- 1Department of Orthopedics (Friedrichsheim), University Hospital Frankfurt, Goethe University Frankfurt, Frankfurt, Germany
- 2Dr. Rolf M. Schwiete Research Unit for Osteoarthritis, Department of Orthopedics (Friedrichsheim), University Hospital Frankfurt, Goethe University Frankfurt, Frankfurt, Germany
Osteoarthritis of the hip is a common condition that affects older adults. Total hip replacement is the end-stage treatment to relief pain and improve joint function. Little is known about the mechanical load distribution during the activity of bipedal stance, which is an important daily activity for older adults who need to rest more frequently. This study investigated the distribution of the hip and knee joint moments during bipedal stance in patients with unilateral hip osteoarthritis and how the distribution changed 1 year after total hip replacement. Kinematic and kinetic data from bipedal stance were recorded. External hip and knee adduction moments were calculated and load distribution over both limbs was calculated using the symmetry angle. Preoperatively, the non-affected limb carried 10% more body weight than the affected limb when standing on two legs. Moreover, the mean external hip and knee adduction moments of the non-affected limb were increased compared to the affected limb. At follow-up no significant differences were observed between the patients’ limbs. Preoperative and postoperative changes in hip adduction moment were mainly explained by the combination of the vertical ground reaction force and the hip adduction angle. Stance width also explained changes in the hip and knee adduction moments of the affected leg. Furthermore, as with walking, bipedal standing also showed an asymmetric mechanical load distribution in patients with unilateral hip osteoarthritis. Overall, the findings suggest the need for preventive therapy concepts that focus not only on walking but also on optimizing stance towards a balanced load distribution of both legs.
1 Introduction
Osteoarthritis (OA) is a leading cause of disability and imposes societal costs in older adults (Hunter and Bierma-Zeinstra, 2019). It is even more prevalent than in previous decades due to an ageing and increasingly obese population. Primary total hip replacement (THR) is the standard treatment for end-stage hip OA, providing pain relief and improved joint function. The demand and volume of this procedure is predicted to increase in the coming years due to higher demand for improved mobility and quality of life in the aging population (Maradit Kremers et al., 2015).
In patients with unilateral hip OA, a pain-induced protective walking pattern results in uneven loading of the lower extremities. Pathological moments in the hip and knee joint during walking have been noted (Hurwitz et al., 1997; Shakoor et al., 2011; Schmidt et al., 2017). Despite good clinical-functional outcomes (Neuprez et al., 2020), some studies found that gait kinematics (i.e., reduced hip extension) and kinetics (i.e., lower knee adduction moments) did not normalize after THR (Foucher et al., 2007; Stief et al., 2018). The development of OA in the hip joint has been shown to be related to increased joint loading during walking (Hurwitz et al., 2001). In this context, the external hip adduction moment (HAM) has been identified as one of the most important determinants of hip contact force and joint loading (Lenaerts et al., 2009; Wesseling et al., 2015). Peak external knee adduction moments (KAM) are associated with the rate of progression and severity of knee OA (Sharma et al., 1998; Miyazaki et al., 2002). Patients with hip OA have also been shown to have altered lower limb joint mechanics during sit-to-stand tasks (Eitzen et al., 2014; Abujaber et al., 2015) and stair climbing (Queen et al., 2015), suggesting that these activities may contribute to the development of OA in adjacent joints (Jungmann et al., 2015; Joseph et al., 2016).
Although standing is an important activity of daily living (Morlock et al., 2001), there is limited information on lower extremity mechanical load distribution in patients with unilateral hip OA. It appears that patients with unilateral hip OA shift more weight to the non-affected leg during standing (Talis et al., 2008; Miura et al., 2018). However, in these studies, leg loading is expressed only as asymmetry between the legs or as uneven distribution of vertical ground reaction force between the legs. There is no information on the hip or knee joint moments of the affected and non-affected leg, nor is there detailed information on what factors influence asymmetrical leg loading. When walking on flat surfaces, patients with unilateral hip OA use compensatory strategies (i.e., greater foot progression angle and increased lateral trunk displacement toward the affected side) that directly affect HAM and KAM (Schmidt et al., 2017). It is therefore reasonable to assume that some of these compensatory strategies also occur during bipedal standing. If this is the case, the symmetry of lower limb joint moments may also be affected. Characteristic gait changes to unload the affected limb include increased lateral trunk displacement (LTD) toward the affected side (Reininga et al., 2012), altered foot progression angle (FPA) at the affected limb (Müller et al., 2012) and increased stride width (Stief et al., 2021). Information on these compensatory strategies for bipedal standing is missing, although their effects on lower limb joint moments may have implications for rehabilitation of patients with hip OA. Rehabilitation focusing on motor control to move and stand more symmetrically could be applied to patients with hip OA and after THR to modify motor strategies (Boonstra et al., 2011). This is in line with Hunter and Bierma-Zeinstra (2019), who stated that management of OA should shift from reactive to proactive and preventive measures.
The aim of the present study was to investigate load distribution before THR and the improvement in load distribution after THR during bipedal standing in patients with unilateral hip OA and finally to examine whether kinematic and kinetic variables in general and compensatory strategies in particular correlate with significant changes in joint loading. It was expected that before THR, the non-affected limb would experience greater lower limb joint moments than the affected limb in patients with unilateral hip OA. Furthermore, it was hypothesized that joint loading asymmetries in patients with unilateral hip OA would differ from those in a healthy control (HC) group and would be due in part to changes in kinematic and kinetic variables.
