- Shanghai Key Laboratory of Orthopaedic Implants, Department of Orthopaedic Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
Aims: In revision total hip arthroplasty (THA), large acetabular bone defects pose challenges for surgeons. Recently, wide application of trabecular tantalum, which has outstanding biocompatibility and mechanical properties, and the development of three-dimensional (3D) printing have led to the introduction of new schemes for acetabular reconstruction. However, few studies have focused on the treatment of bone defects with customized 3D-printed titanium augments combined with tantalum trabecular cup. Thus, we aimed to evaluate the effect of this therapy in patients who underwent revision THAs.
Patients and Methods: We included 23 patients with Paprosky type III acetabular bone defects who underwent revision THA between January 2013 and June 2019. The preoperative hip rotation center and functional score were compared with those at 2–7 years (average 4.7 years) postoperatively to evaluate the midterm prognosis of our treatment choice.
Results: Postoperatively, the rotation centres of all hips were comparable with those of the contralateral hips. Hip function improved with average Harris Hip Score improved from 33.5 (22.7–40.2) to 86.1 (73.5–95.6) and average Oxford Hip Score improved from 8.3 (0–14) to 38.8 (35–48) during follow-up. One dislocation, which occurred due to extreme hip flexion within 6 weeks, was treated with closed reduction, and no recurrent dislocation occurred. No nerve injury, infection, aseptic loosening, or osteolysis were observed and no re-revision was performed in any patient.
Conclusion: Satisfactory midterm outcomes were obtained with 3D-printed titanium augment combined with tantalum cup for the treatment of acetabular defects in revision THA. Changes in the Harris Hip Score and Oxford Hip Score suggested a significant improvement in hip function.
Introduction
Currently, the number of revision hip arthroplasties is increasing rapidly (Schwartz et al., 2016; Gwam et al., 2017). Acetabulum reconstruction by filling the bone defect, initial stability of the prosthesis, and restoration of the hip rotation center are the main objectives of revision surgery (Johnston et al., 1979). In patients with severe bone defects, inadequate and poor-quality residual bone poses challenges to surgeons in terms of providing effective support for prosthesis reconstruction (Knight et al., 1993). Currently, reconstruction of acetabular bone defects are reconstructed using structural allografts, antiprotrusion cages, augments, bone impaction grafting with metal meshes, and customized triflange component (Jain et al., 2014; Baauw et al., 2016). Augments can effectively fill acetabular bone defects, and satisfactory long-term results have been reported (Del Gaizo et al., 2012; Xiao et al., 2021).
Recently, customized implants fabricated using three-dimensional (3D) printing have been applied in clinical practice (Geng et al., 2020; Zampelis and Flivik, 2020). In patients with complex and irregular acetabular defects, 3D printing and rapid prototyping (RP) can be used to fabricate customized prostheses. Since computed tomography (CT) and design of augments can be completed in an outpatient setting, patients’ hospital stay and costs are reduced (Mao et al., 2015; Li et al., 2016).
Tantalum is an ideal implant material with excellent histocompatibility (Bobyn et al., 2004; Levine B. et al., 2006; Weeden and Schmidt, 2007), and previous studies have proven that tantalum does not induce rejection and can effectively promote bone integration (Bobyn et al., 1999; Mrosek et al., 2009; Wei et al., 2016). Additionally, tantalum has excellent mechanical properties including a high friction coefficient. Trabecular tantalum has an elastic modulus similar to that of subchondral bone, which is conducive to the adhesion and growth of osteoblasts, and promotes long-term osteogenesis (Bobyn et al., 1980; Findlay et al., 2004; Meneghini et al., 2010; Wei et al., 2016).
Although 3D printing, RP, and tantalum have been used in clinical practice for many years, there are no reports on the combined application of a tantalum trabecular cup and a 3D-printed titanium augment to the best of our knowledge. Therefore, we retrospectively evaluated whether combined therapy could: 1. effectively reconstruct severe acetabular defects and improve function; 2. restore the hip rotation center; and 3. reduce the occurrence of complications such as aseptic loosening, osteolysis and infection during midterm follow-up.
Methods
Study Participants
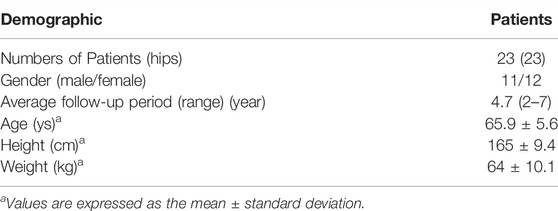
This study was approved by the Ethics Committee of our institution. The medical records of all patients who underwent revision total hip arthroplasty (THA) between January 2013 and June 2019 were retrospectively reviewed. Patients with severe acetabular defects in whom difficulty existted in providing effective support with off-the-shelf augments and cups based on RP-assisted simulative surgery evaluation were included. The detailed evaluation process was similar to that in a previous study (Zhang et al., 2021). A total of 310 patients underwent revision THA, of whom 72 were classified as Paprosky type III. After excluding 49 patients who received other revision schemes (25 cases of cages and 24 cases of conventional augments), 23 patients who received 3D-printed titanium augments combined with tantalum trabecular cups were included. Among them, 17 and six patients were further classified as subtypes IIIA and IIIB, respectively. Demographic statistics are presented in Table 1. The Paprosky classification was proposed by surgeons having >15 years of experience in joint surgery who perform >200 arthroplasties each year (ZZ and HL). The exclusion criteria were as follows: 1. patients with mild bone defects (Paprosky types I and II), 2. patients receiving revision for infections and other causes with no acetabular defects, 3. patients receiving revision THAs without 3D-printed augments and tantalum cups, and 4. patients who refused to participate in our study.
