
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Bioeng. Biotechnol., 05 January 2024
Sec. Biomechanics
Volume 11 - 2023 | https://doi.org/10.3389/fbioe.2023.1289290
This article is part of the Research TopicExperimental and Computational Approaches in Meniscus Mechanics and MechanobiologyView all 6 articles
 M. Severyns1,2
M. Severyns1,2 F. Zot1
F. Zot1 G. Harika-Germaneau3
G. Harika-Germaneau3 A. Germaneau1*
A. Germaneau1* G. Herpe4
G. Herpe4 M. Naudin4
M. Naudin4 V. Valle1
V. Valle1 J. Danion5
J. Danion5 T. Vendeuvre1,6
T. Vendeuvre1,6Introduction: The existing body of literature on the biomechanical implications of ramp lesions is limited, leaving a significant gap in our understanding of how these lesions impact joint kinematics and loading in the medial compartment. This cadaveric biomechanical study aims to address this gap by employing an innovative Digital Volume Correlation (DVC) method, utilizing 7 Tesla Magnetic Resonance Imaging (MRI) images under various loading conditions. The primary objective is to conduct a comprehensive comparison of medial meniscal mobility between native knees and knees affected by grade 4 ramp lesions. By focusing on the intricate dynamics of meniscal mobility and extrusion, this work seeks to contribute valuable insights into the biomechanical consequences of medial meniscus ramp lesions.
Materials and methods: An initial set of 7T MRI imaging sessions was conducted on two intact native knees, applying load values up to 1500N. Subsequently, a second series of images was captured on these identical knees, with the same loads applied, following the creation through arthroscopy of medial meniscus ramp lesions. The application of DVC enabled the precise determination of the three components of displacement and spatial variations in the medial menisci, both with and without ramp lesions.
Results: The measured directional displacements between native knees and injured knees indicate that, following the application of axial compression load, menisci exhibit increased extrusion and posterior mobility as observed through DVC.
Discussion: Injuries associated with Subtype 4 medial meniscus ramp lesions appear to elevate meniscal extrusion and posterior mobility during axial compression in the anterior cruciate ligament of intact knees. Following these preliminary results, we plan to expand our experimental approach to encompass individuals undergoing weight-bearing MRI. This expansion aims to identify meniscocapsular and/or meniscotibial insufficiency or rupture in patients, enabling us to proactively reduce the risk of osteoarthritic progression.
In the context of anterior cruciate ligament (ACL) reconstruction, medial meniscus ramp lesions (RL) and lateral meniscus posterior ramp lesions are prevalent, accounting for over one-third of cases in both primary and revision surgeries (Magosch et al., 2021). Specifically, medial meniscus RLs (Figure 1) are frequently observed traumatic injuries, with a prevalence rate of 21.9% (ranging from 9.0% to 41.7%) at the time of ACL reconstruction (Kunze et al., 2021a; Brophy et al., 2022). They are defined as a distinct category of injuries occurring within the posterior horn of the medial meniscus and its meniscocapsular attachments (Thaunat et al., 2021).
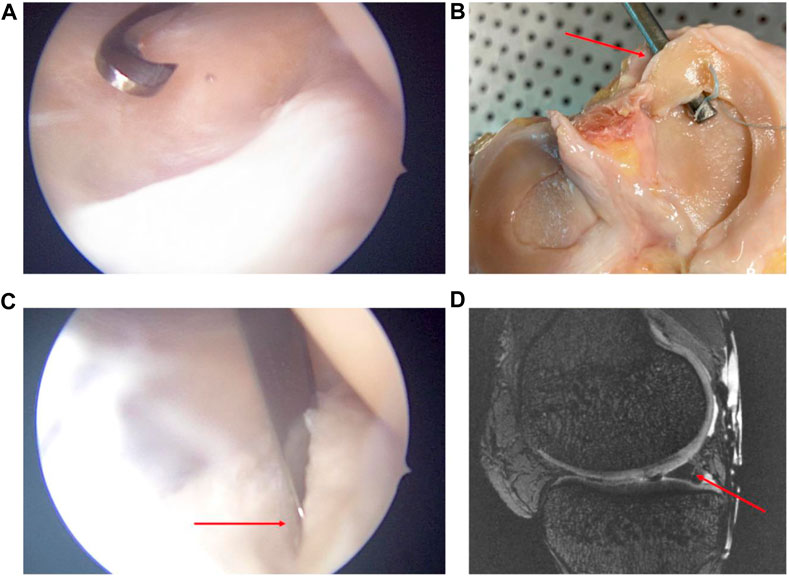
FIGURE 1. Arthroscopic views (A,B) of subtype 4 medial meniscus RL creation by a posteromedial approach. Open view of the knee and its meniscal RL injury after experimentation (C). MRI sagittal view in sequence T2 DESS of the subtype 4 RL injury (D). Red arrows show the subtype 4 RL.
Among the various types of RL, meniscocapsular junction tears, classified as type 1, are the most common, followed by type 4 lesions, which involve a complete tear in the red zone of the meniscus (Thaunat et al., 2021). This underscores the need to understand and address these specific types of meniscal injuries in the context of ACL reconstruction, as they play a crucial role in the overall stability and functionality of the knee joint. Addressing these lesions effectively is essential for optimizing patient outcomes and preventing the long-term complications associated with ACL reconstruction.
