- 1Department of Spine Surgery, Tianjin Hospital, Tianjin University, Tianjin, China
- 2Tianjin Key Laboratory for Advanced Mechatronic System Design and Intelligent Control, School of Mechanical Engineering, Tianjin University of Technology, Tianjin, China
- 3National Demonstration Center for Experimental Mechanical and Electrical Engineering Education, Tianjin University of Technology, Tianjin, China
- 4Department of Orthopaedics, Chinese People’s Liberation Army General Hospital, Beijing, China
Background: The effects of cannulated screws made of polyetheretherketone (PEEK) on the biomechanical properties of the vertebral body during vertebra-pediculoplasty remain unclear. This study aimed to investigate whether PEEK screws have the potential to replace titanium alloy screws.
Methods: The surgical model of two different materials of screws was constructed using the finite element method. The biomechanical effects of the two models on the vertebral body under different working conditions were compared.
Results: ① The peak von Mises stress of PEEK screws was significantly lower than that of titanium screws, with a reduction ranging from 52% to 80%. ② The von Mises stress values for the injured T12 spine were similar for both materials. Additionally, the segmental range of motion and intervertebral disc pressure showed no significant difference between the two materials.
Conclusion: PEEK screws demonstrated advantages over titanium screws and may serve as a viable alternative for screw materials in vertebra-pediculoplasty.
1 Introduction
Vertebra-Pediculoplasty has emerged as a novel treatment approach for managing split and delayed osteoporotic vertebral fractures that were at risk of cement dislocation (Noritaka et al, 2021). It addressed the issue of poor clinical outcomes associated with balloon kyphoplasty for cleft osteoporotic vertebral fractures (Takahashi et al, 2019). The method involved using cannulated screws inserted into the cement block, in combination with balloon kyphoplasty, to create a “pedicle” (Noritaka et al, 2021). Traditional screws were primarily made of titanium, which offered excellent mechanical properties and good biocompatibility. However, their elastic modulus significantly differed from that of bone tissue, thereby increasing the risk of implant-related complications such as screw loosening or fracture, degeneration of adjacent segments, and long-term complications like pseudarthrosis (Zhang and Rong, 2020).
To overcome these limitations, this study proposed the use of polyether-ether-ketone (PEEK) material as an alternative to titanium alloy screws. PEEK has been extensively studied as an orthopedic implant material since the 1990 s (Kurtz and Devine, 2007). It has been a semi-crystalline polymer that exhibited excellent mechanical properties, favorable biocompatibility, X-ray penetrability, and other desirable physical and chemical properties, making it a promising material for orthopedic implants (Panayotov et al, 2016). Furthermore, its elastic modulus closely resembles that of normal human bone tissue, reducing stress-shielding effects (Zhao et al, 2020; Mrówka et al, 2021). Hence, this study aimed to evaluate the potential benefits of using PEEK screws in vertebra-pediculoplasty to minimize the risks associated with titanium alloys.
As vertebra-pediculoplasty was a relatively new method, the biomechanical effects in clinical practice remained unclear. Finite element (FE) analysis served as a valuable tool for assessing the biomechanical parameters of vertebral columns (Marien et al, 2017), and several studies have been conducted to evaluate the biomechanical properties of titanium and PEEK retention bars and spacers during surgery (Li et al, 2023). However, studies on titanium and PEEK screws have been limited to in vitro experiments (Lindtner et al, 2018; Stavros et al, 2020). Therefore, this research employed finite element analysis to compare the biomechanical effects of PEEK and titanium screws in vertebra-pediculoplasty, utilizing a finite element model of the human T11-L1 segment. The findings of this study may provide valuable theoretical guidance for the clinical application of screw materials.
2 Materials and methods
2.1 Establishment of normal thoracolumbar and osteoporotic fracture models
The CT data of a healthy 30-year-old male were imported into Mimics software (Materialise Technologies, Leuven, Belgium) to initially create a geometric model of the thoracolumbar spine (T11-L1). The thoracolumbar spine model was then imported into 3-Matic (Materialise Technologies, Leuven, Belgium) for individual processing of each vertebral body, resulting in a more accurate model structure in Geomagic software (Geomagic Inc., North Carolina, United States). The model was further processed in HyperMesh software (Altair Engineering Corp, Michigan, United States) for meshing, material property assignment, and assembly. Finally, the model was imported into Abaqus software (Dassault Systemes, PA, United States) for calculations and analysis (Tan et al, 2021). The elastic modulus of the osteoporotic vertebral structures was determined based on POLIKEIT et al (POLIKEIT et al, 2003), and specific material properties were determined according to previous studies (SHIM et al, 2008), as shown in Table 1.
