
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Bioeng. Biotechnol., 08 April 2025
Sec. Biomechanics
Volume 13 - 2025 | https://doi.org/10.3389/fbioe.2025.1560597
This article is part of the Research TopicEnhancing Sports Injury Management through Medical-Engineering InnovationsView all 5 articles
 Dianxuan Wu1,2,3†
Dianxuan Wu1,2,3† Zhicheng Wen1,2,3†
Zhicheng Wen1,2,3† Haolin Ke2,3,4†
Haolin Ke2,3,4† Jiexin Zhang1,2,3
Jiexin Zhang1,2,3 Shaozi Zhong1,2,3
Shaozi Zhong1,2,3 Jiachen Teng1,2,3
Jiachen Teng1,2,3 Lan Xu2,5
Lan Xu2,5 Jintao Li1,2,3*‡
Jintao Li1,2,3*‡ Yan Shao1,2,3,4*‡
Yan Shao1,2,3,4*‡ Chun Zeng1,2,3,4*‡
Chun Zeng1,2,3,4*‡Objective: To investigate the effect of specific modes of exercise on rotator cuff-related shoulder pain (RCRSP) patients, aiming to provide a theoretical reference for conservative treatment and exercise prescription.
Methods: Data sources included PubMed/MEDLINE, Web of Science, ScienceDirect, and CNKI, covering studies from database inception to June 2024. Study selection followed pre-set inclusion/exclusion criteria. Cochrane methods guided quality assessment and data extraction. Outcome measures included VAS, CMS, and DASH scores. Publication bias assessed via funnel plots; forest plots created using RevMan 5.4.
Results: 13 studies (n = 690) met inclusion criteria for RCRSP exercise interventions. It is indicated that: (1) specific exercises led to modest improvements in performance of pain (SMD = −0.31, 95% CI: 0.46 to −0.16, P < 0.0001) and function, with enhancements in CMS (SMD = 0.59, 95% CI: 0.44 to 0.74, P < 0.00001) and DASH (SMD = −0.60, 95% CI: 0.80 to −0.39, P < 0.00001). (2) Interventions lasting less than 2 months were slightly more effective than those lasting 2 months or longer, observed in VAS (SMD = −0.35, 95% CI: 0.56 to −0.15, P = 0.0007), CMS (SMD = 0.71, 95% CI: 0.47 to 0.96, P < 0.00001), and DASH (SMD = −0.71, 95% CI: 0.99 to −0.43, P < 0.00001). (3) Subgroup analyses revealed that handgrip strength exercises enhanced shoulder pain relief, shoulder mobilization/stretching improved both function and pain levels over 2 months, scapular stabilization exercise improved pain and DASH performance over 2 months, eccentric exercises boosted CMS and DASH performance over 2 months, while proprioceptive exercises showed no significant improvement in pain or CMS performance.
Conclusion: Compared to non-specific exercises, specific exercise programs moderately alleviate RCRSP symptoms, with shorter interventions (<2 months) demonstrating marginally superior outcomes. Efficacy varies by exercise type, emphasizing the need for individualized prescriptions.
Systematic Review Registration: PROSPERO (CRD42024550602).
The shoulder joint, characterized by its complex interplay of bones, muscles, ligaments, and nerves, is highly mobile. Pain in this area is a prevalent musculoskeletal disorder, affecting up to 70% of individuals over their lifetime (Requejo-Salinas et al., 2022). Prognosis varies widely, with up to 50% of patients experiencing persistent pain 6–12 months after seeking clinical treatment, significantly impacting their work and daily life (Pope et al., 1997; Picavet and Schouten, 2003; Greving et al., 2012; Doiron-Cadrin et al., 2020). The complex patho-anatomy of the area complicates traditional diagnosis and pinpointing a specific pain source (Greenberg, 2014; Gismervik et al., 2017). Rotator cuff-related shoulder pain (RCRSP) is an umbrella term that encompasses a range of shoulder conditions including subacromial pain (impingement) syndrome, rotator cuff tendinopathy, symptomatic partial and full thickness rotator cuff tears, and is the most common cause of shoulder pain (Lewis, 2016; Requejo-Salinas et al., 2022). Characteristic clinical manifestations include painful shoulder elevation/external rotation with concomitant motion restriction and functional impairment. Therapeutic objectives prioritize restoration of pain-free range of motion and optimal shoulder function (Ottenheijm et al., 2011).
The sources of pain in RCRSP are primarily related to decreased joint function, decreased muscle performance, altered shoulder kinematics, and maladaptive pain behaviors such as agoraphobia and exaggeration, and treatment consists of: patient education, exercise therapy, medications, joint cavity injections, and surgical interventions (Dubé et al., 2023). Exercise therapy is a cornerstone in treating shoulder pathology, with numerous reviews highlighting its effectiveness in improving pain and function (Kromer et al., 2009; Abdulla et al., 2015; Steuri et al., 2017; Powell et al., 2024), which takes the form of a physical therapist-initiated, patient-guided strengthening exercise through antigravity exercise followed by progressive resistance exercise, with the patient following a self-management program at home (Greenberg, 2014; McInnis and Morehead, 2020).
The efficacy of exercise therapy is well-established, yet a consensus on the optimal modalities and exercise types remains elusive. Shoulder-specific exercise therapy is distinguished by its targeted, biomechanically-driven approach that simultaneously activates scapulothoracic musculature and glenohumeral stabilizers. This approach encompasses various components, including scapular stabilization, positioning, proprioception, neuromuscular control, strength and extension, all integral to enhancing shoulder joint function (Hanratty et al., 2012; Holmgren et al., 2014; Hanratty et al., 2016). While articles have investigated the effectiveness of exercise-specific therapy for adolescent scoliosis (Xin-jing et al., 2024), there remains a relative paucity of research exploring the efficacy of shoulder-specific exercise therapy.
This systematic review was previously registered with the International Prospective Register of Systematic Reviews (PROSPERO CRD: 42024550602) and adheres to the guidelines set forth by the Cochrane Collaboration (Julian et al., 2019).
Searches across five databases: PubMed/MEDLINE, Web of Science, ScienceDirect, and CNKI were conducted for studies on exercise therapy for rotator cuff-related shoulder pain published from the inception of each database through June 2024. The search terms for databases included exercise, exercise therapy, exercise prescription, training, kinematics, shoulder pain, rotator cuff-related shoulder pain, subacromial impingement syndrome, rotator cuff injury, and rotator cuff tendinopathy. The controlled descriptors and keywords were combined with the ‘AND’ and ‘OR’ Boolean operators when appropriate.
For inclusion, studies were required to involve patients with clinically diagnosed rotator cuff-related shoulder pain (RCRSP), including conditions such as subacromial impingement/pain, rotator cuff injury, and rotator cuff tendinopathy. The intervention group was required to undergo specific exercise therapy, which could include individualized, supervised, progressive, or targeted exercises, or exercise combined with conventional treatments. The control group was to receive other conventional exercise interventions distinct from those in the intervention group. Outcome measures had to include at least one of the following: Pain Visual Analogue Scale (VAS) to assess shoulder pain; Constant-Murley Score (CMS) or Disability of the Arm, Shoulder and Hand Score (DASH) to assess shoulder functional status. The literature types considered were randomized controlled trials published nationally and internationally.