At present, understanding of the biomechanical behavior of meniscus is at the forefront of orthopedic discussions (Kunze et al., 2021b; Ollivier et al., 2022). Meniscocapsular and meniscotibial lesions of the posterior horn of the medial meniscus increase anterior tibial translation, internal and external rotation, and pivot shift in ACL-deficient knees (Ahn et al., 2011; Engebretsen et al., 2012; Peltier et al., 2015; Stephen et al., 2016; DePhillipo et al., 2018; Mouton et al., 2020). However, the available literature discussing the biomechanical consequences of RL remains limited. It is not clear whether these lesions affect joint kinematics and loading in the medial compartment (Chahla et al., 2016; Seil, 2018). Recently, Krych et al. (2017) and Mariani et al. (2022) showed that meniscal extrusion was due not only to root lesions but also to meniscotibial ligament (MTL) injuries. Although meniscal extrusion is often the consequence of hyper-pressure in the medial femorotibial compartment, it could also be the cause in different cases, one of them being RL.
Magnetic Resonance Imaging (MRI) plays a pivotal role in investigating meniscal injuries, particularly RL. Its ability to provide detailed, non-invasive, and precise imaging significantly contributes to early detection, appropriate treatment planning, and successful outcomes for patients dealing with this specific meniscal injury. From a biomechanical point of view, Digital Volume Correlation (DVC) is currently used to determine the three components of displacement and spatial variations of a material or structure from volume images (Bay et al., 1999; Buljac et al., 2018; Disney et al., 2018).
The combination of MRI and DVC ensures powerful synergy in medical imaging and biomechanical analysis. While MRI provides detailed and high-resolution images of internal structures, capturing intricate anatomical information, DVC is a sophisticated image analysis technique used to quantify deformation and strain in complex structures. The integration of MRI with DVC enhances biomechanical studies by correlating structural information with mechanical behavior. This correlation is invaluable in fields such as orthopedics, where understanding the mechanical properties of tissues is crucial for the development of effective treatment strategies and injury prevention programs.
This biomechanical work concerned a case study, of which the objective was to compare medial meniscal mobility between native knees and knees with grade 4 RL by a DVC method using 7 Tesla MRI at different loadings. The hypothesis of this study is that medial meniscus RL increases meniscal mobility and extrusion.
This experimental study was conducted on two cadaveric knees that had a Normo-axial morphotype with a meniscal (and cartilaginous state deemed intact during the 7 Tesla MRI (7T MRI) examination. Specimen preparations were carried out at the Anatomy Laboratory of the University of Poitiers (DC-2019-3704 Université de Poitiers). The epidemiological data showed a 63-year-old man (73 kg, named Knee 1) and an 81-year-old woman (79 kg, named Knee 2) with no osteoarticular history and whose CT scan measurements of HKA angle were 178.9° (leg length: 123.4 cm) and 177.8° (leg length: 127.7 cm) respectively. The knees were then disarticulated below the hip and above the ankle and dissected, preserving the entire capsule and peripheral ligaments without opening the knee joint. Proximal and distal fixations of rigid polyurethane resin were made in order to facilitate fixation of the anatomical parts on an MRI-compatible loading bench without ferromagnetic components and designed specifically for this series of experiments (Figure 2). The knee was positioned in the loading device in the sagittal direction, aligning the loading axis with the orientation of the MRI tube. The loading bench could impose compression loading up to 1500N. Imposed load ability was preliminarily calibrated and controlled during experiments by a specific homemade hydraulic sensor. Biomechanical experiments were conducted in accordance with established guidelines for in vitro studies (Wilke et al., 1998). Cadaveric knees from fresh and non-formalin-fixed specimens were cryopreserved after the primary dissection phase. Before each experiment, the thawing protocol consisted of placing the cadaveric segments at room temperature for 48 h in order to optimize the elasticity/stiffness relationship and to get closer to the physiological conditions found in living patients.
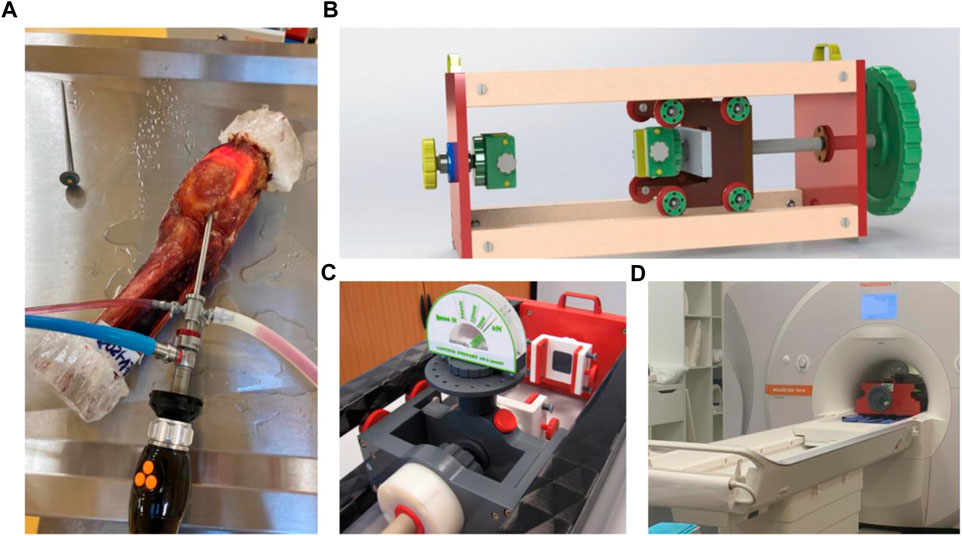
FIGURE 2. Anatomical view of a knee segment with its proximal and distal fixations of rigid polyurethane resin (A). MRI-compatible loading bench, (B) pressure sensor, (C) in situ loading setup in the 7T MRI device (D).
