- Faculty of Architecture, Chiang Mai University, Chiang Mai, Thailand
The unprecedented outbreak of COVID-19 has had a tremendous negative impact on healthcare facilities, especially public hospitals. Thai community hospitals serve as primary care for COVID-19 patients. However, many hospital buildings were constructed in the 1990s and are now becoming outdated. Community hospitals faced many difficulties during the Thailand COVID-19 outbreak. To identify these difficulties this study focused on the physical settings of the community hospital’s outpatient departments (OPD) between 2020 and 2021. Furthermore, the study provided design suggestions for preventing the spread of respiratory infectious diseases. The study used a three-step process of data collection. The first was to observe the physical settings of the OPD buildings of the three hospitals. Secondly, interviews were conducted with thirty healthcare employees: 11 from the first hospital, 11 from the second hospital and 8 from the third hospital. Interviews were transcribed and analyzed using content analysis. Subsequently, the architectural design was produced based on observation and interview analysis. In the third step, the same thirty participants evaluated the architectural design through a focus group. Findings from the interviews led to four themes: 1) factors leading to the accumulation of pathogens, 2) measures for preventing the spread of respiratory diseases, 3) the effect of patient numbers on virus transmission, and 4) suggestions for improving the physical setting of OPDs. The analysis of the four themes led to the preliminary design recommendation, which was evaluated through a focus group, leading to suggestions for the improvement of thirteen areas. The analysis results showed that the participants were satisfied with the architectural design with additional minor recommendations. This study provided originality for the implementation and future development of hospital layout designs that can prevent the spread of COVID-19 throughout Thai community hospitals.
1 Introduction
The outbreak of the unprecedented COVID-19 pandemic led to a large influx of hospital patients (Soria et al., 2021). According to the Center for Disease Control and Prevention (CDC) statistics, the COVID-19 virus has affected more than five hundred million people worldwide, causing almost six million deaths (Centers for Disease Control and Prevention, 2022a). Analogous to the world COVID-19 situation, Thailand reports that there were more than five million COVID-19 cases with thirty thousand deaths (Thailand Ministry of Public Health, 2022). These figures have overwhelmed the country’s healthcare facilities, especially government-owned hospitals. Community hospitals, which are located in every district of Thailand, including the rural areas, act as gatekeepers providing outpatient medical treatments. During the COVID outbreak, the whole community hospital infrastructure was overwhelmed with a high number of patients, causing hygiene and safety standards to become a priority in every hospital. However, the current hygiene standards are outdated and the hospitals were not prepared for the spread of unprecedented respiratory infectious diseases, leading to low-efficiency services in the hospitals (Waroonkun, 2018).
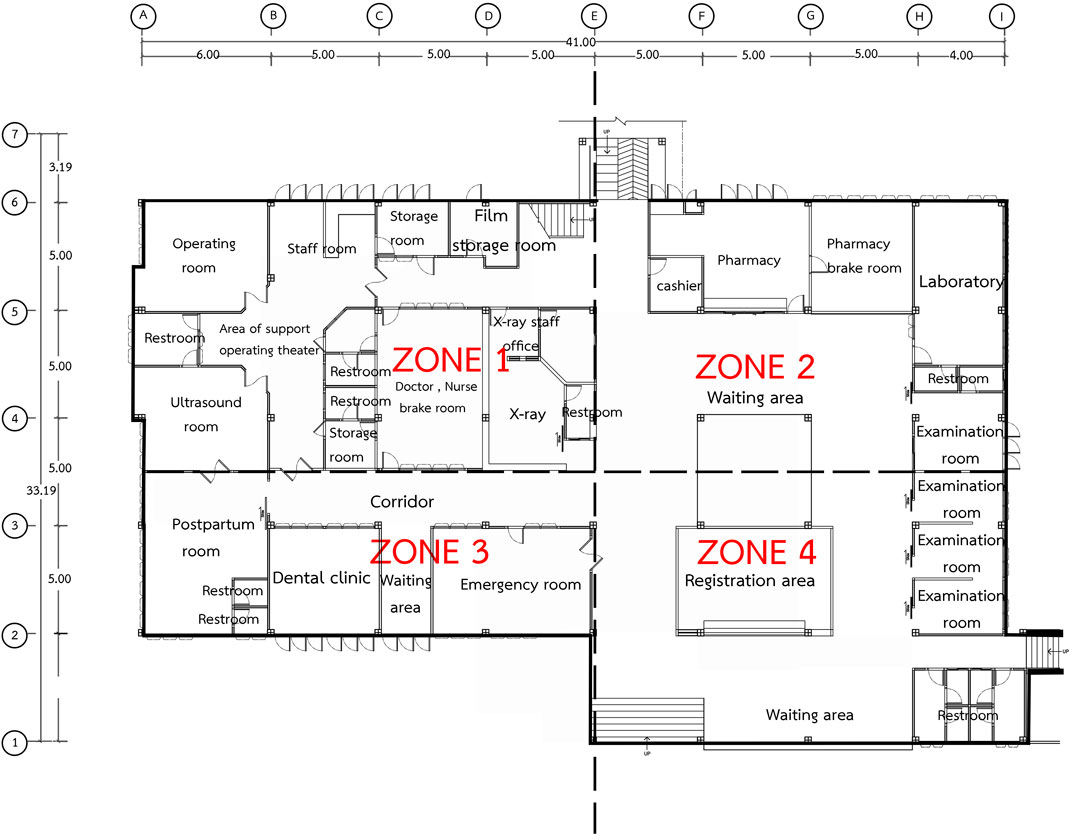
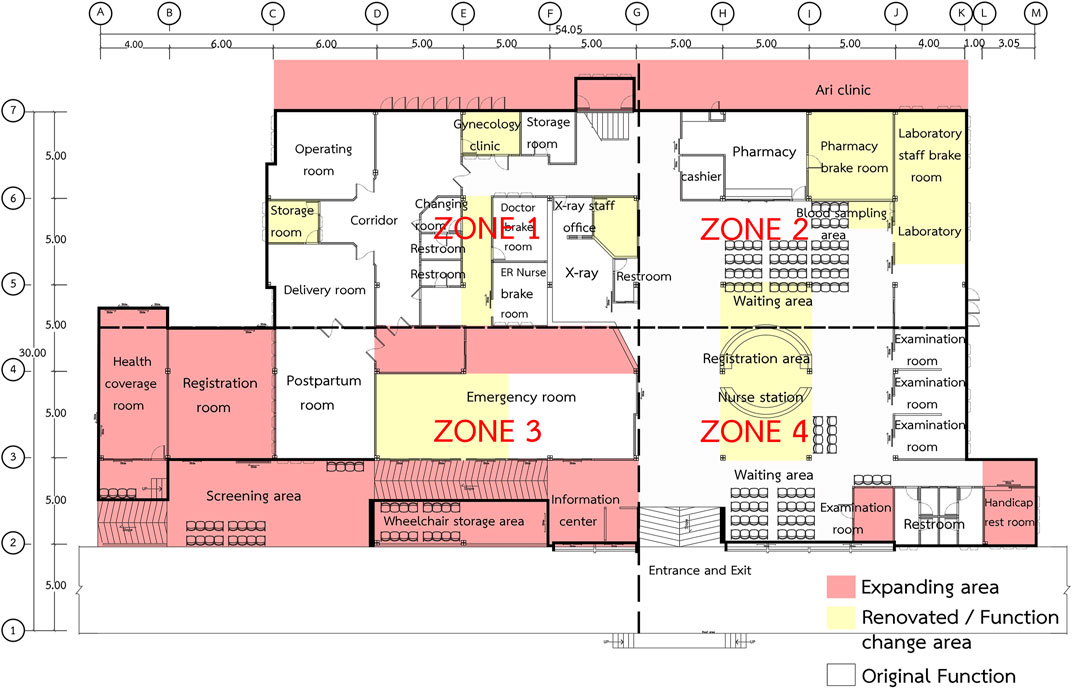
Community hospital outpatient department (OPD) buildings were constructed following the Thai Ministry of Public Health building standard no. 3130 (Figure 1); most of the buildings were built in the 1990s. A recent study conducted by Waroonkun (2018) revealed that most community hospital OPD buildings are obsolete and require rebuilding or renovation. The study also demonstrated that most of the buildings have been through multiple renovations without considering the hygiene standards that would have helped in preventing the spread of COVID-19 (Thailand Ministry of Public Health, 2017; Thailand Ministry of Public Health, 2020). However, it is not possible to demolish and rebuild a new OPD building due to the limited budget of the community hospitals.