Exclusion criteria included studies involving patients with shoulder pain not related to rotator cuff issues (e.g., frozen shoulder) or those who had undergone shoulder surgery. Additionally, studies were excluded if the full text was unavailable, if data were incomplete, or if the literature was duplicated.
Data extraction was carried out by one researcher and subsequently verified for accuracy by a second researcher. Any disagreements were resolved by a third researcher, who facilitated discussions with the first two researchers to reach a consensus. Multi-arm studies were partitioned into multiple two-arm comparisons in accordance with a pre-established table detailing the characteristics of the included studies. This table included details such as: first author’s name, year of publication, characteristics of the study population (diagnosis, sample size, age, gender), intervention details (experimental group, control group), time to assessment (with baseline data collected after the start of the intervention), outcome.
Risk of bias assessment was performed according to the principles of the Cochrane Handbook and operated through Review Manager 5.4 software. Seven indicators of quality were evaluated for the included literature, including: randomized allocation scheme, concealed allocation scheme, blinding method, blinding for outcome assessment, completeness of outcome data, selective reporting of study results, and other biases. The results of bias evaluation for each item were categorized as low risk (green), high risk (red), and unclear risk (yellow).
The article was subjected to traditional meta-analysis and quality assessment using RevMan 5.4 software. Statistical heterogeneity was evaluated with the I2 test, considering the interventions and outcome measures employed. For studies with low statistical heterogeneity (I2≦50%), the fixed-effects model was applied; otherwise, the random-effects model was used. Outcomes from the included studies were analyzed using mean difference (MD) with 95% confidence intervals for consistent measurement tools, and standardized mean difference (SMD) with 95% confidence intervals for varying measurement tools. The analysis focused on effect measures related to pain and functional outcomes. If studies reported means and SDs for baseline and outcomes only, evidence-based medicine analysis methods were referenced (Ming, 2001; da Costa et al., 2013), the mean and SD of the change before and after were calculated, and when the number of intervention groups in the included literature was 3, the groups were combined based on the comparisons, as recommended by the Cochrane Handbook (Cumpston et al., 2019). Finally, the results were presented in two time periods (<2 months and ≧2 months).
The study screening flowchart is outlined by the PRISMA guidelines (Figure 1). Utilizing the specified keywords (including Mesh terms and synonyms), a comprehensive search yielded 5,368 records across multiple databases: Pubmed/MEDLINE (n = 3,170), Web of Science (n = 1,556), Science Direct (n = 222), and China Knowledge Network (CNKI) (n = 420). After duplicates were removed, 3,875 articles proceeded to initial screening. Following the review of titles and abstracts, 3,790 articles were excluded. A full-text assessment of the remaining 85 articles led to the inclusion of 13 studies, which featured 15 pairs of intervention and control groups, encompassing a total of 690 patients for the final analysis (Başkurt et al., 2011; Beaudreuil et al., 2011; Struyf et al., 2013; Hallgren et al., 2014; Dejaco et al., 2017; Boudreau et al., 2019; Gutiérrez-Espinoza et al., 2019; Tahran and Yeşilyaprak, 2020; Eliason et al., 2021; Macías-Hernández et al., 2021; AlAnazi et al., 2022; İğrek and Çolak, 2022; Gutiérrez Espinoza et al., 2023).
The basic characteristics and intervention details of the included literature are shown in Figure 2 and Supplementary Figure S1, including when the study was published, diagnostic type of the study population, sample size, age, gender, interventions and specific details, and time of assessment of outcomes and assessment metrics. Of the RCRSP patients included in the study, diagnosis types included subacromial impingement/pain (10 studies, n = 586) (Başkurt et al., 2011; Beaudreuil et al., 2011; Struyf et al., 2013; Hallgren et al., 2014; Gutiérrez-Espinoza et al., 2019; Tahran and Yeşilyaprak, 2020; Eliason et al., 2021; AlAnazi et al., 2022; İğrek and Çolak, 2022; Gutiérrez Espinoza et al., 2023), rotator cuff tendinopathy (2, n = 78) (Dejaco et al., 2017; Boudreau et al., 2019) and partial rotator cuff tear (1, n = 26) (Macías-Hernández et al., 2021), with a mean age of 49.1 years (range 39–59 years). In terms of interventions, one study used handgrip strength exercises (AlAnazi et al., 2022), five used scapular stabilization exercises (including dynamic humeral centering, glenohumeral adductor activation) (Başkurt et al., 2011; Beaudreuil et al., 2011; Struyf et al., 2013; Boudreau et al., 2019; Gutiérrez Espinoza et al., 2023), three used eccentric exercise (Hallgren et al., 2014; Dejaco et al., 2017; Macías-Hernández et al., 2021), five used joint mobilization/stretching (Gutiérrez-Espinoza et al., 2019; Tahran and Yeşilyaprak, 2020; Eliason et al., 2021; İğrek and Çolak, 2022) and one utilized proprioceptive neuromuscular facilitation exercises (İğrek and Çolak, 2022). Of the included studies, two were multicenter trials (Tahran and Yeşilyaprak, 2020; İğrek and Çolak, 2022), and pairwise comparisons were made between different intervention groups and the same control groups. Since there is no clear definition of the intervention period for rotator cuff-related shoulder pain, this article combines the previous literature and uses 2 months and 6 months as the intervention period for rotator cuff-related shoulder pain (Gebremariam et al., 2014; Hak et al., 2015; Lin et al., 2019). In this article, 2 months and 6 months were designated as the time points for short-term, mid-term, and long-term interventions. Five studies had follow-up periods both <2 months and ≧2 months (Dejaco et al., 2017; Eliason et al., 2021; Macías-Hernández et al., 2021; AlAnazi et al., 2022; İğrek and Çolak, 2022). Besides, four had long-term follow-up (>6 months) (Beaudreuil et al., 2011; Dejaco et al., 2017; Eliason et al., 2021; Macías-Hernández et al., 2021). However, the results of long-term follow-up were excluded from this analysis due to the substantial impact of participant attrition on the experimental outcomes. In addition to shoulder pain, functional scores were reported in 10 studies (Hallgren et al., 2014; Dejaco et al., 2017; Boudreau et al., 2019; Gutiérrez-Espinoza et al., 2019; Tahran and Yeşilyaprak, 2020; Eliason et al., 2021; Macías-Hernández et al., 2021; AlAnazi et al., 2022; İğrek and Çolak, 2022; Gutiérrez Espinoza et al., 2023), two studies only reported shoulder pain scores (Başkurt et al., 2011; Struyf et al., 2013), and one only functional scores (Beaudreuil et al., 2011).