3D-Printed Augment Design
All patients underwent pelvic CT before surgery. Pelvic CT was performed with patients in the supine position with 0.625-mm slices. All CT scans were performed in same medical imaging centre using the same parameters.
Mimics software was used to obtain a digital 3D-reconstructed model of the pelvis from the CT data. During reconstruction, doctors and engineers cooperate to identify effective bone mass to overcome influence of metal artifact and ensure the accuracy of model. Debridement and reaming were predicted and simulated during 3D-reconstruction and a life-size 3D model of the pelvis was printed using stereolithography. Installation simulation was performed on the RP by surgeons with >15 years of experience in joint surgery as mentioned above. Off-the-shelf cups and augments were preferred when they could be properly supported by the host bone. Otherwise, customized prosthesis was considered. Based on the clinical condition, two different strategies were applied. If the anteroinferior and posteroinferior acetabular bone was intact, the defect was reconstructed using a customized augment to support the acetabular cup. A customized cage or even a semi-pelvic prosthesis was considered when anteroinferior and posteroinferior acetabular structure were damaged and even a high risk of pelvic discontinuity exists.
Three points need to be considered while designing customized augments as we discussed in our related work (Li et al., 2013; Li et al., 2016):
1. Ensure reliable fixation of the augment to the host bone to fill bone defects. For a cavity defect, shape matching could be adopted to hold augment with surrounding host bone and we could strengthen fixation with screws if necessary. For an uncontained defect, it is necessary to design augment with flange and fix it with screws. The specific fixation area and location are determined based on the situation of bone defect and host bone presented in the rapid prototype.
2. Ensure effective stress conduction in load-bearing areas, which host in the posterosuperior part of acetabulum. Ideally, augment effectively fills the space between cup and host bone in load-bearing area to facilitate load-bearing stress transmission directly through augment. In such cases, rotational shear stress of cup is converted into compressive stress of augment.
3. The contact surfaces of the augment and cup must be matched with pre-planned cup size and allows for a bigger or smaller one size. Cup size may vary from preoperative plan (Wang et al., 2018) and the augment must therefore be designed to allow adjustment of the cup size.
Customized augments were printed using Ti6Al4V powder as a raw material using the selective laser melting technique. Size and shape of customized augments were determined by experienced surgeons (ZZ and HL) through simulation surgery. The printing process was completed in 1 day and printed augments were verified preoperatively using RP. The augment design is shown in Figure 1 and procedures for RP evaluation and trial installation are illustrated in Figure 2.
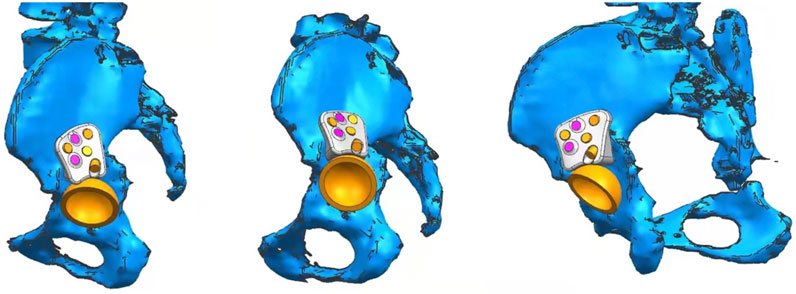
FIGURE 1. Design of customized augment from different angles. Reliable fixation and effective stress conduction were achieved between host bone and augment.
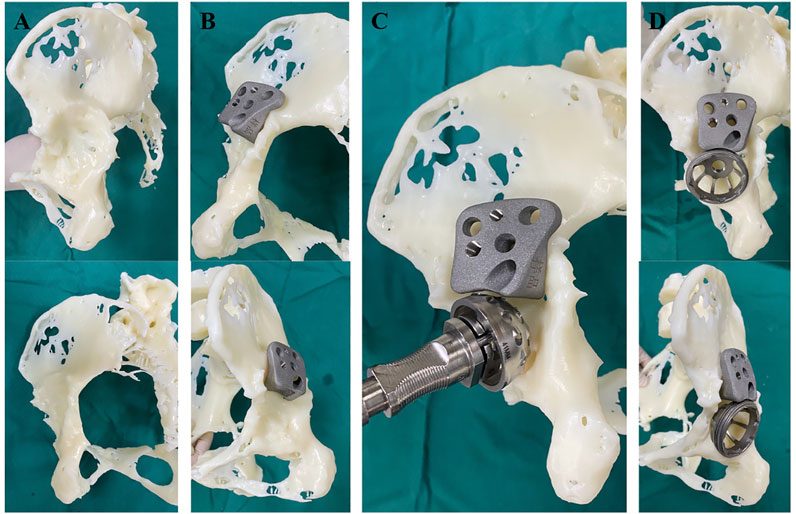
FIGURE 2. Procedure of rapid prototype-assisted evaluation. (A). Reconstruction of a patient’s pelvic with rapid prototype. (B). 3D-printed augment could achieve enough contact with host bone. (C). Acetabulum was further filed to host acetabular cup. (D). Enough contact surface was achieved between cup, augment and host bone. Acetabular defect was filled with this combined therapy.