Based on building standard no. 3130 (Figure 1) we divided the architectural plan into four zones as follows:
Zone 1
Support area: General storage area of sub sterile equipment, film storage, dark room, clean corridor, control room for X-ray.
Clinical area: Operation, X-ray, delivery room.
Staff area: Doctor and nurse lounge.
Zone 2
Support area: Cashier, dispensary, medicine storage room, health promotion room, waiting area.
Clinical area: Laboratory, examination room
Zone 3
Support area: Waiting room for the dental clinic, wheelchair storage, restroom.
Clinical area: Dental clinic, first aid
Zone 4
Support area: Hall entrance, waiting area, registration, storage, information, restroom.
Clinical area: Examination room
This paper focuses on answering the following research questions: 1) What are the physical problems affecting the community OPD building’s environment? 2) How can a user-focused design approach improve the physical environment of OPD buildings to prevent the spread of COVID-19? Furthermore, the outcome of the user-focused design was developed into hospital design recommendations concentrating on the prevention and spread of respiratory infectious diseases. The study was conducted in three community hospitals: Mae Wang, Doi Saket and Saraphi hospitals. All three OPD buildings share the 3130 building standard and have been through many renovations. Observation of the OPD buildings, in-depth interviews and focus groups with medical staff were used as the main source of data collection.
2 Literature review
2.1 Evidence-based design of hospital facilities
Research conducted in recent years related to the planning and design of healthcare facilities has evolved, emphasising hospital user needs and experiences (Page, 2020; Singh and Lillrank, 2022). Singh and Lillrank (2022) stated that the design of hospital facilities used to stress the function of healthcare provision but neglected patient needs and experiences. However, with the rise of evidence-based hospital design, the design process has shifted from hospital function to patient and medical staff needs.
The term Evidence-based design (EBD) refers to “the deliberate attempt to base building decisions on the best available research evidence to improve outcomes and monitor the success or failure of subsequent decision-making” (Malkin, 2008). In terms of hospital facilities design, the EBD concept can be defined as “the design process, which is guided by an empirical understanding of the effect of the healthcare’s physical environments on safety, efficiency and clinical outcomes” (Hamilton and Watkin, 2009; Ulrich et al., 2008). Therefore, the term EBD can be simplified as implementing the research findings, from the study of a hospital’s built environment, to develop hospital designs that can improve patients’ and users’ health outcomes. (Hamilton, 2003; Ulrich et al., 2008). Malkin (2008) described that in some respects, it can be said that the concept of a healing environment has evolved into EBD, but it is mainly in the area of reduction of stress in patients and staff. Therefore, the term healing environment refers to creating/designing a hospital’s physical environment to reduce patients’ stress levels and improve their clinical health outcomes and well-being (Huisman et al., 2012; Ulrich et al., 2004).
In the past 20 years, the EBD research into hospital facilities has developed, where the concept focuses mainly on safety enhancement, visual environment, audio environment, staff and doctor space features, patient room features, wayfinding and navigation (Fay et al., 2016; Prugsiganont and Waroonkun, 2021). However, with the outbreak of the COVID-19 pandemic, infection prevention and hygiene have become some of the most concerning aspects affecting hospital facilities (World Health Organization, 2022b).
Recently, a user-focused design approach has been adopted as a crucial tool to collect empirical data for EBD studies (Bate and Robert, 2006; Fronczek-Munter, 2016). Fronczek-Munter (2016) explained that a user-focused design approach prioritizes user needs and brings user experience to hospital designers, optimising the design outcome.
2.2 Review of OPD building’s environmental design
Studies conducted in past years emphasizing hospital buildings and OPD areas are described in the research of Pilosof (2021), Miedema et al. (2019), and Gulwadi et al. (2009). In their research on hospital buildings and healthcare promotion in outpatient buildings, they identified the following design features:
• Meet the international hospital standards, which include improving accessibility and navigation, providing air ventilation systems, maintaining an appropriate level of noise, controlling infection and increasing patient privacy.
• Prioritize a patient-centred approach, which includes improving communication between medical staff and patients, and offering access to greenery and arts.
• Provide building flexibility, where the building can be expanded and developed due to changes in medical technology.
Based on studies that focus on hospital buildings and OPD areas, we can conclude that the factors influencing the hospital’s physical environment are operation services, the built environment and hospital design standards.
2.3 Hospital evaluation approach
This study emphasized user-focus design, where building observation, in-depth interviews with medical staff and focus groups were used as the main source of data collection. For the OPD buildings observations, we implemented post-occupancy evaluation (POE) as a tool for data collection. POE has been defined as the process of obtaining feedback on a building’s performance in use (Center of Health Design, 2015; Preiser et al., 2015; Van der Voordt and Van Wegen, 2005). A user-focused approach was employed for data collection related to medical staff opinions. A user-focused approach is equivalent to POE in as much as they both aim to improve future building design using some form of input from intended users (Waroonkun, 2020). To further analyze the study, a focus group was used to evaluate the preliminary design recommendation, which was created based on the medical staff’s in-depth interview analysis. A focus group refers to an interview with a small selection of people, chosen from predefined demographic traits and experiences (Edmunds, 1999). In this study medical staff were recruited for the focus group.
2.4 Hospital design preventing respiratory infection
Current evidence suggests that COVID-19 is an infectious respiratory disease, where the virus can be transmitted through the air and droplets. Airborne viruses can transmit to patients through dust (smaller than 5 Micron), in which some viruses can merge with small particulate matter. Airborne viruses can linger in the air for long periods and travel considerable distances. Viruses can also spread through droplets larger than 5 microns. However, the droplet will only last in the air for a short period and can only travel a short distance (in the range of 1 m). Actions causing droplet diffusion include sneezing, talking and coughing (World Health Organization, 2022).
In the case of a respiratory tract infection epidemic or pandemic, the Centers for Disease Control and Prevention (2022b) and the Thailand Ministry of Public Health (2020) have provided the following guidelines:
• Building management approach: this includes, a separate area for the respiratory clinic from the general clinics; an online application service for patient intake, registration, queueing system and appointments; the installation of handwashing basins and alcohol gel in every waiting area; the provision of a zero-touch medicine prescription and payment system.
• Respiratory patient screening: this includes providing a screening point for patients with respiratory symptoms; the separation of operating rooms from general operating rooms for high-risk patients, who can generate aerosols; the separation of hospital staff workspaces from patients. Moreover, open-source web-based software can also be used in the COVID-19 screening process. The studies by Parajuli et al. (2020) and Ghimire et al. (2021) provided a tool for COVID-19 risk management, where the tool (www.covira.info) is designed to collect personal risk assessment (address, age, existing health condition, any current symptoms, exposure to infected persons). The collected data is later processed to provide COVID-19 risk and mitigation measures for end-users in the form of a map and risk card.
• Infection control mandate: medical masks are mandatory for patients and medical staff. A social distance of 1 m is enforced in every area. A combination of natural and mechanical ventilation systems need to be utilised to create high-efficiency ventilation. A HEPA filter (High-Efficiency Particulate Air) is recommended as the mechanical ventilation system (Tang and Li, 2021). Clean hospital service surface areas (doorknobs, staircases and chairs) at least twice a day.
3 Methodology
The study employed a qualitative design with three steps of data collection.
Step 1. This first step was a physical setting observation (we employed walk-through observation) where data was collected through photographs and architectural building plans (Fronczek-Munter and Prugsiganont, 2018; Geng et al., 2021; Pilosof, 2021).
Step 2. In this step in-depth interviews were conducted with medical staff in the three community hospitals (Denham et al., 2018).
Step 3. In the final step a focus group was convened with the same medical staff from the in-depth interviews (Kvande et al., 2017; Telhede et al., 2022). Figure 2 illustrates the overall research design in this study.
3.1 Case descriptive
Building observation was conducted as the first step of empirical data collection through POE and walk-through observation methods. This section provides a general overview of the three community hospitals, which illustrated in Table 1 (general overview of the three case description).
3.2 Participants
The second and third steps of the study included 30 participants who worked as medical staff in the three community hospitals in Northern Thailand: 11 from Mae Wang hospital, 11 from Doi Saket hospital and 8 from Saraphi hospital. The term medical staff used in this study refers to six medical doctors, thirteen nurses and thirteen supportive medical staff.