The distribution of risk of bias studies is generated according to the Cochrane Risk of Bias Tool and a summary table (Figure 3), with green representing low risk, yellow representing unclear risk, and red representing high risk. Overall, seven studies were of high quality (Beaudreuil et al., 2011; Hallgren et al., 2014; Boudreau et al., 2019; Gutiérrez-Espinoza et al., 2019; Tahran and Yeşilyaprak, 2020; Eliason et al., 2021; Gutiérrez Espinoza et al., 2023), four studies were of medium quality (Başkurt et al., 2011; Dejaco et al., 2017; AlAnazi et al., 2022; İğrek and Çolak, 2022) and two studies were of low quality (Struyf et al., 2013; Macías-Hernández et al., 2021). The most common methodological flaw was implementation bias, with all studies being high risk; followed by a small sample size (n < 30), with three being high risk (Struyf et al., 2013; Macías-Hernández et al., 2021; İğrek and Çolak, 2022), and then measurement bias, with four not reporting measurer blinding (Başkurt et al., 2011; Eliason et al., 2021; AlAnazi et al., 2022; İğrek and Çolak, 2022). Furthermore, one study was informed by the measurer (Dejaco et al., 2017). The overall methodological quality of the included literature was good in terms of selection bias (random allocation and allocation scheme concealment) and follow-up bias. The funnel plot scatter is roughly symmetrical (Supplementary Figure S2), indicating that publication bias was low in the included studies.
Figure 4 is a forest plot of the pooled analysis of VAS pain scores (<2 months, 10 studies, n = 378; ≥2 months, eight studies, n = 353), which showed low heterogeneity across studies (I2 = 5%, P = 0.40), and combined effect sizes using a fixed-effects model, which indicated that exercise-specific strategies were more efficacious than non-specific exercises (SMD = −0.31, 95% CI: 0.46 to −0.16, P < 0.0001), but the effect was slight. Similarly, VAS scores were similarly lower in the intervention group than in the control group across the two time periods (<2 months (SMD = −0.35, 95% CI: 0.56 to −0.15, P = 0.0007); and ≥2 months (SMD = −0.26, 95% CI: 0.47 to −0.05, P = 0.01)), and the short-term effect was slightly superior to the mid-term effect.
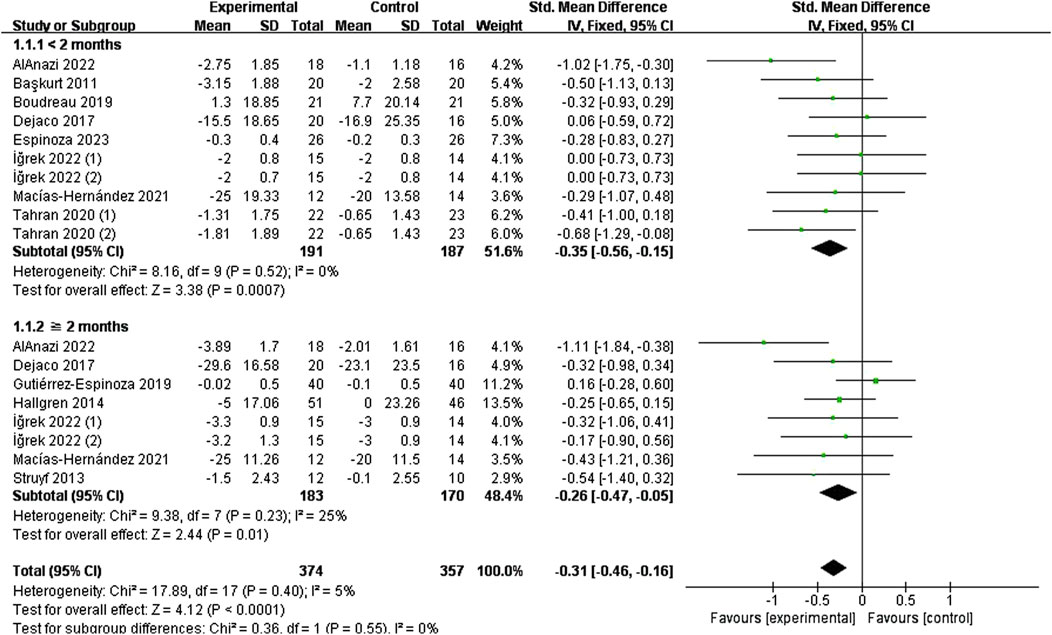
Figure 4. Effect of specific exercise intervention, compared with general exercise or routine physical therapy on shoulder pain over VAS.
The effect of specific exercises on CMS function scores (<2 months, seven studies, n = 291; ≥2 months, eight studies, n = 447), with pooled analyses suggesting low heterogeneity across items (I2 = 21%, P = 0.22), and the combined effect sizes using a fixed-effects model, which showed that the intervention group was higher than the control group (SMD = 0.59, 95% CI: 0.44 to 0.74, P < 0.00001) (Figure 5). The results of the time subgroup analysis showed that the CMS scores of the intervention group were lower than those of the control group (<2 months (SMD = 0.71, 95% CI: 0.47 to 0.96, P < 0.00001); ≥2 months (SMD = 0.51, 95% CI: 0.32 to 0.71, P < 0.00001)), and that short-term effects were better than mid-term effects.
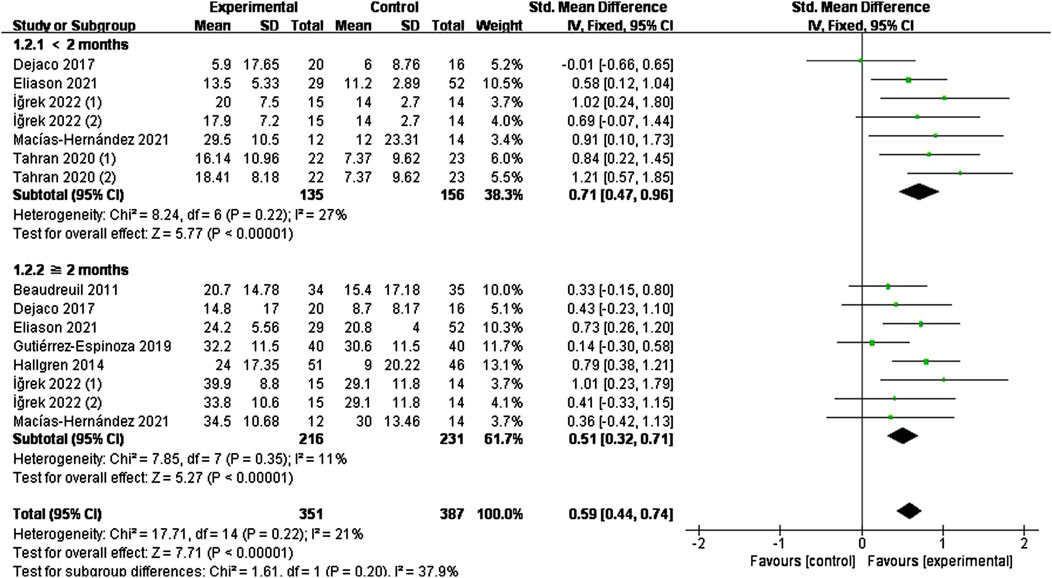
Figure 5. Effect of specific exercise intervention, compared with general exercise or routine physical therapy on shoulder function over CMS.
