- 1School of Exercise and Health, Shanghai University of Sport, Shanghai, China
- 2Henan Sports Science and Technology Center (Henan Anti-Doping Center), Zhengzhou, Henan, China
- 3Huanghe Science and Technology College, Zhengzhou, Henan, China
- 4Henan Provincial Third People’s Hospital, Zhengzhou, Henan, China
- 5China Research Center on Aging, Beijing, Beijing, China
- 6School of Physical Education, Jimei University, Xiamen, Fujian, China
Background: Sedentary behaviour has been associated with an increased risk of falls among older adults. Although gait initiation (GI) is a promising tool used to assess fall risk, it has yet to be quantitatively evaluated for dynamic stability in sedentary populations. Tai Chi exercise is believed to be effective in preventing falls in older adults, but its effect on GI stability has not been quantified. This study aims to compare the stability of GI in sedentary older individuals versus those who are long-term Tai Chi exercisers by using a quantitative approach.
Methods: This study included 17 sedentary older women without exercise habits (age: 65.59 ± 3.66 years, average daily sitting time: 8.735 ± 1.847 h/day) and 19 older women who regularly engage in Tai Chi exercise (age: 65.58 ± 3.63 years, years of exercise: 9.84 ± 3.48 years). Every participant underwent five trials of self-paced GI walking tests. Eight cameras and four force plates were used to obtain kinematic and kinetic parameters. The trajectory of the centre of mass (CoM) and the position of the foot placement were recorded. The anterior–posterior (A-P) and medio–lateral (M-L) dynamic stability at the onset and end moments of the single-legged support was calculated using CoM and gait spatiotemporal parameters. The stepping dynamic stability and foot placement positions of both groups were compared.
Results: The Tai Chi group had greater stability in the M-L directions at the swing leg’s toe-off moment and in the M-L and A-P directions at the heel-strike moment, as well as significantly larger step length, step width and step speed during locomotion than sedentary older women. However, the stability in the A-P directions at the swing leg’s toe-off moment and the foot inclination angle was not statistically different between the two groups.
Conclusion: Long-term regular Tai Chi exercise can enhance the dynamic stability of GI in older women, and effectively improve their foot placement strategy during GI. The findings further confirm the negative effect of sedentary on the stability control of older women and the positive role of Tai Chi in enhancing their gait stability and reducing the risk of falls.
Background
Falling is an increasingly serious public health issue encountered by many aging countries. According to the fourth national health service survey conducted by the Ministry of Health in China, falls are the primary cause of injury (defined as undergoing medical treatment or having restricted activity for over a day after being injured) among key disease prevention and control measures. Falls account for the highest percentage (45.9%) of such injuries (Ministry of Health, 2008). The Centres for Disease Control and Prevention (CDC) in the United States issued a report (Centers for Disease Control and Prevention, 2023a), which highlights that falls are the principal cause of injuries and injury-related fatalities for persons aged 65 years and older. About one in four elderly people, or more than 14 million, experience a fall each year. Medical expenses incurred by such falls surpass $ 50 billion, with Medicare and Medicaid covering 75% of the cost (Kakara, 2023). The report indicates a higher proportion of falls amongst females (28.9%) than males (26.1%). Accidental falls caused the death of 38,742 elderly persons at a rate of 78.0 per 100,000 population in 2021. The mortality rate due to falls has been increasing, with a 30% increase over the past decade (Haddad et al., 2019; Centers for Disease Control and Prevention, 2023b).
The U.S. Preventive Services Task Force (USPSTF) recommends exercise interventions to prevent falls in community-dwelling adults 65 years or older who are at increased risk for falls (U.S.Preventive Services, 2018). Evidence-Based Falls Prevention Programs state that Tai Chi to be one of the most effective exercises for preventing falls (National Council on Aging, 2023). Studies have indicated a significant correlation among physical activity, reaction time and fall risk (Vala et al., 2023; Wang et al., 2023). Engaging in physical activity and avoiding prolonged sedentary behaviour can help reduce the risk of falls among older adults (Lee, 2020). In addition, dynamic stability of gait and lower limb support are considered important risk factors for falls among the older population (Yang and Liu, 2020). Community-dwelling older adults tend to experience falls most frequently during walking activities (Talbot et al., 2005).
With the advancement of sensor technology, wearable sensors of human daily activities provide significant opportunities for the development and evaluation of interventions aimed at improving the mobility of older adults (Boyer et al., 2023). For example, task-oriented movement learning programmes facilitated by sensor technology can enhance the mobility of older adults by improving the skills required for walking (Brach and VanSwearingen, 2013). In addition, neural networks and machine-learning approaches can help monitor human activity and detect and predict potential fall risks (Hartmann et al., 2023). Xue and Liu (2021) provided a comprehensive review of Hidden Markov Models, highlighting their considerable potential in handling sequential data and predicting hidden states, enabling the monitoring of human activities, gait and fall behaviour.
However, older adults are at a high risk of falling whilst performing common daily tasks, such as walking, changing posture or initiating steps in different environments (Talbot et al., 2005). However, there is currently a lack of simple and effective methods for predicting the risk of falls during gait initiation (GI). GI is one of the highest proportions of falls among older adults during motor activities (Robinovitch et al., 2013).
GI refers to the transition from a static standing posture to steady-state walking, which poses challenges to systems responsible for postural control (Winter 1995). GI necessitates the transition from standing to a stable gait, so it provides an ideal task for studying the mechanisms of falls in older adults and the effect of ageing on mobility (Muir et al., 2014). Evaluating the stability of GI in sedentary older adults, who engage in activities, such as sitting, lying down or reclining with energy expenditure ≤1.5 metabolic equivalents while awake (Atkin et al., 2012; Edwardson et al., 2012), may serve as a valuable tool for assessing fall risk.
Tai Chi exercise is an effective intervention for reducing falls among older adults (Chen et al., 2021; National Council on Aging, 2023). Tai Chi movements require slow, continuous and smooth actions, which involve the continuous transformation of weight-bearing and non-weight-bearing movements and maintaining body stability. Various studies have highlighted the positive effects of Tai Chi on balance control and fall prevention in older adults (Chen et al., 2023). The present study aims to quantitatively assess the stability of GI in sedentary older adults and long-term Tai Chi exercisers by using this functional task to determine the risk level of sedentary individuals and the effectiveness of Tai Chi intervention.