The participant ranged in age from 22 to 60 years, and professional experience as medical staff varied between 5 months and 30 years. The participants were identified and recruited by the head nurse of each hospital. The head nurses selected the participants who worked day shifts during the outbreak of COVID-19 in 2021. A preliminary request for participation was distributed together with written information about the aim of the study including interview questions and the consequences of being included. Interested participants left their name and contact information with the head nurse, who in turn provided the information to the researcher. All participants who received information through text messages or e-mail from the researcher agreed to participate in the interview and focus group.
3.3 Data collection
The three-step procedure of data collection was conducted as follows:
3.3 1 Data collection step 1: OPD building observation
The observation of the three OPD hospital buildings was conducted between July and August 2021. Data were collected regarding the current physical setting of the OPD hospital buildings by implementing a walk-through observation as a data collection tool, focusing on building function and layout (Hansen et al., 2011; Prugsiganont and Jensen, 2019). In this step of data collection, the researcher walked around the three OPD buildings with medical staff due to hospital safety rules. Data were also collected through photographs and architectural plans.
3.3.2 Data collection step 2: Medical staff interviews
Data from semi-structured interviews were collected between September and October 2021. The term “semi-structured interview” refers to “a context in which the interviewer has a series of questions that are in the general form of an interview schedule but is able to vary the sequence of the questions” (Bryman and Bell, 2011). The researcher and the participants planned a meeting for an interview during the participants’ working hours. Before the interview, the researcher confirmed that the participant had received written information about the study and understood what it meant to participate, that the study was voluntary and that they could drop out at any time without consequences. At the physical meeting prior to the interview, a written consent form was obtained from the participant. An interview guide with semi-structured open-ended questions was used to ensure the reliability of the short interviews (Blouin et al., 2011). The interview questions were asked consecutively. The interview questions were: Can you express your opinion on the OPD building, which includes the exterior and interior physical environment? Can you also express your opinion about the protocols or guidelines on the preventive measures taken for respiratory diseases and how the protocol or guidelines affect the hospital layout or physical environment? Can you express your opinions on the relationship between OPD layout and medical services? Can you express your opinions on the current layout and design of outpatient clinics? Lastly, can you express your opinions on the current protocol for preventing the accumulation of pathogens in the OPD areas? The interviews lasted between 20 and 50 min. All interviews were conducted on premises near the workplace and were digitally recorded and then transcribed for ethical consideration. Chiang Mai University Research Ethics Committee, CMUREC 64/138, approved the study.
3.3.3 Data collection step 3: Focus group
Step 3. consisted of three focus groups. Bryman and Bell (2011) described the focus group technique as ‘a method of interviewing that involves more than one, usually at least four, interviewees’. However, there is a distinction between a focus group and group interview techniques. In other words, with a focus group, the researcher will be interested in such things as how people respond to each other’s views and build up a view outside of the interaction that takes place within the group.Participants recruited for Step 3 were the same participants from the medical staff interviews as they were expected to be especially informative to the study (Saunders et al., 2016). The focus group was conducted to further develop the design recommendation (Kevern and Webb, 2001; Rasmussen and Jensen, 2020). The preliminary design recommendation was created through the analysis of OPD buildings observation and interviews with medical staff. The focus group convened in January 2022, and the duration of the focus group meeting was between 20 and 60 min. The three focus group interviews were audio-recorded. The preliminary design recommendation was presented to the three focus groups, after which participants discussed and evaluated it, suggested changes, or pointed out the need for clarifications of the design recommendations based on their practical experiences. Based on the feedback, the preliminary design recommendation was further developed.
3.4 Data analysis
Empirical data were analysed in three steps. Data obtained through Step 1, OPD building observation, were analysed using architectural planning, where photographs taken of each area were used to emphasize the details of the plans. Data were collected regarding the current physical setting of the three OPD hospital buildings.
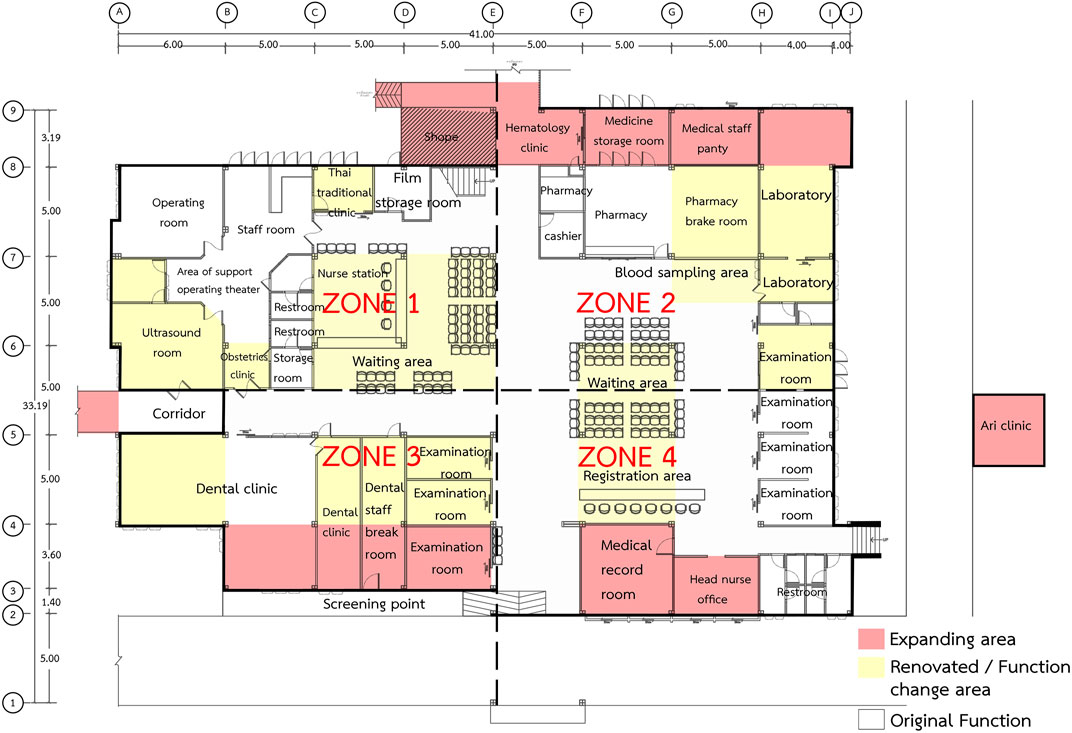
Furthermore, data obtained in Step 2, medical staff interviews, were analyzed with qualitative content analysis (Anåker et al., 2019; Corbin and Strauss, 2015). The researcher listened to the audio recording and re-read the transcript several times. Then the transcribed interviews were discussed in the research group. The text was then divided into meaning units and abbreviated into condensed meaning units. The condensed meaning units were abstracted and labelled with a code. The units of meaning were coded by searching for the important key phrases that indicated OPD building environmental problems. The codes were revised and reviewed, discussed in the research group and then condensed into categories and sub-categories. Examples of meaning units, condensed meaning units, codes, subcategories, and categories are shown in Table 2. Data obtained from the Step 3 focus group, were transcribed, and the process of analysis was similar to Step 2.