The effect of specific exercise on DASH function scores (<2 months, five studies, n = 218; ≥2 months, five studies, n = 269) takes high heterogeneity across studies (I2 = 81%, P < 0.00001). So we conducted a sensitivity analysis to identify the source of the heterogeneity by systematically removing each study. This analysis found it was originated from one study (Gutiérrez-Espinoza et al., 2019), which was subsequently excluded. Figure 6 shows the forest plot after exclusion, where heterogeneity was greatly reduced (I2 = 28%, P = 0.20). Combining effect sizes using a fixed model showed a reduction in DASH scores in the intervention group compared to the control group (SMD = −0.60, 95% CI: 0.80 to −0.39, P < 0.00001). Time subgroup analyses showed moderate heterogeneity in the <2 months subgroup (I2 = 53%, P = 0.07), no heterogeneity in the ≥2 months subgroup (I2 = 0%, P = 0.75). The intervention group demonstrated superior efficacy compared to the control in both time subgroups (short-term (SMD = −0.71, 95% CI: 0.99 to −0.43, P < 0.00001), mid-term (SMD = −0.47, 95% CI: 0.76 to −0.18, P = 0.001)). The short-term effect (<2 months) was similarly superior to the mid-term effect (≥2 months)
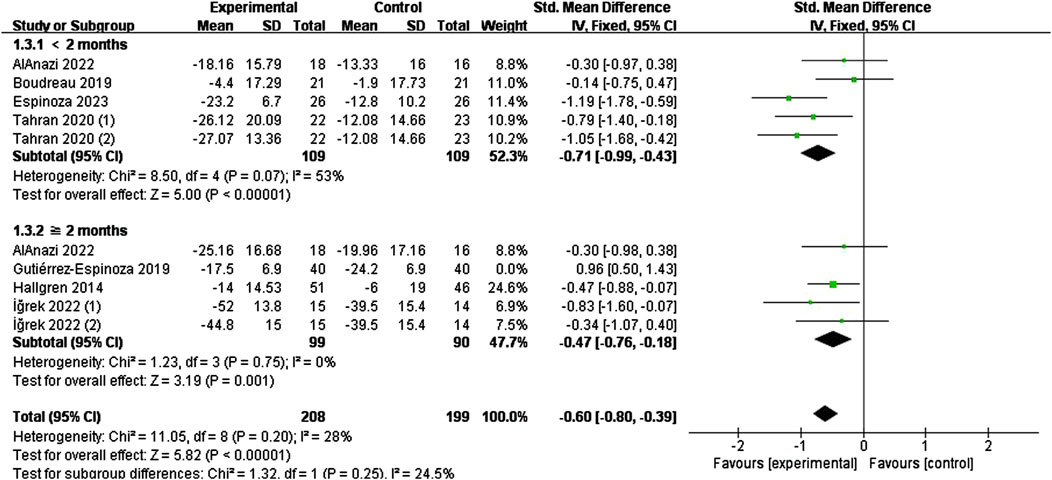
Figure 6. Effect of specific exercise intervention, compared with general exercise or routine physical therapy on shoulder function over DASH.
As shown in Figures 3, 7 specific modes of exercise mildly improved short-term shoulder pain compared with general exercise/conventional physical therapy (handgrip strength exercises (SMD = −1.02, 95% CI: 1.75 to −0.30, P = 0.005), scapular stability training (SMD = −0.36, 95% CI: 0.70 to −0.02, P = 0.04), shoulder mobilization/stretching (SMD = −0.41, 95% CI: 0.77 to −0.04), P = 0.03)), whereas eccentric exercise (SMD = −0.09, 95% CI: 0.59 to −0.42), P = 0.74) and proprioceptive training (SMD = −0.00, 95% CI: 0.73 to 0.73, P = 1.00) did not show improvement.
At ≥2 months of follow-up, no significant improvement was seen in any of the four exercises except for handgrip strength exercises (SMD = −1.11, 95% CI: 1.84 to −0.38, P = 0.003).
CMS score subgroup analyses are shown in Figure 8. During the <2-month follow-up period, shoulder mobilization/stretching (SMD = 0.84, 95% CI: 0.54 to 1.13, P < 0.00001) improved CMS scores, whereas eccentric exercise (SMD = 0.35, 95% CI: 0.16 to 0.87, P = 0.17) and proprioceptive training (SMD = 0.69, 95%CI: 0.07 to 1.44, P = 0.07) did not show any improvement compared to the control group.
At ≥2-month follow-up, improvements were seen in shoulder mobilization/stretching (SMD = 0.50, 95% CI: 0.20 to 0.80, P = 0.0009) and eccentric exercise (SMD = 0.63, 95% CI: 0.31 to 0.96, P = 0.0001) whereas scapular stabilization exercises (SMD = 0.33, 95% CI: 0.15 to 0.80, P = 0.18) and proprioceptive training (SMD = 0.41, 95% CI: 0.33 to 1.15, P = 0.28) did not show improvement.
As shown in Figure 9, scapular stabilization exercise (SMD = −0.67, 95% CI: 1.10 to −0.25, P = 0.002) and shoulder mobilization/stretching (SMD = −0.91, 95% CI: 1.35 to −0.48, P < 0.0001) improved function in the short term in the DASH score. Shoulder mobilization/stretching (SMD = −0.83, 95% CI: 1.60 to −0.07, P = 0.03) and eccentric exercise (SMD = −0.47, 95% CI: 0.88 to −0.07, P = 0.02) improved functional performance in the mid-term period, whereas other types of exercise did not.
This review identified 13 randomized controlled trials (690 participants) comparing specific exercise therapy—defined as exercises targeting the activation and coordination of the scapular pectoralis muscles and/or the dynamic stabilizers of the humerus, including scapular stabilization, positioning, proprioception, neuromuscular control, strengthening, and stretching (Hanratty et al., 2012; Holmgren et al., 2014; Hanratty et al., 2016)— with conventional physical therapy or general exercise for rotator cuff-related shoulder pain. Specific exercise types and dosages were developed by clinicians and physical therapists. Our pooled analysis indicated that specific exercises improved shoulder pain (VAS) and function (CMS, DASH), though the effects were not pronounced and were slightly better within 2 months.