Surgical Techniques
The revision procedures were performed by ZZ and HL using the posterolateral approach. During the preoperative RP trial installation, we evaluated whether the augment could effectively hold the cup together with the residual host bone; thereafter the customized augment was implanted and fixed with screws if necessary. If screw fixation was required, locking screws were used first to avoid positional changes in the augment compared to the trial installation. Bone cement was used between the augment and cup. The cup was fixed with screws after press fit, and morselized bone graft was packed to fill the remaining defect when needed.
Postoperative Care
For the first 2–6 weeks after surgery, patients were allowed no or limited toe-touch weightbearing ambulation. After 6 weeks, patients were allowed partial weightbearing with crutches, and full weightbearing was allowed after 3 months.
Radiographic and Clinical Outcomes
Radiographs and CT scans of all included patients before and after revision surgery were collected. Additionally, anteroposterior and lateral radiographs were taken at 3 weeks, 6 weeks, 3 months, 6 months, and 1 year after surgery and annually thereafter.
The inclination of the cup and hip rotation center were measured on postoperative CT images as shown in Figure 3. On the prosthesis side, 5–7 points were marked on the cambered surface of the prosthesis cup to define a circular plane of orientation of the cup. Based on the circular plane and shape of cup, a concentric ball attached to the cup was reconstructed, and the centre of the ball was defined as the centre of rotation. On the contralateral side, similar approach was applied and the centre of the ball reconstructed by marking the acetabulum was defined as the centre of rotation.
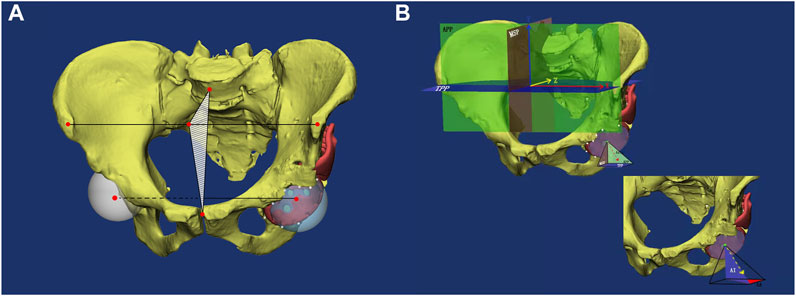
FIGURE 3. A diagram to illustrate choice of reference film, rotation center and measurement of anteversion and abduction angle. (A). Midsagittal plane and reconstruction of rotation center. White points were chosen around cup surface as markers to help reconstruct rotation center (two red points in acetabulum). Midsagittal plane was determined by midpoint of bilateral anterosuperior iliac spines, center of pubic symphysis and the midpoint of fifth lumbar vertebra. (B). Three reference films and the measurement of anteversion and abduction angle of cup. APP: anterior pelvic plane. MSP: midsagittal plane. TPP: transverse pelvic plane. AA: anatomic anteversion. AI: anatomic inclination.
Selection of Reference Planes
The anterior plane was defined as a plane passing through the bilateral anterosuperior iliac spines and the midpoint of the pubic symphysis. The horizontal plane was defined as a plane passing through the bilateral anterosuperior iliac spines and perpendicular to the anterior plane. The midsagittal plane was defined as a plane through the midpoint of the bilateral anterosuperior iliac spines and perpendicular to the horizontal and anterior planes.
For measurement of the relative position of the centres of rotation, vertical lines were drawn from the centres of rotation on both sides to the midsagittal plane, and the difference in their lengths was calculated as the relative mediolateral relationship between the two centres of rotation; similarly, the relative anteroposterior and superoinferior relationships were defined by calculating the difference between the lengths of vertical lines perpendicular to the anterior and horizontal planes, respectively.
For measurement of the anteversion and abduction angles, a circle fitting the outer edge of the acetabular cup was marked. The anteversion and abduction angles were defined as the projection angles between the normal plane of the fitting circle and the anterior pelvic plane and horizontal plane of pelvis, respectively.
The Harris hip score and Oxford score are functional scores to assess pain, deformity, and function of the hip after surgery and are widely used to evaluate the success of revision (Harris, 1969; Murray et al., 2007). Motion range and deformity section in Harris hip score were evaluated independently by three researchers at each follow-up.