4 Findings
4.1 Building observation
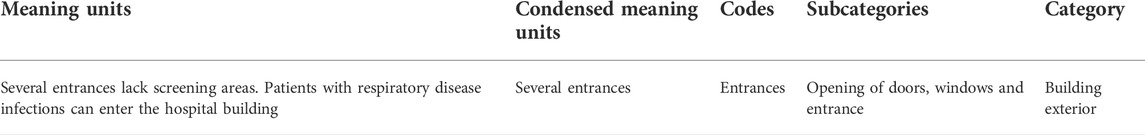
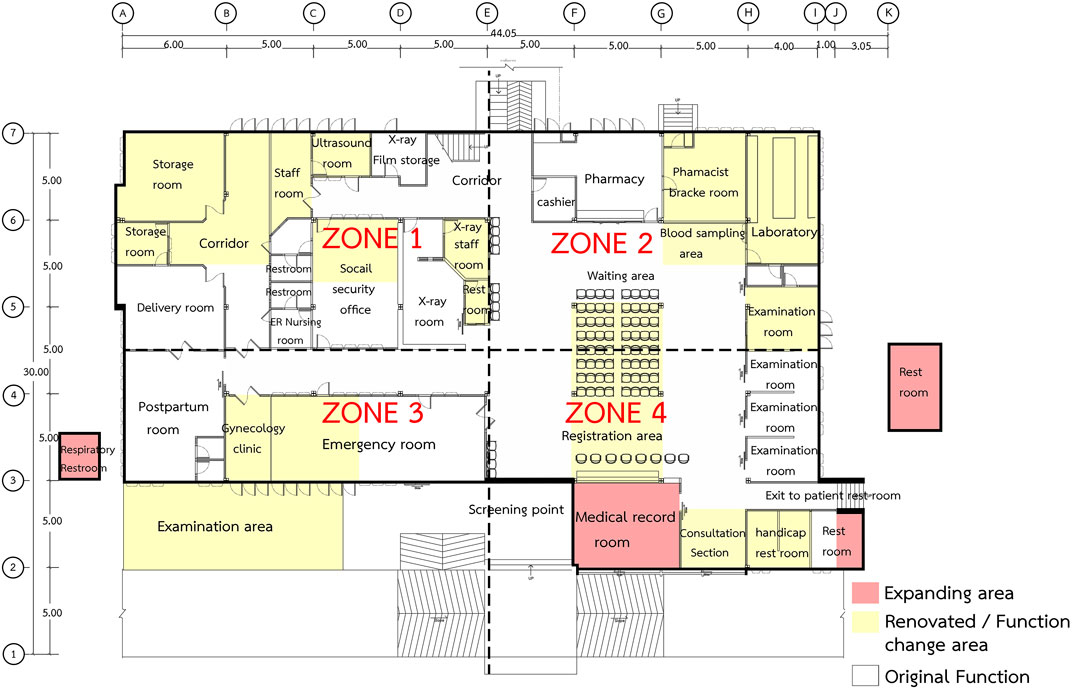
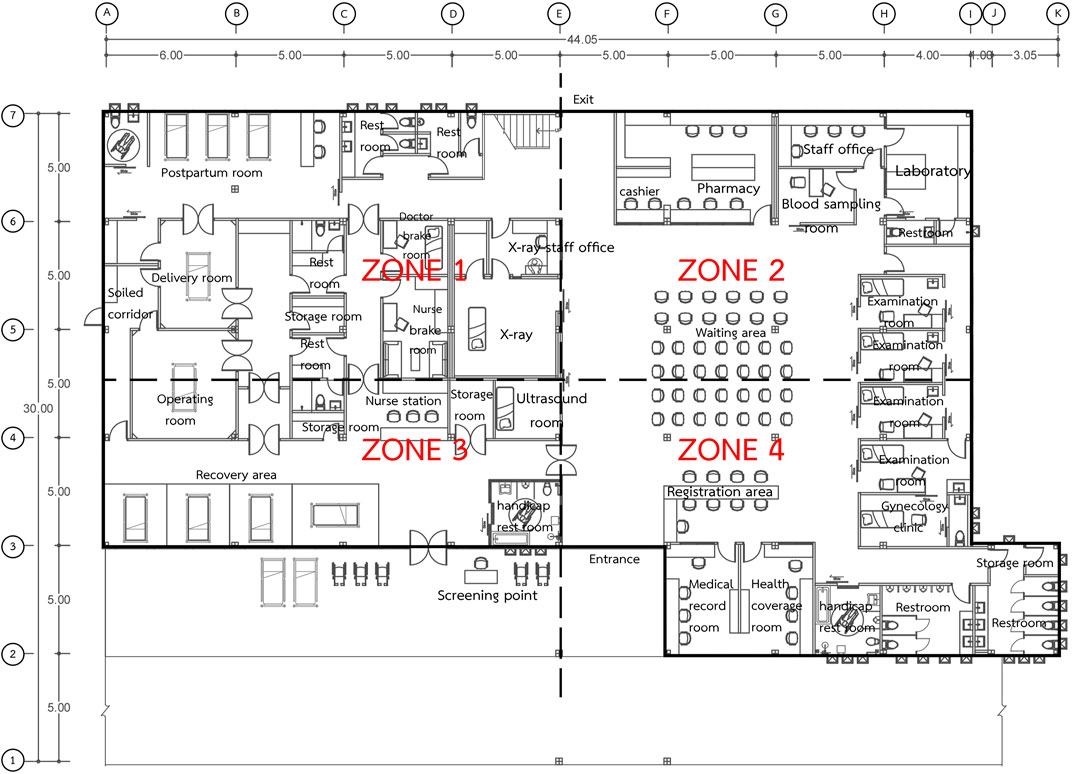
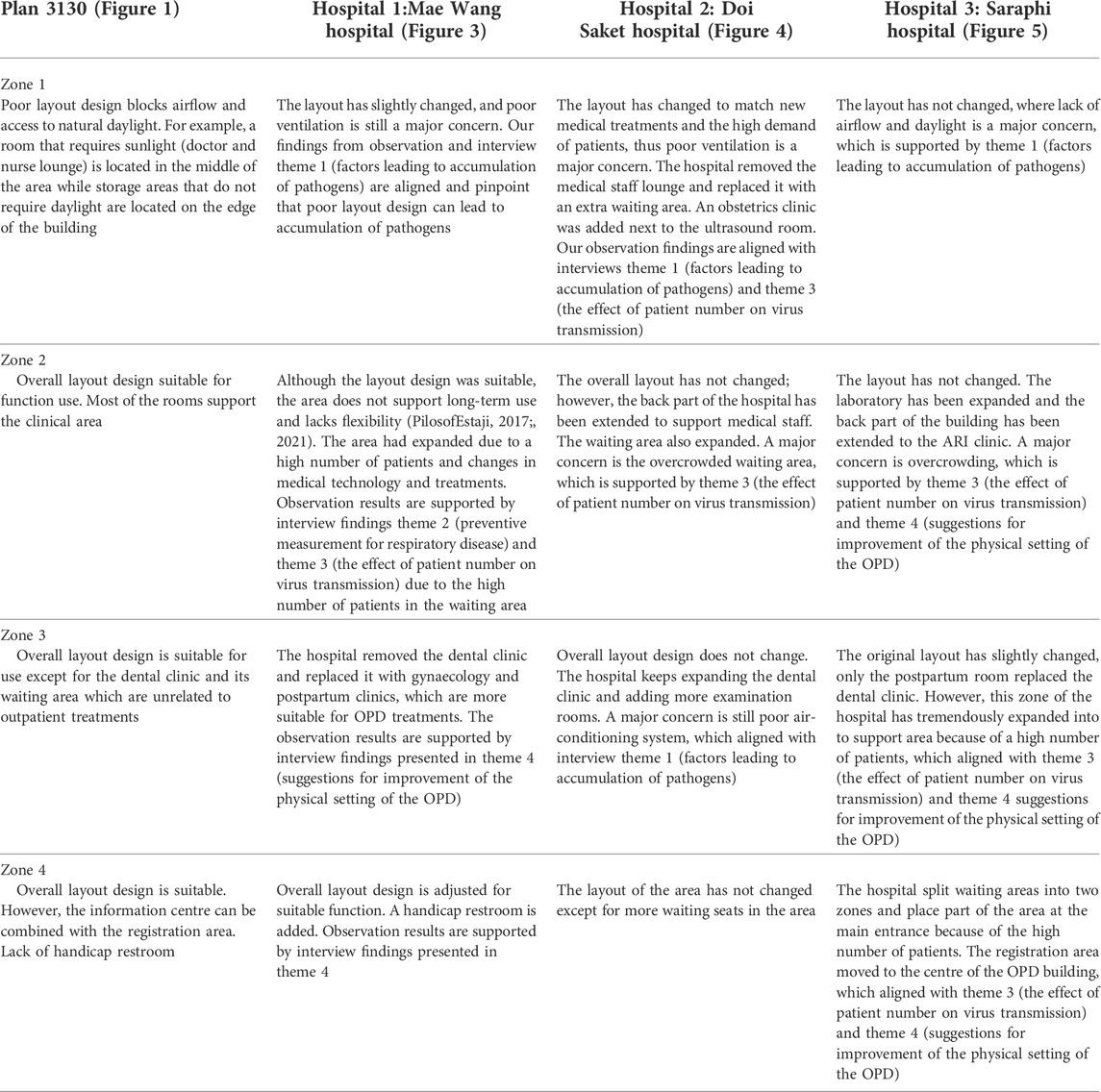
Overall planning of the three hospitals was based on the “no. 3130 planning standards” provided by the Thai Ministry of Public Health. Figures 3–5 provide details of Mae Wang hospital, Doi Saket hospital and Saraphi hospital. Yellow highlighted areas are the renovated areas where the function has been changed. White highlighted areas are the areas where the function remained the same as the original planning. Red highlighted areas are the extension areas of the hospitals.