Subgroup analyses showed that handgrip strength exercises were effective in improving shoulder pain, but did not significantly improve function. Previous studies have revealed that the connection between handgrip strength and rotator cuff function is significant. A stronger handgrip boosts neural signals from the hand to the shoulder. Handgrip-strengthening exercises activate pathways that improve movement control and help integrate sensory information from both the shoulder and hand (Roberts et al., 2008; Kobesova et al., 2015). Besides, it decreases the activation of anterior portion of the deltoid, which contributes to impingement. No pain or functional improvement was seen with proprioceptive training compared to the control group, a finding that remains debatable due to the small study and sample size. On the other hand, proprioceptive training were proved effective in reducing pain in patients with partial supraspinatus tears in long-term follow-up, according to other research (Kim et al., 2015; Salles et al., 2015). This difference could be attributed to patient characteristics, variations in treatments, and differences in assessment methods between the studies. Scapular stabilization training and shoulder mobilization/stretching showed mild improvement in short-term shoulder pain, whereas an eccentric exercise program did not have a significant effect on short-term pain, and none of the three specific exercise types improved the pain level of the reduced shoulder after 2 months. Shoulder mobility/stretching had a positive effect on both CMS and DASH scores in the short to middle term, and eccentric exercise had an effect on the medium-term effect but not the short-term, and more evidence is still needed to demonstrate the effect of scapular stabilization exercises on shoulder function in the short to medium term. Research has shown that the position of the humeral head and scapula affects the width of the subacromial space. As a result, strengthening the depressor muscles, such as the subscapularis, infraspinatus, and teres minor, is crucial (Faber et al., 2006; Camargo et al., 2009). Therefore, shoulder rehabilitation should incorporate scapular stabilization training as well as shoulder mobilization and stretching exercises. One review supports our view, indicating that eccentric exercise offers a slightly better reduction in pain compared to other exercises, though it does not significantly improve function, especially during middle to long-term follow-up (Larsson et al., 2019). On the other hand, incorporating eccentric loads, which are not limited by concentric strength, seem to be more effective than traditional resistance training for enhancing strength, power, and speed performance (Douglas et al., 2017).
The primary factor affecting the quality of the included literature is implementation bias, as all studies are considered high-risk. Due to the specificity of exercise interventions, the exercise programs for different subjects must be continually evaluated and adjusted, making it unrealistic to blind researchers to group assignments. In eight studies, the evaluators were blinded, while one was not, which may lead to distortions in the study results (Chen et al., 2022). Additionally, the second issue is the insufficient sample size, which fails to accurately reflect the overall situation. In the data collection and organization, baseline and outcome score data were given in each of the eight articles (Başkurt et al., 2011; Beaudreuil et al., 2011; Struyf et al., 2013; Hallgren et al., 2014; Dejaco et al., 2017; Eliason et al., 2021; Macías-Hernández et al., 2021; AlAnazi et al., 2022). In order to further assess the effect of the intervention, statistical methods were used to calculate the mean and SD of the before and after changes which may also have some impact on the outcome (da Costa et al., 2013).
Forest plots evaluating DASH function revealed substantial heterogeneity among studies, particularly at the 2-month time point. This heterogeneity was significantly reduced following sensitivity analysis through item-by-item exclusion and subsequent subgroup analyses (Figure 6).
Previous reviews and guidelines have recommended exercise as a therapeutic approach through a variety of mechanisms, including neuromuscular synergism that can reduce pain and improve function in patients with RCRSP (Diercks et al., 2014; Holmgren et al., 2014; Powell et al., 2022). Based on the latest scientific literature and clinical experience, exercise is best performed at low intensity and high frequency, within the pain threshold, with a focus on eccentric exercise to strengthen the rotator cuff and eccentric exercise to strengthen the scapular stabilizers, with specific exercise strategies that can be defined as the activation and coordination of the shoulder-thoracic musculature or movements involving the dynamic humeral stabilizers of the shoulder joint. These exercises include scapular stabilization, postural adjustments, proprioception, neuromuscular control, strength training, and stretching, and the exercises must involve some form of resistance such as one’s own body weight, elastic resistance, weight-bearing equipment, dumbbells, and/or strength training machines.
Aside from the specific exercise modalities, the role of the physiotherapist is often overlooked. However, the physiotherapist can unintentionally influence patients' perceptions of their treatment and even their decisions regarding surgery. As therapists vary in their treatment modalities and patients' physical conditions and rehabilitation goals, the above exercise methods need to be personalized through individualization (Bennell et al., 2014) This reflects the importance of applying exercise prescription (Crookham, 2013; Sijia et al., 2023), which serves as a vehicle for exercise therapy and can specify parameters such as the patient’s exercise modality and dosage, greatly increasing the efficacy of exercise interventions. Although there is a large amount of literature related to the application of exercise therapy in RCRSP, there is a lack of documentation on the prescription of specific exercise modalities and dosages, which has resulted in the existence of limitations in the development of exercise prescription in China, which is currently more widely used in the study of common chronic diseases in middle-aged and old-aged people (e.g., hypertension, diabetes mellitus, osteoarthritis, etc.) (Pedersen and Saltin, 2015; Yuge and Zhenguo, 2021) and fewer studies in shoulder injury diseases. Inspiringly, the publication of an expert consensus to further clarify the definition, development, and implementation process of exercise prescription may help resolve this difficulty (Yuefeng, 2023).
The specific parameters of the exercise are also crucial, and they must be aligned with standardized prescription reports that include detailed intervention information. A study has shown that the Consensus on Exercise Intervention Reporting Template (CERT) was developed specifically to address the issue of incomplete reporting of exercise interventions (Kucksdorf et al., 2024). However, the completeness of reporting of exercise intervention content is currently poor in research trials in patients with rotator cuff disease. CERT is a reliable tool for assessing the completeness of reporting of exercise interventions in trials. Future research should be based on CERT for the assessment of outcomes and reporting of exercise protocols, which can greatly contribute to the analyzability and generalizability of research results.
The results of this article suggest that specific modes of exercise are effective in improving pain levels and functional status in rotator cuff-related shoulder pain, but they do not demonstrate a significant advantage over general exercise or conventional physical therapy. The results of other reviews have shown that eccentric exercise and scapular stability training can lead to a slight reduction in pain levels in patients with subacromial impingement syndrome, but with little clinical significance (Larsson et al., 2019; Naunton et al., 2020; Ravichandran et al., 2020), which is consistent with the findings of this article. Combining the results from the subgroup analysis of intervention types suggests that incorporating shoulder-specific exercise therapies into a tailored shoulder rehabilitation program could be effective. Implementing these therapies through targeted exercise prescriptions, addressing multiple areas, may enhance pain relief and functional improvement for optimal clinical outcomes.
This review has several notable strengths. Firstly, it encompasses a broad range of exercises, incorporating a diverse array of specific intervention types. Secondly, unlike prior studies that have focused solely on subacromial impingement, rotator cuff tendinopathy, or rotator cuff injuries in isolation, this review is the first to examine the overall impact on the efficacy of RCRSP. In clinical practice, pain is usually the main reason for RCRSP patients to visit the clinic (van der Windt et al., 1996; Mitchell et al., 2005), and our results provide a new reference for the development and implementation of appropriate exercise prescriptions. Individualized, supervised, progressive, and targeted exercise regimens based on prescriptions could be a new option in addition to surgery, corticosteroid injections, and physical therapy (Dubé et al., 2023).