The overall survival of revision prostheses and occurrence of complications were recorded. Cup loosening was defined as described in a previous study (Li et al., 2016). Migration of prostheses was determined by comparing radiographs taken at the last follow-up with those taken immediately postoperatively. Definite loosening was defined as acetabular migration of ≥2 mm with implant rotation or screw breakage. Probable loosening was defined as a radiolucent line >1 mm through all three acetabular zones without any signs of migration, rotation, or screw breakage. Osteolysis surrounding the components was evaluated using the DeLee and Charnley and Gruen methods (DeLee and Charnley, 1976; Gruen et al., 1979). Cup loosening and osteolysis were evaluated independently by three experienced surgeons.
Statistical Analysis
Quantitative data with normal distribution are presented as means with ranges, and categorical variables are presented as percentages. Statistical analysis was conducted using SPSS version 17.0 for windows (SPSS Inc., Chicago, IL, United States). Paired Student’s t-test was used to compare the Harris hip score and Oxford hip score. Two-sided p < 0.05 was considered statistically significant. Using the power analysis software PASS 16 (NCSS, LLC. Kaysville, Utah, United States), all the tests in this study with a sample size of 23 participants own a statistical power of more than 0.9 at a two-sided 5% level of significance.
Results
The Harris hip scores before surgery and at the last follow-up were 33.5 ± 11 (22.7–40.2) and 86.1 ± 19 (73.5–95.6), respectively (p < 0.001). Similarly, the Oxford scores before surgery and at the last follow-up were 8.3 ± 2.6 (0–14) and 38.8 ± 1.7 (35–48), respectively (p < 0.001).
Compared with the contralateral side, the centre of rotation was displaced 3.7 ± 3.3 mm (0.3–7.0 mm) upward postoperatively. The absolute anteroposterior displacement was 4.1 ± 6.4 mm (0.7–9.6 mm); however, the actual displacement ranged from −9.6 to + 5.4 mm (-, posterior; +, anterior). The absolute mediolateral displacement was 2.7 ± 3.4 mm (0.3–9.9 mm), and the actual displacement ranged from −9.9 to + 2.2 mm (-, medial; +, lateral).
The anteversion angle of the cup was 15.8 ± 15.4° (−4.2–27.5°), and the abduction angle was 47.7 ± 8.5° (35–60.8°).
Regarding complications, no deep infection or nerve injury were observed during the follow-up. One case of dislocation occurred within 6 weeks after surgery. Posterior dislocation of the hip occurred when the patient bent to pick up things, which caused extreme flexion of the hip joint. The anteversion angle of the acetabular cup was 24.2°, and the anteversion angle of the femur was 23.4° with an abduction angle of 47.6°. After successful closed reduction and 3 weeks’ rest on bed, no recurrent dislocation was observed during the follow-up. No obvious prosthesis loosening and periprosthetic osteolysis, according to our standards defined above, were noted radiographically during the follow-up. No re-revision was performed during our follow-up.
Discussion
Tantalum trabecular augment combined with cup has been used in clinical practice for years and studies have proved its long-term prognosis (Whitehouse et al., 2015; Löchel et al., 2019). In the study by Whitehouse et al (Whitehouse et al., 2015), which had a minimum follow-up of 10 years, the overall survival was 92%, and at the last follow-up, a normal centre of rotation was restored in 90% of patients with a high hip rotation center preoperatively. Different sizes of augment can provide support for the acetabular cup in most bone defects (Issack, 2013; Ting-Xian et al., 2017). However, in some complex bone defects, it is difficult to accurately restore the hip rotation center using a conventional augment combined with an acetabular cup (Xiao et al., 2021). In addition, the variability in defect shape in patients with severe defects often leads to a poor fit of the augment to the defect. Customized 3D-printed prosthesis can precisely match the shape of bone defect, thus restoring the hip rotation center (Hughes et al., 2017). Dion et al. (2020) reported the application of 3D-printed augments in revision total knee arthroplasty and showed better fixture stability than that with conventional therapy. Fu et al. (2020) demonstrated the satisfactory biocompatibility and biomechanical features of a customized augment in a swine model with acetabular defect. Titanium is the most commonly used metal for 3D printing, and use of a 3D-printed customized titanium augment with a tantalum cup combines the bone ingrowth performance of tantalum with the ability of 3D-printed augments to restore the hip rotation center. Thus, all defects were effectively reconstructed in revision surgery based on intraoperative evaluation and satisfactory functional outcomes.