Images were acquired using a 7-Tesla scanner (Magnetom Terra, Siemens Healthineers, Erlangen, Germany) with a dedicated Transmit/Receive 28-channel knee coil (QED, Mayfield Village, OH, United States). Anatomical images were acquired using 3D T2 DESS 0.35 mm isotropic (TR 8ms, TE 2.48 ms, slice 0.35 mm, 464 × 464 matrix size, FA 24°, FOVr 164mm, FOVp 72.4%, 1 Nex, PAT 2). An initial series of 7T MRI imaging sessions were conducted on native knees under axial loads of 750N and 1500N, equivalent to one to two times the body weight load. Subsequently, a second set of images was captured on the same knees, employing the same loads, following the creation of grade 4 medial meniscus RL (Thaunat et al., 2021) using a posteromedial instrumental approach under arthroscopy (Figure 1).
To measure displacement fields through DVC, a sub-volume of voxels (D) is defined at each voxel in the initial image. The position of each sub-volume is subsequently determined by assessing the degree of similarity within the initial image. To achieve this objective, a correlation sub-volume is characterized by the voxel values denoted as
The overlay of constrained and unconstrained MRI images was carried out through semi-automated tibial registration of the image sequences using 3DSlicer software (Version 4.11, Kitware, France). Manual segmentation of the medial meniscus was performed by an experienced surgeon with expertise in medical image analysis, utilizing the first MRI scan to extract the relevant meniscal area. This singular segmentation aimed to delineate the specific region of interest to be analyzed through the DVC process. Given the stationary nature of the knee bones, meticulous image registrations were conducted between steps, referencing the bone structures. This approach ensured precise alignment, facilitating accurate measurements in the DVC computation area associated with the meniscus.
The displacement fields were analyzed in three dimensions. Observation of displacements along the X and Y directions facilitated analysis of anteroposterior and lateromedial migration of the meniscus after axial compression, with the knee positioned in full extension (Figure 3). The measurement uncertainty provided by the DVC process for these MRI data was assessed at 0.05 voxel.
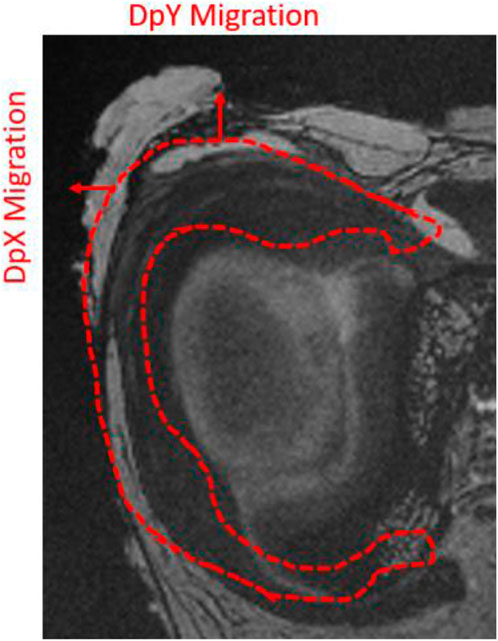
FIGURE 3. Illustration of the orientation of the displacement fields analyzed in DVC on a coronal MRI slice of a right cadaveric knee.
The red contour in Figure 3 illustrates meniscus migration during loading. The directional displacements of the medial meniscus were measured by DVC. Figures 4–7 show the directional displacement fields obtained by DVC after the application of 0N, 750N, and 1500N of axial load.
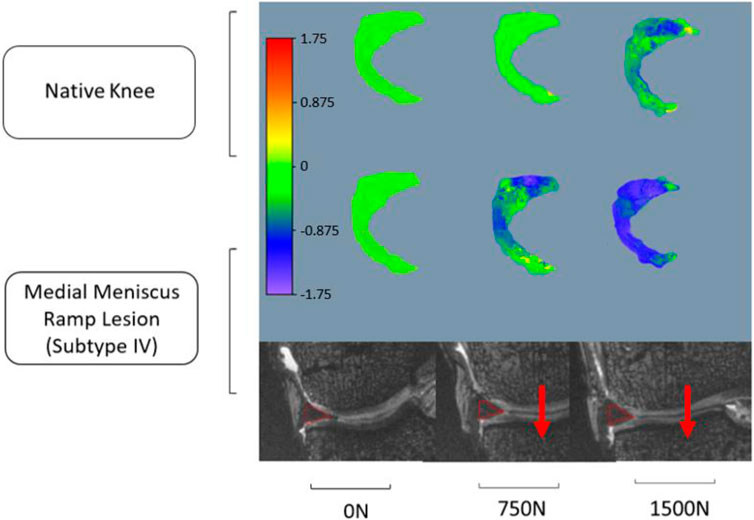
FIGURE 4. Observation of the displacement fields (in mm) after DVC assessment for knee 1 according to the lateromedial direction (X).
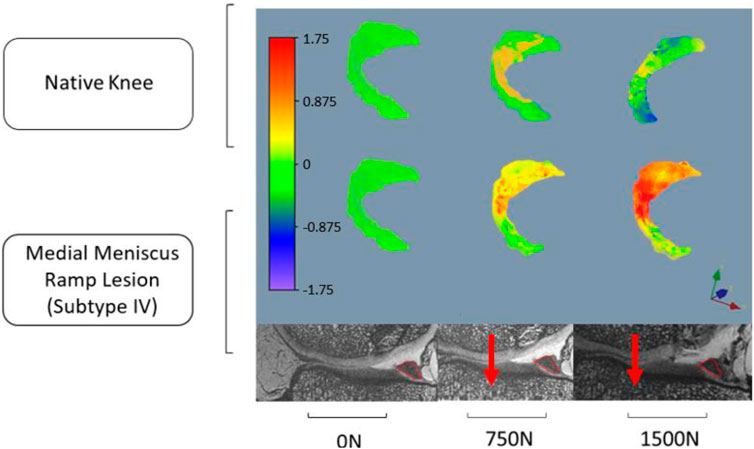
FIGURE 5. Observation of the displacement fields (in mm) after DVC assessment for knee 1 according to the anteroposterior direction (Y).