When considering each building layout, we can see that the first hospital (Mae Wang hospital) has retained most of its original 3130 planning, whereas the third hospital (Saraphi hospital) has undergone considerable changes and expansion from its original planning. Table 3 provides an evaluation of each zone of the three hospitals:
The results of the observation indicated that the three hospital buildings lacked building flexibility. The OPD buildings were built based on the 3130 standard, which neither supports future development nor change in medical services and patient needs. The observation also showed that each hospital room does not provide building flexibility components for any expansion or reduction. The flexibility component is achieved by modifying the physical form of the building; by joining, splitting, extending, and merging spaces (Estaji, 2017). For example, the original planning does not provide a blood-sampling area, which is a requirement for primary medical processes. The hospital solved the problem by an ad-hoc use of plastic partitions in front of the laboratory due to the difficulty of building modification (traditional construction). Moreover, the laboratory does not provide a restroom with an emergency shower. These observation results aligned with the study conducted by Pilosof (2021) (provided in Section 2.2 review on OPD building physical environment design), where the study pinpointed the necessity of hospital building expansion and development due to changes in medical technology.
4.2 Interviews
Four themes were derived from the medical staff’s interviews regarding their experiences of the physical setting of the OPD buildings during the outbreak of the COVID-19 pandemic.
The themes were
• Factors leading to accumulation of pathogens, (medical staff ascertained that physical settings can lead to accumulation of pathogens, especially COVID-19),
• Measures to prevent respiratory disease (medical staff described protocol measures before and during the pandemic outbreak),
• Effects of patient number on virus transmission (medical staff believed that patient number has an impact on the transmission of COVID-19),
• Guidelines for improving the physical setting of outpatient clinics (medical staff expressed suggestions for building design to improve the physical setting of OPD building).
4.2.1 Theme 1: Factors leading to the accumulation of pathogens
The medical staff maintained that the physical setting of the OPD building can influence the transmission and accumulation of respiratory infectious diseases, with the building’s interior and exterior playing the most important roles.
For the building exterior, the medical staff added that the three hospital OPD buildings have several entrances without screening areas. The doors and windows are unsuitable (they mostly have wooden frames and louvre windows) and dust can access the building easily, with a high chance of accumulating pathogens.
For the building interior, the medical staff described the three hospitals as having poor ventilation systems, especially in restroom areas. The hospital installed fans at the main entrance, which is not suitable for hospital ventilation as germs can spread easily. Moreover, there are too many pieces of furniture close to each other, especially the waiting area seats, which makes them difficult to clean. The medical staff added that the hospitals used terrazzo-flooring material, which accumulates dust easily and is difficult to clean.
4.2.2 Theme 2: Measures to prevent respiratory disease
The medical staff said that the three hospitals had different protocols, which can be divided into pre-pandemic and during-pandemic protocols. In the pre-pandemic protocol, none of the three hospitals took any preventative measures. During the outbreak of the COVID-19 pandemic, all three hospitals issued five mandates for disease prevention.
• Daily meetings. The hospitals have to arrange daily meetings with infection control teams as a prevention protocol.
• Mouth masks. The staff at the three hospitals are required to use mouth masks in all areas.
• Social distancing. One meter of social distance is mandatory.
• Partitioning with clear plastic shields. Partitions should be installed at screening areas, nurse stations and blood sampling areas.
• Cleaning. Every area should be cleaned with disinfectant twice a day. There is an intense cleaning day once a month, provided by a cleaning company.
4.2.3 Theme 3: The effect of patient numbers on virus transmission
The medical staff explained that a high number of patients has a negative impact on respiratory infection prevention. They added that respiratory infectious diseases can transmit easily in crowded areas through the air and airborne droplets. The medical staff reported that the daily average number of patients in the three hospitals was between 150 and 300 people. The service time that each patient usually spends was around 60–90 min (from registration to leaving the hospital). However, the time would be longer if there is a complicated medical procedure (X-ray, lab test).
4.2.4 Theme 4: Suggestions for improving the physical setting of OPDs
The medical staff also made suggestions for improving the physical setting of the OPD buildings, which can be categorized into four main areas.
• Overall building. Staff strongly suggested that the hospitals should improve ventilation systems by reducing the use of fans and installing negative pressure, high-efficiency particulate filter systems (HEPA). The medical staff also added that the hospitals should increase incoming natural light and provide screening areas at every entrance and exit.
• Support area. The medical staff expressed that the hospital should remove the restroom from the examination area. Moreover, the hospital should add a medical staff corridor at the back of the examination rooms. Changing rooms should be located in every OR, delivery room, and X-ray area with a negative pressure system.
• Clinical area. The medical staff suggested that the hospitals should build a permanent acute respiratory infection clinic (ARI clinic) outside. They added that the hospitals should install sliding doors and windows. The medical staff in Doi Saket hospital added that the hospital should remove the dental clinic from the OPD building. The staff also suggested that the hospitals should install negative pressure and an emergency shower in the laboratory. The hospitals should also create privacy by providing separate rooms in the blood sampling area.
• Staff area. The medical staff also suggested that the hospitals should provide a washbasin in every staff room and provide a separate staff restroom.
The interviews with the medical staff indicated that there was a lack of user involvement during the expansion and renovation of the three hospitals. Analysis of the medical staff interviews especially in theme 1 (factors leading to accumulation of pathogens) and theme 4 (suggestions for improvement of the physical setting of the OPDs) signified that there are many physical setting problems. Furthermore, details in theme 1 and theme 4 are also aligned with the OPD buildings observation. Based on the interview analysis, the participants pinpointed many physical problems (in almost every area). These problems resulted from a lack of implementation of the users’ opinions during the design process, including the renovation and expansion process.
4.3 Focus group
The third part of data collection, the focus group, evaluated the preliminary design recommendations created through building observation and the medical staff interviews. Three focus groups, formed from the same interview participants, evaluated the design recommendations. They also shared their opinions to further develop the design. Analysis data obtained from the focus group were briefly described in the “13 areas”, where Figure 6 provides a new layout of no. 3130 standard. The design recommendations consist of three aspects which are management, building design and space management. Management referes to hospital management concerning patients safety in relation to respiratory infection control. Building design represents indoor and outdoor environment includes air ventilation, lighting and building material. Space management refers to functional flexibility that can improve clinical efficacy. Details of the new layout plan and each area are described as follows:
Area 1 is the overall building interior and air conditioning systems.
Furniture and covering material should not contain narrow openings and sharp corners, a warm tone colour is recommended. Sliding doors and windows should be installed for better maintenance and ventilation. Variable Refrigerant Flow (VRF) or central air system is mandatory for the OPD building. Positive pressure with an air purifier is also recommended.
4.3.1 Support area
Area 2 is the entrance and exit. Separate entrance and exit areas are needed, the entrance should be located at the front of the building while the exit should be located at the back - barriers should be installed at the exit with specific opening hours. Screening areas should be located at every entrance, and an entrance air curtain is advised.
Area 3 is the registration area. The social security office and registration area should be located close to each other. The area should be open and easy to clean, and online registration is suggested.
Area 4 is the patient restroom. The side exit to the outside patient restrooms should be closed. The restroom needs improvement with ventilation and the provision of a handicap restroom.
Area 5 is the waiting area and nurse station. A single seat is recommended to be placed in the waiting area in place of row seats, providing distance between patients. Wheelchair and stretcher access needs to increase. Air extraction should be installed in the ceiling windows together with insect screens. The nurse station should also install plastic screens.
4.3.2 Clinical area
Area 6 is the examination room. All three hospitals should provide 4 examination rooms, where one room provides equipment for the gynaecology clinic. Restrooms should be removed from the examination rooms, except for the gynaecology clinic. A corridor should be provided at the back of examination rooms.
Area 7 is the laboratory and blood sampling area. Separate areas for the laboratory and office zone are needed and the laboratory should provide a small pass box. The laboratory zone should have two exits in case of emergency with UV lights also restrooms should be provided with an emergency shower and ventilation system. A separate room needs to be provided at the blood sampling area for privacy, with space for wheelchair and stretcher access.