New technologies, such as 3D printing and RP, which have developed rapidly in the recent years (Hughes et al., 2017; Loganathan et al., 2020), help surgeons to visualize local bone defects, design customized implants, and permit preoperative simulation and surgical planning (Li et al., 2013; Li et al., 2016; Zhang et al., 2021). A trial installation is important, and surgeons should ensure the most effective position to stabilize the acetabular cup. A locking screw should be used first to fix the augment position. A representative case is shown in Figure 4. Thus, the amount of intraoperative bleeding and operation time can be significantly reduced (Hughes et al., 2017). In our study, RP was applied for designing and precise positioning of the augment during surgery. RP-assisted pre-operative planning could effectively guide augment implantation during revision THA, and RP-assisted implantation of augments greatly increased the accuracy of restoring centre of rotation (Xiao et al., 2021). In our study, a relatively normal hip rotation center was restored in all patients after surgery. Further, compared with the contralateral side, the hip rotation center was displaced upward by an average of 3.7 mm postoperatively. The average absolute anteroposterior and mediolateral displacement was 4.1 and 2.7 mm, respectively. Compared with those of other studies using conventional augments (Grappiolo et al., 2015; Xiao et al., 2021), our results show a more satisfactory restoration of the hip rotation center. Xiao et al. (2021) reported a wide variation in vertical hip centre distance ranging from 11.7 to 42.9 mm and a horizontal distance from 20.8 to 49.2 mm postoperatively. Moreover, two patients had a high hip rotation center. However, in revision THA in patients with severe bone defects, the placement of the cup is largely restricted by the quality of the residual bone since adequate initial stability is highly emphasized in revision surgery. The installation of a cage is less restricted due to the flexibility of the iliac wings. Therefore, there is some variation in the hip rotation center position and cup anteversion angle in our results. In this study, only one patient suffered a posterior dislocation during early rehabilitation. Since the 24.2° anteversion and 47.6° abduction angles of the cup are within the respective normal ranges, we believe this dislocation was not related to the anteversion and abduction of the cup. The scar tissues around the hip were widely excised during revision, which resulted in loose soft tissues around the prosthesis. Additionally, the dislocation occurred when the patient bent the body to pick up things. Thus, the dislocation probably occurred because of excessive flexion of the hip during movement.
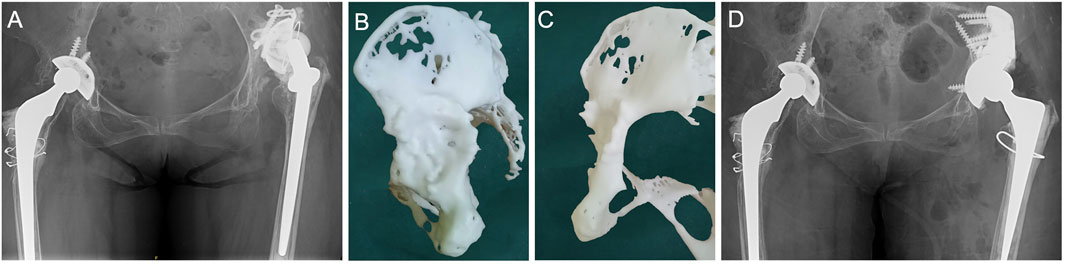
FIGURE 4. A representative patient receiving this combined therapy. (A) Preoperative AP pelvic x-ray of this patient. (B,C) Rapid prototype reconstruction of this patient’s acetabulum. (D) Postoperative AP pelvic x-ray taken 3 years after revision surgery. Reproduced with permission from authors (Zhang et al., 2022).
Theoretically, wear and fretting corrosion will occur when different interface metals rub against each other in the electrolyte environment in vivo, especially in the assembled prosthesis (Brown et al., 2006). Thus, the friction between the titanium and cobalt-chromium alloy will produce metal ions. Back et al. (2005) reported that the levels of cobalt and chromium ions increased continuously in the first 6 months and remained high during a 2-years follow-up. The increase in local metal ion concentrations may cause osteolysis (Back et al., 2005; Delaunay et al., 2010). In our patients, friction between titanium and tantalum may lead to corrosion. However, no osteolysis was detected at the midterm follow-up, and no symptoms of metal ion accumulation such as local pain and inflammatory pseudotumor were noted (Liow and Kwon, 2017). This could be attributed to the fact that the tantalum cup and titanium augment are fixed using bone cement for less peri-implant stress shielding, which isolates the components. Moreover, tantalum is highly inert and relatively corrosion resistant (Levine B. R. et al., 2006).
Our study had some limitations. First, this was a retrospective study without a control group. Severe acetabular defects are challenging for most surgeons, and conventional augments cannot be used for complex cases; thus, it was difficult to define a control group. However, our findings provide sufficient evidence to prove the midterm effectiveness and safety of our approach. Second, due to the limited number of cases of severe acetabular defects treated in our institution, the number of cases included in this study was relatively small. Therefore, multi-centre studies with larger study cohorts are required in the future.
Conclusion
Concurrent use of a 3D-printed augment and tantalum trabecular cup combines the advantages of both, such as the customization of 3D printing and biocompatibility and osteo-induction ability of tantalum. Using this strategy, we could effectively reconstruct severe acetabular defects during surgery Harris hip scores increased, and the survival rate was high with no revision at an average follow-up of 4.7 years.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Medical Ethics Committee of Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conception and design: HL, JZ; Administrative support: HL; Provision of study materials or patients: JZ, HL; Collection and assembly of data: KK, CZ, YC, and HQ; Data analysis and interpretation: KK, CZ, YH; Manuscript writing: All authors Final approval of manuscript.