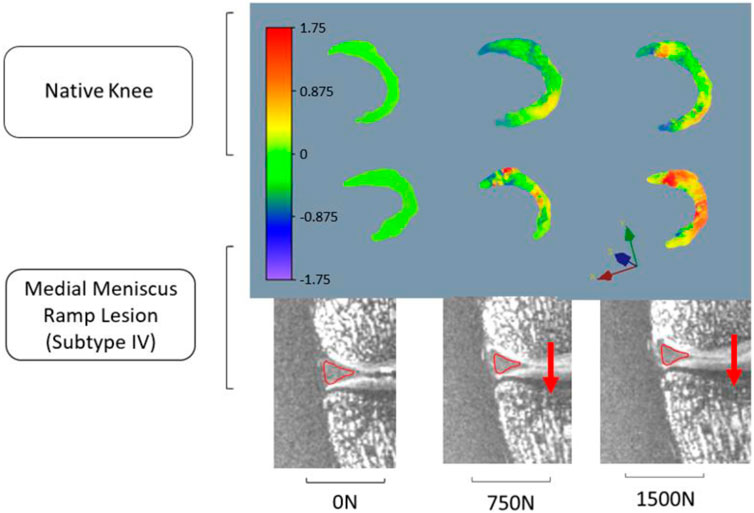
FIGURE 6. Observation of the displacement fields (in mm) after DVC assessment for knee 2 according to the lateromedial direction (X).
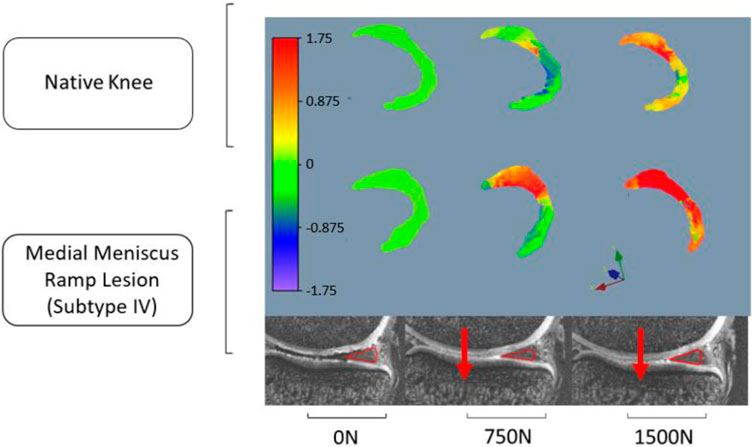
FIGURE 7. Observation of the displacement fields (in mm) after DVC assessment for knee 2 according to the anteroposterior direction (Y).
Mean displacements were measured on the posterior segment of the medial meniscus, anteriorly to the RL. In the lateromedial direction (X), the mean displacements measured at 1500N load were −0.983 mm (±0.027 mm) on the knee 1 versus −1.568 mm (±1.097 mm) on the same knee with RL injury. For knee 2, the mean displacements measured according to X with the same load were 0.738 mm (±0.133 mm) before and 1.647 mm (±0.031 mm) after RL injury. Positive or negative values are associated with the knee’s laterality. With a grade 4 medial meniscal RL, the meniscus increases its extrusion in the frontal plane (Figures 4, 6).
In the anteroposterior direction (Y), the mean displacements measured at 1500N load were 0.167 mm (±0.183 mm) on knee 1 versus 1.150 mm (±0.287 mm) on the same knee with RL injury. For knee 2, the mean displacements measured in Y with the same load were 0.739 mm (±0.132 mm) before and 2.559 mm (±0.459 mm) after RL injury. With grade 4 RL, the posterior segment of the medial meniscus increases its posterior extrusion in the sagittal plane (Figures 5, 7).
All data on the anteroposterior and/or lateromedial migration of the meniscus after axial compression between native knees and injured knees are summarized in Table 1.