Voluntary movement of GI is a means to accomplish stable walking tasks. The human body constantly adapts to natural instability triggered by variations in the supporting surface during movement. The central nervous system (CNS) employs stable and effective mechanisms to handle instability inherent in GI. The effectiveness of executing GI tasks, which refers to the output efficiency of sensory–motor system integration, is typically evaluated based on movement performance during GI, such as speed and accuracy (Bouisset and Do, 2008). The process of GI involves two skills, namely, forward propulsion and balance control, which are accompanied by posture–locomotion coupling (Mille et al., 2014). Successful initiation of gait requires two biomechanical requirements, which are generation of momentum (forward direction and towards the supporting leg) and maintenance of balance (Polcyn et al., 1998). Lifting the swing leg and taking a step forward can result in a potential sideway imbalance of the body, which can be effectively stabilised by the CNS. This task is accomplished by shifting the centre of pressure (CoP) of the anticipatory postural adjustments (APAs) towards the swing leg, moving the centre of mass (CoM) towards the supporting leg and partly through effective stepping (Winter 1995).
A few definitive quantitative studies have been conducted on the stability of GI in sedentary individuals and Tai Chi exercisers. The most commonly used indicator for quantifying dynamic stability during GI is the concept of ‘margin of stability (MoS)’ proposed by Hof et al. (Hof et al., 2005). MoS is a composite variable that considers the relationship among CoM position, velocity and support surface and has been widely applied to quantify stability during GI tasks. MoS is a measure of walking stability derived from dynamic stability theory and the human inverted pendulum model; it represents the minimum distance from a given CoM position–velocity state point to the backward imbalance boundary. Stability during GI is evaluated by calculating MoS in the medial–lateral (M-L) and anterior–posterior (A-P) directions, with the M-L side being considered a key indicator of walking stability.
This study utilises Hof’s gait stability assessment method (Hof et al., 2005; Hof, 2008) to collect biomechanical data on the kinematics and kinetics involved in the GI of older participants. The method calculates the stability of M-L and A-P directions during the double-support to single-support transition of the swing leg’s toe-off as well as at the end of the swing leg heel–strike when shifting from single to double support. The study compares the dynamic stability of sedentary and long-term regular Tai Chi practising older females during voluntary GI and evaluates the foot placement characteristics at the end of GI to explore the potential fall risk for sedentary individuals and the effectiveness of Tai Chi in preventing falls. Based on research findings, older women may be more susceptible to falls than older men (Stevens and Sogolow, 2005; Johansson et al., 2016; Yogi et al., 2018; Peng et al., 2019; Moreland et al., 2020). To minimise gender bias, this study exclusively focused on female participants. The research aims to: (1) determine differences in the dynamic stability of GI between sedentary individuals and those who engage in regular long-term Tai Chi exercise; and (2) compare foot placement strategies during stepping. The hypotheses are as follows: (1) sedentary individuals are expected to present significantly lower dynamic stability of GI than Tai Chi exercisers; and (2) both groups are assumed to exhibit distinct foot placement strategies. Results will provide evidence regarding factors contributing to fall risk in older individuals and the effects of exercise interventions.
Methods
Study sample
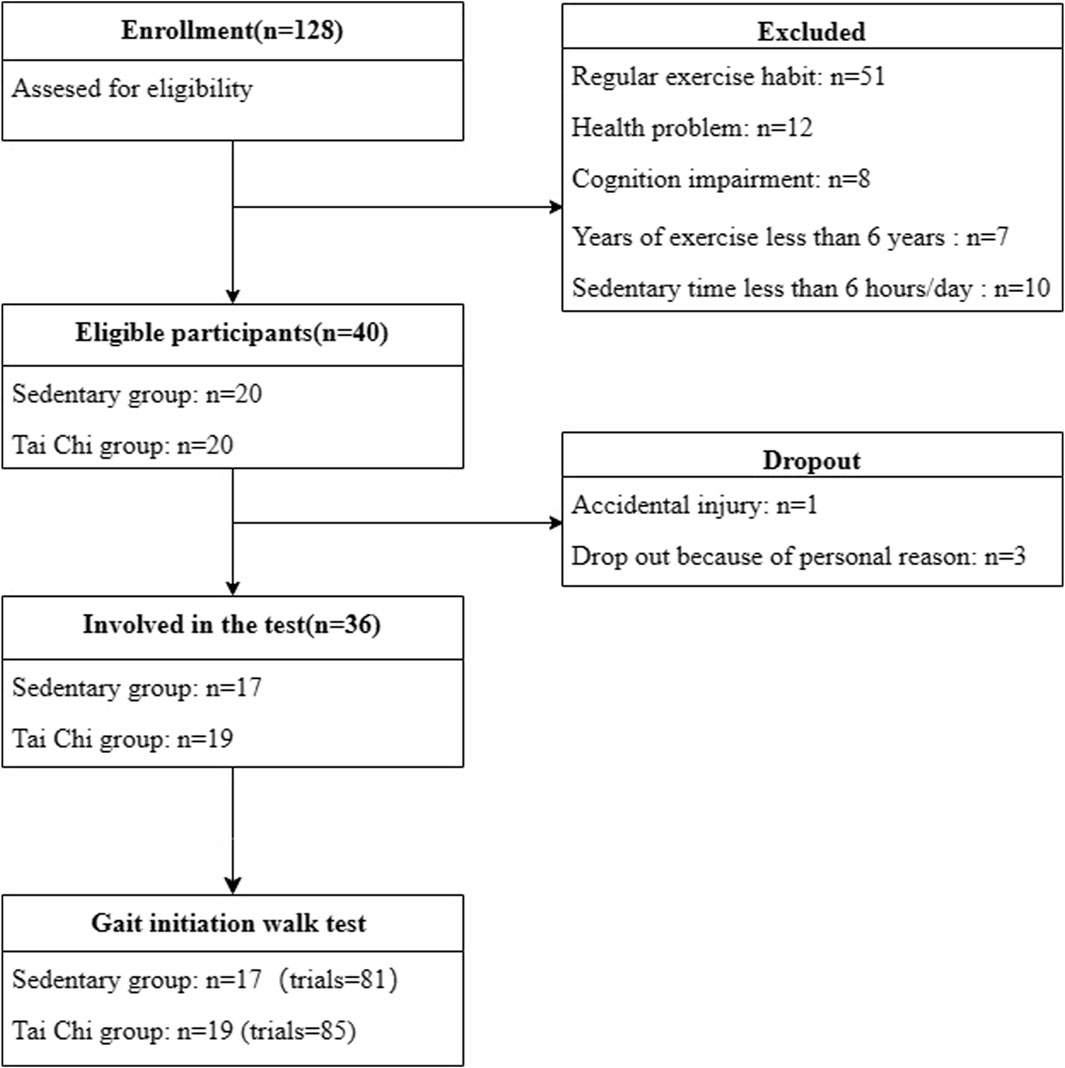
The sample size was estimated using G*power software, which determined that an effect size of 0.5 and a statistical power of 80% (α = 0.05) are necessary to detect a significant difference (Zhang et al., 2002), requiring at least 51 trials in each group. The study finally recruited 128 elderly participants, with ineligible individuals, dropouts and invalid data excluded, included 36 participants, each of them completed five trials, resulting in 166 trials, which satisfied the requirement for statistical significance.