2 Methods
In the present study, data from patients who had participated in previous prospective studies in our clinic were analyzed (Schmidt et al., 2017; Stief et al., 2018; van Drongelen et al., 2019; van Drongelen et al., 2020). In these studies, gait analysis and radiography were performed preoperatively and 1 year after THR. The complete protocol for these studies has been described previously (Stief et al., 2018; van Drongelen et al., 2019). In addition, data from HCs with a similar age distribution that were available in our database were used for comparison.
2.1 Participants
Symptomatic patients with radiologically confirmed unilateral hip OA (Kellgren-Lawrence > 2) between the age of 30 and 80 years, who were scheduled for and received THR were considered for inclusion. Exclusion criteria were: OA of lower limb joints other than the affected hip, chronic or neuromuscular diseases, history of orthopedic surgery of the lower extremities, and use of assistance devices during walking. Only data from patients who had three valid trials of two-leg-standing measured during gait analysis in the week before and 1 year after surgery were included. Patients with a body mass index (BMI) > 35 kgm−2 were excluded from the analyses. Finally, data from 43 patients were included in the study (Table 1).
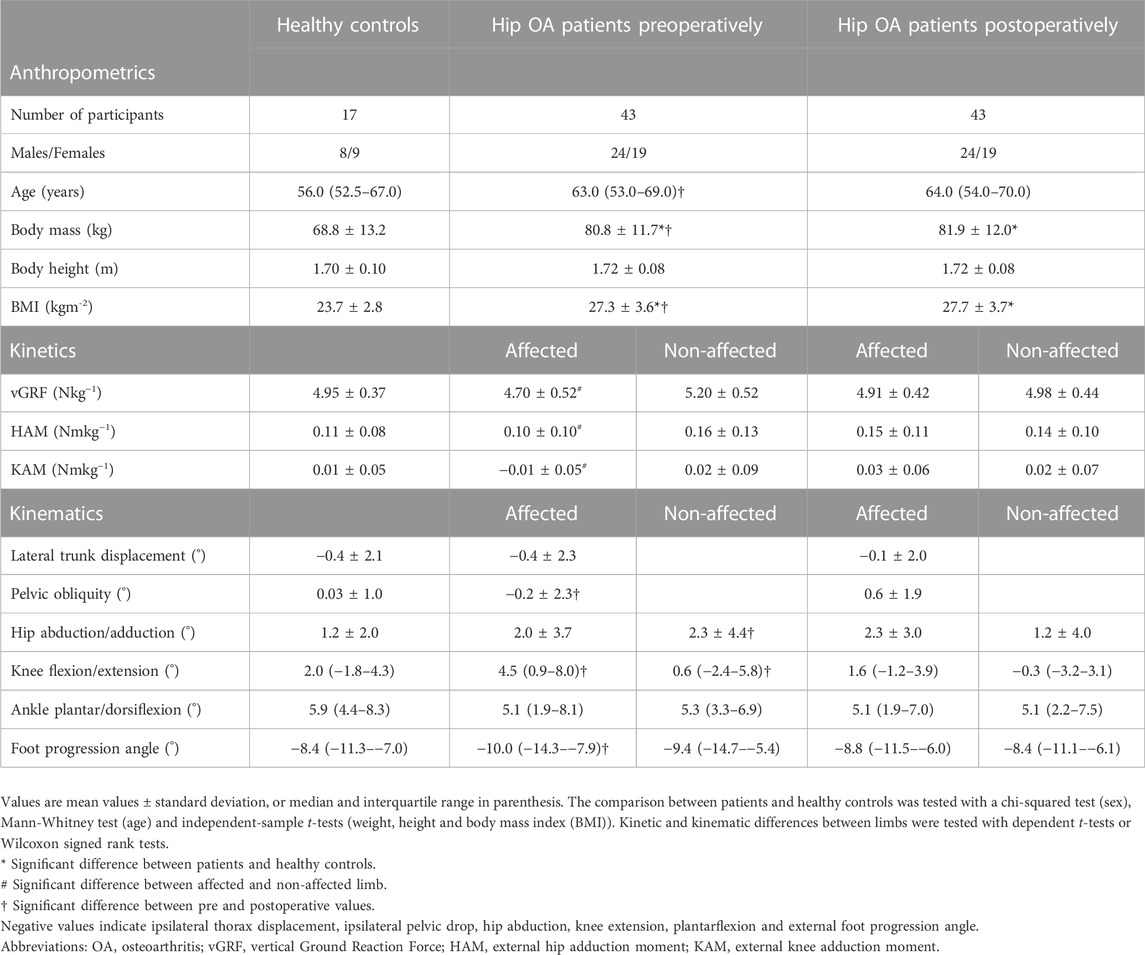
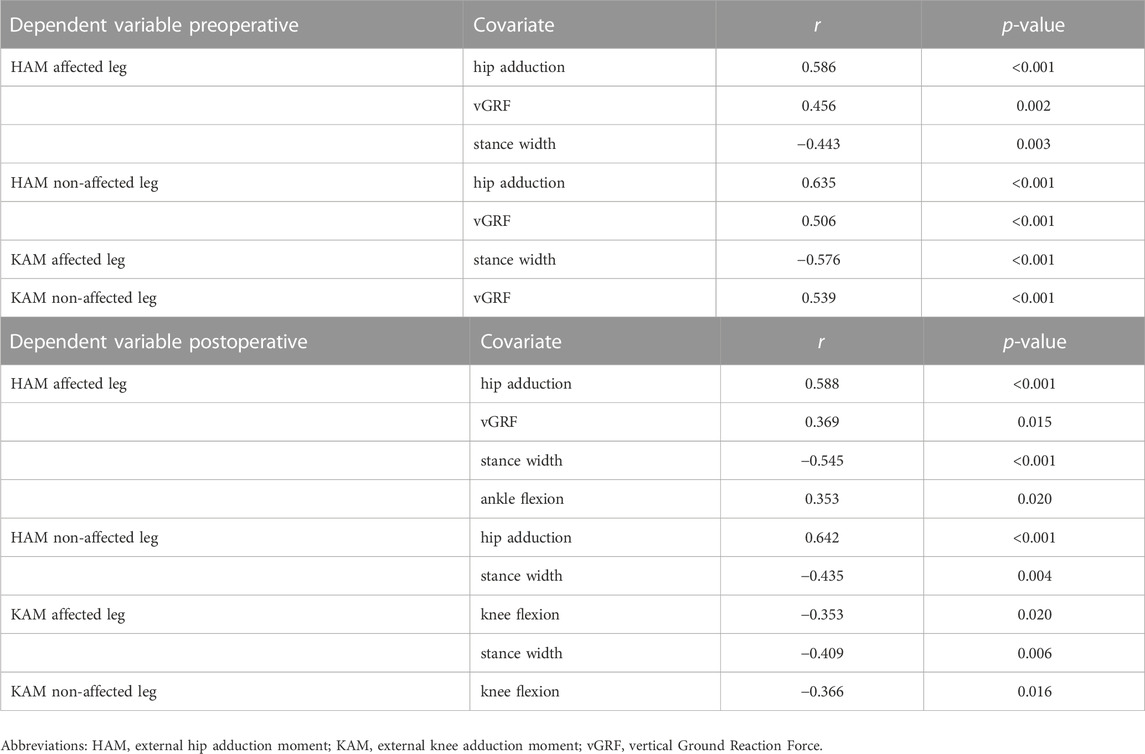
TABLE 1. Anthropometric data, kinetic data and kinematic data of patients with unilateral hip osteoarthritis and healthy controls.
Seventeen participants with a similar age distribution were included as a HC collective for comparison (Table 1). Control participants were included if they had no history of orthopedic surgeries or chronic and neuromuscular disease. All patients and HCs provided written informed consent prior to participation in the original studies. The protocol was approved by the Medical Ethics Committee of the Department of Medicine, Goethe University Frankfurt (reference number 122/14 and 497/15).
2.2 Bipedal standing
An 8-camera Vicon System operating at 200 Hz (8MX T10 cameras, VICON Motion Systems, Oxford, United Kingdom) collected kinematic data, synchronously with the two force plates (Advanced Mechanical Technology, Inc., Watertown, MA, United States). Reflective markers (14 mm) were placed on anatomical landmarks according to the standardized Plug-in-Gait marker set (Kadaba et al., 1990): pelvis (anterior and posterior superior iliac spines), upper leg (lateral thigh and lateral femoral condyle), lower leg (lateral shank and lateral malleolus), foot (heel and toe), shoulder (acromion) and thorax (sternum and spine). To improve the reliability and accuracy of the gait data in the frontal plane, additional markers were placed on the medial malleolus, medial femoral condyle and greater trochanter (Stief et al., 2013). The hip joint center was determined using a geometrical prediction method by Harrington (Harrington et al., 2007).