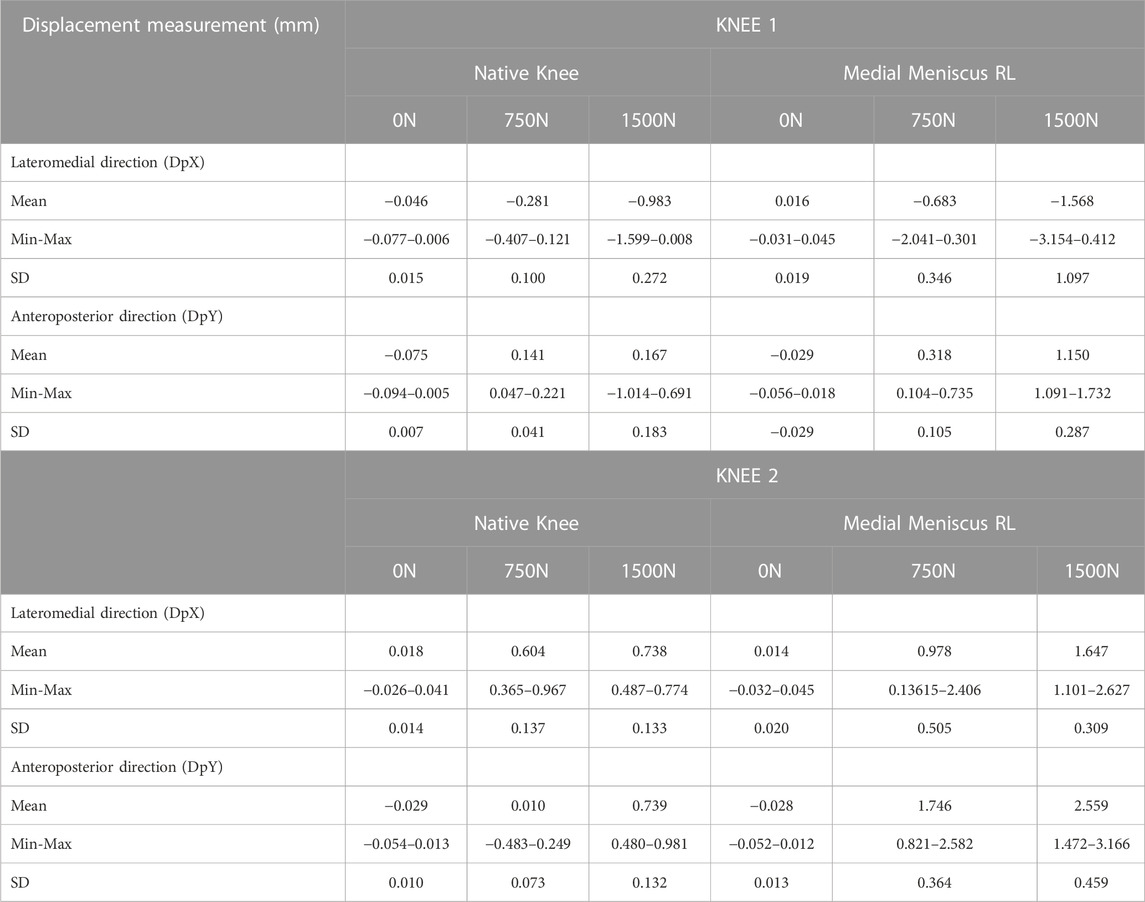
TABLE 1. Displacement measurement obtained by DVC after application of 0N, 750N, and 1500N axial loads between native knees and injured knees (in mm).
The main finding of this study is that medial meniscus RL injury increases meniscal extrusion, which is defined as the internal displacement of the medial meniscus with regard to the medial margin of the tibial plateau, and meniscal posterior mobility during axial compression. This biomechanical study confirms the hypothesis that RL could be responsible for meniscal extrusion usually considered as the result of meniscal root lesion or disruption of the coronary ligaments or isolated MTL injury (Chahla et al., 2016; Krych et al., 2017; Naendrup et al., 2019; Thaunat et al., 2021; Mariani et al., 2022).
Meniscal extrusion is recognized as a significant predictor of accelerated joint degeneration (Hein et al., 2011; Krych et al., 2017). Diagnosing meniscal extrusion is crucial, due not only to the acute functional limitations it imposes on patients but also because of its direct association with osteoarthritis (OA), a condition often observed in the elderly (Sugita et al., 2001; Guermazi et al., 2015). Meniscal extrusion has been shown to diminish the hoop function of the meniscus, increasing the risk of knee OA (Ozeki et al., 2022). In our case, RLs are prevalent meniscal injuries, typically occurring in cases of ACL rupture or knee laxity associated with anterior cruciate ligament insufficiency. These injuries are particularly common in patients under 30 years of age and male patients (Liu et al., 2011). Current literature consensus indicates that meniscal extrusion, whether with or without ACL deficiency, amplifies mechanical loading. Consequently, abnormal mechanical stress can trigger a pathological response in joint tissues, leading to cartilage degradation characteristic of knee OA, particularly in the medial compartment (Daszkiewicz and Łuczkiewicz, 2021). Similarly, a significant correlation has been established between the degree of medial meniscus extrusion and the onset of post-arthroscopic osteonecrosis of the knee (Yamaguchi et al., 2021).
Naendrup et al. (2019) found non-significant results on knee medial stress due to RL injuries. No differences were found with respect to kinematics, in situ forces in the ACL, or bony contact forces between intact knees and knees with a ramp lesion. However, this study was performed on ACL-intact knees with a maximum axial compression load of 200N on a freedom robotic testing system. While the same authors think that the indications for RL repair may be limited, there are a number of reasons that seem to justify meniscal repair in addition to the risk of OA degeneration due to RL. Medial menisci with RL are less stable and could progress toward a bucket-handle tear, especially in subtype 4 or 5 lesions (Thaunat et al., 2021). In addition, DePhilippo et al. (2018) have observed that meniscotibial and meniscocapsular lesions of the posterior segment of the medial meniscus increase knee anterior tibial translation, internal and external rotation, and pivot shift in ACL-deficient knees. Optimal treatment has been debated in the literature, especially for stable RL, although good outcomes have been shown both with and without repair (Brophy et al., 2022). Healing rates of RL were significantly better when lesions were repaired and surgical procedures appeared reliable (Hatayama et al., 2020). Recently, Park et al. (2022) analyzed the joint capsule adjacent to the medial meniscus and found that the perimeniscal joint capsule had collagen fiber orientation similar to that of circumferential meniscal fibers, potentially playing a role in preventing extrusion. They also found that the circumferential rim augmentation suture reduced the degree of meniscal extrusion while restoring meniscal function, potentially preventing the progression of arthritis in a rabbit root tear model and by means of porcine knee biomechanical analysis (Park et al., 2022).
The typical method for quantifying extrusion involves measuring the distance between the medial edge of the tibial plateau and the most prominent medial point of the medial meniscus (Choi et al., 2010). Existing literature suggests that meniscal extrusion exceeding 3–4 mm can have biomechanical implications on the tibiofemoral compartment contact area and pressures (Debieux et al., 2021). It is important to note that our findings, although lower than these thresholds, pertain to knees without osteoarthritis (OA) and ACL insufficiency.