Area 8 is the pharmacy and cashier. To provide more working space for staff the pharmacy needs to reduce the amount of medicine and merge the area with the cashier section.
Area 9 is X-ray and ultrasound. More space should be created in the X-ray area by removing the developing room and restroom and replacing them with a changing room. In Doi Saket hospital, dental radiographs should be installed in the x-ray area and the ultrasound should be located next to the ER to increase medical flow efficiency.
Area 10 is the OR, delivery room, antenatal and postpartum room, these three areas should be connected due to function and air conditioning system. Clean and dirty zones need to be created, where the clean zone is semi-sterile. The OR needs to be moved closer to the ER. The size of the delivery room, antenatal and postpartum rooms need to be decreased, due to low case numbers. Also, the antenatal and postpartum rooms need to be relocated to the back of the building.
Area 11 is the emergency room. This room needs to increase in size due to the high number of cases. Also, a separate entrance to the ER from the OPD building needs to be installed. Specific access for respiratory infected patients needs to be created at the ER entrance. Patient beds should be moved closer to the nurse station, so nurses have a clear vision of patients. Provide a clear zone of observation and cardiopulmonary resuscitation (CPR) area. Increase storage area and clean zone and provide handicap restroom.
4.3.3 Staff area
Area 12 is the medical staff break room. Break rooms should be provided for all medical staff including medical doctors, nurses, pharmacists and supporting staff. Rooms should connect to the clinical area.
Area 13 is the staff restroom. X-ray film and document storage rooms need replacing with a staff restroom.
The focus group provided useful information and insights that supported the design recommendations. Data obtained from the focus group was aligned with the preliminary design guideline; no significant changes nor suggestions were added during the focus group discussion. Opinions exchanged among the medical staff provided insight and useful recommendations for the overall planning of the three hospitals as well as for each hospital. For example, the medical staff from Doi Saket hospital recommended moving the dental clinic closer to the ER.
The results from the interview and focus group aligned with the user-focused, design approach literature (presented in Section 2.1 Evidenced-based design for hospital facilities). For instance, Bate and Robert (2006) and Fronczek-Munter (2016), stated in their studies that a user-focused design approach can help to optimize the design outcome and improve building quality.
5 Discussion
The analysis of the building’s observation and the interviews aided in creating preliminary design guidelines, which were evaluated by the three focus groups. The discussion section provided answers to the research questions as well as reflections on the OPD no. 3130 building standard.
(1) What are the physical problems of community OPD buildings?
Findings analysis pinpointed the underlying problems in the community hospital OPD buildings. The major problem is a lack of management and space management leading to physical problems. Moreover, findings were compared with layout no. 3130 standard, which highlighted specific problems presented in Table 4. The analysis of both the observations and interviews indicated a lack of efficient management, which can lead to a high number of patients, as presented in “Theme 2” (preventive measurement for respiratory disease) and theme 3 (the effect of patient number on virus transmission). The observation and the interview analysis of “themes 2 and 3” are supported by the literature in Section 2.4 (hospital design preventing respiratory infection), which states that the implementation of an IT service can help improve hospital space as well as reduce the number of patients (the Thai Ministry of Public Health, 2017). The IT service includes a risk management tool. This means the hospital can use web-based or mobile phone applications to manage a large number of patients and thus decrease the chance of COVID-19 infection (Chatterjee et al., 2020; Parajuli et al., 2020; Ghimire et al., 2021). Moreover, implementing an IT service can help manage the space of particular areas (e.g., patient record room) and help distribute the number of patients in the waiting areas. The analysis of the interviews also revealed poor hospital space management, where certain areas are no longer in use (e.g., X-ray film storage room, delivery room) while several areas are needed (e.g., handicap restroom, blood sampling area). However, interviews concerning “theme 4” (suggestions for improving the physical setting of OPDs) provided useful information for rearranging hospital space based on medical staff opinions.
From the information provided in “Table 4”, specific building problems can be identified. In zone 1, the main concern is poor layout design, where small rooms located at the edge of the building block air ventilation and daylight. In zones 2 and 3, the major concern is a lack of area flexibility and the spacial arrangement of the clinic making it unsuitable for OPD treatments. In zone 4, the problem is the lack of implementation of user needs in the building layout. Overall, specific problems might occur due to the lack of user involvement during the no. 3130 design process. When considering interview findings, ‘theme 3’ (effect of patient number on virus transmission) has the most decisive effect on the physical problem of the buildings.
(2) How can a user-focused design approach improve the OPD building with the aim of preventing the spread of COVID-19?
The user-focused design approach is an effective and successful technique, but needs to be used with a critical mindset - the literature in Section 2.1 (Evidence-based design for hospital facilities) and 2.3 (Hospital evaluation approach) covered the topic of user-focused design. The approach is used as a tool to collect data from users to improve building design. The user-focused approach in the design process provides the designers with an opportunity to create a design based on user needs (Alexander, 2008; Fronczek-munter, 2016). However, the approach should be used with consideration, which means the approach should not be used with inflated expectations. Furthermore, all involved parties (medical staff and hospital designers) should share the same understanding and expectations (Prugsiganont and Waroonkun, 2021). This “discussion” began by referencing the lack of user involvement in the three community hospitals, which resulted in several physical environment problems. However, after data collection analysis the study demonstrated the importance of user involvement in design implementation, an approach which needs careful deliberation. Based on the study’s findings, positive design recommendations have been formulated. From the medical staff interviews and focus group analysis, it was found that the result align with the literature that emphasises user-focused design (Prugsiganont and Waroonkun, 2021; Fronczek-Munter, 2016). Positive design can be delivered successfully when the involvement of designers and users is managed effectively (Fronczek-Munter, 2016). The study showed that the collaboration of the medical staff contributes to the hospital design process by providing insights that lead to positive design outcomes. User involvement is important and it is a core principle for a user-focused design approach but different users need to be involved in the various stages (Fogarty and Cronin, 2008). Findings from this study yield that the medical staff can pinpoint specific OPD building problems (Fogarty and Cronin, 2008), which are mentioned in Section 4.2 (interviews) and 4.3 (focus group), providing safety and comfort for the patient and COVID-19 prevention.
Preventing the spread of COVID-19 through the experience of medical staff. The interview data showed that before the pandemic outbreak none of the hospitals applied respiratory virus prevention protocol, which is presented in theme 2 (measures to prevent respiratory disease). Even though during the outbreak the hospitals had implemented the Thai Public Health protocol, the protocol was not effective due to the poor physical condition of the buildings. A major concern is poor ventilation and lack of natural daylight, presented in the no. 3130 standard layout. Observation and interview findings showed that currently the hospitals use fans to ventilate the rooms. The study by Huang et al. (2021) revealed that fan-assisted natural ventilation may increase respiratory infection risks because a viral plume can spread upward and downward, driven by buoyancy forces and natural wind. Moreover, too many room panels lead to poor airflow. When comparing the hospitals’ current ventilation to CDC quality standards (Centers for Disease Control and Prevention, 2022b; Tang and Li, 2021) it was found that the hospital should increase its natural airflow and install a mechanical ventilation (HEPA filter) system. The findings were supported by the literature in Section 2.4 (hospital design preventing respiratory infection).
Design suggestions from the observation and interview analysis were evaluated through the focus group. The recommendations from the focus group were subsequently incorporated into the 13 areas for development (presented in Section 4.3 focus group). It was found that recommendations from the medical staff were not only aimed at preventing the spread of COVID-19 but also focused on holistically improving the whole OPD building physical environment. The suggestions can be categorized into management, space management and design recommendations. The obtained information can be used to optimize hospital design, especially for community hospitals. The findings are aligned with the literature on EBD (Section 2.1) and hospital evaluation (Section 2.3).
The findings of this study shared similarities with previous studies that focused on infection prevention of COVID-19 in healthcare facilities. The studies conducted by Emmanuel et al. (2020) and Shepley et al. (2021) recommended several significant factors that can help prevent the spread of viruses. These recommendations include: 1) social distancing, 2) enhancing natural ventilation, 3) improving airflow and use of HEPA filters, 4) enhancing sunlight, 5) minimising multiple entrances into public areas, 6) implementing flexible areas such as additional infrastructure or garages for emergency use, 7) implementing a thorough cleaning protocol, 8) implementing online patient registration and 9) implementing the use of sensors to reduce contact of frequently touched surfaces, such as a door handle.