This article identifies the efficacy of specific exercises, but there are still some limitations. Due to individual differences, such as varying rehabilitation goals and physical conditions among patients, it is unrealistic to establish uniform standards for exercise types and dosages. These factors contribute to the challenges of applying specific exercises in a clinical setting. Among the articles included in this study, two articles were vague in their descriptions of intervention details (Dejaco et al., 2017; Eliason et al., 2021), and the rest of the articles did not establish corresponding exercise dosages norms, such as insufficient description of key features like pain during loading, duration of exercise, rest time between sets of exercise, and the rhythm of exercise. As exercise dosage is another important component that has a status comparable to that of exercise type (Bennell et al., 2014; Holmgren et al., 2014), a full understanding can help to obtain convincing study results. Secondly, participant attrition results in the failure to analyze long-term efficacy (>6 months). Potential reasons include patient crossover to surgical interventions and high participant mobility, particularly in multicenter trials. Only five of the 13 studies included in the analysis reported data beyond 6 months, with small sample sizes. Despite the limited evidence, we advocate for phased exercise prescriptions in clinical practice, with a focus on maintenance programs to ensure sustained benefits. For outcome measurement, rationale for subjective metrics (VAS, CMS, and DASH) are validated tools with well-established minimal clinically important differences (MCID) suitable for meta-analysis pooling. These metrics directly reflect patients’ perceptions of functional recovery and quality of life. Though we recognize the benefits of adding objective measurements, these outcome indicators are diverse. The movement of joints occurs in multiple directions, different studies may describe ROM in diverse ways due to these variations. On the other hand, strength testing protocols vary significantly, from isokinetic testing to manual resistance. Imaging findings, such as MRI measurements of tendon thickness, show a poor correlation with clinical symptoms, and there are no standardized imaging scores available yet.
Exercise is frequently recommended as a treatment for chronic sports injuries according to previous review guidelines. This article demonstrates that specific modes of exercise for the shoulder can enhance both pain relief and functional status in patients with Rotator Cuff-Related Shoulder Pain (RCRSP). While these targeted exercises offer valuable insights for clinical shoulder rehabilitation prescriptions, they do not show a obvious therapeutic advantage over general exercise or conventional physical therapy. Furthermore, the lack of standardized and effective exercise reporting across studies constrains the practical application and development of exercise prescriptions in clinical setting.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
DW: Conceptualization, Formal Analysis, Software, Writing – original draft, Writing – review and editing, Data curation, Methodology. ZW: Data curation, Formal Analysis, Software, Validation, Writing – original draft. HK: Data curation, Investigation, Writing – original draft, Formal Analysis, Validation. JZ: Data curation, Formal Analysis, Writing – original draft. SZ: Data curation, Writing – original draft. JT: Validation, Writing – original draft. LX: Formal analysis, Writing - review and editing. JL: Conceptualization, Project administration, Supervision, Writing – review and editing, Funding acquisition. YS: Project administration, Supervision, Writing – review and editing, Funding acquisition, Conceptualization. CZ: Conceptualization, Project administration, Supervision, Writing – review and editing, Funding acquisition, Resources.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the National Students’ Platform for Innovation and Entrepreneurship Training Program of China (Grant No. 202312121005), The Natural Science Foundation of Guangdong Province (No. 2024A1515011231) and the Clinical Research Special Fund of the president's Foundation of the Third Affiliated Hospital of Southern Medical University (No. YL202206).
The authors declare that this research was conducted without any commercial or financial relationships that could be perceived as potential conflicts of interest.
The authors declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2025.1560597/full#supplementary-material
Abdulla, S. Y., Southerst, D., Côté, P., Shearer, H. M., Sutton, D., Randhawa, K., et al. (2015). Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man. Ther. 20, 646–656. doi:10.1016/j.math.2015.03.013
Alanazi, A., Alghadir, A. H., and Gabr, S. A. (2022). Handgrip strength exercises modulate shoulder pain, function, and strength of rotator cuff muscles of patients with primary subacromial impingement syndrome. Biomed. Res. Int. 2022, 9151831. doi:10.1155/2022/9151831
Başkurt, Z., Başkurt, F., Gelecek, N., and Özkan, M. H. (2011). The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J. Back Musculoskelet. Rehabil. 24, 173–179. doi:10.3233/bmr-2011-0291
Beaudreuil, J., Lasbleiz, S., Richette, P., Seguin, G., Rastel, C., Aout, M., et al. (2011). Assessment of dynamic humeral centering in shoulder pain with impingement syndrome: a randomised clinical trial. Ann. Rheum. Dis. 70, 1613–1618. doi:10.1136/ard.2010.147694
Bennell, K. L., Dobson, F., and Hinman, R. S. (2014). Exercise in osteoarthritis: moving from prescription to adherence. Best. Pract. Res. Clin. Rheumatol. 28, 93–117. doi:10.1016/j.berh.2014.01.009
Boudreau, N., Gaudreault, N., Roy, J. S., Bédard, S., and Balg, F. (2019). The addition of glenohumeral adductor coactivation to a rotator cuff exercise program for rotator cuff tendinopathy: a single-blind randomized controlled trial. J. Orthop. Sports Phys. Ther. 49, 126–135. doi:10.2519/jospt.2019.8240
Camargo, P. R., Haik, M. N., Ludewig, P. M., Filho, R. B., Mattiello-Rosa, S. M., and Salvini, T. F. (2009). Effects of strengthening and stretching exercises applied during working hours on pain and physical impairment in workers with subacromial impingement syndrome. Physiother. Theory Pract. 25, 463–475. doi:10.3109/09593980802662145