Furthermore, even in healthy knees, some studies have demonstrated meniscal mobility. In an ultrasound-based study, Kawaguchi et al. (2012) showed that physiologic loading causes mild meniscal extrusion. Another ultrasound study demonstrated that the posterior portion experiences greater extrusion than the anterior portion, particularly as regards the medial meniscus (Sharafat Vaziri et al., 2022). Additionally, research has explored meniscal displacements and 3D morphological changes under knee weight-bearing and early flexion conditions in healthy adults, utilizing MRI (Liu et al., 2021). Of note, data through MRI regarding injured knees with volume quantification are lacking. Our study stands out as the first to evaluate meniscal displacement using DVC under various axial compression loads. The direct correlation DVC technique is reliable and reproducible, provided that study sub-volumes are optimized (Palanca et al., 2015; Marter et al., 2020).
The study has some limitations. First, it was a cadaver study. Although we tried to optimize the elasticity/stiffness ratio with respect to ethical use and institutional thawing procedure, the performance of this study on fresh cadaver knees would have allowed us to come even closer to reproducing the physiological conditions of meniscal displacement in living patients.
Secondly, the study was conducted using only two anatomical specimens. The results underscored the specific observations associated with each specimen. Mediolateral extrusion was comparable between the two knees, while variability was noted in the anteroposterior direction. In the instance of one knee (knee 2), native anteroposterior mobility surpassed that of the other. The results indicated that mobility after RL could be proportionate to mobility in the intact condition. This work served as a case study and proof of concept, demonstrating the integration of 7T MRI and DVC to characterize the mechanical behavior of the meniscus in knee articulation under loading. While intriguing initial conclusions were drawn, it is essential to validate these results through additional experiments involving a larger number of specimens.
This study was conducted with the knee in extension because of the 7T MRI device. However, extrusion of the meniscus’s medial body seemed to be greater in full extension compared to any other flexing angles. Mechanical loading can significantly deform the menisci in knee extension; however, this effect is limited during knee flexion (Liu et al., 2021). In contrast, anteroposterior mobility commonly increases with the rise of knee flexion motion (Sharafat Vaziri et al., 2022). For this reason, the data concerning lateromedial displacement (X) appear to be more informative.
It is possible that variability between our results and the findings of future studies could be due to the characteristics of the created lesions. The definition of RL is constantly debated, especially in terms of length. RL has been commonly defined as a 25 mm tear (Chahla et al., 2016; Balazs et al., 2019). However, during our experimentation, the RL length we were able to achieve was 20 and 21 mm in accordance with DePhillipo et al. (2018), who clearly established that the length of the posteromedial meniscocapsular junction may not exceed 20 mm because otherwise it would be extended to the midportion of the meniscus.
Utilization of a 7T MRI device brought forth numerous advantages and advancements. 7T MRI offers spatial resolution superior to 3T MRI, enabling the capture of highly detailed images of the knee joint and meniscus. This heightened clarity proves invaluable when evaluating intricate structures such as meniscal root attachments and subtle pathological changes within the meniscus. It bears mentioning that the biomechanical research presented in this study could be designed for routine use on the 1.5T or 3T scanners commonly employed in clinical practice. Subsequent studies need to be conducted to assess the capacity of 1.5T or 3T scanners to perform DVC measurements of mechanical fields within the meniscus with adequate resolution.
In this work, original experiments were developed to perform in situ mechanical loadings of anatomical knee specimens in a 7T MRI device and to measure volume displacements in intact meniscus or after lesion. Subtype 4 medial meniscus RL injury increases meniscal extrusion and meniscal posterior mobility during axial compression in ACL-intact knees. Indeed, the meniscotibial ligament and meniscocapsular junction seem to behave like the belt and suspenders of the medial meniscus. Although these data improve biomechanical knowledge of RL, their clinical impact in ACL-intact knees must be evaluated in the long term before proposing systematic arthroscopic repair. Following the proof of concept developed in this work, the plan is to extend the experimental approach to encompass individuals undergoing weight-bearing MRI. This expansion aims to measure in vivo deformation in soft structures, identifying meniscocapsular and/or meniscotibial insufficiency or rupture in patients.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethics committee of the French Ministry of Health under the number: DC-2019-3704 UNIVERSITE DE POITIERS, ABSLAb F-86000 Poitiers, France. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired as a gift from another research group. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