For the measurement, all participants were instructed to stand comfortably (barefoot) on their two legs for 10 s, with each foot resting on one of two force plates and arms at their sides. To achieve a natural balanced posture, no further instructions were given except when the thigh and pelvic markers were not visible, participants were asked to abduct their arms slightly.
Kinematic and kinetic data were exported to MATLAB for further analysis (version R2022a, The Mathworks Inc., Natick, MA, United States). The following kinematic outcome variables, based on the characteristic gait strategies (Schmidt et al., 2017), were extracted (Baker et al., 2018): mean LTD, mean pelvic obliquity, mean hip adduction, mean knee flexion/extension angle, mean ankle plantar/dorsiflexion angle and mean FPA. Here, negative LTDs refer to lateral displacements of the trunk with respect to the corresponding limb. Pelvic obliquity was negative when the pelvis dropped with respect to the corresponding limb. Adduction of the hip in the frontal plane was defined as a positive angle. Positive values for the knee indicated flexed knees, while negative values for the ankle indicated a plantar flexed ankle joint. FPA was defined as the angle of the long axis of the foot segment relative to the global coordinate system. Negative FPAs here indicate externally rotated feet. External joint moments were calculated from the force plate data and the mathematically derived joint centers by inverse dynamics analysis (Davis et al., 1991). Mean vertical ground reaction forces (vGRFs) of each limb and mean joint moments in the frontal plane for the hip and the knee joint (HAMs, KAMs) were normalized by body mass. Stance width was calculated as the distance between the ankle joint centers.
2.3 Symmetry angle
To quantify inter-limb symmetry with respect to vGRFs, HAMs, and KAMs, the symmetry angle (SA) was calculated using the following equation from Zifchock et al. (2008).
Where XL and XR represent left/affected and right/non-affected limb values, respectively. SA values of 0% indicate perfect symmetry. SA values of 100% indicate two values that are opposite but equal in magnitude. The direction of asymmetry (indicated by a positive or negative value) was ignored and absolute values were used (Zifchock et al., 2008).
2.4 Statistical analyses
Statistical analyses were performed using SPSS Statistics (IBM SPSS Statistics for Windows, version 29, IBM Corp., Armonk, NY, United States). Shapiro-Wilk tests and visual inspection of Q-Q plots were used to check for normal distribution. Normally distributed parameters were compared with respect to differences between limbs (dependent t-test), groups (independent t-tests), and over time (dependent t-test). When data were not normally distributed, parameters were compared using Wilcoxon signed rank tests (differences between limbs and over time) and Mann-Whitney U-Tests (differences between groups). A chi-squared test was used to compare the sex distribution between groups.