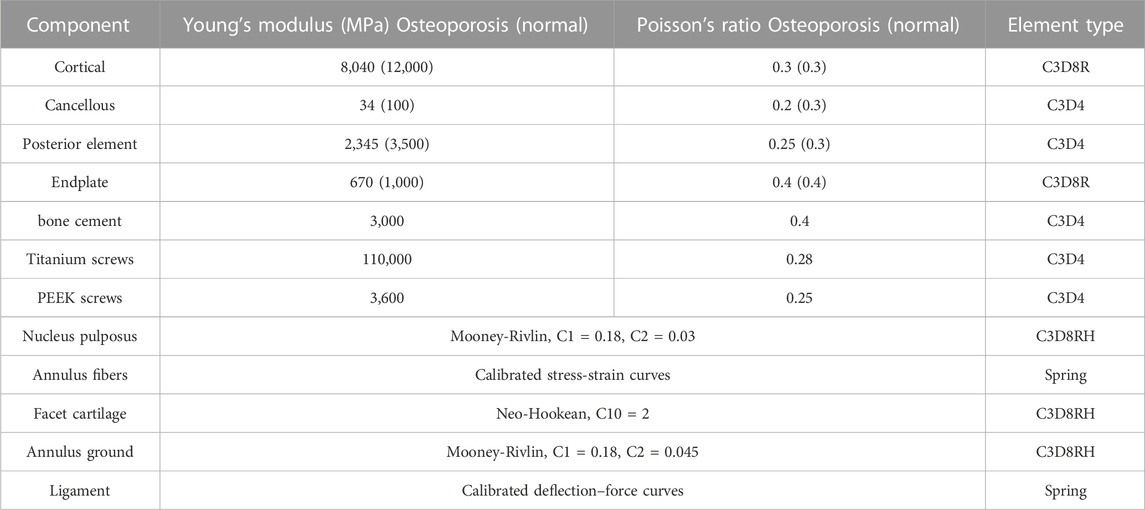
TABLE 1. Material properties of thoracolumbar spine and screws (POLIKEIT et al, 2003; Stavros et al, 2020; Tan et al, 2021).
2.2 Establishment of surgical model
The hollow lateral screw geometry was created in SolidWorks and imported into HyperMesh to assemble it with the vertebral body. The vertebral body-screw connection was simulated using a “binding” constraint, completing the vertebral screw fusion model. Two postoperative models of different materials (titanium and PEEK) for screw placement into the vertebral body were established based on vertebra-pediculoplasty. The cannulated screws used were 6.5 mm in diameter and 50 mm long. During the operation, bone cement was injected into the vertebral body through the hollow screw, and it diffused around the side hole of the screw, wrapping the screw evenly in a cylindrical shape (WANG et al, 2014). Each cannulated screw was injected with 2 ml of bone cement, and a cylindrical block with a radius of 8 mm and a height of 9.95 mm was created in SolidWorks to simulate the bone cement block. The screws of the two different materials had the same structure and shape. The establishment of the surgical operation model is illustrated in Figure 1.
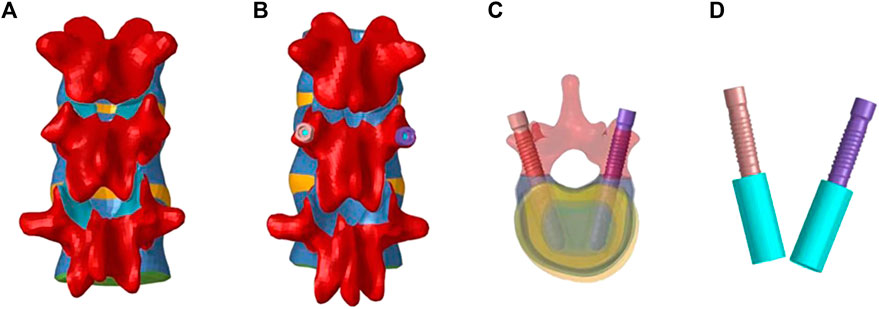
FIGURE 1. Establishment of the model after screw operation. (A): Schematic diagram before T11-L1; (B): Schematic diagram of T11-L1; (C): Screw placement; (D): Screw-cement model.