Chen, J. W., Maldonado, D. R., Kowalski, B. L., Miecznikowski, K. B., Kyin, C., Gornbein, J. A., et al. (2022). Best practice guidelines for propensity score methods in medical research: consideration on theory, implementation, and reporting. A review. Arthroscopy 38, 632–642. doi:10.1016/j.arthro.2021.06.037
Crookham, J. (2013). A guide to exercise prescription. Prim. Care 40, 801–820. vii. doi:10.1016/j.pop.2013.08.002
Cumpston, M., Li, T., Page, M. J., Chandler, J., Welch, V. A., Higgins, J. P., et al. (2019). Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 10, Ed000142. doi:10.1002/14651858.ed000142
Da Costa, B. R., Nüesch, E., Rutjes, A. W., Johnston, B. C., Reichenbach, S., Trelle, S., et al. (2013). Combining follow-up and change data is valid in meta-analyses of continuous outcomes: a meta-epidemiological study. J. Clin. Epidemiol. 66, 847–855. doi:10.1016/j.jclinepi.2013.03.009
Dejaco, B., Habets, B., Van Loon, C., Van Grinsven, S., and Van Cingel, R. (2017). Eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy: a randomized, single blinded, clinical trial. Knee Surg. Sports Traumatol. Arthrosc. 25, 2051–2059. doi:10.1007/s00167-016-4223-x
Diercks, R., Bron, C., Dorrestijn, O., Meskers, C., Naber, R., De Ruiter, T., et al. (2014). Guideline for diagnosis and treatment of subacromial pain syndrome: a multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop. 85, 314–322. doi:10.3109/17453674.2014.920991
Doiron-Cadrin, P., Lafrance, S., Saulnier, M., Cournoyer, É., Roy, J. S., Dyer, J. O., et al. (2020). Shoulder rotator cuff disorders: a systematic review of clinical practice guidelines and semantic analyses of recommendations. Arch. Phys. Med. Rehabil. 101, 1233–1242. doi:10.1016/j.apmr.2019.12.017
Douglas, J., Pearson, S., Ross, A., and Mcguigan, M. (2017). Chronic adaptations to eccentric training: a systematic review. Sports Med. 47, 917–941. doi:10.1007/s40279-016-0628-4
Dubé, M. O., Desmeules, F., Lewis, J. S., and Roy, J. S. (2023). Does the addition of motor control or strengthening exercises to education result in better outcomes for rotator cuff-related shoulder pain? A multiarm randomised controlled trial. Br. J. Sports Med. 57, 457–463. doi:10.1136/bjsports-2021-105027
Eliason, A., Harringe, M., Engström, B., and Werner, S. (2021). Guided exercises with or without joint mobilization or no treatment in patients with subacromial pain syndrome: a clinical trial. J. Rehabil. Med. 53, jrm00190. doi:10.2340/16501977-2806
Faber, E., Kuiper, J. I., Burdorf, A., Miedema, H. S., and Verhaar, J. A. (2006). Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J. Occup. Rehabil. 16, 6–24. doi:10.1007/s10926-005-9003-2
Gebremariam, L., Hay, E. M., Van Der Sande, R., Rinkel, W. D., Koes, B. W., and Huisstede, B. M. (2014). Subacromial impingement syndrome--effectiveness of physiotherapy and manual therapy. Br. J. Sports Med. 48, 1202–1208. doi:10.1136/bjsports-2012-091802
Gismervik, S., Drogset, J. O., Granviken, F., Rø, M., and Leivseth, G. (2017). Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet. Disord. 18, 41. doi:10.1186/s12891-017-1400-0
Greenberg, D. L. (2014). Evaluation and treatment of shoulder pain. Med. Clin. North Am. 98, 487–504. doi:10.1016/j.mcna.2014.01.016
Greving, K., Dorrestijn, O., Winters, J. C., Groenhof, F., Van Der Meer, K., Stevens, M., et al. (2012). Incidence, prevalence, and consultation rates of shoulder complaints in general practice. Scand. J. Rheumatol. 41, 150–155. doi:10.3109/03009742.2011.605390
Gutiérrez-Espinoza, H., Araya-Quintanilla, F., Gutiérrez-Monclus, R., Ríos-Riquelme, M., Álvarez-Bueno, C., Martínez-Vizcaino, V., et al. (2019). Does pectoralis minor stretching provide additional benefit over an exercise program in participants with subacromial pain syndrome? A randomized controlled trial. Musculoskelet. Sci. Pract. 44, 102052. doi:10.1016/j.msksp.2019.102052
Gutiérrez Espinoza, H., Araya-Quintanilla, F., Pinto-Concha, S., Valenzuela-Fuenzalida, J., López-Gil, J. F., and Ramírez-Velez, R. (2023). Specific versus general exercise programme in adults with subacromial impingement syndrome: a randomised controlled trial. BMJ Open Sport Exerc Med. 9, e001646. doi:10.1136/bmjsem-2023-001646
Hak, A., Rajaratnam, K., Ayeni, O. R., Moro, J., Peterson, D., Sprague, S., et al. (2015). A double-blinded placebo randomized controlled trial evaluating short-term efficacy of platelet-rich plasma in reducing postoperative pain after arthroscopic rotator cuff repair: a pilot study. Sports Health 7, 58–66. doi:10.1177/1941738114548413
Hallgren, H. C., Holmgren, T., Oberg, B., Johansson, K., and Adolfsson, L. E. (2014). A specific exercise strategy reduced the need for surgery in subacromial pain patients. Br. J. Sports Med. 48, 1431–1436. doi:10.1136/bjsports-2013-093233
Hanratty, C. E., Kerr, D. P., Wilson, I. M., Mccracken, M., Sim, J., Basford, J. R., et al. (2016). Physical therapists' perceptions and use of exercise in the management of subacromial shoulder impingement syndrome: focus group study. Phys. Ther. 96, 1354–1363. doi:10.2522/ptj.20150427
Hanratty, C. E., Mcveigh, J. G., Kerr, D. P., Basford, J. R., Finch, M. B., Pendleton, A., et al. (2012). The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin. Arthritis Rheum. 42, 297–316. doi:10.1016/j.semarthrit.2012.03.015
Holmgren, T., Hallgren, H. B., Oberg, B., Adolfsson, L., and Johansson, K. (2014). Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. Br. J. Sports Med. 48, 1456–1457. doi:10.1136/bjsports-2014-e787rep
İğrek, S., and Çolak, T. K. (2022). Comparison of the effectiveness of proprioceptive neuromuscular facilitation exercises and shoulder mobilization patients with Subacromial Impingement Syndrome: a randomized clinical trial. J. Bodyw. Mov. Ther. 30, 42–52. doi:10.1016/j.jbmt.2021.10.015
Julian, P. T., Higgins, J. T., Chandler, J., Cumpston, M., Li, T., Page, M. J., et al. (2019). “Cochrane Handbook for systematic reviews of interventions,” in Cochrane Handbook for systematic reviews of interventions. Editors J. T. Julian, P. T. Higgins, J. Chandler, M. Cumpston, T. Li, M. J. Pageet al. i–xxviii.