MS: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing–original draft. FZ: Methodology, Software, Visualization, Writing–review and editing. GH-G: Formal Analysis, Methodology, Visualization, Writing–review and editing. AG: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing–original draft, Writing–review and editing. GH: Investigation, Project administration, Resources, Software, Writing–review and editing. MN: Investigation, Software, Writing–review and editing. VV: Formal Analysis, Software, Supervision, Writing–review and editing. JD: Investigation, Methodology, Resources, Writing–review and editing. TV: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Supervision, Validation, Writing–review and editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to thank ABS Lab of the University of Poitiers; Mr. Christian Normand, design engineer of the Pprime Institute, for the realization of the MRI-compatible load bench and Mr. Jeffrey Arsham, an American translator, for rereading and correcting the original English-language manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahn, J. H., Bae, T. S., Kang, K.-S., Kang, S. Y., and Lee, S. H. (2011). Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am. J. Sports Med. 39, 2187–2193. doi:10.1177/0363546511416597
Balazs, G. C., Greditzer, H. G., Wang, D., Marom, N., Potter, H. G., Marx, R. G., et al. (2019). Ramp lesions of the medial meniscus in patients undergoing primary and revision ACL reconstruction: prevalence and risk factors. Orthop. J. Sports Med. 7, 232596711984350. doi:10.1177/2325967119843509
Bay, B. K., Smith, T. S., Fyhrie, D. P., and Saad, M. (1999). Digital volume correlation: three-dimensional strain mapping using X-ray tomography. Exp. Mech. 39, 217–226. doi:10.1007/BF02323555
Brophy, R. H., Steinmetz, R. G., Smith, M. V., and Matava, M. J. (2022). Meniscal ramp lesions: anatomy, epidemiology, diagnosis, and treatment. J. Am. Acad. Orthop. Surg. 30, 255–262. doi:10.5435/JAAOS-D-21-00091
Buljac, A., Jailin, C., Mendoza, A., Neggers, J., Taillandier-Thomas, T., Bouterf, A., et al. (2018). Digital volume correlation: review of progress and challenges. Exp. Mech. 58, 661–708. doi:10.1007/s11340-018-0390-7
Chahla, J., Dean, C. S., Moatshe, G., Mitchell, J. J., Cram, T. R., Yacuzzi, C., et al. (2016). Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop. J. Sports Med. 4, 232596711665781. doi:10.1177/2325967116657815
Choi, C.-J., Choi, Y.-J., Lee, J.-J., and Choi, C.-H. (2010). Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy 26, 1602–1606. doi:10.1016/j.arthro.2010.05.004
Daszkiewicz, K., and Łuczkiewicz, P. (2021). Biomechanics of the medial meniscus in the osteoarthritic knee joint. PeerJ 9, e12509. doi:10.7717/peerj.12509
Debieux, P., Jimenez, A. E., Novaretti, J. V., Kaleka, C. C., Kriscenski, D. E., Astur, D. C., et al. (2021). Medial meniscal extrusion greater than 4 mm reduces medial tibiofemoral compartment contact area: a biomechanical analysis of tibiofemoral contact area and pressures with varying amounts of meniscal extrusion. Knee Surg. Sports Traumatol. Arthrosc. 29, 3124–3132. doi:10.1007/s00167-020-06363-0
DePhillipo, N. N., Moatshe, G., Brady, A., Chahla, J., Aman, Z. S., Dornan, G. J., et al. (2018). Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am. J. Sports Med. 46, 2422–2431. doi:10.1177/0363546518774315
Disney, C. M., Lee, P. D., Hoyland, J. A., Sherratt, M. J., and Bay, B. K. (2018). A review of techniques for visualising soft tissue microstructure deformation and quantifying strain ex vivo: soft tissue microstructure deformation and quantifying strain. J. Microsc. 272, 165–179. doi:10.1111/jmi.12701
Engebretsen, L., Wijdicks, C. A., Anderson, C. J., Westerhaus, B., and LaPrade, R. F. (2012). Evaluation of a simulated pivot shift test: a biomechanical study. Knee Surg. Sports Traumatol. Arthrosc. 20, 698–702. doi:10.1007/s00167-011-1744-1
Germaneau, A., Doumalin, P., and Dupré, J. C. (2007). Full 3D measurement of strain field by scattered light for analysis of structures. Exp. Mech. 47, 523–532. doi:10.1007/s11340-006-9029-1
Germaneau, A., Doumalin, P., and Dupré, J.-C. (2008). Comparison between X-ray micro-computed tomography and optical scanning tomography for full 3D strain measurement by digital volume correlation. NDT E Int. 41, 407–415. doi:10.1016/j.ndteint.2008.04.001
Guermazi, A., Eckstein, F., Hayashi, D., Roemer, F. W., Wirth, W., Yang, T., et al. (2015). Baseline radiographic osteoarthritis and semi-quantitatively assessed meniscal damage and extrusion and cartilage damage on MRI is related to quantitatively defined cartilage thickness loss in knee osteoarthritis: the Multicenter Osteoarthritis Study. Osteoarthr. Cartil. 23, 2191–2198. doi:10.1016/j.joca.2015.06.017
Hatayama, K., Terauchi, M., Saito, K., Takase, R., and Higuchi, H. (2020). Healing status of meniscal ramp lesion affects anterior knee stability after ACL reconstruction. Orthop. J. Sports Med. 8, 232596712091767. doi:10.1177/2325967120917674
Hein, C. N., Deperio, J. G., Ehrensberger, M. T., and Marzo, J. M. (2011). Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee 18, 189–192. doi:10.1016/j.knee.2010.04.006
Kawaguchi, K., Enokida, M., Otsuki, R., and Teshima, R. (2012). Ultrasonographic evaluation of medial radial displacement of the medial meniscus in knee osteoarthritis. Arthritis Rheum. 64, 173–180. doi:10.1002/art.33319
Krych, A. J., Reardon, P. J., Johnson, N. R., Mohan, R., Peter, L., Levy, B. A., et al. (2017). Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 25, 383–389. doi:10.1007/s00167-016-4359-8
Kunze, K. N., Haddad, A., White, A. E., Cohn, M. R., LaPrade, R. F., and Chahla, J. (2021b). The top 50 most cited publications in meniscus research. J. Knee Surg. 36, 329–334. doi:10.1055/s-0041-1733881