2.3 Loads and boundary conditions
A follower load of 500 N was applied to the upper surface of the T11 vertebral body to simulate physiological compressive loading. A moment load of 7.5 N m was applied to the T11 vertebral body to simulate forward flexion, back extension, lateral bending, and axial rotational motion. During loading, all degrees of freedom of the lower surface of the L1 vertebral body were constrained. (LIAO et al, 2017; DU et al, 2021).
2.4 Main outcome indicators
The maximum von Mises stresses of the screws and the injured T12 vertebral structure were compared for each model with different materials under various gestures such as flexion, extension, left bending, right bending, left rotation, and right rotation. Additionally, the segmental range of motion and intervertebral disc pressure were also evaluated.
3 Results
3.1 Verification of the normal thoracolumbar vertebrae finite element model
The range of motion (ROM) of the vertebral body was calculated under different postures. The ROMs of the T11-T12 segments were found to be 7.4°, 8.9°, and 4.6° for flexion and extension, lateral bending, and axial rotation, respectively. Similarly, the ROMs of the T12-L1 segments were 7.2°, 8.7°, and 3.8° for the corresponding postures. These results were compared with previous experimental data, and they were consistent with the findings reported in the literature (PANJABI et al, 1994; LIANG et al, 2015).
3.2 Maximum stress results of the screw
In the six models, the peak von Mises stress of the PEEK screws was 17.52 MPa, 9.125 MPa, 16.66 MPa, 8.48 MPa, 14.94 MPa, and 17.8 MPa. On the other hand, the peak stress of the titanium alloy screws was 89.03 MPa, 29.93 MPa, 69.06 MPa, 31.37 MPa, 90.88 MPa, and 37.48 MPa (e.g., Figure 2A). Upon comparison, it was observed that the maximum von Mises stress on PEEK screws was significantly lower than that on titanium screws.
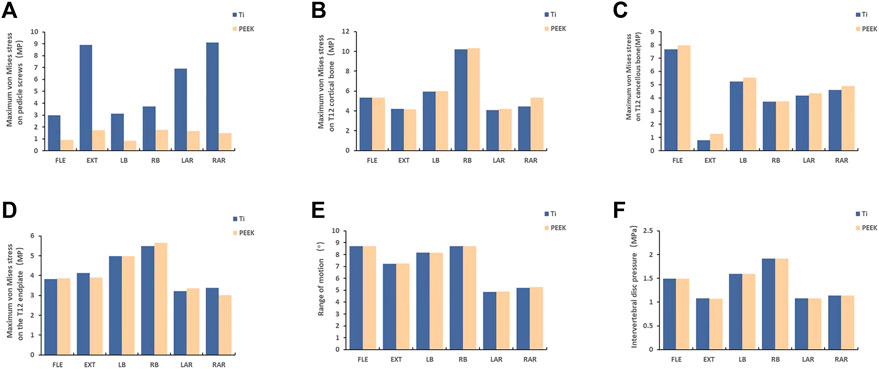
FIGURE 2. The stress results of the structure of the vertebra body [(A) The result of stress on pedicle screw; (B, C, D): The stress results of the T12 structure of the injured vertebra; (E, F): the result of the segmental range of motion and intervertebral disc pressure; FL = flexion, EX = extension, LB = left bending, RB = right bending, LAR = left axial rotation, and RAR = right axial rotation].
3.3 Maximum Stress Analysis of Injured Vertebral T12 Structure and Analysis of Segmental Range of Motion and Intervertebral Disc Pressure
There were no significant differences in the maximum stress of the T12 cortical bone in the injured vertebra when using PEEK screws compared to titanium alloy screws under the six different states. Similarly, no noticeable differences were found in the maximum stress of the T12 cancellous bone or the analysis of the endplates (e.g. Figure 2B–D). Furthermore, the analysis of the range of motion of the vertebral body and the intervertebral disc pressure in the T11-L1 segment yielded similar results (e.g. Figure 2E, F). Upon comparing the results of the finite element analysis, it was concluded that different materials have minimal impact on the vertebral body.