Funding
This study was sponsored by the National Natural Science Foundation of China (Grant No. 31900941 and 82072397), Interdisciplinary Program of Shanghai Jiao Tong University (project No. ZH2018QNA06) and Shanghai Municipal Education Commission Two-hundred Talent.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
references
Baauw, M., van Hooff, M. L., and Spruit, M. (2016). Current Construct Options for Revision of Large Acetabular Defects: A Systematic Review. JBJS Rev. 4 (11), e2. doi:10.2106/JBJS.RVW.15.00119
Back, D. L., Young, D. A., and Shimmin, A. J. (2005). How Do Serum Cobalt and Chromium Levels Change after Metal-On-Metal Hip Resurfacing? Clin. Orthop. Relat. Res. 438, 177–181. doi:10.1097/01.blo.0000166901.84323.5d
Bobyn, J. D., Pilliar, R. M., Cameron, H. U., and Weatherly, G. C. (1980). The Optimum Pore Size for the Fixation of Porous-Surfaced Metal Implants by the Ingrowth of Bone. Clin. Orthop. Relat. Res. 150, 263. doi:10.1097/00003086-198007000-00045
Bobyn, J. D., Poggie, R. A., Krygier, J. J., Lewallen, D. G., Hanssen, A. D., Lewis, R. J., et al. (2004). Clinical Validation of a Structural Porous Tantalum Biomaterial for Adult Reconstruction. J. Bone & Jt. Surg. 86-A Suppl 2, 123–129. doi:10.2106/00004623-200412002-00017
Bobyn, J. D., Stackpool, G. J., Hacking, S. A., Tanzer, M., and Krygier, J. J. (1999). Characteristics of Bone Ingrowth and Interface Mechanics of a New Porous Tantalum Biomaterial. J. Bone Jt. Surg. Br. 81 (5), 907–914. doi:10.1302/0301-620x.81b5.0810907
Brown, C., Fisher, J., and Ingham, E. (2006). Biological Effects of Clinically Relevant Wear Particles from Metal-On-Metal Hip Prostheses. Proc. Inst. Mech. Eng. H. 220 (2), 355–369. doi:10.1243/095441105x63291
Del Gaizo, D. J., Kancherla, V., Sporer, S. M., and Paprosky, W. G. (2012). Tantalum Augments for Paprosky IIIA Defects Remain Stable at Midterm Followup. Clin. Orthop. Relat. Res. 470 (2), 395–401. doi:10.1007/s11999-011-2170-x
Delaunay, C., Petit, I., Learmonth, I. D., Oger, P., and Vendittoli, P. A. (2010). Metal-on-metal Bearings Total Hip Arthroplasty: The Cobalt and Chromium Ions Release Concern. Orthop. Traumatology Surg. Res. 96 (8), 894–904. doi:10.1016/j.otsr.2010.05.008
DeLee, J. G., and Charnley, J. (1976). Radiological Demarcation of Cemented Sockets in Total Hip Replacement. Clin. Orthop. Relat. Res. 121, 20–32. doi:10.1097/00003086-197611000-00003
Dion, C., Yamomo, G., Howard, J., Teeter, M., Willing, R., and Lanting, B. (2020). Revision Total Knee Arthroplasty Using a Novel 3D Printed Titanium Augment: A Biomechanical Cadaveric Study. J. Mech. Behav. Biomed. Mater. 110 (8), 103944. doi:10.1016/j.jmbbm.2020.103944
Findlay, D. M., Welldon, K., Atkins, G. J., Howie, D. W., Zannettino, A. C. W., and Bobyn, D. (2004). The Proliferation and Phenotypic Expression of Human Osteoblasts on Tantalum Metal. Biomaterials 25 (12), 2215–2227. doi:10.1016/j.biomaterials.2003.09.005
Fu, J., Xiang, Y., Ni, M., Qu, X., Zhou, Y., Hao, L., et al. (2020). In Vivo Reconstruction of the Acetabular Bone Defect by the Individualized Three-Dimensional Printed Porous Augment in a Swine Model. Biomed Res. Int. 2020, 4542302. doi:10.1155/2020/4542302
Geng, X., Li, Y., Li, F., Wang, X., Zhang, K., Liu, Z., et al. (2020). A New 3D Printing Porous Trabecular Titanium Metal Acetabular Cup for Primary Total Hip Arthroplasty: a Minimum 2-year Follow-Up of 92 Consecutive Patients. J. Orthop. Surg. Res. 15 (1), 383. doi:10.1186/s13018-020-01913-1
Grappiolo, G., Loppini, M., Longo, U. G., Traverso, F., Mazziotta, G., and Denaro, V. (2015). Trabecular Metal Augments for the Management of Paprosky Type III Defects Without Pelvic Discontinuity. J. Arthroplasty 30 (6), 1024–1029. doi:10.1016/j.arth.2015.01.001
Gruen, T. A., McNeice, G. M., and Amstutz, H. C. (1979). “Modes of Failure” of Cemented Stem-type Femoral Components: A Radiographic Analysis of Loosening. Clin. Orthop. Relat. Res., 17–27. doi:10.1097/00003086-197906000-00002