Kunze, K. N., Wright-Chisem, J., Polce, E. M., DePhillipo, N. N., LaPrade, R. F., and Chahla, J. (2021a). Risk factors for ramp lesions of the medial meniscus: a systematic review and meta-analysis. Am. J. Sports Med. 49, 3749–3757. doi:10.1177/0363546520986817
Liu, T., Shen, X., Ji, Q., Xiao, J., Zuo, J., and Gao, Z. (2021). The MRI-based 3D morphologic changes of knee meniscus under knee weight-bearing and early flexion conditions. Sci. Rep. 11, 22122. doi:10.1038/s41598-021-01531-9
Liu, X., Feng, H., Zhang, H., Hong, L., Wang, X. S., and Zhang, J. (2011). Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am. J. Sports Med. 39, 832–837. doi:10.1177/0363546510388933
Magosch, A., Mouton, C., Nührenbörger, C., and Seil, R. (2021). Medial meniscus ramp and lateral meniscus posterior root lesions are present in more than a third of primary and revision ACL reconstructions. Knee Surg. Sports Traumatol. Arthrosc. 29, 3059–3067. doi:10.1007/s00167-020-06352-3
Mariani, P. P., Torre, G., and Battaglia, M. J. (2022). The post-traumatic meniscal extrusion, sign of meniscotibial ligament injury. A case series. Orthop. Traumatol. Surg. Res. 108, 103226. doi:10.1016/j.otsr.2022.103226
Marter, A., Burson-Thomas, C., Dickinson, A., Rankin, K., Mavrogordato, M., Pierron, F., et al. (2020). Measurement of internal implantation strains in analogue bone using DVC. Mater. (Basel) 13, E4050. doi:10.3390/ma13184050
Mouton, C., Magosch, A., Pape, D., Hoffmann, A., Nührenbörger, C., and Seil, R. (2020). Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg. Sports Traumatol. Arthrosc. 28, 1023–1028. doi:10.1007/s00167-019-05579-z
Naendrup, J.-H., Pfeiffer, T. R., Chan, C., Nagai, K., Novaretti, J. V., Sheean, A. J., et al. (2019). Effect of meniscal ramp lesion repair on knee kinematics, bony contact forces, and in situ forces in the anterior cruciate ligament. Am. J. Sports Med. 47, 3195–3202. doi:10.1177/0363546519872964
Ollivier, M., Batty, L., Murgier, J., and Pujol, N. (2022). Recent advances in ligamentous, meniscal and joint-preserving knee surgery: pushing the limits. Orthop. Traumatol. Surg. Res. 108, 103282. doi:10.1016/j.otsr.2022.103282
Ozeki, N., Koga, H., and Sekiya, I. (2022). Degenerative meniscus in knee osteoarthritis: from pathology to treatment. Life (Basel) 12, 603. doi:10.3390/life12040603
Palanca, M., Tozzi, G., Cristofolini, L., Viceconti, M., and Dall’Ara, E. (2015). Three-dimensional local measurements of bone strain and displacement: comparison of three digital volume correlation approaches. J. Biomech. Eng. 137. doi:10.1115/1.4030174
Park, D. Y., Yin, X. Y., Chung, J. Y., Jin, Y. J., Kwon, H. J., Lee, G. B., et al. (2022). Circumferential rim augmentation suture around the perimeniscal capsule decreases meniscal extrusion and progression of osteoarthritis in rabbit meniscus root tear model. Am. J. Sports Med. 50, 689–698. doi:10.1177/03635465211064297
Peltier, A., Lording, T., Maubisson, L., Ballis, R., Neyret, P., and Lustig, S. (2015). The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg. Sports Traumatol. Arthrosc. 23, 2967–2973. doi:10.1007/s00167-015-3751-0
Seil, R. (2018). Editorial commentary: medial meniscal ramp lesions: lessons learned from the past in the pursuit of evidence. Arthroscopy 34, 1638–1640. doi:10.1016/j.arthro.2018.02.032
Sharafat Vaziri, A., Aghaghazvini, L., Jahangiri, S., Tahami, M., Borazjani, R., Tahmasebi, M. N., et al. (2022). Determination of normal reference values for meniscal extrusion using ultrasonography during the different range of motion: a pilot, feasibility study. J. Ultrasound Med. 41, 2715–2723. doi:10.1002/jum.15955
Stephen, J. M., Halewood, C., Kittl, C., Bollen, S. R., Williams, A., and Amis, A. A. (2016). Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am. J. Sports Med. 44, 400–408. doi:10.1177/0363546515617454
Sugita, T., Kawamata, T., Ohnuma, M., Yoshizumi, Y., and Sato, K. (2001). Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin. Orthop. Relat. Res. 387, 171–177. –7. doi:10.1097/00003086-200106000-00023
Thaunat, M., Ingale, P., Penet, A., Kacem, S., Haidar, I., Bauwens, P.-H., et al. (2021). Ramp lesion subtypes: prevalence, imaging, and arthroscopic findings in 2156 anterior cruciate ligament reconstructions. Am. J. Sports Med. 49, 1813–1821. doi:10.1177/03635465211006103
Valle, V., Bokam, P., Germaneau, A., and Hedan, S. (2019). New development of Digital Volume Correlation for the study of fractured materials. Exp. Mech. 59, 1–15. doi:10.1007/s11340-018-0415-2
Wilke, H.-J., Wenger, K., and Claes, L. (1998). Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur. Spine J. 7, 148–154. doi:10.1007/s005860050045
Keywords: medial meniscus, ramp lesion, digital volume correlation (DVC), magnetic resonace imaging (MRI), displacement fields
Citation: Severyns M, Zot F, Harika-Germaneau G, Germaneau A, Herpe G, Naudin M, Valle V, Danion J and Vendeuvre T (2024) Extrusion and meniscal mobility evaluation in case of ramp lesion injury: a biomechanical feasibility study by 7T magnetic resonance imaging and digital volume correlation. Front. Bioeng. Biotechnol. 11:1289290. doi: 10.3389/fbioe.2023.1289290
Received: 05 September 2023; Accepted: 11 December 2023;
Published: 05 January 2024.
Edited by:
Petri Tanska, University of Eastern Finland, FinlandReviewed by:
Ville-Pauli Karjalainen, University of Oulu, FinlandCopyright © 2024 Severyns, Zot, Harika-Germaneau, Germaneau, Herpe, Naudin, Valle, Danion and Vendeuvre. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: A. Germaneau, YXJuYXVkLmdlcm1hbmVhdUB1bml2LXBvaXRpZXJzLmZy
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.