Participants
The inclusion criteria for the participants were as follows: female, right-leg dominance; good physical health; absence of back and pelvic system issues, neuromuscular disorders or balance impairments; and normal cognitive function. The sedentary group (SG) was defined as those who reported no exercise habits and an average sedentary time greater than 6 h per day in the past 7 days, and the Tai Chi group (TC) had more than 6 years of training.
Participants with a Mini-mental State Examination (MMSE) functional score of 24, frailty, lower limb injuries or surgeries within the past 6 months, a history of falls in the previous 2 years and fatigue or poor condition prior to the experiment were excluded.
All participants were informed about the specific test procedures and signed written informed consent forms. The study was approved by Henan Sports Science and Technology Centre (Henan Anti-Doping Centre), China.
Instrumentations
Kinematic data were obtained using eight 3D near-infrared high-speed cameras (Qualisys, Sweden, model: Oqus 600) with a sampling frequency of 100 Hz. Fifty-two infrared reflective marker points (diameter of 14 mm) were attached to the participants to collect GI kinematic information. The placement method of the markers follows the Helen Hayes model. Kinetic testing was conducted using four Kistler force plates (90 cm × 60 cm ×10 cm, Switzerland, model: 9287C), with a sampling frequency of 1,000 Hz. A remote-controlled start signal lamp was self-constructed and used.
Experimental procedures
Participants were instructed to refrain from engaging in strenuous physical activities for 3 days prior to the experiment and to avoid consuming stimulating beverages, such as alcohol or coffee, which might affect the nervous system on the day before the experiment. Sufficient sleep was ensured. On the day of formal testing, participants were required to familiarize themselves with the experimental procedures and exercise them thoroughly. After the experimental preparations were completed, the participants performed a 5-min warm-up activity before proceeding to the formal testing. The starting action involved participants standing on a force plate with standardised footwear and clothing, with each foot placed on a force plate. They were instructed to stand naturally in a static position with their feet shoulder-width apart. The signal indicator is located at the endpoint, which is opposite to the walking direction of the subject 1.2 m above the horizontal plane and 6 m away from the starting position of GI.
The GI walking test was performed under the experimental condition designed in this study. The participants stood naturally on the force plate for 3–5 s and then initiated a step forward voluntarily. Trials started with the subject in quiet standing, with their feet placed in their preferred natural stance. Following a verbal cue of ‘anytime’, the subjects waited for a self-selected time interval (no less than 3 s) then initiated forward stepping at their self-chosen pace. Five valid trials were collected and reviewed online to ensure a steady-state baseline before the ‘anytime’ instruction. Trials without a period of steady-state standing were discarded and repeated.
Data of gait evaluation were analysed using Visual3D software (C-Motion, USA, v6.01.36). Kinematic and kinetic data were filtered and denoised by using a lowpass filter, with cut-off frequencies of 6 Hz for kinematics and 20 Hz for kinetics.
The GI process is divided into two phases: the APA phase and the locomotion (LOC) phase. This study focused on analysing the stability of the LOC phase. The MoS at the onset of LOC as well as the forward and lateral control stability at the end of LOC were computed.
Dynamic Stability of Gait Initiation
Margin of stability at the onset stepping of locomotion phase
Next to the position and the velocity of the CoM, we can introduce the ‘extrapolated centre of mass (XcoM)’, as shown in Eqs 1, 2, where ω0 is a constant related to stature. XcoM allows the requirements for stable walking to be formulated simply based on the inverted pendulum model of balance.
Where XcoM represents the XcoM position,
The minimum M-L margin of stability MoSML and A-P margin of stability MoSAP were computed as follows in Eqs 3, 4:
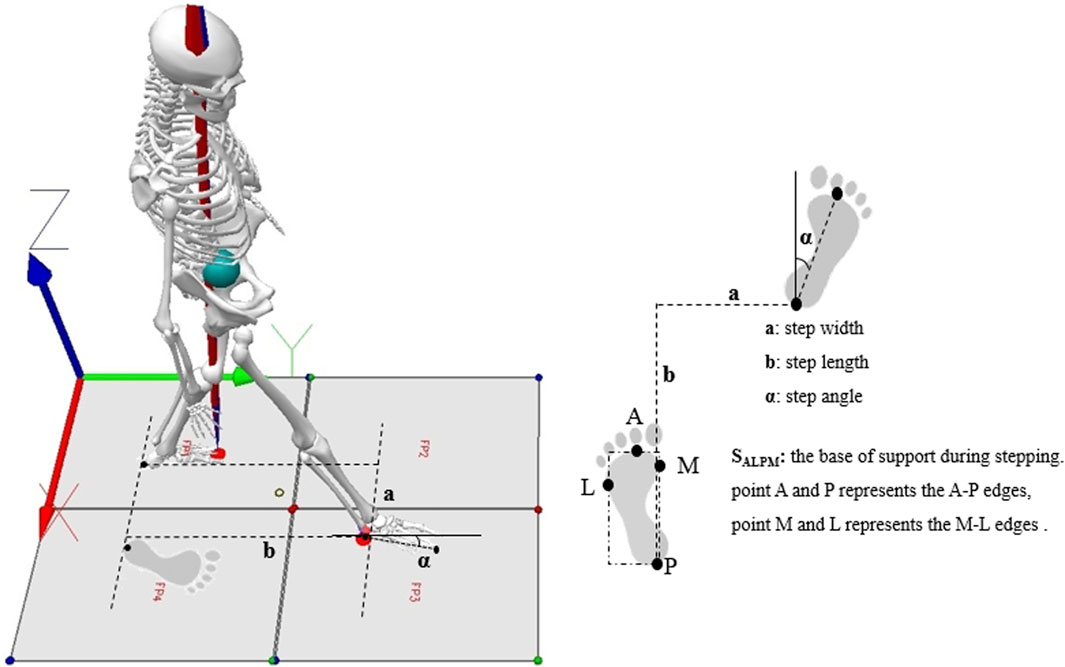
MoSML and MoSAP were calculated as the distance between XcoM and the boundaries of the base of support (BoS) during the single stance from the foot markers, namely, the fifth metatarsal–phalangeal joint for the lateral border and the medial malleolus for the medial border (Hof et al., 2005; Osada et al., 2022), as illustrated in Figure 1.