The left and right sides of the HCs were randomized to a single-leg HC group for comparison with patients. Because significant HAM and KAM changes were expected in patients with unilateral hip OA, regression analysis was performed to determine predictor variables that best explained these changes. Pearson correlation coefficients were calculated to determine significant correlations between kinematic and kinetic predictor variables and HAMs and KAMs, respectively (Bortz, 1999). A stepwise multiple regression analysis was then performed if two or more parameters significantly correlated with the frontal external hip and knee joint moments. Secondary, a forward multiple regression analysis was performed using only the known compensatory strategy parameters (LTD, FPA and stance width). The level of significance was α = 0.05.
3 Results
Participant demographics are listed in Table 1. Patients were measured preoperatively and at a mean follow-up of 12.6 ± 2.5 months after surgery. The patients had significantly higher body mass and BMI compared to HCs, at preoperatory measure (80.8 vs. 68.8 kg, p < 0.001; 27.3 vs. 23.7 kgm−2; p < 0.001, respectively) and during follow-up (81.9 vs. 68.8 kg, p < 0.001; 27.7 vs. 23.7 kgm−2; p < 0.001, respectively). No differences were observed in age (preoperatory 63.0 vs. 56.0 years/postoperatory 64.0 vs. 56.0 years, p > 0.237), height (1.72 vs. 1.70 m, p > 0.379) or sex distribution (24 males and 19 females vs. 8 males and 9 females, p = 0.540) between the patients and HCs (Table 1). HCs stood with a stance width of 18.3 ± 4.3 cm, whereas patients stood with a stance width of 20.5 ± 4.3 cm before surgery and 20.1 ± 4.3 cm after surgery. The differences between HCs and patients were not significant (p > 0.074). Age (p < 0.001), body mass (p = 0.002) and BMI (p = 0.003) were significantly higher when postoperative anthropometrics were compared with preoperative values.
3.1 Kinetics and symmetry
Preoperatively, the non-affected limb carried more body weight than the affected limb in patients with unilateral hip OA (p = 0.003), as expressed by the vGRF (Table 1). In addition, greater HAMs (p = 0.007) and KAMs (p = 0.018) were found for the non-affected limb than for the affected limb. Postoperatively, no differences were found between the affected and non-affected sides (Table 1). Furthermore, no differences were found between HCs and patients pre- or postoperatively.
During bipedal standing, no significantly increased symmetry angles (vGRF, HAM and KAM) were observed in the patients with unilateral hip OA compared with the HCs (Figure 1). Preoperatively, the symmetry angles were all higher for the patients and postoperatively the values all became smaller, but the differences between the patients and HCs never reached significance.
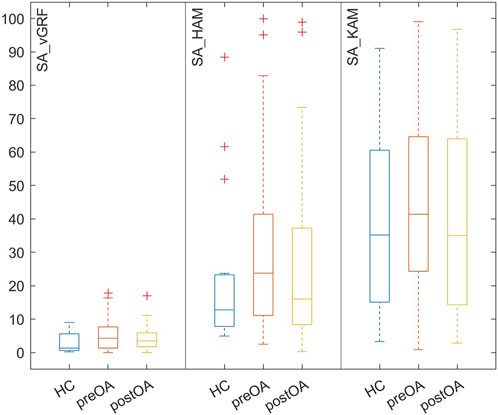
FIGURE 1. Box-and-whisker-plots of the absolute angles of symmetry (SA) of the vertical ground reaction force (vGRF) and external frontal hip (HAM) and knee (KAM) joint moments in healthy controls (HCs) and patients with hip osteoarthritis both preoperatively (preOA) and postoperatively (postOA).
3.2 Kinematics
When considering the kinematics of patients with hip OA while standing on two legs (Table 1), it was found that the affected limb showed no difference from the non-affected limb both preoperatively and postoperatively. No differences were observed between HCs and patients, either preoperatively or postoperatively. Small significant changes were seen in the preoperative to postoperative comparison. The affected foot was less externally rotated, and the knees were less flexed or even extended after THR. In addition, the pelvis was no longer dropped to the affected side; postoperatively the pelvis dropped to the non-affected side with a corresponding change in hip adduction angle on the non-affected side.
3.3 Correlations and regression
All significant correlations to joint loading parameters (HAM and KAM) are shown in Table 2. Preoperatively, hip adduction angle and vGRF were significantly correlated with HAM in both the affected and non-affected limb. A significant correlation with stance width was also found for the affected limb. A significant correlation was found between KAM and stance width in the affected limb, and between KAM and vGRF in the non-affected limb.
Postoperatively, the same significant correlations with HAM were found for the affected limb (hip adduction angle, vGRF and stance width). There was also a significant correlation with the ankle plantarflexion angle. For the non-affected limb, significant correlations with HAM were found for hip adduction angle and stance width. KAM significantly correlated with knee flexion for both the affected and the non-affected limb. A significant correlation with stance width was also found for the affected leg.
Preoperative regression analysis revealed that changes in hip adduction angle and vGRFs explained 42% of HAM changes (R2 = 0.418; F = 14.360; p < 0.001) for the affected limb. Stance width did not significantly improve the outcome using this model (∆R2 = 0.037, ∆F = 2.673, p = 0.110). In the non-affected limb changes in hip adduction angle and vGRFs explained 61% of HAM changes (R2 = 0.612; F = 31.569; p < 0.001).