Gwam, C. U., Mistry, J. B., Mohamed, N. S., Thomas, M., Bigart, K. C., Mont, M. A., et al. (2017). Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J. Arthroplasty 32, 2088–2092. doi:10.1016/j.arth.2017.02.046
Harris, W. H. (1969). Traumatic Arthritis of the Hip after Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty. An End-Result Study Using a New Method of Result Evaluation. J. Bone & Jt. Surg. 51 (4), 737–755. doi:10.2106/00004623-196951040-00012
Hughes, A. J., DeBuitleir, C., Soden, P., O’Donnchadha, B., Tansey, A., Abdulkarim, A., et al. (2017). 3D Printing Aids Acetabular Reconstruction in Complex Revision Hip Arthroplasty. Adv. Orthop. 2017, 8925050. doi:10.1155/2017/8925050
Issack, P. S. (2013). Use of Porous Tantalum for Acetabular Reconstruction in Revision Hip Arthroplasty. J. Bone & Jt. Surg. Am. 95 (21), 1981–1987. doi:10.2106/jbjs.l.01313
Jain, S., Grogan, R. J., and Giannoudis, P. V. (2014). Options for Managing Severe Acetabular Bone Loss in Revision Hip Arthroplasty. A Systematic Review. Hip Int. 24 (2), 109–122. doi:10.5301/hipint.5000101
Johnston, R. C., Brand, R. A., and Crowninshield, R. D. (1979). Reconstruction of the Hip. A Mathematical Approach to Determine Optimum Geometric Relationships. J. Bone. Jt. Surg. 61 (5), 639–652. doi:10.2106/00004623-197961050-00001
Knight, J. L., Fujii, K., Atwater, R., and Grothaus, L. (1993). Bone-grafting for Acetabular Deficiency During Primary and Revision Total Hip Arthroplasty. A Radiographic and Clinical Analysis. J. arthroplasty 8 (4), 371–382. doi:10.1016/s0883-5403(06)80035-5
Levine, B. R., Sporer, S., Poggie, R. A., Della Valle, C. J., and Jacobs, J. J. (2006). Experimental and Clinical Performance of Porous Tantalum in Orthopedic Surgery. Biomaterials 27 (27), 4671–4681. doi:10.1016/j.biomaterials.2006.04.041
Levine, B., Della Valle, C. J., and Jacobs, J. J. (2006). Applications of Porous Tantalum in Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 14 (12), 646–655. doi:10.5435/00124635-200611000-00008
Li, H., Qu, X., Mao, Y., Dai, K., and Zhu, Z. (2016). Custom Acetabular Cages Offer Stable Fixation and Improved Hip Scores for Revision THA With Severe Bone Defects. Clin. Orthop. Relat. Res. 474 (3), 731–740. doi:10.1007/s11999-015-4587-0
Li, H., Wang, L., Mao, Y., Wang, Y., Dai, K., and Zhu, Z. (2013). Revision of Complex Acetabular Defects Using Cages with the Aid of Rapid Prototyping. J. Arthroplasty 28 (10), 1770–1775. doi:10.1016/j.arth.2012.12.019
Liow, M. H. L., and Kwon, Y.-M. (2017). Metal-on-metal Total Hip Arthroplasty: Risk Factors for Pseudotumours and Clinical Systematic Evaluation. Int. Orthop. (SICOT) 41 (5), 885–892. doi:10.1007/s00264-016-3305-1
Löchel, J., Janz, V., Hipfl, C., Perka, C., and Wassilew, G. I. (2019). Reconstruction of Acetabular Defects with Porous Tantalum Shells and Augments in Revision Total Hip Arthroplasty at Ten-Year Follow-Up. Bone & Jt. J. 101-B (3), 311–316. doi:10.1302/0301-620x.101b3.bjj-2018-0959.r1
Loganathan, B., Sharma, V., Kumar, M. R., Soundarapandian, S., Marothi, D. P. S., and Sharma, K. (2020). Acetabulum Reconstruction with TantalumCup and Augments in Dysplastic Hip Type 4 Using 3D Printing Technology. J. Orthop. Case Rep. 10 (7), 18–21. doi:10.13107/jocr.2020.v10.i07.1900
Mao, Y., Xu, C., Xu, J., Li, H., Liu, F., Yu, D., et al. (2015). The Use of Customized Cages in Revision Total Hip Arthroplasty for Paprosky Type III Acetabular Bone Defects. Int. Orthop. (SICOT) 39 (10), 2023–2030. doi:10.1007/s00264-015-2965-6
Meneghini, R. M., Meyer, C., Buckley, C. A., Hanssen, A. D., and Lewallen, D. G. (2010). Mechanical Stability of Novel Highly Porous Metal Acetabular Components in Revision Total Hip Arthroplasty. J. Arthroplasty 25 (3), 337–341. doi:10.1016/j.arth.2009.03.003
Mrosek, E. H., Schagemann, J. C., Chung, H. W., Fitzsimmons, J. S., Yaszemski, M. J., Mardones, R. M., et al. (2009). Porous Tantalum and Poly-Epsilon-Caprolactone Biocomposites for Osteochondral Defect Repair: Preliminary Studies in Rabbits. J. Orthop. Res. 28 (2), 141–148. doi:10.1002/jor.20983