Although there are similarities in findings between this study and previous studies, the researchers believe that this study provided more insightful design recommendations that can be specifically used in Thai community hospitals. The designs can be adopted or modified for more specific healthcare facilities including centres of excellence, oncology centres etc.
6 Conclusion
The conclusions are discussed related to the two main study objectives. The first objective of this study was to identify the difficulties faced by the community hospitals during the Thailand COVID-19 outbreak between 2020 and 2021 by focusing on the physical settings of outpatient departments (OPD). It was found that the major cause of the difficulties was the lack of management and space management.
The lack of management created a high number of patients. This issue can be improved by implementing an IT service, which can help reduce the number of patients. Moreover, using a web-based or mobile phone application risk management tool can help manage patient numbers. The problem of inadequate space management stemmed from the lack of building flexibility and poor layout. The hospitals had expanded without considering the users’ needs. A combination of these factors led to building inefficiency; therefore, the hospital could not properly prevent the spread of COVID-19. To solve the building problem and prevent the spread of COVID-19 the hospital can implement a user involvement approach during the design process.
The second objective was to provide design suggestions for preventing the spread of respiratory infectious diseases. The suggestions for design improvements are split in recommendations for each area in the no. 3130 layout (13 areas). This study showed that medical staff are greatly concerned about the physical environment of hospital buildings. Suggestions to improve the physical environment of the 13 areas came through user involvement and evidence-based design that is covered by literature. The recommendations were categorized into three aspects, which are equally important and intertwined. The first category is management. This includes social distancing, implementing thorough cleaning protocols, implementing IT service and implementing sensors on frequently touched surfaces. The second category, building design, includes enhancing natural ventilation and daylight, especially in waiting areas and restrooms, minimizing entrances into public areas, improving airflow and using HEPA filters. Finally providing area flexibility would facilitate space management.
However, the study also yielded recommendations that are specific to Thai community hospitals. Such recommendations include the installation of gynaecology and obstetric clinics, a large laboratory, a large ER, a blood-sampling area and a handicap restroom. Moreover, the ARI clinic should be located outside the OPD building. Lastly, a dental clinic is not suitable for an OPD building.
Hospital policymakers should ensure the ambition to integrate building flexibility, user involvement, management and space management during the design process. At present, most Thai community hospitals go through a renovation process without any specific research. This study indicated there is a need to pay more attention to user involvement rather than individual bureaucratic decisions.
7 Limitations and implications
The study provides insights for design recommendations for Thai community hospitals. However, it also demonstrates the limitations. First, the study was qualitative, whereas a quantitative approach should be integrated to increase the study’s validity. The study was conducted only in the Northern part of Thailand; other developing countries from South East Asia should be considered for further study. Second, the number of medical staff recruited for this study was limited to only 30 participants. Although there were three building observations and three focus groups (providing opportunities for triangulation), it is difficult to generalize the findings as this is the nature of a qualitative study (Creswell and Poth, 2015). It is advised to recruit a higher number of participants, including operational staff or facility managers, for more insightful recommendations.
The study contributes to five literature topics, including hospital facilities design, evidence-based design for hospital facilities, OPD building physical environments, hospital design evaluation approach and hospital design preventing respiratory infection. Furthermore, this study provides additional practical tools and propositions. First, user involvement for improving the hospital’s physical environment. Second, the future development of hospital physical environmental design that can prevent the spread of COVID-19 in Thai community hospitals. The study also contributes to the future development of community hospital design where the renovation can be adjusted based on the allocated budget and the context of the specific hospital.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributions
SP contributed to conception and design of the study. TW collected the data and organized the database. SP and TW performed the qualitative content analysis. SP wrote the first draft of the manuscript, SP and TW wrote sections of the manuscript, but discussion part were written by SP and TW. Both authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was funded by the National Research Council of Thailand (NRCT) of 2021.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alexander, K. (2008). Usability of workplace - phase 2. Report in CIB conference. Available at: https://www.researchgate.net/publication/264628568_Usability_of_workplaces_-_Phase_2 (Accessed June 10, 2022).
Anåker, A., von Koch, L., Heylighen, A., and Elf, M. (2019). “It’s lonely”: Patients’ experiences of the physical environment at a newly built stroke unit. Health Environ. Res. Des. J. 12, 141–152. doi:10.1177/1937586718806696
Bate, P., and Robert, G. (2006). Experience-Based design from redesigning the system around the patient to co-designing services with the patient. Qual. Saf. Health Care 15 (5), 307–310. doi:10.1136/qshc.2005.016527
Blouin, D., Day, A. G., and Pavlov, A. (2011). Comparative reliability of structured versus unstructured interviews in the admission process of a residency program. J. graduate Med. Educ. 3 (4), 517–523. doi:10.4300/jgme-d-10-00248.1
Bryman, A., and Bell, E. (2011). Business research methods. Oxford, United Kingdom: Oxford University Press. c2011. Available at: https://library.lincoln.ac.uk/items/122618 (Accessed June 5, 2022).
Center of Health Design (2015). Clinic design post-occupancy evaluation toolkit. Available at: https://www.healthdesign.org/insights-solutions/clinic-design-post-occupancy-evaluation-toolkit-pdf-version (Accessed June 5, 2022).
Centers for Disease Control and Prevention (2022b). Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (Accessed June 17, 2022).
Centers for Disease Control and Prevention (2022a). COVID data tracker. Available at: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (Accessed June 2, 2022).
Chatterjee, R., Bajwa, S., Dwivedi, D., Kanji, R., Ahammed, M., and Shaw, R. (2020). COVID-19 risk assessment tool: Dual application of risk communication and risk governance. Prog. Disaster Sci. 7, 100109. doi:10.1016/j.pdisas.2020.100109
Corbin, A., and Strauss, J. (2015). Basics of qualitative research. San California, USA: SAGE Publishing.
Creswell, J. W., and Poth, C. N. (2015). Qualitative inquiry and research design: Choosing among five approaches. Fourth edition. California: SAGE Publishing.
Denham, M. E., Bushehri, Y., and Lim, L. (2018). Through the eyes of the user: Evaluating neonatal intensive care unit design. Health Environ. Res. Des. J. 11 (3), 49–65. doi:10.1177/1937586718761017
Edmunds, H. (1999). The focus group research handbook. Bottom Line 12, 3–46. doi:10.1108/bl.1999.12.3.46.1
Emmanuel, U., Osondu, E. D., and Kalu, K. C. (2020). Architectural design strategies for infection prevention and control (IPC) in health-care facilities: Towards curbing the spread of covid-19. J. Environ. Health Sci. Eng. 18, 1699–1707. doi:10.1007/s40201-020-00580-y
Estaji, H. (2017). A review of flexibility and adaptability in housing design. Int. J. Contemp. Archit. “The New ARCH” 4 (2), 37–49. doi:10.14621/tna.20170204
Fay, L., Carll-White, A., and Harrell, J. (2016). Coming full cycle: Linking POE findings to design application. Health Environ. Res. Des. J. 10 (3), 83–98. doi:10.1177/1937586716672856
Fogarty, C., and Cronin, P. (2008). Waiting for healthcare: A concept analysis. J. Adv. Nurs. 61 (4), 463–471. doi:10.1111/j.1365-2648.2007.04507.x
Fronczek-Munter, A., and Prugsiganont, S. (2018). “Hospital architecture quality- exploratory observation on three continents,” in The 5th international conference on architecture and built environment proceeding. Oslo, Norway: INTEF Academic Press, 156–165.
Fronczek-Munter, A. (2016). Usability briefing for hospital design: Exploring user needs and experiences to improve complex buildings (Lyngby, Denmark: Technical University of Denmark). [PhD thesis]. [Copenhagen].
Geng, S., Chau, H.-W., Yan, S., Zhang, W., and Zhang, C. (2021). Comparative analysis of hospital environments in Australia and China using the space syntax approach. Int. J. Build. Pathology Adapt. 39 (3), 525–546. doi:10.1108/ijbpa-04-2020-0031
Ghimire, B. R., Parajuli, R. R., Khatiwada, B., Poudel, S., Sharma, K., and Mishra, B. (2021). Covira: A COVID-19 risk assessment, visualization and communication tool. SoftwareX 16, 100873. doi:10.1016/j.softx.2021.100873
Gulwadi, G. B., Joseph, A., and Keller, A. B. (2009). Exploring the impact of the physical environment on patient outcomes in ambulatory care settings. Health Environ. Res. Des. J. 2, 21–41. doi:10.1177/193758670900200203
Hamilton, D. K. (2003). The four levels of evidence based practice. Available at: https://sereneview.com/wp-content/uploads/2019/03/4levels_ebd.pdf (Accessed June 17, 2022).