Postoperatively, the regression analysis yielded a model in which hip adduction angle and vGRF explained 42% of HAM alterations (R2 = 0.417; F = 14.310; p < 0.001). Adding stance width (likely due to relatively high correlation to hip adduction) and ankle flexion to the model did not result in a significant increase in the percentage of variance in HAM predicted by the model. For the non-affected limb, hip adduction angle explained 41% of the changes in HAM (R2 = 0.413; F = 28.808; p < 0.001), and adding stance width did not significantly increase the outcome using this model (∆R2 = 0.014, ∆F = 1.004, p = 0.322). For the affected leg only 16% of the changes in KAM were explained by the changes in stance width (R2 = 0.167; F = 8.245; p = 0.006), the inclusion of the knee flexion angle did not significantly increase the percentage of variance in KAM predicted by the model (∆R2 = 0.062, ∆F = 3.198, p = 0081).
Multiple regression analysis with only known parameters of the compensatory strategies showed that only stance width explained part of the variation of the external joint moments in the frontal plane (see Table 2). The other parameters (LTD and FPA) did not significantly improve the outcome using any of the models.
4 Discussion
Altered joint moments in individuals with unilateral hip OA may contribute to the development of OA in adjacent joints (Jungmann et al., 2015). To identify possible abnormal joint moments in the knee and hip joint during standing, this study quantified weight distribution and lower limb joint moments in individuals with unilateral hip OA during bipedal standing before (preoperatively) and 1 year after THR (postoperatively). The results of the current study suggest that weight distribution favoring the affected limb and few kinematic adjustments in the affected limb enable patients with unilateral hip OA to stand comfortably while standing on two legs before THR. At a mean follow-up of 12.6 months, asymmetries in joint loading were no longer present.
4.1 Kinetics and symmetry
To avoid pain caused by the affected hip, individuals with unilateral hip OA appear to adopt an altered bipedal standing position (Figure 2), resulting in a redistribution of lower limb joint moments. As previously noted, the non-affected limb carried more body weight than the affected limb in patients with unilateral hip OA (Talis et al., 2008; Miura et al., 2018). The non-affected limb experienced 38% greater HAMs than the affected limb, indicating a pathological loading of the hip joint. KAM tended to be a valgus moment in the affected limb, which denoted that the vertical GRF vector was slightly lateral from the estimated knee joint center rather than slightly medial, which has been shown to be physiological during walking (Cerny, 1984). During walking, patients with unilateral hip OA exhibited pathological peak external KAM and HAM in the non-affected limb (Hurwitz et al., 1997; Shakoor et al., 2011; Schmidt et al., 2017; Stief et al., 2018). Therefore, it has been suggested that the non-affected limb is at higher risk for developing OA in these joints (Hurwitz et al., 2001). Comparable results have been obtained during sit-to-stand tasks (Eitzen et al., 2014; Abujaber et al., 2015) and stair climbing (Queen et al., 2015).
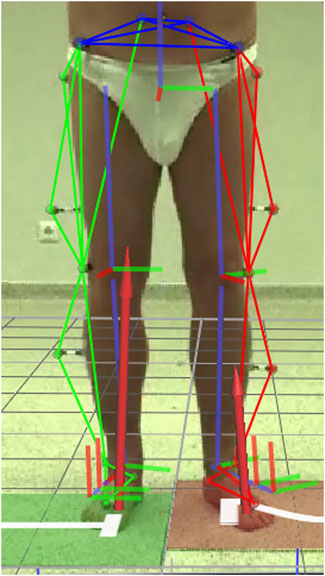
FIGURE 2. Patient with unilateral hip osteoarthritis (preoperatively) in a standing position with a frequently observed extended external foot rotation on the affected (left) side. Kinematic segments and ground reaction force are superimposed on the image.
Miura et al. (2018) showed that the load distribution of the operated leg was restored as early as 1 month after surgery. In the present study it was found that the load distribution and corresponding joint moments had no asymmetries between limbs at a follow-up of 12.6 months on average. Postoperative joint moments were significantly different from preoperative values [i.e., HAM appeared to be 33% higher in the affected leg after surgery (0.15 vs. 0.10 Nmkg−1)]. No differences were observed compared with HCs. Studies also found increased HAM during walking compared to HCs (Stief et al., 2018), although in general, peak HAM values were usually lower but not significantly reduced after THR compared to HCs (Ewen et al., 2012). The increase in HAM may be due to the absence of pain and the resultant increase in vGRF after THR. However, whether other factors such as an altered moment arm due to repositioning of the hip joint center during THR surgery play a role requires further investigation.