4 Discussion
Due to its unique properties, PEEK has gained significant interest in bone implant research. The use of PEEK in orthopedic screws offers a promising avenue for exploration. In this study, we conducted a simulation-based analysis to assess the potential of PEEK as a substitute for the conventional titanium alloy used in screw fabrication. PEEK is a semi-crystalline polymer with excellent properties such as high modulus, melting point, processing performance, and strength (KULKARNI et al, 2007). Its elastic modulus closely resembles cortical bone, which reduces stress-shielding effects (MO et al, 2019). Additionally, PEEK is radiolucent, biocompatible, and does not cause artifacts during magnetic resonance scanning.
Recent efforts have focused on optimizing the mechanical and biological properties of PEEK through various methods such as 3D printing, coating, chemical modification, and the introduction of bioactive or antibacterial substances (Chen et al, 2022). These modifications aim to enhance the overall properties of PEEK and facilitate the treatment of bone injuries, making PEEK materials a promising option for lumbar spine repair.
In recent years, numerous studies have explored the factors that influence screw stability, including screw diameter, shape, length, thread shape, implantation method, angle, and combination (ABSHIRE et al, 2001; KINER et al, 2008; SENGUPTA and Herkowitz, 2012; Karami et al, 2015; JENDOUBI et al, 2018; NAKASHIMA et al, 2019). The current study investigates the effect of screw material in finite element analysis to provide further insights.
By comparing the von Mises stress of screws made from different materials under different vertebral body motions, our analysis reveals that PEEK screws have a significant advantage in reducing peak stress compared to titanium alloy screws. Specifically, the range of reduction observed in the von Mises stress with PEEK screws ranges between 52% and 80%. The observed reduction in peak stress indicates that the use of PEEK screws may lead to reduce the incidence of screw loosening, thereby establishing its potential as a promising alternative material. Some experiments have confirmed the idea that PEEK screws have a low risk of loosening. Richard Lintner et al (Lindtner et al, 2018) conducted cyclic loading tests on ten cadaveric lumbar vertebrae to compare the performance of carbon fiber-reinforced PEEK (CF/PEEK) and standard titanium pedicle screws in reducing screw loosening. The study found that PEEK and CF/PEEK screw/rod configurations had a significant advantage over titanium screws in reducing screw loosening. Similarly, Stavros Oikonomidis (Stavros et al, 2020) conducted cyclic loading tests on ten freshly frozen human cadaveric lumbar vertebrae to investigate the loosening rate of pedicle screws made of CFR/PEEK compared to titanium. The study concluded that the use of CFR/PEEK pedicle screws could reduce the rate of screw loosening. Further investigation is warranted to compensate for the lack of clinical studies using pedicle screws made of PEEK. One avenue for exploration is to compare relevant trials involving PEEK rods. Qian Jiaming et al (QIAN et al, 2022) and Huang Weimin et al (Huang et al, 2016) conducted follow-up studies for 6 months and 2 years, respectively, on patients who underwent posterior lumbar pedicle internal fixation and multi-level fixation using PEEK material. The results of the studies showed no instances of screw fracture or loosening during the respective follow-up periods. Although further clinical follow-up studies are required to ascertain the superiority of PEEK screws over other materials in preventing screw loosening, recent research suggests that PEEK screws may have similar benefits to PEEK rods in this regard.
When assessing the risk of screw fracture, it is important to consider the ratio of peak stress to yield stress rather than focusing solely on stress magnitude. The ratio of peak stress to yield stress for PEEK screws ranged from 8% to 17%, while for titanium screws, it fell within the range of 3%–12% (PEEK: 100 MPa, titanium: 750 MPa). The higher percentage for PEEK screws suggests a potential escalation of breakage risk (e.g., Figure 3), consistent with prior findings by FAN et al (FAN et al, 2021). However, there have been no reported cases of PEEK rod fracture, possibly due to the load experienced under physiological conditions being insufficient to cause rupture. Consequently, screw breakage is unlikely to occur.