Stability control at the end of the locomotion phase
Lateral stability control
We calculated lateral stability with a constant offset control by positioning the right foot BML to the right of the XcoM, which is related to the desired step width SW in Eq. 5 (Hof, 2008).
Where
Forward stability control
The simplest stable control of CoP position could be made by positioning the CoP at a constant distance behind the ‘constant offset control’ of XcoM. The offset value BAP is represented as a constant distance. The equation is as follows in Eq. 6 (Hof, 2008).
Where
Foot placement at the end of stepping
Foot placement was determined based on step length, step width and foot inclination angle, as illustrated in Figure 1.
Statistical analysis
Statistical analysis was performed using SPSS software (version 22, SPSS Inc., Chicago, IL USA). Shapiro–Wilk test was used to verify the normal distribution of parameters; if the parameters were normally distributed, the Independent Samples t-test was applied to compare data between SG and TC groups, if the parameters were not normally distributed, the Mann–Whitney U test was applied. Effects were considered to be significant at p < 0.05.
Results
The recruitment process for participants of both surveys is illustrated in Figure 2.
Sample characteristics
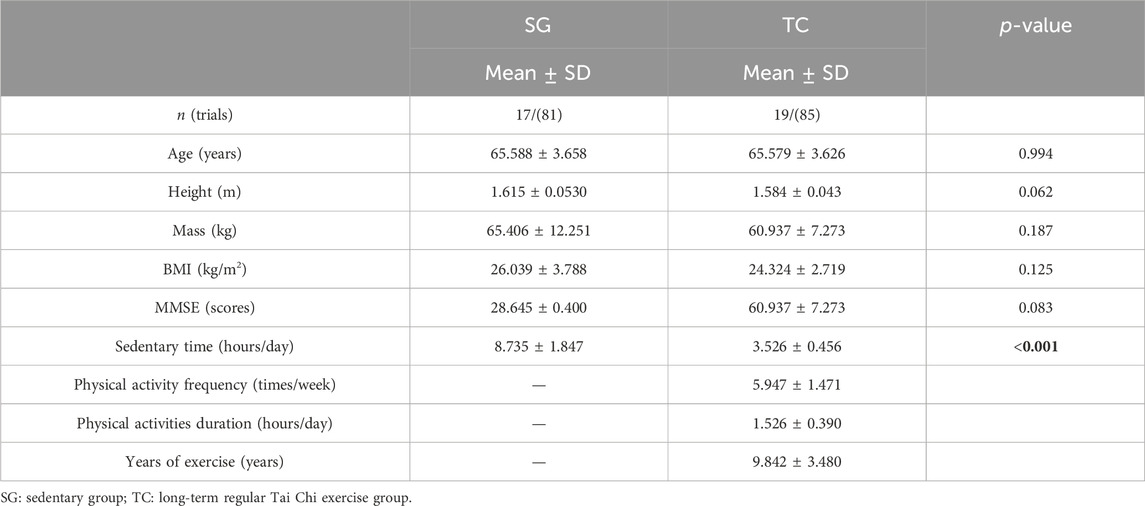
The study included 17 older females who did not engage in regular exercise (age: 65.59 ± 3.66 years; height: 1.62 ± 0.53 m; mass: 65.41 ± 12.25 kg; BMI: 26.04 ± 7.79; MMSE scores: 28.7 ± 0.40) and 19 older females who participated in long-term Tai Chi exercise (age: 65.58 ± 3.63 years; height: 1.58 ± 0.43 m; mass: 60.94 ± 7.27 kg; BMI: 24.32 ± 2.72; MMSE scores: 28.9 ± 0.49). Table 1 provides detailed information about these individuals.
Dynamic stability
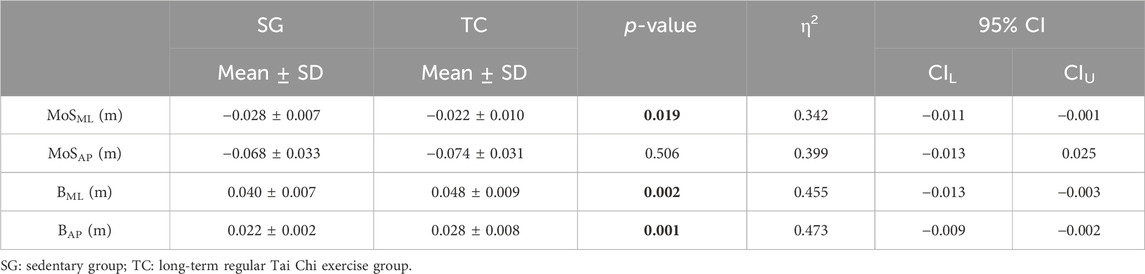
Table 2 indicates statistically significant differences in lateral stability between the SG and TC groups at the beginning of the single-support phase during the transition from double to single support during GI. The MoSML result in SG is significantly lower than that in the TC group (p = 0.19, η2 = 0.342, 95%CI: −0.011, −0.001). M-L and A-P stability also show statistically significant differences at the end of GI when the swing leg touches the ground and shifts from single to double support. The BML (p = 0.002, η2 = 0.455, 95%CI: −0.013, −0.003) and BAP (p = 0.001, η2 = 0.473, 95%CI: −0.009, −0.002) results in SG are significantly lower than those in the TC group.