4.2 Kinematics and correlations
In this study, it was hypothesized that patients with unilateral hip OA adopt a standing position that is significantly different from HCs to reduce the moments in the affected hip joint. However, HAMs in the affected limb were not reduced compared to normal, which partly explains the lack of significant kinematic changes compared with HCs. For example, during walking, patients with unilateral hip OA significantly bend their trunk toward the affected side (Bennett et al., 2007; Reininga et al., 2012). Consequently, HAM in the affected limb was significantly reduced during gait (Hurwitz et al., 1997; Foucher et al., 2007; Shakoor et al., 2011; Foucher and Wimmer, 2012). When standing on two legs, patients with hip OA showed minimal LTD to the affected side, which was not significantly different from HCs. Bending of the trunk towards the affected limb during bipedal standing may be detrimental in terms of postural stability or even non-feasible while at the same time the non-affected limb carries proportionally more body weight. Preoperatively, the foot of the affected limb was significantly more externally rotated during bipedal stance (Figure 2; Table 1) while the knee was more flexed (Table 1) when compared with the postoperative standing position, but not when compared with HCs. Although these kinematic changes during standing did not relate to changes in HAM, they appear to be adopted by patients with unilateral hip OA to unload the affected limb in terms of body weight distribution. Increased FPAs and knee flexion changes are typical of patients with unilateral hip OA during walking (Bennett et al., 2007; Müller et al., 2012; Schmitt et al., 2015). Previous studies on HCs have shown that large changes in LTD (Mündermann et al., 2008) and FPA (Andrews et al., 1996) are required to significantly reduce KAMs during walking. Hip adduction and plantar/dorsiflexion angle of the ankle are known control variables of sway in the medio-lateral and anterior-posterior directions, respectively (Weaver et al., 2017). Therefore, it makes sense that these variables are predictors of the hip joint moments during stance. In the present study, no kinematic differences were found between the affected and non-affected limb. The relatively small kinematic changes observed in the affected limb may be the reason why kinematics did not explain the KAM alterations preoperatively. It appears that vGRF, hip adduction and knee flexion angle explain most of the variance in HAM and KAM. However, stance width also showed correlations to HAM and KAM and since increased stance width influences hip adduction angle, stance width indirectly contributes to explain the variance. When only compensation parameters were considered, stance width was the only parameter that mattered: stance width explained 18.9%–29.7% of the variance of HAM and 16.7%–33.2% of the variance of KAM (Table 2). From walking it is known that increasing stride width reduces knee and hip joint moments in the frontal plane (Stief et al., 2021), so increasing stance width could be a simple adaptation with a reducing effect on knee and hip joint moments in the frontal plane during standing.
4.3 Limitations
This study should be considered in the context of its limitations. Only variables that have been shown to correlate with external KAM and HAM during walking were examined. However, it is likely that patients with unilateral hip OA modify additional kinematic and kinetic parameters to stand comfortably on two legs. In addition, factors such as pain, leg length discrepancy, and pelvic or spinopelvic malalignment have been suggested to contribute toasymmetric loading (Miura et al., 2018) and were not investigated in the current study.
KAM was found to be very small because the GRF was centered on the center of rotation of the knee joint, in contrast to gait where the GRF is directed medially from the center of rotation of the knee joint (Cerny, 1984). Therefore, KAM and consequently the SA for KAM may not be the best parameters for assessing knee loading during bipedal standing. Although knee and hip joint moments in the frontal plane during dynamic activities have been widely used as an indicator of knee joint loading and to characterize intrinsic compressive loading, this parameter itself may not be sufficient to predict the mechanical properties of the cartilage, especially during standing. Therefore, future studies are needed to analyze possible relationships between knee and hip joint loading parameters and compressive properties of joint cartilage, i.e., a combination of musculoskeletal and finite element models (Harlaar et al., 2022).
5 Conclusion
In summary, our elderly patients with unilateral hip OA adopted a standing position preoperatively in which foot progression (more externally rotated) and knee flexion (more flexed) were adapted in the affected limb compared to the postoperative standing position. However, these kinematic adaptations did not explain the lower HAM and KAM in the affected limb compared with the non-affected limb. The non-affected limb experienced 38% greater HAMs than the affected limb, indicating pathological loading of the hip joint during normal standing. Postoperatively, limb load distribution and corresponding joint loads normalized, comparable to findings during walking. The altered preoperative joint moments were mainly caused by a disproportionate weight distribution, expressed by the vGRF, in favor of the affected limb. Of the compensation strategy parameters, stance width showed moderate to high correlations with HAM and KAM and also explained up to 33% of the variance. Therefore, in patients with hip OA, interdisciplinary preventive therapy concepts in which stance width could play a role should be considered to improve the loading situation.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of the Faculty of Medicine of the Goethe University Frankfurt. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SD and FS were involved in the design of the study. SD carried out the data analysis. SD, JH, and FS were involved in the interpretation and discussion of the results. SD took the lead in writing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the German Research Foundation (DFG) (Project number: 492686079). Sponsor had no involvement in this article.
Acknowledgments
The authors would like to thank Hanna Kaldowski and André Schmidt for their help with the data collection and data preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abujaber, S. B., Marmon, A. R., Pozzi, F., Rubano, J. J., and Zeni, J. A. (2015). Sit-to-stand biomechanics before and after total hip arthroplasty. J. Arthroplasty 30, 2027–2033. doi:10.1016/j.arth.2015.05.024
Andrews, M., Noyes, F. R., Hewett, T. E., and Andriacchi, T. P. (1996). Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: A critical analysis of the reliability of gait analysis data. J. Orthop. Res. 14, 289–295. doi:10.1002/jor.1100140218
Baker, R., Leboeuf, F., Reay, J., and Sangeux, M. (2018). “The conventional gait model - success and limitations,” in Handbook of human motion. Editors B. Müller, and S. I. Wolf (Cham: Springer International Publishing), 1–19.