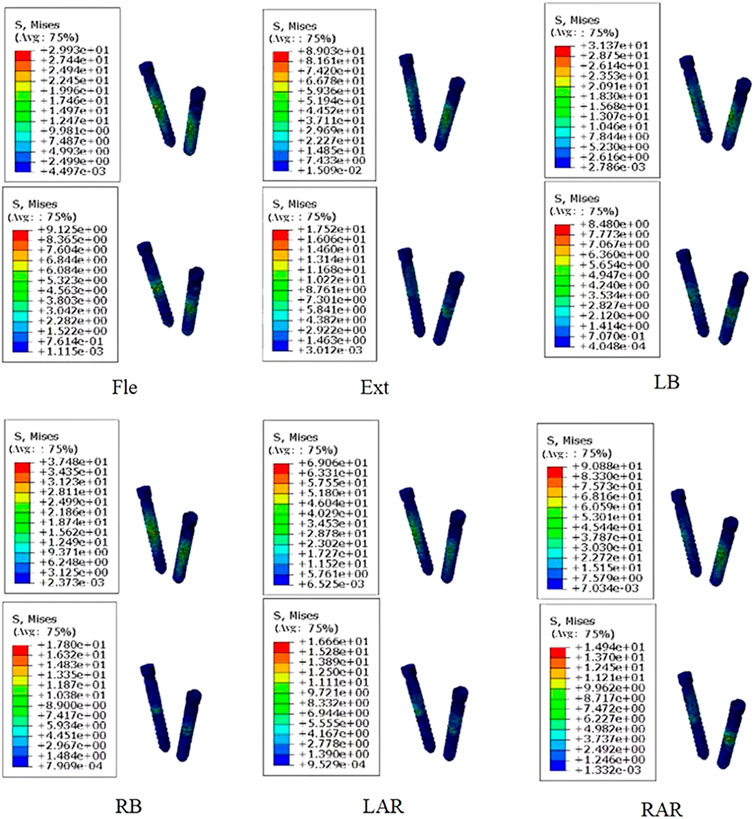
FIGURE 3. Comparison of stress distribution of screws made of two materials under different loading directions. (The figure shows titanium alloy material at the top and PEEK material at the bottom).
Previous investigations have examined the load transmission properties of titanium alloy posterior screw rod systems and PEEK screws in posterolateral lumbar fixation. These studies indicated that the titanium alloy system can transmit approximately 67% of the axial compressive load, while the natural upright state can bear only about 20% of the load (CUNNINGHAM and POLLY, 2002; AHN et al, 2008). PEEK screws have favorable characteristics such as biocompatibility, radiolucency, and a lower elastic modulus compared to titanium alloy screws. These characteristics allow PEEK screws to transfer more load to the front column, improving the load distribution between the front and rear columns. A finite element study by GARNET et al (GORNET et al, 2011) supported this finding, demonstrating that a titanium rod bore at least 6% more load than a PEEK rod. This evidence suggests that the principal advantage of PEEK screws lies in mitigating stress concentration on the screw.
Next, we analyze the finite element results of the vertebral structure. The von Mises stress of the vertebral body, as well as the segmental Range of Motion and Intervertebral Disc Pressure, were obtained through finite element analysis under various conditions. The results show that the stability of the vertebral body remains largely unaffected. Similar findings have been reported in related investigations. Nomidis et al (Stavros et al, 2020) conducted biomechanical experiments using cadaveric specimens and found no macroscopic changes in the vertebral structure. Additionally, YEAGER et al (YEAGER et al, 2015) compared PEEK and titanium rods using human lumbar spine specimens and concluded that both materials offered comparable stability under different loading modes. While PEEK may not match the strength and rigidity of titanium alloys, it possesses adequate strength and rigidity to maintain spinal stability and endure physiological biomechanical demands. The elastic modulus of PEEK closely matches that of bone tissue, allowing PEEK screws to conform to micro-movements and deformations of interconnected spinal bones. This feature reduces the likelihood of stress concentration and ensures a secure connection. Moreover, PEEK demonstrates exceptional biocompatibility, minimizing the risk of inflammatory responses or tissue rejection. PEEK screws can integrate stably with the surrounding bone tissue, exhibiting biostability comparable to that of titanium screws. The adaptive nature of PEEK material to bone morphology enables it to establish minute biological interconnections with bone tissue, enhancing the stability of PEEK screw integration with the spinal bone and reducing the risk of loosening. However, the development of more ideal internal fixation materials warrants further exploration through basic scientific research and clinical trials.
Several limitations should be considered when interpreting the results of this study. Firstly, the finite element model used is based on theoretical numerical simulations and may not fully capture the complexity of the human spine system, as it does not account for factors such as cyclic loads and the influence of muscles. Secondly, the thoracic and lumbar spine models used are limited to a single subject, and the number of models is small, which may limit the generalizability of the findings. Lastly, this study represents a preliminary exploration of finite element analysis. Further research and exploration are necessary to establish a solid foundation for the long-term development of PEEK material in lumbar spine repair.