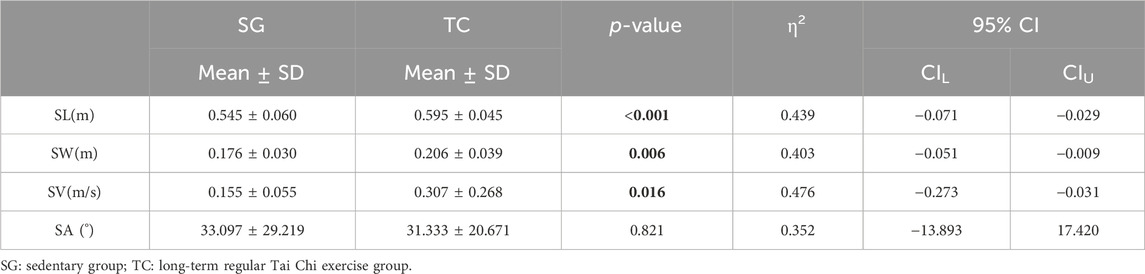
Foot placement
Table 3 shows that the TC group has a greater step length, step width and step speed than SG at the end of the GI process when the swing leg heel makes contact with the ground and transitions from single to double support. The statistical analysis reveals significant differences between the two groups, with a more pronounced difference observed in SL and SW. The foot inclination angle (SG: 33.097 ± 29.219; TC: 31.333 ± 20.671, p = 0.821, η2 = 0.352, 95% CI: 13.893, 17.42) is higher in SG than in the TC group.
Discussion
GI is a voluntary movement task that involves the transition from standing to walking. During GI, the CNS continuously compares the expected movement with the actual movement in the environment, modifying the control of movement to identify the most effective and efficient method to achieve the goal (Hadders-Algra, 2010). The stability of the body’s control changes due to changes in the support surface during GI, and the CNS uses stable and effective mechanisms to deal with the inherent instability of GI. The function of the CNS during GI is to shift the CoM in the desired direction and to determine the placement of the swing foot upon landing (Winter 1995). The efficiency of GI performance, which refers to the output efficiency of sensory–motor system integration, is typically evaluated based on GI movement characteristics, such as speed and accuracy. The present study aims to assess differences in GI performance efficiency between sedentary older women and those who have undergone long-term Tai Chi training by assessing stability at the moment of transition from double support to single support during swing leg initiation and at the moment of transition from single support to double support when the swing leg lands as well as foot placement at the completion of the GI task. The findings will provide valuable insights for the clinical assessment of gait-related neurological disorders and the evaluation of the effectiveness of rehabilitation interventions in older people.
Dynamic stability
GI involves internal self-perturbations of balance, known as endogenous ‘action equilibration’ (Bouisset and Do, 2008). MoS, derived from dynamic stability theory and the human inverted pendulum model, is a measure of walking stability by representing the shortest distance between a given CoM position–velocity state point and the backward imbalance boundary. Gait stability can be evaluated by calculating stability margins in the A-P and M-L directions, with the M-L dynamic MoS as a key indicator of walking stability.
The results show a statistically significant difference in M-L stability between SG and TC groups at the moment the swing leg is lifted off the ground during the transition from double-to single-leg support. M-L stability is an important predictor of fall risk, and the results suggest that sedentary older women are potentially at risk of falling. Nakano et al. also suggested that age-related changes in M-L balance control may increase the risk of lateral falls during GI (Nakano et al., 2016). Breniere and Do. (1986) reported that steady-state gait conditions are achieved at the end of the first step when walking at a habitual speed. The goal of GI is to place participants under steady-state gait conditions during the first step. At the end of the first step, the M-L and A-P stability in SG are significantly lower than those in TC, indicating that Tai Chi significantly improves the stepping gait stability during GI. At the onset of GI, sufficient APAs will ensure that the CoM is repositioned over the new support base (standing/supporting leg), preventing the body from tilting towards the swing leg after transitioning from bipedal to unipedal stance. If APAs fail to effectively reposition the CoM onto the new support surface, then walkers will need to rely on CPAs to reduce the effect of this instability, typically by taking more side steps with the stepping foot to increase the range of the support surface (Zettel et al., 2002). Some adaptation effects are consistent with the role of motor predictions in coupling posture and movement. The CNS anticipates the direction and magnitude of the initial lateral body movement, corresponding to the expected position of the M-L foot placement. Foot placement is adapted by altering posture and movement before stepping to ensure stability during stepping. These adaptations during movement may directly alter stepping performance. Disruptions in frontal plane postural control prompt movement adjustments to maintain stability and efficiency (e.g., maintaining step length) during the first step (Mille et al., 2007).
This study compares the displacement results of the CoP during GI at different angles (45° left anterior, 45° right anterior and 90° right lateral). A 16-week Tai Chi intervention significantly increases the displacement and speed of lateral steps in sedentary older adults. Tai Chi may improve dynamic postural control during the initial phase of GI in older adults by altering the movement characteristics of the CoP. Another study revealed that a 12-week Tai Chi exercise can improve posture control on unstable platforms and reduce the risk of falls in older individuals with sarcopenia (Huang et al., 2023). However, a previous research that compared the minimum postural sway ability of older adults suggested that a 15-week Tai Chi intervention did not improve measures of platform postural stability (Wolf et al., 1997). Our study includes stability calculations and reports that during the end stage of step advancement, the M-L and A-P stability of older women in the TC is significantly higher than that in sedentary older adults. Hence, Tai Chi exercise has a positive effect on improving the stability of GI in older adults. The different results of Tai Chi in improving postural stability may be due to the specific movement characteristics of Tai Chi, such as stable shifts in the centre of gravity (CoG) and slow, smooth transitions in step movements, which may manifest stability in controlling step movements.