Murray, D. W., Fitzpatrick, R., Rogers, K., Pandit, H., Beard, D. J., Carr, A. J., et al. (2007). The Use of the Oxford Hip and Knee Scores. J. Bone Jt. Surg. Br. 89 (8), 1010–1014. doi:10.1302/0301-620x.89b8
Schwartz, B. E., Piponov, H. I., Helder, C. W., Mayers, W. F., and Gonzalez, M. H. (2016). Revision Total Hip Arthroplasty in the United States: National Trends and In-Hospital Outcomes. Int. Orthop. (SICOT) 40 (9), 1793–1802. doi:10.1007/s00264-016-3121-7
Ting-Xian, L., Jin-Long, L., Kai, Z., Qiang, X., Fu-Xing, P., and Zong-Ke, Z. (2017). The Use of Porous Tantalum Augments for the Reconstruction of Acetabular Defect in Primary Total Hip Arthroplasty. J. Arthroplasty 33 (2), 453–459. doi:10.1016/j.arth.2017.09.030
Wang, D., Zhang, H., Sun, S., Zhou, Y., Chen, J., and Hao, L. (2018). Pelvic Height Planning versus Conventional Templating in Preoperative Planning of Acetabulum Cup Size for THA. Acta Orthop. Belg 84 (4), 430
Weeden, S. H., and Schmidt, R. H. (2007). The Use of Tantalum Porous Metal Implants for Paprosky 3A and 3B Defects. J. Arthroplasty 22 (6), 151–155. doi:10.1016/j.arth.2007.04.024
Wei, X., Zhao, D., Wang, B., Wang, W., Kang, K., Xie, H., et al. (2016). Tantalum Coating of Porous Carbon Scaffold Supplemented with Autologous Bone Marrow Stromal Stem Cells for Bone Regeneration In Vitro and In Vivo. Exp. Biol. Med. (Maywood) 241, 592–602. doi:10.1177/1535370216629578
Whitehouse, M. R., Masri, B. A., Duncan, C. P., and Garbuz, D. S. (2015). Continued Good Results With Modular Trabecular Metal Augments for Acetabular Defects in Hip Arthroplasty at 7 to 11 Years. Clin. Orthop. Relat. Research® 473 (2), 521–527. doi:10.1007/s11999-014-3861-x
Xiao, Q., Xu, B., Zhou, K., Ling, T., Yuan, M., Pei, F., et al. (2021). Long-term Results of Combined Porous Tantalum Augments and Titanium-Coated Cups for Paprosky Type III Bone Defects in Acetabular Revision. Int. Orthop. (SICOT) 45 (7), 1699–1706. doi:10.1007/s00264-021-05075-5
Zampelis, V., and Flivik, G. (2020). Custom-made 3D-Printed Cup-Cage Implants for Complex Acetabular Revisions: Evaluation of Pre-planned versus Achieved Positioning and 1-year Migration Data in 10 Patients. Acta Orthop. 92 (1), 23–28. doi:10.1080/17453674.2020.1819729
Zhang, J., Hu, Y., Ying, H., Mao, Y., Zhu, Z., Li, H., et al. (2022). Reliability and Validity Test of a Novel Three-Dimensional Acetabular Bone Defect Classification System Aided With Additive Manufacturing. BMC Musculoskelet. Disord. 23 (1), 432. doi:10.1186/s12891-022-05365-y
Zhang, J. w., Liu, X. l., Zeng, Y. m., Zhai, Z. j., Mao, Y. q., Yu, D. g., et al. (2021). Comparison of 3D Printing Rapid Prototyping Technology with Traditional Radiographs in Evaluating Acetabular Defects in Revision Hip Arthroplasty: A Prospective and Consecutive Study. Orthop. Surg. 13, 1773–1780. doi:10.1111/os.13108
Keywords: revision hip arthroplasty, 3D-printed titanium augment, trabecular tantalum cup, bone defects, rapid prototype
Citation: Kong K, Zhao C, Chang Y, Qiao H, Hu Y, Li H and Zhang J (2022) Use of Customized 3D-Printed Titanium Augment With Tantalum Trabecular Cup for Large Acetabular Bone Defects in Revision Total Hip Arthroplasty: A Midterm Follow-Up Study. Front. Bioeng. Biotechnol. 10:900905. doi: 10.3389/fbioe.2022.900905
Received: 21 March 2022; Accepted: 09 May 2022;
Published: 01 June 2022.
Edited by:
Mika Salmi, Aalto University, FinlandReviewed by:
Johann Henckel, Royal National Orthopaedic Hospital, United KingdomWenbo Mu, First Affiliated Hospital of Xinjiang Medical University, China
Guo-Qiang Zhang, Chinese PLA General Hospital, China
Copyright © 2022 Kong, Zhao, Chang, Qiao, Hu, Li and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiwu Li, aHVpd3UxMjIzQDE2My5jb20=; Jingwei Zhang, emp3X3lzQDE2My5jb20=
†These authors have contributed equally to this work
 Keyu Kong
Keyu Kong Chen Zhao
Chen Zhao Yongyun Chang
Yongyun Chang Hua Qiao
Hua Qiao Yi Hu
Yi Hu Huiwu Li
Huiwu Li Jingwei Zhang
Jingwei Zhang