Bennett, D., Ogonda, L., Elliott, D., Humphreys, L., Lawlor, M., and Beverland, D. (2007). Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard-incision hip arthroplasty: A prospective blinded study. J. Arthroplasty 22, 490–495. doi:10.1016/j.arth.2006.02.173
Boonstra, M. C., Schreurs, B. W., and Verdonschot, N. (2011). The sit-to-stand movement: Differences in performance between patients after primary total hip arthroplasty and revision total hip arthroplasty with acetabular bone impaction grafting. Phys. Ther. 91, 547–554. doi:10.2522/ptj.20090376
Davis, R. B., Õunpuu, S., Tyburski, D., and Gage, J. R. (1991). A gait analysis data collection and reduction technique. Hum. Mov. Sci. 10, 575–587. doi:10.1016/0167-9457(91)90046-z
Eitzen, I., Fernandes, L., Nordsletten, L., Snyder-Mackler, L., and Risberg, M. A. (2014). Weight-bearing asymmetries during sit-to-stand in patients with mild-to-moderate hip osteoarthritis. Gait Posture 39, 683–688. doi:10.1016/j.gaitpost.2013.09.010
Ewen, A. M., Stewart, S., St Clair Gibson, A., Kashyap, S. N., and Caplan, N. (2012). Post-operative gait analysis in total hip replacement patients-a review of current literature and meta-analysis. Gait Posture 36, 1–6. doi:10.1016/j.gaitpost.2011.12.024
Foucher, K. C., Hurwitz, D. E., and Wimmer, M. A. (2007). Preoperative gait adaptations persist one year after surgery in clinically well-functioning total hip replacement patients. J. Biomech. 40, 3432–3437. doi:10.1016/j.jbiomech.2007.05.020
Foucher, K. C., and Wimmer, M. A. (2012). Contralateral hip and knee gait biomechanics are unchanged by total hip replacement for unilateral hip osteoarthritis. Gait Posture 35, 61–65. doi:10.1016/j.gaitpost.2011.08.006
Harlaar, J., Macri, E. M., and Wesseling, M. (2022). Osteoarthritis year in review 2021: Mechanics. Osteoarthr. Cartil. 30, 663–670. doi:10.1016/j.joca.2021.12.012
Harrington, M. E., Zavatsky, A. B., Lawson, S. E., Yuan, Z., and Theologis, T. N. (2007). Prediction of the hip joint centre in adults, children, and patients with cerebral palsy based on magnetic resonance imaging. J. Biomech. 40, 595–602. doi:10.1016/j.jbiomech.2006.02.003
Hunter, D. J., and Bierma-Zeinstra, S. (2019). Osteoarthritis. Lancet 393, 1745–1759. doi:10.1016/s0140-6736(19)30417-9
Hurwitz, D. E., Hulet, C. H., Andriacchi, T. P., Rosenberg, A. G., and Galante, J. O. (1997). Gait compensations in patients with osteoarthritis of the hip and their relationship to pain and passive hip motion. J. Orthop. Res. 15, 629–635. doi:10.1002/jor.1100150421
Hurwitz, D. E., Sumner, D. R., and Block, J. A. (2001). Bone density, dynamic joint loading and joint degeneration. Cells Tissues Organs 169, 201–209. doi:10.1159/000047883
Joseph, G. B., Hilton, J. F., Jungmann, P. M., Lynch, J. A., Lane, N. E., Liu, F., et al. (2016). Do persons with asymmetric hip pain or radiographic hip OA have worse pain and structure outcomes in the knee opposite the more affected hip? Data from the Osteoarthritis Initiative. Osteoarthr. Cartil. 24, 427–435. doi:10.1016/j.joca.2015.10.001
Jungmann, P. M., Nevitt, M. C., Baum, T., Liebl, H., Nardo, L., Liu, F., et al. (2015). Relationship of unilateral total hip arthroplasty (THA) to contralateral and ipsilateral knee joint degeneration - a longitudinal 3T MRI study from the Osteoarthritis Initiative (OAI). Osteoarthr. Cartil. 23, 1144–1153. doi:10.1016/j.joca.2015.03.022
Kadaba, M. P., Ramakrishnan, H. K., and Wootten, M. E. (1990). Measurement of lower extremity kinematics during level walking. J. Orthop. Res. 8, 383–392. doi:10.1002/jor.1100080310
Lenaerts, G., Mulier, M., Spaepen, A., Van der Perre, G., and Jonkers, I. (2009). Aberrant pelvis and hip kinematics impair hip loading before and after total hip replacement. Gait Posture 30, 296–302. doi:10.1016/j.gaitpost.2009.05.016
Maradit Kremers, H., Larson, D. R., Crowson, C. S., Kremers, W. K., Washington, R. E., Steiner, C. A., et al. (2015). Prevalence of total hip and knee replacement in the United States. J. Bone Jt. Surg. Am. 97, 1386–1397. doi:10.2106/jbjs.n.01141
Miura, N., Tagomori, K., Ikutomo, H., Nakagawa, N., and Masuhara, K. (2018). Leg loading during quiet standing and sit-to-stand movement for one year after total hip arthroplasty. Physiother. Theory Pract. 34, 529–533. doi:10.1080/09593985.2017.1422203
Miyazaki, T., Wada, M., Kawahara, H., Sato, M., Baba, H., and Shimada, S. (2002). Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann. Rheum. Dis. 61, 617–622. doi:10.1136/ard.61.7.617
Morlock, M., Schneider, E., Bluhm, A., Vollmer, M., Bergmann, G., Müller, V., et al. (2001). Duration and frequency of every day activities in total hip patients. J. Biomech. 34, 873–881. doi:10.1016/s0021-9290(01)00035-5
Müller, M., Schwachmeyer, V., Tohtz, S., Taylor, W. R., Duda, G. N., Perka, C., et al. (2012). The direct lateral approach: Impact on gait patterns, foot progression angle and pain in comparison with a minimally invasive anterolateral approach. Arch. Orthop. Trauma. Surg. 132, 725–731. doi:10.1007/s00402-012-1467-x