Foot placement
A potential method used to improve postural stability during GI is modifying the initial foot position (IFP). The human body achieves safe and efficient step advancement by adjusting the step length and position of the swing leg foot at ground contact. Considering the significance of appropriate IFP for GI and recovery response, the observed changes in step length during the first step of older fallers may serve as an important predictor of posture-related problems (Azizah Mbourou et al., 2003). During GI, coarse balance control is achieved through the placement of the swing leg’s foot (Jian et al., 1993). This study found statistically significant differences in the step length, width and speed of older females in the SG and TC group, with SG exhibiting significantly shorter step length and width. These findings align with previous research, which indicated that step length and step speed significantly decrease with age during GI (Muir et al., 2014) and that older fallers demonstrate significantly shorter first steps (Azizah Mbourou et al., 2003). Additionally, older adults can modulate their step width to maintain dynamic balance in the M-L direction (Nakano et al., 2016). Muir et al. (2014) compared age-related changes in the first four steps of gait, including the GI phase, for three age groups (20–25 years, 65–79 years and 80–91 years) walking at self-selected speeds. The results showed significant decreases in step speed and length across age groups. Higher variability in step length and step width may reflect increased foot placement errors and/or decreased CoG control among older adults. Healthy individuals aged 80–91 years walked at a slower pace with shorter steps. Furthermore, older fallers had significantly shorter first steps during GI and significantly longer double support time (Azizah Mbourou et al., 2003). Our results further confirm that older adults may utilise their foot placement at touchdown to regulate stable control at the end of the stance phase. A faster gait requires longer anticipation time and shorter execution time (Brenière et al., 1987). No statistically significant differences were observed in the foot inclination angle between the two groups. Inclination of the foot to the outer side (IFP) may be a feasible option to increase ankle muscle activation and improve age-related decline in postural stability (Jeon et al., 2021). Reinmann et al. (Reimann et al., 2017) proposed that foot placement and ankle lateral strategies may be two independent mechanisms that are coupled and coordinated in time to compensate for unstable M-L APAs and stiffened stance leg in the frontal plane to maintain body sagittal stability (Van Dieёn et al., 2008). The foot placement position is actively regulated by the CNS to maintain lateral balance (Bauby and Kuo, 2000; Donelan et al., 2004). The human body maintains gait stability by coordinating the M-L foot placement position and the control of the CoM (O’Connor and Kuo, 2009). The CNS anticipates the initial lateral displacement of the body and adjusts the foot placement accordingly to ensure its alignment with the expected position. The foot position is adapted by altering the pre-step posture to ensure stability during foot strikes (Collins and Kuo, 2013). Even if the foot placement position is slightly inappropriate at foot strike, it can still be compensated by adjusting the M-L position of the CoP, which is known as the ‘ankle lateral strategy’ (Hof et al., 2007). Changes in the length of the first step may be an important predictor of postural problems in older adults considering the importance of appropriate foot placement for GI and recovery responses.
Strengths and limitations
This study compared the GI stability characteristics and foot placement features between two representative older groups, namely, sedentary older women and older women with long-term regular Tai Chi exercise. The results provide a reference for future studies on GI stability in specific population subgroups. However, this study did not investigate the coordination of limb spatial positioning and ground reaction forces. In future research, we will consider the coordination of GI and potential differences in force control that may lead to an increased risk of injury. Previous studies indicated that gender is a major risk factor for falls, with older women being more prone to falls. The present work only included older women participants and did not further categorize them by age group. Further studies will consider additional age groups and physical activity groups for research purposes.
Conclusion
This study quantitatively compared and analysed the dynamic stability and foot placement characteristics of sedentary older women and older women with long-term regular Tai Chi exercise. The findings revealed that long-term regular Tai Chi exercise significantly improved the dynamic stability at the swing leg toe-off moment in M-L directions and at the heel–strike moment in the M-L and A-P directions, moreover, Tai Chi exercisers showed significantly higher step length, step width and step velocity than sedentary older women during GI. The results further confirm the negative effect of sedentary behaviour on stability control among older adults as well as the positive effects of Tai Chi on improving gait stability control and reducing fall risk.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Academic Ethics Committee of Henan Sports Science and Technology Centre (Henan Anti-Doping Centre), China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YC: Writing–original draft, Writing–review and editing, Funding acquisition. CJ: Formal Analysis, Investigation, Writing–review and editing. HT: Resources, Writing–review and editing. JY: Conceptualization, Formal Analysis, Writing–review and editing. YW: Formal Analysis, Investigation, Writing–review and editing. SC: Formal Analysis, Investigation, Writing–review and editing. WM: Funding acquisition, Resources, Writing–review and editing. SZ: Conceptualization, Methodology, Writing–review and editing. XW: Funding acquisition, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Social Science Fund: Research on Fall Risk Assessment and Exercise Intervention Strategies for the older in China (Project No. 23BTY120); and the Nation Key Technologies Research and Development Program: Older People Disability Classification and Assessment Standard System and Early Warning Model Research, Research on older Disability Prevention and Intervention Management Network and Technology in China (Project No. 2020YFC2008501); and the Henan Provincial Science and Technology Research Project: Neuromuscular Control of Balance-Corrected Postural Responses to Sudden Perturbations in Older People (Project No. 2020YFC2008501). The funders had no role in the study design, data collection and analysis, decision to publish or preparation of this paper.
Acknowledgments
The authors thank the participants in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
GI, gait initiation; SG, sedentary group; TC, Tai Chi group; CoM, centre of mass; CoP, centre of pressure; CoG, centre of gravity; APAs, anticipatory postural adjustments; CPAs, compensatory postural adjustments; BMI, body mass index; MMSE, Mini-mental State Examination; BoS, base of support; MoS, margin of stability; M-L, medio-lateral; A-P, anterior-posterior; CNS, central nervous system; XcoM, extrapolated center of mass; SL, step length; SW, step width; SV, step velocity; SA, step inclination angle; IFP, initial foot position.
References
Atkin, A. J., Gorely, T., Clemes, S. A., Yates, T., Edwardson, C., Brage, S., et al. (2012). Methods of measurement in epidemiology: sedentary behaviour. Int. J. Epidemiol. 41, 1460–1471. doi:10.1093/ije/dys118
Azizah Mbourou, G., Lajoie, Y., and Teasdale, N. (2003). Step length variability at gait initiation in elderly fallers and non-fallers, and young adults. Gerontology 49, 21–26. doi:10.1159/000066506
Bauby, C. E., and Kuo, A. D. (2000). Active control of lateral balance in human walking. J. biomechanics 33, 1433–1440. doi:10.1016/s0021-9290(00)00101-9
Bouisset, S., and Do, M.-C. (2008). Posture, dynamic stability, and voluntary movement. Neurophysiol. Clinique/Clinical Neurophysiol. 38, 345–362. doi:10.1016/j.neucli.2008.10.001
Boyer, K. A., Hayes, K. L., Umberger, B. R., Adamczyk, P. G., Bean, J. F., Brach, J. S., et al. (2023). Age-related changes in gait biomechanics and their impact on the metabolic cost of walking: report from a national institute on aging workshop. Exp. Gerontol. 112102. doi:10.1016/j.exger.2023.112102
Brach, J. S., and VanSwearingen, J. M. (2013). Interventions to improve walking in older adults. Curr. Transl. geriatrics Exp. gerontology Rep. 2, 230–238. doi:10.1007/s13670-013-0059-0
Brenière, Y., Cuong Do, M., and Bouisset, S. (1987). Are dynamic phenomena prior to stepping essential to walking? J. Mot. Behav. 19, 62–76. doi:10.1080/00222895.1987.10735400
Brenière, Y., and Do, M. (1986). When and how does steady state gait movement induced from upright posture begin? J. biomechanics 19, 1035–1040. doi:10.1016/0021-9290(86)90120-x
Centers for Disease Control and Prevention (2023a). Centers for disease control and prevention. Available at: https://www.cdc.gov/falls/index.html.
