G. L., Kawakita, C. Y., Machado, M. D., et al. (2009). Performance evaluation of a psychiatric facility in São Paulo, Brasil. Facilities 27, 152–167. doi:10.1108/02632770910933161
Pinals, D. A., Hepburn, B., Parks, J., and Stephenson, A. H. (2020). The behavioral health system and its response to COVID–19: A snapshot perspective. Psychiatr. Serv. 71, 1070–1074. doi:10.1176/appi.ps.202000264
Robert, G., Cornwell, J., Locock, L., Purushotham, A., Sturmey, G., and Gager, M. (2015). Patients and staff as codesigners of healthcare services. BMJ 350, g7714. doi:10.1136/bmj.g7714
Sampaio, M. L., and Bispo Júnior, J. P. (2021). Towards comprehensive mental health care: Experiences and challenges of psychosocial care in Brazil. BMC Public Health 21, 1352–1364. doi:10.1186/s12889-021-11397-1
Sanders, E. B. N. (2013). “Prototyping for the design spaces of the future,” in Prototype: Design and craft in the 21st century. Editor L. Valentine (London: Bloomsbury), 188.
Sanders, E. B. N., and Stappers, P. J. (2008). Co-creation and the new landscapes of design. CoDesign 4, 5–18. doi:10.1080/15710880701875068
Sanoff, H. (2001). School building assessment methods. Washington, DC: National Clearinghouse for Educational Facilities.
Shepley, M. M., Watson, A., Pitts, F., Rity, A. G., Spelman, E., Kelkar, J., et al. (2016). Mental and behavioral health environments: Critical considerations for facility design. Gen. Hosp. Psychiatry 42, 15–21. doi:10.1016/j.genhosppsych.2016.06.003
Smith, J., Gross, C., and Roberts, J. (1996). The evolution of a therapeutic environment for patients with long-term mental illness as measured by the Ward Atmosphere Scale. J. Ment. Health 5, 349–360. doi:10.1080/09638239619266
Springham, N., and Robert, G. (2015). Experience based codesign reduces formal complaints on an acute mental health ward. BMJ Qual. Improv. Rep. 4 (1), u209153.w3970. doi:10.1136/bmjquality.u209153.w3970
Sung, C. W., Chen, C. H., Fan, C. Y., Chang, J. H., Hung, C. C., Fu, C. M., et al. (2021). Mental health crisis in healthcare providers in the COVID-19 pandemic: A cross-sectional facility-based survey. BMJ Open 11 (7), e052184. doi:10.1136/bmjopen-2021-052184
Terp, M., Laursen, B. L., Jørgensen, R., Mainz, J., and Bjørnes, C. B. (2016). A room for design: Through participatory design young adults with schizophrenia become strong collaborators. Int. J. Ment. Health Nurs. 25 (6), 496–506. doi:10.1111/inm.12231
Tyson, G. A., Lambert, G., and Beattie, L. (2002). The impact of ward design on the behaviour, occupational satisfaction and wellbeing of psychiatric nurses. Int. J. Ment. Health Nurs. 11, 94–102. doi:10.1046/j.1440-0979.2002.00232.x
Ulrich, R. S., Bogren, L., Gardiner, S. K., and Lundin, S. (2018). Psychiatric ward design can reduce aggressive behavior. J. Environ. Psychol. 57, 53–66. doi:10.1016/j.jenvp.2018.05.002
Vaaler, A. E., Morken, G., and Linaker, O. M. (2005). Effects of different interior decorations in the seclusion area of a psychiatric acute ward. Nord. J. Psychiatry 59, 19–24. doi:10.1080/08039480510018887
Van Der Schaaf, P. S., Dusseldorp, E., Keuning, F. M., Janssen, W. A., and Noorthoorn, E. O. (2013). Impact of the physical environment of psychiatric wards on the use of seclusion. Br. J. Psychiatry 202, 142–149. doi:10.1192/bjp.bp.112.118422
Van der Voordt, T. (2021). Designing for health and wellbeing: Various concepts, similar goals. Gt. Proj. 16, 13–31. doi:10.11606/gtp.v16i4.178190
Van der Voordt, T. J. M., and Van Wegen, H. B. R. (2005). Architecture in Use: An introduction to the programming, design and evaluation of buildings. 1st ed. Bussum, The Netherlands: Thoth. ISBN: 0750664576.
Keywords: codesign, environmental quality, post-occupancy building evaluation, mental healthcare facilities, user-centered design
Citation: Goulart FdM and Ono R (2022) Post-occupancy evaluation and codesign in mental healthcare buildings: User’s input as a driver for functional and technical adaptations in post COVID-19 reality. Front. Built Environ. 8:962940. doi: 10.3389/fbuil.2022.962940
Received: 06 June 2022; Accepted: 12 September 2022;
Published: 06 October 2022.
Edited by:
Theo Van Der Voordt, Delft University of Technology, NetherlandsReviewed by:
Yorgos Spanodimitriou, University of Campania Luigi Vanvitelli, ItalyHoa Vo, Georgia State University, United States
Copyright © 2022 Goulart and Ono. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fernanda de Moraes Goulart, ZmVybmFuZGFtZ291bGFydEB1c3AuYnI=
 Fernanda de Moraes Goulart
Fernanda de Moraes Goulart Rosaria Ono
Rosaria Ono