5 Conclusion
In conclusion, PEEK screws demonstrate comparable efficacy to titanium alloy screws in providing segmental stability post-surgery. Additionally, PEEK screws facilitated the prevention of loosening, which was a great clinical advantage. Moreover, the radiolucent nature of PEEK screws facilitates postoperative imaging without interfering with radiation therapy. Thus, the PEEK or PEEK composite material may emerge as a viable alternative for screw materials in clinical practice. (Sato et al, 2018).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This study was supported by the National Key R&D Program of China (2020YFC1107402), National Natural Science Foundation of China (81871782), Tianjin Science Fund for Distinguished Young Scholars (18JCJQJC47900), Medical Innovation Fund for Clinical Application of National Clinical Research Center for Orthopedics, Sports Medicine and Rehabilitation (2021-NCRC-CXJJ-ZH-22), Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-026A).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abshire, B. B., Kambic, H. E., and Valdevit, A. (2001). Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J. 1, 408–414. doi:10.1016/s1529-9430(01)00119-x
Ahn, Y. H., Chen, W. M., Lee, K. Y., Park, K. W., and Lee, S. J. (2008). Comparison of the load-sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomed. Mater. 3 (4), 044101. doi:10.1088/1748-6041/3/4/044101
Chen, J., Cao, G., Li, L., Cai, Q., Dunne, N., and Li, X. (2022). Modification of polyether ether ketone for the repairing of bone defects. Biomed. Mater. (Bristol, Engl. 17 (4), 042001. doi:10.1088/1748-605x/ac65cd
Cunningham, B. W., and Polly, D. W. (2002). The use of interbody cage devices for spinal deformity: A biomechanical perspective. Clin. Orthop. Relat. Res. 394, 73–83. doi:10.1097/00003086-200201000-00009
Du, C. F., Cai, X. Y., Gui, W., Sun, M. S., Liu, Z. X., Liu, C. J., et al. (2021). Does oblique lumbar interbody fusion promote adjacent degeneration in degenerative disc disease:A finite element analysis. Comput. Biol. Med. 128, 104122. doi:10.1016/j.compbiomed.2020.104122
Fan, W., Guo, L. X., and Zhang, M. (2021). Biomechanical analysis of lumbar interbody fusion supplemented with various posterior stabilization systems. Eur. Spine J. 30 (8), 2342–2350. doi:10.1007/s00586-021-06856-7
Gornet, M. F., Chan, F. W., Coleman, J. C., Murrell, B., Nockels, R. P., Taylor, B. A., et al. (2011). Biomechanical assessment of a PEEK rod system for semi-rigid fixation of lumbar fusion constructs. J. Biomech. Eng. 133 (8), 081009. doi:10.1115/1.4004862
Huang, W., Chang, Z., Song, R., Zhou, K., and Yu, X. (2016). Non-fusion procedure using PEEK rod systems for lumbar degenerative diseases: Clinical experience with a 2-year follow-up. BMC Musculoskelet. Disord. 17 (1), 53–57. doi:10.1186/s12891-016-0913-2
Jendoubi, K., Bendjaballah, M., and Slimane, N. (2018). Effects of the insertion type and depth on the pedicle screw pullout strength: A finite element study. Appl. Bionics Biomech. 2018, 1460195. doi:10.1155/2018/1460195
Karami, K. J., Buckenmeyer, L. E., Kiapour, A. M., Kelkar, P. S., Goel, V. K., Demetropoulos, C. K., et al. (2015). Biomechanical evaluation of the pedicle screw insertion depth effect on screw stability under cyclic loading and subsequent pullout. J. spinal Disord. Tech. 28 (3), E133–E139. doi:10.1097/bsd.0000000000000178
Kiner, D. W., Bartol, S. W., Vaidya, R., Yeni, Y. N., and Vaidya, R. (2008). Biomechanical analysis of different techniques in revision spinal instrumentation: Larger diameter screws versus cement augmentation. Spine 33, 2618–2622. doi:10.1097/brs.0b013e3181882cac