Centers for Disease Control and Prevention (2023b). Common injuries as we age. Available at: https://www.cdc.gov/stillgoingstrong/about/common-injuries-as-we-age.html.
Chen, W., Li, M., Li, H., Lin, Y., and Feng, Z. (2023). Tai Chi for fall prevention and balance improvement in older adults: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health 11, 1236050. doi:10.3389/fpubh.2023.1236050
Chen, X.-P., Wang, L.-J., Chang, X.-Q., Wang, K., Wang, H.-F., Ni, M., et al. (2021). Tai chi and yoga for improving balance on one leg: a neuroimaging and biomechanics study. Front. Neurol. 12, 746599. doi:10.3389/fneur.2021.746599
Collins, S. H., and Kuo, A. D. (2013). Two independent contributions to step variability during over-ground human walking. PloS one 8, e73597. doi:10.1371/journal.pone.0073597
U.S. Preventive Services (2018). Falls prevention in community-dwelling older adults. Interventions. Available at: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/falls-prevention-in-older-adults-interventions.
Donelan, J. M., Shipman, D. W., Kram, R., and Kuo, A. D. (2004). Mechanical and metabolic requirements for active lateral stabilization in human walking. J. biomechanics 37, 827–835. doi:10.1016/j.jbiomech.2003.06.002
Edwardson, C. L., Gorely, T., Davies, M. J., Gray, L. J., Khunti, K., Wilmot, E. G., et al. (2012). Association of sedentary behaviour with metabolic syndrome: a meta-analysis. PloS one 7, e34916. doi:10.1371/journal.pone.0034916
Haddad, Y. K., Bergen, G., and Florence, C. S. (2019). Estimating the economic burden related to older adult falls by state. J. Public Health Manag. Pract. 25, E17–E24. doi:10.1097/phh.0000000000000816
Hadders-Algra, M. (2010). Variation and variability: key words in human motor development. Phys. Ther. 90, 1823–1837. doi:10.2522/ptj.20100006
Hartmann, Y., Liu, H., and Schultz, T. (2023). “High-level features for human activity recognition and modeling,” in Biomedical engineering systems and Technologies. BIOSTEC 2022. Communications in computer and information science. Editor A. C. A. Roque (Cham: Springer), 1814, 141–163. doi:10.1007/978-3-031-38854-5_8
Hof, A. L. (2008). The ‘extrapolated center of mass’ concept suggests a simple control of balance in walking. Hum. Mov. Sci. 27, 112–125. doi:10.1016/j.humov.2007.08.003
Hof, A. L., Gazendam, M., and Sinke, W. (2005). The condition for dynamic stability. J. biomechanics 38, 1–8. doi:10.1016/j.jbiomech.2004.03.025
Hof, A. L., van Bockel, R. M., Schoppen, T., and Postema, K. (2007). Control of lateral balance in walking: experimental findings in normal subjects and above-knee amputees. Gait posture 25, 250–258. doi:10.1016/j.gaitpost.2006.04.013
Huang, D., Ke, X., Jiang, C., Song, W., Feng, J., Zhou, H., et al. (2023). Effects of 12 weeks of tai chi on neuromuscular responses and postural control in elderly patients with sarcopenia: a randomized controlled trial. Front. Neurology 14, 1167957. doi:10.3389/fneur.2023.1167957
Jeon, W., Griffin, L., and Hsiao, H. Y. (2021). Effects of initial foot position on postural responses to lateral standing surface perturbations in younger and older adults. Gait posture 90, 449–456. doi:10.1016/j.gaitpost.2021.09.193
Jian, Y., Winter, D. A., Ishac, M. G., and Gilchrist, L. (1993). Trajectory of the body cog and cop during initiation and termination of gait. Gait posture 1, 9–22. doi:10.1016/0966-6362(93)90038-3
Johansson, J., Nordström, A., and Nordström, P. (2016). Greater fall risk in elderly women than in men is associated with increased gait variability during multitasking. J. Am. Med. Dir. Assoc. 17, 535–540. doi:10.1016/j.jamda.2016.02.009
Kakara, R., Bergen, G., Burns, E., and Stevens, M. (2023). Nonfatal and fatal falls among adults aged 65 years—United States, 2020–2021. MMWR. Morb. Mortal. Wkly. Rep. 72, 938–943. doi:10.15585/mmwr.mm7235a1
Lee, J. (2020). The association between physical activity and risk of falling in older adults: a systematic review and meta-analysis of prospective cohort studies. Geriatr. Nurs. 41, 747–753. doi:10.1016/j.gerinurse.2020.05.005
Mille, M.-L., Johnson Hilliard, M., Martinez, K. M., Simuni, T., and Rogers, M. W. (2007). Acute effects of a lateral postural assist on voluntary step initiation in patients with Parkinson’s disease. Mov. Disord. 22, 20–27. doi:10.1002/mds.21139
Mille, M.-L., Simoneau, M., and Rogers, M. W. (2014). Postural dependence of human locomotion during gait initiation. J. Neurophysiology 112, 3095–3103. doi:10.1152/jn.00436.2014
Ministry of Health (2008). Main findings of the fourth national health service survey. Available at: https://www.gov.cn/gzdt/2009-02/27/content_1245006.htm.