Hamilton, D. K., and Watkin, D. H. (2009). Evidence-based design for multiple building types. Hoboken, NJ: John Wiley & Sons, Inc.
Hansen, G. K., Blakstad, S. H., and Knudsen, W. (2011). USEtool - evaluating usability. Available at: https://www.ntnu.no/documents/20658136/21235909/USEtool_english.pdf/e891d71b-00ad-4dc0-a985-1766696b17b1 (Accessed May 27, 2022).
Huang, J., Jones, P., Zhang, A., Hou, S. S., Hang, J., and Spengler, J. D. (2021). Outdoor airborne transmission of coronavirus among apartments in high-density cities. Front. Built Environ 7, 2021. doi:10.3389/fbuil.2021.666923
Huisman, E. R. C. M., Morales, E., van Hoof, J., and Kort, H. S. M. (2012). Healing environment: A review of the impact of physical environmental factors on users. Build. Environ. 58, 70–80. doi:10.1016/j.buildenv.2012.06.016
Kevern, J., and Webb, C. (2001). Focus groups as a tool for critical social research in nurse education. Nurse Educ. Today 21 (4), 323–333. doi:10.1054/nedt.2001.0563
Kvande, M., Lykkeslet, E., and Storli, S. L. (2017). ICU nurses and physicians dialogue regarding patients' clinical status and care options-a focus group study. Int. J. Qual. Stud. health well-being 12 (1), 1267346. doi:10.1080/17482631.2016.1267346
Malkin, J. (2008). “Evidence-based design”, in A visual reference to evidence-based design (California, USA: The Center for Health Design), 1, 2–18.
Miedema, E., Lindahl, G., and Elf, M. (2019). Conceptualizing health promotion in relation to outpatient healthcare building design: A scoping review. Health Environ. Res. Des. J. 12, 69–86. doi:10.1177/1937586718796651
Page, R. (2020). “Use beyond usability: Integrating user experience design and human factors to improve the usability of a cochlear implant charging system,” in Design for the health. Available at: https://www.tandfonline.com/doi/full/10.1080/24735132.2020.1727693 (Accessed May 18, 2022).
Parajuli, R. R., Mishra, B., Banstola, A., Ghimire, B. R., Poudel, S., Sharma, K., et al. (2020). Multidisciplinary approach to COVID-19 risk communication: A framework and tool for individual and regional risk assessment. Sci. Rep. 10, 21650. doi:10.1038/s41598-020-78779-0
Pilosof, N. P. (2021). Building for Change: Comparative case study of hospital architecture. Health Environ. Res. Des. J. 14, 47–60. doi:10.1177/1937586720927026
Preiser, W. F. E., White, E., and Rabinowitz, H. (2015). Post-occupancy evaluation. London: Routledge.
Prugsiganont, S., and Jensen, P. A. (2019). Identification of space management problems in public hospitals: The case of maharaj chiang mai hospital. F. 37 (7/8), 435–454. doi:10.1108/f-01-2018-0001
Prugsiganont, S., and Waroonkun, T. (2021). Factors influencing optimal hospital design: A comparative study between Thai and Norwegian public hospitals. Civ. Eng. Archit. 9 (4), 976–991. doi:10.13189/cea.2021.090402
Rasmussen, H. L., and Jensen, P. A. (2020). A facilities manager’s typology of performance gaps in new buildings. J. Facil. Manag. 18 (1), 71–87. doi:10.1108/JFM-06-2019-0024
Saunders, M., Lewis, P., and Thornhill, A. (2016). Research methods for business students. 7th ed. London, United Kingdom: Pearson
Shepley, M. M., Kolakowski, H., Ziebarth, N., and Valenzuela-Mendoza, E. (2021). How COVID-19 will change health, hospitality and senior facility design. Front. Built Environ. 7, 2021. doi:10.3389/fbuil.2021.740903
Singh, V. K., and Lillrank, P. (2022). Planning and designing healthcare facilities. Available at: https://www.routledge.com/Planning-and-Designing-Healthcare-Facilities-A-Lean-Innovative-and-Evidence-Based/Singh-Lillrank/p/book/9781138032262# (Accessed April 17, 2022).
Soria, A., Galimberti, S., Lapadula, G., Visco, F., Ardini, A., Valsecchi, M. G., et al. (2021). The high volume of patients admitted during the SARS-CoV-2 pandemic has an independent harmful impact on in-hospital mortality from COVID-19. PloS one 16 (1), e0246170. doi:10.1371/journal.pone.024617
Tang, H., and Li, C. (2021). Study on ventilation rates and assessment of infection risks of COVID-19 in an outpatient building. J. Build. Eng. 42, 103090. doi:10.1016/j.jobe.2021.103090
Telhede, H. E., Arvidsson, S., and Karlsson, S. (2022). Nursing staff's experiences of how weighted blankets influence resident's in nursing homes expressions of health. Int. J. Qual. Stud. Health Well-being 17 (1), 2009203. doi:10.1080/17482631.2021.2009203
Thailand Ministry of Public Health (2020). Sentinel surveillance of COVID-19 in ARI & CAP patients. Available at: https://ddc.moph.go.th/viralpneumonia/file/g_ari_pneumonia/g_ari_pneumonia_moph.pdf (Accessed June 17, 2022).
Thailand Ministry of Public Health (2022). COVID-19 case statistic Thailand. Available at: https://ddc.moph.go.th/covid19-dashboard/(Accessed June 17, 2022).
Thailand Ministry of Public Health (2017). eHealth strategy, Ministry of public health. Available at: https://ict.moph.go.th/upload_file/files/eHealth_Strategy_ENG_141117.pdf (Accessed May 15, 2022).
Ulrich, R., Quan, X., Zimring, C., Joseph, A., and Choudhary, R. (2004). The role of the physical environment in the hospital of the 21st century: A once-in-a-lifetime opportunity. Available at: https://www.healthdesign.org/system/files/Ulrich_Role%20 of%20Physical_2004.pdf (Accessed June 17, 2022).
Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H. B., Choi, Y. S., et al. (2008). A review of the research literature on evidence-based healthcare design. Health Environ. Res. Des. J. 1 (3), 61–125. doi:10.1177/193758670800100306
Van der Voordt, T. J. M., and Van Wegen, H. B. R. (2005). Architecture in use: An introduction to the programming design and evaluation of buildings. United Kingdom: Routledge.
Waroonkun, T. (2020). Patient attitudes to features of a medical examination room in a Thai hospital. Int. J. Des. Manag. Prof. Pract. 14 (3), 29–45. doi:10.18848/2325-162X/CGP/v14i03/29-45
Waroonkun, T. (2018). The environmental factors affecting service satisfaction of community hospital. J. Des. Built Environ. 1, 19–28. doi:10.22452/jdbe.vol18no1.3
World Health Organization (2022a). COVID-19 weekly epidemiological update, edition 95. Available at: https://apps.who.int/iris/handle/10665/355779 (Accessed June 17, 2022)
World Health Organization (2022b). Infection prevention and control. Available at: https://www.who.int/teams/integrated-health-services/infection-prevention-control (Accessed March 25, 2022).
Keywords: COVID-19, post-occupancy evaluation, evidence-based design, community hospital, hospital design, Thailand, medical staff opinions
Citation: Waroonkun T and Prugsiganont S (2022) Preventing the spread of COVID-19 through environmental design in Thai community hospitals. Front. Built Environ. 8:947211. doi: 10.3389/fbuil.2022.947211
Received: 18 May 2022; Accepted: 25 July 2022;
Published: 07 September 2022.
Edited by:
Theo Van Der Voordt, Delft University of Technology, NetherlandsReviewed by:
Grit Ngowtanasuwan, Mahasarakham University, ThailandRishi Ram Parajuli, University of Bristol, United Kingdom
Copyright © 2022 Waroonkun and Prugsiganont. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Supuck Prugsiganont, c3VwdWNrLnBAY211LmFjLnRo
 Tanut Waroonkun
Tanut Waroonkun Supuck Prugsiganont
Supuck Prugsiganont