Kulkarni, A. G., Hee, H. T., and Wong, H. K. (2007). Solis cage (PEEK) for anterior cervical fusion: Preliminary radiological results with emphasis on fusion and subsidence. Spine J. 7 (2), 205–209. doi:10.1016/j.spinee.2006.03.002
Kurtz, Steven M., and Devine, John N. (2007). PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 28 (32), 4845–4869. ISSN 0142-9612. doi:10.1016/j.biomaterials.2007.07.013
Liao, J. C., Chen, W. P., and Wang, H. (2017). Treatment of thoracolumbar burst fractures by short-segment pedicle screw fixation using a combination of two additional pedicle screws and vertebroplasty at the level of the fracture:a finite element analysis. BMC Musculoskelet. Disord. 18 (1), 262. doi:10.1186/s12891-017-1623-0
Li, J., Cao, S., Guo, D., Zhang, Q. C., He, X. J., Li, H. P., et al. (2023). Finite element analysis of polyetheretherketone and titanium rods in posterior lumbar interbody fusion. Chin. J. Tissue Eng. Res. 27 (22), 3445–3450. doi:10.12307/2023.398
Liang, D., Ye, L. Q., Jiang, X. B., Yang, P., Zhou, G. Q., Yao, Z. S., et al. (2015). Biomechanical effects of cement distribution in the fractured area on osteoporotic vertebral compression fractures:a three-dimensional finite element analysis. J. Surg. Res. 195 (1), 246–256. doi:10.1016/j.jss.2014.12.053
Lindtner, R. A., Schmid, R., Nydegger, T., Konschake, M., and Schmoelz, W. (2018). Pedicle screw anchorage of carbon fiber-reinforced PEEK screws under cyclic loading. Eur. Spine J. 27, 1775–1784. doi:10.1007/s00586-018-5538-8
Marien, C., Arnaud, G., Saget, M., Dupré, J. C., Doumalin, P., Brémand, F., et al. (2017). Biomechanical analysis of the thoracolumbar spine under physiological loadings: Experimental motion data corridors for validation of finite element models. Proc. Institution Mech. Eng. Part H J. Eng. Med. 231 (10), 975–981. doi:10.1177/0954411917719740
Mo, S., Mehrjou, B., Tang, K., Wang, H., Huo, K., Qasim, A. M., et al. (2019). Dimensional-dependent antibacterial behavior on bioactive micro/nano polyetheretherketone (PEEK) arrays. Chem. Eng. J. 392, 123736. doi:10.1016/j.cej.2019.123736
Mrówka, M., Machoczek, T., Jureczko, P., Joszko, K., Gzik, M., Wolański, W., et al. (2021). Mechanical, chemical, and processing properties of specimens manufactured from poly-ether-ether-ketone (PEEK) using 3D printing. Materials 14 (11), 2717. doi:10.3390/ma14112717
Nakashima, D., Ishii, K., Nishiwaki, Y., Kawana, H., Jinzaki, M., Matsumoto, M., et al. (2019). Quantitative CT-based bone strength parameters for the prediction of novel spinal implant stability using resonance frequency analysis: A cadaveric study involving experimental micro-CT and clinical multislice CT. Eur. Radiol. Exp. 3 (1), 1–8. doi:10.1186/s41747-018-0080-3
Noritaka, Y., Yoshiro, Y., Nishimura, T., Yamashiro, T., Shimozaki, K., Mori, A., et al. (2021). Vertebra-pediculoplasty: A new approach to treatment of split-type and delayed-union osteoporotic vertebral fracture with a risk of cement dislodgement. World Neurosurg. 155, e55–e63. doi:10.1016/j.wneu.2021.07.142
Panayotov, I. V., Orti, V., Cuisinier, F., and Yachouh, J. (2016). Polyetheretherketone (PEEK) for medical applications. J. Mater Sci. Mater Med. 27, 118. doi:10.1007/s10856-016-5731-4
Panjabi, M. M., Oxland, T. R., Lin, R. M., and McGowen, T. W. (1994). Thoracolumbar burst fracture.A biomechanical investigation of its multidirectional flexibility. Spine 19 (5), 578–585. doi:10.1097/00007632-199403000-00014
Polikeit, A., Nolte, L. P., and Ferguson, S. J. (2003). The effect of cement augmentation on the load transfer in an osteoporotic functional spinal unit finite-element analysis. Spine 28 (10), 991–996. doi:10.1097/01.brs.0000061987.71624.17