Mündermann, A., Asay, J. L., Mündermann, L., and Andriacchi, T. P. (2008). Implications of increased medio-lateral trunk sway for ambulatory mechanics. J. Biomech. 41, 165–170. doi:10.1016/j.jbiomech.2007.07.001
Neuprez, A., Neuprez, A. H., Kaux, J. F., Kurth, W., Daniel, C., Thirion, T., et al. (2020). Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin. Rheumatol. 39, 861–871. doi:10.1007/s10067-019-04811-y
Queen, R. M., Attarian, D. E., Bolognesi, M. P., and Butler, R. J. (2015). Bilateral symmetry in lower extremity mechanics during stair ascent and descent following a total hip arthroplasty: A one-year longitudinal study. Clin. Biomech. 30, 53–58. doi:10.1016/j.clinbiomech.2014.11.004
Reininga, I. H., Stevens, M., Wagenmakers, R., Bulstra, S. K., Groothoff, J. W., and Zijlstra, W. (2012). Subjects with hip osteoarthritis show distinctive patterns of trunk movements during gait-a body-fixed-sensor based analysis. J. Neuroeng Rehabil. 9, 3. doi:10.1186/1743-0003-9-3
Schmidt, A., Meurer, A., Lenarz, K., Vogt, L., Froemel, D., Lutz, F., et al. (2017). Unilateral hip osteoarthritis: The effect of compensation strategies and anatomic measurements on frontal plane joint loading. J. Orthop. Res. 35, 1764–1773. doi:10.1002/jor.23444
Schmitt, D., Vap, A., and Queen, R. M. (2015). Effect of end-stage hip, knee, and ankle osteoarthritis on walking mechanics. Gait Posture 42, 373–379. doi:10.1016/j.gaitpost.2015.07.005
Shakoor, N., Dua, A., Thorp, L. E., Mikolaitis, R. A., Wimmer, M. A., Foucher, K. C., et al. (2011). Asymmetric loading and bone mineral density at the asymptomatic knees of patients with unilateral hip osteoarthritis. Arthritis Rheum. 63, 3853–3858. doi:10.1002/art.30626
Sharma, L., Hurwitz, D. E., Thonar, E. J., Sum, J. A., Lenz, M. E., Dunlop, D. D., et al. (1998). Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 41, 1233–1240. doi:10.1002/1529-0131(199807)41:7<1233::aid-art14>3.0.co;2-l
Stief, F., Böhm, H., Michel, K., Schwirtz, A., and Döderlein, L. (2013). Reliability and accuracy in three-dimensional gait analysis: A comparison of two lower body protocols. J. Appl. Biomech. 29, 105–111. doi:10.1123/jab.29.1.105
Stief, F., Holder, J., Feja, Z., Lotfolahpour, A., Meurer, A., and Wilke, J. (2021). Impact of subject-specific step width modification on the knee and hip adduction moments during gait. Gait Posture 89, 161–168. doi:10.1016/j.gaitpost.2021.07.008
Stief, F., Schmidt, A., van Drongelen, S., Lenarz, K., Froemel, D., Tarhan, T., et al. (2018). Abnormal loading of the hip and knee joints in unilateral hip osteoarthritis persists two years after total hip replacement. J. Orthop. Res. 36, 2167–2177. doi:10.1002/jor.23886
Talis, V. L., Grishin, A. A., Solopova, I. A., Oskanyan, T. L., Belenky, V. E., and Ivanenko, Y. P. (2008). Asymmetric leg loading during sit-to-stand, walking and quiet standing in patients after unilateral total hip replacement surgery. Clin. Biomech. 23, 424–433. doi:10.1016/j.clinbiomech.2007.11.010
van Drongelen, S., Kaldowski, H., Fey, B., Tarhan, T., Assi, A., Stief, F., et al. (2020). Determination of leg alignment in hip osteoarthritis patients with the EOS® system and the effect on external joint moments during gait. Appl. Sci. 10, 7777. doi:10.3390/app10217777
van Drongelen, S., Kaldowski, H., Tarhan, T., Assi, A., Meurer, A., and Stief, F. (2019). Are changes in radiological leg alignment and femoral parameters after total hip replacement responsible for joint loading during gait? BMC Musculoskelet. Disord. 20, 526. doi:10.1186/s12891-019-2832-5
Weaver, T. B., Glinka, M. N., and Laing, A. C. (2017). Stooping, crouching, and standing - characterizing balance control strategies across postures. J. Biomech. 53, 90–96. doi:10.1016/j.jbiomech.2017.01.003
Wesseling, M., de Groote, F., Meyer, C., Corten, K., Simon, J. P., Desloovere, K., et al. (2015). Gait alterations to effectively reduce hip contact forces. J. Orthop. Res. 33, 1094–1102. doi:10.1002/jor.22852
Keywords: posture, ground reaction forces, external hip adduction moment, external knee adduction moment, symmetry angle
Citation: van Drongelen S, Holder J and Stief F (2023) Lower limb joint loading in patients with unilateral hip osteoarthritis during bipedal stance and the effect of total hip replacement. Front. Bioeng. Biotechnol. 11:1190712. doi: 10.3389/fbioe.2023.1190712
Received: 21 March 2023; Accepted: 06 June 2023;
Published: 16 June 2023.
Edited by:
Juan Ramírez, National University of Colombia, Medellin, ColombiaReviewed by:
Vasilios (Bill) Baltzopoulos, Liverpool John Moores University, United KingdomWillians Fernando Vieira, Massachusetts General Hospital and Harvard Medical School, United States
Abdelwahed Barkaoui, International University of Rabat, Morocco
Copyright © 2023 van Drongelen, Holder and Stief. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: S. van Drongelen, c3RlZmFuLnZhbmRyb25nZWxlbkBrZ3UuZGU=
†Present address: J. Holder, University of Salzburg, Department of Sport and Exercise Science, Salzburg, Austria
 S. van Drongelen
S. van Drongelen J. Holder
J. Holder F. Stief
F. Stief