Kim, J. J., Lee, S. Y., and Ha, K. (2015). The effects of exercise using PNF in patients with a supraspinatus muscle tear. J. Phys. Ther. Sci. 27, 2443–2446. doi:10.1589/jpts.27.2443
Kobesova, A., Dzvonik, J., Kolar, P., Sardina, A., and Andel, R. (2015). Effects of shoulder girdle dynamic stabilization exercise on hand muscle strength. Isokinet. Exerc. Sci. 23, 21–32. doi:10.3233/ies-140560
Kromer, T. O., Tautenhahn, U. G., De Bie, R. A., Staal, J. B., and Bastiaenen, C. H. (2009). Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J. Rehabil. Med. 41, 870–880. doi:10.2340/16501977-0453
Kucksdorf, J. J., Bartley, J., Rhon, D. I., and Young, J. L. (2024). Reproducibility of exercise interventions in randomized controlled trials for the treatment of rotator cuff-related shoulder pain: a systematic review. Arch. Phys. Med. Rehabil. 105, 770–780. doi:10.1016/j.apmr.2023.09.007
Larsson, R., Bernhardsson, S., and Nordeman, L. (2019). Effects of eccentric exercise in patients with subacromial impingement syndrome: a systematic review and meta-analysis. BMC Musculoskelet. Disord. 20, 446. doi:10.1186/s12891-019-2796-5
Lewis, J. (2016). Rotator cuff related shoulder pain: assessment, management and uncertainties. Man. Ther. 23, 57–68. doi:10.1016/j.math.2016.03.009
Lin, M. T., Chiang, C. F., Wu, C. H., Huang, Y. T., Tu, Y. K., and Wang, T. G. (2019). Comparative effectiveness of injection therapies in rotator cuff tendinopathy: a systematic review, pairwise and Network meta-analysis of randomized controlled trials. Arch. Phys. Med. Rehabil. 100, 336–349.e15. doi:10.1016/j.apmr.2018.06.028
Macías-Hernández, S. I., García-Morales, J. R., Hernández-Díaz, C., Tapia-Ferrusco, I., Velez-Gutiérrez, O. B., and Nava-Bringas, T. I. (2021). Tolerance and effectiveness of eccentric vs. concentric muscle strengthening in rotator cuff partial tears and moderate to severe shoulder pain. A randomized pilot study. J. Clin. Orthop. Trauma 14, 106–112. doi:10.1016/j.jcot.2020.07.031
Mcinnis, L. A., and Morehead, A. (2020). Exercise as a therapeutic intervention. Nurs. Clin. North Am. 55, 543–556. doi:10.1016/j.cnur.2020.06.019
Mitchell, C., Adebajo, A., Hay, E., and Carr, A. (2005). Shoulder pain: diagnosis and management in primary care. Bmj 331, 1124–1128. doi:10.1136/bmj.331.7525.1124
Naunton, J., Street, G., Littlewood, C., Haines, T., and Malliaras, P. (2020). Effectiveness of progressive and resisted and non-progressive or non-resisted exercise in rotator cuff related shoulder pain: a systematic review and meta-analysis of randomized controlled trials. Clin. Rehabil. 34, 1198–1216. doi:10.1177/0269215520934147
Ottenheijm, R. P., Joore, M. A., Walenkamp, G. H., Weijers, R. E., Winkens, B., Cals, J. W., et al. (2011). The Maastricht Ultrasound Shoulder pain trial (MUST): ultrasound imaging as a diagnostic triage tool to improve management of patients with non-chronic shoulder pain in primary care. BMC Musculoskelet. Disord. 12, 154. doi:10.1186/1471-2474-12-154
Pedersen, B. K., and Saltin, B. (2015). Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 25 (Suppl. 3), 1–72. doi:10.1111/sms.12581
Picavet, H. S., and Schouten, J. S. (2003). Musculoskeletal pain in The Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain 102, 167–178. doi:10.1016/s0304-3959(02)00372-x
Pope, D. P., Croft, P. R., Pritchard, C. M., and Silman, A. J. (1997). Prevalence of shoulder pain in the community: the influence of case definition. Ann. Rheum. Dis. 56, 308–312. doi:10.1136/ard.56.5.308
Powell, J. K., Lewis, J., Schram, B., and Hing, W. (2024). Is exercise therapy the right treatment for rotator cuff-related shoulder pain? Uncertainties, theory, and practice. Musculoskelet. Care 22, e1879. doi:10.1002/msc.1879
Powell, J. K., Schram, B., Lewis, J., and Hing, W. (2022). You have (rotator cuff related) shoulder pain, and to treat it, I recommend exercise. A scoping review of the possible mechanisms underpinning exercise therapy. Musculoskelet. Sci. Pract. 62, 102646. doi:10.1016/j.msksp.2022.102646
Ravichandran, H., Janakiraman, B., Gelaw, A. Y., Fisseha, B., Sundaram, S., and Sharma, H. R. (2020). Effect of scapular stabilization exercise program in patients with subacromial impingement syndrome: a systematic review. J. Exerc Rehabil. 16, 216–226. doi:10.12965/jer.2040256.128
Requejo-Salinas, N., Lewis, J., Michener, L. A., La Touche, R., Fernández-Matías, R., Tercero-Lucas, J., et al. (2022). International physical therapists consensus on clinical descriptors for diagnosing rotator cuff related shoulder pain: a Delphi study. Braz J. Phys. Ther. 26, 100395. doi:10.1016/j.bjpt.2022.100395
Roberts, L. V., Stinear, C. M., Lewis, G. N., and Byblow, W. D. (2008). Task-dependent modulation of propriospinal inputs to human shoulder. J. Neurophysiology 100, 2109–2114. doi:10.1152/jn.90786.2008
Salles, J. I., Velasques, B., Cossich, V., Nicoliche, E., Ribeiro, P., Amaral, M. V., et al. (2015). Strength training and shoulder proprioception. J. Athl. Train. 50, 277–280. doi:10.4085/1062-6050-49.3.84
Sijia, F., Han, G., Jun, C., Yunxia, L., Yuefeng, H., and Shiyi, C. (2023). Exercise therapy in the treatment of diseases related to the locomotor system. Chin. J. Sports Med. 42, 74–79.
Steuri, R., Sattelmayer, M., Elsig, S., Kolly, C., Tal, A., Taeymans, J., et al. (2017). Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br. J. Sports Med. 51, 1340–1347. doi:10.1136/bjsports-2016-096515
Struyf, F., Nijs, J., Mollekens, S., Jeurissen, I., Truijen, S., Mottram, S., et al. (2013). Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin. Rheumatol. 32, 73–85. doi:10.1007/s10067-012-2093-2
Tahran, Ö., and Yeşilyaprak, S. S. (2020). Effects of modified posterior shoulder stretching exercises on shoulder mobility, pain, and dysfunction in patients with subacromial impingement syndrome. Sports Health 12, 139–148. doi:10.1177/1941738119900532
Van Der Windt, D. A., Koes, B. W., Boeke, A. J., Devillé, W., De Jong, B. A., and Bouter, L. M. (1996). Shoulder disorders in general practice: prognostic indicators of outcome. Br. J. Gen. Pract. 46, 519–523.
Xin-Jing, W., Chun-Xiao, L., and Jin-Zhu, B. (2024). Meta analysis of the efficacy of physiotherapeutic scoliosis specific exercises in the treatment of adolescent idiopathic scoliosis. Chin. J. Bone Jt. 13, 33–40.
Yuefeng, L. G. W. Z. H. (2023). Chinese expert consensus on exercise prescription (2023). Chin. J. Sports Med. 42, 3–13.
Keywords: exercise therapy, specific exercise, chronic sports injuries, rotator cuff-related shoulder pain, meta-analysis
Citation: Wu D, Wen Z, Ke H, Zhang J, Zhong S, Teng J, Xu L, Li J, Shao Y and Zeng C (2025) Specific modes of exercise to improve rotator cuff-related shoulder pain: systematic review and meta-analysis. Front. Bioeng. Biotechnol. 13:1560597. doi: 10.3389/fbioe.2025.1560597
Received: 14 January 2025; Accepted: 24 March 2025;
Published: 08 April 2025.
Edited by:
Wei Song, Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, ChinaReviewed by:
Gen Li, Shanghai Jiao Tong University School of Medicine, ChinaCopyright © 2025 Wu, Wen, Ke, Zhang, Zhong, Teng, Xu, Li, Shao and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun Zeng, emVuZ2RhdmlkQDEyNi5jb20=; Yan Shao, c2hhb3lhbl9uQDE2My5jb20=; Jintao Li, bGlqaW50YW80OTc5QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.