Moreland, B., Kakara, R., and Henry, A. (2020). Trends in nonfatal falls and fall-related injuries among adults aged 65 years—United States, 2012–2018. Morb. Mortal. Wkly. Rep. 69, 875–881. doi:10.15585/mmwr.mm6927a5
Muir, B., Rietdyk, S., and Haddad, J. M. (2014). Gait initiation: the first four steps in adults aged 20–25 years, 65–79 years, and 80–91 years. Gait posture 39, 490–494. doi:10.1016/j.gaitpost.2013.08.037
Nakano, W., Fukaya, T., Kobayashi, S., and Ohashi, Y. (2016). Age effects on the control of dynamic balance during step adjustments under temporal constraints. Hum. Mov. Sci. 47, 29–37. doi:10.1016/j.humov.2016.01.015
National Council on Aging (2023). Evidence-based falls prevention Programs. Available at: https://www.ncoa.org/article/evidence-based-falls-prevention-programs.
O’Connor, S. M., and Kuo, A. D. (2009). Direction-dependent control of balance during walking and standing. J. neurophysiology 102, 1411–1419. doi:10.1152/jn.00131.2009
Osada, Y., Motojima, N., Kobayashi, Y., and Yamamoto, S. (2022). Differences in mediolateral dynamic stability during gait initiation according to whether the non-paretic or paretic leg is used as the leading limb. Plos one 17, e0267577. doi:10.1371/journal.pone.0267577
Peng, K., Tian, M., Andersen, M., Zhang, J., Liu, Y., Wang, Q., et al. (2019). Incidence, risk factors and economic burden of fall-related injuries in older Chinese people: a systematic review. Inj. Prev. 25, 4–12. doi:10.1136/injuryprev-2018-042982
Polcyn, A. F., Lipsitz, L. A., Kerrigan, D. C., and Collins, J. J. (1998). Age-related changes in the initiation of gait: degradation of central mechanisms for momentum generation. Archives Phys. Med. rehabilitation 79, 1582–1589. doi:10.1016/s0003-9993(98)90425-7
Reimann, H., Fettrow, T. D., Thompson, E. D., Agada, P., McFadyen, B. J., and Jeka, J. J. (2017). Complementary mechanisms for upright balance during walking. PloS one 12, e0172215. doi:10.1371/journal.pone.0172215
Robinovitch, S. N., Feldman, F., Yang, Y., Schonnop, R., Leung, P. M., Sarraf, T., et al. (2013). Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. lancet 381, 47–54. doi:10.1016/s0140-6736(12)61263-x
Stevens, J. A., and Sogolow, E. D. (2005). Gender differences for non-fatal unintentional fall related injuries among older adults. Inj. Prev. 11, 115–119. doi:10.1136/ip.2004.005835
Talbot, L. A., Musiol, R. J., Witham, E. K., and Metter, E. J. (2005). Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC public health 5, 86–89. doi:10.1186/1471-2458-5-86
Vala, H., Padnani, R., Dave, S., et al. (2023). A study to find out the correlation between physical activity, reaction time, and fall risk in the elderly. Int. J. Health Sci. Res. 13, 43–48. doi:10.52403/ijhsr.20230506
Van Dieёn, J. H., Spanjaard, M., Könemann, R., Bron, L., and Pijnappels, M. (2008). Mechanics of toe and heel landing in stepping down in ongoing gait. J. biomechanics 41, 2417–2421. doi:10.1016/j.jbiomech.2008.05.022
Wang, M., Wu, F., Callisaya, M. L., Jones, G., and Winzenberg, T. M. (2023). Longitudinal associations of objectively measured physical activity and sedentary time with leg muscle strength, balance and falls in middle-aged women. Eur. J. sport Sci. 23, 2240–2250. doi:10.1080/17461391.2023.2222096
Winter, D. A. (1995). Human balance and posture control during standing and walking. Gait posture 3, 193–214. doi:10.1016/0966-6362(96)82849-9
Wolf, S. L., Barnhart, H. X., Ellison, G. L., Coogler, C. E., and Group, A. F. (1997). The effect of tai chi quan and computerized balance training on postural stability in older subjects. Phys. Ther. 77, 371–381. doi:10.1093/ptj/77.4.371
Xue, T., and Liu, H. (2021). “Hidden markov model and its application in human activity recognition and fall detection: a review,” in International conference in communications, signal processing, and systems (Germany: Springer), 863–869.
Yang, F., and Liu, W. (2020). Biomechanical mechanism of tai-chi gait for preventing falls: a pilot study. J. biomechanics 105, 109769. doi:10.1016/j.jbiomech.2020.109769
Yogi, R. R., Sammy, I., Paul, J. F., Nunes, P., Robertson, P., and Ramcharitar Maharaj, V. (2018). Falls in older people: comparing older and younger fallers in a developing country. Eur. J. trauma Emerg. Surg. 44, 567–571. doi:10.1007/s00068-017-0818-2
Zettel, J. L., McIlroy, W. E., and Maki, B. E. (2002). Environmental constraints on foot trajectory reveal the capacity for modulation of anticipatory postural adjustments during rapid triggered stepping reactions. Exp. brain Res. 146, 38–47. doi:10.1007/s00221-002-1150-5
Keywords: Tai Chi, gait initiation, dynamic stability control, margin of stability, foot placement strategy, older women
Citation: Chen Y, Jin C, Tang H, Yu J, Wang Y, Chen S, Miao W, Zhang S and Wang X (2024) Effects of sedentary behaviour and long-term regular Tai Chi exercise on dynamic stability control during gait initiation in older women. Front. Bioeng. Biotechnol. 12:1353270. doi: 10.3389/fbioe.2024.1353270
Received: 10 December 2023; Accepted: 11 April 2024;
Published: 09 May 2024.
Edited by:
Cristian Romagnoli, Università telematica San Raffaele, ItalyReviewed by:
Hui Liu, University of Bremen, GermanyZhi-Wei Yan, Shenyang Sport University, China
Wei Sun, Shandong Sport University, China
Wenxin Niu, Tongji University, China
Copyright © 2024 Chen, Jin, Tang, Yu, Wang, Chen, Miao, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuxia Chen, MjAxMTUxNjAyNUBzdXMuZWR1LmNu; Xiangdong Wang, d2FuZ3hpYW5nZG9uZ0BqbXUuZWR1LmNu
†These authors share first authorship
 Yuxia Chen
Yuxia Chen Chunxia Jin3†
Chunxia Jin3† Jinglun Yu
Jinglun Yu Xiangdong Wang
Xiangdong Wang