Qian, J., Li, C. G., Yin, X. C., Chen, C., Zheng, H. Y., Zhu, Y. G., et al. (2022). Polyetheretherketone versus titanium rods used in pedicle screw fixation for lumbar degenerative diseases. Orthop. J. China 30 (9), 1–5. doi:10.3977/j.issn.1005-8478.2022.09.06
Sato, T., Yonezawa, I., Todo, M., Takano, H., and Kaneko, K. (2018). Biomechanical effects of implant materials on posterior lumbar interbody fusion: Comparison of polyetheretherketone and titanium spacers using finite element analysis and considering bone density. J. Biomed. Sci. Eng. 11 (04), 45–59. doi:10.4236/jbise.2018.114005
Sengupta, D. K., and Herkowitz, H. N. (2012). Pedicle screw-based posterior dynamic stabilization: Literature review. Adv. Orthop. 2012, 1–7. doi:10.1155/2012/424268
Shim, C. S., Park, S. W., Lee, S. H., Lim, T. J., Chun, K., and Kim, D. H. (2008). Biomechanical evaluation of an interspinous stabilizing device, locker. Locker. Spine (Phila Pa 1976) 33 (22), E820–E827. doi:10.1097/brs.0b013e3181894fb1
Stavros, O., Johannes, G., Jan, B., Madita, E., Andreas, P., Horst, F., et al. (2020). Biomechanical effects of posterior pedicle screw-based instrumentation using titanium versus carbon fiber reinforced PEEK in an osteoporotic spine human cadaver model. Clin. Biomech. 80, 105153. ISSN 0268-0033. doi:10.1016/j.clinbiomech.2020.105153
Takahashi, S., Hoshino, M., Yasuda, H., Hori, Y., Ohyama, S., Terai, H., et al. (2019). Characteristic radiological findings for revision surgery after balloon kyphoplasty. Sci. Rep. 9, 18513–18517. doi:10.1038/s41598-019-55054-5
Tan, Q., Liu, Z., Zhao, Y., Huang, X. y., Bai, H., Yang, Z., et al. (2021). Biomechanical comparison of four types of instrumentation constructs for revision surgery in lumbar adjacent segment disease: A finite element study. Comput. Biol. Med. 134, 104477. doi:10.1016/j.compbiomed.2021.104477
Wang, W., Baran, G. R., Garg, H., Betz, R. R., Moumene, M., and Cahill, P. J. (2014). The benefits of cement augmentation of pedicle screw fixation are increased in osteoporotic bone: AFinite element analysis. Spine deform. 2 (4), 248–259. doi:10.1016/j.jspd.2014.03.002
Yeager, M. S., Cook, D. J., and Cheng, B. C. (2015). In vitro comparison of dynesys, PEEK, and titanium constructs in the lumbar spine. Adv. Orthop. 2015, 895931. doi:10.1155/2015/895931
Zhang, J., and Rong, Q. (2020). Effect of new titanium alloy on biomechanical behavior of dental implant. J. Syst. Simul. 32 (11), 2100–2104. doi:10.16182/j.issn1004731x.joss.19-FZ0521
Keywords: screw, finite element analysis, biomechanics, PEEK, vertebra-pediculoplasty
Citation: Wang Y-N, Ren Y-N, Han J, Chen C, Sun X, Di M-Y, Dou Y-M, Ma X-L, Wang Z, Du C-F and Yang Q (2023) Biomechanical effects of screws of different materials on vertebra-pediculoplasty: a finite element study. Front. Bioeng. Biotechnol. 11:1225925. doi: 10.3389/fbioe.2023.1225925
Received: 20 May 2023; Accepted: 21 June 2023;
Published: 29 June 2023.
Edited by:
Xijin Hua, University of Exeter, United KingdomReviewed by:
Xuesong Zhu, The First Affiliated Hospital of Soochow University, ChinaJun Zou, Soochow University, China
Copyright © 2023 Wang, Ren, Han, Chen, Sun, Di, Dou, Ma, Wang, Du and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng-Fei Du, ZGRjY2ZiMzFAaG90bWFpbC5jb20=; Qiang Yang, eWFuZ3FpYW5nMTk4MEAxMjYuY29t
†These authors have contributed equally to this work
 Yan-Ni Wang1†
Yan-Ni Wang1† Xun Sun
Xun Sun Ming-Yuan Di
Ming-Yuan Di Yi-Ming Dou
Yi-Ming Dou Xin-Long Ma
Xin-Long Ma Zheng Wang
Zheng Wang Qiang Yang
Qiang Yang